Abstract
Entrapment of the suprascapular nerve (SSN) is an increasingly recognized entity that can occur due to traction or compression-related etiology. Traction injuries of the SSN are unlikely to respond to surgical management and frequently improve with rest and avoidance of overhead activity. Compression injuries, on the other hand, frequently require surgical decompression for pain relief. SSN entrapment caused by compression at the suprascapular notch by the transverse scapular ligament gives rise to pain and atrophy of both the supraspinatus and infraspinatus muscles. However, compression at the spinoglenoid notch is more insidious because pain fibers may not be involved, causing isolated external rotation weakness. We present our preferred surgical technique for safe decompression of the SSN at the suprascapular and spinoglenoid notch using a subacromial and intra-articular approach, respectively. The key to ensuring efficient and uncomplicated decompression of the SSN relies on an intimate knowledge of the neurovascular anatomy and related landmarks.
Entrapment of the suprascapular nerve (SSN) is an increasingly recognized entity and should remain in the differential of otherwise unexplained shoulder pain or weakness. Though typically a diagnosis of exclusion, accurate diagnosis and treatment of this condition is essential for alleviating pain and preventing chronic supraspinatus or infraspinatus atrophy.1 The SSN, a branch off the upper trunk of the brachial plexus, contains contributions from C5, C6, and intermittently, C4. From the plexus, the nerve courses from anteromedial to posterolateral through the posterior triangle of the neck. It then passes through the suprascapular notch, which lies just medial to the base of the coracoid, 2 cm from the glenoid rim, and 3 cm from the supraglenoid tubercle2 (Fig 1). Sensory fibers contributing to the glenohumeral joint exit between the suprascapular notch and the transverse scapular ligament (TSL). From here, the nerve supplies motor function to the infraspinatus.
Figure 1.
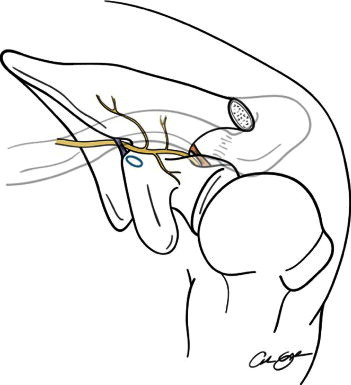
Anatomic schema displaying the course of the SSN from the brachial plexus (left side of image) to its muscular target. The SSN branches off the upper trunk of the brachial plexus and courses from anteromedial to posterolateral through the posterior triangle of the neck. It then passes through the suprascapular notch at the base of the coracoid under the TSL (labeled in purple). Sensory fibers travel to the glenohumeral joint while motor fibers innervate the supraspinatus muscle. The nerve then traverses the spinoglenoid notch under the variable spinoglenoid ligament (labeled in orange). From here, the nerve supplies motor function to the infraspinatus.
Suprascapular neuropathy can occur due to traction or compression-related etiology, and it is imperative to ascertain the cause before embarking on a treatment plan.3,4 Traction injuries of the SSN are unlikely to respond to surgical management and frequently improve with rest and avoidance of overhead activity. Compression injuries, on the other hand, frequently require surgical decompression for pain relief.
Compression at the suprascapular notch by the TSL gives rise to pain and atrophy of both the supraspinatus and infraspinatus muscles. However, compression at the spinoglenoid notch is more insidious because pain fibers may not be involved, causing isolated external rotation weakness. This is compounded by the ability of the teres minor to compensate for this decreased strength, presenting in vague fatigue-related weakness. Compression at this site is typically due to the spinoglenoid ligament or paralabral cysts5,6 (Fig 2).
Figure 2.
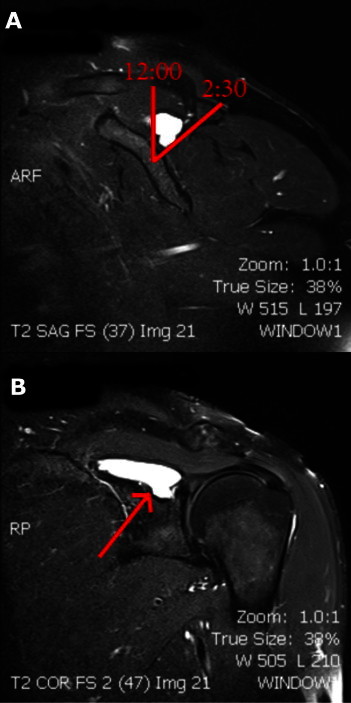
Compression of the SSN at the spinoglenoid notch may occur because of paralabral cysts such as the cyst pictured in this T2-weighted magnetic resonance sagittal cut image of the glenohumeral articulation at the level of the base of the coracoid. (A) Before arthroscopy, the surgeon should try to be aware of the cyst's exact clock-face location relative to the glenoid in the sagittal plane to know where to search for the cyst (e.g., 12 o'clock to 2:30 position). (B) The arrow points to a large paralabral cyst, which is frequently associated with SLAP lesions.
We present our preferred surgical technique for safe decompression of the SSN at the suprascapular and spinoglenoid notch using a subacromial and intra-articular approach, respectively. Advantages to using an arthroscopic approach include the ability to directly visualize the nerve without disruption of musculature, a decreased theoretic risk of iatrogenic neurovascular injury, and decreased postoperative morbidity. The primary limitation of this approach is that it requires the surgeon to have an excellent grasp of pertinent anatomy. Thus the key to ensuring efficient and uncomplicated decompression of the SSN relies on an intimate knowledge of the neurovascular structures and related landmarks (Table 1).
Table 1.
Pearls and Common Pitfalls in Arthroscopic SSN Decompression
| Pearls | Pitfalls |
|---|---|
| Rely on your knowledge of anatomy | Incomplete cyst decompression |
| TSL always medial to base of conoid ligament | Failure to recognize ossified TSL |
| SSN 2-3 cm medial | Poor visualization of SSN |
| Use blunt trocar to protect SSN | Excessive medial capsular dissection |
| Operate efficiently | |
| Use SLAP approach to reach cyst | |
| Visualize SSN during TSL release | |
| Debride cyst wall entirely |
Surgical Technique
Patient Setup
Although a lateral decubitus position may be useful when one is addressing concomitant SLAP pathology, it is our preference to place patients in the beach-chair position for this technique. To achieve adequate hemostasis, the operating room and anesthesia staff should be instructed to maintain pump pressure at 50 mm Hg with a systolic blood pressure of approximately 100 mm Hg. After sterile preparation and draping of the shoulder, the acromion, distal clavicle, and coracoid process are outlined with a marking pen (Fig 3). The general course of the SSN is also provisionally outlined to give the surgeon an anatomic perspective.
Figure 3.
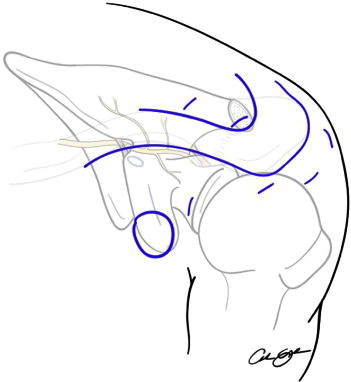
Anatomic schema displaying the surface anatomy and underlying course of the SSN in a left shoulder. After sterile preparation and draping of the shoulder, the acromion, distal clavicle, and coracoid process are outlined with a marking pen. The portal sites should also be marked (shown in blue) before insufflation because palpable anatomic landmarks can be lost with intraoperative edema. The posterior, midlateral, anterolateral, anterior, Neviaser, and accessory Neviaser portals are marked.
Diagnostic Arthroscopy
After creation of a posterior portal approximately 3 cm directly inferior to the posterolateral corner of the acromion, a 30° arthroscope is inserted into the glenohumeral joint and a diagnostic arthroscopy is performed. An anterior portal can be created in the rotator interval with an outside-in technique by use of an 18-gauge spinal needle. Particular attention should be directed toward the superior labrum, because a SLAP tear is generally present in patients with spinoglenoid notch cysts.
Transarticular Spinoglenoid Notch Decompression
If the patient has a SLAP tear that will need to be addressed, it is recommended to decompress the spinoglenoid notch cyst from a sublabral approach before repair (Fig 4). Decompression of the spinoglenoid notch does not necessarily require direct visualization of the SSN as in releasing the TSL. Though a source of controversy, it is our preference to decompress the cyst associated with a SLAP tear, opposed to repair alone.
Figure 4.
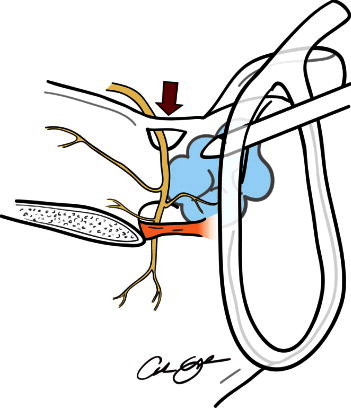
Anatomic schema showing a posterior view of a right shoulder. The probe entering from the right from an anterolateral portal is elevating a labral tear to evacuate a paralabral ganglion cyst (shown in yellow) that is compressing the SSN at the spinoglenoid notch (shown in orange). Typically, an egress of cloudy fluid is encountered with disturbance of the cyst. When one is performing subacromial SSN release, in rare cases, the TSL may be ossified (arrow). In these instances, it is described as a type VI TSL and usually needs to be taken down with a quarter-inch osteotome.
Before arthroscopy, the surgeon should try to be aware of the cyst's exact “clock-face” location relative to the glenoid in the sagittal plane to know where to search for the cyst (e.g., 1 o'clock to 3 o'clock) (Fig 2A). This location is best ascertained from magnetic resonance imaging and is an essential component of the preoperative plan. Type I SLAP tears can be gently debrided and dissection then carried out between the remaining labrum and capsule for cyst decompression.
To perform cyst decompression, the arthroscope should be in the posterior portal while an accessory anterolateral portal is established 2 cm lateral to the anterolateral corner of the acromion and anterior to the anterior aspect of the supraspinatus. A capsulotomy can then be performed starting at the biceps origin and moving posterior to the area of interest using an arthroscopic scissors brought in from the anterior portal. On completion of the capsulotomy, a switching stick is inserted into the anterolateral portal and used to probe into the cyst (Fig 4). Typically, an egress of cloudy fluid is encountered with this step. The camera is then switched to the anterior portal to visualize the capsule through another angle. A shaver and switching stick can be introduced through the posterior or accessory anterolateral portal for further cyst decompression. When one is using the shaver, it is important to remember that the SSN lies 1.5 cm medial to the glenoid rim and can be injured if debridement is carried too medially.
Subacromial Spinoglenoid Notch Decompression
In cases where it is ambiguous whether the cyst was successfully decompressed intra-articularly, a subacromial approach for spinoglenoid notch decompression may be used. Standard anterior, midlateral, and posterior portals are established, and a complete bursectomy is performed. The camera is placed in the midlateral portal so that further medial bursectomy can be performed and good visualization of the scapular spine can be achieved. The supraspinatus and infraspinatus muscle bellies lie anterior and posterior to this landmark, respectively. At the base of the scapular spine, the SSN is located in the spinoglenoid notch and should be avoided when one is using a mechanical shaver. The SSN runs from the deep undersurface of the supraspinatus to the floor of the notch before innervating the infraspinatus. By use of a probe, the posterior glenoid can be palpated and the cyst sometimes localized. The mechanical shaver, Wissinger rod, and radiofrequency device (ArthroCare, Austin, TX) can also be advanced from anterior to posterior for further cyst decompression and debridement of thickened soft tissue within the notch. However, great care must be taken to avoid SSN injury.
Subacromial Suprascapular Notch Decompression
For decompression of the TSL, the arthroscope is placed subacromially through the posterior portal and the shaver introduced laterally to allow debridement of the subacromial bursa. Video 1 shows a review of the surgical technique. The bursa should be debrided until there is clear visualization of the coracoacromial ligament anteriorly. At this point, the arthroscope should be inserted through the lateral portal, reorienting oneself to the coracoacromial ligament, and the shaver and electrocautery can be introduced through either the posterior or anterior portal. Dissection is carried out anteromedially in the plane anterior to the supraspinatus until the coracoid and coracoclavicular ligaments are encountered and can be further exposed (Fig 5). The conoid ligament is followed inferiorly to the base of the coracoid, which lies just lateral to the suprascapular notch. This landmark is crucial for proper orientation and underscores the need to have good exposure of adjacent structures and adequate hemostasis.
Figure 5.
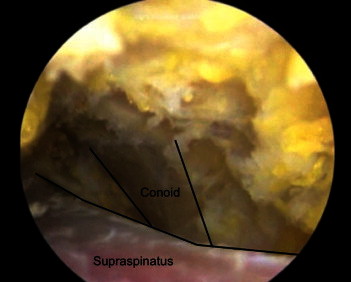
Image from a right shoulder arthroscopy with the camera viewing from the midlateral portal showing the view of the conoid ligament after dissection medial along the anterior edge of the supraspinatus. This ligament is an important landmark because the TSL and SSN lie at the base of the conoid ligament.
Once the conoid has been identified and exposed carefully, an accessory Neviaser portal can be established with a spinal needle 2 cm medial to the standard Neviaser position. A switching stick is inserted and used to further dissect and provide retraction of the SSN. The switching stick can also be used to palpate the TSL, located at the conoid ligament's base, and to bluntly retract the suprascapular vasculature, which typically runs superior to the TSL. At this juncture, a spinal needle should then be introduced in the standard Neviaser portal (working portal) and visualized to easily reach the TSL. The portal is established, and further exposure of the TSL is carried out with a blunt probe. Adipose tissue inferior to the TSL is gently pushed inferiorly to protect the SSN. The TSL can then be released under direct visualization with a straight biter (Arthrex, Naples, FL) introduced through the Neviaser working portal followed by a shaver to trim the excess tissue. In rare cases, when an ossified (type VI) ligament is encountered, a quarter-inch osteotome can accomplish the same task (Fig 4). After TSL release, the SSN is gently probed to ensure complete release (Fig 6).
Figure 6.
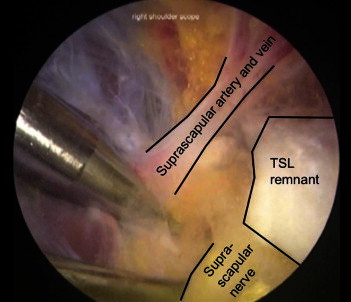
Image from a right shoulder arthroscopy with the camera viewing from the anterolateral portal showing the view of the SSN after resection of the TSL. The suprascapular artery and vein can be seen passing above the resected end of the ligament.
Discussion
As orthopaedic surgeons become more aware of suprascapular neuropathy and arthroscopic decompressions are performed with increasing frequency,7 clinical understanding of suprascapular neuropathy has improved. Several recent series have shown excellent results with arthroscopic decompression, with 100% of patients having improvement in their sensory disturbance8 and 75% of patients showing functional improvement as measured with the American Shoulder and Elbow Surgeons score.9 One recent comparative retrospective cohort study has also shown significantly greater improvement in external rotation strength in patients with SLAP tears undergoing concomitant repair and decompression of the SSN at the spinoglenoid notch as compared with those undergoing labral repair alone.10 With these improvements, it is important to remember the potential for iatrogenic SSN injury from either suture anchors placed for labral stabilization11 or screw fixation for Latarjet glenoid augmentation.12 However, several important clinical questions remain unanswered. For instance, massive rotator cuff tears medialize the innervated target muscle fibers and can result in suprascapular neuropathy due to traction phenomena. Repair may decrease this traction, but the difficulty remains in indicating patients for release where the nerve has become adhered. Further research will be necessary to more fully understand the role of decompression, as well as the long-term outcomes of arthroscopic decompression.
Suprascapular neuropathy is relatively uncommon, comprising only 4.5% of new patients presenting to an academic referral shoulder practice in 1 series.13 However, suprascapular neuropathy is an important pathologic entity for surgeons evaluating shoulder complaints because the diagnosis can be obscure and is often missed. Keeping a high index of suspicion is arguably the most important aspect of treating suprascapular neuropathy.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary data
Surgical technique for arthroscopic decompression of the SSN at the suprascapular notch with resection of the TSL. The positioning, approach, pertinent anatomic structures encountered during the exposure, and relevant pathology are reviewed. Pearls and pitfalls are also reviewed as they are encountered.
References
- 1.Lafosse L., Tomasi A., Corbett S., Baier G., Willems K., Gobezie R. Arthroscopic release of suprascapular nerve entrapment at the suprascapular notch: Technique and preliminary results. Arthroscopy. 2007;23:34–42. doi: 10.1016/j.arthro.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Bigliani L.U., Dalsey R.M., McCann P.D., April E.W. An anatomical study of the suprascapular nerve. Arthroscopy. 1990;6:301–305. doi: 10.1016/0749-8063(90)90060-q. [DOI] [PubMed] [Google Scholar]
- 3.Warner J.P., Krushell R.J., Masquelet A., Gerber C. Anatomy and relationships of the suprascapular nerve: Anatomical constraints to mobilization of the supraspinatus and infraspinatus muscles in the management of massive rotator-cuff tears. J Bone Joint Surg Am. 1992;74:36–45. [PubMed] [Google Scholar]
- 4.Ferretti A., De Carli A., Fontana M. Injury of the suprascapular nerve at the spinoglenoid notch: The natural history of infraspinatus atrophy in volleyball players. Am J Sports Med. 1998;26:759–763. doi: 10.1177/03635465980260060401. [DOI] [PubMed] [Google Scholar]
- 5.Piasecki D.P., Romeo A.A., Bach B.R., Jr, Nicholson G.P. Suprascapular neuropathy. J Am Acad Orthop Surg. 2009;17:665–676. doi: 10.5435/00124635-200911000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Westerheide K.J., Dopirak R.M., Karzel R.P., Snyder S.J. Suprascapular nerve palsy secondary to spinoglenoid cysts: Results of arthroscopic treatment. Arthroscopy. 2006;22:721–727. doi: 10.1016/j.arthro.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 7.Moen T.C., Babatunde O.M., Hsu S.H., Ahmad C.S., Levine W.N. Suprascapular neuropathy: What does the literature show? J Shoulder Elbow Surg. 2012;21:835–846. doi: 10.1016/j.jse.2011.11.033. [DOI] [PubMed] [Google Scholar]
- 8.Oizumi N., Suenaga N., Funakoshi T., Yamaguchi H., Minami A. Recovery of sensory disturbance after arthroscopic decompression of the suprascapular nerve. J Shoulder Elbow Surg. 2012;21:759–764. doi: 10.1016/j.jse.2011.08.063. [DOI] [PubMed] [Google Scholar]
- 9.Shah A.A., Butler R.B., Sung S.-Y., Wells J.H., Higgins L.D., Warner J.J.P. Clinical outcomes of suprascapular nerve decompression. J Shoulder Elbow Surg. 2011;20:975–982. doi: 10.1016/j.jse.2010.10.032. [DOI] [PubMed] [Google Scholar]
- 10.Pillai G., Baynes J.R., Gladstone J., Flatow E.L. Greater strength increase with cyst decompression and SLAP repair than SLAP repair alone. Clin Orthop Relat Res. 2011;469:1056–1060. doi: 10.1007/s11999-010-1661-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim S.-H., Koh Y.-G., Sung C.-H., Moon H.-K., Park Y.-S. Iatrogenic suprascapular nerve injury after repair of type II SLAP lesion. Arthroscopy. 2010;26:1005–1008. doi: 10.1016/j.arthro.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 12.Lädermann A., Denard P.J., Burkhart S.S. Injury of the suprascapular nerve during Latarjet procedure: An anatomic study. Arthroscopy. 2012;28:316–321. doi: 10.1016/j.arthro.2011.08.307. [DOI] [PubMed] [Google Scholar]
- 13.Boykin R.E., Friedman D.J., Zimmer Z.R., Oaklander A.L., Higgins L.D., Warner J.J.P. Suprascapular neuropathy in a shoulder referral practice. J Shoulder Elbow Surg. 2011;20:983–988. doi: 10.1016/j.jse.2010.10.039. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for arthroscopic decompression of the SSN at the suprascapular notch with resection of the TSL. The positioning, approach, pertinent anatomic structures encountered during the exposure, and relevant pathology are reviewed. Pearls and pitfalls are also reviewed as they are encountered.


