Abstract
Despite growing interest in hip arthroscopy and labral preservation, some patients have severely damaged, degenerative, or deficient labrums and may be candidates for arthroscopic labral reconstruction. The ligamentum teres has been used as a graft source for open hip labral grafting, and the iliotibial band has been used in the arthroscopic setting. We present an alternative method of hip labral reconstruction using the gracilis autograft, which does not require post-harvest manipulation. Arthroscopic techniques for graft tensioning and labrum-graft overlap are introduced that may facilitate restoration of labral function in patients with otherwise non-salvageable labrums.
The acetabular labrum appears to have a significant role in hip preservation. The supple labrum acts as a gasket apposing the femoral head chondral surface, providing a fluid seal effect that may optimize hip microstability and contact force distribution.1,2 Recent dramatic examples of iatrogenic instability in the form of hip subluxation3 and hip dislocation4 have been attributed to uncorrected labral deficiency. Because of the potential benefit of the intact acetabular labrum on hip preservation, there is a growing trend toward labral preservation.5,6
Until recently, surgical options for management of pathologic labral tissue included debridement, labral repair, and labral refixation (when repaired to an altered attachment site, e.g., after acetabular rim trimming). However, the labrum may not always be salvageable. In such cases, labral reconstruction may restore a fluid seal and theoretically prolong hip longevity.7 Thus labral reconstruction may be considered in patients with severely damaged, degenerative, and/or deficient tissue deemed non-salvageable with currently available techniques (Table 1).
Table 1.
Suggested Indications for Hip Labral Reconstruction
| Non-salvageable acetabular labrum (insufficient quality and/or quantity) |
| Absent/insufficient longitudinal (global or segmental) labral tissue |
| Traumatic |
| Degenerative |
| Iatrogenic (e.g., after labrectomy, labral suture cut-through, or labral damage during joint access) |
| Insufficient labral width |
| Traumatic |
| Degenerative |
| Iatrogenic |
| Insufficient labral quality |
| Ossification |
| Global |
| Focal (one should note that these may be reparable after careful resection of ossified regions) |
| Traumatic |
| Degenerative |
| Age |
| Perhaps = or < 50 yr |
| Physiologic age including absence of medical comorbidities and any osteoarthrosis may extend this arbitrary age criterion |
| Absence of significant osteoarthrosis (Tönnis grade 0 or 1) |
In contrast to the rapid growth in hip preservation and hip arthroscopy literature, there are only 2 published case series on labral reconstruction. The incised and unfolded ligamentum teres (round ligament) has been published as a graft source for reconstruction in the open dislocation setting,7 and the tubularized iliotibial band has been used (with encouraging preliminary outcomes) in the arthroscopic setting.8 In this technical note we introduce arthroscopic hip labral reconstruction using the gracilis (or semitendinosus) autograft as an alternate graft source and present new techniques that may facilitate labral fluid seal restoration in select patients with otherwise non-salvageable labrums.
Technique
We perform dual-portal supine arthroscopic hip surgery with the patient under general anesthesia. The fluoroscopic templating technique9 is routinely used; by aligning the pelvis in the coronal and sagittal planes with the vertical C-arm device, hip positioning is standardized. A 70° arthroscope is used in the anterolateral portal, and instrumentation is performed through the modified midanterior portal (MMAP). The MMAP is approximately 3 cm anterior and 4.5 mm distal to the anterolateral portal, adjusted proportionately for patient size, and is more lateral and proximal than the midanterior portal. Interportal capsulotomy facilitates instrument navigation and arthroscopic visualization. The condition of the labrum and the extent of pathologic involvement, as well as any segmental and/or width deficiency, are determined. Table 1 summarizes the indications for labral reconstruction.
The non-salvageable labrum is debrided back to stable margins. Arthroscopic acetabuloplasty is performed in patients with pincer impingement by fluoroscopic templating. A typical labral longitudinal defect after anterosuperior debridement may be approximately 2.5 cm; we will use this example. The acetabular rim is prepared for labral graft fixation by predrilling suture anchor sites under arthroscopic and fluoroscopic guidance with care taken to avoid iatrogenic articular cartilage damage (Fig 1). We use anterior-posterior fluoroscopic confirmation of safe drilling divergent from the articular cartilage at the direct superior acetabular rim. Because the pelvis is aligned in the coronal and sagittal planes during setup, drilling parallel to the floor while viewing the adjacent articular cartilage permits safe anterior rim preparation. We have found that drilling from the MMAP typically permits safe anchor placement for the posterior rim when needed in cases of global pincer impingement (i.e., coxa profunda or protrusio acetabuli) with concomitant global acetabuloplasty and labral refixation or reconstruction. Although performing interportal exchange is always an option, we have been able to perform the vast majority of procedures including labral reconstruction without doing so. Intentional intimate overlap of the ends of the labral graft with the native labrum is achieved by drilling on the capsular side of the native labral margin. Typically, 4 to 5 suture anchors with 8 mm of spacing are used to span this segmental labral defect.
Figure 1.
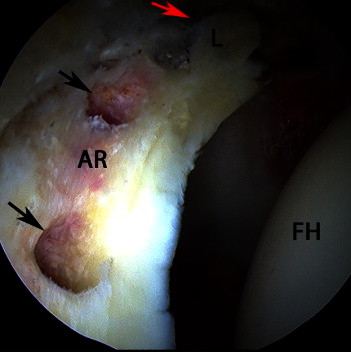
Supine arthroscopic view of right hip with 70° arthroscope in anterolateral portal showing anterosuperior acetabulum after rim trimming and predrilling of suture anchor sites (black arrows) close to but not in violation of acetabular articular cartilage. The red arrow indicates the location of the anterior suture anchor drill hole, which is hidden by the stable labral margin (L); the posterosuperior drill hole is not visible in the field of view. (AR, acetabular rim; FH, femoral head.)
Once the rim has been prepared, the instruments are atraumatically removed from the hip and traction released; we also release contralateral counter-distraction to minimize traction-related complications. The ipsilateral knee is flexed to approximately 90° and allowed to gravitate into external rotation (figure-of-4 position) to facilitate autograft harvest through a 2-cm vertical incision just medial and distal to the tibial tuberosity. Harvest of the gracilis tendon (or adjacent semitendinosus tendon if a larger labral graft is desired) is performed; in this example we would perform harvesting of a graft approximately 2 cm longer than the estimated labral defect length while avoiding the saphenous nerve and the superficial medial collateral ligament. Suture preparation of the labral graft is completed on a sterile table with the secure application of a No. 2 nonabsorbable whip stitch to each end and 2 to 3 intercalary simple midsubstance stitches (Fig 2).
Figure 2.
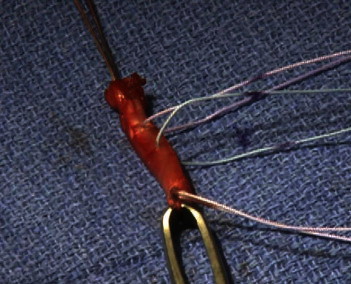
Gracilis autograft after suture placement. The simple midsubstance sutures and whip stitches at the terminal ends should be noted.
We use a knotless anchor insertion device (PushLock; Arthrex, Naples, FL) attached to 1 pair of the terminal end sutures to insert the fully prepared graft construct into the hip joint through an 8.25-mm clear cannula positioned in the MMAP (Figs 3 and 4). Fixation of the labral graft begins at the acetabular rim anchor site furthest from the arthroscopic lens (typically anterior) with successive fixation sequentially performed toward the lens (typically superior or posterosuperior) to minimize obstructed arthroscopic visualization.
Figure 3.

Passage of fully prepared labral graft construct through cannula in MMAP. The arthroscope is in the anterolateral portal of the right hip.
Figure 4.
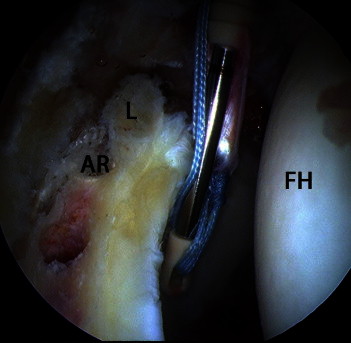
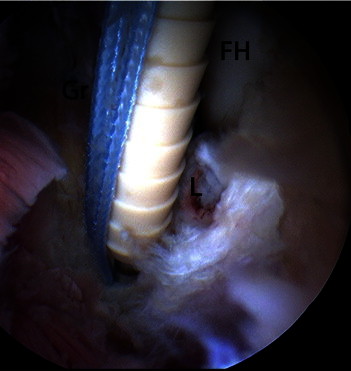
Supine arthroscopic view of gracilis autograft being “pulled” via terminal sutures into central compartment of right hip before initial anchor fixation “behind” anterior labral margin (L) onto acetabular rim (AR). (FH, femoral head.)
The leading graft end is partially inserted into a 3.2-mm drill hole with the suture anchor inserter, followed by deployment of the 3.5-mm anchor with an interference fit (Fig 5). If the graft does not enter the 3.2-mm anchor site, we will slightly widen the entrance with an arthroscopic blunt obturator tip. The midsubstance suture anchors secure the graft along the acetabular rim. The “tail” end of the gracilis graft is inserted into the final anchor site located in an overlapping position with the debrided labral margin (Fig 6). It is during this step that controlled graft tensioning is performed so that a favorable force vector of this arced tendon toward the femoral head centroid occurs, encouraging a fluid seal by direct graft apposition to the femoral head (Fig 7). Moreover, in situ graft tensioning and deployment of the final knotless suture anchor buttress and compress the capsular side of the native labral margins for a conceptually similar net effect. The desired result is a labral construct with some capsular-side overlap adjacent to the stable native labral margins re-creating an immediate fluid seal without any end-to-end gap (Fig 8).
Figure 5.
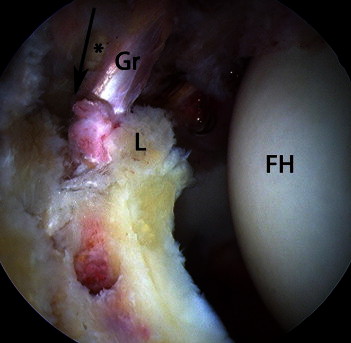
Supine arthroscopic view of right hip during partial insertion of leading end of gracilis autograft (Gr) into first suture anchor drill site with intimate contact and intentional overlap with labral margin (L). The arrow shows the direction of the suture anchor (asterisk) placement into the acetabular rim. (FH, femoral head.)
Figure 6.
Supine arthroscopic view of right hip showing terminal end of gracilis autograft (Gr) being seated into final suture anchor site in overlapped position with posterosuperior labral remnant (L) permitting graft tensioning just before deployment of suture anchor. (FH, femoral head.)
Figure 7.
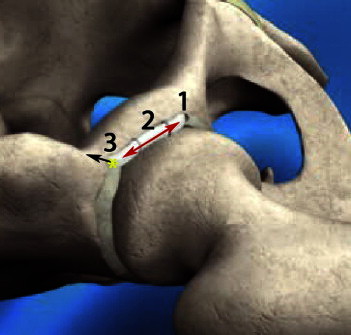
Animated image of right hip showing key steps of graft fixation to acetabular rim: 1, seating and fixation of leading autograft end into anterior suture anchor site; 2, labral graft fixation of intercalary section to anterosuperior rim; and 3, seating of “tail” end of graft into final suture anchor site in direction of black arrow with resultant tensioning of graft (red arrow) before final knotless suture anchor fixation to facilitate fluid seal. The yellow asterisk shows the region of intentional overlap at the labrum-graft junction.
Figure 8.
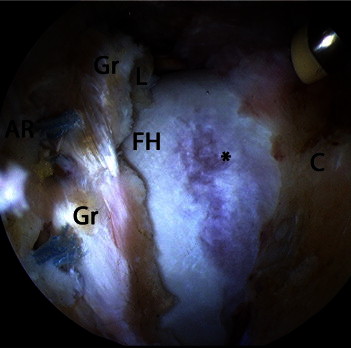
Supine arthroscopic view of right hip after dual-portal arthroscopic acetabuloplasty and labral reconstruction with gracilis autograft (Gr) and preceding femoroplasty of cam deformity of femoral head-neck junction (asterisk). Two sites of suture anchor fixation can be seen. One should note the overlap of the graft with the labral remnant (L) and the restored fluid seal. The posterosuperior anchor site overlapping the corresponding labral margin cannot be seen on this view. (AR, acetabular rim; C, capsule; FH, femoral head.)
We typically then perform any needed arthroscopic femoral head-neck resection osteoplasty through the MMAP to eradicate any cam component of femoroacetabular impingement (FAI), thereby protecting the labral graft from subsequent mechanical failure (Fig 9). The procedure is similar if labral reconstruction with the larger semitendinosus tendon is desired and may be performed in single-stage bilateral procedures (Fig 10). We have summarized surgical pearls and pitfalls in Table 2 and have included a supplemental video emphasizing key concepts and technical steps of this procedure (Video 1).
Figure 9.
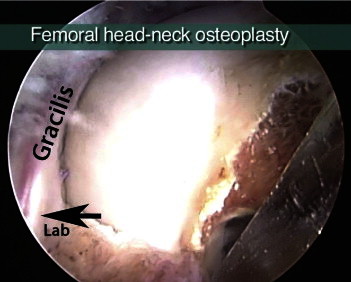
Supine arthroscopic view of right hip showing gracilis autograft overlapping posterosuperior labral remnant (Lab) with restoration of fluid seal as femoroplasty is performed to eradicate cam impingement and prevent mechanical conflict with labral construct.
Figure 10.
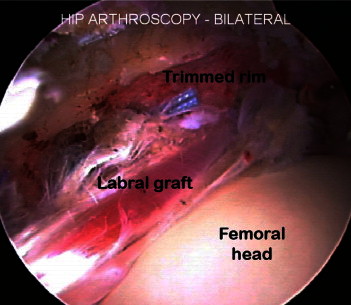
Supine arthroscopic image of right hip of another patient who underwent single-staged bilateral arthroscopic surgery for cam-pincer femoroacetabular impingement with labral reconstruction performed on the right hip and labral refixation performed on the left hip. One should note the fluid seal of the gracilis graft with the femoral head and the junctional overlap with the labral margin at the right side of the image.
Table 2.
Pearls and Pitfalls of Hip Labral Reconstruction With Gracilis Autograft
| Pearls | Pitfalls |
|---|---|
|
|
Permit an immediate fluid seal restoration.
Compromising fluid seal restoration.
The postoperative protocol is similar to that of our patients undergoing arthroscopic labral refixation with concomitant acetabuloplasty and/or femoroplasty. The labral reconstruction does not alter our outpatient protocol with institution of early low-resistance exercise cycling (as early as postoperative day 1), crutch-protected ambulation for 2 weeks (6 weeks in cases of microfracture chondroplasty), jogging chest deep in a pool and/or freestyle swimming (when incisions healed), elliptical trainer use at 4 weeks, and running/jumping at 12 weeks (with typical femoroplasty). Our protocol is similar for patients who have undergone single-stage bilateral arthroscopic FAI surgery (with or without labral reconstruction) because we have found that these patients prefer immediate crutch-protected ambulation over even short-term wheelchair use.
Discussion
The goals of hip labral surgery include symptomatic relief/functional improvement and hip preservation through the retention or restoration of labral function. Arthroscopic hip labral reconstruction may play an expanding role in the less invasive management of select patients with severe labral insufficiency whether in quantity or in quality. Although evidence suggests that selective labral debridement (not segmental labrectomy) may yield durable successful long-term outcomes,10,11 several studies suggest that labral refixation, at least in the setting of FAI, yields better clinical outcomes.5,6,12 Despite theoretic basic science support for the preservation or restoration of labral function, the clinical evidence for this conceptually rational procedure is very limited and merits further investigation. The open labral reconstruction case series using the ligamentum teres autograft included 5 patients with minimum 5-month follow-up, limiting conclusions.7 A recent larger arthroscopic series using the iliotibial band autograft had encouraging outcomes with 12-month minimum follow-up.8 Until further evidence suggests otherwise, we choose to perform labral reconstruction in relatively young, active patients without advanced degenerative change (i.e., Tönnis grade 0 or 1) when the labrum is not salvageable by selective debridement or repair/refixation. We do not consider grade 3 or 4 chondral damage at the anterior and/or superior rim to be a contraindication to labral reconstruction if the visibly damaged cartilage can be safely removed during acetabuloplasty without causing iatrogenic dysplasia from inadvertent over-resection. Fluoroscopic techniques and recent formulas may facilitate precision acetabuloplasty.9,13-15 Arthroscopic femoroplasty is important not only to eradicate cam impingement but to prevent early mechanical failure of the labral graft construct. We have not had inadvertent damage to the reconstructed labrum during subsequent femoroplasty but would support femoroplasty preceding labral reconstruction if desired.
Labral pathology commonly occurs because of FAI16; most of our labral reconstructions occur in this setting. We do not recommend labral reconstruction as an isolated procedure sans acetabuloplasty and/or femoroplasty in patients with FAI; causative skeletal deformities should be addressed lest chondrolabral procedures fail. However, it may have value as an isolated procedure in some instances (e.g., to treat severe labral deficiency in the setting of normal or borderline dysplastic acetabular morphology or to provide clot containment of acetabular rim full-thickness cartilage defects undergoing microfracture chondroplasty in the setting of labral insufficiency).
Arthroscopic hip labral reconstruction with the gracilis tendon offers potential benefits of a homogeneous autograft requiring no post-harvest manipulation with universal availability through a user-friendly harvest from the knee familiar to many surgeons. The adjacent larger semitendinosus tendon is an immediately available option that may be desirable, for example, to reconstruct the hypertrophic labrum in the dysplastic acetabulum (possibly with periacetabular osteotomy). External graft suturing and intra-articular insertion of the fully prepared graft construct encourage a surgeon-friendly approach to an inherently challenging arthroscopic procedure. Suture anchor systems that permit insertion of the graft ends into the terminal anchor sites allow graft tensioning, theoretic osteointegration, and flexibility in graft length. Finally, by overlapping the free graft ends in intimate contact with the capsular side of the native labral margins, a combination of graft tensioning and buttressing effect may immediately restore a fluid seal even at the graft–native labrum junction. We anticipate the future evolution of labral reconstruction with other autograft and allograft sources (M. Philippon, oral communication, August 2010) and are aware of at least 1 other autograft (reflected head of rectus femoris) that has been used in this capacity (T. Sampson, oral communication, October 2011). We submit that this technique gives surgeons another option for hip labral reconstruction that may be used with open dislocation, mini-open, or arthroscopic methods. A clinical investigation with 2-year minimum follow-up is under way.
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
Supplementary data
References
- 1.Ferguson S.J., Bryant J.T., Ganz R., Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;36:171–178. doi: 10.1016/s0021-9290(02)00365-2. [DOI] [PubMed] [Google Scholar]
- 2.Crawford M.J., Dy C.J., Alexander J.W. The 2007 Frank Stinchfield Award: The biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res. 2007;465:16–22. doi: 10.1097/BLO.0b013e31815b181f. [DOI] [PubMed] [Google Scholar]
- 3.Benali Y., Katthagen B.D. Hip subluxation as a complication of arthroscopic debridement. Arthroscopy. 2009;25:405–407. doi: 10.1016/j.arthro.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 4.Matsuda D.K. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy. 2009;25:400–404. doi: 10.1016/j.arthro.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 5.Espinosa N., Rothenfluh D.A., Beck M., Ganz R., Leunig M. Treatment of femoro-acetabular impingement: Preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88:925–935. doi: 10.2106/JBJS.E.00290. [DOI] [PubMed] [Google Scholar]
- 6.Larson C.M., Giveans M.R. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369–376. doi: 10.1016/j.arthro.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 7.Sierra R.J., Trousdale R.T. Labral reconstruction using the ligamentum teres capitis: Report of a new technique. Clin Orthop Relat Res. 2009;467:753–759. doi: 10.1007/s11999-008-0633-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Philippon M.J., Briggs K.K., Hay C.J., Kuppersmith D.A., Dewing C.B., Huang M.J. Arthroscopic labral reconstruction in the hip using iliotibial band autograft: Technique and early outcomes. Arthroscopy. 2010;26:750–756. doi: 10.1016/j.arthro.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 9.Matsuda D.K. Fluoroscopic templating technique for precision arthroscopic rim trimming. Arthroscopy. 2009;25:1175–1182. doi: 10.1016/j.arthro.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 10.Byrd J.W., Jones K.S. Hip arthroscopy for labral pathology: Prospective analysis with 10-year follow-up. Arthroscopy. 2009;25:365–368. doi: 10.1016/j.arthro.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 11.McCarthy J.C., Jarrett B.T., Ojeifo O., Lee J.A., Bragdon C.R. What factors influence long-term survivorship after hip arthroscopy? Clin Orthop Relat Res. 2011;469:362–371. doi: 10.1007/s11999-010-1559-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Philippon M.J., Briggs K.K., Yen Y.M., Kuppersmith D.A. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: Minimum two-year follow-up. J Bone Joint Surg Br. 2009;91:16–23. doi: 10.1302/0301-620X.91B1.21329. [DOI] [PubMed] [Google Scholar]
- 13.Larson C.M., Wulf C.A. Intraoperative fluoroscopy for evaluation of bony resection during arthroscopic management of femoroacetabular impingement in the supine position. Arthroscopy. 2009;25:1183–1192. doi: 10.1016/j.arthro.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 14.Philippon M.J., Wolff A.B., Briggs K.K., Zehms C.T., Kuppersmith D.A. Acetabular rim reduction for the treatment of femoroacetabular impingement correlates with preoperative and postoperative center-edge angle. Arthroscopy. 2010;26:757–761. doi: 10.1016/j.arthro.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Colvin A.C., Koehler S.M., Bird J. Can the change in center-edge angle during pincer trimming be reliably predicted? Clin Orthop Relat Res. 2011;469:1071–1074. doi: 10.1007/s11999-010-1581-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wenger D.E., Kendell K.R., Miner M.R., Trousdale R.T. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004:145–150. doi: 10.1097/01.blo.0000136903.01368.20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


