Abstract
Objective
To determine if the addition of nurse case managers (NCMs) trained in motivational interviewing (MI) to usual care would result in improved outcomes in high risk type 2 diabetes patients.
Methods
A 2-year randomized controlled pragmatic trial randomized 545 patients to usual care control (n=313) or those who received the intervention (n= 232) with additional practice embedded NCM care, including MI-guided behavior change counseling. NCMs received intensive MI training with ongoing fidelity assessment.
Results
Systolic BP was better in the intervention group (131±15.9 vs. 135±18.2, p < 0.05). HbA1c, LDL, and diastolic BP improved in both groups: HbA1c (control group 9.1% to 8.0%, intervention group 8.8% to 7.8%), LDL (control group 127 to 100 mg/dL, intervention group 128 to 102 mg/dL), diastolic BP (control group 78 to 74 mm Hg, intervention group 80 to 74 mm Hg). Depression symptom scores were better in the intervention group. The reduction in diabetes-related distress approached statistical significance.
Conclusions
NCMs and MI improved systolic BP and complications screening. The large decrease in HbA1C and LDL in the control group may have obscured any further intervention effect. Although nurses prompted providers for medication titration, strategies to reduce provider clinical inertia might also be needed.
Significant findings of the study
In patients with type 2 diabetes, an intervention with nurse case management and motivational interviewing improves systolic blood pressure, depression, and screening for complications.
What this study adds
First study to look at the benefit of the addition of motivational interviewing to nurse case management in the care of the high-risk adult with type 2 diabetes. Particular attention was given to ensuring fidelity to the motivational interviewing approach.
Keywords: Behavior change, Motivational interviewing, Nurse Case Management
Introduction
Type 2 diabetes is a chronic disease that requires ongoing interdisciplinary collaboration and patient self-management. Adherence with blood glucose monitoring, appropriate diet, medications, and regular exercise are important self-care behaviors that improve clinical outcomes. This is not easily achieved, as reflected by the fact that less than 60% of U.S. adults with diabetes achieve the HbA1c goal of under 7%.[1]
Motivational interviewing (MI) is a patient-centered, directive method for enhancing the intrinsic motivation to change.[2] The aim of this counseling approach is to empower the patient to change behavior. Studies have shown that MI improves systolic blood pressure, total blood cholesterol, weight loss, well-being, and quality of life, and reduces waist circumference and fat intake.[3–8] Studies on its effect on HbA1c, however, are conflicting.[8–10]
Nurse case management is a collaborative process that provides and coordinates health care services to meet an individual’s health needs. It decreases fragmentation and duplication of care while enhancing quality cost-effective clinical outcomes.[11] The multi-disciplinary nature of diabetes lends itself well to nurse case management. However, studies on nurse case management and diabetes clinical outcomes have shown conflicting effects on blood pressure and lipids, with some showing improvement and others showing no effect.[12] Similarly, effects on HbA1c have been mixed.[12–14] However, a meta-analysis of twenty-nine studies by Welch et al found a mean HbA1c reduction of 0.89%.[15] Thus, overall, it seems to be a promising approach to the management of diabetes patients and is often considered a key element in the adoption of more coordinated primary care systems such as the Patient-Centered Medical Home (PCMH).[16]
The specific aim of this study was to determine if the addition of nurse case managers (NCMs) trained in MI to usual care would result in improved outcomes over two years in patients with type 2 diabetes who are at high risk for cardiovascular complications.
Methods
A 2-year randomized controlled pragmatic trial was conducted in 12 primary care clinics within two health systems in Central Pennsylvania (Penn State Milton S. Hershey Medical Center and Reading Hospital). None of the clinics employed an NCM. A bilingual and bicultural NCM was employed for the three clinics that served an urban underserved population that was primarily Hispanic.
The intervention protocol was approved by the ethics committee of both hospitals. The study aimed to look at effects on patients at high risk for complications. Patients aged 18–75 with type 2 diabetes were eligible if they had one or more of the following: (1) HbA1c > 8.5%, (2) blood pressure > 140/90, or (3) LDL > 130. Patients were excluded if they could not communicate in either English or Spanish, or if they were residents of nursing homes. Recruitment commenced in August 2006 and ended in March 2008.
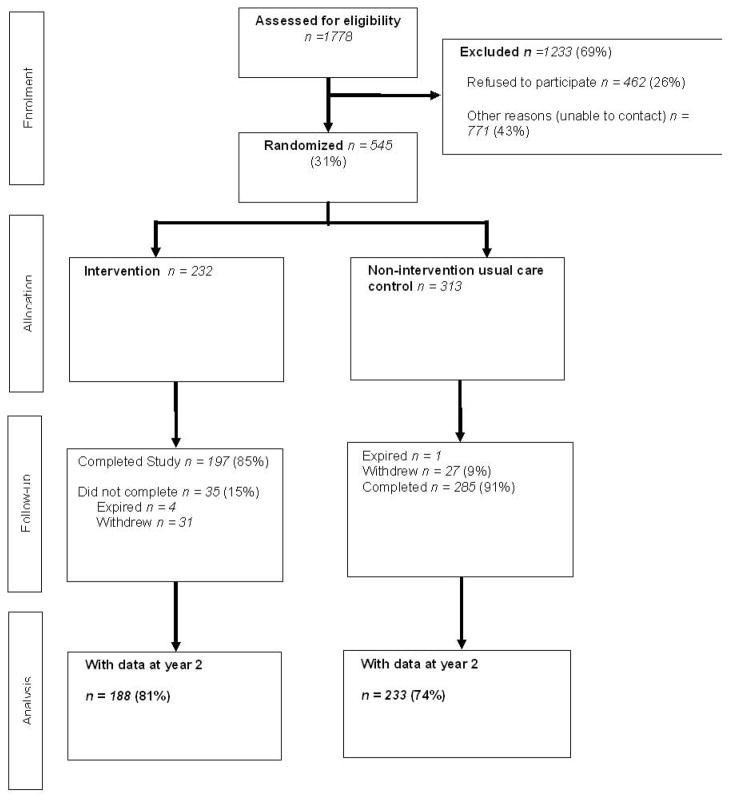
A total of 1178 patients were assessed for eligibility. Of these, 545 participants were randomized to an untreated usual care control or the intervention group (Figure 1). At the time of randomization, a small number of patients in the intervention group (n=42) never received any intervention (never met or had any interaction with the NCM) and therefore were added to the untreated usual care control group. For the final data analysis, there were thus 232 participants in the intervention group while there were 313 participants in the control. All participants provided informed consent.
Figure 1.
CONSORT Diagram
Participants were randomized to usual care control or the intervention group. Those assigned to the intervention group met individually within their primary care clinic with their nurse case managers at baseline, 2 weeks, 6 weeks, 3 months, 6 months, 12 months, and at least every 6 months thereafter. Visits were approximately 1 hour long and were usually not held on the same days as their PCP visits. Intervention group participants could also contact their NCMs by phone and e-mail in between visits when appropriate. The frequency of these phone and e-mail conversations varied based on participant need as assessed by the nurse care manager. As requested by participants, there were more phone calls in between visits than there were e-mails. Visits were conducted in English or Spanish, depending on participant preference. The visits typically included a review of patients’ clinical laboratory test results, health-related lifestyle behavior relevant to managing type 2 diabetes, and medication adherence. The NCMs also checked whether the patient was due for complications screening and reminded them of follow-up specialist visits when they were due. Referrals to a certified diabetes nurse educator or a dietitian were done where appropriate. Finally, NCMs prompted the PCPs for medication titrations when necessary. These were done via e-mail, in person, or phone call, depending on the PCP’s preference.
As a pragmatic trial, participants in both the control and intervention groups received routine care from their primary care providers (PCP), including routine physical examinations and laboratory tests. Routine care typically involved visits with a PCP every three months. PCPs were not taught MI and control group participants had no contact with the NCMs. Laboratory data as well as dates of the most recent ophthalmologic and foot exams were entered into the computerized Penn State Diabetes Registry.[17] For the intervention group, nurses had standing orders for yearly ophthalmologic and foot exams and laboratory tests. Clinical data was abstracted from the participants’ medical records.
Three nurses (BSN level) were employed to deliver the NCM intervention. Nurse A was in her 40s and had worked for 15 years as a case manager. Nurse B was in her 20s and had worked for 4 years in an acute care inpatient setting. Nurse C was in her 30s and had been employed as a middle manager in a hospital inpatient unit. All three nurses underwent a standardized training with an 80-hour curriculum developed by the investigators in the year preceding the study, using experts in MI, nurse case management, and diabetes. Techniques for teaching MI included classroom lectures, role plays, videoconferences, journal article reviews, attending conferences and lectures, and mock interviews with standardized patients. The content was presented by two health care professionals certified in MI. Fidelity to the MI approach was ensured by MI experts who monitored audiotaped sessions monthly using the Behavior Change Counseling Index (BECCI), a reliable and validated tool that has been developed specifically for use in the healthcare setting.[18] NCMs were given feedback based on these evaluations. In addition, audiotapes were reviewed by a PhD prepared nurse practitioner who had worked clinically in home health. Initially, these reviews occurred weekly then diminished as the NCMs became more proficient. The NCMs and two investigators met to review study progress biweekly or more frequently if needed.
All study participants were asked to fill out 5 self-report questionnaires at baseline, 1 year, and 2 years: (1) the Problem Areas in Diabetes (PAID) scale, (2) the Diabetes Treatment Satisfaction Questionnaire (DTSQ), (3) the Center for Epidemiologic Studies Depression (CES-D) scale, (4) the Summary of Diabetes Self-Care Activities (SDSCA), and (5) the Audit of Diabetes Dependent Quality of Life (ADDQoL). Surveys were mailed to the participants with reminders as needed. The survey data was collected and compiled by the Penn State Survey Research Center.
The PAID scale is a 20-item self-report measure of diabetes-related emotional distress. A 5-point scale is used to rate each item and the score is rescaled from 0 to 100, with a high score indicating greater emotional distress from diabetes.[19]
The DTSQ is a 6-item measure of satisfaction with the diabetes regimen, rated from 0 to 6. Total scores range from 0 to 36. A higher score indicates higher satisfaction.[20]
The ADDQoL evaluates the impact of diabetes on quality of life. It includes two overview items that assess the global quality of life and the impact of diabetes on quality of life. Patients also rate the impact of diabetes on each of 19 specific domains and rate the importance of each domain for their quality of life. A weighted impact score is computed and can range from −9 to +3 with more negative scores indicating poorer quality of life from diabetes.[21] DTSQ and ADDQoL were kindly provided by Dr. Clare Bradley (UK).
The CES-D measures depression symptoms. Scores are based on a patient’s response to 20 statements assessing behavior and feelings within the past week. Each response is given a corresponding score of 0 to 3 so the total score can range from 0 to 60. A cutoff scores of 16 or greater identifies individuals at risk for clinical depression, with good sensitivity and specificity and high internal consistency..[22,23]
The SDSCA measure is a 25-item self-report questionnaire of diabetes self-management. It includes items that assess the following aspects of the diabetes regimen: general diet, specific diet, exercise, blood glucose testing, foot care, and smoking.[24]
Qualitative data regarding patients’ perspectives about the use of motivational interviewing has been previously published.[25]
Statistical Analysis
Data were cleaned, coded, and analyzed using SAS Version 9.1 (SAS Inc., Cary NC). Descriptive statistics, including the mean, standard deviation and quartiles for quantitative outcomes and frequency tables for screening examinations, were used to profile the sample and the groups were compared using t-tests and chi-square tests for quantitative and screening examination outcomes respectively.
The primary quantitative outcomes including HbA1c, LDL, BP, PAID, DTSQ, CES-D, SDSCA and ADDQoL were analyzed within the framework of mixed-effects linear models incorporating the longitudinal nature of the data. Mean values of the outcomes were estimated for each group at each time point. Linear contrasts were used to test for differences between groups at each time point, between time points within each group separately, and for differences between groups with respect to change from baseline. Outcomes including performance measures (screening exams) were analyzed using chi-square tests for differences between groups. This sample size (n= 545) provides 90% power to detect a treatment group difference in HbA1c of 0.72 at the p <0.05 level, assuming a 20% dropout rate and a standard deviation of 2.3.
Results
Baseline characteristics of the study population are provided in Table 1. There was no significant difference in study measures between the two groups. A considerable percentage of the participants were Hispanic (39% of control and 38% of intervention group). The majority of participants (71%) had an annual household income of $35,000 or under.
Table 1.
Baseline characteristics of the study population
| Characteristic | Control | Treatment | p-value |
|---|---|---|---|
| Demographics | |||
| Population data (n = 545) | 313 | 232 | |
| Age in years, mean (SD) | 58 (11.34) | 58 (11.41) | 0.7018 |
| Female | 55% | 62% | 0.0914 |
| Race | |||
| (% White) | 47% | 46% | 0.7679 |
| (% Hispanic) | 123 (39%) | 88 (38%) | 0.8374 |
| Education (% some college) | 34% | 35% | 0.3853 |
| Income | |||
| (<$15,000/y per family) | 166/277 = 58% | 105/192 = 55% | 0.057 |
| (=$35,000/y per family) | 197/277 = 71% | 134/192 = 70% | 0.76 |
| Clinical data outcomes | |||
| BMI, mean (SD) kg/m2 | 34.8 (8.78) | 34.0 (7.41) | 0.2615 |
| A1c, mean (SD) % | 9.05 (2.27) | 8.82 (2.38) | 0.2807 |
| LDL, mean (SD) mg/dL | 127 (45.55) | 128 (39.70) | 0.8245 |
| Systolic BP, mean (SD) mm Hg | 142 (20.54) | 145 (18.84) | 0.1724 |
| Diastolic BP, mean (SD) mm Hg | 78 (11.53) | 80 (12.55) | 0.0563 |
| A1c in control (=7%) | 30% | 36% | 0.1684 |
| Lipids in control (LDL =100 mg/dL) | 45% | 40% | 0.2800 |
| Systolic BP in control (=130) | 45% | 46% | 0.7767 |
| Diastolic BP in control (=80) | 63% | 69% | 0.2329 |
| Overall control (A1c, LDL, and BP) | 2% | 3% | 0.6142 |
| Survey data | |||
| PAID -emotional distress (SD) | 29 (24.32) | 29 (22.64) | 0.8520 |
| DTSQ -treatment satisfaction (SD) | 27 (8.17) | 26 (8.3) | 0.6791 |
| CES-D - depression (SD) | 15 (15.24) | 14 (14.76) | 0.6132 |
| SDSCA self-care (SD) | |||
| General diet score | 4 (2.24) | 3 (2.27) | 0.1559 |
| Specific diet score | 4 (1.64) | 4 (1.61) | 0.1944 |
| Exercise score | 2 (1.97) | 2 (2.04) | 0.1941 |
| Glucose score | 4 (2.98) | 4 (2.90) | 0.9540 |
| Foot score | 4 (2.58) | 4 (2.67) | 0.1003 |
| ADDQoL (quality of life) | −0.88 (3.32) | −1.15(3.33) | 0.3515 |
The mean number of NCM visits was 5.7 ± 3.6 within the 2-year intervention period. 197 (85%) participants from the intervention group completed the study (Figure 1). Of these, 75 (32% of intervention group) lost engagement with the NCM in that they did not see the NCM in the last 8 months of the study despite multiple attempts at contact (three calls followed by three reminder letters). Despite this 81% of the intervention group still had clinical and laboratory data available for analysis. This is because this was a pragmatic trial and the participants’ clinical data was still accessible through the registry as long as they continued to follow-up with their PCPs.
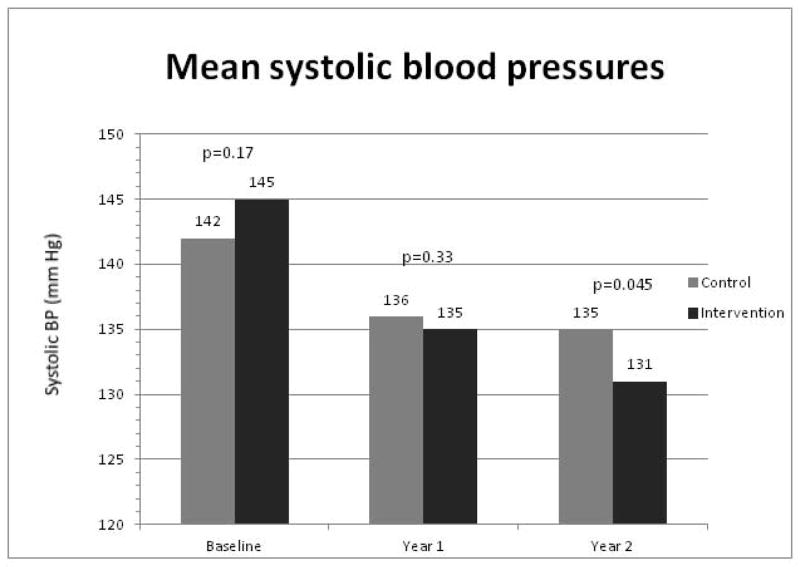
There was a statistically significant improvement in systolic BP for the intervention group compared to the control group at year 2 (131±15.9 vs. 135±18.2, p < 0.05) (Figure 2). The remainder of the clinical outcomes including HbA1c, LDL, and diastolic BP showed significant within group improvement but were not different between the two groups at the completion of the study. HbA1c improved from 9.1±2.3 % to 8.0±1.8 % at year 2 in the control group and from 8.8±2.4 % to 7.8±1.7 % in the intervention group. LDL improved from 127±45.6 to 100±35.5 mg/dL at year 2 in the control group and from 128±39.7 to 102±35.6 mg/dL in the intervention group. Diastolic BP improved from 78±11.5 to 74±11.0 mm Hg at year 2 in the control group and from 80±12.6 to 74±11.4 mm Hg in the intervention group. All within group differences were statistically significant with a p value < 0.05.
Figure 2.
Mean systolic blood pressures of the study groups.
At year 1, the survey response rate was 56% for the control group and 68% for the intervention group. At year 2, response rates were very similar for the two groups (42% for the control and 43% for the intervention group) with no significant difference between responders and non-responders in terms of blood pressure or HbA1c values. The baseline survey data results were not different between the two. Baseline depression scores, as measured by the CES-D scale, were 15±15 and 14±15 for the control and intervention groups, respectively. 34% of the study population had a CES-D score of at least 16 at baseline, implying clinically significant depression, with no significant difference between the two groups. At the completion of the study, CES-D scores were better in the intervention group (14±14 for the control and 10±11 for intervention group, p = 0.02) consistent with a marked reduction in depressive symptoms (Figure 3). Scores for treatment satisfaction (DTSQ), self- care activities (SDSCA), and diabetes-specific quality of life (ADDQoL) showed within group improvement but did not differ significantly between the two groups at the end of the study. The baseline PAID score was 29 for both groups. Although PAID scores were not statistically different at year 1, the scores were better and approached statistical significance for the intervention group at year 2 (29±27 for the control and 23±21 for the intervention group, p = 0.08).
Figure 3.
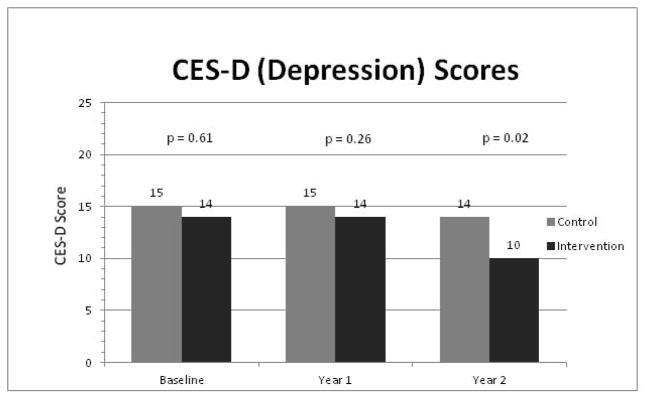
Center for Epidemiologic Studies Depression (CES-D) scores of the study groups. A score of at least 16 indicates clinically significant depression.
Significantly more participants in the intervention group received annual screening for complications during both years of the study. For neuropathy screening with monofilament foot examinations, 22% of the intervention group was screened compared to 14% of the control group (p < 0.001). For retinopathy screening with documented ophthalmologic examinations, 34% of the intervention group was screened compared to 24% of the control group (p <0.001). For nephropathy screening 92% of the intervention group was screened compared to 85% of the control group (p = 0.017).
Discussion
Care management has emerged as an attractive approach to improve diabetes outcomes and is being increasingly reimbursed through programs focused on the implementation of the Patient-Centered Medical Home (PCMH) model.[16] Training in MI might be expected to enhance clinical outcomes.
MI holds significant promise to improve patient outcomes but has shown mixed results in patients with diabetes.[8–10,15] When delivered by diabetes educators, the addition of MI to diabetes self-management education was not found to improve HbA1c.[9] Similar results were reported when MI was delivered by general practitioners.[26] In a study of overweight type 2 patients, an 18-month intervention of MI as an adjunct to a weight control program resulted in greater weight loss at 6 months and 18 months and an HbA1c reduction of 0.3% at 6 months but this was not sustained at 18 months. MI delivered in a group setting of diabetes patients who participated in a 4-day diabetes education program also did not have any benefit on HbA1c, PAID scores, or perceived competence for diabetes.[27] An MI intervention given by dietitians decreased saturated fat intake but had no effects on HbA1c, BMI, and waist circumference.[28] However, in a small study conducted on a group of older obese women with diabetes, the addition of a 3-session MI intervention to a 16-week group behavioral weight-control program found better attendance in group meetings, increased food diary logs, and higher frequency of blood glucose monitoring as well as a 1% decrease in HbA1c.[4] MI delivered by a nurse practitioner via videoconference in a 6-month intervention study decreased HbA1c by 1.7%, compared to the control group that had a 0.6% decrease in HbA1c, and improved diabetes knowledge and self-efficacy.[10] In this study, MI was delivered weekly for 3 months then monthly thereafter. In addition, patients were asked to read a diabetes handout prior to each videoconference. It is not completely clear, however, whether the improvement in HbA1c was a result of MI, the frequent videoconference consultations and greater provider interaction, or improved knowledge from reading the handouts. These findings may indicate that although MI can improve some outcomes, improving overall glycemic control may require additional factors.
Previous reviews on motivational interviewing and its adaptations have shown variability in the dose and method of delivery of MI and in what skills were actually used.[29] Developing and maintaining proficiency in MI can also be challenging.[30] One shortcoming of some previous studies using MI has been a lack of attention to MI fidelity. In this study, however consistency in MI use was ensured by performing monthly reviews of audiotaped sessions and providing feedback to the NCMs. A standardized tool (BECCI) was also used to evaluate audiotapes.
In a high risk group with elevated emotional distress and depression symptoms at baseline, we found that an intervention with nurse case management and MI results in a statistically significant 4 mm Hg decrease in systolic BP. This decrease in systolic BP appears to be clinically relevant. Previous studies have found that a modest systolic BP decrease of 2–5 mm Hg is associated with improved cardiovascular outcomes.[31] In the MICRO-HOPE sub-study, patients with a blood pressure lowering of only 2.4/1.0 mm Hg had a significant reduction in cardiovascular events.[32]
Lower depression symptom scores (CES-D) were seen in the intervention group and there was a trend toward improved emotional distress based on PAID scores. This improvement in mental health may lead to better diabetes control.[33,34] NCMs followed the MacArthur protocol for patients in the intervention group that had CES-D scores of at least 16.[35] Based on this protocol, recommendations were made to the PCPs about potentially starting an SSRI medication and referring to a therapist. In the usual care group, there was no systematic screening for depression. Detection and treatment of depression in the usual care group was based on the PCP’s discretion. It is possible that this is more systematic screening, evaluation, and treatment lead to improved depression scores in the intervention group.
The intervention group was screened for diabetes complications more frequently, which has important implications for disease prevention and health maintenance. This finding is similar to a previous meta-analysis on nurse case management where an improvement in process measures was also seen.[36]
It is noteworthy that there were significant improvements in all the clinical parameters, even in the control group. Specifically, HbA1c decreased by 1.1%, LDL by 27 mg/dL, and diastolic BP by 4 mm Hg, which are greater than expected from a placebo effect. Since this was a pragmatic trial, primary care practices were not prevented from participating in other ongoing quality improvement initiatives. Specifically, other changes happening in the study practice during the trial were: (1) the Penn State Diabetes Registry [17] was introduced and (2) the Pennsylvania Chronic Care Initiative (PCCI) [37] was being actively implemented. The PCCI was a statewide initiative where practices received increased reimbursement coupled with learning collaborative participation and practice coaching for adoption of the PCMH. These changes probably improved clinical outcomes for all the patients, regardless of the group they were assigned, and may have obscured any further treatment benefit from our intervention. In addition, the Hawthorne effect may have affected provider behavior. Having NCMs at the providers’ practice sites may have caused a spill-over effect that improved how providers managed their patients, resulting in improved outcomes.
It is surprising, however, that despite strict adherence to the MI approach, measures of patient behavior (SDSCA) and treatment satisfaction (DTSQ) did not improve. This is in line with the findings of a study by Welch where they found that an MI intervention did not affect patient-reported diabetes self-care behaviors.[9] However, this finding is particularly unexpected in our study given the findings of a focus group discussion with intervention group participants who were very receptive to the MI approach and offered only positive feedback about their experiences with the NCMs.[25] Perhaps because most of the participants were low income, they were limited by the high cost of resources such as nutrition, medications, and transportation to clinic visits. Also, our participants were a high risk group who may have had more difficulty implementing self-care behaviors due to co-morbidities and lack of social support systems.
One of the limitations of this study was that over the course of the two year study, a significant number of patients lost active engagement with the nurse (32%). The NCMs noted that many of the patients had complained about transportation being an issue in their adherence with follow-up visits, especially because the NCM visits were typically not held at the same time as their PCP visits. It is possible that in a low-income population such as ours, a more focused, shorter intervention might be more effective than long-term care management. In fact, a 1-year NCM intervention on a similar study population showed better clinical improvements with lower BP, depression scores, and improved diabetes complications screening.[13] The decrease in blood pressure was 9/6 mm Hg for the intervention group in this particular study.
In summary, we found that the use of NCMs trained in motivational interviewing resulted in improvements in systolic BP as well as depression symptoms. It is possible that more robust clinical improvement will be seen if nurse case management and MI are used alongside other approaches. In particular, strategies where nurses have standing orders for medication adjustments might need to be employed. Indeed, previous studies where NCMs were allowed to titrate medications without awaiting physician approval found better clinical outcomes.[38,39] In a study where physicians were receptive to medication changes recommended by medically supervised NCMs, significant improvements in HbA1c, LDL, systolic BP, and depression were seen.[40] In our trial, the nurses prompted providers for medication titration. However, the physicians were not always responsive. Ultimately, strategies to reduce provider clinical inertia might also be needed.[41] It is clear that diabetes is best managed with an integrated, multi-disciplinary approach.
In the current national effort to make primary care more coordinated within the framework of the PCMH, care management is considered a central feature and a key component for recognition by the National Committee for Quality Assurance.[42] Incorporating MI into NCM holds significant promise to improve patient outcomes but the optimal dose and type of intervention require further study.
Acknowledgments
This study was supported by a grant from National Institutes of Health and National Institute of Diabetes and Digestive and Kidney Diseases grant R18-DK067495. The authors thank Kendra Durdock, RN, Nancy Martinez-King, RN, and David George, MD (Reading Hospital) for their contributions in conducting the study. R.G. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Disclosure – None declared.
References
- 1.Ford ES, Li C, Little RR, Mokdad AH. Trends in A1C concentrations among U.S. adults with diagnosed diabetes from 1999 to 2004. Diabetes Care. 2008;31:102–104. doi: 10.2337/dc07-0565. [DOI] [PubMed] [Google Scholar]
- 2.Rollnick S, Miller WR, Butler CC. Motivational Interviewing in Health Care. New York: The Guilford Press; 2008. [Google Scholar]
- 3.Clark M. Diabetes self-management education: a review of published studies. Prim Care Diabetes. 2008;2:113–120. doi: 10.1016/j.pcd.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Smith DE, Heckemeyer CM, Kratt PP, Mason DA. Motivational interviewing to improve adherence to a behavioral weight-control program for older obese women with NIDDM. A pilot study. Diabetes Care. 1997;20:52–54. doi: 10.2337/diacare.20.1.52. [DOI] [PubMed] [Google Scholar]
- 5.Greaves CJ, Middlebrooke A, O’Loughlin L, Holland S, Piper J, et al. Motivational interviewing for modifying diabetes risk: a randomised controlled trial. Br J Gen Pract. 2008;58:535–540. doi: 10.3399/bjgp08X319648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Channon SJ, Huws-Thomas MV, Rollnick S, Hood K, Cannings-John RL, et al. A multicenter randomized controlled trial of motivational interviewing in teenagers with diabetes. Diabetes Care. 2007;30:1390–1395. doi: 10.2337/dc06-2260. [DOI] [PubMed] [Google Scholar]
- 7.Viner RM, Christie D, Taylor V, Hey S. Motivational/solution-focused intervention improves HbA1c in adolescents with Type 1 diabetes: a pilot study. Diabet Med. 2003;20:739–742. doi: 10.1046/j.1464-5491.2003.00995.x. [DOI] [PubMed] [Google Scholar]
- 8.Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55:305–312. [PMC free article] [PubMed] [Google Scholar]
- 9.Welch G, Zagarins SE, Feinberg RG, Garb JL. Motivational interviewing delivered by diabetes educators: does it improve blood glucose control among poorly controlled type 2 diabetes patients? Diabetes Res Clin Pract. 91:54–60. doi: 10.1016/j.diabres.2010.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hawkins SY. Improving glycemic control in older adults using a videophone motivational diabetes self-management intervention. Res Theory Nurs Pract. 24:217–232. doi: 10.1891/1541-6577.24.4.217. [DOI] [PubMed] [Google Scholar]
- 11.Glettler E, Leen MG. The advanced practice nurse as case manager. J Case Manag. 1996;5:121–126. [PubMed] [Google Scholar]
- 12.Norris SL, Nichols PJ, Caspersen CJ, Glasgow RE, Engelgau MM, et al. The effectiveness of disease and case management for people with diabetes. A systematic review. Am J Prev Med. 2002;22:15–38. doi: 10.1016/s0749-3797(02)00423-3. [DOI] [PubMed] [Google Scholar]
- 13.Gabbay RA, Lendel I, Saleem TM, Shaeffer G, Adelman AM, et al. Nurse case management improves blood pressure, emotional distress and diabetes complication screening. Diabetes Res Clin Pract. 2006;71:28–35. doi: 10.1016/j.diabres.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 14.Anderson DR, Christison-Lagay J, Villagra V, Liu H, Dziura J. Managing the space between visits: a randomized trial of disease management for diabetes in a community health center. J Gen Intern Med. 25:1116–1122. doi: 10.1007/s11606-010-1419-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Welch G, Garb J, Zagarins S, Lendel I, Gabbay RA. Nurse diabetes case management interventions and blood glucose control: results of a meta-analysis. Diabetes Res Clin Pract. 88:1–6. doi: 10.1016/j.diabres.2009.12.026. [DOI] [PubMed] [Google Scholar]
- 16.Bojadzievski T, Gabbay RA. Patient-centered medical home and diabetes. Diabetes Care. 34:1047–1053. doi: 10.2337/dc10-1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khan L, Mincemoyer S, Gabbay RA. Diabetes registries: where we are and where are we headed? Diabetes Technol Ther. 2009;11:255–262. doi: 10.1089/dia.2008.0057. [DOI] [PubMed] [Google Scholar]
- 18.Lane C, Huws-Thomas M, Hood K, Rollnick S, Edwards K, et al. Measuring adaptations of motivational interviewing: the development and validation of the behavior change counseling index (BECCI) Patient Educ Couns. 2005;56:166–173. doi: 10.1016/j.pec.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 19.Welch GW, Jacobson AM, Polonsky WH. The Problem Areas in Diabetes Scale. An evaluation of its clinical utility. Diabetes Care. 1997;20:760–766. doi: 10.2337/diacare.20.5.760. [DOI] [PubMed] [Google Scholar]
- 20.Bradley C. Diabetes treatment satisfaction questionnaire. Change version for use alongside status version provides appropriate solution where ceiling effects occur. Diabetes Care. 1999;22:530–532. doi: 10.2337/diacare.22.3.530. [DOI] [PubMed] [Google Scholar]
- 21.Bradley C, Todd C, Gorton T, Symonds E, Martin A, et al. The development of an individualized questionnaire measure of perceived impact of diabetes on quality of life: the ADDQoL. Qual Life Res. 1999;8:79–91. doi: 10.1023/a:1026485130100. [DOI] [PubMed] [Google Scholar]
- 22.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. App Psych Measurement. 1977;1:385–401. [Google Scholar]
- 23.Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and aging. 1997;12:277–287. doi: 10.1037//0882-7974.12.2.277. [DOI] [PubMed] [Google Scholar]
- 24.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 25.Dellasega C, Anel-Tiangco RM, Gabbay RA. How patients with type 2 diabetes mellitus respond to motivational interviewing. Diabetes Res Clin Pract. 95:37–41. doi: 10.1016/j.diabres.2011.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rubak S, Sandbaek A, Lauritzen T, Borch-Johnsen K, Christensen B. Effect of “motivational interviewing” on quality of care measures in screen detected type 2 diabetes patients: a one-year follow-up of an RCT, ADDITION Denmark. Scand J Prim Health Care. 29:92–98. doi: 10.3109/02813432.2011.554271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosenbek Minet LK, Wagner L, Lonvig EM, Hjelmborg J, Henriksen JE. The effect of motivational interviewing on glycaemic control and perceived competence of diabetes self-management in patients with type 1 and type 2 diabetes mellitus after attending a group education programme: a randomised controlled trial. Diabetologia. 54:1620–1629. doi: 10.1007/s00125-011-2120-x. [DOI] [PubMed] [Google Scholar]
- 28.Brug J, Spikmans F, Aartsen C, Breedveld B, Bes R, et al. Training dietitians in basic motivational interviewing skills results in changes in their counseling style and in lower saturated fat intakes in their patients. J Nutr Educ Behav. 2007;39:8–12. doi: 10.1016/j.jneb.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 29.Martins RK, McNeil DW. Review of Motivational Interviewing in promoting health behaviors. Clin Psychol Rev. 2009;29:283–293. doi: 10.1016/j.cpr.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 30.Miller WR, Mount KA. A small study of training in motivational interviewing: Does one workshop change clinician and client behavior? Behavioural and Cognitive Psychotherapy. 2001:457–471. [Google Scholar]
- 31.Fox KM. Efficacy of perindopril in reduction of cardiovascular events among patients with stable coronary artery disease: randomised, double-blind, placebo-controlled, multicentre trial (the EUROPA study) Lancet. 2003;362:782–788. doi: 10.1016/s0140-6736(03)14286-9. [DOI] [PubMed] [Google Scholar]
- 32.Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Heart Outcomes Prevention Evaluation Study Investigators. Lancet. 2000;355:253–259. [PubMed] [Google Scholar]
- 33.Echeverry D, Duran P, Bonds C, Lee M, Davidson MB. Effect of pharmacological treatment of depression on A1C and quality of life in low-income Hispanics and African Americans with diabetes: a randomized, double-blind, placebo-controlled trial. Diabetes Care. 2009;32:2156–2160. doi: 10.2337/dc09-0785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lustman PJ, Clouse RE, Nix BD, Freedland KE, Rubin EH, et al. Sertraline for prevention of depression recurrence in diabetes mellitus: a randomized, double-blind, placebo-controlled trial. Arch Gen Psychiatry. 2006;63:521–529. doi: 10.1001/archpsyc.63.5.521. [DOI] [PubMed] [Google Scholar]
- 35. [Accessed November 26, 2012];The MacArthur Initiative on Depression and Primary Care at Dartmouth and Duke [article online] Available from http://www.depression-primarycare.org/clinicians/toolkits.
- 36.Renders CM, Valk GD, Griffin SJ, Wagner EH, Eijk Van JT, et al. Interventions to improve the management of diabetes in primary care, outpatient, and community settings: a systematic review. Diabetes Care. 2001;24:1821–1833. doi: 10.2337/diacare.24.10.1821. [DOI] [PubMed] [Google Scholar]
- 37.Bricker PL, Baron RJ, Scheirer JJ, DeWalt DA, Derrickson J, et al. Collaboration in Pennsylvania: rapidly spreading improved chronic care for patients to practices. J Contin Educ Health Prof. 30:114–125. doi: 10.1002/chp.20067. [DOI] [PubMed] [Google Scholar]
- 38.Davidson MB. Effect of nurse-directed diabetes care in a minority population. Diabetes Care. 2003;26:2281–2287. doi: 10.2337/diacare.26.8.2281. [DOI] [PubMed] [Google Scholar]
- 39.Shojania KG, Ranji SR, McDonald KM, Grimshaw JM, Sundaram V, et al. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA. 2006;296:427–440. doi: 10.1001/jama.296.4.427. [DOI] [PubMed] [Google Scholar]
- 40.Katon WJ, Lin EH, Von Korff M, Ciechanowski P, Ludman EJ, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 363:2611–2620. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shah BR, Hux JE, Laupacis A, Zinman B, van Walraven C. Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians? Diabetes Care. 2005;28:600–606. doi: 10.2337/diacare.28.3.600. [DOI] [PubMed] [Google Scholar]
- 42.National Committee for Quality Assurance. Standards and Guidelines for Physician Practice Connections -Patient-Centered medical Home [article online] [Accessed March 22 2012];2008 [Google Scholar]