Abstract
Tenodesis is an accepted treatment option in the management of pathology involving the long head of the biceps (LHB). Among the common causes for revision surgery after tenodesis are residual pain within the bicipital groove, cramping, early biceps fatigue, and biceps deformity. Most technical descriptions of arthroscopic biceps tenodesis involve fixation of the LHB tendon within or proximal to the intertubercular sulcus and thus fail to address the described sources of pain within this proximal anatomic location. Suprapectoral tenodesis offers the surgeon the ability to remove the LHB from within the bicipital groove by fixating the biceps more distally. Cramping, early fatigue, and biceps deformity have been described when the appropriate length-tension relation of the biceps tendon has not been restored after LHB tenodesis. Our described procedure allows for a more consistent restoration of the anatomic length-tension relation of the LHB, therefore reducing the symptoms associated with this variable. This all-arthroscopic, suprapectoral biceps tenodesis with interference fixation addresses the most common causes for revision surgery and offers a comprehensive solution for LHB pathology.
Lesions of the long head of the biceps (LHB) are commonly encountered during shoulder arthroscopy. When these lesions are symptomatic, biceps tenodesis is an accepted treatment option. Several different techniques for tenodesis of the LHB have been described.1-3 Although evidence exists that tenodesis of the diseased tendon can improve patient symptoms, consensus is lacking regarding the method to perform this procedure. Some authors describe an intra-articular method of tenodesis; others advocate an extra-articular approach.1-5 Several surgeons describe an arthroscopic method, whereas others prefer an open technique.1,3-5 Even the fixation types vary widely. Some authors advocate soft-tissue fixation, whereas others describe suture anchors or interference screws for fixation.1-3,6,7 Also controversial is the appropriate location along the proximal humerus at which to perform this procedure, with some surgeons preferring a proximal location and others describing a more distal site.1-3
Somewhat lost in the midst of these technical considerations has been the importance of re-establishing the appropriate length-tension relation of the LHB. With under-tensioning of the LHB, the procedure may result in a persistent biceps deformity, early muscle fatigue, and subjective cramping.8,9 With over-tensioning of the LHB, the pullout forces at the site of tenodesis increase, potentially leading to fixation failure (Table 1). In our experience with tenodesis, it has been this length-tension relation that has been most challenging to reproduce with arthroscopic techniques. Whereas open tenodesis procedures (such as the popular subpectoral technique) have the benefit of referencing the LHB musculotendinous junction to the inferior border of the pectoralis major tendon, arthroscopic techniques do not provide for visualization of this relation. Some authors have described procedures that externalize the LHB to gain control of the free end; however, we believe that this can make restoration of the LHB tension all the more difficult, given the displacement of the tendon during externalization.
Table 1.
Common Causes for Revision After Biceps Tenodesis
| • Failure of fixation |
| • Residual pain in intertubercular sulcus |
| • Inadequate restoration of length-tension relation |
We describe a method of LHB tenodesis that is entirely arthroscopic and does not require externalization of the LHB. Furthermore, we believe that this unique approach and the site of tenodesis described in this technique will allow the surgeon to more consistently restore the anatomic length-tension relation of the LHB.
Surgical Technique
Pathology of the LHB is rarely encountered as a sole entity. Therefore a patient position allowing surgical arthroscopy of the glenohumeral joint and the subacromial space should be used. Our preferred patient position is a beanbag-supported lateral decubitus position with the affected arm in balanced suspension. The procedure is performed with the patient under general anesthesia, and an interscalene block is often used. The arm is suspended in approximately 30° of abduction, 15° of forward flexion, and neutral rotation. Preoperative antibiotics are administered, and a “time out” is performed by the surgical team.
Diagnostic Arthroscopy
A standard viewing portal is established 1 cm distal to the posterolateral border of the acromion. A working portal is established 1 cm distal to the acromioclavicular joint and through the rotator interval. Diagnostic evaluation of the glenohumeral joint is performed with a standard 30° arthroscope, and fluid pressure is established through gravity.
The intra-articular portion of the LHB is inspected for partial tearing or degenerative fraying that is often obvious on initial inspection. Some lesions of the LHB, however, are less obvious. The biceps anchor's insertion onto the supraglenoid tubercle must be assessed with a probe because labral separation may be exacerbated through the deforming contractile force of the LHB. The arm should be internally and externally rotated to evaluate for medial subluxation of the tendon. Among the restraints to medial subluxation of the LHB are the superficial and deep insertions of the subscapularis, the coracohumeral ligament, and the superior glenohumeral ligament. Subluxation is often due to a disruption to 1 of the soft-tissue restraints to the LHB in its sulcus. Often, the intra-articular portion of the LHB will appear healthy. For this reason, a probe, placed through a rotator interval portal, is used to pull the LHB into the glenohumeral joint (Fig 1). Often, the portion of the LHB within the intertubercular groove is pathologic and tenosynovitis is encountered.
Figure 1.
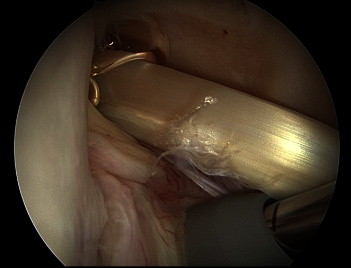
LHB tendon with a longitudinal split tear within the biceps groove in a left shoulder viewed from the standard posterior portal. This lesion was not identified until the tendon was pulled into the glenohumeral joint.
Once the decision to perform tenodesis of the LHB has been made, a spinal needle is used to pierce the intra-articular portion of the tendon through the rotator interval. The LHB is then released proximal to the spinal needle by use of electrocautery (Fig 2). The spinal needle keeps the LHB from retracting distally when its origin is released at the superior labrum and therefore maintains the anatomic length-tension relation of the muscle-tendon unit until the surgeon performs the tenodesis (Video 1).
Figure 2.

LHB tendon stabilized with a spinal needle before release with electrocautery in a right shoulder viewed from the standard posterior portal.
Portals and Visualization
Arthroscopic suprapectoral tenodesis is initiated with the addition of 2 portals. Because neither of these portals is used as part of our standard arthroscopy, we prefer to complete any intra-articular procedure (including tenotomy of the LHB in preparation for later tenodesis) before establishing the new portals.
The first (viewing) portal is created between the anterior and middle heads of the deltoid muscle adjacent to the anterolateral edge of the acromion. The arthroscopic trocar is directed underneath the deltoid fascia and parallel to the long axis of the humerus. The subdeltoid fascia is gently swept to create space.
The second (working) portal is then established in the sagittal plane of the lateral acromial edge and 4 cm distal to the viewing portal. The portal should correspond to the superior edge of the sternal head of the pectoralis major insertion. Until the surgeon develops a comfort level with this portal, we recommend localizing its position under direct visualization using a spinal needle. A 5-mm cannula is then inserted, and a 4.0-mm arthroscopic shaver is used to debride the clavipectoral fascia (Fig 3). An underwater electrosurgical pencil (Megadyne, Draper, UT) can be used to cauterize the fascia before debridement to minimize bleeding.
Figure 3.

The surgeon's right hand is directing the arthroscope through the viewing portal parallel to the long axis of the humerus in a left shoulder in the lateral decubitus position. The surgeon's left hand is controlling electrocautery through the working (transdeltoid) portal.
The falciform ligament of the pectoralis tendon is important to identify in this region, because it is a landmark beneath which the LHB can be found. Arthroscopically, this structure can be identified by the intersection of the transverse fibers of the pectoralis fascia with the longitudinal fibers of the biceps sheath (Fig 4). Once recognized, the ligament is released with controlled electrocautery exposing the underlying LHB. A small ascending branch from the anterior humeral circumflex vessel is often encountered in the lateral aspect of the groove and cauterized. Tenosynovium is then excised from the level of the lesser tuberosity to the superior border of the pectoralis major insertion. This is the so-called suprapectoral region of the proximal humeral metaphysis (Video 2). A piloted headed reamer with built-in guide tip (Arthrex, Naples, FL) is then introduced through the transdeltoid portal, and the anterior cortex of the suprapectoral humerus is drilled to a depth of 20 mm. The guide tip eliminates the need to ream over a guide pin. We have found that the LHB diameter at this level is usually 7 mm in female patients and 8 mm in male patients. Generally, the drill bit diameter is oversized by 1 mm, resulting in an 8-mm-diameter tunnel for female patients and a 9-mm-diameter tunnel in male patients.
Figure 4.
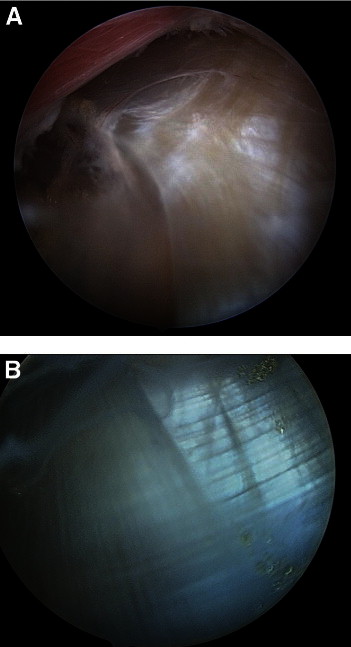
(A) Proximal-to-distal view of falciform ligament in a right shoulder, with the arthroscope through the accessory anterolateral portal, viewing distal within the subdeltoid bursae. The intersection between the longitudinal fibers of the biceps sheath and the transverse fibers of the superior edge of the pectoralis major should be noted. (B) Close-up view of intersecting fibers that make up falciform ligament. The LHB lies just beneath this visual landmark.
Once the tunnel is drilled, the drill is removed and a shaver is used to clear the tunnel edges of periosteum and improve visualization. For fixation, we use the SwiveLock Tenodesis implant (Arthrex), which is designed for all-arthroscopic biceps tenodesis. It features a polyetheretherketone (PEEK) forked tip that is used to steer the biceps tendon into the bottom of the bone socket without the need to externalize or whipstitch the tendon. A suture can be passed around the tendon and through the holes in the forked tip for greater control of the tendon. The tenodesis device is then introduced through the transdeltoid portal, and the tendon is guided into the drilled socket. The spinal needle that was previously placed through the rotator interval and into the intra-articular portion of the LHB is removed as the implant and tendon are guided into the tunnel. While the tendon is held in the tunnel with the forked tip, the tenodesis screw is inserted under direct visualization (Video 3). The interference screw depth is inspected with a probe, and the LHB is assessed for appropriate tension and pullout resistance. The excess proximal tendon is then removed with a basket or shaver.
Discussion
We believe that the ideal LHB tenodesis procedure should (1) be arthroscopic, (2) provide secure fixation, (3) resect the proximal segment of the LHB, and (4) restore the native length-tension relation of the tendon.
In recent years a growing number of outpatient shoulder procedures have evolved from open techniques to arthroscopic methods. Although there is certainly a learning curve involved in making this transition, outcome studies have generally supported this evolution. Tenodesis of the LHB is usually an add-on procedure to an arthroscopic procedure. In the midst of an arthroscopic surgical case, an open procedure generally requires a separate surgical tray for retractors and dissecting instruments, an alteration in patient positioning, and closure of a larger incision, which can add to the operative time. We believe that, by nature, arthroscopists prefer to perform their procedures through the arthroscope and, when given a comparable choice, would select an arthroscopic method over an open method.
Use of an interference screw is an accepted method of fixation for biceps tenodesis.1-3,10,11 In a recent cadaveric biomechanical analysis by Patzer et al.,10 methods and locations for LHB tenodesis were investigated. They compared suture anchor with tenodesis screw fixation and confirmed that a suture anchor construct showed failure at 45% to 51% relative to a suprapectoral interference screw construct. In addition, fixation within the suprapectoral region was compared with the more distal, subpectoral location. The authors discovered that the highest ultimate load to failure was shown with fixation within the suprapectoral region. The subpectoral fixation group achieved a mean ultimate load to failure of 92% compared with the suprapectoral site. The device used in this technique (SwiveLock Tenodesis implant) incorporates screw fixation with a forked tip that allows manipulation of the tendon into the drilled tunnel. This adaptation bypasses the need to externalize or whipstitch the LHB to gain control of the end that has undergone tenotomy. This technique also provides insertion of 2 tunnel lengths of tendon-to-bone contact versus traditional tenodesis screws that allow just a single tunnel length of tendon-to-bone contact.
We recommend resection of any portion of the LHB proximal to the lesser tuberosity. The commonly proposed sites of pain generation for the LHB are at its origin on the supraglenoid tubercle, at its intra-articular portion as it angles sharply over the humeral head, and at its passage within the intertubercular groove.12 Arthroscopic techniques that describe fixation of the LHB tendon proximal to the lesser tuberosity of the humerus may not adequately provide pain relief because of the inability of these techniques to address intertubercular pathology. Sanders et al.13 found higher revision rates after biceps tenodesis procedures that did not release the biceps sheath or remove the tendon from the sheath. We have often seen pathologic conditions of the LHB within the bicipital groove extending distally to the lesser tuberosity, including synovitis, loose bodies, and longitudinal split tears. Only a method of tenodesis that removes the tendon from each of these sites can address these potential sources of pain. Whereas the subpectoral tenodesis achieves this goal as well, we have found revision of the subpectoral tenodesis challenging because of the excessive tendon resection necessary when performing this distal tenodesis technique (Table 2).
Table 2.
Advantages of Arthroscopic Suprapectoral Tenodesis
| • Less surgical dissection |
| • No tendon externalization |
| • Easier revision because of tendon preservation |
| • Accurate restoration of native LHB length-tension relation |
We believe that restoring the native length-tension relation of the LHB is an important and often difficult step when performing tenodesis of this structure. Our experience with tenotomy has not been favorable and supports the existing data that tenotomy alone results in a cosmetic deformity in a significant number of patients and can produce muscle cramping in young male patients.8,14 The cause of muscle cramping that occurs commonly after tenotomy may be the resultant altered resting tension of the LHB. We have often performed the subpectoral tenodesis and believe that this technique appropriately addresses the proposed sites of pain generation. However, recent anatomic work by Jarrett et al.15 has questioned the ability of the subpectoral tenodesis to adequately restore the LHB length-tendon relation. They found that the musculotendinous junction of the native LHB is far closer to the superior border of the pectoralis major tendon than its inferior border, making restoration of the anatomic LHB tension through a subpectoral approach a near technical impossibility.
Several anatomic considerations should be made when one is performing this procedure (Table 3). First, when establishing the transdeltoid portal, the surgeon should make the skin incision superficially. The cephalic vein within the deltopectoral interval is located less than 1 cm medial to the portal. Second, a proximal branch of the anterior humeral circumflex artery often traverses the suprapectoral region of the humerus; as such, shaver suction should be well controlled during resection of the clavipectoral fascia along the medial humeral border. To prevent loss of visualization, electrocautery should be used immediately because bleeders are encountered. Finally, dissection into the short head of the biceps should be avoided because the musculocutaneous nerve lies within the muscle fibers at this level (Video 4). Jarrett et al.15 have found that, on average, the musculocutaneous nerve was 3.47 cm medial to the LHB at the superior border of the pectoralis tendon and 2.6 cm medial to the LHB at the musculocutaneous junction. These data show that the musculocutaneous nerve is further away from the LHB when one is performing our described procedure as compared with an open subpectoral tenodesis.
Table 3.
Anatomic Considerations in Suprapectoral Region
| • Cephalic vein crosses medial to anterior (working) portal |
| • Proximal branch of anterior humeral circumflex artery |
| • Musculocutaneous nerve within short head of biceps |
We believe that the suprapectoral arthroscopic LHB tenodesis described in this article removes the tendon from its sites of pain generation and enables the restoration of the anatomic length-tension relation in a technically reproducible manner.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary data
Left shoulder visualized from standard posterior viewing portal. It should be noted that most of the intra-articular portion of the LHB appears normal. However, when the tendon is pulled into the joint with the shaver, the portion of the tendon residing in the intertubercular groove is noted to show a longitudinal tear. This video highlights the point that lesions of the LHB may exist within the groove; such lesions may not be adequately addressed by tenodesis techniques that fixate the tendon proximal to the lesser tuberosity.
Left shoulder visualized from viewing portal created off of anterolateral edge of acromion. A 4.0-mm shaver is introduced through the working portal, and the clavipectoral fascia is swept off of the superior edge of the pectoralis major tendon. The falciform ligament is identified by the intersection of the transverse fibers of the crossing pectoralis major tendon and the longitudinal fibers of the biceps tendon sheath. The LHB lies just deep to this intersection. An electrocautery unit can be used to release the falciform ligament, beneath which the LHB can be identified.
Left shoulder visualized from anterolateral viewing portal. A spiked drill bit (Arthrex) allows for drilling of the unicortical tunnel without the need for a guidewire. The inferior cortical edge of the tunnel can then be chamfered with a shaver to minimize tendon amputation upon compression with the screw. A suture is passed around the LHB for better control of the tendon. This can also allow for proximal-distal maneuverability.
Right shoulder visualized from anterolateral viewing portal. A probe is inserted through the transdeltoid portal. The pectoralis major tendon is seen crossing the proximal humerus. As the arthroscope optic is directed medially, the musculocutaneous nerve is identified below the short head of the biceps.
References
- 1.Romeo A.A., Mazzocca A.D., Tauro J.C. Arthroscopic biceps tenodesis. Arthroscopy. 2004;2:206–213. doi: 10.1016/j.arthro.2003.11.033. [DOI] [PubMed] [Google Scholar]
- 2.Mazzocca A.D., Rios C.G., Romeo A.A., Arciero A. Subpectoral biceps tenodesis with interference screw fixation. Arthroscopy. 2005;7:896.e1–896.e7. doi: 10.1016/j.arthro.2005.04.002. www.arthroscopyjournal.org [DOI] [PubMed] [Google Scholar]
- 3.Boileau P., Krishnan S.G., Coste J.S., Walch G. Arthroscopic biceps tenodesis: A new technique using bioabsorbable interference screw fixation. Arthroscopy. 2002;9:1002–1012. doi: 10.1053/jars.2002.36488. [DOI] [PubMed] [Google Scholar]
- 4.Sekiya J.K., Elkousy H.A., Rodosky M.W. Arthroscopic biceps tenodesis using the percutaneous intra-articular transtendon technique. Arthroscopy. 2003;10:1137–1141. doi: 10.1016/j.arthro.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 5.Moros C., Levine W.N., Ahmad C.S. Suture anchor and percutaneous intra-articular transtendon biceps tenodesis. Sports Med Arthrosc. 2008;16:177–179. doi: 10.1097/JSA.0b013e3181824efd. [DOI] [PubMed] [Google Scholar]
- 6.Castagna A., Conti M., Mouhsine E., Bungaro P., Garofalo R. Arthroscopic biceps tendon tenodesis: The anchorage technical note. Knee Surg Sports Traumatol Arthrosc. 2006;6:581–585. doi: 10.1007/s00167-005-0026-1. [DOI] [PubMed] [Google Scholar]
- 7.Nord K.D., Smith G.B., Mauck B.M. Arthroscopic biceps tenodesis using suture anchors through the subclavian portal. Arthroscopy. 2005;2:248–252. doi: 10.1016/j.arthro.2004.10.019. [DOI] [PubMed] [Google Scholar]
- 8.Kelly A., Drakos M., Fealy S., Taylor S., O'Brien S. Arthroscopic release of the long head of the biceps tendon. Am J Sports Med. 2005;2:208–213. doi: 10.1177/0363546504269555. [DOI] [PubMed] [Google Scholar]
- 9.Lim T., Moon E., Koh K., Chul Yoo J. Patient-related factors and complications after arthroscopic tenotomy of the long head of the biceps tendon. Am J Sports Med. 2011;4:783–789. doi: 10.1177/0363546510388158. [DOI] [PubMed] [Google Scholar]
- 10.Patzer T., Santo G., Olender G.D., Wellmann M., Hurschler C., Schofer M.D. Suprapectoral or subpectoral position for biceps tenodesis: Biomechanical comparison of four different techniques in both positions. J Shoulder Elbow Surg. 2012;21:116–125. doi: 10.1016/j.jse.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 11.Boileau P., Krishnan S.G., Coste J.S., Walch G. A new technique for tenodesis of the long head of the biceps using bioabsorbable screw fixation. Tech Shoulder Elbow Surg. 2001;2:153–165. [Google Scholar]
- 12.Alpantaki K., McLaughlin D., Karagogeos D., Hadjipavlou A., Kontakis G. Sympathetic and sensory neural elements in the tendon of the long head of the biceps. J Bone Joint Surg Am. 2005;87:1580–1583. doi: 10.2106/JBJS.D.02840. [DOI] [PubMed] [Google Scholar]
- 13.Sanders B., Lavery B.A., Pennington S., Warner J.P. Clinical success of biceps tenodesis with and without release of the transverse humeral ligament. J Shoulder Elbow Surg. 2012;21:66–71. doi: 10.1016/j.jse.2011.01.037. [DOI] [PubMed] [Google Scholar]
- 14.Hsu A.R., Ghodadra N.S., Provencher M.T., Lewis P.B., Bach B.R. Biceps tenotomy versus tenodesis: A review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg. 2011;20:326–332. doi: 10.1016/j.jse.2010.08.019. [DOI] [PubMed] [Google Scholar]
- 15.Jarrett C.D., McClelland W.B., Jr, Xerogeanes J.W. Minimally invasive proximal biceps tenodesis: An anatomical study for optimal placement and safe surgical technique. J Shoulder Elbow Surg. 2011;20:477–480. doi: 10.1016/j.jse.2010.08.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Left shoulder visualized from standard posterior viewing portal. It should be noted that most of the intra-articular portion of the LHB appears normal. However, when the tendon is pulled into the joint with the shaver, the portion of the tendon residing in the intertubercular groove is noted to show a longitudinal tear. This video highlights the point that lesions of the LHB may exist within the groove; such lesions may not be adequately addressed by tenodesis techniques that fixate the tendon proximal to the lesser tuberosity.
Left shoulder visualized from viewing portal created off of anterolateral edge of acromion. A 4.0-mm shaver is introduced through the working portal, and the clavipectoral fascia is swept off of the superior edge of the pectoralis major tendon. The falciform ligament is identified by the intersection of the transverse fibers of the crossing pectoralis major tendon and the longitudinal fibers of the biceps tendon sheath. The LHB lies just deep to this intersection. An electrocautery unit can be used to release the falciform ligament, beneath which the LHB can be identified.
Left shoulder visualized from anterolateral viewing portal. A spiked drill bit (Arthrex) allows for drilling of the unicortical tunnel without the need for a guidewire. The inferior cortical edge of the tunnel can then be chamfered with a shaver to minimize tendon amputation upon compression with the screw. A suture is passed around the LHB for better control of the tendon. This can also allow for proximal-distal maneuverability.
Right shoulder visualized from anterolateral viewing portal. A probe is inserted through the transdeltoid portal. The pectoralis major tendon is seen crossing the proximal humerus. As the arthroscope optic is directed medially, the musculocutaneous nerve is identified below the short head of the biceps.


