Abstract
This study examines the cross-lagged relationships between posttraumatic distress symptoms and physical functioning, using a sample of 413 persons who were hospitalized for injuries resulting from community violence. Posttraumatic distress was assessed at one week, 3-months and 12-months post injury, and posttraumatic physical functioning was assessed at 3-months and 12-months. Structural equation modeling was used to assess the prospective relationship between posttraumatic distress symptoms and physical functioning while controlling for demographic characteristics and objective measures of injury severity. Results indicate that posttraumatic distress and physical functioning are reciprocally related. Individuals with high levels of psychological distress at one week post trauma have worse physical functioning at 3-months. Psychological distress at 3-months was not significantly associated with subsequent change in physical functioning at 12-months. Individuals with poor physical functioning at 3-months had higher than expected levels of psychological distress at 12-months. These findings demonstrate a reciprocal relationship between physical and mental health following traumatic injury. Interventions targeting physical recovery may influence subsequent mental health and therapies aimed at improving early mental health may also have long term benefits for physical recovery.
Keywords: Posttraumatic distress, physical functioning, trauma, structural equation modeling
In 2005, over 5 million non-fatal violent attacks occurred in the United States (Catalano, 2006). Survivors of these attacks are vulnerable to a range of poor health outcomes, including injuries that may impair physical functioning as well as adverse psychological reactions. Injured assault survivors are particularly at risk for experiencing symptoms of posttraumatic stress disorder (PTSD). PTSD is disabling, and often chronic, condition characterized by three clusters of symptoms (i.e., re-experiencing, avoidance, and hyperarousal) that persist for at least one month after trauma exposure (American Psychiatric Association [APA], 1994). Although violence-related physical injuries may independently cause both physical impairment and emotional distress, it is also possible that physical and emotional health may influence one another.
Prior research has converged in indicating that lower levels of physical functioning are associated with greater posttraumatic distress. Primary care patients with untreated PTSD, for example, have been found more likely to report lower levels of physical functioning than their counterparts without PTSD (Schofeld et al., 1997). Moreover, investigations of individuals who experience sudden physical injuries have revealed that symptoms of posttraumatic distress are associated with reduced physical functioning (Holbrook et al., 2001; Zatzick, Jurkovich, Gentilello, Wisner, & Rivara, 2002; Michaels et al., 1999; Wong et al., 2007). Similar findings have also been reported in studies of veterans (Magruder et al., 2004; Zatzick et al., 1997). Finally, among patients treated for life-threatening illnesses, i.e., breast cancer survivors undergoing bone marrow transplantation (Jacobsen et al., 1998) or long-term survivors of acute respiratory distress syndrome (Kampfhammer, Rothenhausler, Krauseneck, Stoll, & Schellig, 2004), those who report increased symptoms of post-intervention posttraumatic distress reported lower levels of physical functioning.
Research has also examined the relationship between PTSD symptoms and physical health with a range of physical health measures. In particular, impaired physical health has been variously conceptualized as symptoms of poor health (Zatzick et al., 1997; Beckham et al., 1998), the existence of medical conditions (e.g., Beckham et al., 1998; Breslau & Davis, 1992; Seng, Clark, McCarthy, & Ronis, 2006) and the presence of key potentially health-compromising behaviors such as tobacco use (e.g., Beckham et al., 1998; Lauterbach, Vora, & Rakow, 2005). Although all of these constructs are useful ways in which to conceive of poor health, measures of physical functioning do possess some advantages over other strategies for measuring health outcomes. In particular, self-report measures of physical functioning typically reflect the degree to which performance of common physical functions and social roles is compromised and may more closely reflect the actual burden of poor physical health. A variety of well-validated scales have been used to measure physical functioning in relation to PTSD, e.g., the Short Form 36 (SF-36; Michaels et al., 1999; Schonfeld et al., 1997), the Quality of Well-being scale (Holbrook, Hoyt, Stein, & Seiber, 2001), the WHOQoL-Bref (O’Donnell, Creamer, Elliott, Atkin, & Kossmann, 2005), and the Quality of Life Inventory (Schnurr, Hayes, Lunney, McFall, & Uddo, 2006).
Although the foregoing research suggests that posttraumatic distress and poor physical health are related, the existing studies documenting this relationship have not been able to determine whether PTSD symptoms precede the development of poor physical functioning or vise versa. Until the field has a better understanding of the temporal course of these constructs, it is difficult to know if PTSD causes physical health problems, if physical health problems exacerbate PTSD, or if these problems form a vicious cycle. First, the majority of available studies have employed cross-sectional designs. These designs provide an inherently inadequate basis for drawing causal inferences regarding the relations between constructs. Moreover, although some longitudinal investigations have examined the link between physical functioning and posttraumatic distress (e.g., Holbrook et al., 2001; Michaels et al., 1999; Zatzick et al., 2002; O’Donnell et al., 2005; Schnurr et al., 2006; Blanchard et al., 1997) these studies have not been able to determine if PTSD precedes the development of physical health problems or visa versa. In perhaps the most rigorous of these investigations, Schnurr et al. (2006) used latent growth modeling to assess the association between changes in symptoms of posttraumatic distress on changes in physical functioning. Examining data collected at three time points from 325 military veterans receiving psychotherapy for PTSD, these researchers found evidence that individuals who had increasing psychological distress over a time period tended to have decreasing physical functioning over the same interval (Schnurr et al., 2006).1 This evidence of correlated changes supports the view that PTSD and physical functioning are causally linked, although this data did not allow the authors to choose among the three possible causal theories.
The absence of systematic research examining these potential reciprocal relations between physical impairment and trauma-related distress leaves critical questions unanswered. For example, little is known about whether treatment of posttraumatic distress following trauma exposure can improve subsequent physical health outcomes. Similarly, a dearth of knowledge exists regarding the possibility that interventions aimed at improving physical health might also reduce posttraumatic distress. These issues are particularly important in the context of persons who experience sudden physical injuries that render them at high risk for significant posttraumatic distress.
Theoretical accounts of the relationship between physical functioning and posttraumatic distress have posited that posttraumatic distress may contribute to poor physical health (Friedman & Schnurr, 1995; Kimmerling, Clum, & Wolfe, 2000; Lauterbach et al., 2005; Schnurr et al., 2006; Schnurr & Jankowski, 1999). Various mechanisms have been proposed to explain this relationship. There is some evidence, for example, that persons with elevated levels of posttraumatic distress may experience neurobiological or immunologic alterations that influence physical functioning (Friedman & McEwan, 2004; Dougall & Baum, 2004). Noting the frequent comorbidity of depression and PTSD, some have suggested that the depressive symptoms of trauma-exposed individuals may influence health outcomes either directly or via health behaviors (Ford, 2004; Schnurr & Jankowski, 1999), though studies have shown an independent effect of PTSD on health outcomes when accounting for depressive symptoms (Boscarino & Chang, 1999; Kubzansky, Koenen, Spiro, Vokonas, & Sparrow, 2007). Psychological distress may influence a trauma survivor’s decision to seek medical care either directly (Walker, Newman, & Koss, 2004) or indirectly via either poor familial and social functioning (Stein, Walker, Hazen, & Forde, 1997) or unemployment (Smith, Schnurr, & Rosenheck, 2005; Savoka & Rosensheck, 2000). Trauma-exposed persons with elevated levels of distress may also engage in health-risk behaviors such as substance use and abuse which, over time, can contribute to adverse health outcomes (Rheingold, Acierno, & Resnick, 2004). Schnurr and Green (2004) and Schnurr and Jankowski (1999) have proposed an integrative model in which these proposed mechanisms collectively lead to poor health.
Most previous studies on posttraumatic distress and health are based on persons with chronic posttraumatic distress and, for the most part, the proposed mechanisms attempt to explain how posttraumatic distress might adversely influence physical health outcomes over lengthy periods of time. Few studies have examined whether posttraumatic distress might impact physical health and physical recovery in the near-term aftermath of trauma exposure. On the one hand, psychological distress may impact physical recovery from a trauma in many of the same ways identified above. On the other hand, the possibility also exists that poor physical health may contribute to symptoms of posttraumatic distress (Paylo & Beck, 2005; Resnick, Acierno, & Kilpatrick, 1997; Roccia, Dell’Acqua, Angelini, & Berrone, 2005; Vermetten & Bremmer, 2003). Case reports and small scale epidemiologic studies have suggested, for example, that physical impairment, such as disfigurement or pain after trauma, may serve as reminders of traumatic events, thereby stimulating posttraumatic psychological distress (Paylo & Beck, 2005; Roccia et al., 2005). Resnick, Acierno, and Kilpatrick (1997) propose, for example, that physiological symptoms such as increased heart rate or pain may cue cognitions associated with the initial trauma (e.g., danger). These cognitions, in turn, can lead to avoidance or other symptoms of posttraumatic distress.
In the current study, we examine the relationship between physical health and posttraumatic distress among a sample of individuals who were hospitalized for treatment of physical injuries resulting from community violence. Functional status and posttraumatic distress were assessed within days following the assault and twice thereafter. Using cross-lagged path analysis, we assess both the cross-sectional and prospective relationships between these variables to assess the extent to which each one precedes the development of the other.
Methods
Participants
The current investigation uses data collected as part of a prospective study of the natural course of adjustment in young adults following community violence resulting in significant physical injury (Denson, Marshall, Schell, & Jaycox, 2007; Marshall & Orlando, 2002, Schell, Marshall, & Jaycox, 2004). Between October, 1998 and June 2000, all consecutively hospitalized young adults who were admitted to a large Level I trauma facility in Los Angeles for treatment of wounds from community violence were screened for eligibility. To be eligible for the study, participants had to (a) have sustained an injury inflicted by a person other than a family member or a former sexual partner, (b) be between 18 and 40 years of age, and (c) be able to communicate fluently in English or Spanish. Individuals were screened for eligibility by trained lay interviewers only at such time as potential participants were capable of giving informed consent. Fully-structured interviews were conducted face-to-face, and were carried out in either English or Spanish as needed. Three- and 12-month follow-up interviews were conducted in participants’ homes. Participants were given $25 for completing each interview. The study was approved and monitored by the Institutional Review Boards of RAND and the University of Southern California School of Medicine.
In total, 653 persons were screened for eligibility of which 423 (65%) met the study requirements. Four hundred and thirteen (98%) completed a face-to-face baseline interview conducted by trained lay interviewers; the median interval between hospital admission and the baseline interview was 5 days. Of these, 294 (71%) completed a three month follow-up assessment and 304 (74%) were assessed at 12-months; 260 (63%) were assessed at all three waves. There were minimal differences in attrition with respect to the constructs used in the current analysis: those lost-to-follow up at the three month assessment were more likely to think, at the time of their injury, that their physical recovery would occur sooner and the mean age at follow-up was about one year younger than the mean age of those lost-to-follow up at both three and twelve months. We used missing data procedures to minimize biases that may result from sample attrition.
Measures
Symptoms of posttraumatic distress
Symptoms of posttraumatic distress were assessed using the Civilian Version of the Posttraumatic Stress Disorder (PTSD) Checklist (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993). The PCL consists of 17 items corresponding to one of the three DSM-IV symptom clusters of re-experiencing, avoidance, and hyperarousal (APA, 1994). Responses are provided regarding the extent to which participants were bothered by each symptom, ranging from 1 (not at all) to 5 (extremely). The PCL has demonstrated solid psychometric properties (Andrynowski, Cordova, Studts, & Miller, 1998; Blanchard, Jones-Alexander, Buckley, & Forneris, 1996; Gallagher, Riggs, Byrne, & Weathers, 1998). Items were tailored to refer to the specific incident that resulted in hospitalization. At the baseline survey, respondents reported on symptoms during the period since the attack. For the follow-up surveys, respondents reported on symptoms experienced over the preceding 7 days. For the current study, PTSD symptoms at each wave were analyzed as a latent variable that was indicated by four symptom clusters: re-experiencing, avoidance, numbing, and hyperarousal.
Physical functioning
Physical health and functioning was derived from 15 items drawn from the physical domain of the RAND-36 Health Status Inventory (HSI; Hays, Prince-Embury, & Chen, 1998). The RAND-36 is perhaps the most widely used instrument to measure health-related quality of life; the scale and its sub-scales have been associated with chronic medical conditions such as heart disease (e.g., Stewart et al., 1989) and mortality among the critically ill (e.g., Kaarlola, Pettila, & Kekki, 2004). Questions from the physical domain cover four areas: general health perception, physical functioning, physical pain and physical health-related role limitations. Items assessed respondents’ general health status and were not tailored to refer specifically to their injury. Because of our interest in physical, rather than emotional, health functioning, RAND-36 items that measure emotional well-being, limitations due to emotional health, and energy/fatigue were excluded.
At the baseline interview, pretrauma physical health and functioning was assessed, and the question stems were modified to reflect health “before your injury.” For example, the item, “How much bodily pain did you have ‘during the past 4 weeks’”? was changed to ‘during the 4 weeks before your injury’. For the 3- and 12-month interviews, the standard RAND-36 time frames were used; questions were keyed to current health perceptions and physical functioning while role limitation and pain items referenced the past 4 weeks. Individual items were answered with various response options (i.e., yes/no; not at all/a little/a lot). The scale was administered in the standard format; for analysis, responses to all questions were rescaled to range between 0 and 100, with low numbers corresponding to greater impairment. Physical functioning was measured as a latent variable indicated by three item-parcels created using every third item, each composed as the average of 5 scale items.
Other Covariates
Our research topic addresses the relationship between physical health and distress. We pursued a modeling strategy that accounted for demographic factors and characteristics associated with the injury that are not endogenous with posttraumatic distress or physical functioning yet which might confound this relationship, thereby modeling the portion of distress and physical functioning not accounted for by these other factors. Specifically, the covariates included in our model were:
Length of hospitalization
Duration of hospitalization, obtained from medical records, was included as a measure of injury severity. We used the square-root transform of this item to better meet the distributional assumptions of the analyses and improve the prediction of mental health and physical functioning outcomes.
Injury severity
Injury severity scores (ISS) were obtained from hospital records (Baker, O’Neill, Haddon, & Long, 1974). Values range from 1 to 75 and are based on the site and extent of injuries with higher values reflecting a higher likelihood of death from the injuries. We used the square-root transform of this item to better meet the distributional assumptions of the analyses and improve the prediction of mental health and physical functioning outcomes.
Perceived injury severity
Respondents were asked at baseline to rate, using a single item, the severity of their injury, at its worst. Responses ranged from 0 (not at all severe) to 5 (life-threatening).
Perceived physical recovery
Respondents were asked at baseline, using a single item, how long they felt it would take for them to “fully physically recover” from the injury. Responses ranged from 0 (a few days) to 5 (may not recover).
Demographic factors
Respondent age was assessed by self-report; gender was assessed by interviewer observation.
Data Analysis
We implemented structural equation modeling, using Mplus (Muthén and Muthén, 2006), as our general analytic strategy to assess the relationship between posttraumatic distress and physical functioning after a violent attack. A longitudinal measurement model was estimated for both PTSD and physical functioning in which the factor loadings for each indicator were constrained to be invariant across waves, and error terms were allowed to correlate with themselves across adjacent waves.
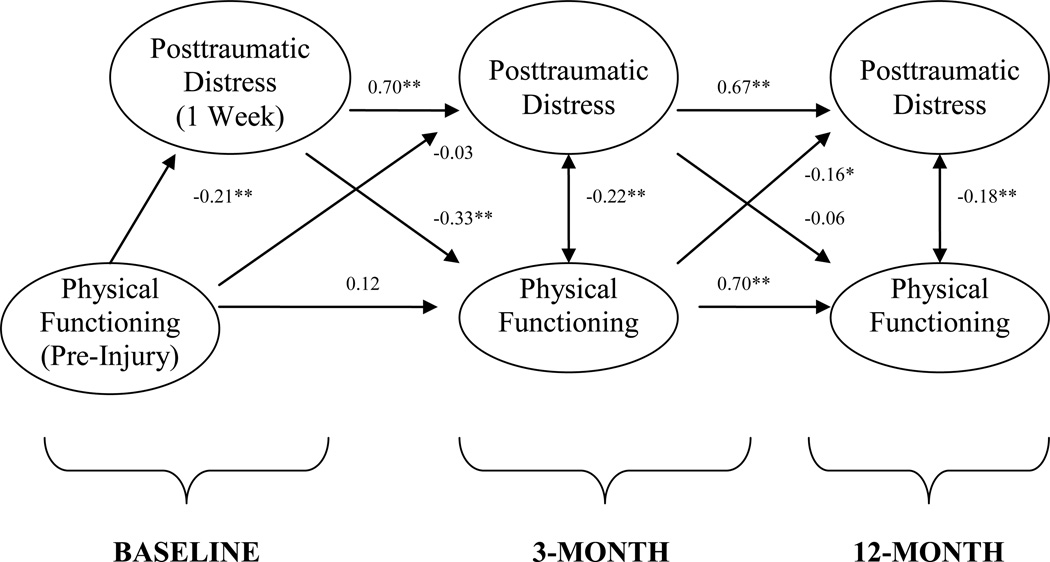
A cross-lagged structural model was then fit to these latent variables, as shown in Figure 1. Each construct from the follow up waves was regressed on both constructs from the prior wave. Correlations between the residuals of PTSD and physical health functioning within a follow up wave were also estimated. Because baseline physical health functioning was assessed with respect to a pre-injury time frame and PTSD symptoms with respect to a post-injury time frame, baseline PTSD was regressed on baseline physical health functioning.
Figure 1. Final Structural Model of Posttraumatic Distress and Physical Functioning.
Notes. Numbers denote standardized path coefficients that were estimated while controlling for seven covariates not shown in the figure. *p<0.05, **p<0.001
In addition to the theoretically defined paths between posttraumatic distress symptoms and physical functioning, we included several covariates in the model (i.e., gender, age, injury severity, length of hospitalization, perceived injury severity at baseline, and perceived likelihood of recovery). In an initial model, we regressed both PTSD symptoms and physical health status from all waves on all covariates. To create a more parsimonious model and improve the reliability of our estimates, we removed unnecessary covariate paths using a pruning procedure. Paths between covariates and outcomes were removed iteratively in a stepwise manner until there was no further reduction in the Akaike Information Criteria (AIC). This strategy is a conservative approach to exclusion, retaining all effects that have p-values less than approximately .20.
To account for sample attrition, we conducted all analyses using expectation maximization (EM) parameter estimates (McLachlan & Krishnan, 1996). EM avoids sample biases that can occur when cases are omitted from the analysis for having missed at least one follow-up interview (Little & Rubin, 1987). When data are “missing at random” or “missing completely at random”, EM is an unbiased method for increasing inferential power. Muthén & Muthén (2006) recommend a minimum of 10% covariance coverage (the proportion of data present to estimate each pairwise relationship); in the current study, covariance coverage ranges from 59% to 100%. All standard error estimates were derived with sandwich estimation which is robust to deviations from normality (Huber, 1964).
Results
Descriptive Analysis
The sample consists of 413 individuals assessed at baseline. The majority of the sample was male (94%) and the average age was 25 (SD = 5.8). Fifty-nine percent had sustained gunshot injuries and the remainder was injured from other penetrating or blunt objects. Seventy-eight percent self-identified as Hispanic, 13% self-identified as Black; 3% identified as non-Hispanic Caucasian; 3% identified as Asian; and 4% identified as Native American, multiracial, or other. The average injury severity score was 9 (SD = 8.41) which is considered to be of mild severity (Baker et al., 1974); average length of hospitalization was approximately 7 days (SD = 8 days). On average, respondents reported that their injuries were very severe (M = 3.0; SD = 1.2) and that it would take them between a few weeks and a few months (M = 1.9; SD = 0.90) to fully physically recover from the injury.
The mean level of pre-injury physical functioning across all items (recorded at baseline) is close to the maximum level of 100 (M = 92; SD = 14). At 3-months, the mean level of physical functioning was 67 (SD = 27), and at 12-months the mean level was 75 (SD = 24). The mean level of posttraumatic distress for the group was 39 at baseline (SD = 13.77), 36 (SD = 14.28) at 3-months and 34 (SD = 14.45) at 12-months (range: 17 to 85).
Different strategies have been suggested for using the PCL to identify persons who meet screening criteria for PTSD. We used two of these strategies to illustrate the degree of distress in this sample. First, individual symptoms receiving a score of 3 (moderately) or greater were treated as indicating symptom presence and mapped against the DSM–IV criteria B–D (Weathers et al., 1993). Following this scoring strategy, 25% of participants met screening criteria for PTSD at the initial assessment (excluding duration), whereas 26% and 20% met criteria at 3- and 12-month assessments. In addition, using a total PCL score of 44 as a cut point (Blanchard et al., 1997), 33%, 25%, and 24% meet screening criteria for PTSD and baseline, 3- and 12-month assessments, respectively.
Structural Equation Model
Our longitudinal measurement model including only PTSD and physical functioning fit the data well (χ2 (174) = 286.7, CFI=0.98, SRMR=0.04). We then estimated the full cross-lagged structural model including associations between the selected covariates and each of the mental and physical health constructs. After an iterative pruning procedure, 12 of 36 paths between covariates and the outcome measures were estimated in the final model. This final model fit the data well, χ2 (298) = 519.48, CFI = 0.95, RMSEA = 0.04. Factor loadings from the complete SEM are presented in Table 1.
Table 1.
Final Model Factor Loadings
| Average Standardized Loadings |
Unstandardized Loadings |
|
|---|---|---|
| Posttraumatic | ||
| Distress | ||
| Re-experiencing | 0.83 | 1.00 |
| Avoidance | 0.69 | 0.95 |
| Numbing | 0.74 | 0.83 |
| Hyperarousal | 0.82 | 0.96 |
| Physical | ||
| Functioning | ||
| Item parcel 1 | 0.85 | 1.00 |
| Item parcel 2 | 0.90 | 0.80 |
| Item parcel 3 | 0.90 | 0.93 |
Note. Unstandardized loadings were constrained to be equal across the three time points, but variances were not. The standardized loadings presented are the unweighted means of the standardized loadings across three timepoints.
Figure 1 shows the standardized path coefficients that relate physical functioning to psychological distress over time from the final model. As is common in longitudinal studies with closely spaced measurement intervals, the constructs were relatively stable over time resulting in large autoregressive paths. One expected deviation from this pattern was that pre-injury physical functioning was not a strong predictor of post-injury physical functioning.
The model revealed a somewhat complex relationship between posttraumatic distress and physical functioning over time. Higher levels of acute distress one week post injury were associated with worse than expected levels of physical functioning 3-months later, while controlling for the severity of the injury and all other covariates. This finding is consistent with a causal model in which acute psychological distress inhibits the recovery of physical functioning after injury. However, the analogous path relating 3-month PTSD symptoms to 12-month physical functioning was not significantly different from zero. Moreover, the effect of distress on physical functioning was significantly stronger in the earlier interval (delta-χ2 (1) = 10.45, p = 0.001). The cross-lagged path from physical functioning to PTSD symptoms for the 3- to 12-month interval indicates that individuals with poor physical functioning at 3-months had more severe psychological distress at 12-months than would be expected based on their earlier distress and injury severity. This observation is consistent with a causal model in which impaired physical functioning exacerbates PTSD symptoms. The standardized path from 3-month physical functioning to 12-month posttraumatic distress was not significantly greater than the reciprocal effect of 3-month distress on 12-month functioning (delta-χ2 (1) = 1.02, p = 0.31).
The model also revealed significant negative associations between the residual variability of physical functioning and the residual variability in PTSD symptoms within both the 3- and 12-month waves. Individuals who have greater distress than would be expected at a given wave tend to also have worse physical functioning than would be expected at that wave. This finding may be due to a shared source of error, the common cause of an omitted covariate, or causal effects between psychological distress and physical functioning that are not captured in this model (e.g., an effect of physical functioning on PTSD symptoms that occurred at 8 months and is therefore not measured).
The final model also revealed associations between the covariates and both physical functioning and posttraumatic distress (see Table 2). For the most part, the associations between covariates and all outcomes are consistent with prior epidemiologic research on PTSD, attesting to the construct validity of our chosen outcome measures. For example, individuals who perceived the injury as either more severe or requiring a longer recovery tended to have worse psychological outcomes. In contrast, those who were hospitalized longer or predicted a longer recovery period had worse subsequent physical functioning. In addition, most of the effects of covariates on 12-month outcomes were indirectly influenced by early outcomes; thus, the direct paths of covariates to 12-month outcomes could often be parsimoniously omitted from the final model.
Table 2.
Association of Covariates with Posttraumatic Distress and Physical Functioning
| Pre-Injury | Post-Injury | ||||||
|---|---|---|---|---|---|---|---|
| Initial | 3 Months | 12 Months | |||||
| Construct | Physical Functioning |
Post- traumatic Distress |
Post- traumatic Distress |
Physical Functioning |
Post- traumatic Distress |
Physical Functioning |
|
| Male | --- | --- | −0.10* | --- | --- | 0.07* | |
| Age | −0.22 | --- | 0.09 | --- | --- | --- | |
| Injury Severity | --- | 0.14* | −0.09 | --- | --- | --- | |
| Length of Hospitalization | --- | −0.08 | --- | −0.32** | --- | --- | |
| Self-perception of Injury | --- | 0.20** | --- | --- | --- | --- | |
| Self-perception of Recovery | −0.14 | 0.16* | --- | −0.19* | --- | --- | |
Notes. Numbers denote standardized path coefficients in the final model.
p < .05;
p < .001.
Dashes indicate coefficients that could parsimoniously be assumed to be zero the final model.
Discussion
This longitudinal study of hospitalized survivors of community violence examined key issues concerning the interrelationship between posttraumatic distress and physical functioning. To our knowledge, this study is the first to systematically estimate the reciprocal cross-lagged relationships between these constructs over time. This investigation differs from other similar research in focusing on posttraumatic distress and physical functioning in the relatively immediate aftermath of trauma exposure. Results suggest a complex pattern of reciprocal effects. First, these findings document that early posttraumatic distress has a negative influence on subsequent physical functioning. Specifically, individuals who experienced greater distress in the days immediately following physical injury were more likely to report poorer than expected physical functioning at 3 month follow-up. This finding held, even after accounting for objective and subjective measures of injury severity. However, posttraumatic distress experienced 3-months post-injury was a less important determinant of long term physical functioning. Although the negative effects of acute posttraumatic distress may persist over time due to the high degree of stability in physical functioning after three months, we did not find significant evidence that later psychological distress continues to directly degrade physical functioning between three and 12 months. Findings also demonstrate that poor physical functioning is associated with subsequent posttraumatic distress. Specifically, we found that physical impairment at 3-month follow-up was linked to higher than expected levels of psychological distress at 12-month follow-up.
Our findings are particularly notable inasmuch as psychological research has previously shown relationships between distress and physical functioning, but has not demonstrated a temporal order in the development of these two constructs. The present study found evidence that PTSD symptoms and physical functioning problems can each precede the development of (or inhibit recovery from) the other problem. Individuals with high acute PTSD symptoms subsequently developed worse physical functioning at 3-month follow-up, whereas those with physical functioning problems at 3-months went on to develop worse than expected PTSD symptoms at 12-months. In prior longitudinal analyses, Schnurr and colleagues (2006) examined PTSD symptoms among Vietnam veterans and found that changes in PTSD symptoms were negatively associated with changes in physical-health related quality of life during the same time. Similarly, Blanchard and colleagues (1997) showed that physical recovery between a traumatic event and 4 months later was associated with remission of PTSD 6-months after the event. These earlier studies did not establish, however, whether physical health problems preceded changes in mental health or visa versa. Therefore, the present research goes beyond the previous investigations by documenting a temporal pattern that is consistent with reciprocal causal effects.
Our research was not designed to address the specific mechanisms that might underlie the effect of physical health on the subsequent development of PTSD symptoms and vice versa, although there are several mechanisms that may be operating. For example, one possibility is that physiological symptoms become cues of the cognitive, psychological, or behavioral response to the index trauma, and lead to posttraumatic distress (Resnick, Acierno, & Kilpatrick, 1997). Another possibility is that lingering inability to perform basic tasks may make survivors more mindful of their traumatic experience than they otherwise might be. Recollection of the traumatic event may then trigger hyperarousal, avoidance, and other symptoms of posttraumatic stress disorder (Wessa & Flor, 2007). Alternatively, physical impairment may limit occupational or social functioning, thereby increasing a traumatized individual’s reliance on coworkers, family, and friends to accomplish basic tasks which might also exacerbate symptoms of distress (Stein et al., 1997). Another conjecture is that that poor physical functioning might also interfere with seeking mental health care for psychiatric problems, thus resulting in greater psychiatric distress (Smith, Schnurr, & Rosenheck, 2005; Savoka & Rosenheck, 2000). Research on the mechanisms underlying the observed relationships is needed, and might be informed by the results of the current study inasmuch as mechanisms should account not only for the association of distress and physical functioning in individuals with chronic PTSD but also must explain how distress might influence health relatively soon after trauma exposure.
Inasmuch as these data suggest that initial posttraumatic distress was more important than subsequent distress in predicting changes in physical functioning following sudden physical injury, our findings have important clinical implications. Currently, with few exceptions (Zatzick, 2003), evaluation and treatment is uncommon for individuals at risk for PTSD following hospitalization for traumatic injury. This pattern is particularly true of our own sample in which less than 50% of individuals with mental health needs received care in the year following their assault (Jaycox et al., 2004). Early intervention in trauma centers has been recommended as a means of preventing the development of PTSD (Zatzick, Russo, Roy-Byrne, Jurkovich, & Katon, 2005). The current findings suggest that these interventions may promote both physical and emotional recovery in at least two ways. First, early intervention may reduce the likelihood of acute distress, which is directly and strongly linked with later PTSD symptoms. Moreover, the benefits of psychological interventions on acute posttraumatic distress may directly improve short-term (e.g., 3-month) physical functioning. Given that acute distress independently predicts physical functioning, the possibility exists that early psychological interventions aimed at reducing acute distress may improve subsequent physical functioning. To the extent that acute psychological distress may hamper posttraumatic physical functioning as well as posttraumatic mental health, these findings underscore the potential value of developing and implementing interventions for acute psychological care within the general trauma setting (e.g., Zatzick et al., 2005).2 Data from the current study suggest both that research examining the effectiveness of psychological interventions following trauma should continue to include physical functioning outcomes, and that new interventions be designed to consider the potential effects on physical functioning.
There are several limitations of the current study that highlight the need for additional research. First, like virtually all research on the relationship of posttraumatic distress and functional status (e.g., Holbrook et al., 2001; Jacobsen et al., 1998; Kapfhammer et al., 2004; Schnurr et al., 2006; Kimerling et al., 2000; Michaels et al., 1999; Paylo & Beck, 2005; Magruder et al., 2004), we relied on self-reported functional status. Although this strategy has proven valuable for many purposes, future research is needed to corroborate self-reported functional status with objective measures of functional status or other measures of health status. Moreover, given that we have no measure of self-reported physical health immediately after the attack, these data do not permit examination of the potential impact of physical functioning immediately following physical injury on subsequent health and well-being. Of course, it is likely that these measures would be highly collinear with our existing measures of injury severity inasmuch as physical functioning for physically injured patients who are interviewed shortly after hospitalization is likely to be heavily determined by their injury. To the extent that this information would prove valuable, however, further research is indicated. In addition, our sample also consisted primarily of young, urban, male, and Hispanic victims of community violence. Although studies of this group of individuals fills an important gap in the literature (Cabassa, Zayas, & Hansen, 2006), future research is needed to discern the extent to which these findings may be generalizable to survivors from other sociodemographic backgrounds as well as survivors of different types of trauma. Furthermore, inasmuch as we studied individuals who had required hospitalization for the treatment of injuries, the relevance of these findings to those who experience less severe physical injuries is unclear. In addition, we introduced a minor change to a well-validated instrument assessing health status and health-related functioning to adjust for pre-existing differences in physical health (Hays, Prince-Embury, & Chen, 1998). To the extent that this alteration introduced bias, additional research using truly prospective design to assess health status pre-injury would prove useful.
Finally, although this study examined symptoms of PTSD, our findings do not imply that symptoms of PTSD are uniquely related to functional impairment independently of other mental health constructs such as general distress or depressive symptoms. Research indicates, in fact, that symptoms of PTSD and depression are highly correlated following traumatic injury (e.g., O'Donnell, Creamer, & Pattison, 2004; Shalev et al., 1998). Moreover, much research has focused on the relationship between impaired physical functioning and symptoms of depression (Hays, Marshall, Wang, & Sherbourne, 1994; Kosloski, Stull, Kercher, & Van Dussen, 2005; Wells et al., 1989). Although research has documented an independent effect of PTSD symptoms on physical health, particularly cardiovascular outcomes, independent of depressive symptoms (Boscarino & Chang, 1999; Kubzansky et al., 2007), future research might investigate whether symptoms of PTSD influence physical functioning independently of depressive symptoms and visa versa.
In summary, this longitudinal study examined the relationship between posttraumatic distress and physical functioning over time. Results indicate that higher levels of posttraumatic distress immediately following a violent injury presage a poorer physical recovery from the injury. In addition, lower physical functioning after an injury is linked with greater than expected posttraumatic distress at 12-month follow-up. Given the prevalence of community violence in the United States, further research on this topic has significant clinical and public health relevance. Interventions aimed at improving health in one domain should be investigated as having the potential to promote health in the other.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health (R01MH056122 and R01MH071636), the National Institute of Alcohol Abuse and Alcoholism (R01AA014246) and the William T. Grant Foundation (99-1959-99). The views expressed are those of the authors and do not necessarily reflect those of the NIMH, the NIAAA, the William T. Grant Foundation, or the RAND Corporation. We gratefully acknowledge the generosity of the assault survivors who participated in this study as well as the efforts of the RAND Survey Research Group interview team.
Footnotes
In this study, the authors report estimating the unidirectional relationship from physical functioning to PTSD symptoms in a separate model that yielded roughly equivalent findings. It is difficult to interpret this finding, however, inasmuch as no data are presented and the authors do not appear to have modeled relevant paths simultaneously.
The few reported trials of clinical interventions for PTSD have found the interventions to be more effective in reducing psychological distress than in improving physical functioning (e.g., Schnurr et al., 2007; Malik et al., 1999). It should be noted, however, that this research has not examined acute posttraumatic distress per se.
References
- American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Andrynowski MA, Cordova MJ, Studts JL, Miller TW. Posttraumatic stress disorder after treatment for breast cancer: Prevalence of diagnosis and the use of the PTSD Checklist-Civilian Version (PCL-C) as a screening instrument. Journal of Consulting and Clinical Psychology. 1998;66:586–590. doi: 10.1037//0022-006x.66.3.586. [DOI] [PubMed] [Google Scholar]
- Association for the Advancement of Automotive Medicine. The Abbreviated Injury Scale (revision) Des Plaines, IL: Author; 1990. [Google Scholar]
- Baker SP, O’Neil B, Haddon WJ, Long WB. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. Journal of Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- Beckham JC, Moore SD, Feldman ME, Herzberg MA, Kirby AC, Fairbank JA. Health status, somatization, and severity of posttraumatic stress disorder in Vietnam combat veterans with posttraumatic stress disorder. American Journal of Psychiatry. 1998;155:1565–1569. doi: 10.1176/ajp.155.11.1565. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley T, Forneris CA. Psychometric properties of the PTSD checklist (PCL) Behaviour Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Hickling EJ, Forneris CA, Taylor AE, Buckley TC, Loos WR, Jaccard J. Prediction of remission of acute posttraumatic stress disorder in motor vehicle accident victims. Journal of Traumatic Stress. 1997;10:215–234. doi: 10.1023/a:1024826028483. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Chang J. Electrocardiogram abnormalities among men with stress-related psychiatric disorders: Implications for coronary heart disease and clinical research. Annals of Behavioral Medicine. 1999;21:227–234. doi: 10.1007/BF02884839. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC. Posttraumatic stress disorder in an urban population of young adults: Risk factors for chronicity. American Journal of Psychiatry. 1992;149:671–675. doi: 10.1176/ajp.149.5.671. [DOI] [PubMed] [Google Scholar]
- Cabassa LJ, Zayas LH, Hansen MC. Latino adults’ access to mental health care: A review of epidemiological studies. Administration and Policy in Mental Health. 2006;33:316–330. doi: 10.1007/s10488-006-0040-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano SM. Criminal victimization, 2005, Bureau of Justice Statistics Bulletin, NCJ 214644. Washington, DC: U.S. Department of Justice; 2006. Sep, [Google Scholar]
- Collopy BT, Tulloh BR, Rennie GC, Fink RL, Rush JH, Trinca GW. Correlation between injury severity scores and subjective ratings of injury severity: A basis for trauma audit. Injury. 1992;23:489–492. doi: 10.1016/0020-1383(92)90074-3. [DOI] [PubMed] [Google Scholar]
- Denson TF, Marshall GN, Shell TL, Jaycox LH. Predictors of posttraumatic distress 1 year after exposure to community violence: the importance of acute symptom severity. Journal of Consulting and Clinical Psychology. 2007;75:683–692. doi: 10.1037/0022-006X.75.5.683. [DOI] [PubMed] [Google Scholar]
- Dougall AL, Baum A. Psychoneuroimmunology and trauma. In: Schnurr PP, Green BL, editors. Trauma and health: Physical health consequences of exposure to extreme stress. Washington, DC: American Psychological Association; 2004. pp. 129–155. [Google Scholar]
- Friedman MJ, McEwan BS. Posttraumatic stress disorder, allostatic load, and medical illness. In: Schnurr PP, Green BL, editors. Trauma and health: Physical health consequences of exposure to extreme stress. Washington, D.C: American Psychological Association; 2004. pp. 157–188. [Google Scholar]
- Friedman MJ, Schnurr PP. The relationship between trauma, PTSD, and physical health. In: Friedman MJ, Charney DS, Deutch AY, editors. Neurobiological and clinical consequences of stress: From normal adaptation to PTSD. Philladelphia, PA: Raven; 1995. pp. 507–524. [Google Scholar]
- Ford DE. Depression, trauma, and cardiovascular health. In: Schnurr PP, Green BL, editors. Trauma and health: Physical health consequences of exposure to extreme stress. Washington, DC: American Psychological Association; 2004. pp. 73–97. [Google Scholar]
- Gallagher JG, Riggs DS, Byrne CA, Weathers FW. Female partners’ estimations of male veterans’ combat-related PTSD severity. Journal of Traumatic Stress. 1998;11:367–374. doi: 10.1023/A:1024411422586. [DOI] [PubMed] [Google Scholar]
- Hays RD, Prince-Embury S, Chen H. RAND-36 Health Status Inventory. San Antonio, TX: The Psychological Corporation; 1998. [Google Scholar]
- Hays RD, Marshall GN, Wang EYI, Sherbourne CD. Four-year cross-lagged associations between physical and mental health in the Medical Outcomes Study. Journal of Consulting and Clinical Psychology. 1994;62:441–449. doi: 10.1037//0022-006x.62.3.441. [DOI] [PubMed] [Google Scholar]
- Holbrook TL, Hoyt DB, Stein MB, Seiber WJ. Perceived threat to life predicts posttraumatic stress disorder after major trauma: Risk factors and functional outcomes. Journal of Trauma. 2001;51:287–293. doi: 10.1097/00005373-200108000-00010. [DOI] [PubMed] [Google Scholar]
- Huber PJ. Robust estimation of a location parameter. Annals of Mathematical Statistics. 1964;35:73–101. [Google Scholar]
- Jacobsen PB, Widows MR, Hann DM, Andrykowski MA, Kronish LE, Fields KK. Posttraumatic stress disorder symptoms after bone marrow transplantation for breast cancer. Psychosomatic Medicine. 1998;60:366–371. doi: 10.1097/00006842-199805000-00026. [DOI] [PubMed] [Google Scholar]
- Jaycox LH, Marshall GN, Schell TL. Use of mental health services by men injured through community violence. Psychiatric Services. 2004;55:415–420. doi: 10.1176/appi.ps.55.4.415. [DOI] [PubMed] [Google Scholar]
- Kampfhammer HP, Rothenhausler HB, Krauseneck T, Stoll C, Schellig G. Posttraumatic stress disorder and health-related quality of life in long-term survivors of acute respiratory distress syndrome. American Journal of Psychiatry. 2004;161:45–52. doi: 10.1176/appi.ajp.161.1.45. [DOI] [PubMed] [Google Scholar]
- Kaarlola A, Pettila V, Kekki P. Performance of two measures of general health-related quality of life, the EQ-5D and the RAND-36 among critically ill patients. Intensive Care Medicine. 2004;30:2245–2252. doi: 10.1007/s00134-004-2471-6. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Greenberg DF. Linear panel analysis: Models of quantitative change. San Diego, CA: Academic Press; 1981. [Google Scholar]
- Kimmerling R, Clum GA, Wolfe J. Relationships among trauma exposure, chronic posttraumatic stress disorder symptoms, and self-reported health in women: Replication and extension. Journal of Traumatic Stress. 2000;13:115–128. doi: 10.1023/A:1007729116133. [DOI] [PubMed] [Google Scholar]
- Kosloski K, Stull DE, Kercher K, Van Dussen DJ. Longitudinal analysis of the reciprocal effects of self-assessed global health and depressive symptoms. Journal of Gerontology. Series B, Psychological Sciences and Social Sciences. 2005;60B:296–303. doi: 10.1093/geronb/60.6.p296. [DOI] [PubMed] [Google Scholar]
- Kubzansky LD, Koenen KC, Spiro A, 3rd, Vokonas PS, Sparrow D. Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the Normative Aging Study. Archives of General Psychiatry. 2007;64:109–116. doi: 10.1001/archpsyc.64.1.109. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. New York: Wiley; 1987. [Google Scholar]
- Lauterbach D, Vora R, Rakow M. The relationship between posttraumatic stress disorder and self-reported health problems. Psychosomatic Medicine. 2005;67:939–947. doi: 10.1097/01.psy.0000188572.91553.a5. [DOI] [PubMed] [Google Scholar]
- Magruder KM, Frueh BC, Knapp RG, Johnson MR, Vaughan JA, Carson TC, Powell DA, Hebert R. PTSD symptoms, demographic characteristics, and functional status among veterans treated in VA primary care clinics. Journal of Traumatic Stress. 2004;17:293–301. doi: 10.1023/B:JOTS.0000038477.47249.c8. [DOI] [PubMed] [Google Scholar]
- Malik ML, Connor KM, Sutherland SM, Smith RD, Davison RM, Davidson JRT. Quality of life and posttraumatic stress disorder: A pilot study assessing changes in SF-36 scores before and after treatment in a placebo-controlled trial of fluoxetine. Journal of Traumatic Stress. 1999;12:387–393. doi: 10.1023/A:1024745030140. [DOI] [PubMed] [Google Scholar]
- Marshall GN, Orlando M. Acculturation and peritraumatic dissociation in young adult Latino survivors of community violence. Journal of Abnormal Psychology. 2002;111:166–174. doi: 10.1037//0021-843x.111.1.166. [DOI] [PubMed] [Google Scholar]
- Mayer L, Carrol S. Testing for lagged, contemporal and total dependence in cross-lagged panel analysis. Sociological Methods and Research. 1987;16:187–217. [Google Scholar]
- McLachlan GJ, Krishnan T. The EM algorithm and extensions. New York: Wiley-Interscience; 1996. [Google Scholar]
- Michaels AJ, Michaels CE, Moon CH, Smith JS, Zimmerman MA, Taheri PA, Peterson C. Posttraumatic stress disorder after injury: Impact on general health outcome and early risk assessment. Journal of Trauma. 1999;47:460–466. doi: 10.1097/00005373-199909000-00005. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus: The comprehensive modeling program for applied researchers [Computer Program] Los Angeles: Muthé & Muthén; 2006. [Google Scholar]
- O’onnell ML, Creamer M, Elliott P, Atkin C, Kossmann T. Determinants of quality of life and role-related disability after injury: Impact of acute psychological responses. Journal of Trauma. 2005;59:1328–1335. doi: 10.1097/01.ta.0000197621.94561.4e. [DOI] [PubMed] [Google Scholar]
- O'onnell ML, Creamer M, Pattison P. Posttraumatic stress disorder and depression following trauma: Understanding comorbidity. American Journal of Psychiatry. 2004;161:1390–1396. doi: 10.1176/appi.ajp.161.8.1390. [DOI] [PubMed] [Google Scholar]
- Paylo SA, Beck JG. Posttraumatic stress disorder symptoms, pain, and perceived life control: Associations with psychosocial and physical functioning. Pain. 2005;117:121–127. doi: 10.1016/j.pain.2005.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick HS, Acierno R, Kilpatrick DG. Health impact of interpersonal violence 2: Medical and mental health outcomes. Behavioral Medicine. 1997;23:65–78. doi: 10.1080/08964289709596730. [DOI] [PubMed] [Google Scholar]
- Rheingold AA, Acierno R, Resnick HS. Trauma, posttraumatic stress disorder, and health risk behaviors. In: Schnurr PP, Green BL, editors. Trauma and health: Physical health consequences of exposure to extreme stress. Washington, DC: American Psychological Association; 2004. pp. 217–243. [Google Scholar]
- Roccia F, Dell’Acqua A, Angelini G, Berrone S. Maxillofacial trauma and psychiatric sequelae: Posttraumatic stress disorder. Journal of Craniofacial Surgery. 2005;16:355–360. doi: 10.1097/01.scs.0000157028.44315.b8. [DOI] [PubMed] [Google Scholar]
- Savoka E, Rosenheck R. The civilian labor market experiences of Vietnam-era veterans: The influence of psychiatric disorders. The Journal of Mental Health Policy and Economics. 2000;3:199–207. doi: 10.1002/mhp.102. [DOI] [PubMed] [Google Scholar]
- Schell TL, Marshall GN, Jaycox LH. All symptoms are not created equal: The prominent role of hyperarousal in the natural course of posttraumatic psychological distress. Journal of Abnormal Psychology. 2004;113:189–197. doi: 10.1037/0021-843X.113.2.189. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Freidman MJ, Engel CC, Foa EB, Shea MT, Chow BK, Resick PA, Thurston V, Orsillo SM, Haug R, Turner C, Bernardy N. Cognitive behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. Journal of the American Medical Association. 2007;297:820–830. doi: 10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Hayes AF, Lunney CA, McFall M, Uddo M. Longitudinal analysis of the relationship between symptoms and quality of life in veterans treated for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2006;74:707–713. doi: 10.1037/0022-006X.74.4.707. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Green BL. Understanding relationships among trauma, posttraumatic stress disorder, and health outcomes. In: Schnurr PP, Green BL, editors. Trauma and health: Physical health consequences of exposure to extreme stress. Washington, DC: American Psychological Association; 2004. pp. 247–275. [Google Scholar]
- Schnurr PP, Jankowski MK. Physical health and posttraumatic stress disorder: review and synthesis. Seminars in Clinical Neuropsychiatry. 1999;4:295–304. doi: 10.153/SCNP00400295. [DOI] [PubMed] [Google Scholar]
- Schonfeld WH, Verboncoeur CJ, Fifer SK, Lipschutz RC, Lubeck DB, Buesching DP. The functioning and well-being of patients with unrecognized anxiety disorders and major depressive disorder. Journal of Affective Disorders. 1997;43:105–119. doi: 10.1016/s0165-0327(96)01416-4. [DOI] [PubMed] [Google Scholar]
- Seng JS, Clark MK, McCarthy AM, Ronis DL. PTSD and physical comorbidity among women receiving Medicaid: Results from service-use data. Journal of Traumatic Stress. 2006;19:45–56. doi: 10.1002/jts.20097. [DOI] [PubMed] [Google Scholar]
- Shalev AY, Freedman S, Peri T, Brandes D, Sahar T, Orr SP, Pitman RK. Prospective study of posttraumatic stress disorder and depression following trauma. American Journal of Psychiatry. 1998;155:630–637. doi: 10.1176/ajp.155.5.630. [DOI] [PubMed] [Google Scholar]
- Smith MW, Schnurr PP, Rosenheck RA. Employment outcomes and PTSD symptom severity. Mental Health Services Research. 2005;7:89–101. doi: 10.1007/s11020-005-3780-2. [DOI] [PubMed] [Google Scholar]
- Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: Findings from a community survey. American Journal of Psychiatry. 1997;154:1114–1119. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Greenfield S, Hays RD, Wells K, Rogers WH, Berry SD, McGlynn EA, Ware JE. Functional status and well-being of patients with chronic conditions: Results from the medical outcomes study. Journal of the American Medical Association. 1989;262:907–913. [PubMed] [Google Scholar]
- Vermetten E, Bremner JD. Olfaction as a traumatic reminder in posttraumatic stress disorder: Case reports and review. Journal of Clinical Psychiatry. 2003;64:202–207. doi: 10.4088/jcp.v64n0214. [DOI] [PubMed] [Google Scholar]
- Walker EA, Newman E, Koss MP. Costs and health care utilization associated with traumatic experiences. In: Schnurr PP, Green BL, editors. Trauma and health: Physical health consequences of exposure to extreme stress. Washington, DC: American Psychological Association; 2004. pp. 43–69. [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): Reliability, validity, and diagnostic validity. San Antonio, TX: Paper presented at the International Society for Traumatic Stress Studies; 1993. Oct, [Google Scholar]
- Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, Berry S, Greenfield S, Ware H. The functioning and well-being of depressed patients: results from the Medical Outcomes Study. Journal of the American Medical Association. 1989;262:914–919. [PubMed] [Google Scholar]
- Wessa M, Flor H. Failure of extinction of fear responses in posttraumatic stress disorder: Evidence from second-order conditioning. American Journal of Psychiatry. 2007;164:1684–1692. doi: 10.1176/appi.ajp.2007.07030525. [DOI] [PubMed] [Google Scholar]
- Wong EC, Schell TL, Marshall GN, Elliott MN, Babey SH, Hambarsoomians K. The legacy of violence exposure: The relative physical health status of Cambodian refugees 2 decades after resettlement. Manuscript under review. 2007 doi: 10.1007/s10903-010-9392-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick DF. Posttraumatic stress, functional impairment, and service utilization after injury: A public health approach. Seminars in Clinical Neuropsychiatry. 2003;8:149–157. doi: 10.1016/s1084-3612(03)00017-0. [DOI] [PubMed] [Google Scholar]
- Zatzick DF, Russo J, Roy-Byrne P, Jurkovich G, Katon W. The detection and treatment of posttraumatic distress and substance intoxication in the acute care inpatient setting. General Hospital Psychiatry. 2005;27:57–62. doi: 10.1016/j.genhosppsych.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Zatzick DF, Marmar CR, Weiss DS, Browner WS, Metzler TJ, Golding JM, Stewart A, Schlenger WE, Wells KB. Posttraumatic stress disorder and functioning and quality of life outcomes in a nationally representative sample of male Vietnam veterans. American Journal of Psychiatry. 1997;154:1690–1695. doi: 10.1176/ajp.154.12.1690. [DOI] [PubMed] [Google Scholar]
- Zatzick DF, Jurkovich GJ, Gentilello L, Wisner D, Rivara FP. Posttraumatic stress, problem drinking, and functional outcomes after injury. Archives of Surgery. 2002;137:200–205. doi: 10.1001/archsurg.137.2.200. [DOI] [PubMed] [Google Scholar]