Abstract
This study examined suicide ideation, attempts, and subsequent mental health service among a sample of 948 youth from substance abuse treatment facilities across the U.S. Youth were surveyed at intake and every three months for a one year period. Thirty percent of youth reported ideating in at least one interview and 12% reported attempting suicide; almost half reported receiving outpatient mental health treatment at least once and close to one-third reported being on prescription drugs for an emotional or behavioral problem. Higher levels of conduct disorder symptoms were associated with ideation and attempts, while higher levels of depressive symptoms and being female were associated with ideation only. Older youth were less likely to receive outpatient and prescription drug treatment, and Black and Hispanic youth were less likely to receive prescription drug treatment than white youth. Among youth who reported ideating, those with conduct disorder were less likely to receive prescription drug treatment three months later. These findings emphasize a high prevalence of suicide risk behavior in substance abuse treatment programs, and provide insight into the specialized treatment youth in substance abuse treatment at risk for suicide currently receive.
Keywords: Suicide, adolescent, substance abuse treatment, conduct disorder
Introduction
In 2004, roughly 4,600 ten to twenty-four year olds killed themselves in the United States, making suicide the third leading cause of adolescent mortality behind unintentional injuries and homicide (Centers for Disease Control and Prevention, 2007). According to the Youth Risk Behavior Survey, 17% of high school students reported that they seriously considered a suicide attempt, and 8% reported attempting suicide in the past year (Eaton et al., 2006). These numbers stress the importance of preventing suicide among adolescents, a fact reiterated by Healthy People 2010 and recent legislation that earmarks funds specifically for preventing suicide (e.g., Garret Lee Smith Memorial Act).
Young people with substance use disorders are among those at highest risk for suicide. Post-mortem studies have shown substance use disorders are prominent among adolescents who have killed themselves (Brent et al., 1993; Fowler, Rich, & Young, 1986; Rich, Sherman, & Fowler, 1990; Runeson, 1990; Shaffer, 1998; Shaffer et al., 1996). Epidemiological surveys have also revealed an association between substance use and suicide attempts among youth in the National Longitudinal Study of Adolescent Health (Borowsky, Ireland, & Resnick, 2001) and in various community samples (Brent et al., 1988; Fowler et al., 1986; Garrison, McKeown, Valois, & Vincent, 1993; Wilcox & Anthony, 2004). Different theories have been proposed to explain the link between substance use and suicide. For instance, drug and alcohol misuse may be linked to suicide by increasing individuals’ impulsivity (Hirschfeld & Davidson, 1988) or via a common root factor that independently leads to both sets of behaviors (Jessor, 1991). These theories may explain the link between substance use and suicide outcomes for different youth; for example, youth with high levels of conduct disorder or other externalizing behaviors may make impulsive suicide attempts after drinking alcohol or using drugs, while youth with depressive symptoms or other internalizing mental health symptoms may use substances to self-medicate these symptoms, though it is these symptoms that lead to the suicide (Esposito-Smythers & Spirito, 2004).
Given the strong association between substance use and suicide, one would expect youth entering substance abuse treatment to have elevated rates of suicide ideation and attempts relative to non-clinical samples of youth. This expectation is heightened when one considers the high rates of co-morbid mental health problems, which often independently predict suicide, among youth in substance abuse treatment (Grella, Hser, Joshi, & Rounds-Bryant, 2001; Jainchill, 1997; Jaycox, Morral, & Juvonen, 2003; Stowell & Estroff, 1992). Adolescents who present at emergency departments for suicide attempts that involve drugs are also often frequently released to substance abuse treatment (The New DAWN Report: Disposition of Emergency Department Visits for Drug-Related Suicide Attempts by Adolescents: 2004, 2006). Prior studies of drug users in treatment reveal these expected high rates of suicide behaviors, though have focused primarily on retrospective reports of suicide attempts. Among youth in residential treatment, one study indicated that 20% of youth had attempted suicide at least once during the 2 years before intake (Cavaiola & Lavender, 1999), while another study found that 28% of boys and 60% of girls in treatment reported at least one suicide attempt in their lifetime (Deykin & Buka, 1994). A study of 300 youth in outpatient treatment reported that 30% reported a lifetime history of a suicide attempt (Berman & Schwartz, 1990). To our knowledge, no study has yet documented the course of suicide ideation and non-fatal attempts among youth attending substance use treatment facilities in the United States.
Although the empirical data are limited, there is sufficient reason to believe that upon entering substance abuse treatment, youth are routinely asked about suicide, though the exact questions they are asked vary. For example, under the Government Performance and Results Act (GPRA), the Center for Substance Abuse Treatment (CSAT) requires that any program receiving discretionary funding collect a uniform set of information from each client at intake and regularly thereafter, including a question about suicide attempts in the past 30 days ("CSAT GPRA Client Outcome Measures for Discretionary Programs," 2007). However, upon learning that their patient has thought about or attempted suicide in the past, providers in substance abuse treatment settings have very little guidance on how to manage the patient’s suicide risk. A key component of most published guidelines call upon providers to discern the degree of “seriousness” of a particular patient, which reflects his or her likelihood of a subsequent fatal attempt. Available criteria list current alcohol and/or drug use as well as the presence of a substance use disorder as factors that indicate serious suicide risk (American Academy of Child and Adolescent Psychiatry, 2001). Many youth entering substance abuse treatment will meet these criteria, which limits its utility in substance abuse treatment settings.
If clients acknowledge suicide ideation or attempts, the American Academy of Child and Adolescent Psychiatry provide a few general referral strategies that depend on clinicians’ assessments of the risk that clients pose to themselves. It is recommended that youth considered ‘serious’ and who exhibit unpredictable behavior should be hospitalized. For youth that providers believe are not likely to act on impulses and have sufficient support at home, outpatient treatment may be adequate. To complement these services, there is some evidence that psychopharmacological interventions can reduce suicide attempts, especially for youth with co-morbid mental disorders (American Academy of Child and Adolescent Psychiatry, 2001). This research, however, is controversial because research on the efficacy of these drugs (e.g., lithium for treating mood or other affective disorders and selective serotonin reuptake inhibitors for depression) has focused primarily on adults (Blader & Kafantaris, 2007) and may have unintended adverse consequences for youth, including possibly increasing suicide risk (Hammad, Laughren, & Racoosin, 2006). Emergency departments also play an important role in caring for adolescents who have tried to kill themselves. Within emergency departments, clinicians are encouraged to screen patients who are admitted for a suicide attempt, and to ensure the patients’ safety both in the short (e.g., making sure the patient is away from potentially lethal substances) and long-term (e.g., stressing the importance of follow-up care) (Kennedy, Baraff, Suddath, & Asarnow, 2004). Thus, there are some recommendations for treating youth with suicide risk; however, very little is known about what kinds of specialized care or referrals are actually offered to youth with established suicide risk in substance abuse treatment.
In this paper, we examine suicide ideation, attempts, and follow-up mental health treatment within a large, prospective cohort of youth attending substance abuse treatment programs. Using longitudinal methods, we investigate: (1) the prevalence of suicide ideation and non-fatal attempts among youth receiving substance abuse treatment; (2) the characteristics of youth presenting at substance abuse programs at greatest risk for suicide ideation and attempts; and (3) the type of follow-up mental health care youth report receiving upon reporting suicide ideation or attempts in this setting.
Materials and Methods
Participants
Data for this study come from the Adolescent Treatment Models (ATM) program. In brief, the ATM program was funded by the Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration (CSAT/SAMHSA) to examine longitudinal outcomes for youth admitted to substance abuse treatment programs (M.L. Dennis, Dawud-Noursi, Muck, & McDermeit, 2003). In total, 11 programs representing 10 treatment sites were awarded funding— three long-term residential programs, four outpatient programs, and four short-term residential programs (Stevens & Morral, 2003). Attempts were made at all sites to contact youth at 6-months and at 12 months post-intake; in addition, 7 of the 10 sites made attempts to contact youth at 3-months post-intake and 6 of the 10 made attempts to contact youth at 9-months post-intake. At these follow-up assessments, efforts were made to contact all youth, including youth still attending the same treatment program to which they were admitted at baseline, youth receiving treatment in a new program (including aftercare), and youth who were not attending any type of substance abuse treatment program. Due to the lagged model in the analysis plan presented below, sites that did not provide information at 3 or 9 months were excluded from the analysis. As a result, the final sample consisted of 948 youth assessed at intake from six sites (110 long-term residential, 468 short-term residential, and 370 outpatient). These 948 youth provided a total of 4362 observations. The rates of follow-up were relatively high in the sample; at 3-months, 94% of this baseline cohort was interviewed, 92% were interviewed at 6-months, 87% at 9-months, and 86% at 12-months. Nearly all youth who were admitted to treatment in each of the facilities participated in the study, with the baseline assessment conducted at intake for the residential programs and at the second visit for outpatient programs. Table 1 presents demographic and select covariate characteristics of the study sample at baseline.
Table 1.
Descriptive Characteristics of the Restricted ATM Sample.*
| Intake |
||
|---|---|---|
| n | Col % | |
| Total | 948 | 100 |
| Site | ||
| A (Long Term Residential) | 53 | 5.59 |
| B (Short Term Residential) | 153 | 16.14 |
| C (Short Term Residential & Outpatient) | 286 | 30.17 |
| E (Long & Short Term Residential) | 206 | 21.73 |
| H (Outpatient) | 138 | 14.56 |
| I (Outpatient) | 112 | 11.81 |
| Sex | ||
| Male | 684 | 72.15 |
| Female | 264 | 27.85 |
| Race | ||
| White | 525 | 55.38 |
| American Indian | 17 | 1.79 |
| Black | 91 | 9.60 |
| Hispanic | 146 | 15.40 |
| Other | 169 | 17.83 |
| Preferred Drug | ||
| Cannabis | 620 | 65.40 |
| Alcohol | 124 | 13.08 |
| Crack or cocaine | 43 | 4.54 |
| Opiates | 50 | 5.27 |
| Hallucinogens | 42 | 4.43 |
| Amphetamines | 52 | 5.49 |
| Other | 6 | 0.63 |
| N/A | 11 | 1.16 |
| M | SD | |
| Age | 15.99 | 1.36 |
| Mental Health Problems | ||
| Conduct Disorder (1) | 5.65 | 3.49 |
| Depression (2) | 3.12 | 1.96 |
| Substance Use Disorder (3) | 7.34 | 3.01 |
Sites were excluded that did not conduct follow-up assessments and 3 or 9 months.
Conduct Disorder Scale ranges from 0 to 15
Depression Severity Scale ranges from 0 to 6
Substance Use Disorder Scale ranges from 0 to 11
To assess whether there were differential rates of follow-up in the sample, we examined differences between those who were and were not interviewed at each wave with respect to sex, race, site of care, and previous suicide ideations and attempts. Bonferroni adjustments were made to determine statistically significant associations in the presence of multiple testing. Although there were no significant differences with respect to sex, there were noticeable differences with respect to race and site of care. At the 3-month assessments, Black youth were less likely to be interviewed than their counterparts of other races. In addition, one site reporting less success at achieving follow-up interviews at most waves relative to the other sites.1 Persons who reported either thinking about suicide or having attempted to kill themselves at one wave (defined below) were no more or less likely to be followed-up at the next wave.
Measures
At all waves, youth were assessed with the Global Appraisal of Individual Needs (GAIN) (M.L. Dennis, 1999). The GAIN is a structured, clinical interview including symptom, change scores, and utilization indices with sound psychometric properties (M. Dennis et al., 2004; M. Dennis et al., 2002; M.L. Dennis, 1999; M.L. Dennis et al., 2003). At baseline, youth were asked “during the past year, have you thought about ending your life or committing suicide,” an endorsement of this item was defined as suicide ideation (SI). If youth did endorse this item, they were then asked “during the past year, have you attempted to commit suicide.” An endorsement of this item was defined as a suicide attempt (SA). At three, six, nine, and 12-month follow-up visits, the referent time interval for these questions was during the past 90 days.
Four indicators of mental health service utilization, each taken from follow-up assessments, were measured. Treatment with prescription drugs was assessed using a question that asked “are you currently taking medication for mental, emotional, behavioral, or psychological problems?” Other mental health care outcomes were assessed with three separate questions that asked “During the past 90 days, how many (a) nights total did you spend in the hospital for mental, emotional, behavioral or psychological problems; (b) times did you see a doctor in an office or outpatient clinic for mental, emotional, behavioral or psychological problems; (c) times have you had to go to the emergency room for mental, emotional, behavioral, or psychological problems.” For each of these three items, responses were collapsed to create four dichotomous outcomes indicating any of the specific types of care (i.e., response was greater than 0) versus no care (response = 0).
At each wave, scales that measured symptoms of depression, conduct disorder, and substance use disorders were also assessed. The depression symptom scale is based on six items and is a count of depressive symptoms in the past year (at baseline) or past 90 days (at follow-up visits) and ranges from 0 to 6 with higher scores indicating higher depressive symptom levels (15% at baseline were categorized as in the high range of the scale, as indicated by a total score=6) (M. L. Dennis, Ives, & Funk, 2007). The conduct disorder scale is based on 15 items and is a count of DSM-IV symptoms associated with conduct disorder in the past year (at baseline) and past 90 days (at follow-up visits) and ranges from 0 to 15, with higher scores indicating greater behavioral problems (31% at baseline were categorized as in the high range of the scale, as indicated by a total score > 7) (M. L. Dennis et al., 2007). The substance use disorder scale is based on 11 items and is a count of DSM-IV symptoms of either substance abuse or dependence in the past year and ranges from 0 to 11, though the scale is not indexed to specific substances (55% at baseline were categorized as in the high range of the scale, as indicated by a total score > 7) (M. L. Dennis et al., 2007).
Baseline covariates included sex, race/ethnicity assessed via self-report and collapsed into five categories (White, American Indian, Black, Hispanic, and other), age, and a treatment site identifier.
Analysis
Prevalence of suicide ideation, suicide attempts, and mental health treatment
First, we estimated the prevalence of SI/SA at least once during the one year of observation (i.e., denominator=948 subjects) and the frequency of SI/SA across all assessments. Next, we calculated the prevalence of SI/SA across all observations within each wave (i.e., 4362 observations, broken up by wave). The same approach was followed to measure the prevalence of each specific type of mental health treatment (i.e., prescription drug, outpatient, emergency room, overnight at a hospital).
We used the longitudinal data to calculate (a) the extent to which SI/SA is preceded by SI/SA in prior assessments, and (b) the degree to which SI/SA predicts subsequent mental health treatment. For (a), we collapsed the data across waves and counted the number of times SI or SA was preceded by SI or SA at exactly 3-months prior. We divided this number by the total number of positive reports of SI/SA at waves 3, 6, 9, and 12. Reports from intake were excluded in this calculation because we did not have reports prior to intake. For (b), we estimated the share of suicide mentions that were followed exactly three months later with each of the four specific types of mental health treatment. For this calculation, we kept cases from intake but excluded cases from 12-months because we did not have subsequent mental health information on reports at the twelfth month of follow-up. Responses with missing values at time t or t-1 were excluded when deriving all the estimates above.
Characteristics associated with suicide ideation and attempts
To identify characteristics of youth likely to report SI/SA accounting for past SI/SA, we began with logistic regression models with lagged variables, whereby suicide ideation at time t was regressed on suicide ideation at time t-1 and, in a separate model, attempt at time t was regressed on both ideation and attempt at time t-1.
Next, we estimated what factors predicted SI/SA independent of the effects of past SI/SA. We extended our lagged models above to include sociodemographic terms (age, sex, and race/ethnicity), as well as indicators of treatment site and interview wave. From time t-1, we also included scales of conduct disorder symptoms, depression symptoms, and substance use disorder symptoms, along with a single indicator of any mental health treatment.
Finally, we were interested in whether there were differential effects by our covariates of interest among youth who did report suicide ideation at time t-1 and those who did not. To examine this question, we estimated additional multivariate regression models using a backward-type model selection technique to help inform our choice of the final adjusted model for SI/SA. Our final model included the main effects of past SI/SA, all three mental health symptoms, the indicator of past mental health treatment, race, sex, age, treatment site, and interview wave as well as interaction terms that existed between suicide ideation at time t-1 and the other variables in the model. If any one of the interaction terms between suicide ideation at time t-1 and our three mental health symptoms was found to be significant, all three were retained in the model. Interaction terms between sociodemographics were included in the model if the specific term was found to be significant. To account for correlation among observations of youth with repeated observations over time, we used a sandwich estimator to estimate standard errors. Any clustering specific to treatment sites is accounted for with the site of care fixed effects included in the model.
Characteristics associated with mental health treatment
The final stage of our analysis was to examine the characteristics of youth more or less likely to receive mental health care. Because emergency room care and overnight hospital care were relatively rare, but in general both indicated intense care, we collapsed these outcomes into one category. In general, we followed the strategy described above for our models of characteristics associated with SI/SA. Thus, first we included a lagged indicator of the specific outcome (e.g., prescription drug treatment at time t was regressed on prescription drug treatment at time t-1). Next, we estimated whether, independent of this effect, youth with either suicide ideation or attempts at time t-1 were more or less likely to receive the specific form of mental health care at time t. We then included symptoms of conduct disorder, depression, and substance use disorder at time t-1, as well as race/ethnicity, age, sex, interview wave, and site of care to see if any of these factors was associated with mental health treatment above and beyond treatment at time t-1 and SI/SA. Finally, we were interested in assessing whether there were differential effects of factors that predicted treatment at time t among youth who ideated at time t-1 and those who did not. We included interaction terms using the same model selection criteria as described above, and followed the same strategy for determining which product terms to include in the final model. As in the previous models, a sandwich estimator was used to estimate robust standard errors which controlled for correlation among observations of youth with repeated observations over time.
Results
Prevalence of suicide ideation, attempts, and follow-up mental health treatment
Among the 948 youth who entered into the study at baseline, 30% reported thinking about committing suicide during at least one of the five interview sessions and 12% reported attempting suicide at least once during that period (data not shown). Twenty-percent (n=189) of those who were interviewed at least once (n=948) reported SI at one of the five assessments. Of those interviewed at least twice (n=930), 7% (n=62) reported ideation twice. Continuing this strategy of accounting for the differential rates of follow-up, 2% reported SI three times, 1.5% reported SI four times, and approximately 1% of those interviewed at all five assessments reported thinking about committing suicide all five times they were asked. With respect to suicide attempts, 11% (n=100) reported SA at one of the assessments, 1% reported SA twice, 4 youth reported SA three times, 1 reported attempting suicide four times, and no young person reported attempting at all five assessments.
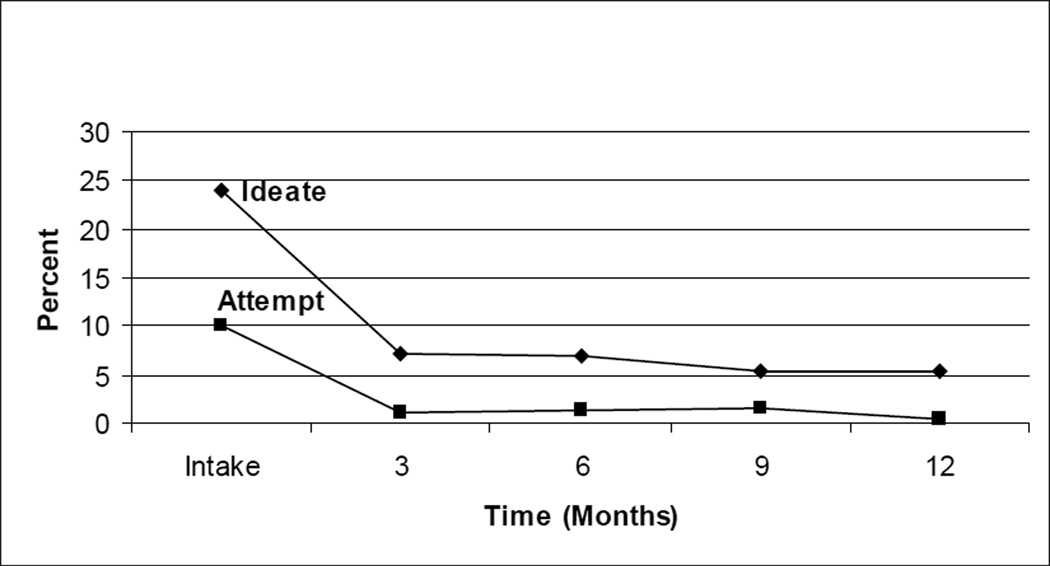
Figure 1 presents descriptive statistics regarding SI/SA among the youth in the sample over time. As would be expected, both suicide ideation and attempts had the highest prevalence at baseline, when the questions referred to the past year, versus the follow-up assessments when the questions referenced the past 90 days. That is to say, at the follow-up assessments, a little over 5% of responding youth reported ideating across the waves, and two-percent or fewer reported a prior attempt.
Figure 1.
Suicide Ideation and Attempts, by Wave
* Questions at intake reference the past year; at follow-up questions reference the past 90 days
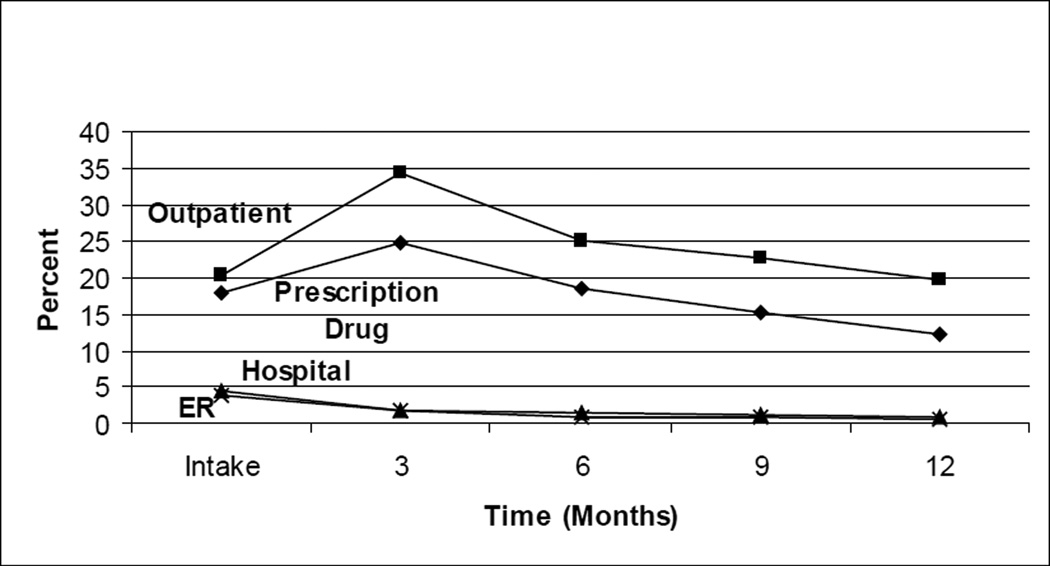
Almost half of the youth reported receiving outpatient treatment at least once; one-third reported being on prescription drugs for an emotional or behavioral problem and 8% and 7% respectively reported, at least once, staying in the hospital overnight or going to the emergency room for an emotional or behavioral problem (data not shown). The prevalence of mental health treatment across waves is presented in Figure 2. Across waves, we see that prescription drug and outpatient treatment became more prevalent between intake and 3-months later. However, rates of mental health treatment of these types declined over the remainder of the study. Rates of overnight hospital and emergency room care also decreased over the course of the study, declining from 4% at intake to 1% at 12-months.
Figure 2.
Mental Health Treatment, by Wave
* Questions at intake reference the past year; at follow-up questions reference the past 90 days
Table 2 presents information on the proportion of SI/SA preceded by prior SI/SA. Excluding reports at intake, there were 214 mentions of ideation and 40 reports of a suicide attempt. Sixty percent of attempts (n=24) were preceded by an ideation report three-months earlier and 27.5% of non-fatal attempts were preceded by a similar attempt three-months prior. Table 2 also presents the proportion of SI/SA followed by each of the specific types of mental health treatment. Excluding reports at 12-months, there were 397 ideations and 132 attempts. Among youth who ideated, close to half received some type of outpatient treatment between when they reported ideating and 3-months later, over one-third received prescription drug treatment, and 6% reported receiving care for emotional or behavioral problems in the emergency room or overnight at a hospital. Mental health treatment was more prevalent among youth who reported a non-fatal attempt. Close to one-half reported receiving subsequent outpatient treatment and a similar proportion reported that they were on prescription drug treatment 3-months later. Approximately 7% of persons who reported a suicide attempt reported going to the emergency room or spending at least one night in a hospital for an emotional or behavioral problem between when they reported attempting and the next assessment 3-months later.
Table 2.
Longitudinal Associations between SI/SA and Mental Health Treatment
| Time t* | ||||
|---|---|---|---|---|
| Ideation |
Attempt |
|||
| n | Col % | n | Col % | |
|
Total (excluding reports at intake) Time t-1* |
214 | 100 | 40 | 100 |
| Ideation | 107 | 50.0 | 24 | 60.0 |
| Attempt | 36 | 16.8 | 11 | 27.5 |
|
Ideation |
Attempt |
|||
| n | Col % | n | Col % | |
|
Total (excluding reports at 12 months) Mental Health Treatment at time t+1 |
397 | 100 | 132 | 100 |
| Prescription Drug | 149 | 37.5 | 63 | 47.7 |
| Outpatient | 189 | 47.6 | 65 | 49.2 |
| Emergency Room | 24 | 6.0 | 9 | 6.8 |
| Hospital | 23 | 5.8 | 9 | 6.8 |
By definition, all youth who report suicide attempts also have positive values for ideation
Characteristics associated with suicide ideation and attempts
The results from the regression models for both suicide ideation and attempts are presented in Table 3. First, for both suicide ideation and attempts, our tests for differential effects among suicide ideators yielded no effects (e.g. there were no significant interactions with the indicator of ideating at time t-1). Thus, by including the lagged outcome variable in the model, the regression coefficients represent the change in the likelihood that someone ideated or attempted at time t for both those who ideated at time t-1 and those who did not. Past suicide ideation was the factor most strongly associated with subsequent ideation (adjusted odds ratio (aOR)=7.11, 95 % confidence interval (CI) =4.73, 10.72). Higher levels of conduct disorder and depression at time t-1 each positively predicted subsequent ideation at time t. In addition, youth who reported receiving any type of mental health treatment at time t-1 were more likely to report ideation at time t, as were females. Black youth in substance abuse treatment were less likely than their white counterparts to report ideation.
Table 3.
Multivariate Logistic Regression: Predictors of Suicide Ideation and Attempts
| Ideation (t) | Attempt (t) | |||
|---|---|---|---|---|
| Total Effect Among All Youth |
Total Effect Among All Youth |
|||
| aOR | 95% CI | aOR | 95% CI | |
| Time t-1 | ||||
| Ideate | 7.11 | (4.73, 10.72) | 8.55 | (3.62, 20.17) |
| Attempt | N/A | N/A | 2.13 | (0.72, 6.27) |
| Mental Health Problems | ||||
| Conduct Disorder | 1.09 | (1.03, 1.15) | 1.23 | (1.10, 1.38) |
| Depression | 1.22 | (1.10, 1.36) | 0.87 | (0.67, 1.14) |
| Substance Use Disorder | 0.98 | (0.92, 1.04) | 0.95 | (0.81, 1.11) |
| Age | 1.12 | (0.96, 1.31) | 1.25 | (0.86, 1.84) |
| Any Mental Health Treatment | 1.80 | (1.32, 2.46) | 5.27 | (2.17, 12.80) |
| Constant | ||||
| Sex | ||||
| Male (Reference) | ||||
| Female | 1.40 | (1.00, 1.97) | 1.40 | (0.61, 3.20) |
| Race | ||||
| White (Reference) | ||||
| American Indian | 1.42 | (0.64, 3.17) | 0.95 | (0.14, 6.70) |
| Black | 0.24 | (0.08, 0.73) | -- | -- |
| Hispanic | 1.06 | (0.64, 1.75) | 0.87 | (0.22, 3.39) |
| Other | 1.06 | (0.71, 1.58) | 1.19 | (0.51, 2.81) |
Multivariate analyses adjusted for treatment site and interview wave.
aOR=adjusted odds ratio
With respect to suicide attempts, ideation at time t-1 was linked with subsequent attempts (aOR=8.55, 95% CI=3.62, 20.17). However, attempting suicide at t-1 was not associated with attempts conditional on prior ideation and other risk factors. Independent of past suicide ideation and attempts, youth with high levels of conduct disorder were more likely to report attempting suicide, as were youth who reported receiving some kind of mental health treatment at time t-1. There were no noticeable race differences, yet we note that only three Black youth reported a suicide attempt, which impeded estimates for this term.
Characteristics associated with mental health treatment
The results from the regression models of our mental health treatment outcomes are shown in Table 4. As expected, treatment at time t-1 for each of the outcomes was the variable most strongly linked with treatment at time t. With respect to prescription drug treatment, neither suicide ideation nor attempts at time t-1 were linked to prescription drug treatment at time t. Regardless of their prescription drug treatment at t-1, older youth were less likely to receive prescription drug treatment at time t. Black and Hispanic youth were also less likely to receive prescription drug treatment relative to their white counterparts. Although SI/SA at time t-1 was not linked with prescription drug treatment at time t, there was evidence of a differential effect among ideators with respect to mental health symptoms. Among youth who did not ideate at time t-1, higher levels of depressive symptoms and substance use problems were positively associated with prescription drug treatment; there was no significant association between conduct disorder symptoms and prescription drug treatment among this group (aOR=1.01, 95% CI=0.96, 1.06). Among youth who did ideate at time t-1, those with higher levels of depression and substance use problems were also more likely to receive prescription drug treatment at time t. However, among ideators, those with higher levels of conduct disorder were less likely to receive subsequent prescription drug treatment (total effect for ideators at t-1: aOR=0.92, 95% CI=0.85, 1.00).
Table 4.
Multivariate Logistic Regression: Predictors of Mental Health Treatment
| Prescription Drug* | Outpatient* | Hospital/Emergency** | ||||
|---|---|---|---|---|---|---|
| Main Effects |
Main Effects |
Main Effects |
||||
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | |
| Time t-1 | ||||||
| Ideate | 0.87 | (0.26, 2.95) | 4.31 | (1.46, 12.76) | 3.60 | (1.33, 9.75) |
| Attempt | 1.65 | (0.91, 3.00) | 0.90 | (0.53, 1.53) | 0.79 | (0.35, 1.81) |
| Mental Health | ||||||
| Problems | ||||||
| Conduct | 1.01 | (0.96, 1.06) | 1.01 | (0.97, 1.05) | 1.07 | (0.97, 1.19) |
| Disorder | ||||||
| Depression | 1.13 | (1.04, 1.22) | 1.12 | (1.05, 1.20) | 0.99 | (0.82, 1.18) |
| Substance Use | 1.05 | (1.00, 1.10) | 1.08 | (1.04, 1.12) | 1.05 | (0.96, 1.16) |
| Disorder | ||||||
| Prescription Drug | 33.83 | (24.79, 46.15) | -- | --- | -- | --- |
| Treatment | ||||||
| Outpatient | -- | --- | 6.95 | (5.24, 8.77) | -- | --- |
| Treatment | ||||||
| Emergency/ Hospital Care |
-- | --- | -- | --- | 4.11 | (2.03, 8.36) |
| Age | 0.82 | (0.74, 0.91) | 0.85 | (0.78. 0.93) | 0.82 | (0.66, 1.02) |
| Constant | ||||||
| Sex | ||||||
| Male (Ref) | ||||||
| Female | 1.19 | (0.92, 1.55) | 1.19 | (0.94, 1.49) | 1.92 | (1.04, 3.54) |
| Race | ||||||
| White (Ref) | ||||||
| American Indian | 0.91 | (0.45, 1.83) | 0.98 | (0.54, 1.77) | -- | --- |
| Black | 0.42 | (0.23, 0.76) | 0.87 | (0.62, 1.24) | 0.29 | (0.04, 2.01) |
| Hispanic | 0.62 | (0.39, 0.97) | 0.77 | (0.53, 1.12) | 0.26 | (0.03, 2.01) |
| Other | 0.96 | (0.71, 1.30) | 1.15 | (0.87, 1.53) | 0.51 | (0.15, 1.70) |
|
Differential Effects for Ideators at t-1 |
Differential Effects for Ideators at t-1 |
Differential Effects for Ideators at t-1 |
||||
| Conduct Disorder | 0.92 | (0.85, 1.00) | 0.96 | ((0.90, 1.02) | -- | --- |
| Depression | 1.26 | (1.04, 1.53) | 1.14 | (0.94, 1.39) | -- | --- |
| Substance Use | 1.16 | (1.05, 1.29) | 1.02 | (0.93, 1.12) | -- | --- |
| Disorder | ||||||
| Prescription Drug | 7.31 | (4.13, 12.94) | -- | --- | -- | --- |
| Treatment | ||||||
| Outpatient | -- | --- | 6.95 | (5.24, 8.77) | -- | --- |
| Treatment | ||||||
| Hispanic | -- | --- | -- | --- | 1.13 | (0.26, 4.86) |
| Other | -- | --- | -- | --- | 3.45 | (1.44, 8.26) |
Multivariate analyses adjusted for treatment site and interview wave
aOR=adjusted odds ratio
For outpatient care, we see that ideation at time t-1 predicts receipt of outpatient treatment at time t independent of the lagged effect of outpatient care. In addition to this finding, we see similar trends as we did for prescription drug treatment. Older youth were again less likely to receive outpatient care and, among non-ideators, higher levels of depressive and substance use disorder symptoms were linked with this type of care. There was also evidence of a differential effect, however, unlike prescription drug care, among youth who ideated at time t-1, mental health symptoms did not differentially predict the likelihood of receiving subsequent outpatient care.
Finally, ideating at time t-1 and being female were the only factors linked with receiving hospital or emergency room care at time t. However, there was again evidence of a differential effect among ideators for this outcome with respect to the effects of race. Noticeably, compared to white ideators, ideators whose race/ethnicity was categorized as “other” were more likely to receive subsequent care in an emergency room or overnight at a hospital (total effect for ideators at t-1: aOR=3.45, 95% CI=1.44, 8.26).
Discussion
The results from this study reveal that over the course of two years (one year pre-intake and one year post-intake), close to one third of this sample of youth in adolescent substance abuse treatment facilities reported thinking about committing suicide and over ten percent reported having tried to kill themselves. At intake, 24% of youth reported having thought about suicide and 10% reported having attempted suicide in the past year. These estimates are only slightly higher than those generated from school-attending youth across the United States in the same year, in which the estimated prevalence of ideation was 21% and attempts was 8% (Kann et al., 1998). Among the youth in substance abuse treatment, SI and SA were also high at follow-up: almost half of all reports of ideation over the period of observation and one quarter of attempts occurred post-treatment entry. The majority of these reports were preceded by some mention of suicidal risk in the past, with a particularly strong link between suicide ideation at one time point and either suicide ideation or attempts at the next assessment. Collectively, these results stress that youth who report SI/SA in substance abuse treatment should be targeted for specific suicide prevention, and that this prevention should begin as soon as they enter treatment.
With respect to psychopathology, conduct disorder emerged as a significant predictor of suicide ideation and attempts among youth in substance abuse treatment. Even after controlling for prior SI/SA, youth with higher levels of conduct disorder were more likely to both have incident ideations and attempts within the three month intervals, potentially signaling impulsive suicide attempts. Without mention of a prior suicide to gear youth toward special suicide interventions, clients with high levels of conduct disorder symptoms within substance abuse treatment should be, at the very least, closely monitored for self-harm behaviors. The result was very different for depressive symptoms which only predicted subsequent ideation but not subsequent attempts. Given that our sample is close to three-quarters male at intake, these findings are consistent with prior research that indicates gender differences in the psychopathology of young suicide attempters as well as suicide cases: aggressive and antisocial behaviors are strong predictors of suicide for boys, while depressive symptoms are stronger predictors of suicide among girls (Gould et al., 1998; Lewinsohn, Rohde, Seeley, & Baldwin, 2001; Marttunen et al., 1995; Shaffer et al., 1996). Finally, substance problem severity was not related to SI/SA after controlling for other covariates. Although treatment guidelines indicate that the presence of a substance use disorder should mark the “seriousness” of a young person’s suicidal intent (American Academy of Child and Adolescent Psychiatry, 2001), by definition, most youth in the sample have high levels of substance use problems which limits the utility of this indicator in substance abuse treatment settings.
In general, specialized mental health treatment among adolescents in substance abuse treatment is relatively low, even though youth in these programs have high levels of mental health problems (Jaycox et al., 2003). However, it does appear that youth who report ideating are more likely than youth who do not report such behavior to receive certain types of treatment. Independent of common internalizing (e.g., depressive) and externalizing (e.g., conduct disorder) symptoms, youth who report thinking about suicide are more likely than youth who do not to receive outpatient mental health care even if they were not already receiving outpatient care, with approximately half of all SI/SA followed-up with at least one outpatient mental health care visit. Ideators are also more likely than those who do not report ideating to receive mental health care at the hospital and emergency departments. These findings may represent that policies exist within adolescent substance abuse treatment centers, whereby providers triage youth with more serious suicidal tendencies to hospitals and emergency departments while less serious cases receive outpatient care. However, even with these closely spaced intervals, temporality is impossible to discern. Thus, higher levels of hospitalization and emergency department visits among ideators may indicate subsequent suicide attempts or other illness or injury that resulted in an emergency department visit and/or hospitalization. Youth with high levels of conduct disorder were also less likely to report being on prescription drug treatment, even among youth with a history of suicide ideation, though these results do not necessarily reflect inadequate care. Although selective serotonin reuptake inhibitors reduce the frequency of impulsive and aggressive behaviors in adults (Coccaro & Kavoussi, 1997), there is the possibility that youth with high levels of conduct disorder symptoms will not properly adhere to these medications. Also, there exists the possibility that these medications may harm youth, particularly by increasing the risk of ruminative suicide ideation (Hammad et al., 2006).
Finally, there appear to be some racial differences in the mental health services that both non-ideators and ideators receive. After controlling for ideation, psychopathology, and past mental health care, Black and Hispanic youth were less likely to report receiving prescription drug treatment for emotional and behavioral problems. This is consistent with recent studies that have documented disparities in prescription drug use for mental illnesses among the general U.S. population (Han & Liu, 2005) and in disparities in access to mental health services among youth with drug and alcohol problems (Garland et al., 2005). As of 2002, Black and Hispanic youth made up 20% and 15%, respectively, of admissions among young people admitted to substance abuse treatment facilities in the U.S. (Office of Applied Studies, 2004). Efforts should be made to ensure equitable access to treatment among these groups, and future research should focus on the causes for the observed disparities which may include differences in access to care and insurance coverage, cultural barriers and racial differences in familiarity with mental health treatment, or bias held by practitioners and administrators against minority groups (Snowden, 2003).
These findings should be considered with respect to certain limitations of the current study. The primary of these is that we do not have mortality data, including completed suicide, on youth who participated in the ATM study. There is evidence that youth with a history of suicide ideation and attempts are more likely than youth without such histories to go on to die from suicide (Shaffer et al., 1996), but most individuals who make a non-fatal suicide attempt do not go on to die this way (Spirito & Esposito-Smythers, 2006). However, youth who die by suicide may “practice up” to killing themselves, and that non-fatal attempts enhance fearlessness and competence which can help facilitate completed suicide (Joiner et al., 2005; Stellrecht et al., 2006). Thus, there are reasons for treating non-fatal attempts and ideation seriously and resources and protocols should be developed for dealing with these symptoms in substance abuse treatment settings.
We assume in this study that the survey questions asked of respondents reflect the same information that clients in substance abuse treatment tell their treatment providers, though it is impossible with the current data to discern concordance between these measures. In addition, detailed information was not available about the types of mental health services offered (for example, the types of drugs prescribed, compliance to these medications, the duration of a hospital/ER stay, or type of outpatient care offered) or whether or not youth were still in treatment for their substance use disorders at the follow-ups; these are areas for future research.
While longitudinal studies permit inferences above and beyond what one could infer from cross-sectional designs, attrition of the study sample can bias results. Although consistent with other studies, the loss of Black respondents at 3 months may have biased our results about prescription drug treatment if Black youth lost to follow-up were more likely to be receiving prescription drugs than those who remained in the study; loss of respondents from one treatment site may have similarly biased results. Additionally, the relatively low number of suicide attempts at each wave may result in a lack of power to detect anything but large effect sizes of previous attempts on future attempts.
Notwithstanding these limitations, the findings of this study highlight the high prevalence of suicide ideation and attempts among youth in substance abuse treatment. Interventions to combat suicide have shown success in reducing suicide ideation and attempts and are considered most effective among young people with prior ideation and attempts (Donaldson, Spirito, & Esposito-Smythers, 2005; Gould, Greenberg, Velting, & Shaffer, 2003; Harrington et al., 1998; Rudd et al., 1996; Wingate, Van Orden, Joiner, Williams, & Rudd, 2005). Unfortunately, such interventions have not often been tested on young people with substance use problems. The reason is two-fold. First, studies of interventions targeting suicide often exclude patients with substance use disorders. Conversely, interventions targeting substance use either exclude suicidal youth or do not measure suicide-related outcomes (Esposito-Smythers & Spirito, 2004). We believe that targeted interventions focusing on preventing suicide specific to youth in substance abuse programs are warranted and that increasing attention should be given to preventing suicide ideation and attempts among youth in these settings.
Footnotes
This site had a total of 53 respondents at intake, and rates of follow-up were 88% (n=47) at 3-months, 81% (n=43) at 6-months, 64% (n=34) at 9-months, and 64% (n=34) at 12-months. Excluding this site from the analysis resulted in no appreciable differences from results presented here.
References
- American Academy of Child and Adolescent Psychiatry. Practice parameter for the assessment and treatment of children and adolescents with suicidal behavior American Academy of Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychiatry1t. 2001;40(7 Suppl) doi: 10.1097/00004583-200107001-00003. 24S–51S. [DOI] [PubMed] [Google Scholar]
- Berman AL, Schwartz RH. Suicide attempts among adolescent drug users. Am J Dis Child. 1990;144(3):310–314. doi: 10.1001/archpedi.1990.02150270060026. [DOI] [PubMed] [Google Scholar]
- Blader JC, Kafantaris V. Pharmacological treatment of bipolar disorder among children and adolescents. Expert Rev Neurother. 2007;7(3):259–270. doi: 10.1586/14737175.7.3.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borowsky IW, Ireland M, Resnick MD. Adolescent suicide attempts: risks and protectors. Pediatrics. 2001;107(3):485–493. doi: 10.1542/peds.107.3.485. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Goldstein CE, Kolko DJ, Allan MJ, Allman CJ, et al. Risk factors for adolescent suicide. A comparison of adolescent suicide victims with suicidal inpatients. Arch Gen Psychiatry. 1988;45(6):581–588. doi: 10.1001/archpsyc.1988.01800300079011. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, Allman C, Friend A, Roth C, et al. Psychiatric risk factors for adolescent suicide: a case-control study. J Am Acad Child Adolesc Psychiatry. 1993;32(3):521–529. doi: 10.1097/00004583-199305000-00006. [DOI] [PubMed] [Google Scholar]
- Cavaiola AA, Lavender N. Suicidal behavior in chemically dependent adolescents. Adolescence. 1999;34(136):735–744. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, N. C. f. I. P. a. C. p. Web-based Injury Statistics Query and Reporting System (WISQARS) [Online] 2007 Retrieved June 4, 2007, from http://www.cdc.gov/ncipc/wisqars/default.htm.
- Coccaro EF, Kavoussi RJ. Fluoxetine and impulsive aggressive behavior in personality-disordered subjects. Arch Gen Psychiatry. 1997;54(12):1081–1088. doi: 10.1001/archpsyc.1997.01830240035005. [DOI] [PubMed] [Google Scholar]
- CSAT GPRA Client Outcome Measures for Discretionary Programs. 2007 Retrieved June 6, 2007, from https://www.samhsa-gpra.samhsa.gov/home/index.htm.
- Dennis M, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, et al. The Cannabis Youth Treatment (CYT) Study: main findings from two randomized trials. J Subst Abuse Treat. 2004;27(3):197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Dennis M, Titus JC, Diamond G, Donaldson J, Godley SH, Tims FM, et al. The Cannabis Youth Treatment (CYT) experiment: rationale, study design and analysis plans. Addiction. 2002;97(Suppl 1):16–34. doi: 10.1046/j.1360-0443.97.s01.2.x. [DOI] [PubMed] [Google Scholar]
- Dennis ML. Global Appraisal of Individual Needs (GAIN): Administration guide for the GAIN and related measures (Version 1299) Bloomington, IL: Lighthouse Publications; 1999. [Google Scholar]
- Dennis ML, Dawud-Noursi S, Muck RD, McDermeit M. The need for developing and evaluating adolescent treatment models. In: Stevens SJ, Morral AR, editors. Adolescent Substance Abuse Treatment in the United States: Exemplary Models from a National Evaluation Study. New York: Haworth Press; 2003. pp. 3–34. [Google Scholar]
- Dennis ML, Ives M, Funk R. GAIN-I encyclopedia of supplemental documentation on scales and other calculated variables [Electronic version] 2007 Retrieved February 19, 2008, from http://www.chestnut.org/LI/gain/Scales_Crosswalks/GI_Scales_and_Variables.xls.
- Deykin EY, Buka SL. Suicidal ideation and attempts among chemically dependent adolescents. Am J Public Health. 1994;84(4):634–639. doi: 10.2105/ajph.84.4.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson D, Spirito A, Esposito-Smythers C. Treatment for adolescents following a suicide attempt: results of a pilot trial. J Am Acad Child Adolesc Psychiatry. 2005;44(2):113–120. doi: 10.1097/00004583-200502000-00003. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Ross J, Hawkins J, Harris WA, et al. Youth risk behavior surveillance--United States, 2005. MMWR Surveill Summ. 2006;55(5):1–108. [PubMed] [Google Scholar]
- Esposito-Smythers C, Spirito A. Adolescent substance use and suicidal behavior: a review with implications for treatment research. Alcohol Clin Exp Res. 2004;28(5 Suppl):77S–88S. doi: 10.1097/01.alc.0000127417.99752.87. [DOI] [PubMed] [Google Scholar]
- Fowler RC, Rich CL, Young D. San Diego Suicide Study. II. Substance abuse in young cases. Arch Gen Psychiatry. 1986;43(10):962–965. doi: 10.1001/archpsyc.1986.01800100056008. [DOI] [PubMed] [Google Scholar]
- Garland AF, Lau AS, Yeh M, McCabe KM, Hough RL, Landsverk JA. Racial and ethnic differences in utilization of mental health services among high-risk youths. Am J Psychiatry. 2005;162(7):1336–1343. doi: 10.1176/appi.ajp.162.7.1336. [DOI] [PubMed] [Google Scholar]
- Garrison CZ, McKeown RE, Valois RF, Vincent ML. Aggression, substance use, and suicidal behaviors in high school students. Am J Public Health. 1993;83(2):179–184. doi: 10.2105/ajph.83.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42(4):386–405. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- Gould MS, King R, Greenwald S, Fisher P, Schwab-Stone M, Kramer R, et al. Psychopathology associated with suicidal ideation and attempts among children and adolescents. J Am Acad Child Adolesc Psychiatry. 1998;37(9):915–923. doi: 10.1097/00004583-199809000-00011. [DOI] [PubMed] [Google Scholar]
- Grella CE, Hser YI, Joshi V, Rounds-Bryant J. Drug treatment outcomes for adolescents with comorbid mental and substance use disorders. J Nerv Ment Dis. 2001;189(6):384–392. doi: 10.1097/00005053-200106000-00006. [DOI] [PubMed] [Google Scholar]
- Hammad TA, Laughren T, Racoosin J. Suicidality in pediatric patients treated with antidepressant drugs. Arch Gen Psychiatry. 2006;63(3):332–339. doi: 10.1001/archpsyc.63.3.332. [DOI] [PubMed] [Google Scholar]
- Han E, Liu GG. Racial disparities in prescription drug use for mental illness among population in US. J Ment Health Policy Econ. 2005;8(3):131–143. [PubMed] [Google Scholar]
- Harrington R, Kerfoot M, Dyer E, McNiven F, Gill J, Harrington V, et al. Randomized trial of a home-based family intervention for children who have deliberately poisoned themselves. J Am Acad Child Adolesc Psychiatry. 1998;37(5):512–518. [PubMed] [Google Scholar]
- Hirschfeld RMA, Davidson L. Risk factors for suicide. In: Frances AJ, Hales RE, editors. American Psychiatric Press review of psychiatry. Vol. 7. Washington, DC: American Psychiatric Press; 1988. pp. 307–333. [Google Scholar]
- Jainchill N. Therapeutic communities for adolescents: The same and not the same. In: De Leon G, editor. Community as Method: Therapeutic Communities for Special Populations and Special Settings. Westport, CT: Praeger; 1997. pp. 161–177. [Google Scholar]
- Jaycox LH, Morral AR, Juvonen J. Mental health and medical problems and service use among adolescent substance users. J Am Acad Child Adolesc Psychiatry. 2003;42(6):701–709. doi: 10.1097/01.CHI.0000046846.56865.F9. [DOI] [PubMed] [Google Scholar]
- Jessor R. Risk behavior in adolescence: a psychosocial framework for understanding and action. J Adolesc Health. 1991;12(8):597–605. doi: 10.1016/1054-139x(91)90007-k. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jr, Conwell Y, Fitzpatrick KK, Witte TK, Schmidt NB, Berlim MT, et al. Four studies on how past and current suicidality relate even when “everything but the kitchen sink” is covaried. J Abnorm Psychol. 2005;114(2):291–303. doi: 10.1037/0021-843X.114.2.291. [DOI] [PubMed] [Google Scholar]
- Kann L, Kinchen SA, Williams BI, Ross JG, Lowry R, Hill CV, et al. Youth risk behavior surveillance--United States, 1997. MMWR CDC Surveill Summ. 1998;47(3):1–89. [PubMed] [Google Scholar]
- Kennedy SP, Baraff LJ, Suddath RL, Asarnow JR. Emergency department management of suicidal adolescents. Ann Emerg Med. 2004;43(4):452–460. doi: 10.1016/j.annemergmed.2003.09.009. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Baldwin CL. Gender differences in suicide attempts from adolescence to young adulthood. J Am Acad Child Adolesc Psychiatry. 2001;40(4):427–434. doi: 10.1097/00004583-200104000-00011. [DOI] [PubMed] [Google Scholar]
- Marttunen MJ, Henriksson MM, Aro HM, Heikkinen ME, Isometsa ET, Lonnqvist JK. Suicide among female adolescents: characteristics and comparison with males in the age group 13 to 22 years. J Am Acad Child Adolesc Psychiatry. 1995;34(10):1297–1307. doi: 10.1097/00004583-199510000-00015. [DOI] [PubMed] [Google Scholar]
- The New DAWN Report: Disposition of Emergency Department Visits for Drug-Related Suicide Attempts by Adolescents: 2004. Rockville, Maryland: Office of Applied Studies, Substance Abuse and Mental Health Services Administration; 2006. [Google Scholar]
- Rich CL, Sherman M, Fowler RC. San Diego Suicide Study: the adolescents. Adolescence. 1990;25(100):855–865. [PubMed] [Google Scholar]
- Rudd MD, Rajab MH, Orman DT, Joiner T, Stulman DA, Dixon W. Effectiveness of an outpatient intervention targeting suicidal young adults: preliminary results. J Consult Clin Psychol. 1996;64(1):179–190. doi: 10.1037//0022-006x.64.1.179. [DOI] [PubMed] [Google Scholar]
- Runeson B. Psychoactive substance use disorder in youth suicide. Alcohol Alcohol. 1990;25(5):561–568. [PubMed] [Google Scholar]
- Shaffer D. Epidemiological aspects of some problems in child and adolescent psychiatry. Epidemiol Psichiatr Soc. 1998;7(3):151–155. doi: 10.1017/s1121189x00007326. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Fisher P, Trautman P, Moreau D, Kleinman M, et al. Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry. 1996;53(4):339–348. doi: 10.1001/archpsyc.1996.01830040075012. [DOI] [PubMed] [Google Scholar]
- Snowden LR. Bias in mental health assessment and intervention: theory and evidence. Am J Public Health. 2003;93(2):239–243. doi: 10.2105/ajph.93.2.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spirito A, Esposito-Smythers C. Attempted and completed suicide in adolescence. Annu Rev Clin Psychol. 2006;2:237–266. doi: 10.1146/annurev.clinpsy.2.022305.095323. [DOI] [PubMed] [Google Scholar]
- Stellrecht NE, Gordon KH, Van Orden K, Witte TK, Wingate LR, Cukrowicz KC, et al. Clinical applications of the interpersonal-psychological theory of attempted and completed suicide. J Clin Psychol. 2006;62(2):211–222. doi: 10.1002/jclp.20224. [DOI] [PubMed] [Google Scholar]
- Stevens SJ, Morral ARe. Adolescent Substance Abuse Treatment in the United States: Exemplary Models from a National Evaluation Study. New York: Haworth Press; 2003. [Google Scholar]
- Stowell RJ, Estroff TW. Psychiatric disorders in substance-abusing adolescent inpatients: a pilot study. J Am Acad Child Adolesc Psychiatry. 1992;31(6):1036–1040. doi: 10.1097/00004583-199211000-00006. [DOI] [PubMed] [Google Scholar]
- Wilcox HC, Anthony JC. The development of suicide ideation and attempts: an epidemiologic study of first graders followed into young adulthood. Drug Alcohol Depend. 2004;(76 Suppl):S53–S67. doi: 10.1016/j.drugalcdep.2004.08.007. [DOI] [PubMed] [Google Scholar]
- Wingate LR, Van Orden KA, Joiner TE, Jr, Williams FM, Rudd MD. Comparison of compensation and capitalization models when treating suicidality in young adults. J Consult Clin Psychol. 2005;73(4):756–762. doi: 10.1037/0022-006X.73.4.756. [DOI] [PubMed] [Google Scholar]