Abstract
Purpose
Burn-out syndrome (BOS) has frequently been reported in healthcare workers, and precipitating factors include communication problems in the workplace, and stress related to end-of-life situations. We evaluated the effect of an intensive communication strategy on BOS among caregivers working in intensive care (ICU).
Methods
Longitudinal, monocentric, before-and-after, interventional study. BOS was evaluated using the Maslach Burnout Inventory (MBI) and depression using the Centre for Epidemiologic Studies Depression Scale (CES-D) in 2007 (period 1) and 2009 (period 2). Between periods, an intensive communication strategy on end-of-life practices was implemented, based on improved organisation, better communication, and regular staff meetings.
Results
Among 62 caregivers in the ICU, 53 (85%) responded to both questionnaires in period 1 and 49 (79%) in period 2. We observed a significant difference between periods in all three components of the MBI (emotional exhaustion, p=0.04; depersonalization p=0.04; personal accomplishment, p=0.01). MBI classified burnout as severe in 15 (28%) caregivers in period 1 vs 7 (14%) in period 2, p<0.01, corresponding to a 50% risk reduction. Symptoms of depression as evaluated by the CES-D were present in 9 (17%) caregivers in period 1 vs 3 (6%) in period 2, p<0.05, corresponding to a risk reduction of almost 60%.
Conclusion
The implementation of an active, intensive communication strategy regarding end-of-life care in the ICU was associated with a significant reduction in the rate of burn-out syndrome and depression in a stable population of caregiving staff.
Keywords: Adult; Female; France; Hospitals, University; Humans; Intensive Care Units; Interdisciplinary Communication; Male; Medical Staff, Hospital; psychology; Middle Aged; Questionnaires; Stress, Psychological; prevention & control; Terminal Care; Young Adult
Keywords: ethics, critical care organisation, communication
Introduction
Burn-out syndrome (BOS) among health professionals was first described in the 1970s, and corresponds to an inability to cope with emotional stress at work, or an excessive expenditure of energy accompanied by a feeling of failure and exhaustion [1–3]. The most common symptoms of BOS are fatigue, headaches, eating disorders, insomnia, irritability, emotional instability, and excessive rigidity in interpersonal relations.
Wide variations in symptoms of BOS have been reported in different categories of healthcare workers [4–6], and it would appear that it is particularly frequent among doctors [7] and nurses [8] in the setting of critical care. In one multicentre French study of 2,392 nurses [8], BOS was classified as severe in 33% of participants, and predictive factors included age, organisational factors (choice of days off…), communication problems with hierarchy (head nurse, doctors), a high number of end-of-life decisions and caring for dying patients. Factors protective against BOS included participation in ICU research groups, and good quality working relations. A similar study among doctors [7] reported a prevalence of severe BOS of 46.5%, and the predictive factors identified in this study were a heavy workload or conflicts with colleagues and/or nurses, whereas good relations with the caregiving team was a protective factor.
The consequences of BOS are manifold and can be harmful for both the caregiver themselves, and the patients, with decreased well-being of caregiving staff leading to diminished quality of care [9–10] and poor communication with patients and families [11], high societal costs related to absenteeism and high turnover rates [12]. BOS is often reported to have its basis in communication problems, particularly in end-of-life situations [13–14], and we hypothesized that an improvement in communication could help to alleviate the symptoms and consequences of BOS.
Therefore, we performed a longitudinal, before-and-after, interventional study to investigate whether an intensive communication strategy regarding end-of-life practices would have an influence on the incidence of burn-out syndrome in healthcare workers in critical care.
The results of this study were presented in part at the annual congress of the European Society of Intensive Care Medicine, Barcelona, September 2010.
Methods
This monocentric study was performed over two periods, with an initial evaluation of BOS performed in early 2007 (period 1) before the implementation of the intensive communication strategy, and a second evaluation in the second semester 2009 (period 2). The institutional review board (Comité de Protection des Personnes, Dijon) approved the protocol and all participants gave informed consent.
All caregivers who agreed to participate received a questionnaire in a sealed envelope to be completed and returned anonymously to the lead investigator. No data were recorded on caregivers who declined to participate.
Between the 2 phases of the study, our healthcare team (physicians, nurses, nurses’ aids, psychologist) developed an intensive strategy for communication regarding end-of-life practices in the intensive care unit (ICU). In a preliminary study [15], clinical interviews were performed with caregivers by 2 hospital psychologists in order to identify the individual components of BOS and identify areas for intervention. The communication strategy was then developed from this preliminary study, based on the questions more frequently reported to arise in the context of end-of-life decisions in the critical care unit. The main objective of this strategy was to improve communication between the triad of caregivers, patients and patients’ families, in the aim of alleviating stress for the caregivers. The communication strategy was phased into routine practice over a period of 6 months.
The communication strategy and related structural organisation within the department is described in Table 1. In addition, caregivers were encouraged to participate in working groups or brainstorming groups within the ICU with a view to improving delivery of care and management of conflicts. All staff also participated regularly in congresses and meetings to remain abreast of latest developments and improve quality of care. These two approaches (working groups, conference participation) were both innovative for our unit, where such outside activities were not previously common.
Table 1.
Description of the elements comprising the intensive communication strategy regarding end-of-life practices implemented in the intensive care unit
Organisation:
|
Communication:
|
Data Collection
For all participating healthcare workers, we recorded the following data : age; sex; marital status; number of children; professional status (physician, nurse, nurse’s aid); number of years in practice since qualification; number of years experience in critical care; working rhythm (days only, nights only, days and nights).
To evaluate BOS, we used the Maslach Burnout Inventory (MBI) and the Centre for Epidemiologic Studies Depression Scale (CES-D) to evaluate symptoms of depression.
The MBI is a 22-item questionnaire evaluating three domains of burnout, namely the emotional exhaustion subscale (9 items), assessing feelings of being emotionally overextended and exhausted by one’s work; the depersonalization subscale (5 items), measuring an unfeeling and impersonal response toward recipients of one’s service, care, or treatment; and a personal accomplishment subscale (8 items); assessing feelings of competence and successful achievement in one’s work with people. The scoring method used was the standard scoring method suggested by the developers. Severe burnout was defined as a score >30 on the emotional exhaustion subscale, or a score >12 on the depersonalisation subscale, or a score <33 on the personal accomplishment subscale, or a high total score [7–8, 16].
The CES-D scale evaluates symptoms of depression through 20 questions that cover domains including self-deprecation, somatic problems, sadness, apathy and persecution) [17].
Statistical analysis
Quantitative variables are presented as median [Interquartile range] and categorical variables as number (percentage). Quantitative variables were compared using the Wilcoxon test and categorical data with the Chi square test or Fisher’s exact test as appropriate. All tests were two-tailed and a p-value <0.05 was considered statistically significant. All analyses were performed using SAS version 9.1 (SAS Institute, Cary, NC, USA).
Results
Among 62 healthcare workers employed in the critical care department of our University Hospital, 53 (85%) responded to both questionnaires (MBI and CES-D) in period 1, and 49 (79%) in period 2. No questionnaire was excluded because of missing data. The main characteristics of respondents in both periods are described in table 2. In both periods, the majority of respondents were nurses (29 (55%) nurses, 20 (38%) nurses’ aids, 4 (7%) physicians in period 1; 27 (55%) nurses, 18 (37%) nurses’ aids, 4 (8%) physicians in period 2). Median age [Interquartile range] was 27 [23–38] in period 1 and 26 [22–38] in period 2. The majority of participants had <5 years experience in the ICU (33 (63%) in period 1 vs 32 (65%) in period 2).
Table 2.
Characteristics of respondents in both study periods
| Variable | Period 1 (n=53) | Period 2 (n=49) |
|---|---|---|
| Age, yrs | ||
| Median | 27 | 26 |
| Interquartile range | 23–38 | 22–38 |
| Age group | ||
| 20–30 | 14 (26) | 15 (31) |
| 30–40 | 18 (34) | 17 (35) |
| 40–50 | 15 (29) | 14 (28) |
| > 50 | 6 (11) | 3 (6) |
| Women, n (%) | 40 (75) | 36 (73) |
| Professional status, n (%) | ||
| Nurses | 29 (55) | 27 (55) |
| Nursing assistants | 20 (38) | 18 (37) |
| Physicians | 4 (7) | 4 (8) |
| Marital status n (%) | ||
| Married | 29 (55) | 26 (53) |
| Single | 19 (36) | 19 (44) |
| Divorced | 5 (9) | 4 (8) |
| Number of children, n (%) | ||
| 0 | 27 (51) | 27 (55) |
| 1 | 16 (31) | 13 (27) |
| 2 | 5 (9) | 4 (8) |
| 3 or more | 5 (9) | 5 (10) |
| Years experience since qualification, n (%) | ||
| < 5 | 18 (35) | 17 (35) |
| 5–10 | 23 (43) | 21 (43) |
| >10 | 12 (22) | 11 (22) |
| Years experience in ICU, n (%), | ||
| < 5 | 27 (51) | 27 (55) |
| 5–10 | 15 (28) | 14 (29) |
| >10 | 11 (21) | 8 (16) |
| Working rhythm | ||
| Day only | 10 (18) | 9 (18) |
| Night only | 9 (17) | 9 (18) |
| Day and night | 34 (65) | 31 (64) |
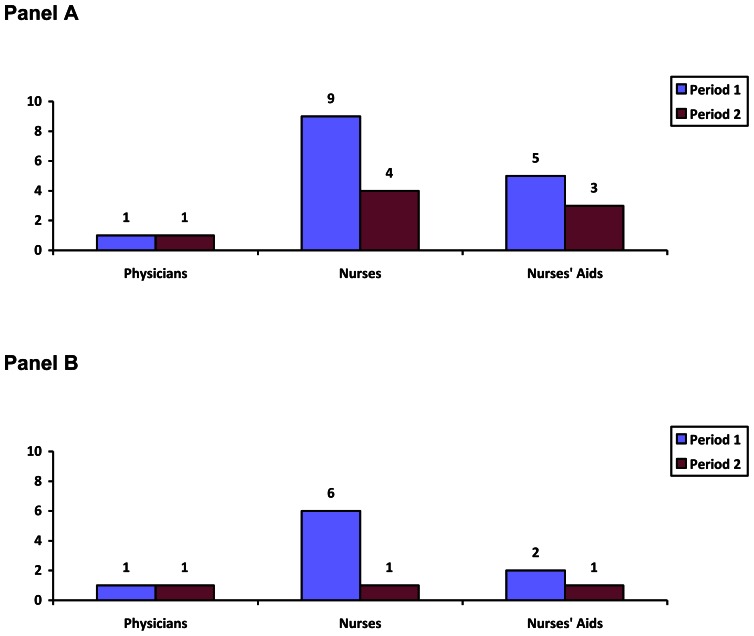
The results of the MBI and CES-D questionnaires are presented in table 3. We observed a significant difference between periods in all three components of the MBI. MBI classified burnout as severe in 15 (28%) caregivers (9 nurses, 5 nurses’ aids, 1 physician) in period 1, and in 7 (14%) in period 2 (4 nurses, 3 nurses’ aids, 1 physician), p<0.01 (figure 1, panel A). This corresponds to a reduction of 50% in the relative risk of BOS between periods. All respondents with a high CES-D score also presented severe BOS.
Table 3.
Results of the Maslach Burnout Inventory and CES-D in both periods
| Period 1 (n=53) | Period 2 (n=49) | P | |
|---|---|---|---|
| MBI# | |||
| Emotional exhaustion | 33.4±4.5 | 26.5±3.9 | 0.04 |
| Depersonalization | 13.5±5.3 | 9.4±2.7 | 0.04 |
| Personal accomplishment | 35.4± 4.8 | 41.5±5.8 | 0.01 |
| CES-D# n (%) | 9 (17) | 3 (6) | 0.03 |
Figure 1.
Number of physicians, nurses and nurses’ aids with a high score on the Maslach Burnout Index (panel A) and high CES-D score (panel B) in periods 1 and 2.
Symptoms of depression as evaluated by the CES-D were present in 9 (17%) caregivers in period 1 (6 nurses, 2 nurses’ aids, 1 physician) vs 3 (6%) in period 2 (1 nurse, 1 nurse’s aid, 1 physician), p<0.05 (figure 1, panel B). The difference in CES-D between periods was statistically significant, representing a reduction of approximately 60% in the relative risk.
There was no difference in overall mortality rate in the ICU between periods (21% mortality in the ICU in period 1 vs 23% in period 2, p = NS).
Discussion
The main finding of this study is that the implementation of an intensive communication strategy regarding end-of-life practices in the ICU was associated with a reduction in the relative risk of severe BOS by 50% as measured by the MBI, and a reduction the relative risk of depression by 60%, as evaluated by the CES-D. To the best of our knowledge, this is the first longitudinal, before-and-after study to evaluate the effects of interventions aiming to reduce burnout among ICU caregiving staff.
Wide variations in the prevalence of BOS in healthcare professionals have been reported across specialities, both in doctors [18] and in nurses [19]. The perceived workplace climate and workload have been shown to contribute to BOS [20]. Higher levels of severe BOS have been reported in oncologists [21], anaesthesiologists [22], physicians caring for patients with AIDS [23], and physicians working in emergency departments [24].
ICUs are characterized by a high level of work-related stress [25], a factor known to increase the risk of BOS [26]. Burn-out syndrome can be difficult to identify and recognise. The results of our study underline the importance of the MBI to evaluate the level of work-related stress and suffering among caregivers.
In a study concerning 253 members the Section of Internal Medicine of the Society of Critical Care Medicine, Guntupalli reported that among the MBI subscales, the average emotional exhaustion subscale score was 22.2± 9.5, average depersonalization score was 7.1± 5.1, and average personal accomplishment score was 30.9± 6.4 [27]. In our study, the average value on all these subscales was higher, regardless of the study period under consideration, showing that although the level of stress may have been higher in our cohort, this was compensated by a greater feeling of personal achievement. This could explain why some caregivers continue to work in this stressful environment.
In a French study concerning 306 general practitioners, the emotional exhaustion subscale score was 21.9± 12.4, the depersonalization score was 9.1±6.7, and the personal achievement score was 38.7±7.1 [28]. These figures are similar to those observed in our study on the latter two scales, whereas the mean emotional exhaustion observed in our study was considerably higher, perhaps related to the high number of stressful end-of-life situations encountered in critical care.
Almost one-half of intensivists presented a high level of BOS in the one-day study in a sample of French ICUs performed by Embriaco et al [7], and one third of nursing staff had severe BOS in a similar study by Poncet [8]. In our study, the low number of participating physicians precludes any formal conclusions regarding the prevalence of BOS among this category of healthcare worker, although we did observe BOS among 28% of nursing staff. These results highlight how the ICU is a highly stressful work environment and may, therefore, be associated with a high rate of BOS in staff members [25, 29].
Based on the predictive factors of BOS in critical care previously identified in the literature [7–8], such as organisational factors, communication problems in end-of-life situations, and conflicts in the workplace, we developed a BOS prevention programme by introducing a detailed strategy of intensive communication. In a preliminary study [15], clinical interviews were performed with caregivers by 2 hospital psychologists in order to identify the individual components of BOS in our department, and based on the feedback from these interviews, it became clear that three main areas were suitable for intervention.
The first objective was to reduce, as much as possible, the « stressors » in the working environment, in both organisational and institutional terms. We attempted to improve the integration of the workplace organisation with personal organisation (such as work schedules and family commitments), improve communication between the caregiving team, foster a climate of confidence, ensure that the hierarchical superiors were available to listen and be consulted, and to improve manifestations of gratitude on the part of our institution. The second main axis of our communication strategy was focused on each individual, and personal strategies for coping. The death of a young patient, or patients with whom the staff member had considerable personal or emotional investment, strong identification with patients or their close family, accompanying families in difficult times, and the rapport with the patient’s body were just some of the points raised by the caregiving staff. In this context, the support of staff psychologists is extremely helpful for all the staff of the ICU. Psychological adjustments for the most difficult situations helped each staff member, according to their personality, to adapt their defence strategies in order to better deal with such situations, thus reducing the ensuing stress.
The third and final orientation of our intensive communication strategy was a collective, multidisciplinary approach. The suffering of the ICU caregivers is at the crossroads of a range of areas for reflection in medical, psychological, ethical, social and ergonomic terms. When caregivers are questioned about sources contributing to their suffering, initial responses relating to the volume of work and under-staffing rapidly give way to more philosophical questions about the overall meaning of their work, hopeless therapeutic cases, ethical questions on end-of-life matters, and quality of life. This reflection on the meaning of care was given particular attention in our department, so that the suffering endured by both caregivers and patients and their families would be given precedence. Giving greater meaning to the work of the caregivers may have contributed to the increased level of personal accomplishment observed in our study, as measured on the MBI subscale. The implementation of this active communication strategy made it possible to significantly reduce both the number of caregivers with BOS, as measured by the emotional exhaustion and depersonalization subscales of the MBI, but also to significantly increase the feeling of personal achievement.
Several perspectives exist that have the potential to improve BOS, and we tried to implement these to the best of our ability. The following are just some examples:
Improving communication within the triad of the caregiving team, the patient and the patient’s family. This requires constant effort on a 24/7 basis.
Orienting care towards the patient as a person, without any judgement or prejudice.
Facilitating access to physicians for patients’ families, and reception of families within the department, to demystify the caregiving activity in the ICU and help involve the family in the care of their relative.
Developing palliative care, with dedicated reference personnel within the ICU.
Improving psychological management for all concerned (i.e. caregivers, patients, families), with ICU-based psychologists.
Widening the scope for continuing medical education and training for the caregiving staff, oriented towards ethics of care and end-of-life practices.
Implementing standardised protocols and guidelines to be reviewed regularly by audits, in order to standardise quality of care. Random samples of patient files are regularly monitored within our hospital to verify the completeness of documentation as regards end-of-life practices, as required in the framework of a new programme for the evaluation of professional practices introduced into French legislation in 2004.
Strengths and Weaknesses of the Study
One of the main strong points of this study was the high level of participation among the staff in both periods. The project was strongly supported and even solicited by the staff members. The communication strategy was developed after interviews between the staff members and psychologists, and after several training courses in end-of-life ethics. Furthermore, there was very little turnover in the staff between periods, with 95% of all staff members present in both periods. We aimed in particular to work on preventive strategies for BOS (such as debriefing and psychological coping strategies for difficult situations) rather than curative measures.
Conversely, the limitations of this work include the fact that it was a monocentric study with a small sample size. In particular, the observation that nurses presented more frequently with BOS or depression than doctors is likely due to the low number of participating physicians as compared to nurses. We did not evaluate predictive factors for BOS in our population. Other confounding factors could have influenced our results, since the study took place over a period of 2 years, and we cannot exclude that other changes in work conditions may have occurred during this time, independently of our study measures. Similarly, symptoms of burnout may have changed over time without any relation to the intervention under study. We evaluated the level of suffering as measured by burn-out and depression, although these two measures alone are likely insufficient to fully apprehend professional suffering. Further investigations are warranted to explore more fully all the factors that comprise suffering in the workplace. Lastly, it should be noted that the same population was studied in both study periods, thus the results are not independent.
Conclusions
The implementation of an active, intensive communication strategy regarding end-of-life care in the ICU was associated with a reduction in the rate of burn-out syndrome and depression among a stable population of healthcare professionals. These preliminary data warrant confirmation in a larger population.
References
- 1.Freudenberger HJ. The issues of staff burnout in therapeutic communities. J Psychoactive Drugs. 1986;18:247–251. doi: 10.1080/02791072.1986.10472354. [DOI] [PubMed] [Google Scholar]
- 2.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 3.Pines A, Maslach C. Characteristics of staff burnout in mental health settings. Hosp Community Psychiatry. 1978;29:233–237. doi: 10.1176/ps.29.4.233. [DOI] [PubMed] [Google Scholar]
- 4.Blenkin H, Deary I, Sadler A, Agius R. Stress in NHS consultants. BMJ. 1995;310:534. doi: 10.1136/bmj.310.6978.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caplan RP. Stress, anxiety, and depression in hospital consultants, general practitioners, and senior health service managers. BMJ. 1994;309:1261–1263. doi: 10.1136/bmj.309.6964.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coomber S, Todd C, Park G, Baxter P, Firth-Cozens J, Shore S. Stress in UK intensive care unit doctors. Br J Anaesth. 2002;89:873–881. doi: 10.1093/bja/aef273. [DOI] [PubMed] [Google Scholar]
- 7.Embriaco N, Azoulay E, Barrau K, Kentish N, Pochard F, Loundou A, Papazian L. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med. 2007;175:686–692. doi: 10.1164/rccm.200608-1184OC. [DOI] [PubMed] [Google Scholar]
- 8.Poncet MC, Toullic P, Papazian L, Kentish-Barnes N, Timsit JF, Pochard F, Chevret S, Schlemmer B, Azoulay E. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med. 2007;175:698–704. doi: 10.1164/rccm.200606-806OC. [DOI] [PubMed] [Google Scholar]
- 9.Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358–367. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 10.Thomas NK. Resident burnout. JAMA. 2004;292:2880–2889. doi: 10.1001/jama.292.23.2880. [DOI] [PubMed] [Google Scholar]
- 11.Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114:513–519. doi: 10.1016/s0002-9343(03)00117-7. [DOI] [PubMed] [Google Scholar]
- 12.Ackerman AD. Retention of critical care staff. Crit Care Med. 1993;21:S394–395. doi: 10.1097/00003246-199309001-00063. [DOI] [PubMed] [Google Scholar]
- 13.Ferrand E, Lemaire F, Regnier B, Kuteifan K, Badet M, Asfar P, Jaber S, Chagnon JL, Renault A, Robert R, Pochard F, Herve C, Brun-Buisson C, Duvaldestin P. Discrepancies between perceptions by physicians and nursing staff of intensive care unit end-of-life decisions. Am J Respir Crit Care Med. 2003;167:1310–1315. doi: 10.1164/rccm.200207-752OC. [DOI] [PubMed] [Google Scholar]
- 14.Puntillo KA, McAdam JL. Communication between physicians and nurses as a target for improving end-of-life care in the intensive care unit: challenges and opportunities for moving forward. Crit Care Med. 2006;34:S332–340. doi: 10.1097/01.CCM.0000237047.31376.28. [DOI] [PubMed] [Google Scholar]
- 15.Chahraoui K, Bioy A, Cras E, Gilles F, Laurent A, Valache B, Quenot JP. Psychological experience of health care professionals in intensive care unit: A qualitative and exploratory study. Ann Fr Anesth Reanim. 2011;30:342–348. doi: 10.1016/j.annfar.2011.01.020. [DOI] [PubMed] [Google Scholar]
- 16.Canouï P, Mauranges A. Le burn out: le syndrome d’épuisement professionel des soignants. Editions Masson; Paris: 2004. [Google Scholar]
- 17.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 18.Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet. 1996;347:724–728. doi: 10.1016/s0140-6736(96)90077-x. [DOI] [PubMed] [Google Scholar]
- 19.Lu H, While AE, Barriball KL. Job satisfaction among nurses: a literature review. Int J Nurs Stud. 2005;42:211–227. doi: 10.1016/j.ijnurstu.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 20.McManus IC, Keeling A, Paice E. Stress, burnout and doctors’ attitudes to work are determined by personality and learning style: a twelve year longitudinal study of UK medical graduates. BMC Med. 2004;2:29. doi: 10.1186/1741-7015-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lyckholm L. Dealing with stress, burnout, and grief in the practice of oncology. Lancet Oncol. 2001;2:750–755. doi: 10.1016/S1470-2045(01)00590-3. [DOI] [PubMed] [Google Scholar]
- 22.Nyssen AS, Hansez I, Baele P, Lamy M, De Keyser V. Occupational stress and burnout in anaesthesia. Br J Anaesth. 2003;90:333–337. doi: 10.1093/bja/aeg058. [DOI] [PubMed] [Google Scholar]
- 23.Lert F, Chastang JF, Castano I. Psychological stress among hospital doctors caring for HIV patients in the late nineties. AIDS Care. 2001;13:763–778. doi: 10.1080/09540120120076922. [DOI] [PubMed] [Google Scholar]
- 24.Weibel L, Gabrion I, Aussedat M, Kreutz G. Work-related stress in an emergency medical dispatch center. Ann Emerg Med. 2003;41:500–506. doi: 10.1067/mem.2003.109. [DOI] [PubMed] [Google Scholar]
- 25.Donchin Y, Seagull FJ. The hostile environment of the intensive care unit. Curr Opin Crit Care. 2002;8:316–320. doi: 10.1097/00075198-200208000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Bakker AB, Le Blanc PM, Schaufeli WB. Burnout contagion among intensive care nurses. J Adv Nurs. 2005;51:276–287. doi: 10.1111/j.1365-2648.2005.03494.x. [DOI] [PubMed] [Google Scholar]
- 27.Guntupalli KK, Fromm RE., Jr Burnout in the internist--intensivist. Intensive Care Med. 1996;22:625–630. doi: 10.1007/BF01709737. [DOI] [PubMed] [Google Scholar]
- 28.Cathebras P, Begon A, Laporte S, Bois C, Truchot D. Burn out among French general practitioners. Presse Med. 2004;33:1569–1574. doi: 10.1016/s0755-4982(04)98994-4. [DOI] [PubMed] [Google Scholar]
- 29.Soupios MA, Lawry K. Stress on personnel working in a critical care unit. Psychiatr Med. 1987;5:187–198. [PubMed] [Google Scholar]