Abstract
Context
Many youth with depression do not respond to initial treatment with selective serotonin reuptake inhibitors (SSRIs), and this is associated with higher costs. More effective treatment for these youth may be cost-effective.
Objective
To evaluate the incremental cost-effectiveness over 24 weeks of combined cognitive behavior therapy plus switch to a different antidepressant medication vs medication switch only in adolescents who continued to have depression despite adequate initial treatment with an SSRI.
Design
Randomized controlled trial.
Setting
Six US academic and community clinics.
Patients
Three hundred thirty-four patients aged 12 to 18 years with SSRI-resistant depression.
Intervention
Participants were randomly assigned to (1) switch to a different medication only or (2) switch to a different medication plus cognitive behavior therapy.
Main Outcome Measures
Clinical outcomes were depression-free days (DFDs), depression-improvement days (DIDs), and quality-adjusted life-years based on DFDs (DFD-QALYs). Costs of intervention, nonprotocol services, and families were included.
Results
Combined treatment achieved 8.3 additional DFDs (P=.03), 0.020 more DFD-QALYs (P=.03), and 11.0 more DIDs (P=.04). Combined therapy cost $1633 more (P=.01). Cost per DFD was $188 (incremental cost-effectiveness ratio [ICER]=$188; 95% confidence interval [CI], −$22 to $1613), $142 per DID (ICER=$142; 95% CI, −$14 to $2529), and $78 948 per DFD-QALY (ICER=$78 948; 95% CI, −$9261 to $677 448). Cost-effectiveness acceptability curve analyses suggest a 61% probability that combined treatment is more cost-effective at a willingness to pay $100 000 per QALY. Combined treatment had a higher net benefit for subgroups of youth without a history of abuse, with lower levels of hopelessness, and with comorbid conditions.
Conclusions
For youth with SSRI-resistant depression, combined treatment decreases the number of days with depression and is more costly. Depending on a decision maker’s willingness to pay, combined therapy may be cost-effective, particularly for some subgroups.
Major depression in adolescence is common and causes significant impairment in functioning, frequently leading to substantial costs to the health care system, families, and other social sectors.1 Effective treatments include selective serotonin reuptake inhibitors (SSRIs), psychotherapy, and a combination of both. Evidence suggests that the short-term direct cost associated with these treatments varies: combined cognitive behavior therapy (CBT) and medication therapy is most expensive, CBT alone is less expensive, and medication therapy alone is least expensive.2
Evidence is mixed regarding the relative clinical effectiveness and cost-effectiveness of combined psychotherapy and medication compared with medication alone in teens with a typical depressive episode. Using data from the Treatment for Adolescents With Depression Study, Domino et al2,3 found that combination therapy was not as cost-effective as medication alone in treating short-term (up to 12 weeks) major depression in youth. However, in a longer-term analysis (up to 36 weeks),4 they found that combination therapy was highly likely to be cost-effective, although clinical differences were not statistically significant. Goodyer et al5 used data from the Adolescent Depression Antidepressant and Psychotherapy Trial in the context of the United Kingdom health service and found that combined therapy was unlikely to be more cost-effective than medication alone for youth with major depression.
Given these mixed results and the scarcity of resources in most health systems, more information is needed about the cost-effectiveness of treatment for youth depression.6,7 For example, although combination therapy may not be as cost-effective as a first-line treatment for initial episodes of major youth depression, it might be a cost-effective alternative for some sub groups. For example, for approximately 40% of youth who do not respond to initial depression treatment, more intense services, such as combined psychotherapy and medication, might be cost-effective.
Recent results from the Treatment of SSRI-Resistant Depression in Adolescents (TORDIA) study indicate that youth who received combined CBT and medication switch showed a higher response rate than did those receiving a medication switch alone. The direct cost and relative cost-effectiveness of these treatments in this population have not been previously studied, to our knowledge. This article examines the incremental cost-effectiveness of combined CBT and medication switch and medication switch alone in youth with treatment-resistant depression, information that could help health plan managers and decision makers assess the relative value of alternative treatments.
METHODS
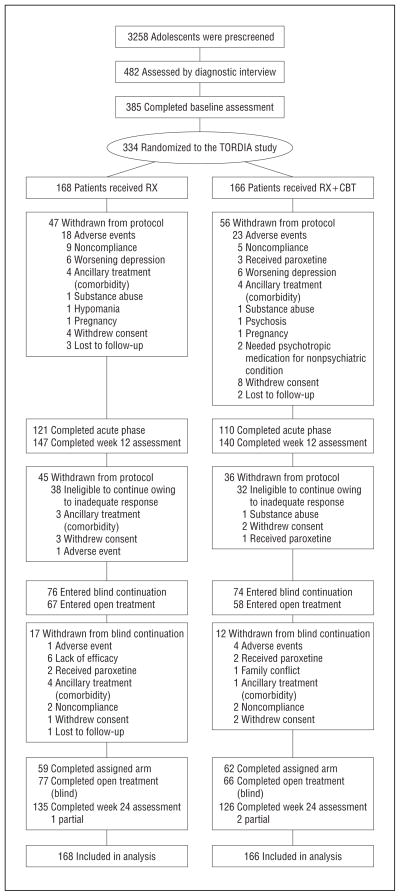
The TORDIA study was a multicenter randomized clinical trial designed to evaluate the effectiveness of treating adolescents with depression who failed initial SSRI treatment. Patients were 334 adolescents undergoing active treatment for moderate to severe DSM-IV major depressive disorder. Failure to respond to treatment was defined by continuation of major depression meeting DSM-IV criteria of at least moderate severity despite having adequate treatment with an SSRI regimen for at least 8 weeks. Youth were randomly assigned to receive combined CBT and medication switch or medication switch only (the switch was to a different medication than the one they had been treated with before the trial) (Figure 1). Clinical outcome analyses indicated that the medications to which youth were switched had an equivalent effect.8,9 Everyone received the randomized treatment strategy for the first 12 weeks of the study; patients with a clinically acceptable response received 12 additional weeks of continuation treatment. Non responders were offered open treatment with medication, CBT, or both. Patients were recruited at 6 sites (University of Pittsburgh, Brown University, University of California at Los Angeles, University of Texas Southwestern Medical Center at Dallas, University of Texas Medical Branch at Galveston, and Kaiser Permanente Northwest). More details about the design, methods, sample, interventions, and clinical outcomes are given elsewhere.8,9
Figure 1.
Study participants from prescreening through analysis. RX indicates medication switch only; RX + CBT, combined medication switch and cognitive behavior therapy; and TORDIA, Treatment of SSRI-Resistant Depression in Adolescents.
MEASURES
Clinical Outcomes
Depressive disorder diagnoses were assessed by evaluators blinded to treatment assignment at baseline and at 6-, 12-, and 24-week follow-ups using the Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime Version.10 Because of the chronicity of depression and the treatment resistance of study participants, the primary clinical outcome was “adequate clinical response,” defined by a Clinical Global Impression–Improvement Scale score of 2 or less11 (Guy 1976) and an improvement in the Children’s Depression Rating Scale–Revised score of at least 50%.8,12 This measure reflects whether patients had significant clinical depression symptom improvement rather than total remission of depression.
Following previous cost-effectiveness analyses in depression treatment, we used these clinical data to create several summary measures for the cost-effectiveness analysis. To compare the cost-effectiveness of this intervention with that of others, we created a measure of depression-free days (DFDs).2,13–15 We used Children’s Depression Rating Scale–Revised scores at each assessment point and accepted clinical cutoff points2,16 to categorize days as DFDs, days with some depression but not meeting the full criteria, and days in a depression episode. We interpolated using quadratic weighting between the non depressed and fully depressed thresholds to assign a value to each day in the interval. We then calculated the number of DFDs as the number of days in the study minus days with significant depression symptoms. This approach more completely captures the effects of the intervention, including elevated-symptom days and days in a full depression episode; similar methods have been used in previous studies.2,4,15
We transformed DFDs into quality-adjusted life-years (QALYs) by using preference weights assigned to depression from the literature, which reflect the value of different health or disease states derived from empirical studies. For example, DFDs are typically assigned a utility weight of 1.0 (full health), whereas days in a depression episode are estimated to have a lower weight, such as 0.6. Results of empirical studies17–22 indicate that major depression is associated with a decrease in health-related quality of life of 0.2 to 0.6. On the basis of previous studies,14,23–25 we used 0.4 as the preference weight for the base case analysis.
Given the TORDIA study’s focus on depression symptom improvement (vs full remission), we created an additional exploratory summary measure for the cost-effectiveness analyses, depression-improvement days (DIDs), which is the number of days that patients had significant improvement in depression symptoms from baseline. Using the study’s clinical criteria for “adequate clinical response,” we calculated the number of DIDs between each assessment. Days that met the full improvement criteria were weighted as full DIDs; days with some improvement but that did not meet the full criteria were given a partial-improvement weight; days with no improvement were weighted as zero; and days with worsening symptoms were given a negative weight consistent with the degree of worsening observed.
Cost Outcomes
We estimated total intervention services costs. Accounting records provided costs for payroll, facilities and overhead, and goods and services. Staff estimated time to complete intervention tasks and use of capital equipment, space, and supplies. We included costs of medication management visits, CBT, biweekly expert supervision conference calls, training, and materials. We excluded research-specific costs, such as randomization.
We created comprehensive profiles of community services that youth used outside of the study protocol using the Child and Adolescent Services Assessment,26,27 which collects comprehensive data on youth mental health services use. We estimated health care costs by applying unit costs developed for other recent teen depression studies.2,28 At baseline, participants or their parents were asked to report on any services they received in the previous 3 months; at 6-, 12-, and 24-week follow-up visits, they reported service use since the previous assessment.
Following recommended guidelines,29 we estimated costs for the time parents spent taking youth to related services. We created profiles of parent time spent for the intervention, non-protocol services, travel to services, and waiting using published research14,15,23–25 and wages to value parent time.29 We did not include the costs of the teen’s time.
STATISTICAL METHODS
Analyses were performed on an intent-to-treat basis including all 334 randomized youth. Incremental cost-effectiveness ratios (ICERs) were estimated from a societal perspective for 24 weeks after intervention. In each instance, the ratio was computed as the mean cost difference between combined CBT and medication switch and medication switch only divided by the mean difference in clinical outcome (DFDs, DIDs, or DFD-QALYs). As is typical, costs were not normally distributed. We used the net benefit regression method30 with ordinary least squares regression analyses to examine cost-effectiveness. The robustness of the parametric tests was confirmed using non-parametric bootstrapping31 with a single model with 1000 replications using the bias-corrected and accelerated method.32–34 Hypotheses tests and adjusted differences between the groups were estimated using ordinary least squares regression models with bootstrap interval estimates; all analyses were adjusted for baseline characteristics, including baseline Children’s Depression Rating Scale–Revised score, baseline costs, race, age, sex, and study site.
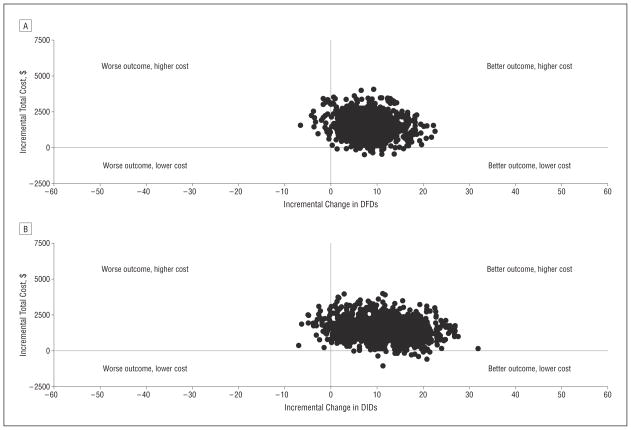
To represent uncertainty in estimates, we first used the bootstrap observations to estimate 95% confidence intervals (CIs) around the mean ICERs. We then created a scatterplot of the bootstrapped incremental cost-and-effect pairs to create an incremental cost-effectiveness plane35 divided into 4 quadrants, centered at zero. Incremental cost-effect pairs that fall into the southeast quadrant indicate that the intervention is less costly and more effective than alternative treatment; northwest quadrant pairs indicate a more costly and less effective intervention; northeast quadrant pairs indicate a more costly and more effective intervention; and southwest quadrant pairs indicate a less costly and less effective intervention. If most of the cost-effect observations are located in the southeast quadrant, the new treatment is “dominant” over the alternative treatment; similarly, if most observations are in the northwest quadrant, the treatment is “dominated” by the alternative.
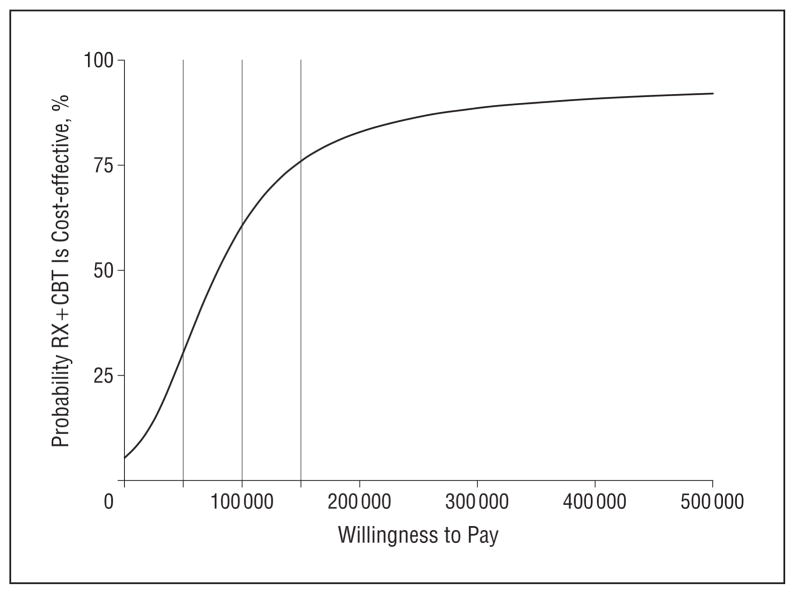
Commonly, a new intervention is more costly and more effective than an alternative. In these circumstances, a cost-effectiveness acceptability curve (CEAC)35 presents the probability that a new intervention is cost-effective compared with its alternative across a range of maximum dollar levels that a decision maker is willing and able to pay for an additional increment of the clinical outcome (eg, DFDs) given budgetary and other constraints.
MISSING DATA
Of the 334 study patients, 24.9% (n=83) had missing data at 1 or more assessments; (27.7% in the combined group vs 22.0% in the medication-only group; P=.23). Missing data were imputed using multiple imputation with chained equations36–38 using a statistical software program (STATA; StataCorp LP, College Station, Texas). The procedures assumed that data were missing at random. We included all non missing values of costs or outcomes at all time points and baseline demographics in the models that generated imputed estimates. We created 5 imputation data sets and combined estimates so that standard errors reflected the variability introduced by the imputation process.38
Additional Analyses
In addition, we evaluated several models to examine how sensitive the cost-effectiveness results were to the assumptions and to include some secondary outcomes. We conducted (1) a sensitivity analysis to examine whether the results would differ if we used a more conservative preference weight, indicating that depression had a less negative effect on health-related quality of life; (2) a sensitivity analysis that used a preference weight for severe depression when estimating QALYs17,19; and (3) an alternative analysis following the original method of Lave and colleagues14 for calculating DFDs. We wanted to examine the effect of the difference between methods.
We conducted the following secondary analyses: (1) excluding 1 high-cost outlier (with high depression-related inpatient and outpatient costs); (2) excluding 1 study participant (hospitalized for most of the study period); (3) excluding all participants hospitalized during the study period (n=24); and (4) including only outpatient costs. Given the small sample sizes in most depression treatment randomized controlled trials, many cost-effectiveness studies of adult depression limit costs to outpatient only.
Subgroup Analyses
Analyses of treatment response moderation in the TORDIA study indicated that youth with comorbid conditions, no history of abuse, and lower levels of hopelessness were more likely to benefit from combined treatment.9 Given these differential clinical effects for youth subgroups, we examined cost-effectiveness by subgroup following the net benefit regression method.30
RESULTS
Clinical results of the TORDIA trial indicated that combined CBT and a switch to another antidepressant agent resulted in a higher rate of clinical response than did medication switch alone, and a switch to another SSRI was just as efficacious as a switch to venlafaxine hydrochloride.8 Moderation analyses indicated that combined therapy was more effective for youth with comorbid disorders, youth with low levels of hopelessness, and youth with no history of abuse.9
Table 1 reports selected baseline characteristics of the randomized participants; detailed group comparisons are available else where.8,9 There were no statistically significant differences between the medication switch only (RX) and the combined medication switch and CBT (RX + CBT) groups at baseline.
Table 1.
Sample Description
| Variable | RX (n=168) | RX + CBT (n=166) | P Value |
|---|---|---|---|
| Demographic characteristics | |||
| Age, mean (SD), y | 15.8 (1.6) | 16.0 (1.5) | .25 |
| White race/ethnicity, No. (%) | 136 (81.0) | 141 (84.9) | .33 |
| Female sex, No. (%) | 117 (69.6) | 116 (69.9) | .96 |
| Household income (in thousands), median (range), $ | 70 (8–500) | 68 (0–190) | .58 |
| Parent education: college graduate No. (%) | 76 (45.2) | 76 (45.8) | .83 |
| Clinical characteristics, mean (SD) | |||
| Children’s Depression Rating | 58.4 (9.7) | 59.2 (11.0) | .50 |
| Scale–Revised score Clinical Global Impression–Severity Scale score | 4.5 (0.6) | 4.5 (0.7) | .91 |
| Cost for previous 3 mo at baseline, $ | 3590 (8733) | 3860 (7283) | .76 |
Abbreviations: RX, medication switch only; RX + CBT, combined medication switch and cognitive beharior therapy.
CLINICAL OUTCOMES
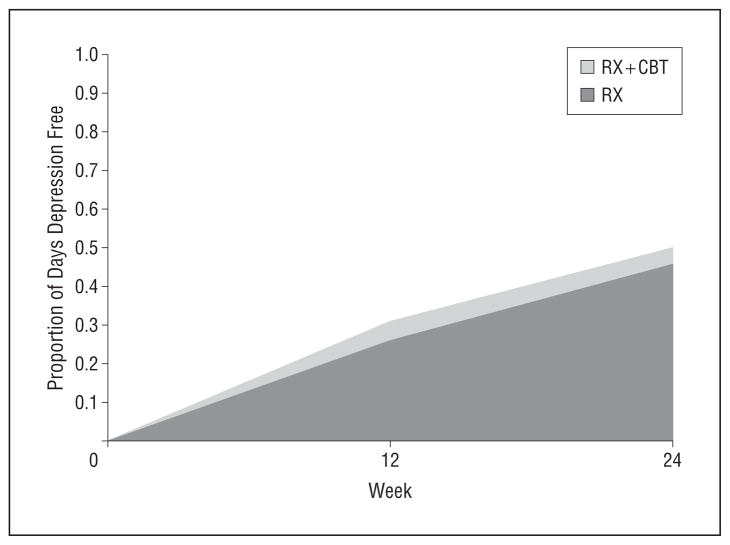
Table 2 describes the primary intent-to-treat analysis of the incremental differences in clinical outcomes between the RX + CBT group compared with the RX group through 24 weeks for the base case analysis. Compared with the RX group, participants in the RX + CBT group had an average of 8.3 more DFDs (P=.03), 0.020 more DFD-QALYs (P=.03), and 11.0 more DIDs (P=.04). Figure 2 demonstrates that the proportion of DFDs increased across time for both groups but that the proportion of days that were depression free in the RX + CBT group was greater at each follow-up assessment.
Table 2.
Incremental Differences in Clinical Outcomes at 24 Weeks
| Outcome | Unadjusted Mean (SD)
|
Incremental Effect (RX-CBT Only)a | P Valueb | |
|---|---|---|---|---|
| RX (n=168) | RX + CBT (n=166) | |||
| No. of DFDs | 77.0 (52.9) | 83.7 (56.7) | 8.3 | .03 |
| DFD-QALYs | 0.783 (0.126) | 0.799 (0.135) | 0.020 | .03 |
| No. of DIDs (exploratory outcome) | 133.9 (82.1) | 144.3 (87.5) | 11.0 | .04 |
Abbreviations: DFD, depression-free day; DID, depression-improvement day; QALY, quality-adjusted life-year; RX, medication switch only; RX + CBT, combined medication switch and cognitive behavior therapy.
Adjusted incremental effect.
Hypotheses tests are based on regression results adjusted for differences in baseline Children’s Depression Rating Scale–Revised score, baseline costs, race, age, sex, and study site.
Figure 2.
Proportion of days that are depression free across 24 weeks in the medication switch only (RX) and combined medication switch and cognitive behavior therapy (RX + CBT) groups.
RESOURCE USE AND COST
Table 3 provides descriptive estimates of nonprotocol service use, nonprotocol service costs, costs associated with the interventions, and total costs by group during the 24-week study. The pattern of nonprotocol service use was generally similar between the 2 groups. The mean number of inpatient days was higher for the RX + CBT group than for the RX group. Some families reported that some youth received additional antidepressant medications through nonprotocol health care services during follow-up. The mean total cost of nonprotocol services was higher in the RX + CBT group, but this difference was not significant (P=.14). Total intervention costs were higher in the RX + CBT group (P<.001). The cost of medication and medication management was similar between the groups. The higher cost in the RX + CBT group was due to the additional CBT cost. Total cost, the sum of nonprotocol service costs, intervention costs, and family costs, was $1633 higher in the RX + CBT group than in the RX group; this difference was significant (P=.01).
Table 3.
Unadjusted Service Use and Cost (2006 US $) by Randomization Condition Through 24 Weeks
| Variable | With Use or Cost, %
|
Visits or Costs, Mean (SD)
|
||
|---|---|---|---|---|
| RX | RX + CBT | RX (n=168) | RX + CBT (n=166) | |
| Nonprotocol services | ||||
| Inpatient mental health days | 3.6 | 3.0 | 0.9 (7.9) | 2.0 (16.2) |
| Inpatient alcohol or drug days | 0.6 | 0 | 0.0 (0.1) | 0 |
| Counseling or medication management visits | 22.9 | 19.6 | 1.9 (4.7) | 2.1 (5.4) |
| Day hospital days | 1.8 | 2.4 | 0.2 (1.7) | 0.5 (2.8) |
| Alcohol or drug treatment visits | 1.2 | 0.6 | 0.1 (1.1) | 0.1 (1.1) |
| Crisis services | 0 | 1.8 | 0.1 (0.9) | 0.1 (0.9) |
| Medical physician visits | 1.2 | 4.2 | 0.1 (0.5) | 0.1 (0.4) |
| Emergency department visits | 3.0 | 4.8 | 0.2 (0.7) | 0.1 (0.4) |
| Antidepressant medication from nonprotocol care providers | 9.5 | 12.0 | NA | NA |
| Stimulant medication | 0 | 3.0 | NA | NA |
| Other psychotropic medication | 0.6 | 1.8 | NA | NA |
| Any school services | 16.3 | 11.9 | 4.6 (14.8) | 2.8 (11.5) |
| Juvenile correction contact | 1.2 | 1.2 | 0.1 (0.5) | 0.2 (1.4) |
| Nonprotocol costs, $ | ||||
| Any | 53.6 | 48.2 | 1646 (5092) | 2435 (8878)a |
| Total nonprotocol family | NA | NA | 305 (1178) | 325 (973) |
| Intervention costs, $ | ||||
| Medication | NA | NA | 460 (182) | 460 (183) |
| Medication management | NA | NA | 665 (326) | 628 (365) |
| CBT | NA | NA | NA | 232 (108) |
| Total intervention family | NA | NA | 1204 (1479) | 1606 (1200) |
| Total intervention costs | NA | NA | 2481 (1718) | 3224 (1609)b |
| Total costsc | NA | NA | 4673 (7173) | 6306 (12 029)b |
Abbreviations: NA, not applicable; RX, medication switch only; RX + CBT, combined medication switch and cognitive behavior therapy.
Not statistically significant.
Statistically significant, P<.001.
Total costs were imputed using multiple imputation with chained equations if missing.
COST-EFFECTIVENESS ANALYSIS
Table 4 reports the mean ICERs for each type of clinical outcome during the 24-week study, adjusted for baseline characteristics. At 24 weeks, the estimated cost per DFD was $188 (ICER=$188; 95% CI, −$22 to $1613) and per DID was $142 (ICER=$142; 95% CI, −$14 to $2529). Using DFD-QALYs as the outcome, we estimated a cost of $78 948 per QALY (ICER=$78 948; 95% CI, −$9261 to $677 448).
Table 4.
Adjusted Cost-effectiveness Ratios at 24 Weeks (2006 US $)
| Variable | ICERa
|
||
|---|---|---|---|
| DFD | ICERa DFD-QALYs | DID (Exploratory) | |
| Full sample (n=334) | 188 | 78 948 | 142 |
| Sensitivity analyses | |||
| More conservative QALY weight | NA | 105 264 | NA |
| QALY weight for severe depression | NA | 63 158 | NA |
| Alternative DFD calculation method | 205 | 86 204 | NA |
| Secondary analyses | |||
| Excluding cost outlier (n=333) | 166 | 69 796 | 127 |
| Excluding patient hospitalized for large portion of study period (n=333) | 128 | 53 560 | 94 |
| Excluding patients with any inpatient visits (n=310) | 103 | 43 066 | 79 |
| Outpatient costs only | 113 | 47 350 | 90 |
| Subgroup analyses | |||
| History of abuse | |||
| No | 83 | 34 895 | 55 |
| Yes | Dominatedb | Dominatedb | Dominatedb |
| Comorbid conditions | |||
| 0 | Dominatedb | Dominatedb | 654 |
| ≥1 | 167 | 69 937 | 118 |
| Level of hopelessness | |||
| Low | 34 | 14 338 | 27 |
| High | Dominatedb | Dominatedb | Dominatedb |
Abbreviations: DFD, depression-free day; DID, depression-improvement day; ICER, incremental cost-effectiveness ratio; NA, not applicable; QALY, quality-adjusted life-year.
Bias corrected.
Average clinical effect is negative, so combined medication switch and cognitive behavior therapy is never preferred for thius group.
Figure 3 presents the incremental cost-effectiveness planes for the base case analysis. Each point in the figure represents an incremental cost–clinical outcome pair for a single bootstrap replication at 24 weeks. For each outcome, most observations indicated that the RX + CBT intervention had better clinical effects and higher costs compared with RX, with better outcomes and higher costs for 96.0% of DFD observations and 94.8% of DID observations. For both outcomes, less than 5% of the incremental cost–clinical outcome pairs had higher costs and worse outcomes.
Figure 3.
Cost-effectiveness planes for the base case analysis. Incremental total costs at 24 weeks are shown by incremental Children’s Depression Rating Scale–Revised (CDRS-R) depression-free days (DFDs) (A) and incremental depression-improvement days (DIDs) (B). The model used 1000 replications adjusted for site, age, baseline CDRS-R score, baseline cost, race, and sex differences.
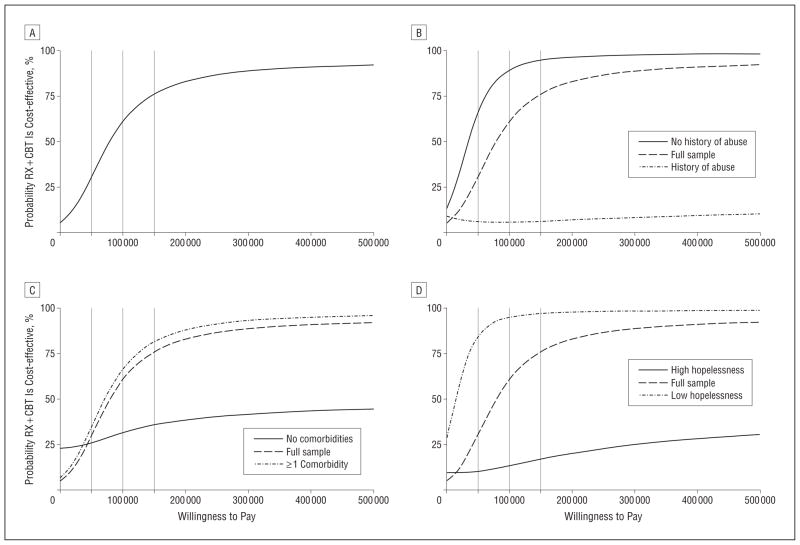
Figure 4 presents the CEAC for DFD-QALYs at 24 weeks, showing the probability that RX + CBT is cost-effective compared with RX across a range of maximum dollar values that a decision maker might be willing and able to pay for an additional clinical outcome (eg, QALY). The x-axis shows the maximum dollar amounts a decision maker is able and willing to pay to achieve an additional clinical outcome. The y-axis shows the probability that the true cost-effectiveness ratio falls at or below maximum dollar-value amounts.39 To provide a concrete example of how a decision maker might interpret the CEAC, each CEAC figure has a vertical bar at $100 000 as an example level of payment; if a decision maker is willing and able to pay this amount per QALY, the probability that RX + CBT is cost-effective compared with RX at 24 weeks is 61% for DFD-QALY. Tests beyond the $100 000 value found that the probability that RX + CBT is cost-effective compared with RX at 24 weeks is 90% at $350 000 and 95% at $3 060 000.
Figure 4.
Cost-effectiveness acceptability curve for the base case analysis showing quality-adjusted life-years based on depression-free days at week 24. RX + CBT indicates combined medication switch and cognitive behavior therapy.
We conducted several sensitivity analyses and secondary analyses, outlined in the “Additional Analyses” subsection, to examine whether the cost-effectiveness estimates would be different using various parameters (Table 4). The results indicate some variation in incremental cost per QALY for different assumptions, with a range of $43 066 to $105 264 per DFD-QALY, and in incremental cost per DFD for different assumptions, with a range of $103 to $205 per DFD.
We also explored differential cost-effectiveness for subgroups (Table 4). We found that RX + CBT had a much higher net benefit for youth without a history of abuse and with lower levels of hopelessness. For youth with a history of abuse or high hopelessness levels, the average clinical effect on DFDs and DIDs was negative, so the RX + CBT intervention was dominated by the RX intervention. The RX + CBT intervention was also dominated by the RX intervention in DFDs only for those youth with no comorbid conditions.
Figure 5 presents the CEACs for DFD-QALYs at 24 weeks for the subgroup analyses. Assuming that a decision maker is willing and able to pay a maximum of $100 000 per QALY gained, the probability that RX + CBT is cost-effective compared with RX for the subgroup with a history of abuse is 6%; for the subgroup without a history of abuse, the probability is 89%. For youth without a history of abuse, tests beyond the $100 000 value found that the probability that RX + CBT is cost-effective compared with RX at 24 weeks is 90% at $105 000 and 95% at $150 000. For youth with a history of abuse, tests beyond the $100 000 value found that the probability that RX + CBT is cost-effective compared with RX at 24 weeks does not approach 90% even at the very high threshold of $10 million.
Figure 5.
Cost-effectiveness acceptability curves showing quality-adjusted life-years based on depression-free days at week 24 for the full sample (A) and for subgroups according to history of abuse (B), comorbidities (C), and hopelessness (D). RX + CBT indicates combined medication switch and cognitive behavior therapy.
For the subgroup with no comorbid conditions, and assuming that a decision maker is willing and able to pay a maximum of $100 000 per QALY gained, the probability that RX + CBT is cost-effective compared with RX for this subgroup is 32%; for those with 1 or more comorbid conditions, the probability is 67%. For youth with no comorbid conditions, tests beyond the $100 000 value found that the probability that RX + CBT is cost-effective compared with RX at 24 weeks does not approach 90% even at the very high threshold of $10 million. For youth with 1 or more comorbid conditions, tests beyond the $100 000 value found that the probability that RX +CBT is cost-effective compared with RX at 24 weeks is 90% at $220 000 and 95% at $410 000.
For the subgroup with high levels of hopelessness, and assuming that a decision maker is willing and able to pay a maximum of $100 000 per QALY gained, the probability that RX + CBT is cost-effective compared with RX for this subgroup is 13%; for those with low levels of hopelessness, the probability is 95%. For youth with high levels of hopelessness, tests beyond the $100 000 value found that the probability that RX + CBT is cost-effective compared with RX at 24 weeks does not approach 90% even at the very high threshold of $10 000 000. For youth with low levels of hopelessness, tests beyond the $100 000 value found that the probability that RX + CBT is cost-effective compared with RX at 24 weeks is 90% at $65 000 and 95% at $100 000.
COMMENT
We found that among depressed teens who failed a previous adequate course of SSRI medication treatment, CBT combined with medication switch achieved 8.3 more DFDs and 11.0 more DIDs across a 24-week treatment period. Combination therapy was significantly more expensive than medication switch alone. In the base case analysis, the mean ICER comparing combination treatment with medication switch alone was $188 per DFD and $78 948 per DFD-QALY. The CEAC analyses suggest that combination therapy has a 61% probability of being more cost-effective than medication alone if a decision maker is willing to pay $100 000 per QALY.
Interpretation of cost-effectiveness depends on a decision maker’s willingness to pay for an additional unit of clinical outcome (eg, QALY). There is no official standard for cost-effectiveness in the United States,29 and there is ongoing discussion about the appropriateness and amount of a standard.40–42 One frequently cited criterion is that if an intervention has an incremental cost per QALY of $50 000 or less, it is a reasonable value compared with many of the medical treatments currently covered under typical insurance packages.40,42 Several experts have recently argued that this criterion is too conservative, suggesting that more appropriate criteria might be in the range of $109 000 to $297 000.42 Results of the present base case analysis and all sensitivity analyses fall below the latter-range, but the base case analysis is higher than the $50 000-per-QALY level.
In the literature on the cost-effectiveness of adult depression treatments, researchers have commonly reported incremental cost-effectiveness results using a cost-per-DFD metric. Comparing interpersonal psychotherapy with usual care for depression treatment, Lave and colleagues14 reported average cost-effectiveness for 2 types of depression treatment at $13 and $18 per DFD for direct costs only and $15 and $25 per DFD for costs including patient time and transportation. Simon and colleagues43 reported average cost-effectiveness for systematic depression treatment for high users of general medical care of approximately $41 per DFD for direct costs and $52 per DFD including patient time cost. Another study24 comparing cost-effectiveness of collaborative care for persistent depression reported cost per DFD of $21 to $35 depending on the types of costs included. Finally, a review44 of studies comparing cost-effectiveness of enhanced primary care for depression reported cost per DFD of $13 to $24 depending on the types of costs included. The present base case result ($188 per DFD) and most of the additional analyses are substantially higher than these results.
We also found that the cost per clinical outcome was much more favorable for some subgroups. For teens with no history of abuse and youth with low hopelessness levels, the ICERs for combined therapy compared with medication switch alone were always $50 000 per QALY or less; the CEAC analysis found that there was a 90% probability that RX + CBT is cost-effective compared with RX for low levels of hopelessness at a value of $65 000 per QALY and a 90% probability that RX + CBT is cost-effective compared with RX for youth with no history of abuse at a value of $105 000 per QALY. For youth with comorbid conditions, we found somewhat more favorable, albeit modest, cost-effectiveness results compared with the base case.
The present findings add to the growing literature about the efficiency of providing combined therapy to youth with depression. Domino and colleagues2,4 found that the incremental cost-effectiveness of combined treatment compared with medication alone was $458 818 per QALY at 12 weeks, concluding that combination therapy was not more cost-effective at 12 weeks; however, in a longer-term analysis, they found that combination therapy is likely to be cost-effective compared with medication alone at 36 weeks. Byford and colleagues45 found that combination CBT and medication was unlikely to be more cost-effective compared with medication alone in the UK health system in the short-term. The present results are somewhat more favorable than those of previous studies, with lower estimated incremental costs per QALY that have a reasonably good probability of being cost-effective for some subgroups.
The results of this analysis also contribute to the understanding of the efficiency of combined therapy for youth depression because of differences in the TORDIA population. Some previous trials have been limited to youth in an initial episode of depression2 or have not included youth who failed a previous trial of medication,5 whereas the TORDIA study included youth with chronic depression who failed previous adequate medication treatment. In the present base case analysis, we used a preference weight to convert DFDs and QALYs used in multiple previous studies of depression treatment.2,14,15 Given the high-risk population in the TORDIA study, use of a preference weight for more severe depression may be more appropriate. The sensitivity analyses indicate that when we used a preference weight for severe depression and DFD-QALY as the outcome, combined therapy was likely to be cost-effective compared with medication assuming that a decision maker is willing and able to pay $100 000 per QALY.
The results of this study should be interpreted in light of several limitations. First, we did not include productivity costs for youth associated with depression. A growing body of research indicates that adult depression is associated with a significant reduction in workplace outcomes.46,47 Other recent research has found that depression in adolescence is associated with a variety of negative educational outcomes48,49 and reduced earnings in adulthood.48,50 Together, these findings suggest that youth depression may reduce human capital development. For example, approximately 4% of the youth in the TORDIA trial were hospitalized during the 24-week study, with an average stay of 12 days. Therefore, a subgroup with treatment-resistant depression may be missing a significant number of school days due to hospitalization, and this does not include school days missed when the youth were not hospitalized or had reduced productivity in school.
Other family costs may also be important.1 For example, although we included some travel and visit time costs for parents of hospitalized youth while the youth was in the hospital, families likely spent considerable additional time related to the hospitalizations, such as time spent on insurance-related issues and coordinating and planning for care for the youth once they were released from the hospital. These costs were not included in this analysis.
There are 2 other limitations related to the methods. The TORDIA trial did not include a preference-based measure of health-related quality of life, which would have allowed direct measurement of the impact of the interventions on youth QALYs. Therefore, we had to rely on indirect methods to calculate QALYs. We followed an established method for translating DFDs into QALYs,2,4,14,15 but we had to use preference weights reported in the literature for adults with depression because no empirical ones exist for teens. Adult weights may not accurately represent the impact of depression on teen quality of life.51 The preference weights we used measure only the decrease in health-related quality of life associated with depression; changes in health-related quality of life associated with comorbidities were not captured. Finally, we used nationally representative unit costs for nonprotocol services that were developed for another study of teen depression, which may not accurately represent the actual unit costs at all 6 study sites.
In conclusion, many youth do not respond to a first course of treatment for major depression, yet the clinical outcomes and costs for persistent depression are significant. If a decision maker is willing and able to pay $100 000 per QALY, combined therapy has a moderate probability of being cost-effective compared with medication switch alone for all youth with treatment-resistant depression across 24 weeks of treatment. In addition, we find that combined therapy is much more likely to be cost-effective compared with medication switch alone for some subgroups of youth with treatment-resistant depression. At minimum, expansion of the use of combined therapy for targeted subgroups of youth with treatment-resistant depression is warranted.
Acknowledgments
Funding/Support: This work was supported by grants MH61835 (Pittsburgh site), MH61856 (Galveston site), MH61864 (UCLA site), MH61869 (Portland site), MH61958 (Dallas site), and MH62014 (Brown University site) from the National Institute of Mental Health and by grant MH66371 from the Advanced Center for Early-Onset Mood and Anxiety Disorders (Dr Brent).
Footnotes
Author Contributions: Dr Lynch had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Financial Disclosure: Dr Wagner reports receiving past research support from Abbott Laboratories, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Forest Laboratories GlaxoSmithKline, Johnson & Johnson, Novartis, Organon, Pfizer, and Wyeth-Ayerst and is a consultant/advisory board member for Abbott Laboratories, Astra-Zeneca, Bristol-Myers Squibb, Cyberonics, Eli Lilly, Forest Laboratories, GlaxoSmithKline, Janssen, Jazz Pharmaceuticals, Novartis, Organon, Ortho-McNeil, Otsuka, Pfizer, Solvay, UCB Pharma, and Wyeth Ayerst. Dr Emslie reports receiving research support from Biobehavioral Diagnostics Inc, Eli Lilly, Forest Laboratories, Organon, Shire, and Somerset; consulting for Biobehavioral Diagnostics Inc, Eli Lilly, GlaxoSmithKline, Shire, and Wyeth-Ayerst; and is on the speaker’s bureau for McNeil. Dr Asarnow reports consulting on CBT and CBT for depression supported by an unrestricted grant from Pfizer and has funding from Philip Morris; a family member has funding from Bristol-Myers Squibb and has consulted for Roche. Dr Keller reports receiving research support from Pfizer and Wyeth Pharmaceuticals; receiving consulting fees from Abbott, Bristol-Meyers Squibb, CENEREX, Cephalon, Cypress Bioscience, Cyberonics, Forest Laboratories, GlaxoSmithKline, Janssen, JDS, Medtronic, Organon, Novartis, Pfizer, Roche, Sierra Neuropharmaceuticals, Solvay, and Wyeth; and serving on advisory boards for Abbott Laboratories, Bristol-Myers Squibb, CENEREX, Cyberonics, Cypress Bioscience, Forest Laboratories, Janssen, Neuronetics, Novartis, Organon, and Pfizer. Dr Birmaher reports participating in forums sponsored by Abcomm Inc and Solvay Pharmaceuticals Inc; presenting on bipolar disorders in children at a meeting sponsored by Solvay; and receiving royalties from Random House Inc. Dr McCracken reports receiving research support from Bristol-Myers Squibb, Eli Lilly, McNeil, and Shire and consulting fees from Eli Lilly, Janssen, Johnson & Johnson, McNeil, Novartis, Pfizer, Shire, and Wyeth.
Additional Contributions: Dana Foley, BA, and Terresa Fair provided excellent editorial and administrative support, respectively.
References
- 1.Lynch FL, Clarke GN. Estimating the economic burden of depression in children and adolescents. Am J Prev Med. 2006;31(6 suppl 1):S143–S151. doi: 10.1016/j.amepre.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 2.Domino ME, Burns BJ, Silva SG, Kratochvil CJ, Vitiello B, Reinecke MA, Mario J, March JS. Cost-effectiveness of treatments for adolescent depression: results from TADS. Am J Psychiatry. 2008;165(5):588–596. doi: 10.1176/appi.ajp.2008.07101610. [DOI] [PubMed] [Google Scholar]
- 3.March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, Burns B, Domino M, McNulty S, Vitiello B, Severe J Treatment for Adolescents With Depression Study (TADS) Team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA. 2004;292(7):807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- 4.Domino ME, Foster EM, Vitiello B, Kratochvil CJ, Burns BJ, Silva SG, Reinecke MA, March JS. Relative cost-effectiveness of treatments for adolescent depression: 36-week results from the TADS randomized trial. J Am Acad Child Adolesc Psychiatry. 2009;48(7):711–720. doi: 10.1097/CHI.0b013e3181a2b319. [DOI] [PubMed] [Google Scholar]
- 5.Goodyer I, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, Breen S, Ford C, Barrett B, Leech A, Rothwell J, White L, Harrington R. Selective serotonin re-uptake inhibitors (SSRIs) and routine specialist care with and without cognitive behaviour therapy in adolescents with major depression: randomised controlled trial [published online ahead of print June 7, 2007] BMJ. 2007;335(7611):142. doi: 10.1136/bmj.39224.494340.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kraemer HC, Frank E, Kupfer DJ. Moderators of treatment outcomes: clinical, research, and policy importance. JAMA. 2006;296(10):1286–1289. doi: 10.1001/jama.296.10.1286. [DOI] [PubMed] [Google Scholar]
- 7.Insel TR. Translating scientific opportunity into public health impact: a strategic plan for research on mental illness. Arch Gen Psychiatry. 2009;66(2):128–133. doi: 10.1001/archgenpsychiatry.2008.540. [DOI] [PubMed] [Google Scholar]
- 8.Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, Vitiello B, Ritz L, Iyengar S, Abebe K, Birmaher B, Ryan N, Kennard B, Hughes C, DeBar L, McCracken J, Strober M, Suddath R, Spirito A, Leonard H, Melhem N, Porta G, Onorato M, Zelazny J. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA. 2008;299(8):901–913. doi: 10.1001/jama.299.8.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Asarnow JR, Emslie G, Clarke G, Wagner KD, Spirito A, Vitiello B, Iyengar S, Shamseddeen W, Ritz L, McCracken J, Strober M, Suddath R, Leonard H, Porta G, Keller M, Brent D. Treatment of selective serotonin reuptake inhibitor–resistant depression in adolescents: predictors and moderators of treatment response. J Am Acad Child Adolesc Psychiatry. 2009;48(3):330–339. doi: 10.1097/CHI.0b013e3181977476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 11.Guy W ECDEU. Assessment Manual for Psychopharmacology. 2. Washington, DC: US Government Printing Office; 1976. DHEW publication ADM 76–338. [Google Scholar]
- 12.Poznanski EO, Mokros HB. Children’s Depression Rating Scale–Revised, Manual. Los Angeles, CA: Western Psychological Services; 1996. [Google Scholar]
- 13.Pyne JM, Tripathi S, Williams DK, Fortney J. Depression-free day to utility-weighted score: is it valid? Med Care. 2007;45(4):357–362. doi: 10.1097/01.mlr.0000256971.81184.aa. [DOI] [PubMed] [Google Scholar]
- 14.Lave JR, Frank RG, Schulberg HC, Kamlet MS. Cost-effectiveness of treatments for major depression in primary care practice. Arch Gen Psychiatry. 1998;55 (7):645–651. doi: 10.1001/archpsyc.55.7.645. [DOI] [PubMed] [Google Scholar]
- 15.Lynch FL, Hornbrook M, Clarke GN, Perrin N, Polen MR, O’Connor E, Dickerson J. Cost-effectiveness of an intervention to prevent depression in at-risk teens. Arch Gen Psychiatry. 2005;62(11):1241–1248. doi: 10.1001/archpsyc.62.11.1241. [DOI] [PubMed] [Google Scholar]
- 16.Kennard B, Silva S, Vitiello B, Curry J, Kratochvil C, Simons A, Hughes J, Feeny N, Weller E, Sweeney M, Reinecke M, Pathak S, Ginsburg G, Emslie G, March J TADS Team. Remission and residual symptoms after short-term treatment in the Treatment of Adolescents with Depression Study (TADS) J Am Acad Child Adolesc Psychiatry. 2006;45(12):1404–1411. doi: 10.1097/01.chi.0000242228.75516.21. [DOI] [PubMed] [Google Scholar]
- 17.Pyne JM, Fortney JC, Tripathi S, Feeny D, Ubel P, Brazier J. How bad is depression? preference score estimates from depressed patients and the general population. Health Serv Res. 2009;44(4):1406–1423. doi: 10.1111/j.1475-6773.2009.00974.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wells KB, Sherbourne CD. Functioning and utility for current health of patients with depression or chronic medical conditions in managed, primary care practices. Arch Gen Psychiatry. 1999;56(10):897–904. doi: 10.1001/archpsyc.56.10.897. [DOI] [PubMed] [Google Scholar]
- 19.Revicki DA, Wood M. Patient-assigned health state utilities for depression-related outcomes: differences by depression severity and antidepressant medications. J Affect Disord. 1998;48(1):25–36. doi: 10.1016/s0165-0327(97)00117-1. [DOI] [PubMed] [Google Scholar]
- 20.Fryback DG, Dasbach EJ, Klein R, Klein BE, Dorn N, Peterson K, Martin PA. The Beaver Dam Health Outcomes Study: initial catalog of health-state quality factors. Med Decis Making. 1993;13(2):89–102. doi: 10.1177/0272989X9301300202. [DOI] [PubMed] [Google Scholar]
- 21.Pyne JM, Patterson TL, Kaplan RM, Ho S, Gillin JC, Golshan S, Grant I. Preliminary longitudinal assessment of quality of life in patients with major depression. Psychopharmacol Bull. 1997;33(1):23–29. [PubMed] [Google Scholar]
- 22.Unützer J, Patrick DL, Simon G, Grembowski D, Walker E, Rutter C, Katon W. Depressive symptoms and the cost of health services in HMO patients aged 65 years and older: a 4-year prospective study. JAMA. 1997;277(20):1618–1623. doi: 10.1001/jama.1997.03540440052032. [DOI] [PubMed] [Google Scholar]
- 23.Schoenbaum M, Unützer J, Sherbourne C, Duan N, Rubenstein LV, Miranda J, Meredith LS, Carney MF, Wells K. Cost-effectiveness of practice-initiated quality improvement for depression: results of a randomized controlled trial. JAMA. 2001;286(11):1325–1330. doi: 10.1001/jama.286.11.1325. [DOI] [PubMed] [Google Scholar]
- 24.Simon GE, Katon WJ, VonKorff M, Unützer J, Lin EH, Walker EA, Bush T, Rutter C, Ludman E. Cost-effectiveness of a collaborative care program for primary care patients with persistent depression. Am J Psychiatry. 2001;158(10):1638–1644. doi: 10.1176/appi.ajp.158.10.1638. [DOI] [PubMed] [Google Scholar]
- 25.Simon GE, Von Korff M, Ludman EJ, Katon WJ, Rutter C, Unützer J, Lin EH, Bush T, Walker E. Cost-effectiveness of a program to prevent depression relapse in primary care. Med Care. 2002;40(10):941–950. doi: 10.1097/00005650-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Ascher BH, Farmer EM, Burns BJ, Angold A. The Child and Adolescent Services Assessment (CASA): description and psychometrics. J Emot Behav Disord. 1996;4:12–20. [Google Scholar]
- 27.Farmer EM, Angold A, Burns BJ, Costello EJ. Reliability of self-reported service use: test-retest consistency of children’s responses to the Child and Adolescent Services Assessment (CASA) J Child Fam Stud. 1994;3:307–325. [Google Scholar]
- 28.Lynch FL, Striegel-Moore RH, Dickerson J, Perrin N, DeBar L, Wilson GT, Kraemer HC. Cost-effectiveness of a guided self-help intervention for recurrent binge eating. J Consult Clin Psychol. 2010;78(3):322–333. doi: 10.1037/a0018982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-Effectiveness in Health and Medicine. New York, NY: Oxford Press University; 1996. [Google Scholar]
- 30.Hoch JS, Briggs AH, Willan AR. Something old, something new, something borrowed, something blue: a framework for the marriage of health econometrics and cost-effectiveness analysis. Health Econ. 2002;11(5):415–430. doi: 10.1002/hec.678. [DOI] [PubMed] [Google Scholar]
- 31.Efron B, Tibshirani RJ. An Introduction to the Bootstrap. London, United Kingdom: Chapman & Hall; 1993. [Google Scholar]
- 32.Thompson SG, Barber JA. How should cost data in pragmatic randomised trials be analysed? BMJ. 2000;320(7243):1197–1200. doi: 10.1136/bmj.320.7243.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.O’Brien BJ, Briggs AH. Analysis of uncertainty in health care cost-effectiveness studies: an introduction to statistical issues and methods. Stat Methods Med Res. 2002;11(6):455–468. doi: 10.1191/0962280202sm304ra. [DOI] [PubMed] [Google Scholar]
- 34.O’Brien BJ, Drummond MF, Labelle RJ, Willan A. In search of power and significance: issues in the design and analysis of stochastic cost-effectiveness studies in health care. Med Care. 1994;32(2):150–163. doi: 10.1097/00005650-199402000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Fenwick E, Byford S. A guide to cost-effectiveness acceptability curves. Br J Psychiatry. 2005;187:106–108. doi: 10.1192/bjp.187.2.106. [DOI] [PubMed] [Google Scholar]
- 36.Royston P. Multiple imputation of missing values. Stata J. 2004;4(3):227–241. [Google Scholar]
- 37.Royston P. Multiple imputation of missing values: update. Stata J. 2005;5(2):118–201. [Google Scholar]
- 38.Little RJA, Rubin DB. Statistical Analysis With Missing Data. 2. Hoboken, NJ: John Wiley & Sons; 2002. [Google Scholar]
- 39.van Hout BA, Al MJ, Gordon GS, Rutten FF. Costs, effects and C/E-ratios alongside a clinical trial. Health Econ. 1994;3(5):309–319. doi: 10.1002/hec.4730030505. [DOI] [PubMed] [Google Scholar]
- 40.Ubel PA, Hirth RA, Chernew ME, Fendrick AM. What is the price of life and why doesn’t it increase at the rate of inflation? Arch Intern Med. 2003;163(14):1637–1641. doi: 10.1001/archinte.163.14.1637. [DOI] [PubMed] [Google Scholar]
- 41.Weinstein MC. How much are Americans willing to pay for a quality-adjusted life year? Med Care. 2008;46(4):343–345. doi: 10.1097/MLR.0b013e31816a7144. [DOI] [PubMed] [Google Scholar]
- 42.Braithwaite RS, Meltzer DO, King JT, Jr, Leslie D, Roberts MS. What does the value of modern medicine say about the $50,000 per quality-adjusted life-year decision rule? Med Care. 2008;46(4):349–356. doi: 10.1097/MLR.0b013e31815c31a7. [DOI] [PubMed] [Google Scholar]
- 43.Simon GE, Manning WG, Katzelnick DJ, Pearson SD, Henk HJ, Helstad CS. Cost-effectiveness of systematic depression treatment for high utilizers of general medical care. Arch Gen Psychiatry. 2001;58(2):181–187. doi: 10.1001/archpsyc.58.2.181. [DOI] [PubMed] [Google Scholar]
- 44.Gilbody S, Bower P, Whitty P. Costs and consequences of enhanced primary care for depression: systematic review of randomised economic evaluations. Br J Psychiatry. 2006;189:297–308. doi: 10.1192/bjp.bp.105.016006. [DOI] [PubMed] [Google Scholar]
- 45.Byford S, Barrett B, Roberts C, Wilkinson P, Dubicka B, Kelvin RG, White L, Ford C, Breen S, Goodyer I. Cost-effectiveness of selective serotonin reuptake inhibitors and routine specialist care with and without cognitive behavioural therapy in adolescents with major depression. Br J Psychiatry. 2007;191:521–527. doi: 10.1192/bjp.bp.107.038984. [DOI] [PubMed] [Google Scholar]
- 46.Wang PS, Beck AL, Berglund P, McKenas DK, Pronk NP, Simon GE, Kessler RC. Effects of major depression on moment-in-time work performance. Am J Psychiatry. 2004;161(10):1885–1891. doi: 10.1176/ajp.161.10.1885. [DOI] [PubMed] [Google Scholar]
- 47.Donohue JM, Pincus HA. Reducing the societal burden of depression: a review of economic costs, quality of care and effects of treatment. Pharmacoeconomics. 2007;25(1):7–24. doi: 10.2165/00019053-200725010-00003. [DOI] [PubMed] [Google Scholar]
- 48.Berndt ER, Koran LM, Finkelstein SN, Gelenberg AJ, Kornstein SG, Miller IM, Thase ME, Trapp GA, Keller MB. Lost human capital from early-onset chronic depression. Am J Psychiatry. 2000;157(6):940–947. doi: 10.1176/appi.ajp.157.6.940. [DOI] [PubMed] [Google Scholar]
- 49.Fletcher J, Wolfe B. Child mental health and human capital accumulation: the case of ADHD revisited. J Health Econ. 2008;27(3):794–800. doi: 10.1016/j.jhealeco.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 50.Marcotte DE, Wilcox-Gök V. Estimating earnings losses due to mental illness: a quantile regression approach. J Ment Health Policy Econ. 2003;6(3):123–134. [PubMed] [Google Scholar]
- 51.De Civita M, Regier D, Alamgir AH, Anis AH, Fitzgerald MJ, Marra CA. Evaluating health-related quality-of-life studies in paediatric populations: some conceptual, methodological and developmental considerations and recent applications. Pharmacoeconomics. 2005;23(7):659–685. doi: 10.2165/00019053-200523070-00003. [DOI] [PubMed] [Google Scholar]