Abstract
Establishing the introductory viewing portal is a key step in hip arthroscopy. Most hip arthroscopists initially gain access to the central compartment of the hip through the anterolateral portal. Iatrogenic injury to the labrum or the femoral head chondral surface is a common yet under-reported complication of the procedure. Instead of directing the needle toward the clear space of the distracted joint, labral penetration can be minimized by directing the needle slightly anteroinferior to the clear space, overlapping the superior femoral head. Femoral head scuffing can be minimized by adjusting the position of the beveled needle and confirming a straight guidewire trajectory before trocar placement. This technical note addresses surgical pearls to minimize iatrogenic injury during initial central compartment access.
The utility of hip arthroscopy has certainly increased over the past decade. This procedure was initially used for diagnostic purposes and for simple procedures such as labral debridement and loose body removal. With an improved understanding of hip pathology, hip arthroscopy has been increasingly used to address intra-articular pathology including femoroacetabular impingement, internal snapping hip, and several other conditions.
Hip arthroscopy has a difficult learning curve. Although the first documented hip arthroscopies were performed in the early 1900s, the utility of this procedure is still in its infancy compared with other arthroscopically treated joints.1 Currently, there is a paucity of opportunities to learn the procedure because few residencies and fellowships offer adequate training in hip arthroscopy.
One of the technical challenges encountered during hip arthroscopy occurs with establishing the introductory portal. Although there are multiple approaches described to access the hip,2-4 initial setup of the anterolateral portal into the central compartment is currently the most common. Previously published drawings and fluoroscopic figures appear to recommend aiming for the clear space of the distracted hip joint when establishing this portal5-9 (Fig 1). This is typically accomplished under fluoroscopic assistance. However, without direct visualization of the hip joint, there is a risk of iatrogenic injury to the labrum or femoral head articular surface from the needle and trocar. Strategies to minimize labral injury include using adequate distraction, joint distention, and tactile feedback, as well as spinal needle repositioning (Video 1).
Figure 1.

Fluoroscopic image with the spinal needle aiming at the radiolucent clear space in a right hip in the supine position. The clear space is defined as the radiographic interval between the bony structures of the superior femoral head and inferior edge of the acetabulum. The labrum lies within this space but is not visualized radiographically and is therefore at risk.
Despite strategies to protect the labrum during initial portal placement, risk of injury can be high. A recent study reported an iatrogenic labral puncture rate of 20% (50 of 250).6 Initial spinal needle placement is paramount to minimize iatrogenic injury. An understanding of the 3-dimensional anatomy may explain a high rate of labral injury when directing the initial portal toward the clear space. When aiming for the clear space, anterior placement is safe but posterior placement will penetrate the labrum. Unfortunately, placement of a needle in the clear space on a fluoroscopic image only confirms the superior/inferior location using a 2-dimensional anteroposteriorly directed fluoroscopic image, whereas the anteroposterior location can be difficult to discern. Both of these positions will look the same on an anteroposterior fluoroscopic image to the surgeon. However, if the spinal needle is aimed to overlap the superior dome of the femoral head, the spinal needle will need to be positioned anterior to the femoral head to allow access to the central compartment and therefore positioned away from the labrum (Fig 2). Thus this technique minimizes the chances of iatrogenic labral injury in establishing the introductory portal.
Figure 2.
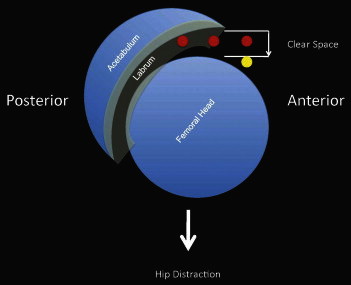
Traditional introductory portal trajectory along the radiographic clear space (red dots) compared with a position anterior to the femoral head (yellow dot) and its relation to the labrum.
The purpose of this technical note is to specifically address initial anterolateral portal placement to minimize iatrogenic injury to the labrum and femoral head. It is believed that aiming for the clear space puts the labrum at risk of penetration. The steps to fluoroscopy-guided portal placement are discussed, along with the rationale behind this technique. It is recommended that the initial spinal needle be placed under fluoroscopic guidance in a position overlapping the superior femoral head. By doing this, labral penetration can be minimized. Femoral head injury can be minimized through proper anterior-to-posterior placement by establishing initial needle contact with the capsule just lateral to the femoral head.
Technique
The hip is first distracted by use of an appropriate traction table. With adequate distraction, the hip will create a vacuum sign. The foot is internally rotated to compensate for anatomic anteversion of the femoral neck. Dedicated hip arthroscopy instruments (Smith & Nephew, Andover, MA) are used to demonstrate this technique; however, this technique can be accomplished with any cannulated system. Required arthroscopic instruments include a cannulated needle, guidewire, trocar, and 70° arthroscope.
The spinal needle is placed over the anterior thigh to establish the insertion angle for the needle (Fig 3A). Fluoroscopy is used to confirm a position overlapping the superior dome of the femoral head (Fig 3B). Once this angle is established, a marking pen is used to maintain this angle as a guide. The cannulated needle is then placed just anterior to the greater trochanter, in line with the skin marking. The needle is initially angled posterior approximately 10° to 15°, and the needle is advanced through the skin and down to the capsule. Once the capsule has been reached, a fluoroscopic spot is obtained to determine placement of the needle. The needle should reproduce the same angle aimed at a position to overlap the superior dome of the femoral head. The needle is advanced to the hip capsule, as signified by an increase in resistance. Before capsular penetration, the needle should be located in a position just lateral to the femoral head on the fluoroscopic image. This position helps establish initial anteroposterior placement. The needle tip should also be positioned away from the femoral head to minimize scuffing (Fig 3C). It is then advanced through the capsule with tactile feedback used to feel a give in resistance while penetrating capsule. Once resistance is diminished, one should be careful not to advance the needle any further, because this increases the risk of femoral head scuffing and anterior labrum penetration. On fluoroscopy, the air arthrogram will further improve distraction once the vacuum seal is broken. The spinal needle can be repositioned at this time if needed.
Figure 3.
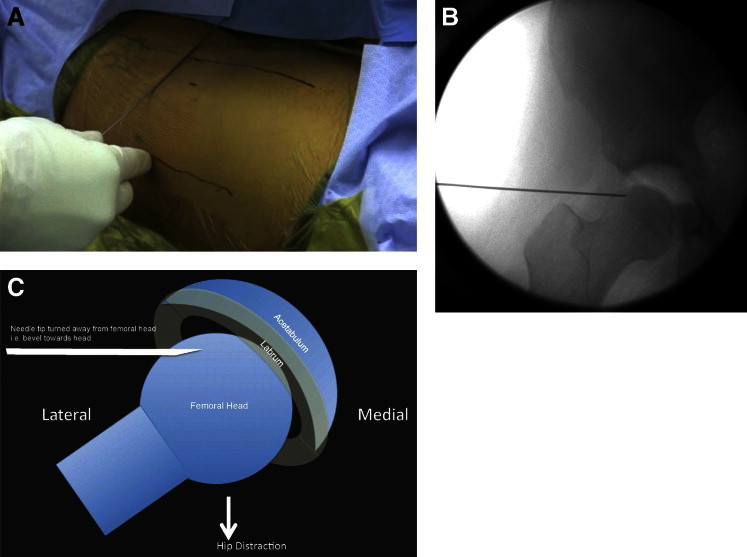
Technique for establishing the anterolateral portal, shown in a right hip in the supine position. (A) Before insertion, a spinal needle is positioned by fluoroscopy with the desired trajectory marked. (B) The spinal needle is inserted and directed anterior to the femoral head to penetrate the hip capsule. (C) The bevel of the spinal needle is directed away from the cartilaginous surface of the femoral head to prevent scuffing.
The guidewire is then inserted into the joint until it makes contact with the medial wall of the acetabulum. This ensures that the placement of the portal is intra-articular. If the guidewire does not enter the hip in a straight pathway, this signifies a portal angle that is aimed too posteriorly, that is, the guidewire trajectory changes as it comes into contact with the superior femoral head (Fig 4A). The guidewire should be repositioned slightly anteriorly until a straight trajectory is obtained to minimize femoral head scuffing (Fig 4B). The trocar is then advanced by use of a twisting motion through the capsule until resistance decreases. Again, it is important not to overly advance the trocar to minimize a femoral-sided injury (Fig 4C).
Figure 4.
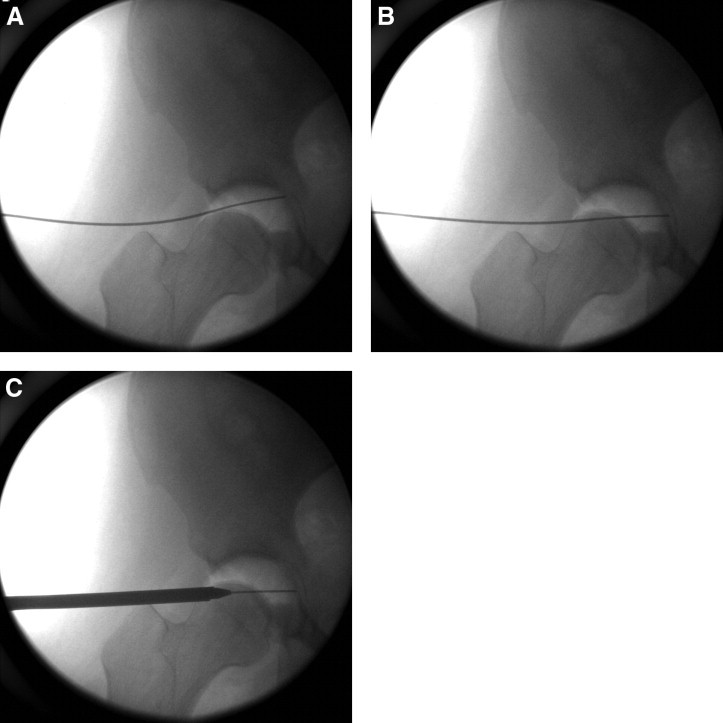
Confirmation of introductory portal positioning, shown in a right hip in the supine position. (A) Deflection of the guidewire indicates malpositioning of the portal that can endanger the femoral head. (B) Anteroposterior adjustment is necessary, should this occur, until the wire passes smoothly without deflection along its trajectory through the capsule to the acetabulum. (C) After proper guidewire placement, the Seldinger technique is used to advance the trocar into the hip joint.
The 70° arthroscope is then inserted into the hip. It is important to establish visualization of the capsular triangle seen between the labrum and femoral head (Fig 5). Confirmation of this view ensures proper placement of the anterolateral portal. To visualize the central compartment, the placement of the arthroscope does not need to be advanced between the acetabulum and femoral head. Of note, if the initial visualization of the joint is more central and the labrum is blocking visualization of the capsular triangle, this may represent penetration of the labrum and the portal should be redirected. However, in our series labral penetration has not occurred since moving the portal placement toward the femoral head instead of the clear space. In our experience this technique is particularly useful in the over-covered, pincer-type hip.
Figure 5.
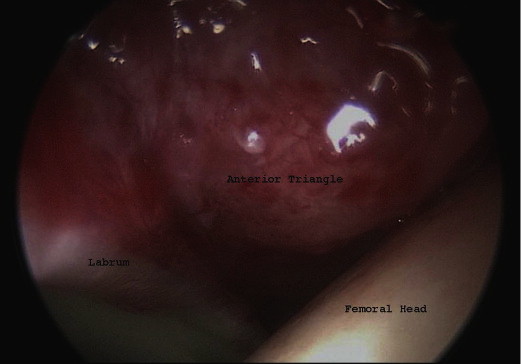
View from the introductory anterolateral portal in a right hip in the supine position. The anterior triangle of the capsule is clearly visualized for secondary portal placement, along with the femoral head, labrum, and acetabular cartilage.
Once portals have been established, a greater understanding of anterolateral spinal needle placement can be gained by placing the arthroscope into the anterior portal. The spinal needle can then be placed into the anterolateral portal, and its position can be compared with fluoroscopic images. In Figure 6 the spinal needle is positioned between the labrum and femoral head in a safe position (Fig 6A) versus placement into a position just before labral penetration (Fig 6C). Corresponding fluoroscopic views are shown in Fig 6B and 6D, respectively. Table 1 summarizes the technique.
Figure 6.
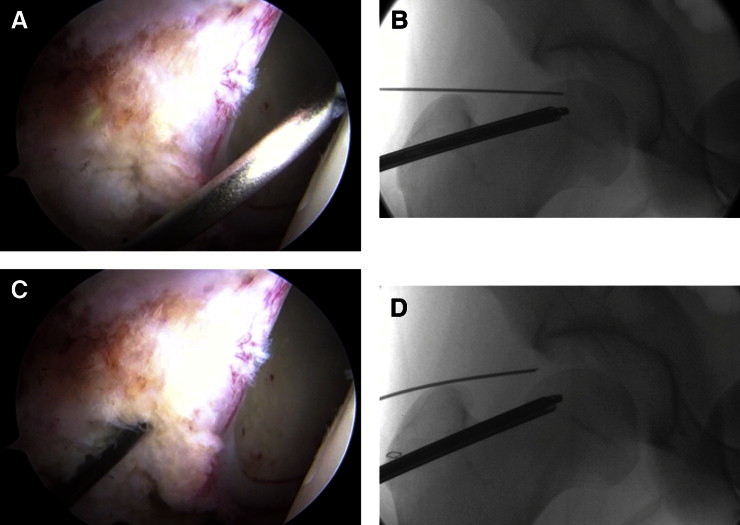
Anterolateral spinal needle position visualized from the anterior portal with corresponding fluoroscopic images in a right hip in the supine position. (A) The spinal needle is aimed between the labrum and femoral head in a safe position. (B) Corresponding fluoroscopic image of needle position. (C) The spinal needle is aimed at the labrum just before penetration. (D) Corresponding fluoroscopic image of needle position.
Table 1.
Anterolateral Portal Placement Pearls
| Description | |
|---|---|
| Equipment needed | Distraction table, fluoroscopy device, cannulated needle, guidewire, cannulated trocar system, 70° arthroscope |
| Setup | Use adequate distraction to create a vacuum sign. Internally rotate the foot to compensate for femoral neck anteversion. |
| Anterolateral portal needle placement | The trajectory of the spinal needle should overlap the superior femoral head. The needle should come into initial contact with the capsule in a position lateral to the femoral head. The needle bevel should be turned to avoid scuffing of the femoral head. Tactile feedback is used to insert the needle through the capsule (do not overly advance to avoid intra-articular injury). An air arthrogram will confirm an intra-articular position. |
| Guidewire placement | The guidewire should be advanced until it contacts the medial wall of the acetabulum. Ideally, the guidewire trajectory should be straight. If the guidewire trajectory curves superiorly (bouncing off the femoral head), then redirect the position slightly more anterior to improve the position and minimize articular injury. |
| Trocar placement | The trocar is advanced through the capsule using tactile feedback; do not overly advance the trocar to avoid iatrogenic injury. |
| 70° Arthroscope view | If correctly placed, the anterior capsular triangle, labrum, acetabulum, and femoral head should be easily visualized. If the anterior triangle is difficult to view, the portal may be aimed too posteriorly and labral penetration may have occurred. Redirect the initial needle further down on the femoral head side to improve positioning. |
Discussion
In the literature there are many proposed technical pearls described to minimize iatrogenic injury during hip arthroscopy. Labral penetration and femoral head articular injury are complications seen with initial anterolateral portal placement. With fluoroscopy-guided placement of cannulated needles during anterolateral portal positioning, the needles are often aimed toward the clear space of the distracted hip joint. However, aiming toward the clear space increases the potential of labral penetration. Placing the needle anterior at the level of the superior femoral head will reduce injury to the labrum. Although aiming toward the femoral head may be worrisome with regard to a femoral-sided injury, we have found this not to be the case. Avoiding over-insertion of the cannulated needle and trocar, as well as paying close attention to the trajectory of the guidewire, will minimize articular scuffing of the femoral head.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary data
Technique for anterolateral portal placement in a right hip in the supine position.
References
- 1.Burman M. Arthroscopy or the direct visualization of joints: An experimental cadaver study. J Bone Joint Surg Am. 1931;13:669–695. doi: 10.1097/00003086-200109000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Horisberger M., Brunner A., Herzog R.F. Arthroscopic treatment of femoroacetabular impingement of the hip: A new technique to access the joint. Clin Orthop Relat Res. 2010;468:182–190. doi: 10.1007/s11999-009-1005-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simpson J., Sadri H., Villar R. Hip arthroscopy technique and complications. Orthop Traumatol Surg Res. 2010;96:S68–S76. doi: 10.1016/j.otsr.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 4.Dienst M., Seil R., Kohn D.M. Safe arthroscopic access to the central compartment of the hip. Arthroscopy. 2005;21:1510–1514. doi: 10.1016/j.arthro.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 5.Byrd J.W. Avoiding the labrum in hip arthroscopy. Arthroscopy. 2000;16:770–773. doi: 10.1053/jars.2000.7686. [DOI] [PubMed] [Google Scholar]
- 6.Badylak J.S., Keene J.S. Do iatrogenic punctures of the labrum affect the clinical results of hip arthroscopy? Arthroscopy. 2011;27:761–767. doi: 10.1016/j.arthro.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 7.Boyle J.R., Silva J.A., McMillan S., Busconi B.D. Mechanics of hip arthroscopy. Clin Sports Med. 2011;30:285–292. doi: 10.1016/j.csm.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Bond J.L., Knutson Z.A., Ebert A., Guanche C.A. The 23-point arthroscopic examination of the hip: Basic setup, portal placement, and surgical technique. Arthroscopy. 2009;25:416–429. doi: 10.1016/j.arthro.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 9.Domb B., Hanypsiak B., Botser I. Labral penetration rate in a consecutive series of 300 hip arthroscopies. Am J Sports Med. 2012;40:864–869. doi: 10.1177/0363546512437152. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique for anterolateral portal placement in a right hip in the supine position.


