Abstract
Capsulotomy, which is commonly performed in hip arthroscopy, assists visualization and instrument navigation. Despite the necessity, the optimal technique, amount of resection, and indications for capsulotomy remain unknown. Capsular repair is increasingly considered because of concerns raised about the long-term effects of extensive capsulotomies and reports of devastating postoperative side effects. It was recently recommended that any patient undergoing hip arthroscopy with a large capsular defect or ligamentous laxity should be considered for capsular repair and/or plication. We present a novel technique for capsular repair using the SpeedStitch device (ArthroCare, Austin, TX), originally designed for shoulder rotator cuff repair. This capsular repair technique has proven to be easy, fast, and reproducible. If performed in the correct manner, this technique has the potential to preserve the anatomy and integrity of the iliofemoral ligament and reduce the rates of postoperative instability and pain.
Hip arthroscopy is a surgical treatment technique that commonly addresses intra-articular cartilage and labral pathologies. Surgical management of the hip capsule during the procedure is critical and must allow improved exposure without compromising stability. Hip joint stability is determined by static (osseous, labral, and capsuloligamentous) and dynamic (neuromuscular and adhesional forces) factors.1-3 Understanding of the hip capsuloligamentous complex and its importance with regard to hip stability, postoperative function level, and pain continues to grow.4,5 Although capsulotomy is commonly performed in hip arthroscopy and assists visualization and instrument navigation, the optimal technique, amount of resection, and indications for capsular repair remain unknown.6 Described approaches have included capsulectomy, limited capsulotomy, extensile capsulotomy, capsular plication, and capsular shift.7
Capsular repair is increasingly considered because of concerns raised about the long-term effects of extensive capsulotomies and reports of devastating postoperative side effects.1-3 As a result, it has been recommended that any patient undergoing hip arthroscopy with a large capsular defect or ligamentous laxity should be considered for capsule repair and/or plication.4 Many centers are now performing routine capsular repair at the conclusion of procedures where capsulotomy has been performed. We present a novel technique for capsular repair using the SpeedStitch (SS) device (ArthroCare, Austin, TX) originally designed for shoulder rotator cuff repair. Over the past 2 years, this method has proven useful; being easier, faster, and reproducible in our hands.
Technique
Hip arthroscopy is performed in a routine manner using standard portals. Central and peripheral compartment work is completed with the assistance of a “trapdoor” capsulotomy. Confirmation of the required resection is obtained through fluoroscopy and visual dynamic assessment by impingement test. The anterior aspect of the capsulotomy, where the iliofemoral ligament (IFL) was compromised, is recognized before the conclusion of the procedure. At the end of the hip arthroscopy work, the operated limb is brought back to a neutral hip position while no traction, flexion, or rotation is applied. Approximation of both sides of the capsule is confirmed, ensuring that anatomic side-to-side reduction (or plication, if needed) can be achieved and determining the point of entry for next-stage suture penetration.
The SS is loaded with a suture cartridge (MagnumWire; ArthroCare) and inserted through the anterolateral portal while an arthroscopic view is obtained from the midtrochanteric or parallel posterior portal (Figs 1 and 2, Video 1). The SS grabs the proximal (medial) capsular stump with a sufficient bite of tissue to allow strong knot tying and avoiding possible suture cut-through. The SS is pulled out of the joint, and a knot pusher and “suture clip” are placed on the “needle-retrieved” (short) side of the suture. The free side of the suture is then reloaded on the SS, and the device is reinserted into the joint through the same portal. Caution should be taken to enter along the exact same (first) stitch tract. Alternatively, one can use a slotted cannula to eliminate soft-tissue entrapment between both suture ends. The SS is then used to grab the corresponding side of the capsular stump, just opposite of the previously applied suture end. After penetrating this distal (lateral) side of the capsule, the SS is pulled out and the side-to-side stitches are retrieved and tied in a standard fashion. The process can be repeated until adequate capsular closure and tension have been obtained to the surgeon's satisfaction.
Figure 1.
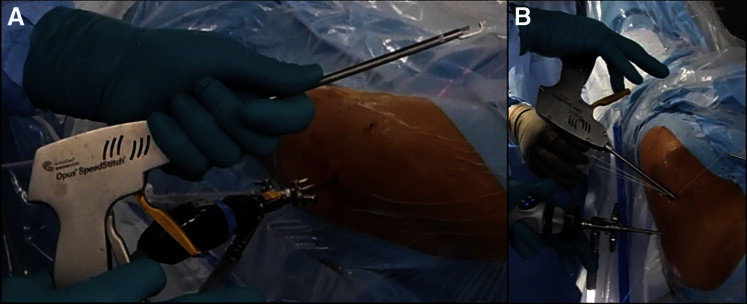
(A) SS device. (B) Management is performed with a single hand and is straightforward. It should be noted that a stay suture comes out through each of the 2 portals. These sutures are used in the corners of the trapdoor capsulotomy for retraction and improved visualization of the femoral neck.
Figure 2.
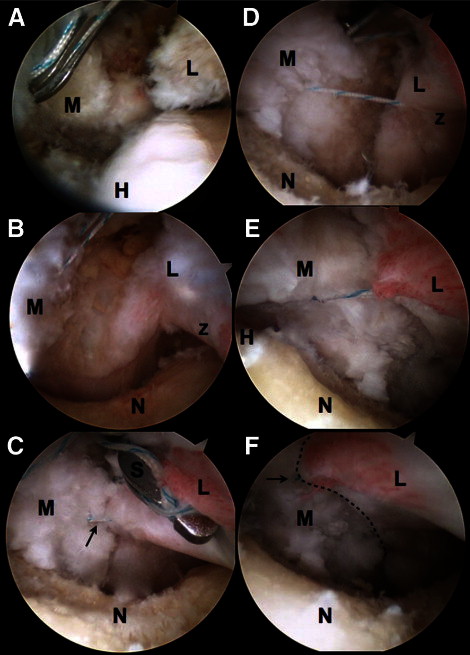
The peripheral compartment of the right hip after cam resection is completed and capsular repair is obtained. The camera is positioned at the anterolateral portal under the capsule. Repair work, as shown, is performed through an anterolateral portal in an “inside-out” manner. (A) The SS is grasping the medial capsule stump overlying the labrum and passing a suture with a “good enough” bite of tissue. (B) The SS is pulled out of the joint to reload with the “free” side of the suture. The medial capsule suture can be seen on the left. (C) The SS is brought back into the joint to pass the “other” side of the suture through the corresponding lateral (L) side of the capsule. The first capsular repair stitch can be seen in the background (arrow). (D) Arthroscopic knot tying is performed, bringing both medial and lateral capsule stumps together. A knot pusher can be seen (inside-out view) at the upper part of the picture. (E) Capsular stumps are now approximated and tied. (F) The dashed line presents the capsular repair line. A capsular repair stitch can be seen (arrow): 2 to 3 consecutive stitches commonly are used to repair the anterior and mid part of the “trapdoor” capsulotomy (which runs diagonally, lateral from the anterior extension of the intraportal capsulotomy), corresponding with the IFL. (H, femoral head; L, lateral capsule stump; M, medial capsule stump; N, femoral neck; S, SpeedStitch; Z, zona orbicularis.)
We have also been using the same device to repair and reconstruct the labrum during hip arthroscopy and to apply traction sutures to the capsule (Fig 3, Video 1). For capsular traction, sutures to the capsule are placed through both arthroscopy portals at the beginning of the surgical procedure, just after intraportal capsulotomy is achieved. By use of this method, damage to the soft tissues surrounding the portals, particularly muscle damage, is minimized with each passage of instruments. Changing leg position does not present a problem of losing the tract through the muscle mantle because the original tract is maintained by the portal capsular suture. Furthermore, the traction suture can serve as a “pseudo slotted cannula” whereby instruments can be shuttled along the suture into the joint. Elevating the capsule from the femoral head using the traction (stay) suture keeps the radiofrequency device, or blade, away from the femoral head during the cutting process. Finally, capsulotomy size can also be reduced using traction sutures, because increased visualization is achieved when the assistant is pulling on the sutures (Table 1).
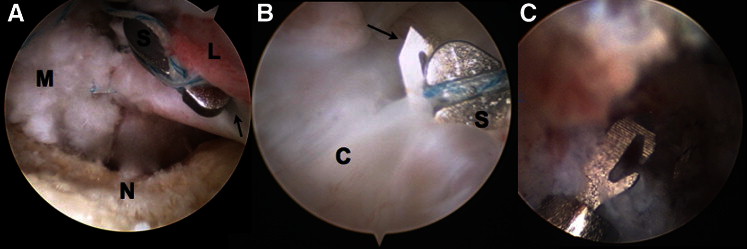
Figure 3.

Central-compartment labral repair in a left hip. The camera is positioned at the anterolateral portal. SS and anchoring work is performed through an anterolateral portal. (C, capsule; H, femoral head; S, SpeedStitch.) (A) The SS is being positioned between the labrum (asterisks), which was taken down for rim trimming, and the acetabular rim. The surgeon judges the point where he or she wants to penetrate with the suture to achieve optimal fixation. (B) The labrum is then being grasped by the SS from both sides, so a very accurate and controlled suture penetration can be achieved, without “pushing” it further down into the joint or scratching the femoral head with the penetrating device. (C) The SS is retrieved out of the joint, all in a quick single step. (D) The suture is then used to refix the labrum using a knotless anchor. (The dashed arrow shows the anchor tip, and the dashed circle shows the anchor-drilled hole.) (E) According to surgeon preference, the suture can also be placed around the labrum (not through the labral tissue). (F) Labral reconstruction with ITB autograft (right hip, same portals as described earlier). When the labrum is to be refixated without a complete takedown (separation of labrum from rim), the SS can penetrate it from the “joint side” (in this case, however, suture retrieval should follow, to prevent labral eversion). (Cr, cartilage [acetabular cartilage]; ITB, ilio tibial band; R, rim [acetabular rim].)
Table 1.
Advantages of SS for Hip Arthroscopy
| Capsular repair |
| • Can grasp tissue (capsule or labrum) that lays 90° to the line of the portals and work |
| • Very easy and fast to operate |
| • Enables manual reloading (in a few seconds) of the “free” side of the stitch and reapplying it to the corresponding side of the capsule (so a continuous repair can be achieved) |
| • Enables an “inside-out” capsular repair without the need for extended extracapsular soft-tissue trimming (of the iliocapsularis) |
| Capsular traction |
| • Enables the fast placement of capsular traction (stay) suture in the beginning of the procedure (even before intraportal capsulotomy) when the view is minimal and no other device, such as a suture penetrator, can achieve this goal |
| Labral repair |
| • Grasping the labrum before penetrating it with a stitch will enable a very accurate and controlled positioning of this stitch |
| • No need to duck dive into the joint to retrieve the suture because both sides come out in 1 shot (camera can stay in 1 spot and free surgeon's hand) |
| • When dealing with a small weak labrum that dictates an “around-the-labrum” suture-passing method, the SS can achieve that in 1 quick step, eliminating the need for the common “pass under and fish for” technique |
Discussion
Capsular management during hip arthroscopy is important to allow for complete exposure of both central and peripheral compartments. Inadequate capsulotomy frequently contributes to inadequate correction and failure to achieve preplanned surgery goals. On the other hand, capsular management must not compromise postoperative hip stability and kinematics. Repair of the compromised IFL may be of critical importance during hip arthroscopy, particularly for patients with hyperlaxity, anterior instability, and/or dysplasia.7 The iatrogenic compromised integrity of this ligament may result in pain or instability in certain terminal positions of hip range of motion. Several case reports recently reported on postoperative hip instability after arthroscopy.1-3
Various capsulotomy and capsular repair techniques have been described. The commonly used intraportal capsulotomy allows controlled and precise resection of the extra-articular side of the labrum and rim, all under direct vision. The intraportal capsulotomy also assists in protecting the periarticular soft tissues during labral repair and confirming a safe trajectory for anchor drilling and placement. Bedi et al.7 recently recommended the T-shaped capsulotomy for peripheral compartment work. They showed how this technique provides an excellent view of the head-neck junction as distal as the intertrochanteric line. The T-shaped capsulotomy can then be easily repaired with side-to-side stitches, achieving an anatomic restoration of the IFL.7 The technique used to repair the capsule was initially based on a suture-passer device applied through the distal anterolateral portal and a tissue penetrator applied through the proximal anterolateral portal.7 Anatomic side-to-side stitches are placed from distal to proximal until a complete closure is achieved.7 This side-to-side technique can be applied to various capsulotomies and is very similar to the repair technique used in shoulder surgery. However, we have tried this method and found it cumbersome and time-consuming and have found that it requires many steps including numerous suture-shuttling stages. There is also a need to replace the polydioxanone used by the suture passer with a stronger braided and permanent stitch, because the latter is not compatible with the suture-passer device. Moreover, the side-to-side repair technique is an “outside-in” technique, meaning a good view of the capsule must be obtained from “above” the capsule (outside). To achieve this view, an extended extracapsular soft-tissue (i.e., iliocapsularis) trimming must precede the repair.
Our described technique using the SS is an “inside-out” technique. Similar to the method described by Bedi et al.,7 the SS technique can be performed with every type of capsulotomy, regardless of direction (T shaped, interportal, or trapdoor) or extent. The SS can be used when the view is obtained from underneath or in line with the capsule, which eliminates the need for excessive extracapsular soft-tissue shaving. The unique design of the SS also enables an easy grasp of the capsule stump, which is horizontal to the line and direction of the portal and device entry. That is opposite to subacromial rotator cuff work where the torn cuff tendon is in line (continuous) with the grasping suture-penetrating device, used from the lateral portal. The SS has the ability to grasp, stabilize, and then place a braided stitch within the capsule or labrum all in 1 step. To our knowledge, no other device in hip arthroscopy has the capability to conduct this sequence in a quick, single step.
Nevertheless, the SS in its current form has a limitation. We have found some scenarios where the capsule was, presumably, too thick for the device's needle to penetrate through and several attempts were needed to achieve a suture pass (Fig 4). This is most likely because of the small needle, which was designed for work in the shoulder, with thinner tissue. In addition, at times, the cartridge itself might “stick” in the soft tissue and come off the SS gun. (The cartridge is long, so its proximal end will always stay out of the joint.) The cartridge can then be retrieved easily by rotating it clock and counterclockwise, to release the needle grab. This seems to be because of undersized “wings,” which secure the disposable cartridge to the SS gun.
Figure 4.
Several pitfalls of the technique should be noted. Often, when the capsular tissue is very thick, the needle will not be able to penetrate through and grasp the stitch with it, resulting in a need for multiple attempts. At times, when “releasing” the needle, it may stay “stuck” in the thick capsular tissue, and when pulling the SS out of the joint, the cartridge may come off the SS. The cartridge can then be retrieved easily by rotating it clockwise and counterclockwise, to release the needle grab. (A) The SS is grasping the lateral capsule stump, passing a suture with a “good enough” bite of tissue. (B) The needle of the SS is seen passing through to the other side of the capsule tissue. The surgeon now releases the SS handle, and the needle will be drawn back, taking the loaded stitch with it, to the other side of the capsule. (C) Close-up view of the needle showing the recess designed to grab the stitch. If this recess is filled/blocked with soft tissue, the needle would not be able to grab the stitch, resulting in a failed attempt.
We have described an easy, fast, and reproducible sequence of capsular repair using a shoulder device known as the SpeedStitch. This technique, if performed in a correct manner, has the potential to preserve the anatomy and integrity of the IFL and reduce rates of postoperative instability and pain.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary data
References
- 1.Matsuda D.K. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy. 2009;25:400–404. doi: 10.1016/j.arthro.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 2.Benali Y., Katthagen B.D. Hip subluxation as a complication of arthroscopic debridement. Arthroscopy. 2009;25:405–407. doi: 10.1016/j.arthro.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 3.Mei-Dan O., McConkey M.O., Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic instability: Can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy. 2012;28:440–445. doi: 10.1016/j.arthro.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 4.Shu B., Safran M.R. Hip instability: Anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med. 2011;30:349–367. doi: 10.1016/j.csm.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 5.Telleria J.J., Lindsey D.P., Giori N.J., Safran M.R. An anatomic arthroscopic description of the hip capsular ligaments for the hip arthroscopist. Arthroscopy. 2011;27:628–636. doi: 10.1016/j.arthro.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Myers C.A., Register B.C., Lertwanich P. Role of the acetabular labrum and the iliofemoral ligament in hip stability: An in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39(Suppl):85S–91S. doi: 10.1177/0363546511412161. [DOI] [PubMed] [Google Scholar]
- 7.Bedi A., Galano G., Walsh C., Kelly B.T. Capsular management during hip arthroscopy: From femoroacetabular impingement to instability. Arthroscopy. 2011;27:1720–1731. doi: 10.1016/j.arthro.2011.08.288. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


