Abstract
Objective:
To investigate whether community engagement (participation in grassroots organizations) contributed to increases in HIV testing in Zimbabwe.
Methods:
Prospective data on membership of local community organizations (e.g. women's groups and burial societies) and uptake of HIV testing and counselling (HTC) and prevention-of-mother-to-child transmission (PMTCT) services were collected from 5260 adults interviewed in two consecutive rounds of a general-population cohort survey in eastern Zimbabwe between 2003 and 2008. The effects of community engagement on uptake of services during the follow-up period were measured using logistic regression to adjust for observed confounding factors.
Results:
Sixteen percent of men and 47% of women were consistent members of community organizations; 58 and 35% of these people discussed HIV in their meetings and were members of externally sponsored organizations, respectively. Fewer men (10.1%) than women (32.4%) took up HTC during follow-up [adjusted odds ratio (aOR) = 4.08, 95% confidence interval (CI) 3.43–4.86, P < 0.001]. HTC uptake was higher for members of community organizations than for nonmembers: men, 15.0 versus 9.2% (1.67, 1.15–2.43, P = 0.007); women, 35.6 versus 29.6% (1.26, 1.06–1.49, P = 0.008). Membership of community organizations showed a nonsignificant association with PMTCT uptake amongst recently pregnant women (42.3 versus 34.2%; 1.30, 0.94–1.78, P = 0.1). The most consistent positive associations between community participation and HTC and PMTCT uptake were found in organizations that discussed HIV and when external sponsorship was absent.
Conclusion:
Grassroots organizations contributed to increased uptake of HTC services in eastern Zimbabwe in the mid-2000s. Partnerships with these organizations could harness community support for the further increases in HIV testing needed in sub-Saharan Africa.
Keywords: community engagement, HIV testing and counselling uptake, prevention-of-mother-to-child transmission, social capital, Zimbabwe
Introduction
HIV testing and counselling services (HTC) are widely recognized as the gateway to effective HIV control [1]. This is increasingly important in sub-Saharan Africa following the roll-out of antiretroviral treatment (ART) as achieving high uptake of HTC services is a critical first step if universal access to treatment is to be reached [2] and the prevention benefits of ART realized [3,4].
However, despite increases in the uptake of HIV testing services as the switch to provider-initiated approaches [5] and the expansion of treatment services, many people in sub-Saharan African countries remain unaware of their HIV infection status [6]. In seven countries with data from nationally representative surveys conducted between 2009 and 2011, the proportion of men who had never had an HIV test varied from 27% in Rwanda and 47.5% in Malawi to 81% in Mozambique and 91% in Madagascar, whereas the equivalent proportion for women ranged from 23% in Rwanda and 27% in Malawi to 74% in Congo and 86% in Madagascar [7]. A particular concern is that almost 40% of pregnant women in sub-Saharan Africa in 2010 did not receive an HIV test in routine antenatal care [6] despite the efficacy of ART treatment to prevent infant infection and the UNAIDS goal to eliminate vertical transmission by 2015.
In the UNAIDS Investment Framework, community mobilization is suggested as a key social enabler for increasing the uptake of HIV services [8]. The World Health Organization, in its strategic policy framework for HTC, recommends the promotion of services through community-based options and innovation to reach beyond facilities [9]. However, although community engagement is seen as essential to address stigma and other social obstacles to use of HIV services [10], to date, there is little scientific evidence for increased uptake of HTC services resulting from community responses to the HIV epidemic or on the causal mechanisms through which such increases may occur.
In previous research in eastern Zimbabwe, participation in community-based organizations was found to be associated with reductions in incidence of HIV infection and linked sexual-risk behaviours [11] and HIV-associated stigma [12]. Here, we use prospective data from a general population cohort survey to measure associations between participation in community organizations on uptake of HTC and prevention-of-mother-to-child transmission (PMTCT) services during the scale-up of these services in Zimbabwe, and to investigate whether social spaces for dialogue about HIV/AIDS provided by community organizations and external sponsorship contributed to these associations.
Methods
Data
The data for the study were taken from the third and fourth rounds of a population-based open cohort survey conducted in 12 sites stratified by socioeconomic location (two small towns, four agricultural estates, two roadside settlements and four subsistence farming areas) in Manicaland province in eastern Zimbabwe [13]. These two rounds covered a period (2003–2008) when HTC and PMTCT services were scaled-up throughout Zimbabwe [14].
In round three (the baseline for this study), a phased census was conducted of all households in the 12 sites, one site at a time, between July 2003 and August 2005. All adults aged between 15 and 54 years at last birthday who stayed in the households enumerated in the census on the night before the survey visit (i.e. including visitors) were invited to participate in an individual interview and to provide a dried blood spot specimen for anonymized HIV testing for use in the research [13]. In the interview, data were collected on sociodemographic characteristics, sexual risk behaviour, recent pregnancy history, knowledge and perceptions on HIV/AIDS, participation in local community organization activities, and uptake of HTC and PMTCT services. At each survey round, a parallel free voluntary counselling and testing service is provided for study participants.
The fourth round of the survey (the follow-up for this study) was conducted 3 years after the third round in each site. Once again, a complete census of preexisting and new households was conducted in the 12 sites. However, because of funding constraints, individual interviews (including follow-up interviews for persons who had participated at baseline) were limited to individuals meeting the eligibility criteria (adults aged 15–54 years) from a random sample of two-thirds of households in each site. Similar data were collected to those collected at baseline.
Written informed consent was sought as a condition of enrolment and continuation in the study. Prior ethical approval for the study was obtained from the Medical Research Council of Zimbabwe (MRCZ/A/681) and the St. Mary's Local Research Ethics Committee in the United Kingdom (03.66 R&D 03/SB/004E).
Data analysis
Research participants were included in this analysis if they were interviewed and provided a blood sample for anonymous HIV testing at both the baseline survey and the follow-up survey.
Participation in community organizations was defined by membership of functional community groups which included church groups, women's groups (sewing and other income-generating activities), cooperatives, farmers’ groups, rotating credit societies (savings clubs for income-generating projects), burial societies (community insurance schemes for funeral expenses), youth groups, sports clubs, AIDS groups and political parties. Individuals were treated as participating in community organizations if they were members of at least one such organization at baseline and also at follow-up. Individuals were treated as participating in multiple community organizations if they were members of more than one different type of group at both rounds of the survey. In testing the hypothesis that community organizations contribute to greater uptake of testing services by providing social spaces for dialogue about HIV, groups were treated as providing social spaces for dialogue about HIV when members were reported to discuss care for people living with HIV (PLHIV) either formally or informally when attending group meetings.
Responses to a question asked at baseline on whether respondents had ever had an HIV test were used to construct a variable on prior uptake of HTC services. A variable on uptake of HTC services during the intersurvey period was constructed from responses to a question asked at follow-up on the number of HIV tests taken in the previous 3 years.
For the analysis of uptake of PMTCT during the intersurvey period, women were treated as having had a recent pregnancy if, at follow-up, they reported at least one pregnancy in the previous 3 years. For women who were not pregnant at the time of the follow-up interview, data on the most recent pregnancy were used. For women who were pregnant at follow-up and for whom the pregnancy had lasted for less than 4 months, data on the most recent previous pregnancy were used for assessing uptake on HIV testing services for PMTCT when there had been another pregnancy within the last 3 years. For all women who were pregnant at follow-up, data on the previous pregnancy in the last 3 years were used for assessing uptake of the ART regimen used for PMTCT (at the time, this was single dose nevirapine for the mother and baby at delivery).
Differences in participation in community organizations by sociodemographic characteristic were investigated for each sex using logistic regression controlling for age and socioeconomic stratum. The sociodemographic variables were measured at baseline and included education, church denomination, marital status, employment status, poverty tercile – based on an asset index [15], pregnancy in the last 3 years (for women), HIV infection status and prior history of HIV testing. Levels of uptake of HTC and PMTCT were calculated and compared by sociodemographic characteristic using logistic regression controlling for age and socioeconomic stratum. Characteristics associated with differences in uptake of HIV services (P < 0.1) were included in multivariable logistic regression models used to test for evidence of statistical associations between participation in community organizations and uptake of HIV services. The possibility of a greater effect on uptake of services with increasing number of group memberships was investigated by replacing the binary variable on participation in community organizations in the models with dummy variables denoting membership of zero, one, two and more than two community organizations. Similarly, the effect of dialogue about HIV was investigated by replacing the binary variable on participation in community organizations in the models with dummy variables denoting membership of community organizations that did and did not discuss care for PLHIV.
In an ecological analysis of the effects of community group membership at village level, the 12 study locations were subdivided into clusters based on villages (in rural villages and roadside settlements), residential compounds (agricultural estates) and suburbs (small towns). Clusters with less than 10 males or females in the study were excluded from the corresponding analyses. Ordinary least squares regression was used to test for associations between greater participation in community organizations and increased uptake of HIV services.
Results
Participation in the study
In total, 9543 of 9951 (95.9%) households identified in the baseline census were enumerated. In these households, 15 818 people eligible for interview were listed and 13 125 (83.0%) participated in the study. At baseline, 10 336 of these people stayed in households selected for individual interviews 3 years later at follow-up, and 5498 (53.2%) were reinterviewed. Most of the loss-to-follow-up in the survey is due to out-migration [13]. For 5260 (97.4%) of the individuals reinterviewed, there was complete information on the variables required for the current analysis.
Participation in community organizations
Sixteen percent (286/1812) of men and 47% (1612/3448) of women reported participation in at least one community organization at baseline and also again at follow-up. For both sexes, participation rates were highest at older ages and tended to be lower among individuals living in towns than among those living in more rural areas (Table 1). Men in agricultural estates had higher participation levels, whereas women in estates had lower participation rates than those living in other locations. After adjustment for age and place of residence, participation rates were higher among more educated and married individuals, among those from Christian churches and less poor households, and in people who had previously taken up HTC. However, men and women infected with HIV were less likely than uninfected individuals to participate in community organizations. For women, participation was lower among those in employment, from Apostolic churches, and with a recent pregnancy.
Table 1. Sociodemographic determinants of participation in community organizations, 2003–2008.
| Males | Females | |||||||
| CBO participation | Test for difference | CBO participation | Test for difference | |||||
| Characteristic (at baseline) | n | N (%) | aOR (95% CI) | P | n | N (%) | aOR (95% CI) | P |
| All males and females | 286 | 1812 (15.8) | – | 1612 | 3448 (46.8) | – | ||
| Age-group | ||||||||
| 15–19 | 39 | 426 (9.2) | 1 | 103 | 421 (24.5) | 1 | ||
| 20–34 | 131 | 836 (15.7) | 1.79 (1.22–2.63) | 0.003 | 579 | 1432 (40.4) | 2.21 (1.73–2.84) | <0.001 |
| 35–54 | 116 | 550 (21.1) | 2.57 (1.74–3.82) | <0.001 | 930 | 1595 (58.3) | 4.32 (3.38–5.52) | <0.001 |
| Residence | ||||||||
| Village | 83 | 606 (13.7) | 1 | 768 | 1466 (52.4) | 1 | ||
| Roadside settlement | 53 | 334 (15.9) | 1.26 (0.86–1.84) | 0.23 | 382 | 745 (51.3) | 0.95 (0.79–1.14) | 0.59 |
| Agricultural estate | 120 | 619 (19.4) | 1.39 (1.02–1.89) | 0.039 | 361 | 864 (41.8) | 0.68 (0.57–0.81) | <0.001 |
| Small town | 30 | 253 (11.9) | 0.81 (0.52–1.27) | 0.36 | 101 | 373 (27.1) | 0.35 (0.27–0.45) | <0.001 |
| School education | ||||||||
| Primary or none | 81 | 518 (15.6) | 1 | 849 | 1726 (49.2) | 1 | ||
| Secondary or higher | 205 | 1294 (15.8) | 1.35 (0.99–1.84) | 0.057 | 763 | 1722 (44.3) | 1.50 (1.27–1.78) | <0.001 |
| Church | ||||||||
| Protestant | 103 | 633 (16.3) | 1 | 695 | 1316 (52.8) | 1 | ||
| Roman Catholic | 48 | 273 (17.6) | 1.19 (0.81–1.75) | 0.38 | 307 | 565 (54.3) | 1.02 (0.83–1.26) | 0.83 |
| Apostolic | 78 | 393 (19.8) | 1.22 (0.87–1.71) | 0.25 | 411 | 999 (41.1) | 0.65 (0.55–0.78) | <0.001 |
| Pentecostal | 28 | 126 (22.2) | 1.38 (0.85–2.25) | 0.19 | 146 | 311 (46.9) | 0.94 (0.72–1.22) | 0.64 |
| Traditional | 22 | 338 (6.5) | 0.28 (0.17–0.47) | <0.001 | 23 | 175 (13.1) | 0.15 (0.09–0.23) | <0.001 |
| Other | 7 | 49 (14.3) | 0.82 (0.35–1.90) | 0.65 | 30 | 82 (36.6) | 0.56 (0.35–0.91) | 0.019 |
| Marital status | ||||||||
| Currently married | 191 | 982 (19.5) | 1 | 1158 | 2272 (51.0) | 1 | ||
| Never married | 82 | 758 (10.8) | 0.71 (0.48–1.04) | 0.079 | 125 | 475 (26.3) | 0.62 (0.46–0.84) | 0.002 |
| Formerly married | 13 | 72 (18.1) | 0.99 (0.53–1.85) | 0.97 | 329 | 701 (46.9) | 0.73 (0.61–0.87) | <0.001 |
| Employment status | ||||||||
| Unemployed | 171 | 1170 (14.6) | 1 | 1488 | 3083 (48.3) | 1 | ||
| Employed | 115 | 642 (17.9) | 0.91 (0.66–1.25) | 0.56 | 124 | 365 (34.0) | 0.53 (0.42–0.69) | <0.001 |
| Poverty tercile | ||||||||
| Least poor | 128 | 711 (18.0) | 1 | 571 | 1175 (48.6) | 1 | ||
| Poor | 87 | 628 (13.9) | 0.71 (0.52–0.96) | 0.025 | 550 | 1190 (46.2) | 0.80 (0.68–0.95) | 0.010 |
| Poorest | 71 | 473 (15.0) | 0.79 (0.57–1.10) | 0.17 | 491 | 1083 (45.3) | 0.76 (0.63–0.91) | 0.002 |
| Pregnancy in last 3 years | ||||||||
| No | – | – | 1257 | 2492 (50.4) | 1 | |||
| Yes | – | – | 355 | 956 (37.1) | 0.83 (0.70–0.99) | 0.035 | ||
| HIV infection status | ||||||||
| Uninfected | 252 | 1577 (16.0) | 1 | 1352 | 2846 (47.5) | 1 | ||
| Infected | 34 | 235 (14.5) | 0.71 (0.48–1.07) | 0.099 | 260 | 602 (43.2) | 0.81 (0.68–0.98) | 0.031 |
| Ever taken up HTC | ||||||||
| No | 262 | 1703 (15.4) | 1 | 1395 | 3094 (45.1) | 1 | ||
| Yes | 24 | 108 (22.2) | 1.43 (0.88–2.31) | 0.14 | 217 | 353 (61.5) | 1.80 (1.41–2.28) | <0.001 |
HTC, HIV testing and counselling. Community-based organization (CBO) participation, reporting membership of at least one community organization at baseline and again, after 3 years, at follow-up. aOR, age and residence-adjusted odds ratio for participation in a community organization.
The most popular types of community organizations for men were church groups (7.0% of men), burial societies (3.7%), political parties (1.8%) and sports clubs (1.7%). For women, the most popular organizations joined were church groups (31.7%), burial societies (29.2%), savings clubs (6.8%) and farmers groups (6.6%). Less than one percent (0.7%) of men and 3.8% of women were members of specialist AIDS groups.
Among the men in community organizations, 56.6% (162/286) were members of groups that discussed care for PLHIV and 36.4% (104/286) were members of groups that received external sponsorship. For women, the results were similar, with 58.7% (947/1612) being members of groups that discussed HIV and 35.1% (566/1612) being members of groups with sponsorship. The most common sponsors of community organizations were churches (46%), NGOs (16%), political parties (8%) and employers (2%). Community organizations with external sponsorship were more likely than other groups to discuss care for PLHIV (67.8 versus 53.3%; aOR 1.87, 95% CI 1.54–2.29).
Uptake of HIV testing and counselling
At baseline, 6.0% (108/1812) of men and 10.2% (353/3448) of women reported ever having taken up HTC. During the 3-year intersurvey period, 10.1% (95% CI, 8.7–11.5%, N = 1812) of men and 32.4% (30.8–34.0%, 3448) of women received HTC. The results on patterns and determinants of HIV testing are shown in Table 2. For men, HTC was less common in younger men and those living on estates. For women, no differences by age were found but testing was more common in rural villages than in agricultural estates and more urban areas. After adjusting for age and place of residence, greater poverty was associated with lower uptake of HTC and a prior history of testing was associated with higher levels of HTC. For men – but not for women – HIV testing was more common in those with HIV infection. For women, HTC was more common in those who were widowed or divorced and less common in those who had never been married. HTC also was less common in women from Apostolic churches but more common in those with a recent pregnancy.
Table 2. Associations between participation in community-based organizations and uptake of HIV testing and counselling, 2003–2008.
| Males | Females | |||||||
| HTC uptake | Test for difference | HTC uptake | Test for difference | |||||
| Characteristic | n | N (%) | aOR* (95% CI) | P | n | N (%) | aOR* (95% CI) | P |
| CBO participation | ||||||||
| Yes | 43 | 286 (15.0) | 1.67 (1.15–2.43) | 0.007 | 574 | 1612 (35.6) | 1.26 (1.06–1.49) | 0.008 |
| No | 140 | 1526 (9.2) | 1 | 543 | 1836 (29.6) | 1 | ||
| Age-group | ||||||||
| 15–19 | 29 | 426 (6.8) | 1 | 127 | 421 (30.2) | 1 | – | |
| 20–34 | 97 | 836 (11.6) | 1.52 (0.95–2.43) | 0.082 | 520 | 1432 (36.3) | 0.90 (0.65–1.25) | 0.51 |
| 35–54 | 57 | 550 (10.4) | 1.31 (0.74–2.33) | 0.35 | 470 | 1595 (29.5) | 0.96 (0.64–1.43) | 0.83 |
| Residence | ||||||||
| Village | 67 | 606 (11.1) | 1 | 576 | 1466 (39.3) | 1 | ||
| Roadside settlement | 38 | 334 (11.4) | 1.05 (0.63–1.75) | 0.84 | 252 | 745 (33.8) | 0.73 (0.59–0.90) | 0.004 |
| Agricultural estate | 49 | 619 (7.9) | 0.63 (0.41–0.97) | 0.034 | 183 | 864 (21.2) | 0.41 (0.30–0.56) | <0.001 |
| Small town | 29 | 253 (11.5) | 0.89 (0.55–1.42) | 0.62 | 106 | 373 (28.4) | 0.55 (0.40–0.74) | <0.001 |
| School education | ||||||||
| Primary or none | 43 | 518 (8.3) | 1 | 488 | 1726 (28.3) | 1 | ||
| Secondary or higher | 140 | 1294 (10.8) | 1.22 (0.80–1.85) | 0.35 | 629 | 1722 (36.5) | 1.21 (1.00–1.46) | 0.055 |
| Church | ||||||||
| Protestant | 64 | 633 (10.1) | – | 445 | 1316 (33.8) | 1 | ||
| Roman Catholic | 31 | 273 (11.4) | – | 232 | 565 (41.1) | 1.23 (0.98–1.54) | 0.72 | |
| Apostolic | 37 | 393 (9.4) | – | 267 | 999 (26.7) | 0.76 (0.63–0.92) | 0.004 | |
| Pentecostal | 8 | 126 (6.3) | – | 105 | 311 (33.8) | 1.15 (0.88–1.51) | 0.31 | |
| Traditional | 37 | 338 (10.9) | – | 41 | 175 (23.4) | 0.88 (0.58–1.32) | 0.53 | |
| Other | 6 | 49 (12.2) | – | 27 | 82 (32.9) | 1.16 (0.72–1.87) | 0.54 | |
| Marital status | ||||||||
| Currently married | 105 | 982 (10.7) | – | 758 | 2272 (33.4) | 1 | ||
| Never married | 68 | 758 (9.0) | – | 126 | 475 (26.5) | 0.67 (0.50–0.90) | 0.008 | |
| Formerly married | 10 | 72 (13.9) | – | 233 | 701 (33.2) | 1.38 (1.15–1.65) | <0.001 | |
| Employment status | ||||||||
| Unemployed | 114 | 1170 (9.7) | – | 1020 | 3083 (33.1) | – | ||
| Employed | 69 | 642 (10.7) | – | 97 | 365 (26.6) | – | ||
| Poverty tercile | ||||||||
| Least poor | 85 | 711 (12.0) | 1 | 381 | 1175 (32.4) | 1 | ||
| Poor | 60 | 628 (9.6) | 0.80 (0.58–1.10) | 0.17 | 410 | 1190 (34.5) | 1.07 (0.87–1.31) | 0.52 |
| Poorest | 38 | 473 (8.0) | 0.66 (0.43–1.03) | 0.068 | 326 | 1083 (30.1) | 0.80 (0.65–0.98) | 0.033 |
| Pregnancy in last 3 years | ||||||||
| No | – | – | 650 | 2492 (26.1) | 1 | |||
| Yes | – | – | 467 | 956 (48.8) | 3.49 (2.81–4.36) | <0.001 | ||
| HIV infection status | ||||||||
| Uninfected | 147 | 1577 (9.3) | 1 | 919 | 2846 (32.3) | – | ||
| Infected | 36 | 235 (15.3) | 1.76 (1.12–2.76) | 0.014 | 198 | 602 (32.9) | – | |
| Ever taken up HTC | ||||||||
| No | 152 | 1703 (8.9) | 1 | 909 | 3094 (29.4) | 1 | ||
| Yes | 31 | 108 (28.7) | 3.60 (2.16–5.99) | <0.001 | 208 | 353 (58.9) | 3.37 (2.64–4.31) | <0.001 |
Results based on individuals reporting membership of at least one community organization at baseline and again, after 3 years, at follow-up.
*Odds ratio for reporting HTC uptake between survey rounds for community-based organization (CBO) members compared with reports from nonmembers adjusted for other characteristics showing statistically significant (P < 0.1) effects after adjustment for age-group and location.
Uptake of HTC was higher for men in community organizations (15.0%, 11.1–19.7%) than for other men (9.2%, 7.8–10.7%); the difference remaining statistically significant after adjustment for other characteristics associated with testing (Table 2). HTC also was more common for women in community organizations (35.6%, 33.3–38.0%) than among other women (29.6%, 27.5–31.7%). For women, there was evidence for a possible dose effect with 39.3% of the women who participated in more than two types of groups at the beginning and at the end of the study period taking up HTC compared with 35.9, 32.5 and 31.2% for those participating in two types, one type or no type of group, respectively (aOR 1.16, 95% CI 0.97–1.37, P = 0.10). Few men participated in multiple groups (2.3%, 42/1812) and there was no evidence for a dose effect for men.
For men, HTC uptake was higher in those participating in community organizations with and without discussions about care for PLHIV than in those not in community organizations (15.4 versus 9.2%; aOR 1.65, 95% CI 1.00–2.72, P = 0.051; and 14.5 versus 9.2%; 1.70, 1.01–2.86, P = 0.046) (Fig. 1a). For women, the effect was found for women whose organizations discussed care for PLHIV (37.7 versus 29.6%; 1.35, 1.11–1.63, P = 0.002) but not for those whose organizations did not discuss care for PLHIV (32.6 versus 29.6%, P = 0.3).
Fig. 1.
The effects of discussion about care for people living with HIV and external sponsorship of community organizations on uptake of HIV testing and counselling and prevention-of-mother-to-child transmission services, 2003–2008.
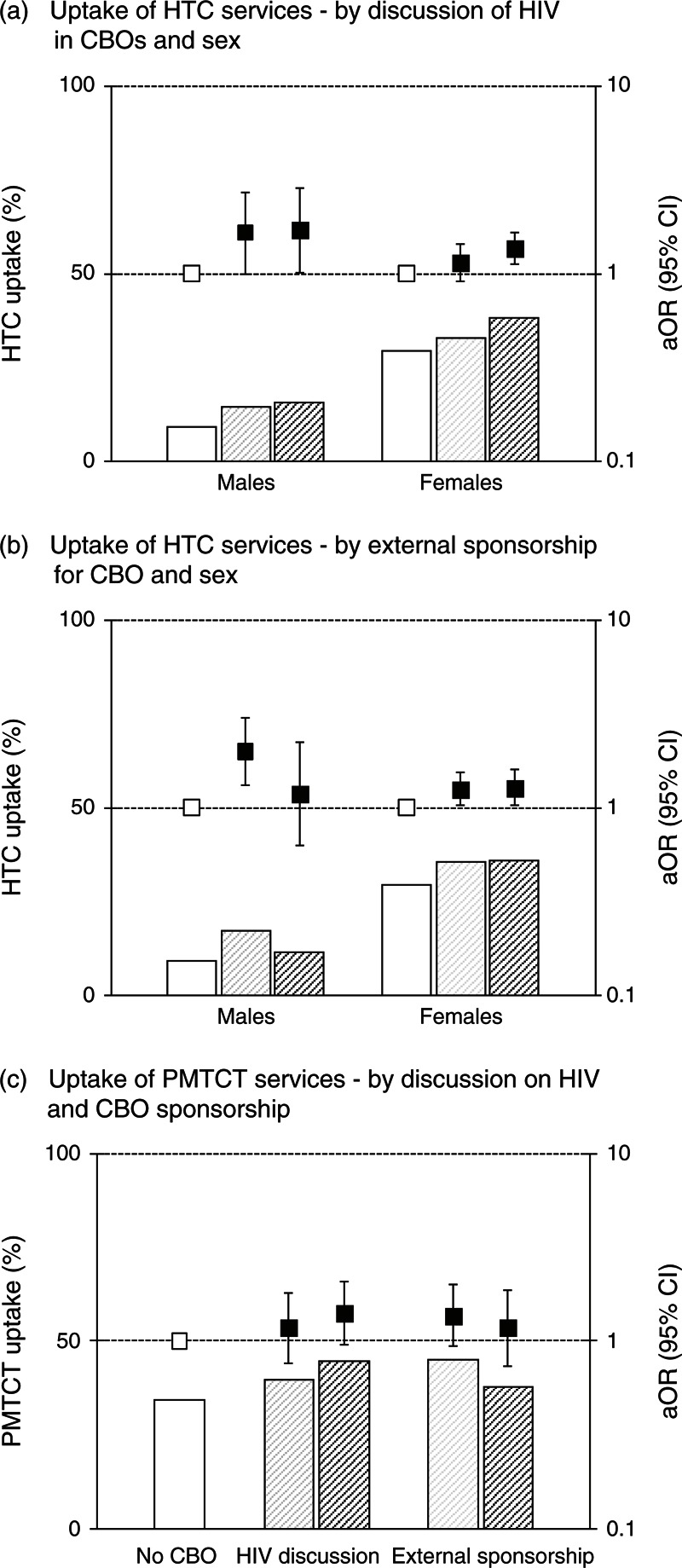
Histograms show the levels of uptake; un-shaded bars – not in a community-based organization (CBO); light-shaded bars – in a CBO without HIV discussions or sponsorship; dark-shaded bars – in a CBO with HIV discussions or sponsorship. aOR, odds ratio adjusted for characteristics with significant effects (P < 0.1) in Table 2 [HIV testing and counselling (HTC)] or Table 3 [prevention-of-mother-to-child transmission (PMTCT)].
HTC uptake was increased for men in community organizations without external sponsorship (17.0 versus 9.2%, 1.98, 1.31–3.00, P = 0.001) but not for men in sponsored organizations (11.5 versus 9.2%, 1.18, 0.63–2.22, P = 0.6) (Fig. 1b). For women, the increase was seen in both unsponsored (35.6 versus 29.6%, 1.25, 1.02–1.53, P = 0.033) and sponsored (35.7 versus 29.6%, P = 0.026) organizations.
Uptake of prevention-of-mother-to-child transmission services
Nine hundred and ninety-three women reported pregnancies during the study period. Of these women, 22 had been pregnant for less than 4 months at the interview date and had no previous pregnancy in the study period. Thus, 971 women were included in the analysis.
Among women with a pregnancy during the study period, 37.2% (95% CI 34.1–40.2%) reported taking up PMTCT. Uptake varied little by age but was lower among women on agricultural estates. PMTCT uptake was higher among Catholics and women with more education but those experiencing greater poverty and HIV infection had lower uptake.
Uptake of PMTCT was higher for women participating in community organizations (42.3%, 37.2–47.6%) than for other women (34.2%, 30.4–38.1%), but the difference ceased to be statistically significant after adjustment for other characteristics associated with PMTCT uptake (aOR 1.30, 95% CI 0.94–1.78, P = 0.11) (Table 3). There was weak evidence for a dose effect with 70.6% of the pregnant women who participated in more than two types of groups at the beginning and at the end of the study period taking up PMTCT compared with 47.8, 42.6 and 33.8% for those participating in two types, one type or no type of group, respectively (aOR 1.41, 0.88–2.25, P = 0.15).
Table 3. Associations between participation in community-based organizations and uptake of prevention-of-mother-to-child transmission services, 2003–2008.
| PMTCT uptake | Test for difference | |||
| Characteristic | n | N (%) | aOR* (95% CI) | P |
| CBO participation | ||||
| Yes | 152 | 359 (42.3) | 1.30 (0.94–1.78) | 0.108 |
| No | 209 | 612 (34.2) | 1 | |
| Age-group | ||||
| 15–19 | 68 | 177 (38.4) | 1 | |
| 20–34 | 252 | 679 (37.1) | 1.02 (0.71–1.47) | 0.92 |
| 35–54 | 41 | 115 (35.7) | 1.02 (0.56–1.82) | 0.97 |
| Residence | ||||
| Village | 178 | 400 (44.5) | 1 | |
| Roadside settlement | 84 | 174 (48.3) | 1.09 (0.71–1.69) | 0.69 |
| Agricultural estate | 45 | 285 (15.8) | 0.28 (0.17–0.44) | <0.001 |
| Small town | 54 | 112 (48.2) | 1.12 (0.66–1.89) | 0.68 |
| School education | ||||
| Primary or none | 72 | 301 (23.9) | 1 | |
| Secondary or higher | 289 | 670 (43.1) | 2.06 (1.47–2.88) | <0.001 |
| Church | ||||
| Protestant | 129 | 330 (39.1) | 1 | |
| Roman Catholic | 75 | 137 (54.7) | 1.76 (1.07–2.87) | 0.025 |
| Apostolic | 98 | 331 (29.6) | 0.94 (0.66–1.35) | 0.75 |
| Pentecostal | 38 | 98 (38.8) | 1.16 (0.71–1.92) | 0.55 |
| Traditional | 14 | 53 (26.4) | 0.99 (0.47–2.09) | 0.98 |
| Other | 7 | 22 (31.8) | 1.52 (0.49–4.69) | 0.47 |
| Marital status | ||||
| Currently married | 270 | 734 (36.8) | – | |
| Never married | 67 | 165 (40.6) | – | |
| Formerly married | 24 | 72 (33.3) | – | |
| Employment status | ||||
| Unemployed | 338 | 888 (38.1) | – | |
| Employed | 23 | 83 (27.7) | – | |
| Poverty tercile | ||||
| Least poor | 138 | 321 (43.0) | 1 | |
| Poor | 115 | 313 (36.7) | 0.73 (0.49–1.08) | 0.114 |
| Poorest | 108 | 337 (32.0) | 0.65 (0.44–0.94) | 0.023 |
| HIV infection status | ||||
| Uninfected | 328 | 844 (38.9) | 1 | |
| Infected | 33 | 127 (26.0) | 0.53 (0.33–0.84) | 0.007 |
| Ever taken up HTC | ||||
| No | 299 | 883 (33.9) | 1 | |
| Yes | 62 | 88 (70.5) | 3.83 (2.24–6.56) | <0.001 |
CBO, community-based organizations; PMTCT, prevention-of-mother-to-child transmission. Results based on individuals reporting membership of at least one community organization at baseline and again, after 3 years, at follow-up.
*Odds ratio for reporting PMTCT uptake between survey rounds for CBO members compared with reports from nonmembers adjusted for other characteristics showing statistically significant (P < 0.1) effects after adjustment for age-group and location.
The association between participation in community organizations and PMTCT uptake was borderline significant for women in groups that discussed HIV (44.5 versus 34.2% for those not in organizations; aOR 1.41, 95% CI 0.96–2.06, P = 0.079) (Fig. 1c). The association with PMTCT uptake was stronger for women in community organizations without external sponsorship (45.0 versus 34.2%; 1.37, 0.94–1.99, P = 0.098) than for women in sponsored organizations (37.7 versus 34.2%; 1.17, 0.73–1.87, P = 0.5).
Village-level effects
Fifty-one villages for men and 140 villages for women had 10 or more participants in the study. No association was found between proportion of men participating in community organizations and HTC uptake (Co-eff 0.058, P = 0.6). For women, greater participation in community organizations was associated with higher HTC uptake (Co-eff 0.213, 95% CI 0.070–0.356, P = 0.004) but the difference reduced after controlling for age, place of residence, education and recent pregnancy (adjusted-Co-eff 0.121, P = 0.081). Greater participation in community organizations was associated with increased uptake of PMTCT among women with a recent pregnancy (adjusted-Co-eff 0.291, 95% CI 0.012–0.570, P = 0.041). PMTCT uptake was higher in the quartile of villages with the greatest participation in community organizations (53.2%, 42.5–63.9%) than in the quartile of villages with the least participation (30.4%, 18.6–42.2%) and was intermediate in the middle two quartiles (Fig. 2).
Fig. 2.
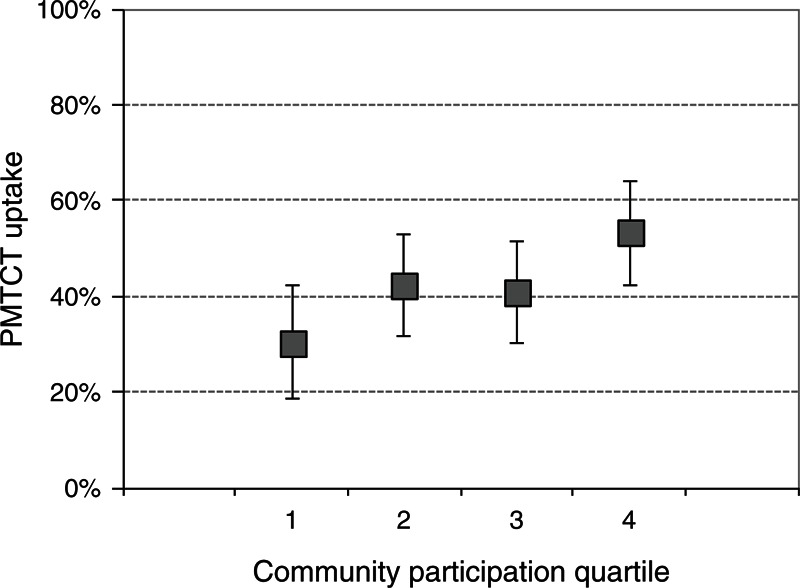
Prevention-of-mother-to-child transmission uptake by proportion of village members participating in community organizations.
Discussion
We investigated the contribution of participation in grassroots community organizations to the early scale-up of HTC and PMTCT services in populations in eastern Zimbabwe with an HIV prevalence of 18% [13,16,17]. We found that more than a third of adults were members of local community organizations and uptake of HTC and PMTCT, over a 3-year interval, was higher in members of community organizations than among nonmembers and also was higher in villages with greater community participation.
Community mobilization through indigenous grassroots organizations could be an effective strategy for increasing uptake of HIV services. However, such mobilization may be more effective when it is initiated by communities themselves rather than (say) by external NGOs. We found the most consistently positive effects in community organizations that had not received sponsorship from an external source. Some organizations that receive external sponsorship in Manicaland are linked to Apostolic churches that emphasize faith healing over medical care [18,19], whereas others undertake activities (e.g. sports and political activities) that can reinforce unhelpful masculine identities and endorse risk [20]. Sponsorship also may lead to reliance on outsiders for leadership and support, undermining community agency in the face of the epidemic. In some instances, sponsorship may result in imposition of externally formulated solutions that do not resonate with the local context [20]. Thus, outside agencies seeking to engage with local community organizations must proceed with sensitivity, so as not to dilute the localism that may be the key to their beneficial effects.
The proportional increase in HTC uptake associated with community participation was greater for men (63%) than for women (20%) in circumstances where more women than men have HIV tests due to sex differences in healthcare seeking behaviour and inclusion of HIV testing within PMTCT services. However, fewer men than women are members of community organizations. For women, the increases in HTC and PMTCT uptake were most evident in community organizations that discussed HIV; a finding that supports social psychology theory on HIV competent communities which suggests that community organizations can provide social spaces for critical dialogue about HIV, exchange of information, and sharing of first-hand experiences of AIDS, which, in turn, can lead to greater uptake of services [18–20]. For men, discussion about HIV was not an important mechanism for increasing HTC uptake among those who participated in community organizations – possibly reflecting the negative effects that dialogue can have in spreading false information and in entrenching unhelpful social norms [20,21].
Strengths of this study include its large general population sample and the availability of data for village-level analysis. The findings were obtained from prospective analyses of longitudinal cohort data in which the effects on outcomes, over the study period, of prior exposure to community organization activities were measured. Therefore, the observed statistical associations are more likely to be causal and to reflect effects of community participation on the study outcomes rather than vice versa than would be the case for results from cross-sectional analyses. However, participation in community organizations is an endogenous variable which is affected by self-selection. Although we adjusted for differences in baseline characteristics including prior uptake of services, unobserved characteristics may have predisposed individuals or communities with greater community participation to have higher uptake of HIV services. Therefore, the results cannot be taken as fully establishing a causal link between participation in community organizations and uptake of these services.
Internationally, various approaches to increasing HTC uptake are being tried to support the roll-out of HIV treatment and prevention programmes. These include couple testing [22], mobile outreach services [23,24], workplace-based testing [25], home-based testing [26,27], self-testing [28,29] and offering monetary incentives [30]. Our findings are consistent with those from previous studies on the value of social capital [11,31], social networks and community mobilization [32] to support externally introduced programmes in African settings. In recent studies, Godlonton and Thornton reported that uptake of clinic-based VCT increased uptake amongst neighbours in Malawi [30], and Sweat and colleagues found that mobile VCT services, backed up by community mobilization and support activities, increased uptake of HTC in Tanzania, Zimbabwe and Thailand [23]. However, to our knowledge, this is the first study to provide evidence for a causal link between spontaneous community responses to HIV and greater uptake of HTC.
In Zimbabwe, substantial increases in uptake of HTC (from 580 000 to 1.1 m) and PMTCT (from 15 to 59%) occurred between 2006 and 2008 [14]. Nonetheless, uptake of HTC remains worryingly low – in a 2010/2011 national survey, 57% of women and 36% of men reported having ever had an HIV test [33]. Our results, which span the initial scale-up of HTC and PMTCT services, suggest that community organizations contributed to the early increases in uptake and lend support for the country's plans for greater community engagement in HIV control activities [14]. Specialist AIDS groups had low uptake (less than one percent (0.7%) for men and 3.8% for women); thus, integrating HIV discussions into other groups seems more popular and may be more acceptable than establishing dedicated AIDS groups. However, our findings emphasize that correct information needs to be made available to these groups and that any external support must be provided sensitively. Similar approaches could be considered elsewhere since grassroots organizations have the potential to play a greater part in HIV control activities in most countries [34].
Acknowledgements
S.G., C.A.N., L.S., O.M. and C.C. contributed substantially to the conceptualization and design of the study. C.A.N. and S.G. organized the data collection. S.G. undertook the data analysis. S.G., C.C. and L.S. drafted and edited the manuscript. S.G., C.A.N., L.S., O.M. and C.C. contributed to the interpretation of findings and approved the final version.
We are grateful to the Wellcome Trust for funding this research and the World Bank, DFID and UNAIDS who funded the writing of this paper, prepared as part of the ‘Evaluation of the Community Response to HIV and AIDS’. We also thank the Manicaland HIV/STD Prevention Project team and the local communities in Manicaland, Zimbabwe for their assistance with this work.
Sources of financial support: World Bank, Wellcome Trust, DFID and UNAIDS.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Correspondence to Simon Gregson, Department of Infectious Disease Epidemiology, Imperial College London School of Public Health, London, UK. E-mail: Sajgregson@aol.com
References
- 1.UNAIDS HIV Voluntary counselling and testing: a gateway to prevention and care. Five case studies related to prevention of mother-to-child transmission of HIV, tuberculosis, young people, and reaching general population groups. UNAIDS Best Practice Collection. Geneva, Switzerland: UNAIDS; 2002. 100 [Google Scholar]
- 2.UNAIDS Universal access to HIV prevention, treatment, care and support from countries to regions to the high level meeting on AIDS and beyond. Geneva, Switzerland: UNAIDS; 2011. 16 [Google Scholar]
- 3.Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011; 365:493–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Granich RM, Gilks CF, Dye C, De Cock KM, Williams B. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet 2009; 373:48–57 [DOI] [PubMed] [Google Scholar]
- 5.UNAIDS, World Health Organisation UNAIDS/WHO policy statement on HIV testing. Geneva, Switzerland: UNAIDS; 2004 [Google Scholar]
- 6.World Health Organisation, UNAIDS, UNICEF Global HV/AIDS response - Epidemic update and health sector progress towards Universal Access: 2011 Progress Report. Geneva, Switzerland: World Health Organisation; 2011. 233 [Google Scholar]
- 7.MEASURE DHS HIV/AIDS Survey indicators Database. 2012. Voluntary counselling and testing statistics. [Google Scholar]
- 8.Schwartlander B, Stover J, Hallet TB, Atun R, Avila C, Gouws E, et al. Towards an improved investment approach for an effective response to HIV/AIDS. Lancet 2011; 377:2031–2041 [DOI] [PubMed] [Google Scholar]
- 9.World Health Organisation Service delivery approaches to HIV testing and counselling (HTC): a strategic HTC policy framework. Geneva, Switzerland: World Health Organisation; 2012. 75 [Google Scholar]
- 10.Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med 2003; 57:13–24 [DOI] [PubMed] [Google Scholar]
- 11.Gregson S, Mushati P, Grusin H, Nhamo M, Schumacher C, Skovdal M, et al. Social capital and reduced female vulnerability to HIV infection in rural Zimbabwe. Popul Dev Rev 2011; 37:333–359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gregson S, Nhamo M, Campbell C. Community group membership and stigmatising attitudes towards people living with HIV in eastern Zimbabwe. AIDS Impact. Santa Fe; 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gregson S, Garnett GP, Nyamukapa CA, Hallett TB, Lewis JJC, Mason PR, et al. HIV decline associated with behaviour change in eastern Zimbabwe. Science 2006; 311:664–666 [DOI] [PubMed] [Google Scholar]
- 14.Zimbabwe National AIDS Council Zimbabwe National HIV and AIDS Strategic Plan 2011–2015 [ZANSP II]. Harare, Zimbabwe: Zimbabwe National AIDS Council; 2011 [Google Scholar]
- 15.Lopman B, Lewis JJC, Nyamukapa CA, Mushati P, Chandiwana SK, Gregson S. HIV incidence and poverty in Manicaland, Zimbabwe: is HIV becoming a disease of the poor?. AIDS 2007; 21:S57–S66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gregson S, Nyamukapa CA, Lopman B, Mushati P, Garnett GP, Chandiwana SK, et al. A critique of early models of the demographic impact of HIV/AIDS in sub-Saharan Africa based on empirical data from Zimbabwe. Proc Natl Acad Sci 2007; 104:14586–14591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lopman B, Nyamukapa CA, Mushati P, Wambe M, Mupambireyi Z, Mason PR, et al. Determinants of HIV incidence after 3 years follow-up in a cohort recruited between 1998 and 2000 in Manicaland, Zimbabwe. Int J Epidemiol 2008; 37:88–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daneel ML. Bourdillon MFC. The growth and significance of Shona Independent Churches. Christianity south of the Zambezi: Volume II. Gweru, Zimbabwe:Mambo Press; 1977. 177–192 [Google Scholar]
- 19.Gregson S, Zhuwau T, Anderson RM, Chandiwana SK. Apostles and Zionists: the influence of religion on demographic change in rural Zimbabwe. Popul Stud 1999; 53:179–193 [DOI] [PubMed] [Google Scholar]
- 20.Skovdal M, Campbell C, Madanhire C, Mupambireyi Z, Nyamukapa CA, Gregson S. Masculinity as a barrier to men's uptake of HIV services in Zimbabwe. Global Health 2011; 7:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Campbell C, Scott K, Nhamo M, Nyamukapa CA, Madanhire C, Skovdal M, et al. Social capital and HIV Competent Communities: the role of community groups in managing HIV/AIDS in rural Zimbabwe. AIDS Care. doi: 10.1080/09540121.2012.748170. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Desgrees du Lou A, Orne-Gliemann J. HIV serodiscordance in heterosexual couples and the need for couple-centred HIV counselling and testing approaches. Reproduct Health Matters 2008; 16:151–161 [DOI] [PubMed] [Google Scholar]
- 23.Sweat M, Morin SF, Celentano DD, Mulawa M, Singh B, Mbwambo J, et al. Community-based intervention to increase HIV testing and case detection in people aged 16-32 years in Tanzania, Zimbabwe, and Thailand (NIMH Project Accept, HTPN 043): a randomised study. Lancet Infect Dis 2011; 11:525–532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morin SF, Khumaol-Satutukwa G, Charlebois ED. Removing barriers to knowing HIV status: same-day mobile HIV testing in Zimbabwe. J Acquir Immune Defic Syndr 2006; 41:218–224 [DOI] [PubMed] [Google Scholar]
- 25.Corbett EL, Dauya E, Matambo R, Cheung YB, Makamure B, Bassett MT, et al. Uptake of workplace HIV counselling and testing: a cluster-randomised trial in Zimbabwe. Public Library Sci Med 2006; 3:e238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Negin J, Wariero J, Mutuo P, Jan S, Pronyk P. Feasibility, acceptability and cost of home-based HIV testing in rural Kenya. Trop Med Int Health 2009; 14:849–855 [DOI] [PubMed] [Google Scholar]
- 27.Helleringer S, Kohler H-P, Frimpong JA, Mkandawire J. Increasing uptake of HIV tsting and counelling among the poorest in sub-Saharan African countries through home-based service provision. J Acquir Immune Defic Syndr 2009; 51:185–193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Choko AT, Desmond N, Webb EL, Chavula K, Napierala-Mavedzenge S, Gaydos CA, et al. The uptake and accuracy of oral kits for HIV self-testing in high HIV prevalence setting: a cross-sectional feasibility study in Blantyre. Malawi Public Library Sci Med 2011; 8:e1001102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spielberg F, Levine RO, Weaver M. Self-testing for HIV: a new option for HIV prevention?. Lancet Infect Dis 2004; 4:640–646 [DOI] [PubMed] [Google Scholar]
- 30.Godlonton S, Thornton R. Peer effects in learning HIV results. J Dev Economics 2012; 97:118–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ware NC, Idoko J, Kaaya S, Biraro IA, Wyatt MA, Agbaji O, et al. Explaining adherence success in sub-Saharan Africa: an ethnographic study. Public Library Sci Med 2009; 6:e1000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Parker RG. Empowerment, community mobilization and social change in the face of HIV/AIDS. AIDS 1996; 10:S27–S32 [PubMed] [Google Scholar]
- 33.Zimbabwe Central Statistical Office Zimbabwe demographic and health survey, 2010–2011. Harare, Zimbabwe: Zimbabwe Central Statistical Office and Macro International; 2012 [Google Scholar]
- 34.Rodriguez-Garcia R, Bonnel R, Wilson D, N’Jie N. Investing in communities achieves results: findings from an evaluation of community responses to HIV and AIDS. Washington DC:The World Bank; 2013 [Google Scholar]


