Abstract
We present our novel arthroscopic anatomic double-bundle coracoclavicular ligament reconstruction technique using a semitendinosus tendon autograft. The dorsal limb of the graft is positioned around the dorsal edge of the clavicle, re-creating the conoid ligament. The anterior limb proceeds superiorly and re-creates the trapezoid ligament. The solution effectively stabilizes the acromioclavicular joint and prevents anterior posterior translation. This new arthroscopic double-bundle coracoclavicular joint reconstruction is an effective and reliable method in stabilizing the clavicle and neutralizing the anterior-posterior translation, and we find it to be technically practical for the surgeon.
Dislocation of the acromioclavicular (AC) joint is a common injury, especially in contact sports. Frequently, the treatment is conservative, especially in types I and II dislocations, in which the joint is typically stable. In types III, IV, and V dislocations, the instability of the distal clavicle, pronounced superiorly raised clavicular head, and pain may cause problems. The anterior-posterior translation of the clavicle on movement and rotation of the arm are often the most prevalent symptoms. Numerous arthroscopic techniques for coracoacromial ligament reconstructions can be found in the literature. Some of these techniques are based on the Weaver-Dunn technique or its modifications.1-3 A number of arthroscopic reconstructions using hamstring graft have been described.4,5
Our arthroscopic technique is anatomically accurate because it uses a double-bundle coracoclavicular ligament reconstruction with a semitendinosus autograft. The anterior limb of the graft is fixed to the middle of the clavicle, re-creating the trapezoid ligament. The posterior limb is wrapped around the posterior edge of the clavicle, re-creating the conoid ligament. Reconstruction of both limbs prevents the clavicle from lifting superiorly. More importantly, the posterior limb effectively prevents the clavicle from translating posteriorly (Fig 1). The goal was to minimize the risk of fracture of the clavicle. Therefore only a single drill hole in the clavicle was used. A further aim was to use a bony tunnel in the coracoid that was as small as possible.
Figure 1.

The semitendinosus graft first runs through the clavicular and coracoid drill holes; turns up, around the dorsal edge of the clavicle; and runs again through the clavicular drill hole. Right shoulder, anteromedial view.
Technique
A newly created fixation device was used. The device comprised a GraftWasher (Arthrex, Naples, FL) on the clavicle and a BicepsButton (Arthrex) inferiorly on the coracoid. The washer and the button were attached to one another with No. 5 FiberWire (Arthrex). The fixation device and the graft shared the same bony tunnels in the coracoid as well as in the clavicle (Fig 2). The tunnel was 6 mm in the clavicle and 4.5 mm in the coracoid.
Figure 2.
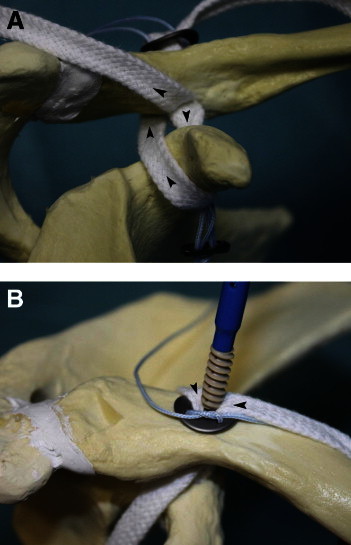
(A) Alignment of graft and fixation apparatus shown anteriorly in right shoulder. (B) A 5.5-mm polyether ether ketone interference screw is inserted to fix the graft limbs into the clavicular drill hole in a right shoulder. The arrowheads indicate the direction of the graft.
The patient is placed in the beach-chair position. The semitendinosus tendon graft is harvested from the ipsilateral leg. The graft thickness is measured and adjusted if needed. A passing suture is fixed in 1 end of the graft. The fixation apparatus, comprising the GraftWasher, the BicepsButton, and a No. 5 FiberWire, is assembled. A No. 2 FiberWire passing suture is added to the distal button. Five portals are made: posterior, lateral, anterosuperior, anterior, and clavicular portal/incision. The 2-cm clavicular incision is made on the dorsal edge of the clavicle. A standard 30° arthroscope is used. The primary camera positions are in the lateral or anterolateral portal. The operational field around the clavicle is marked with 2 needles to optimize the directions of the instruments and the position of the clavicular opening. Debridement is performed and sufficient exposure is obtained around the coracoid process and the clavicle. First, a 4.5-mm hole is drilled through the clavicle and the coracoid by use of conventional drill guides for this purpose. Then, the clavicular drill hole is enlarged to 6 mm. The cortex of the dorsal edge of the clavicle is roughened with a file to enhance the attachment of the dorsal graft limb. The passing sutures for both the graft and the fixation apparatus are positioned in their bone tunnels by the lasso technique.
The graft is first pulled through the clavicular and coracoid drill holes to the anterolateral portal. The end of the distal limb is then pulled from the anterolateral portal to the clavicular portal behind the clavicle. The distal button is passed through the drill holes into its position under the coracoid. The end of the dorsal limb is slipped through the GraftWasher and then into the clavicular drill hole adjacent to the anterior graft limb and is then drawn to the anterolateral portal. With the entire length of the graft in place, the temporary fixation system is tightened concurrently with tensioning of the graft. The posterior limb is tensioned by pulling horizontally from the anterolateral portal. The anterior limb is tensioned by pulling directly superior. When the clavicle has been repositioned and both the apparatus and the graft have been tensioned, the No. 5 sutures of the apparatus may be tied. Finally, the graft tension is checked by pulling the ends of the graft. The graft is fixed to the clavicular tunnel with a 5.5-mm × 8- to 10-mm polyether ether ketone interference screw. The excess graft ends are removed. The arthroscopic portals are closed with interrupted sutures while the clavicular wound is closed in layers (Figs 3 and 4). The mean operation time is 1.5 hours (Video 1).
Figure 3.
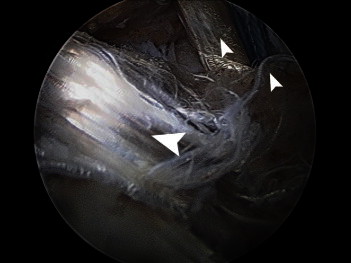
Finished double-bundle reconstruction of right shoulder seen from lateral portal. The anterior limb is seen to the right with the No. 5 FiberWire sutures (small arrowheads). The dorsal limb is seen to the left (large arrowhead).
Figure 4.

The postoperative radiograph of the right shoulder shows the reduced clavicle, the GraftWasher on the clavicle, and the BicepsButton under the coracoid.
So far, surgery has been performed in 14 patients (12 men and 2 women). The age of the patients at the time of surgery varied between 18 and 64 years (mean, 39 years). The dislocations were of types III, IV, and V. Of the cases, 8 were considered chronic and 6 were acute.
The coracoclavicular ligament reconstruction patients are followed up at the outpatient clinic at 2 and 4 weeks and thereafter at 3, 6, and 12 months after surgery. In this group, early recovery has been good and postoperative pain has been mild. None of the reconstructions have failed, and no fractures have occurred. All clavicles have remained stable, and the preoperative pathologic anterior-posterior translation has not recurred. There have been no infections.
In this series the first results of the operation were evaluated 6 months after the operation. The outcomes of the operation were divided into 4 categories: excellent, good, fair, and poor. The outcome was considered excellent if the patient was able to return to work or sports with no difficulty, had normal range of motion of the arm with no restrictions, and subjectively considered the outcome excellent. The result was regarded as good if the range of motion was full but there was still some stiffness, if the patient had occasional pain using the arm, or if a small bump (<10 mm) remained in the AC joint. The outcome was considered fair if there was a bump (>10 mm) remaining in the AC joint and the patient had frequent pain in the AC joint. If the stabilization of the clavicle failed, the outcome was considered poor. Preliminary patient outcomes were identified at 6 months postoperatively. In 6 patients the outcome was excellent. In 1 patient the outcome was determined to be good. In 1 patient the outcome was judged fair because there was persisting pain in the AC joint. Six patients are still in the early phase of recovery.
Postoperatively, the patients use a gunslinger brace for 4 weeks. The patients are allowed to flex and extend the elbow. Light waistline movements are also allowed within the limits of pain. Rehabilitation is started 4 weeks after surgery with gentle passive exercises. At 8 weeks, free range of motion is allowed. Returning to contact sports, such as ice hockey, is permitted after 6 months.
Discussion
An abundance of operative methods have been proposed to solve the problem of AC joint dislocation. Some arthroscopic techniques do not include a ligamentous reconstruction. These techniques are mostly used in acute cases in which the coracoclavicular ligament complex is expected to heal after reduction has been achieved.6,7 Anatomic reconstructions have been shown to provide stable solutions regarding anterior and posterior translation.8 Many of the reconstructions using a semitendinosus graft use 2 or more drill holes in the clavicle, thereby increasing late fracture risk from an impact to the clavicle. On the other hand, some techniques can produce a large coracoid drill hole (up to 6 mm), which may also impair the strength of the bone.
The unique aspect of our technique is the position of the dorsal limb of the graft around the dorsal edge of the clavicle reconstructing the conoid ligament. The anterior limb projects superiorly and replaces the trapezoid ligament. A significant advantage is that there is only one 6-mm drill hole in the clavicle and a 4.5-mm drill hole in the coracoid. An additional advantage is that the temporary fixation apparatus uses the same drill holes. These drill holes are the smallest possible if a distal button fixation and semitendinosus graft are used. A further advantage of the technique is that there are bony channels on both sides of the reconstruction. Tunnel widening of the clavicular drill hole may become a problem long-term. However, when one is using the GraftWasher on the clavicle, the titanium edge—where the dorsal limb turns down to the bone channel—may prevent erosion of the edge of the drill hole. The washer also proved to be a very practical solution to combine the temporary fixation and the graft into the same bony channels.
An all-arthroscopic double-bundle coracoclavicular joint reconstruction is an effective and reliable method in stabilizing the clavicle and neutralizing the anterior-posterior translation, and we find it to be technically practical for the surgeon.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary data
References
- 1.Boileau P., Jason O., Gastaud O., Brassart N., Roussanne Y. All-arthroscopic Weaver-Dunn-Chuinard procedure with double-button fixation for chronic acromioclavicular joint dislocation. Arthroscopy. 2010;26:149–160. doi: 10.1016/j.arthro.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 2.Carofino B.C., Mazzocca A.D. The anatomic coracoclavicular ligament reconstruction: Surgical technique and indications. J Shoulder Elbow Surg. 2010;19:37–46. doi: 10.1016/j.jse.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 3.Tauber M., Gordon K., Koller H., Fox M., Resch H. Semitendinosus tendon graft versus a modified Weaver-Dunn procedure for acromioclavicular joint reconstruction in chronic cases: A prospective comparative study. Am J Sports Med. 2009;37:181–190. doi: 10.1177/0363546508323255. [DOI] [PubMed] [Google Scholar]
- 4.Garcia J.C. Arthroscopic Weaver-Dunn procedure: Surgical technique. Tech Shoulder Elbow Surg. 2010;11:41–43. [Google Scholar]
- 5.DeBerardino T.M., Pensak M.J., Ferreira J., Mazzocca A.D. Arthroscopic stabilization of acromioclavicular joint dislocation using the AC graftrope system. J Shoulder Elbow Surg. 2010;19:47–52. doi: 10.1016/j.jse.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 6.Walz L., Salzmann G.M., Fabbro T., Eichhorn S., Imhoff A.B. The anatomic reconstruction of acromioclavicular joint dislocations using 2 TightRope devices: A biomechanical study. Am J Sports Med. 2008;36:2398–2406. doi: 10.1177/0363546508322524. [DOI] [PubMed] [Google Scholar]
- 7.Lim Y.W., Sood A., van Riet R.P., Bain G.I. Acromioclavicular joint reduction and reconstruction using metallic buttons—Early results and complications. Tech Shoulder Elbow Surg. 2007;8:213–221. [Google Scholar]
- 8.Mazzocca A.D., Santangelo S.A., Johnson S.T., Rios C.G., Dumonski M.L., Arciero R.A. A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med. 2006;34:236–246. doi: 10.1177/0363546505281795. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


