Abstract
Although the exact biomechanical function of the ligamentum teres (LT) remains unclear, an important role in hip stability has been suggested. In some patients, perhaps because of their specific anatomy or physical activity, it seems to have a major function as a hip stabilizer. Therefore, after a complete LT tear, this group of patients may have persistent hip pain and mechanical symptoms probably related to microinstability and subtle subluxation. We present the case of a female patient with a complete LT tear. This had been treated by debridement and anterior capsule tightening, followed by prolonged rehabilitation. However, she had persistent symptoms. An LT reconstruction with a novel surgical technique was performed. The LT was reconstructed with double-stranded semitendinosus graft. The acetabular end was fixed with 2 anchors, and the femoral end was passed into a bone tunnel and fixed with an interference screw. After surgery, the patient's modified Harris Hip Score and Non-Arthritic Hip Score improved from 53 and 73 to 100 and 95, respectively, at 12 months of follow-up. At repeat arthroscopy 15 months after surgery, it was observed that the graft had resorbed, although the 2 Ticron stitches (Covidien, Mansfield, MA) remained firmly attached and were still acting as a small synthetic ligament.
Ligamentum teres (LT) tears have been recognized as a source of hip pain,1-5 and Gray and Villar2 classified these tears as complete (type 1), partial (type 2), and degenerative (type 3). One of the possible injury mechanisms of LT tears is a major traumatic event, with or without concomitant hip dislocation. In these cases the LT tear is often accompanied by other intra-articular injuries and is commonly complete. Alternatively, the tears can be caused by a subtle injury, repetitive stress, stretching, and microinstability, which are more likely to cause a partial LT tear.1,3,5,6 Radiofrequency ablation treatment has shown excellent results in both complete and partial tears.3,5
Although the exact biomechanical function of the LT remains unclear, one study has suggested that the LT is an important component in hip stability.1 The tensile strength of the LT in a porcine model is similar to the anterior cruciate ligament (ACL).7 Moreover, Martin et al.8 reported that the LT may contribute to hip stability when the hip is in flexion/external rotation and extension/internal rotation. The movements that bring the hip into those positions are squatting and attempting to cross one leg behind the other when standing, respectively. In addition, Martin et al. noted that of 9 patients with a complete LT tear, 5 had instability complaints when they were asked to squat. However, despite the increasing number of scientific articles, the precise role of the LT is not fully clear.
In some patients, perhaps because of their specific anatomy or physical activity, the LT seems to have an important function as a hip stabilizer. Therefore, after a complete LT tear, this group of patients may have persistent hip pain and mechanical symptoms probably related to microinstability and subtle subluxation. Simpson et al.9 have reported a successful LT reconstruction in a young patient who had pain and mechanical symptoms after a complete LT tear.
We present the case of a female patient who presented initially with a complete LT tear. This had been treated by debridement and anterior capsule tightening, followed by prolonged rehabilitation. However, she had persistent symptoms. An LT reconstruction with a novel surgical technique was performed. We will describe the surgical technique, clinical outcome, and findings at follow-up arthroscopy.
Surgical Technique
Before the arthroscopy was commenced, the semitendinosus tendon was harvested from the ipsilateral leg, as is performed for ACL reconstruction,10 and prepared as a double-stranded 7-mm graft. Two No. 5 Ticron nonabsorbable sutures (Covidien, Mansfield, MA) were passed along the graft and long tails left from each end to use later to place the graft.
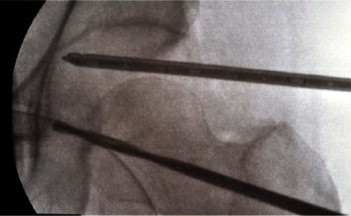
The patient was positioned in the lateral decubitus position and traction applied, with the McCarthy lateral hip distractor (Innomed, Savannah, GA), as described previously (Fig 1).11 A general anesthetic was given without additional muscle relaxation. The countertraction post was raised an additional 4 cm to ensure greater lateral traction on the hip and increase the lateral displacement of the femoral head. Two arthroscopic portals were created. The first, the midtrochanteric portal, was created with image intensifier guidance, and the second, the anterior paratrochanteric portal, was created under direct arthroscopic vision. The midtrochanteric portal was the viewing portal, and the anterior paratrochanteric portal was the instrument portal.
Figure 1.

Lateral decubitus position for hip arthroscopy with McCarthy lateral hip distractor.
The area of attachment for the graft in the acetabular fossa was cleared of soft tissue and a bleeding bone bed created with a standard radiofrequency probe (Arthro Wand; ArthroCare, Sunnyvale, CA), a flexible radiofrequency probe (Eflex; Smith & Nephew, Andover, MA), and a bendable shaver (Great White 15° bendable to 30°; ConMed Linvatec, Largo, FL). This area was on the posterior and outer edge of the fossa adjacent to the transverse acetabular ligament. In the hip with an intact LT, this area is normally very difficult to access, but in the LT-deficient hip, this area is easier to reach because of the increased laxity in the hip. An 8.25-mm cannula was then inserted in the anterior paratrochanteric portal. Two anchors (2.3-mm Bioraptor; Smith & Nephew) were inserted through the cannula into the outer, posterior part of the fossa (Fig 2).
Figure 2.

Anchors inserted in previously prepared acetabular fossa (left side with patient in lateral decubitus position, viewed from midtrochanteric portal).
Through a separate incision, a guide drill was passed through the greater trochanter and along the femoral neck to exit on the fovea. This was performed with image intensifier control but could readily be performed with a modified ACL guide (Fig 3).9 A 9-mm cannulated trephine was used to take a bone plug from the proximal femur, and a 9-mm drill was then used to complete the bone tunnel. One strand of each anchor stitch was passed through the looped end of the prepared, doubled graft, and the graft was then passed down the cannula and securely tied into position against the prepared bone bed (Fig 4). A Beath pin with a long loop stitch attached to its eye was passed retrograde through the femoral tunnel and the suture was captured and then withdrawn out the cannula. The Ticron stitch attached to the femoral end of the graft was passed through the loop and then drawn back through the femoral tunnel. Traction on this stitch took the femoral end of the graft down the cannula and into the proximal end of the femoral tunnel.
Figure 3.
Femoral tunnel drilled.
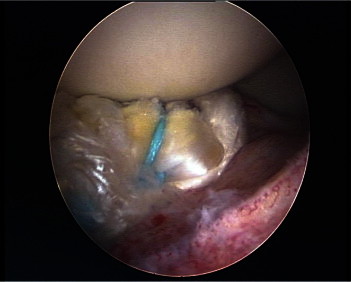
Figure 4.

Semitendinosus double-stranded graft with 1 strand of each anchor stitch passed through looped end.
The arthroscope was left in the joint to check that the graft was in situ (Fig 5) and the traction partially released. The leg was rotated externally 20°, and the graft was pulled tight and then fixed with a 9-mm interference screw (RCI Fixation Screw; Smith & Nephew). Additional fixation was obtained by tying the Ticron stitch outside the femur. The bone plug was reinserted to seal the bone tunnel. Long-acting local anesthetic was injected into the joint, and the 3 incisions were sutured.
Figure 5.
Graft in situ before tensioning (left side with patient in lateral decubitus position, viewed from midtrochanteric portal).
After surgery, the patient undertook our standard post–hip arthroscopy rehabilitation program12 but did not externally rotate the leg beyond 30° for 4 weeks.
Recently, we have improve this surgical technique. We have found that it is possible to obtain better debridement of the acetabular fossa by adding a posterior paratrochanteric portal and also by working directly through the femoral tunnel. Furthermore, we have been able to achieve a better position, fixation, and tension of the graft by inserting the anchors and fixing the graft directly through the femoral tunnel (Fig 6). The complete current technique is demonstrated in Video 1.
Figure 6.
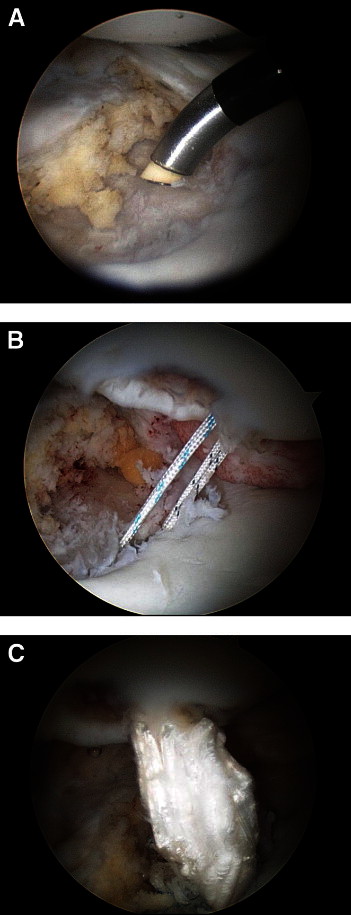
Modifications of original technique to improve debridement of acetabular fossa and to achieve better graft fixation (right side with patient in lateral decubitus position, viewed from midtrochanteric portal). (A) Debridement of posterior zone of acetabular fossa through posterior paratrochanteric portal. (B) Anchors inserted in posterior zone of acetabular fossa through femoral tunnel. (C) Final appearance of the semitendinosus graft after use of aforementioned modifications to original surgical technique.
Clinical Outcome and Follow-Up
After surgery, at 12 months' follow-up, the patient's modified Harris Hip Score and Non-Arthritic Hip Score improved from 53 and 73 to 100 and 95, respectively, and she also returned to running. However, 15 months after surgery, new lateral hip pain developed. The hip joint remained painless and stable. Ultrasound examination showed a small fluid collection associated with the Ticron knot at the point of maximal tenderness. The knot was removed arthroscopically, and the hip was also evaluated. The graft had resorbed, although the 2 Ticron stitches remained firmly attached and were still acting as a small synthetic ligament (Fig 7).
Figure 7.
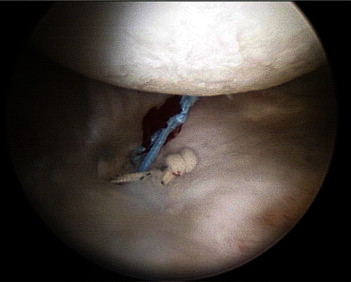
Graft resorption and intact sutures and anchors at second-look arthroscopy (left side with patient in lateral decubitus position, viewed from midtrochanteric portal).
Discussion
Traditionally, the hip has been recognized as a very stable joint because of its osseous anatomy. Previously, the function and anatomy of the ligaments and labrum of the hip have been studied and described. The research in these areas has led to an increased awareness of hip instability, although there is controversy regarding definition, diagnosis, and treatment.13,14
Hip instability has been defined as traumatic or atraumatic. Traumatic instability comprises a broad spectrum ranging from major injuries to microtrauma caused by repetitive motions. On the other hand, atraumatic instability is commonly associated with anatomic abnormalities such as developmental dysplasia of the hip and connective tissue disorders or may be iatrogenic. In addition, idiopathic instability, defined as instability that occurs in the absence of trauma, bony dysplasia, overuse, or connective tissue disorders, is also possible.13
The initial assessment of a patient with suspected hip instability should include a thorough medical history, directed physical examination, and imaging studies, to elucidate the type of instability present. The initial treatment of atraumatic and idiopathic hip instability, once diagnosed, usually consists of rest, activity modification, and physical therapy. Surgical treatment should be considered when conservative treatment has failed. Usually, the hip laxity and labral pathology can be treated by labral repair or debridement and capsular tightening.13,15
Little has been written about the role of the LT in hip instability.1,9,16 Taking into account the work of Martin et al.,8 we believe that the LT has a role, not yet completely understood, as a hip stabilizer and it should be included in the evaluation of hip instability. In those patients with a ruptured LT and persisting mechanical symptoms of instability, consideration should be given to reconstructing the ligament, even though this remains a developing and experimental technique.
Our patient initially was treated by complete debridement of the LT and capsular tightening for hip pain and a complete LT tear. After her first surgery, she had persisting mechanical symptoms of hip instability, despite a prolonged rehabilitation process. She was thoroughly evaluated, and no other correctable cause of hip instability was identified other than the absence of the LT. Hence, after discussion with the patient, the decision to perform an LT reconstruction was made.
Our hypothesis is that the patients who might benefit from an LT reconstruction are those with some degree of anterior capsular laxity, possibly as a result of microtrauma caused by repetitive motions or hip kinematics. In these patients the LT seems to play an important role restraining hip movement and compensating for the impaired function of the anterior capsule as a stabilizer. As a result of increased load, the LT tears, partially at the beginning, causing pain, but over time evolving to a complete tear. This leads to loss of the stabilizing function of the LT and results in the onset of hip instability symptoms. A similar stabilizing role of the LT has been proposed in dysplastic hips.16
The technique used was developed by adapting ligament reconstruction procedures that have been extensively studied and applied in other joints previously. The fixation method chosen on the acetabular side was the use of anchors instead of an endopelvic fixation device. We believe that this diminishes the risk of serious vascular or neurologic injuries and makes the technique more accessible for hip arthroscopy surgeons. Moreover, the anchor seems to be a solid method of fixation, with a mean load to failure in cortical bone of 172.2 N for the 2.3-mm Bioraptor anchor used.17 The graft chosen was semitendinosus autograft because it has been widely used in ACL reconstruction and the load to failure for a single brand of semitendinosus graft is 1,216 N.18 We did not choose patellar bone–tendon–bone graft to avoid the donor-site morbidity, as well as because the structure of the patellar bone–tendon–bone graft was not suitable for the type of fixation we were looking for.19,20 Other graft options are available and include allograft or new synthetic graft. These options were discarded, the first because of concerns about disease transmission and the weakening of the tissue related to the sterilization process.20 Some good early results have been reported with new synthetic grafts (Ligament Augmentation and Reconstruction System [LARS], Arcsur-Tille, France), but we believe that long-term results are needed to prove their security and suitability.21 We have concerns regarding their use in the hip, where the movement patterns are quite different from the knee and may make it more likely that the synthetic ligaments will fray and fail. We also have concerns about inflammatory synovitis, which could accompany any such fraying.22
The resorption of the graft in our patient was an unexpected outcome. During the follow-up arthroscopy, there were no signs of inflammation or synovitis in the hip joint. One of the possible explanations could be impingement of the graft, as has been described previously for ACL grafts; in these cases the impingement, over time, leads to localized chronic synovitis and failure.23 Although isolated cases of idiopathic ACL graft resorption have been described, we could find no reference for this outcome of ACL reconstruction. We cannot, with certainty, explain this occurrence of graft resorption. It is possible that it is a 1-off event, or it may be a problem associated with the technique.
In addition, the findings of persistence of the anchors and 2 nonabsorbable sutures acting as a small synthetic ligament were unexpected, and the continuing stabilizing effect on the joint, as well as absent instability symptoms, seemed to us an encouraging result.
The increasing interest in LT biomechanics and hip instability has led to the development of LT reconstruction techniques. However, these techniques are still evolving, and we do not know yet which method will prove to be the best in terms of a durable, long-term result. As has been learned with the ACL, ligament reconstructions are complex techniques in which many variables, mostly related to the surgical technique, are important to obtain the optimum results. Furthermore, the indications for this type of procedure are not yet clearly defined.
On the basis of our short-term results and those previously published by Simpson et al.,9 we believe that LT reconstruction will be a useful procedure in selected patients. Our current indications for LT reconstruction are those patients with hip instability symptoms and a complete LT tear who have not responded to physiotherapy and arthroscopic anterior capsular plication (Tables 1 and 2).
Table 1.
Suggested Indications for LT Reconstruction
| Patient with a complete or nearly complete (insufficient) LT tear; either traumatic or atraumatic rupture in origin |
| Diagnosis of hip instability after a thorough medical history and physical examination; any other correctable cause of hip instability should be ruled out |
| Failure of previous physical therapy or activity modification |
| Failure of previous surgical treatment (i.e., partial LT debridement and capsular tightening) |
Table 2.
Surgical Tips for Arthroscopic LT Reconstruction
| Harvest a graft of adequate length. |
| Perform lateralization of the countertraction post to increase lateral displacement of the femoral head and allow better visualization of the acetabular fossa. |
| Remove all the soft tissue from the area of attachment of the graft in the acetabular fossa. Use a flexible radiofrequency probe and bendable shavers. Add a posterior paratrochanteric portal or debride the fossa through the femoral tunnel if necessary. |
| Achieve a correct exit of the drill guide through the femoral fovea, guided by image intensifier and direct visualization. |
| Perform placement of the anchors emulating the anatomic origin (i.e., posteroinferior aspect of the acetabular fossa); to achieve this, insert the anchors through the femoral tunnel. |
| Fix the graft to the femoral end after tightening it, with the leg in 20° of external rotation. |
Finally, the ideal surgical technique regarding technical issues, such as graft selection and its tension, fixation method and its position, and rehabilitation protocols and length, still needs to be defined.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary data
References
- 1.Bardakos N.V., Villar R.N. The ligamentum teres of the adult hip. J Bone Joint Surg Br. 2009;91:8–15. doi: 10.1302/0301-620X.91B1.21421. [DOI] [PubMed] [Google Scholar]
- 2.Gray A.J., Villar R.N. The ligamentum teres of the hip: An arthroscopic classification of its pathology. Arthroscopy. 1997;1:1–4. doi: 10.1016/s0749-8063(97)90182-1. [DOI] [PubMed] [Google Scholar]
- 3.Haviv B., O'Donnell J. Arthroscopic debridement of the isolated ligamentum teres rupture. Knee Surg Sports Traumatol Arthrosc. 2011;19:1510–1513. doi: 10.1007/s00167-010-1318-7. [DOI] [PubMed] [Google Scholar]
- 4.Rao J., Zhou Y.X., Villar R.N. Injury to the ligamentum teres: Mechanism, findings, and results of treatment. Clin Sports Med. 2001;20:791–799. doi: 10.1016/s0278-5919(05)70285-4. [DOI] [PubMed] [Google Scholar]
- 5.Byrd J.W.T., Jones K.S. Traumatic rupture of the ligamentum teres as a source of hip pain. Arthroscopy. 2004;20:385–391. doi: 10.1016/j.arthro.2004.01.025. [DOI] [PubMed] [Google Scholar]
- 6.Botser I.B., Martin D.E., Stout C.E., Domb B.G. Tears of the ligamentum teres: Prevalence in hip arthroscopy using 2 classification systems. Am J Sports Med. 2011;39(suppl):117S–125S. doi: 10.1177/0363546511413865. [DOI] [PubMed] [Google Scholar]
- 7.Wenger D., Miyanji F., Mahar A., Oka R. The mechanical properties of the ligamentum teres: A pilot study to assess its potential for improving stability in children's hip surgery. J Pediatr Orthop. 2007;27:408–410. doi: 10.1097/01.bpb.0000271332.66019.15. [DOI] [PubMed] [Google Scholar]
- 8.Martin R.L., Palmer I., Martin H.D. Ligamentum teres: A functional description and potential clinical relevance. Knee Surg Sports Traumatol Arthrosc. 2012;20:1209–1214. doi: 10.1007/s00167-011-1663-1. [DOI] [PubMed] [Google Scholar]
- 9.Simpson J.M., Field R.E., Villar R.N. Arthroscopic reconstruction of the ligamentum teres. Arthroscopy. 2011;27:436–441. doi: 10.1016/j.arthro.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 10.Lawhorn K.W., Howell S.M. Principles for using hamstring tendons for anterior cruciate ligament reconstruction. Clin Sports Med. 2007;26:567–585. doi: 10.1016/j.csm.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 11.Mason J.B., McCarthy J.C., O'Donnell J. Hip arthroscopy: Surgical approach, positioning, and distraction. Clin Orthop Relat Res. 2003;406:29–37. doi: 10.1097/01.blo.0000043041.84315.cc. [DOI] [PubMed] [Google Scholar]
- 12.Haviv B., O'Donnell J. Arthroscopic treatment for acetabular labral tears of the hip without bony dysmorphism. Am J Sports Med. 2011;39(Suppl):79S–84S. doi: 10.1177/0363546511412915. [DOI] [PubMed] [Google Scholar]
- 13.Boykin R.E., Anz A.W., Bushnell B.D., Kocher M.S., Stubbs A.J., Philippon M.J. Hip instability. J Am Acad Orthop Surg. 2011;19:340–349. doi: 10.5435/00124635-201106000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Shu B., Safran M.R. Hip instability: Anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med. 2011;30:349–367. doi: 10.1016/j.csm.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 15.Philippon M.J. The role of arthroscopic thermal capsulorrhaphy in the hip. Clin Sports Med. 2001;20:817–829. doi: 10.1016/s0278-5919(05)70287-8. [DOI] [PubMed] [Google Scholar]
- 16.Mei-Dan O., McConkey M.O., Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic instability: Can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy. 2012;28:440–445. doi: 10.1016/j.arthro.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 17.Barber F.A., Herbert M.A., Beavis R.C., Barrera Oro F. Suture anchor materials, eyelets, and designs: Update 2008. Arthroscopy. 2008;24:859–867. doi: 10.1016/j.arthro.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 18.Shelton W.R., Fagan B.C. Autografts commonly used in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2011;19:259–264. doi: 10.5435/00124635-201105000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Gulotta L.V., Rodeo S.A. Biology of autograft and allograft healing in anterior cruciate ligament reconstruction. Clin Sports Med. 2007;26:509–524. doi: 10.1016/j.csm.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 20.Reinhardt K.R., Hetsroni I., Marx R.G. Graft selection for anterior cruciate ligament reconstruction: A level I systematic review comparing failure rates and functional outcomes. Orthop Clin North Am. 2010;41:249–262. doi: 10.1016/j.ocl.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 21.Legnani C., Ventura A., Terzaghi C., Borgo E., Albisetti W. Anterior cruciate ligament reconstruction with synthetic grafts: A review of literature. Int Orthop. 2010;34:465–471. doi: 10.1007/s00264-010-0963-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Glezos C.M., Waller A., Bourke H.E., Salmon L.J., Pinczewski L.A. Disabling synovitis associated with LARS artificial ligament use in anterior cruciate ligament reconstruction: A case report. Am J Sports Med. 2012;40:1167–1171. doi: 10.1177/0363546512438510. [DOI] [PubMed] [Google Scholar]
- 23.George M.S., Dunn W.R., Spindler K.P. Current concepts review: Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34:2026–2037. doi: 10.1177/0363546506295026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


