Abstract
With the significant increase in use of the arthroscope around the hip have come several less invasive techniques to manage pathologies around this joint. This technical note with a video details one such technique that allows for the endoscopic management of proximal hamstring tears and chronic ischial bursitis, which until now have been managed exclusively with much larger open approaches. This procedure allows for complete exposure of the posterior aspect of the hip in a safe, minimally invasive fashion.
With the advent and further refinement of hip arthroscopy has come the endoscopic management of several pathologies previously treated with more invasive, open approaches.1,2 The development of this endoscopic technique is another such evolution. Hamstring injuries are common in athletic populations and can affect all levels of athletes.3-7 There is a continuum of hamstring injuries that can range from musculotendinous strains to avulsion injuries.3,4 By definition, a strain is a partial or complete disruption of the musculotendinous unit.4 A complete tear or avulsion, in contrast, is a discontinuity of the tendon-bone unit. Most hamstring strains resolve with a variety of modalities and rest and do not require surgical intervention.3-7
With the exception of the short head of the biceps femoris, the hamstring complex originates from the ischial tuberosity and inserts distally below the knee on the proximal tibia. The tibial branch of the sciatic nerve innervates the semitendinosus, semimembranosus, and long head of the biceps femoris, whereas the short head of the biceps femoris is innervated by the peroneal branch of the sciatic nerve.5
The proximal hamstring complex has a strong bony attachment on the ischial tuberosity (Fig 1). Its footprint on the ischium is composed of the semitendinosus and long head of the biceps femoris beginning as a common proximal tendon and footprint, whereas there is a distinct semimembranosus footprint.8 The semimembranosus footprint is just lateral (and anterior) to the crescent-shaped footprint of the common origin of the semitendinosus and long head of the biceps femoris (Fig 1).
Figure 1.
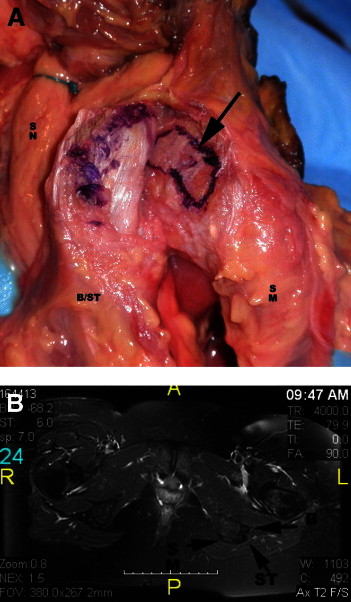
(A) Cadaveric dissection of the ischium in a left hip, viewed from the posterior aspect. The arrow points to the origin of the biceps/semitendinosus (B/ST), which has been elevated and retracted laterally. (B) Axial T2-weighted magnetic resonance image depicting the anatomy of the hamstring origin in a left hip. (B, biceps origin; SM, origin of semimembranosus; SN, sciatic nerve; ST, semitendinosus.)
The history of an acute injury usually involves a traumatic event with forced hip flexion and knee in extension, as is classically observed in waterskiing.9,10 However, the injury can result from a wide variety of sporting activities that require rapid acceleration and deceleration.11,12
Proximal hamstring tears can be categorized as complete tendinous avulsions, partial tendinous avulsions, apophyseal avulsions, and degenerative (tendinosis) avulsions.11 Degenerative tears of the hamstring origin are more insidious in onset and are commonly seen as overuse injuries. The mechanism of injury is presumably repetitive irritation of the medial aspect of the hamstring tendon (typically along the lateral aspect of the tuberosity, where the bursa resides) ultimately causing an attritional tear of the tendon.
Commonly, athletes with proximal hamstring tendon tears describe a popping or tearing sensation with associated acute pain and bruising over the posterior hip.13,14 Occasionally, patients who present with either acute or chronic tears may complain of a pins-and-needles sensation in the sciatic nerve distribution, much like sciatica.14,15 This may be due to the acute compression of a hematoma in the proximity of the sciatic nerve or chronic scarring and tethering of the tendon to the nerve. Similarly, symptoms of ischial bursitis include buttock pain or hip pain, as well as localized tenderness overlying the ischial tuberosity. Additional symptoms of chronic ischial bursitis may also include tingling into the buttock that spreads down the leg.14
One aspect that briefly deserves mention is the need for advance imaging in many of the cases of partial tears. To begin with, standard radiographs of the pelvis and a lateral view of the affected hip are obtained to rule out any apophyseal avulsions, particularly of the ischial tuberosity in younger patients (Fig 2). Most commonly, no fractures are identified, and magnetic resonance imaging (MRI) is used to assess the proximal hamstring origin on the ischial tuberosity, where several types of injuries may be seen. A complete rupture of all 3 tendons is common and is easily identified on MRI.
Figure 2.

Anteroposterior radiograph of the pelvis showing bilateral bony avulsions of the ischial tuberosities (arrows) in a 14-year-old athlete.
Partial hamstring origin tears, however, are more difficult to delineate. This is particularly the case in 2-tendon tears, which commonly have an associated musculotendinous junction injury to the third tendon. The most common situation is an avulsion of the common semitendinosus and biceps origin, with the semimembranosus remaining intact.7 In addition, partial tears without any significant retraction can be seen on MRI as a sickle sign. These are typically partial avulsions of the semimembranosus (Fig 3).
Figure 3.
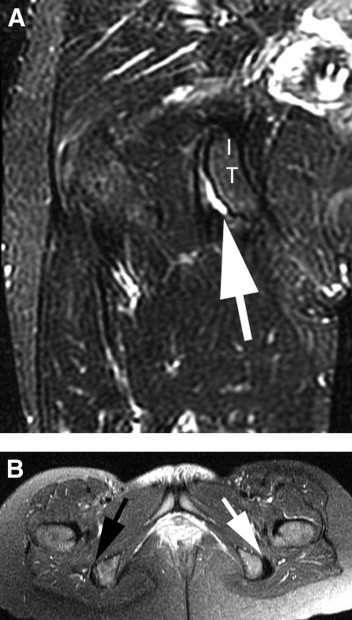
MRI views of a partial insertional tear with a sickle sign, indicating fluid within the ischial bursa. (A) A coronal T2-weighted view of a right hip showing the sickle sign (arrow). (IT, ischial tuberosity.) (B) Axial T2-weighted view showing both ischial tuberosities. One should note the right side (black arrow) showing the sickle sign and the normal left side (white arrow).
Nonoperative treatment of proximal hamstring injuries is most commonly recommended in the setting of low-grade partial tears and insertional tendinosis. Initial treatment consists of active rest, oral nonsteroidal anti-inflammatory medications, and a physical therapy program.16 If the patient is unable to improve with this program, an ultrasound-guided corticosteroid injection may be used and has been shown to provide initial relief in up to 50% of patients at 1 month.17 Failure of nonoperative treatment of partial tears may benefit from surgical debridement and repair, similar to other commonly seen partial tendon tears (patella, quadriceps, and biceps).18
There are several series and descriptions of open surgical techniques that are available in the literature.12-14,19-22 To date, there has been no report of endoscopic management of these injuries. After developing experience in the open management of these injuries, the senior author has developed an endoscopic technique that allows a safe approach to the area of damage in most tears. It is expected that the benefits of this endoscopic approach, without elevation of the gluteus maximus and with the use of endoscopic magnification to protect the sciatic nerve, will improve the management of these injuries and reduce the morbidities associated with the open approach.
Surgical Technique
The technique positions the patient in the prone position after induction of anesthesia, with all prominences and neurovascular structures protected (Video 1 at 20 seconds). The posterior aspect of the hip is then sterilized, with the surgeon ensuring that the leg and thigh are free so that the leg and hip can be freely manipulated during the case (Fig 4).
Figure 4.

Image of patient positioned prone with the left hip and leg draped free.
Two portals are created, 2 cm medial and lateral to the palpable ischial tuberosity (Fig 5, Video 1 at 27 seconds). The lateral portal is established first, through blunt dissection with a switching stick, as the gluteus maximus muscle is penetrated and the submuscular plane is developed. The prominence of the ischial tuberosity is identified, and the medial and lateral borders are located. The medial portal is then established, taking care to palpate the medial aspect of the ischium. A 30° arthroscope is inserted in the lateral portal, and an electrocautery device is placed in the medial portal. Any remaining fibrous attachments between the ischium and the gluteus muscle are released, staying along the central and medial portions of the ischium to avoid any damage to the sciatic nerve (Video 1 at 40 seconds). Once the tip and medial aspect of the ischium are delineated, the lateral aspect is exposed with the use of a switching stick as a soft-tissue dissector. With the lateral aspect identified, the dissection continues anteriorly and laterally toward the known area of the sciatic nerve (Fig 6, Video 1 at 1 minute). Very careful and methodical release of any soft-tissue bands is then undertaken in a proximal-to-distal direction to mobilize the nerve and protect it throughout the exposure and ultimate repair of the hamstring tendon (Video 1 at 1 minute 25 seconds). The posterior femoral cutaneous nerve is often the first branch of the nerve identified during dissection and serves as a harbinger of the main sciatic nerve.
Figure 5.

Image of a left hip with the patient in the prone position showing the standard portals for endoscopic hamstring repair. The arthroscope is in the medial portal, and the shaver is in the distal portal.
Figure 6.
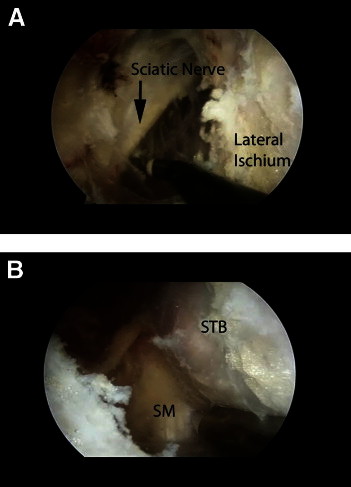
Endoscopic views of the subgluteal space in a left hip. The arthroscope is in the lateral portal. (A) With the instrument in the medial portal, a branch of the sciatic nerve has been exposed along with the lateral ischium. (B) The separate attachments of the semimembranosus (SM) tendon more anterior and lateral and the common biceps and semitendinosus (STB) tendon more posterior and medial.
With the nerve identified and protected, the tip of the ischium is identified (Video 1 at 1 minute 35 seconds). The tendinous origin is then inspected to identify any obvious tearing (Fig 7, Video 1 at 1 minute 40 seconds). In acute tears the tear is obvious and the tendon is often retracted distally. In these cases there is occasionally a large hematoma that requires evacuation. It is especially important to protect the sciatic nerve during this portion of the procedure, because it may be obscured by the hematoma.
Figure 7.
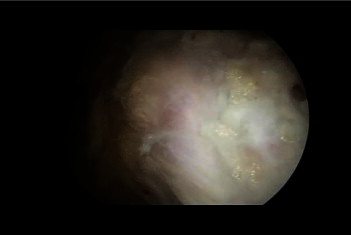
Endoscopic view of the proximal hamstring origin in a left hip with the arthroscope in the lateral portal. The distal end of the ischium has been cleared of soft tissue.
Once the area of pathology is identified (in incomplete tears), an endoscopic knife can be used to longitudinally split the tendon along its fibers (Fig 8, Video 1 at 1 minute 50 seconds). This area can be identified through palpation, because there is typically softening over the detachment, making the tissue ballotable against the ischium. The hamstring footprint is then undermined, and the partial tearing and lateral ischial wall are debrided with an oscillating shaver (Video 1 at 2 minutes). The devitalized tissue is removed, and a bleeding cancellous bed is created in preparation for tendon repair. The more distal and inferior ischium and the ischial bursa can also be resected and cleared of inflamed tissue as the lateral ischial tissue is mobilized (Video 1 at 2 minutes 10 seconds). By retracting the anterior tissues, the bursa can be entered and debrided (Fig 9, Video 1 at 2 minutes 25 seconds).
Figure 8.
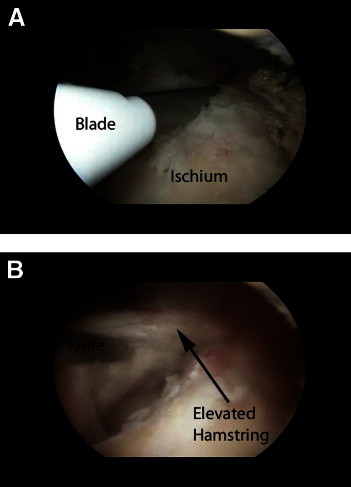
Endoscopic views of the proximal hamstring origin in a left hip with the arthroscope in the lateral portal. (A) A knife has been inserted through the distal portal, and the biceps-semitendinosus attachment has been incised. (B) The common biceps-semitendinosus origin has been elevated.
Figure 9.
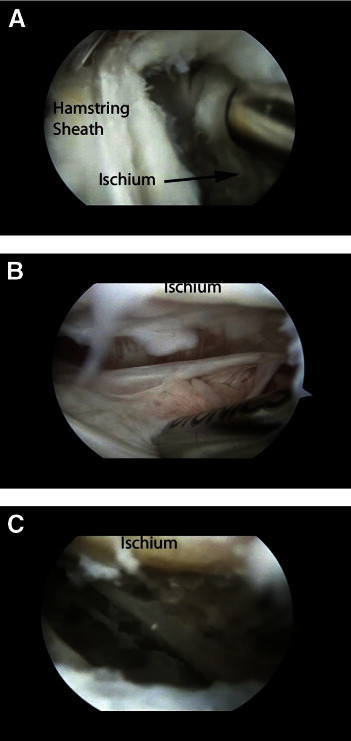
Endoscopic views of the proximal hamstring origin in a left hip with the arthroscope in the lateral portal. (A) The common biceps-semitendinosus origin has been incised and elevated. The tool serves to retract the detached tissue. (B) Ischial bursa before debridement. Hypertrophic inflammatory tissue is present in the bursal space. (C) Final debridement of bursa. The exposed bony surface at the top of the image should be noted.
In preparation for the repair, an inferior portal is created approximately 4 cm distal to the tip of the ischium and equidistant from the medial and lateral portals (Fig 5). This portal is used for insertion of suture anchors, as well as suture management. Any variety of suture passing devices can then be used for the repair (Video 1 at 2 minutes 35 seconds). The principles are essentially the same as those used in arthroscopic rotator cuff repair (Video 1 at 2 minutes 45 seconds). Once all of the sutures are passed through the tissue of the avulsed hamstring, the sutures are tied and a solid repair of the tendon is completed (Video 1 at 3 minutes 20 seconds). In general, one suture anchor is used per centimeter of detachment (Fig 10).
Figure 10.
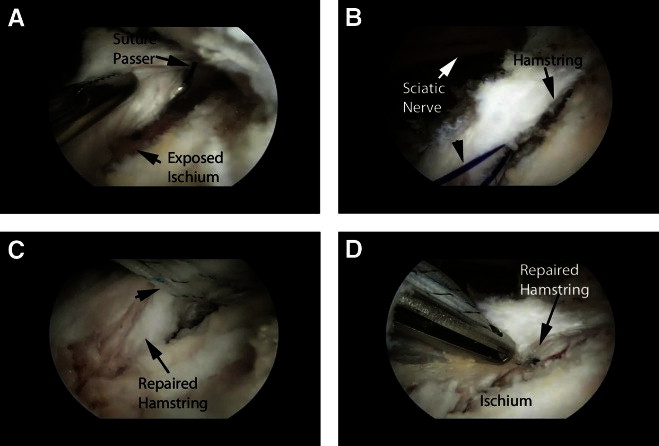
Endoscopic views of repair of the proximal hamstring origin in a left hip with the arthroscope in the lateral portal. (A) The ischium has been prepared, and the suture passer is in place. (B) Shuttle suture in place (arrowhead). The proximity of the sciatic nerve to the repair should be noted. (C) Final mattress sutures in place in the substance of the tendon (arrowheads). (D) Final tendon repair with the tendon edges reattached to the ischial footprint.
Postoperatively, the patient is fitted with a hinged knee brace that is fixed at 90° of flexion for 4 weeks to maintain non–weight bearing (Video 1 at 3 minutes 45 seconds). The brace will also serve to restrict excursion of the hamstring tendons and protect the repair. At 4 weeks, the knee is gradually extended by about 30° per week to allow full weight bearing by 6 to 8 weeks, while the patient continues to use crutches. Physical therapy is instituted at this point, with the initial phase focused on hip and knee range of motion. Hamstring strengthening is begun at 10 to 12 weeks, predicated on full range of motion and a painless gait pattern. Full, unrestricted activity is allowed at approximately 4 months.
Discussion
Historically, the surgical approach to hamstring repairs has received limited attention, because this is not a common area for surgical treatment encountered throughout orthopaedic training. Those patients with partial tears and chronic bursitis comprise an even smaller percentage of patients with hamstring problems, with few clinical studies available.23 With the advent of hip arthroscopy, further development of techniques has allowed us to explore the use of the arthroscope in many previously uncharted areas. The treatment of these hamstring injuries is one such area.
One of the most important aspects in the treatment of proximal hamstring ruptures is early recognition and early treatment. Patients with acute repairs have had better outcomes in the literature when compared with chronic repair.13,14 Delayed complications of nonoperative treatment of proximal hamstring ruptures have been described, and these include knee flexion and hip extension weakness, difficulty sitting, and hamstring deformity.24 The senior author has used the described technique successfully on several acute ruptures as well as chronic partial tears.
Surgical repair of proximal hamstring ruptures also has its inherent risks. With open methods, superficial as well as deep wound infections can occur similar to other surgeries; however, the location of the incision can potentially increase this risk because of the location of the incision within the perineal region. With the endoscopic technique, this possibility is substantially lessened. In addition, the 3 main nervous structures at risk of iatrogenic injury are the posterior femoral cutaneous, inferior gluteal, and sciatic nerves.18,25 The sciatic nerve is in close proximity to the ischial tuberosity, running along its lateral aspect. With our endoscopic technique, the need for retraction is nonexistent, because the nerve is identified, visualized, and protected during the repair.
A concern unique to the endoscopic approach is fluid extravasation into the pelvis as a result of the fluid used in the distension of the potential space around the hamstring tendon. Every effort should be made to regularly check the abdomen for any evidence of abdominal distension. Likewise, any unusual blood pressure decreases may be due to fluid compression from retroperitoneal extravasation. In general, an attempt should be made to maintain the fluid inflow pressures as low as is feasible for adequate visualization, and an attempt should be made to keep track of fluid ingress and egress volumes to ensure that extravasation is avoided.
Through the judicious application of the described technique, many of the chronic hamstring injuries and some of the acute injuries previously addressed through a more invasive, open method can be effectively addressed endoscopically. With this improved technique, it is hoped that a further understanding of hamstring injuries and their sequelae can be developed.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary data
Endoscopic repair of a chronic proximal hamstring avulsion with ischial bursectomy. A step-by-step explanation of our preferred technique is shown.
References
- 1.Martin H.D., Shears S.A., Johnson J.C., Smathers A.M., Palmer I.J. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy. 2011;27:172–181. doi: 10.1016/j.arthro.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 2.Byrd J.W.T., Polkowski G., Jones K.S. Endoscopic management of the snapping iliopsoas tendon. Arthroscopy. 2009;25:e18. (Abstr) [Google Scholar]
- 3.Brown T. Thigh. In: Drez D.D., DeLee J.C., Miller M.D., editors. Vol 2. WB Saunders; Philadelphia: 2003. pp. 1481–1523. (Orthopaedic sports medicine: Principles and practice). [Google Scholar]
- 4.Clanton T.O., Coupe K.J. Hamstring strains in athletes: Diagnosis and treatment. J Am Acad Orthop Surg. 1998;6:237–248. doi: 10.5435/00124635-199807000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Garrett W.E., Jr Muscle strain injuries. Am J Sports Med. 1996;24(Suppl):S2–S8. [PubMed] [Google Scholar]
- 6.Garrett W.E., Jr, Rich F.R., Nikolaou P.K., Vogler J.B. Computed tomography of hamstring muscle strains. Med Sci Sports Exerc. 1989;2:506–514. [PubMed] [Google Scholar]
- 7.Elliott M.C., Zarins B., Powell J.W., Kenyon C.D. Hamstring muscle strains in professional football players: A 10-year review. Am J Sports Med. 2011;39:843–850. doi: 10.1177/0363546510394647. [DOI] [PubMed] [Google Scholar]
- 8.Miller S.L., Gill J., Webb G.R. The proximal origin of the hamstrings and surrounding anatomy encountered during repair: A cadaveric study. J Bone Joint Surg Am. 2007;89:44–48. doi: 10.2106/JBJS.F.00094. [DOI] [PubMed] [Google Scholar]
- 9.Blasier R.B., Morawa L.G. Complete rupture of the hamstring origin from a water skiing injury. Am J Sports Med. 1990;18:435–437. doi: 10.1177/036354659001800419. [DOI] [PubMed] [Google Scholar]
- 10.Orava S., Kujala U.M. Rupture of the ischial origin of the hamstring muscles. Am J Sports Med. 1995;23:702–705. doi: 10.1177/036354659502300612. [DOI] [PubMed] [Google Scholar]
- 11.Klingele K.E., Sallay P.I. Surgical repair of complete proximal hamstring tendon rupture. Am J Sports Med. 2002;30:742–747. doi: 10.1177/03635465020300051901. [DOI] [PubMed] [Google Scholar]
- 12.Mica L., Schwaller A., Stoupis C., Penka I., Vomela J., Vollenweider A. Avulsion of the hamstring muscle group: A follow-up of 6 adult non-athletes with early operative treatment: A brief report. World J Surg. 2009;33:1605–1610. doi: 10.1007/s00268-009-0099-y. [DOI] [PubMed] [Google Scholar]
- 13.Sallay P.I., Ballard G., Hamersly S., Schrader M. Subjective and functional outcomes following surgical repair of complete ruptures of the proximal hamstring complex. Orthopedics. 2008;31:1092–1096. [PubMed] [Google Scholar]
- 14.Sarimo J., Lempainen L., Mattila K., Orava S. Complete proximal hamstring avulsions: A series of 41 patients with operative treatment. Am J Sports Med. 2008;36:1110–1115. doi: 10.1177/0363546508314427. [DOI] [PubMed] [Google Scholar]
- 15.Konan S., Haddad F. Successful return to high level sports following early surgical repair of complete tears of the proximal hamstring tendons. Int Orthop. 2010;34:119–123. doi: 10.1007/s00264-009-0739-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mendiguchia J., Brughelli M. A return-to-sport algorithm for acute hamstring injuries. Phys Ther Sport. 2011;12:2–14. doi: 10.1016/j.ptsp.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 17.Zissen M.H., Wallace G., Stevens K.J., Fredericson M., Beaulieu C.F. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. AJR Am J Roentgenol. 2010;195:993–998. doi: 10.2214/AJR.09.3674. [DOI] [PubMed] [Google Scholar]
- 18.Lempainen L., Sarimo J., Mattila K., Vaittinen S., Orava S. Proximal hamstring tendinopathy: Results of surgical management and histopathologic findings. Am J Sports Med. 2009;37:727–734. doi: 10.1177/0363546508330129. [DOI] [PubMed] [Google Scholar]
- 19.Chakravarthy J., Ramisetty N., Pimpalnerkar A., Mohtadi N. Surgical repair of complete proximal hamstring tendon ruptures in water skiers and bull riders: A report of four cases and review of the literature. Br J Sports Med. 2005;39:569–572. doi: 10.1136/bjsm.2004.015719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cross M.J., Vandersluis R., Wood D., Banff M. Surgical repair of chronic complete hamstring tendon rupture in the adult patient. Am J Sports Med. 1998;26:785–788. doi: 10.1177/03635465980260060801. [DOI] [PubMed] [Google Scholar]
- 21.Cohen S., Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15:350–355. doi: 10.5435/00124635-200706000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Birmingham P., Muller M., Wickiewicz T., Cavanaugh J., Rodeo S., Warren R. Functional outcome after repair of proximal hamstring avulsions. J Bone Joint Surg Am. 2011;93:1819–1826. doi: 10.2106/JBJS.J.01372. [DOI] [PubMed] [Google Scholar]
- 23.Harris J.D., Griesser M.J., Best T.M., Ellis T.J. Treatment of proximal hamstring ruptures—A systematic review. Int J Sports Med. 2011;32:490–495. doi: 10.1055/s-0031-1273753. [DOI] [PubMed] [Google Scholar]
- 24.Puranen J., Orava S. The hamstring syndrome: A new diagnosis of gluteal sciatic pain. Am J Sports Med. 1988;16:517–521. doi: 10.1177/036354658801600515. [DOI] [PubMed] [Google Scholar]
- 25.Lempainen L., Sarimo J., Heikkilä J., Mattila K., Orava S. Surgical treatment of partial tears of the proximal origin of the hamstring muscles. Br J Sports Med. 2006;40:688–691. doi: 10.1136/bjsm.2006.028191. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic repair of a chronic proximal hamstring avulsion with ischial bursectomy. A step-by-step explanation of our preferred technique is shown.


