Abstract
The anatomic single-bundle, all-inside anterior cruciate ligament graft-link technique requires meticulous graft preparation. The graft choice is no-incision allograft or gracilis-sparing, posterior semitendinosus autograft. The graft is linked, like a chain, to femoral and tibial TightRope cortical suspensory fixation devices with adjustable-length graft loops (Arthrex, Naples, FL) in the following manner: the graft is quadrupled, and the free ends are first whip-stitched and then sutured with a buried-knot technique, 4 times through each strand in a loop. The graft is placed on a tensioning station under approximately 20 lb of tension during arthroscopic preparation of the knee and then removed from the tensioner and inserted into all-inside femoral and tibial sockets through the anteromedial arthroscopic portal.
The anatomic single-bundle, all-inside anterior cruciate ligament (ACL) graft-link technique requires a meticulous graft preparation technique. The technique has evolved since the original description.1
No-tunnel, all-inside ACL reconstruction using graft link requires learning advanced graft preparation techniques. “Graft preparation requires consideration of no-incision cosmesis when selecting graft source, ensuring that graft length is less than the sum of socket lengths plus intra-articular graft distance so that the graft will not bottom out in the sockets during final graft tensioning, and learning the graft-link preparation technique.”1
Video 1 illustrates the graft-link graft preparation technique.
Surgical Technique
A graft preparation station facilitates preparation and tensioning of the graft construct (Fig 1). High-strength sutures (No. 0 FiberWire; Arthrex, Naples, FL) secure the graft in a loop. The loop is sewn in linkage with an ACL femoral TightRope cortical suspensory fixation device with adjustable-length graft loop (Arthrex) and an ACL tibial buttonless TightRope (Arthrex) (Figs 2 to 4).
Figure 1.

A graft preparation station facilitates preparation and tensioning of the graft construct. The 2 posts (silver, far left with button-holding post and calibrated tensioner [in pounds and Newtons], and right with suture-holding post) of an ACL graft preparation stand are, respectively, loaded with ACL Femoral TightRope Reverse Tension (white adjustable graft loop on left with silver button in holder and blue passing suture) and ACL Tibial Buttonless TightRope (white larger adjustable loop on right for the Attachable Button System (ABS) with white tensioning sutures on far right). Graft tissue (above) meets preparation specifications including length of no more than 270 mm and diameter (doubled) of no more than 8.5 mm.
Figure 2.
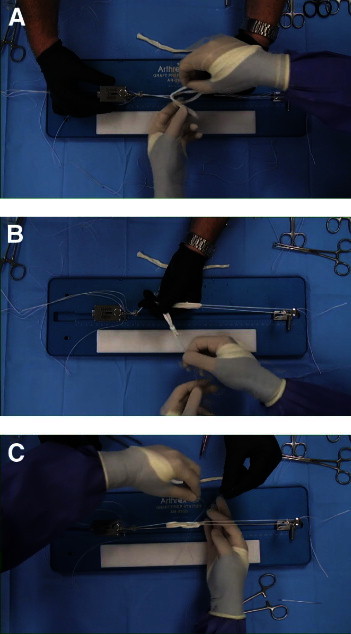
(A) Before the graft (white tissue held in white gloves) is sewn, it must be loaded, looped, in linkage with ACL femoral (left, attached to tensioner) and tibial (right, obscured by white glove) TightRopes. (B) The graft (white tissue) is loaded, quadrupled, in linkage with ACL femoral (left, attached to tensioner, partially obscured by black glove) and tibial (right, attached to suture-holding post) TightRopes, and the free ends of the graft are passed to the same side of the loop (below black glove) so that they may be whipstitched together with No. 2 FiberLoop (blue whipstitch suture tails in white glove). (C) Next, the graft is baseball stitched into the final, quadrupled loop using 4 interrupted, traditional strands of No. 0 FiberWire high-strength suture. Each stitch is passed through each of the 4 strands of graft collagen (white tissue), and the suture free limb is wrapped once around the collagen bundles, creating a self-reinforcing suture noose.
Figure 3.
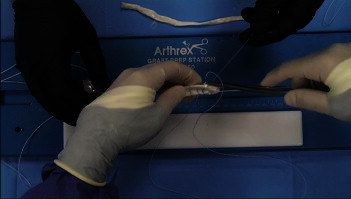
The graft (white tissue) is baseball stitched into the final, quadrupled loop using an interrupted, traditional strand of No. 0 FiberWire high-strength suture (blue suture in free needle). One should note that the central 2 free limbs of the graft have previously been whipstitched with No. 2 FiberLoop (blue suture placed in previously placed rows, below free needle). Each stitch must pass through each strand of graft collagen, and the suture limbs are wrapped once around the collagen bundles, creating a self-reinforcing suture noose when tied. In addition, the central strands are the first sutured, so on completion of the suture noose, the final stitch from peripheral to central (as illustrated) will result in a buried-knot technique. Video 1 provides full details.
Figure 4.
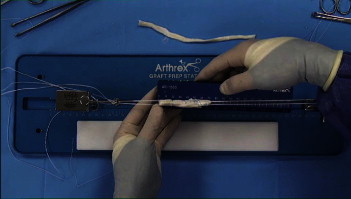
The GraftLink collagen loop (white central tissue) is sewn in linkage with an ACL femoral TightRope adjustable graft loop (white adjustable graft loop on left with silver button in holder and blue passing suture) and ACL Tibial Buttonless TightRope (white larger adjustable loop on right for Attachable Button System with white tensioning sutures on far right). The surgeon holds the graft diameter sizing block measuring one-half–millimeter sizing increments and graft length in mm (shown). Two sutures are placed on the tibial side of the graft and 2 on the femoral side, using a total of 4 interrupted, traditional strands of No. 0 FiberWire high-strength suture. Each of these 4 stitches is passed through each of the 4 strands of graft collagen (white tissue), and the suture free limb is wrapped once around the collagen bundles, creating a self-reinforcing suture noose. The graft, prior to tensioning, should be 50 to 70 mm in length, with a goal of not measuring more than 75 mm after tensioning. A graft-link construct is created, similar to the links in a chain, where a femoral ACL TightRope and tibial ACL TightRope Reverse Tension are linked within each end of the loop.
Graft Length
“An all-inside technique results in sockets, not full bone tunnels. Therefore, to tension the graft, it must not bottom out in the sockets … Graft length must be less than the sum of femoral socket length plus intra-articular graft distance plus tibia socket length.1,2 This prevents bottoming out of the graft in the sockets, preventing graft tensioning. A graft length of no more than 75 mm, after tensioning, is a general guideline (Fig 4), and this distance is adjusted according to patient size.”1
Specifications for graft preparation are summarized in Table 1.
Table 1.
Specifications for Graft-Link Graft Preparation
| Starting length ≤270 mm |
| Final goal length (when quadrupled and tensioned) of 50-75 mm |
| Starting diameter <9 mm doubled |
| Final goal diameter (when quadrupled and tensioned) <12 mm quadrupled |
Graft Selection
Single Semitendinosus
“For autograft, [the authors] recommend the posterior hamstring harvest technique.3 The technique is cosmetic, in keeping with a no-incision philosophy.” In cases where the semitendinosus is short or of inadequate diameter (less than approximately 8 mm)4 when quadrupled, the gracilis can be secondarily harvested.1
Allograft
“Indications for allograft continue to evolve; for proper indications, soft-tissue allograft may also be prepared for graft link as the cosmetic, ‘no-incision' graft choice with no harvest-site morbidity.”1
Graft Linkage
“Before the graft loop is … sewn, it must be loaded (Fig 2), creating links like a chain. [The authors] create a graft-link construct, similar to the links in a chain, where a femoral ACL TightRope and tibial ACL TR-RT [TightRope Reverse Tension, or TightRope ABS (Attachable Button System, the authors preferred technique)] are linked within each end of the loop (Fig 4).”1
Graft Preparation
Graft selection and graft length determination are performed as described earlier.
The 2 posts of an ACL graft preparation stand are, respectively, loaded with ACL Femoral TightRope Reverse Tension and ACL Tibial TightRope for the Attachable Button System (Arthrex) (Fig 1), and the free ends of the graft are passed to the same side of the loop (Fig 2A) so that they may be whipstitched together with No. 2 FiberLoop (Arthrex) (Fig 2B). The graft, prior to tensioning, should be 50 to 70 mm in length, with a goal of not measuring more than 75 mm after tensioning (Fig 4).
Next, the graft is baseball stitched in a loop using a traditional strand of No. 0 FiberWire high-strength suture (Fig 3). Two sutures are placed on the tibial side of the graft and 2 on the femoral side. Each stitch must pass through each strand of graft collagen, and the suture limbs are wrapped once around the collagen bundles, creating a self-reinforcing suture noose when tied. In addition, the central strands are the first sutured, so on completion of the suture noose, the final stitch from peripheral to central will result in a buried-knot technique (Fig 3).
Marking the Graft
“The first distance that should be measured and marked on the graft-link construct is the femoral interosseous distance (flip-distance). This distance should be marked on the adjustable graft loop (suture material), measuring from the tip of the cortical suspensory button, while the surgeon holds the button in a ‘pre-flipped' position. During graft passage, when the mark on the adjustable graft loop reaches the femoral socket orifice, this indicates to the surgeon that the button is in position to flip.
The second distance that should be measured and marked on the graft-link construct is the length of collagen to be placed within the femoral socket. The goal is to maximize collagen in the socket but ensure that the graft is not bottoming out during tensioning, and to allow adequate length of graft tissue remaining to traverse the intraarticular distance, and to adequately fill the tibial socket. A typical amount of collagen in the femoral socket is 25 mm. This distance is marked on the graft itself, measuring from the femoral graft end. During graft passage, when the mark on the graft itself reaches the femoral socket orifice, this indicates to the surgeon that femoral graft tensioning is complete. This is repeated for the tibial side of the graft.”
The graft-link technique is then performed as has been previously described and illustrated.1
Summary
The anatomic single-bundle, all-inside ACL graft-link technique requires meticulous graft preparation. Before preparation, suturing, and tensioning, graft specifications are as follows: no greater than 270 mm in length and no greater than 8.5 mm in diameter doubled. The graft choice is no-incision allograft or gracilis-sparing, posterior semitendinosus harvest. The graft is linked to femoral and tibial adjustable TightRope graft loops and is first quadrupled with the free ends whipstitched and then sutured 4 times through each strand with a wrapped stitch to an ultimate graft length of no greater than 75 mm after tensioning at 20 lb (Fig 4).
Footnotes
The author reports the following potential conflict of interest or source of funding in relation to this article: Arthrex.
Supplementary data
ACL graft-link graft preparation technique.
References
- 1.Lubowitz J.H., Amhad C.S., Anderson K. All-inside anterior cruciate ligament graft-link technique: Second-generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:717–727. doi: 10.1016/j.arthro.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 2.Lubowitz J.H. No-tunnel anterior cruciate ligament reconstruction: The transtibial all-inside technique. Arthroscopy. 2006;22:900.e1–900.e11. doi: 10.1016/j.arthro.2006.06.003. www.arthroscopyjournal.org [DOI] [PubMed] [Google Scholar]
- 3.Prodromos C.C., Han Y.S., Keller B.L., Bolyard R.J. Posterior mini-incision technique for hamstring anterior cruciate ligament reconstruction graft harvest. Arthroscopy. 2005;21:130–137. doi: 10.1016/j.arthro.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 4.Magnussen R.A., Lawrence J.T.R., West R.L., Toth A.P., Taylor D.C., Garrett W.E. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28:526–531. doi: 10.1016/j.arthro.2011.11.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ACL graft-link graft preparation technique.


