Surgical treatment of type II odontoid fracture in this elderly population did not negatively impact survival, even after adjusting for age, sex, and comorbidities. The data suggest that there is a 30-day survival advantage and a trend toward improved longer-term survival for operatively treated over nonoperatively treated patients.
Keywords: odontoid fracture, elderly, geriatric, surgery, conservative care, outcomes, mortality
Abstract
Study Design.
Retrospective, multicenter cohort study.
Objective.
Assess for differences in short- and long-term mortality between operative and nonoperative treatment for elderly patients with type II odontoid fractures.
Summary of Background Data.
There is controversy regarding whether operative or nonoperative management is the best treatment for elderly patients with type II odontoid fractures.
Methods.
This is a retrospective study of consecutive patients aged 65 years or older with type II odontoid fracture from 3 level I trauma centers from 2003–2009. Demographics, comorbidities, and treatment were abstracted from medical records. Mortality outcomes were obtained from medical records and a public database. Hazard ratios (HRs) and 95% confidence intervals (CI) were calculated.
Results.
A total of 322 patients were included (mean age, 81.8 yr; range, 65.0–101.5 yr). Compared with patients treated nonoperatively (n = 157), patients treated operatively (n = 165) were slightly younger (80.4 vs. 83.2 yr, P = 0.0014), had a longer hospital (15.0 vs. 7.4 d, P < 0.001) and intensive care unit (1.5 vs. 1.1 d, P = 0.008) stay, and were more likely to receive a feeding tube (18% vs. 5%, P = 0.0003). Operative and nonoperative treatment groups had similar sex distribution (P = 0.94) and Charlson comorbidity index (P = 0.11). Within 30 days of presentation, 14% of patients died, and at maximal follow-up (average = 2.05 yr; range = 0 d–7.02 yr), 44% had died. On multivariate analysis, nonoperative treatment was associated with higher 30-day mortality (HR = 3.00, 95% CI = 1.51–5.94, P = 0.0017), after adjusting for age (HR = 1.10, 95% CI = 1.05–1.14; P < 0.0001), male sex (P = 0.69), and Charlson comorbidity index (P = 0.16). At maximal follow-up, there was a trend toward higher mortality associated with nonoperative treatment (HR = 1.35, 95% CI = 0.97–1.89, P = 0.079), after adjusting for age (HR = 1.07, 95% CI = 1.05–1.10; P < 0.0001), male sex (HR = 1.55, 95% CI = 1.10–2.16; P = 0.012), and Charlson comorbidity index (HR = 1.28, 95% CI = 1.16–1.40; P < 0.0001).
Conclusion.
Surgical treatment of type II odontoid fracture in this elderly population did not negatively impact survival, even after adjusting for age, sex, and comorbidities. The data suggest a significant 30-day survival advantage and a trend toward improved longer-term survival for operatively treated over nonoperatively treated patients.
Level of Evidence: 4
The high incidence of spine fractures in the elderly, coupled with the rapid expansion of this segment of the population in the United States, prompted the recent description of spine fractures in the geriatric population as a serious emerging health care crisis.1 The population of the United States older than 65 years is expected to double to more than 70 million between the years 2000 and 2030,2 and the population older than 85 years is the fastest growing age group, expected to double by 2025 and quintuple by 2050.1,3
Odontoid fractures are among the most common spine fractures in general, but in the elderly, these injuries are the most common isolated spine fracture.4,5 A majority of these are classified as type II fractures on the basis of the classification by Anderson and D'Alonzo.6 A recent report has demonstrated that the number and frequency of type II odontoid fractures, in comparison with other spine injuries, seems to be increasing during the past 2 decades and may correlate with the increasing elderly population.7
There is controversy regarding whether operative or nonoperative management is the best treatment option for elderly patients with type II odontoid fractures.8–12 Type II fractures by definition occur through the base of the dens, which in comparison with the body of the C2 vertebra, has a less robust blood supply and bone quality, and together with its high-strain location renders this fracture more vulnerable to nonunion.13 This risk of nonunion seems to be particularly high in the elderly, in which the rate of pseudarthrosis has been reported to be as high as 85% with nonoperative management.14 In contrast, fusion rates of up to 100% have been reported with posterior C1–C2 instrumentation.15 However, surgical treatment in these often medically compromised patients is also associated with adverse outcomes, with a recent report documenting a mortality rate of 19.2% and major complication rate of 27% in an operatively treated cohort of elderly patients with type II odontoid fractures.16
Adding to the controversy of management of type II odontoid fractures has been uncertainty regarding the clinical significance of chronic fracture nonunion. Reports from Crockard et al17 and Kirankumar et al18 had raised the concern of delayed myelopathy in the setting of nonunion. However, a case series by Hart et al19 suggested that development of delayed myelopathy in the setting of pseudarthrosis of type II odontoid fracture in the elderly to be a rare event. A subsequent report further endorsed a lack of correlation between fracture healing and clinical outcomes.11 Thus, the optimal management of elderly patients with type II odontoid fractures remains controversial, with advocates of both operative and nonoperative approaches.20,21
Our objectives in this study were to evaluate short- and long-term mortality in geriatric patients with type II odontoid fracture and to assess whether these mortality rates differed significantly based on operative versus nonsurgical treatment approach.
MATERIALS AND METHODS
Patient Population
Prospectively collected electronic spine trauma databases from 3 large level I trauma centers were used to identify consecutive patients 65 years or older treated for type II odontoid fractures between the years 2003 and 2009. These centers are all members of the AOSpine North America Research Network and included (Harborview Hospital at the University of Washington, Thomas Jefferson University Medical Center, and University of Kansas Medical Center). Although there may be patients who present on a delayed basis in the outpatient clinical setting, this study only included patients who were initially evaluated in the emergency room setting and admitted to the hospital. The medical records of the 322 identified patients were reviewed. This study was approved by the institutional review boards of the participating institutions and the institutional review board of the Data Management Center at (University of Washington).
Data Collection
Admission, hospital, and clinical follow-up records were retrospectively reviewed for each patient. Extracted data included: age, sex, living arrangement prior to injury (independent vs. assisted living facility), mechanism of injury, comorbidities, initial treatment modality (operative vs. nonoperative), length of hospital and intensive care unit stay, whether a feeding tube was placed, and discharge disposition. Comorbidity was assessed on the basis of the Charlson comorbidity index (CCI).22 Mortality was assessed using a combination of medical records and the hospital access to death records systems. The abstracted data were transferred to the Data Management Center at (University of Washington) for analysis.
Statistical Analysis
Frequency distributions and summary statistics were calculated for demographic, clinical, and operative variables. For categorical variables, cross-tabulations were generated and Fisher exact or Pearson χ2 tests were used to compare distributions. For continuous variables, t tests were used to investigate differences in the distribution between operative and nonoperative groups. The Kruskal-Wallis test was used for data that were not normally distributed. Differences in survival between the operative and nonoperative groups were modeled using Cox proportional hazards models to assess the prognostic significance of treatment approach (operative vs. nonoperative), including adjustment for age, sex, and CCI. Post-treatment variables were not considered for inclusion into the model because of the potential for introduction of confounding effects related to the treatment. Two Cox models were developed, one for mortality within 30 days of presentation and the other for mortality on the basis of maximum follow-up time. Four covariates (treatment, age, sex, and CCI) were introduced into both mortality Cox models. The maximum follow-up time was defined as time to death for deceased patients or time from injury to date of medical record abstraction for patients who were alive at the time of research (censored observations). Treatment allocation was according to initial treatment. Kaplan-Meier survival plots were created for illustrative purposes for mortality within 30 days and for mortality at the time of maximum follow-up. Statistical analyses were 2-sided, and P < 0.05 was considered statistically significant. All analyses were performed using SAS/STAT version 9.3 (SAS Institute Inc., Cary, NC).
RESULTS
Patient Population
Average follow-up was 647.5 days (range 0–2456 d) for the nonoperative group and 851.2 days (range 1–2565 d) in the operative group. Patient characteristics and mechanism of injury for the 322 patients are summarized in Table 1. The overall mean patient age was 81.8 ± 7.8 years and ranged from 65.0 to 101.5 years. The operatively treated patients were younger than nonoperative patients (80.4 and 83.2 yr, respectively, P = 0.0014). The operative and nonoperative treatment groups did not differ significantly in the proportion of males versus females (P = 0.9395). Prior to the injury, significantly more nonoperative patients were living independently than operative patients (55% vs. 34%, P < 0.0001); however, both groups had moderate numbers of patients for whom preinjury living arrangements were not documented. The vast majority of patients (92%) sustained their odontoid fracture from a ground level fall, and this mechanism of injury was significantly more common among surgically treated patients (96%), compared with nonoperative patients (88%) (P = 0.0097).
TABLE 1. Patient Demographics for 322 Geriatric Patients With Type II Odontoid Fracture, Stratified on the Basis of Operative Versus Nonoperative Treatment.
| All (N = 322) | Operative (N = 165) | Nonoperative (N = 157) | P | |
|---|---|---|---|---|
| Age (yr) | 81.8 ± 7.8 | 80.4 ± 7.7 | 83.2 ± 7.7 | 0.0014 |
| Sex | 0.9395 | |||
| Male | 134 (42%) | 69 (42%) | 65 (41%) | |
| Female | 188 (58%) | 96 (58%) | 92 (59%) | |
| Living arrangements prior to injury | <0.0001 | |||
| Independent | 142 (44%) | 56 (34%) | 86 (55%) | |
| Assisted living facility | 44 (14%) | 16 (10%) | 28 (18%) | |
| Unknown | 136 (42%) | 93 (56%) | 43 (27%) | |
| Mechanism of injury | 0.0097 | |||
| Fall | 296 (92%) | 158 (96%) | 138 (88%) | |
| Motor vehicle collision | 26 (8%) | 7 (4%) | 19 (12%) | |
| Hospital length of stay (d) | 11.3 ± 15.0 | 15.0 ± 18.5 | 7.4 ± 8.7 | <0.0001* |
| ICU stay (d) | 1.3 ± 4.1 | 1.5 ± 4.4 | 1.1 ± 3.8 | 0.0008* |
| Feeding tube placement | 38 (12%) | 30 (18%) | 8 (5%) | 0.0003 |
| Discharge disposition | <0.0001 | |||
| Skilled nursing facility | 81 (25%) | 32 (19%) | 49 (31%) | |
| Home | 76 (24%) | 29 (18%) | 47 (30%) | |
| Rehabilitation facility | 29 (9%) | 17 (10%) | 12 (8%) | |
| Homeless | 1 (<1%) | 0 (0%) | 1 (1%) | |
| Died | 30 (9%) | 9 (5%) | 21 (13%) | |
| Unknown | 105 (33%) | 78 (47%) | 27 (17%) |
*Kruskal-Wallis test.
ICU indicates intensive care unit.
Compared with the nonoperative treatment group, the operative group have significantly longer mean length of hospital stay (15.0 ± 18.5 vs. 7.4 ± 8.7 d, P < 0.0001) and had significantly longer length of stay in the intensive care unit (1.5 ± 4.4 vs. 1.1 ± 3.8 d, P = 0.0008) (Table 1). Operative patients were significantly more likely to be treated with a feeding tube, compared with nonoperatively treated patients (18% vs. 5%, P = 0.0003). The discharge disposition for the overall population included skilled nursing facility for 25%, home for 24%, rehabilitation facility for 9%, and death for 9%. Both operative and nonoperative patient groups had moderate numbers of patients for whom discharge disposition was not documented, which limits the ability to provide definitive comparisons between the groups with regard to this parameter.
The CCI and rates of specific comorbidities are summarized in Table 2. The most common comorbidity was hypertension (33%). None of the rates of the specific comorbidities assessed differed significantly between the operative and nonoperative groups. The mean CCI also did not differ significantly between the operative and nonoperative groups (1.1 ± 1.5 and 1.4 ± 1.5, respectively; P = 0.11).
TABLE 2. Baseline Comorbidities by Treatment for 322 Geriatric Patients With Type II Odontoid Fracture, Stratified on the Basis of Operative Versus Nonoperative Treatment.
| All (N = 322) | Operative (N = 165) | Nonoperative (N = 155) | P | |
|---|---|---|---|---|
| Charlson comorbidity score | 1.2 ± 1.5 | 1.1 ± 1.5 | 1.4 ± 1.5 | 0.11 |
| Comorbidity | ||||
| Chronic obstructive pulmonary disease | 37 (11%) | 14 (8%) | 23 (15%) | 0.0829 |
| Congestive heart failure | 49 (15%) | 20 (12%) | 29 (18%) | 0.1128 |
| Dementia | 48 (15%) | 22 (13%) | 26 (17%) | 0.4164 |
| Diabetes | 52 (16%) | 22 (13%) | 30 (19%) | 0.1592 |
| Hypertension | 106 (33%) | 49 (30%) | 57 (36%) | 0.2072 |
| Myocardial infarction | 16 (5%) | 9 (5%) | 7 (4%) | 0.6810 |
| Other | 187 (58%) | 83 (50%) | 104 (66%) | 0.0038 |
Short-term (30-day) Mortality Analysis
Within 30 days of presentation, 46 of the 322 (14%) patients overall had died. This included 11 (7%) operatively treated patients and 35 (22%) nonoperatively treated patients (Fisher exact P < 0.0001) (Table 3). The rates of mortality for males and females at 30-day follow-up did not differ significantly (13% and 15%, respectively; P = 0.7119). The hazard ratio of death within the first 30 days of presentation in nonoperatively treated patients compared with operatively treated patients was 3.00 (95% [confidence interval] CI = 1.51–5.94, P = 0.0017), reflecting significantly poorer survival among nonoperatively treated patients. This analysis was performed with adjustment for the effects of patient age, sex, and CCI (Table 4, Figure 1).
TABLE 3. 30-day Mortality Rates for 322 Geriatric Patients With Type II Odontoid Fracture, Stratified on the Basis of Sex and Operative Versus Nonoperative Treatment.
| Variable | Died (N = 46) | Alive (N = 276) | P |
|---|---|---|---|
| Sex | 0.7119 | ||
| Male | 18 (13%) | 116 (87%) | |
| Female | 28 (15%) | 160 (85%) | |
| Treatment | <0.0001 | ||
| Operative | 11 (7%) | 154 (93%) | |
| Nonoperative | 35 (22%) | 122 (78%) |
TABLE 4. Survival Adjusted for Age, Sex, and Charlson Comorbidity Index at 30-day Follow-up and at Maximum Follow-up for 322 Geriatric Patients With Type II Odontoid Fracture.
| Variable | Hazard Ratio | 95% CI | P |
|---|---|---|---|
| 30-day mortality | |||
| Management (nonoperative vs. operative) | 3.00 | 1.51–5.94 | 0.0017 |
| Age (yr) | 1.10 | 1.05–1.14 | <0.0001 |
| Male | 1.13 | 0.62–2.08 | 0.6804 |
| Charlson comorbidity index | 1.14 | 0.95–1.36 | 0.1593 |
| Mortality at maximum follow-up | |||
| Management (nonoperative vs. operative) | 1.35 | 0.97–1.89 | 0.0793 |
| Age (yr) | 1.07 | 1.05–1.10 | <0.0001 |
| Male | 1.55 | 1.10–2.16 | 0.0118 |
| Charlson comorbidity index | 1.28 | 1.16–1.40 | <0.0001 |
CI indicates confidence interval.
Figure 1.
Kaplan-Meier plot of 30-day survival from presentation stratified based on operative versus nonoperative treatment for 322 geriatric patients with type II odontoid fracture.
Long-term Mortality Analysis
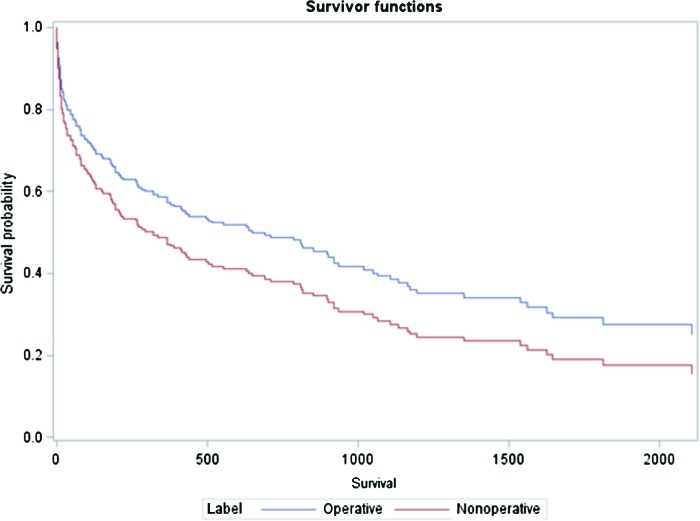
Altogether, there were 661.3 patient-years of follow-up (2.05 yr on average, in the range of 0 d to 7.02 yr). Of these, 276.74 patient-years were from nonoperative patients and 384.51 person-years were from operative patients. At maximum follow-up, 142 of 322 (44%) patients overall had died (21.5 per 100 person-years). This included 62 (38%) of the operatively treated patients and 80 (51%) of the nonoperatively treated patients (P = 0.016; Table 5). The mortality rate for males (52%) was significantly higher than that of females (38%; P = 0.013). After adjusting for the effects of patient age, sex, and CCI, patients treated operatively had a nonsignificant trend toward lower risk of mortality at the time of last assessment, compared with patients treated nonoperatively (HR = 1.35, 95% CI = CI = .97–1.89, P = 0.0793) (Table 4, Figure 2).
TABLE 5. Overall Mortality Rates for 322 Geriatric Patients With Type II Odontoid Fracture at Maximum Follow-up, Stratified on the Basis of Sex and Operative Versus Nonoperative Treatment.
| Variable | Died (N = 142) | Alive (N = 180) | P |
|---|---|---|---|
| Sex | 0.013 | ||
| Male | 70 (52%) | 64 (48%) | |
| Female | 72 (38%) | 116 (62%) | |
| Treatment | 0.016 | ||
| Operative | 62 (38%) | 103 (62%) | |
| Nonoperative | 80 (51%) | 77 (49%) |
Figure 2.
Kaplan-Meier plot of survival at maximum follow-up from presentation stratified based on operative versus nonoperative treatment for 322 geriatric patients with type II odontoid fracture.
DISCUSSION
Despite a large number of publications, optimal management of odontoid fractures in the elderly remains controversial.23–25 On the basis of a systematic review of the literature, Harrop et al26 recently recommended that type II odontoid fractures in this population should be treated operatively, but the quality of evidence supporting this recommendation ranged from very low to low. However, whether the potential risks of morbidity and mortality incurred by operative treatment are offset by improvements in outcome is an unsettled issue.19,27–30
This study provides an assessment of 30-day and long-term mortality rates for a cohort of 322 elderly patients with type II odontoid fracture, including stratification based on operative versus nonoperative treatment approach. The findings demonstrate high general rates of mortality in this patient population, specifically 14% within 30 days of presentation. After adjusting for the effects of patient age, sex, and CCI, operatively treated patients had a significantly better 30-day survival rate compared with nonoperatively treated patients. At maximum follow-up, patients treated operatively had a nonsignificant trend toward lower risk of mortality compared with patients treated nonoperatively.
Collectively, these data, demonstrate that surgical treatment of type II odontoid fracture in this elderly population did not negatively impact survival, even after adjusting for patient age and comorbidities, and, that operative treatment may be associated with a significant 30-day survival advantage compared with nonoperatively treated patients. The observation that this survival advantage seems to diminish to the level of a nonsignificant trend during longer term follow-up may relate to a dilutional effect of deaths occurring due to unrelated comorbid conditions in both groups of this elderly population. It is also important to recognize that, although the mortality rates between the operative and nonoperative treatment groups were not significantly different at longer-term follow-up, our data do not permit assessment for potential differences between the groups with regard to neurological or functional status.
White et al25 recently performed a meta-analysis of elderly patients treated surgically for type II odontoid fracture and reported overall, in-hospital, postdischarge, and 12-month mortality rates of 10.1%, 6.2%, 8.8%, and 7.7%, respectively.25 The surgically treated patients in this study had 30-day and 12-month follow-up mortality rates of 7% and 26%, respectively. Although the 30-day mortality rate for surgically treated patients from this study is comparable with the postdischarge mortality rate from the systematic review of White et al.25 (7% vs. 8.8%, respectively), the 12-month mortality rate of this study is substantially higher than the 12-month mortality rate reported by White et al25 (26% vs. 7.7%). This difference is likely due to inconsistencies and limitations in the 12-month mortality rate reported by White et al.25 Their data are based on 12 small, mostly retrospective studies with differing methodological and reporting approaches, thus limiting the reliability of the reported 12-month estimate. The largest study in the systemic review of White et al25 had only 75 patients, with many having fewer than 20 patients, and several of the studies had exclusion criteria that could artificially lower mortality rates.31–37
Based on a recent systematic review from Harrop et al,26 the rates of mortality for nonoperative care for type II odontoid fractures in the elderly range from 4% to 42%. These rates were based on studies with typically low numbers of patients and varying lengths of follow-up. The 30-day and maximum follow-up rates of mortality in this study for patients treated nonoperatively were 22% and 51%, respectively. Our reported rates are toward the higher end of the range reported by Harrop et al26 and may reflect our specific emphasis on collecting mortality events in this study.
Few previous studies provide direct comparison of mortality rates between operative and nonoperative care for elderly patients with type II odontoid fractures.38 Smith et al34 reported similar in-hospital mortality rates for 72 octogenarians with type II odontoid fractures treated operatively or nonoperatively (mortality rates of 15% and 12.5%, respectively). Chen et al39 compared 28 surgically and 28 nonsurgically treated elderly patients with type II odontoid fracture and reported no significant differences in 30-day survival (3.6% vs. 7.1%, respectively, P > 0.05) or longer-term survival at a mean of approximately 200 days. Schoenfeld et al40 compared 112 nonoperatively treated with 44 operatively treated type II odontoid fractures in elderly patients, and reported higher 3-month mortality (25% vs. 11%) and 1-year mortality (36% vs. 21%) in nonoperatively treated patients. Fagin et al27 assessed 108 elderly patients with odontoid fracture and reported that nonoperative and operative treatment approaches were associated with similar short-term mortality and concluded that nonoperative management should be given strong consideration in these patients.
It is important to recognize potential limitations of this study in order to add context to the interpretation of the data and to highlight important factors for future studies. The most significant limitation is the retrospective design, which limits the ability to assess and control for potential biases in the decision of treatment approach. It is possible that modest trends of increased age and comorbidities could have negatively impacted survival among the nonoperative patients. In addition, our data do not enable assessment of neurological and functional status at follow-up, which may differ between the treatment groups. This study does not include assessment of complication rates (except for mortality) associated with either treatment approach, although there was a significantly greater incidence of feeding tube placement in operatively treated patients. This study suggests that a greater number of patients treated operatively were able to be discharged to home compared with nonoperatively treated patients; however, the retrospective design limited our ability to collect this parameter for a substantial number of patients, which considerably limits the ability to draw conclusions on the basis of this finding. Lastly, although the longer hospital and intensive care unit stay in the operatively treated group suggests that operative treatment may have greater short-term cost compared with nonoperative treatment, this study does not provide assessment of potential long-term cost differences between the treatment groups. However, this study may offer important insights into the ongoing controversies. This study is of a larger group of patients than previously reported with a greater emphasis on patient survival. After adjustment for patient comorbidities, there is a suggestion that at least short-term survival of elderly patients is improved with surgical care. Also, nonsurgical care is not benign. While it is clear that there is no simple answer for the treatment of elderly patients, surgical care may improve chances for survival of elderly patients with type II odontoid fractures. Whether operative treatment is associated with improved neurological and functional status warrants further study.
KEY POINTS
Odontoid fractures are the most common isolated spine fracture in the elderly, and the majority of these are type II fractures. Patients who sustain these injuries experience high mortality, and their management, whether operative or nonoperative, remains controversial.
Operative treatment for geriatric patients with type II odontoid fractures is associated with improved 30-day survival compared with nonoperative treatment, with adjustment for patient age, sex, and comorbidities.
Operative treatment for geriatric patients with type II odontoid fractures is associated with a nonsignificant trend toward higher long-term survival compared with nonoperative treatment, with adjustment for patient age, sex, and comorbidities.
At a minimum, the findings demonstrate that surgical treatment for type II odontoid fracture in this elderly population did not negatively impact either short- or long-term survival.
Footnotes
Address correspondence and reprint requests to Justin S. Smith, MD, PhD, Department of Neurosurgery, University of Virginia Health Sciences Center, PO Box 800212, Charlottesville VA, 22908; E-mail: jss7f@virginia.edu
The manuscript submitted does not contain information about medical device(s)/drug(s).
The AOSpine North America Inc., a 501(c) 3 nonprofit corporation's funds were received to support this work.
Relevant financial activities outside the submitted work: consultancy, board membership, consulting fee or honorarium, fees for participation in review activities, expert testimony, payment for lectures, royalties, payment for development of educational presentations, patents, stock/stock options, and travel/accommodations/meeting expenses.
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivitives 3.0 License, where it is permissible to download and share the work provided it is properly cited. The work cannot be changed in any way or used commercially.
References
- 1.Chapman J, Bransford R. Geriatric spine fractures: an emerging healthcare crisis. J Trauma 2007;62:S61–2 [DOI] [PubMed] [Google Scholar]
- 2.U.S. Census Bureau, Population Division: Interim State Population Projections. 2005
- 3.U.S. Census Bureau: Population Projections of the United States by Age, Sex, Race, and Hispanic Origin: 1995–2050; report 25–1130
- 4.Ryan MD, Henderson JJ. The epidemiology of fractures and fracture-dislocations of the cervical spine. Injury 1992;23:38–40 [DOI] [PubMed] [Google Scholar]
- 5.Golob JF, Jr, Claridge JA, Yowler CJ, et al. Isolated cervical spine fractures in the elderly: a deadly injury. J Trauma 2008;64:311–5 [DOI] [PubMed] [Google Scholar]
- 6.Anderson LD, D'Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am 1974;56:1663–74 [PubMed] [Google Scholar]
- 7.Smith HE, Kerr SM, Fehlings MG, et al. Trends in epidemiology and management of type II odontoid fractures: 20-year experience at a model system spine injury tertiary referral center. J Spinal Disord Tech 2010;23:501–5 [DOI] [PubMed] [Google Scholar]
- 8.Denaro V, Papalia R, Di Martino A, et al. The best surgical treatment for type II fractures of the dens is still controversial. Clin Orthop Relat Res 2011;469:742–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Butler JS, Dolan RT, Burbridge M, et al. The long-term functional outcome of type II odontoid fractures managed non-operatively. Eur Spine J 2010;19:1635–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel AA, Lindsey R, Bessey JT, et al. Surgical treatment of unstable type II odontoid fractures in skeletally mature individuals. Spine (Phila Pa 1976) 2010;35:S209–18 [DOI] [PubMed] [Google Scholar]
- 11.Molinari RW, Khera OA, Gruhn WL, et al. Rigid cervical collar treatment for geriatric type II odontoid fractures. Eur Spine J 2012;21:855–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chaudhary A, Drew B, Orr RD, et al. Management of type II odontoid fractures in the geriatric population: outcome of treatment in a rigid cervical orthosis. J Spinal Disord Tech 2010;23:317–20 [DOI] [PubMed] [Google Scholar]
- 13.Heggeness MH, Doherty BJ. The trabecular anatomy of the axis. Spine (Phila Pa 1976) 1993;18:1945–9 [DOI] [PubMed] [Google Scholar]
- 14.Sasso RC. C2 dens fractures: treatment options. J Spinal Disord 2001;14:455–63 [DOI] [PubMed] [Google Scholar]
- 15.Campanelli M, Kattner KA, Stroink A, et al. Posterior C1-C2 transarticular screw fixation in the treatment of displaced type II odontoid fractures in the geriatric population–review of seven cases. Surg Neurol 1999;51:596–600; discussion 1. [DOI] [PubMed] [Google Scholar]
- 16.Molinari RW, Dahl J, Gruhn WL, et al. Functional outcomes, morbidity, mortality, and fracture healing in 26 consecutive geriatric odontoid fracture patients treated with posterior fusion. [published online ahead of print December 2, 2011]. J Spinal Disord Tech; 2011 [DOI] [PubMed] [Google Scholar]
- 17.Crockard HA, Heilman AE, Stevens JM. Progressive myelopathy secondary to odontoid fractures: clinical, radiological, and surgical features. J Neurosurg 1993;78:579–86 [DOI] [PubMed] [Google Scholar]
- 18.Kirankumar MV, Behari S, Salunke P, et al. Surgical management of remote, isolated tye II odontoid fractures with atlantoaxial dislocation causing cervical compressive myelopathy. Neurosurgery 2005;56:1004–12 [PubMed] [Google Scholar]
- 19.Hart R, Saterbak A, Rapp T, et al. Nonoperative management of dens fracture nonunion in elderly patients without myelopathy. Spine (Phila Pa 1976) 2000;25:1339–43 [DOI] [PubMed] [Google Scholar]
- 20.Bednar DA, Parikh J, Hummel J. Management of type II odontoid process fractures in geriatric patients; a prospective study of sequential cohorts with attention to survivorship. J Spinal Disord 1995;8:166–9 [PubMed] [Google Scholar]
- 21.Shilpakar S, McLaughlin MR, Haid RWJ, et al. Management of acute odontoid fractures: operative techniques and complication avoidance. Neurosurg Focus 2000;8:e3. [PubMed] [Google Scholar]
- 22.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83 [DOI] [PubMed] [Google Scholar]
- 23.Hsu WK, Anderson PA. Odontoid fractures: update on management. J Am Acad Orthop Surg 2010;18:383–94 [DOI] [PubMed] [Google Scholar]
- 24.Pal D, Sell P, Grevitt M. Type II odontoid fractures in the elderly: an evidence-based narrative review of management. Eur Spine J 2011;20:195–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.White AP, Hashimoto R, Norvell DC, et al. Morbidity and mortality related to odontoid fracture surgery in the elderly population. Spine (Phila Pa 1976) 2010;35:S146–57 [DOI] [PubMed] [Google Scholar]
- 26.Harrop JS, Hart R, Anderson PA. Optimal treatment for odontoid fractures in the elderly. Spine (Phila Pa 1976) 2010;35:S219–27 [DOI] [PubMed] [Google Scholar]
- 27.Fagin AM, Cipolle MD, Barraco RD, et al. Odontoid fractures in the elderly: should we operate? J Trauma 2010;68:583–6 [DOI] [PubMed] [Google Scholar]
- 28.Koech F, Ackland HM, Varma DK, et al. Nonoperative management of type II odontoid fractures in the elderly. Spine (Phila Pa 1976) 2008;33:2881–6 [DOI] [PubMed] [Google Scholar]
- 29.Ryan MD, Taylor TK. Odontoid fractures in the elderly. J Spinal Disord 1993;6:397–401 [DOI] [PubMed] [Google Scholar]
- 30.Kuntz C, IV, Mirza SK, Jarell AD, et al. Type II odontoid fractures in the elderly: early failure of nonsurgical treatment. Neurosurg Focus 2000;8:e7. [DOI] [PubMed] [Google Scholar]
- 31.Berlemann U, Schwarzenbach O. Dens fractures in the elderly. Results of anterior screw fixation in 19 elderly patients. Acta Orthop Scand 1997;68:319–24 [DOI] [PubMed] [Google Scholar]
- 32.Borm W, Kast E, Richter HP, et al. Anterior screw fixation in type II odontoid fractures: is there a difference in outcome between age groups? Neurosurgery 2003;52:1089–92; discussion 92–4. [PubMed] [Google Scholar]
- 33.Platzer P, Thalhammer G, Ostermann R, et al. Anterior screw fixation of odontoid fractures comparing younger and elderly patients. Spine (Phila Pa 1976) 2007;32:1714–20 [DOI] [PubMed] [Google Scholar]
- 34.Smith HE, Kerr SM, Maltenfort M, et al. Early complications of surgical versus conservative treatment of isolated type II odontoid fractures in octogenarians: a retrospective cohort study. J Spinal Disord Tech 2008;21:535–9 [DOI] [PubMed] [Google Scholar]
- 35.Smith HE, Vaccaro AR, Maltenfort M, et al. Trends in surgical management for type II odontoid fracture: 20 years of experience at a regional spinal cord injury center. Orthopedics 2008;31:650. [PubMed] [Google Scholar]
- 36.Platzer P, Thalhammer G, Oberleitner G, et al. Surgical treatment of dens fractures in elderly patients. J Bone Joint Surg Am 2007;89:1716–22 [DOI] [PubMed] [Google Scholar]
- 37.Tashjian RZ, Majercik S, Biffl WL, et al. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma 2006;60:199–203 [DOI] [PubMed] [Google Scholar]
- 38.Nourbakhsh A, Shi R, Vannemreddy P, et al. Operative versus nonoperative management of acute odontoid type II fractures: a meta-analysis. J Neurosurg Spine 2009;11:651–8 [DOI] [PubMed] [Google Scholar]
- 39.Chen YR, Boakye M, Arrigo RT, et al. Morbidity and mortality of C2 fractures in the elderly: surgery and conservative treatment. Neurosurgery 2012;70:1055–9; discussion 9. [DOI] [PubMed] [Google Scholar]
- 40.Schoenfeld AJ, Bono CM, Reichmann WM, et al. Type II odontoid fractures of the cervical spine: do treatment type and medical comorbidities affect mortality in elderly patients? Spine (Phila Pa 1976) 2011;36:879–85 [DOI] [PMC free article] [PubMed] [Google Scholar]