Abstract
The arthroscopic treatment of the “bony Bankart lesion” continues to evolve. We present a novel technique that we developed at Orthopaedic Research of Virginia, the “transosseous bony Bankart repair,” which incorporates several essential concepts to provide for optimal healing and rehabilitation. We promote arthroscopic repair emphasizing bone preservation, a fracture interface without interposing sutures, the ability to reduce capsular volume, and multiple points of stable glenolabral fixation. Our technique positions suture anchors within the subchondral bone of the intact glenoid to allow for an anatomic reduction of the bony fragment. By use of an arthroscopic drill, spinal needle, and nitinol suture passing wire, the sutures are passed in a retrograde fashion through the bony Bankart fragment and anterior capsule in a mattress configuration. Additional inferior and superior anchors are placed to further provide stability and reduce capsular volume. While maximizing fracture surface area and optimizing bony healing, the end result is an anatomic reduction of the bony fragment and the glenoid articular surface.
Treatment of traumatic anterior instability of the shoulder is a controversial topic that frequently requires surgical intervention. Arthroscopic techniques continue to evolve, and surgical outcomes erode the gold standard of open stabilization. The most common consequence of traumatic glenohumeral instability involves pathology of the anterior-inferior glenoid–capsulolabral complex. First described in 1923, the “Bankart lesion” described a shearing of the joint fibrous capsule from the “fibrocartilaginous glenoid ligament.”1 More recent literature has differentiated between a soft-tissue Bankart lesion and that which involves a fracture of the glenoid rim, termed a “bony Bankart.” Advances in imaging (magnetic resonance imaging and computed tomography) and enhanced arthroscopic visualization of the shoulder have enabled us to better define and address the pathology of instability.2,3 We can now tailor our surgical approach to the amount of anterior bone loss, the degree of capsulolabral laxity, and the size of the Hill-Sachs lesion.
Arthroscopic techniques have evolved to treat both soft-tissue and bony Bankart lesions. Soft-tissue repair techniques initially involved staple fixation and subsequently transitioned to transglenoid techniques.4,5 Because of the high complication rate and variable success, these techniques disappeared with the advent of the suture anchor.6
First described by Wolf7 in 1993, the development of suture anchors revolutionized the arthroscopic treatment of shoulder instability. Multiple studies have documented improved shoulder function and decreased recurrent dislocation rates with this technique.8,9
Several recent studies have noted that recurrent instability is directly related to the amount of anterior bone loss, and preserving bone is imperative to repair techniques.10,11 The most essential part of surgical repair involves stable fixation of the bony Bankart lesion in an effort to achieve osseous union and prevent recurrent instability. This has generated substantial awareness concerning bone preservation and precipitated a number of innovative techniques, ranging from screw fixation to multiple configurations of suture repair.2,12-19 We present an arthroscopic transosseous technique that we developed at Orthopaedic Research of Virginia that provides anatomic reduction, compressive fixation, and reinforces capsulolabral stability to maximize osseous union and reduce capsular volume.
Surgical Technique
Our technique uses the traditional lateral decubitus position with a bolster under the arm for optimal visualization. A standard posterior portal is created, and a diagnostic arthroscopy is performed. Special attention to the size and integrity of the bony fragment is noted during the initial inspection. By use of an outside-in technique, an 18-gauge spinal needle is used to establish anterior-inferior and anterior-superior portals (Fig 1, Video 1). As with soft-tissue repair, care is taken to ensure access to the inferior aspect of the glenoid and adequate working distance between the 2 portals.
Figure 1.
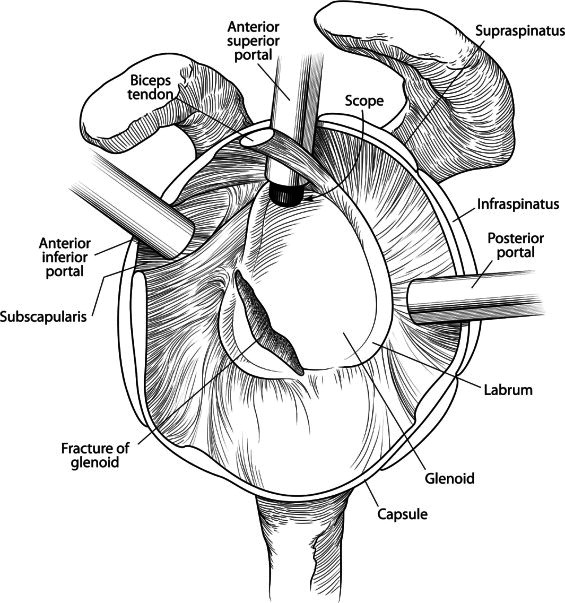
Sagittal view of the glenoid showing arthroscopic portal placement and the bony Bankart lesion.
The anterior-superior portal is the primary viewing portal throughout the procedure. An arthroscopic liberator is helpful to mobilize the bony fragment and capsular tissue, which are often healed medial to the glenoid surface. The importance of this step cannot be overstated, because the capsule–labrum–bony fragment must be mobilized so that it can be elevated just above the glenoid surface for retrograde drilling. Similar to soft-tissue Bankart mobilization, it is important to mobilize the fragment enough to visualize deeper subscapularis muscle fibers. An arthroscopic shaver and bur are used to remove all fibrous soft tissue from both fragments, to achieve a bleeding bed for optimal bony healing.
Typically, the first anchor is positioned on the inferior aspect of the native glenoid through a percutaneous posterolateral approach (Fig 2). The sutures are passed through the inferior capsule in an effort to reduce the inferior capsular volume. These sutures are left untied, so as not to limit the mobility of the bony fragment.
Figure 2.
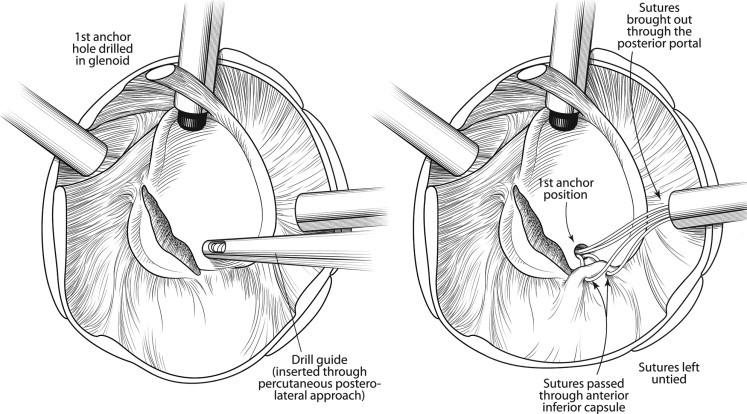
Sagittal view of the glenoid showing the placement of the first anchor within the native glenoid and suture passage within the anterior-inferior capsule.
The bony fragment is again assessed for size and integrity. The second anchor may be inserted through the anterior-inferior portal or by use of a percutaneous trans-subscapularis approach. It is imperative to place this anchor in the subchondral bone just below the glenoid articular surface. Multiple anchors may be placed during this step, depending on the size of the bony fragment, as well as the anticipated corresponding drill holes within the bony fragment.
Once the anchor(s) has been implanted, a long drill guide and 1.6-mm drill are brought through the posterior portal parallel to the glenoid face. An arthroscopic grasper is used through the anterior-inferior portal to control the bony fragment. Holes are drilled in the bony fragment at the corresponding level as the anchor to accommodate a horizontal mattress configuration (Fig 3). Once drilling is complete, a long spinal needle is brought in from the posterior portal and placed through the drill hole. The grasper is again positioned to tension the anterior capsule to facilitate visualization of the tip of the spinal needle as it penetrates the capsule just anterior to the labrum. The amount of capsule incorporated into each stitch may be tailored to the desired capsular reduction. A nitinol suture passing wire is passed through the spinal needle and retrieved through the anterior-inferior portal.
Figure 3.
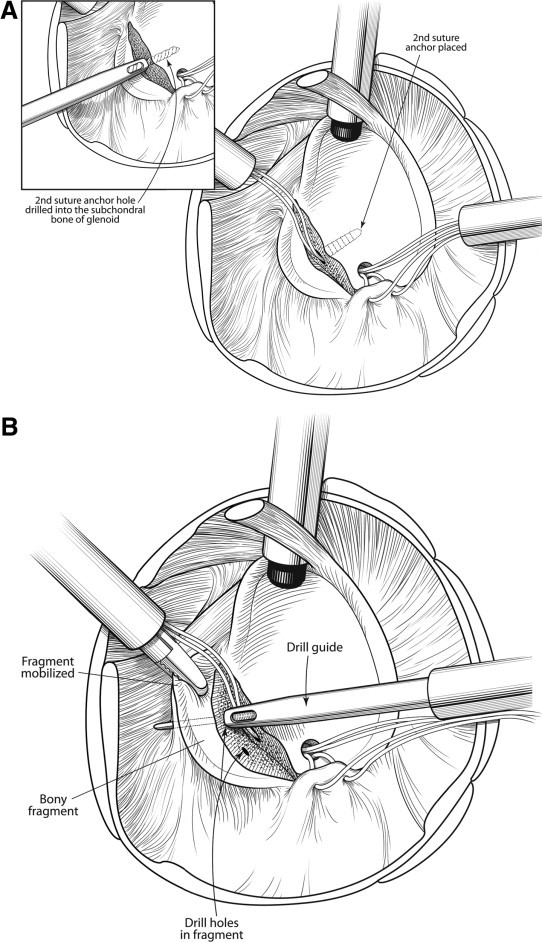
Sagittal view of the glenoid showing (A) the placement of the second anchor within the subchondral bone of the glenoid and (B) drilling of the bony fragment.
Standard suture shuttling techniques are used to create a horizontal mattress configuration, and the sutures are tied from inferior to superior by use of standard arthroscopic techniques (Figs 4 and 5). The horizontal mattress stitch provides compression at the fracture site and plication of the anterior capsule. An additional anchor may be placed superior to the bony fragment to further augment the repair. Standard immobilization is used postoperatively, followed by a traditional instability rehabilitation protocol.
Figure 4.
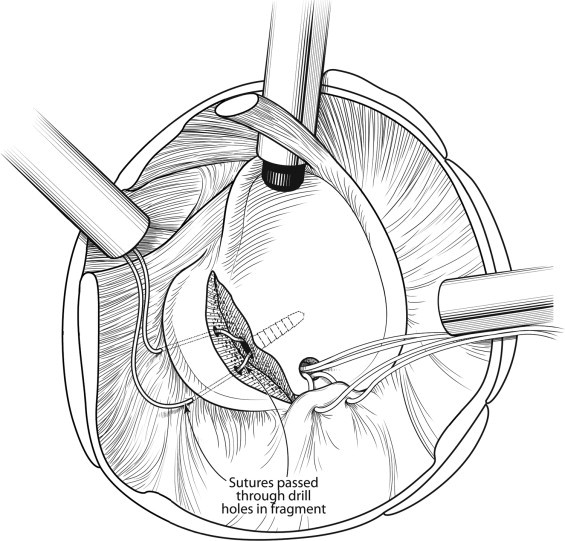
Sagittal view of the glenoid showing suture passage through the bony fragment.
Figure 5.
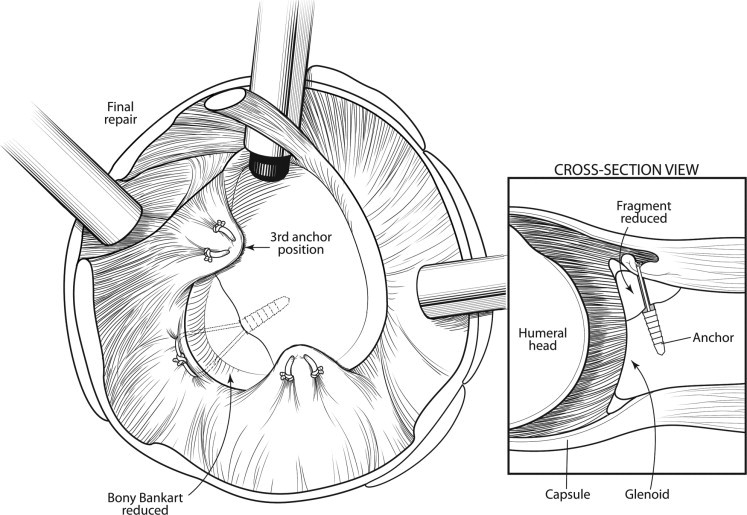
Final repair of the bony Bankart with cross section.
Discussion
Many techniques for the repair of the bony Bankart lesion with preservation of the bony fragment have been described. Arthroscopically assisted percutaneous screw fixation can be precarious because of neurovascular proximity. Most arthroscopic surgeons are very familiar with the use of suture anchors and suture passing techniques to repair soft-tissue instability. One of the more common arthroscopic techniques for bony Bankart repair involves sutures that circumferentially encompass the bony fragment.13 Though generally successful, this technique places suture material at the fracture interface and thus potentially reduces the surface area and stability, which are essential for healing. Circumferential sutures may also present a potential risk for abrasion to the articular surface of the humerus.
Other arthroscopic procedures, such as the “bony Bankart bridge” technique and a hybrid transglenoid/suture anchor technique, achieve excellent bony apposition without interposing suture at the fracture interface. However, many of these techniques provide indirect compression of the bony fragment and fail to reduce capsular volume. Suture also remains along the glenolabral articular surface, increasing the risk for abrasion.14-19 Optimal fixation requires maximizing the healing potential without sacrificing fixation. We advocate bone preservation with stable fixation for repair through a transosseous approach to fixation. This technique eliminates the dangers of anterior drilling yet optimizes bone-to-bone healing by use of existing techniques (Table 1). Tying the sutures anterior to the labrum in a mattress fashion also further reduces the capsular volume and decreases the risk of articular abrasion. The transosseous approach is a reproducible technique using traditional suture anchor fixation that offers an anatomic reduction while maximizing the healing potential and stability of the bony fragment.
Table 1.
Advantages of Arthroscopic Transosseous Bony Bankart Repair
| Standard arthroscopic setup |
| No special instrumentation |
| Familiar arthroscopic techniques |
| Preservation of bony Bankart fragment |
| Direct fracture compression without interposing sutures |
| Reinforced labral stability both superior and inferior to bony Bankart fragment |
| Elimination of potential suture abrasion of articular surfaces |
| Incorporation of capsular volume reduction techniques along with fracture stabilization |
Acknowledgment
The authors acknowledge Paul Graves, surgical technician at St. Mary's Ambulatory Surgery Center, Richmond, Virginia.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary data
Novel technique for arthroscopic transosseous fixation of a bony Bankart lesion.
References
- 1.Bankart A.S., Cantab M.C. Recurrent or habitual dislocation of the shoulder-joint. BMJ. 1923;2:1132–1133. doi: 10.1136/bmj.2.3285.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim Y.K., Cho S.H., Moon S.H. Arthroscopic repair of small and medium sized bony Bankart lesions (SS-04) Arthroscopy. 2012;28:e3. doi: 10.1177/0363546513509062. (Abstr) [DOI] [PubMed] [Google Scholar]
- 3.Milano G., Grasso A., Russo A. Analysis of risk factors for glenoid bone defect in anterior shoulder instability. Am J Sports Med. 2011;39:1870–1876. doi: 10.1177/0363546511411699. [DOI] [PubMed] [Google Scholar]
- 4.Johnson L.L. Arthroscopy of the shoulder. Orthop Clin North Am. 1980;11:197–204. [PubMed] [Google Scholar]
- 5.Morgan C.D., Bodenstab A.B. Arthroscopic Bankart suture repair: Technique and early results. Arthroscopy. 1987;3:111–122. doi: 10.1016/s0749-8063(87)80027-0. [DOI] [PubMed] [Google Scholar]
- 6.Zuckerman J.D., Matsen F.A. Complications about the glenohumeral joint related to the use of screws and staples. J Bone Joint Surg Am. 1984;66:175–180. [PubMed] [Google Scholar]
- 7.Wolf E.M. Arthroscopic capsulolabral repair using suture anchors. Orthop Clin North Am. 1993;24:59–69. [PubMed] [Google Scholar]
- 8.Cole B.J., Romeo A.A. Arthroscopic shoulder stabilization with suture anchors: Technique, technology, and pitfalls. Clin Orthop Relat Res. 2001;390:17–30. doi: 10.1097/00003086-200109000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Kim S.H., Ha K.I., Cho Y.B., Ryu B.D., Oh I. Arthroscopic anterior stabilization of the shoulder: Two to six-year follow-up. J Bone Joint Surg Am. 2003;85:1511–1518. [PubMed] [Google Scholar]
- 10.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 11.Tauber M., Resch H., Forstner R., Raffl M., Schauer J. Reasons for failure after surgical repair of anterior shoulder instability. J Shoulder Elbow Surg. 2004;13:279–285. doi: 10.1016/j.jse.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 12.Cameron S.E. Arthroscopic reduction and internal fixation of an anterior glenoid fracture. Arthroscopy. 1998;14:743–746. doi: 10.1016/s0749-8063(98)70102-1. [DOI] [PubMed] [Google Scholar]
- 13.Porcellini G., Campi F., Paladini P. Arthroscopic approach to acute bony Bankart lesion. Arthroscopy. 2002;18:764–769. doi: 10.1053/jars.2002.35266. [DOI] [PubMed] [Google Scholar]
- 14.Millett P.J., Braun S. The “bony Bankart bridge” bridge procedure: A new arthroscopic technique for reduction and internal fixation of a bony Bankart lesion. Arthroscopy. 2009;25:102–105. doi: 10.1016/j.arthro.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Kim S.J., Kim T.W., Moon H.K., Chang W.H. A combined transglenoid and suture anchor technique for bony Bankart lesions. Knee Surg Sports Traumatol Arthrosc. 2009;17:1443–1446. doi: 10.1007/s00167-009-0845-6. [DOI] [PubMed] [Google Scholar]
- 16.Sugaya H., Kon Y., Tsuchiya A. Arthroscopic repair of glenoid fractures using suture anchors. Arthroscopy. 2005;21:625.e1–625.e5. doi: 10.1016/j.arthro.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 17.Bauer T., Abadie O., Hardy P. Arthroscopic treatment of glenoid fractures. Arthroscopy. 2006;22:569.e1–569.e6. doi: 10.1016/j.arthro.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 18.Zhang J., Jiang C. A new “double-pulley” dual-row technique for arthroscopic fixation of bony Bankart lesion. Knee Surg Sports Traumatol Arthrosc. 2011;19:1558–1562. doi: 10.1007/s00167-010-1390-z. [DOI] [PubMed] [Google Scholar]
- 19.Kim K.C., Rhee K.J., Shin H.D. Arthroscopic three-point double-row repair for acute bony Bankart lesions. Knee Surg Sports Traumatol Arthrosc. 2009;17:102–106. doi: 10.1007/s00167-008-0659-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Novel technique for arthroscopic transosseous fixation of a bony Bankart lesion.


