Abstract
Background
Much about the long-term course of anxiety disorders is unknown. The present study utilizes a naturalistic, longitudinal, short-interval follow-up design to elucidate the course of anxiety disorders over 14 years in a largely middle-aged adult sample recruited from out-patient psychiatry and primary care facilities.
Method
The sample consisted of 453 participants with a diagnosis of panic disorder (PD), social phobia (SP) and/or generalized anxiety disorder (GAD). Anxiety symptom ratings were tracked using weekly psychiatric status ratings (PSRs). Controlling for demographic and clinical variables, the course of PD, GAD and SP were examined using longitudinal growth models, with the most severe PSR at each follow-up point as the main outcome variable.
Results
PSRs significantly decreased in severity over time in each of the three disorders. In the interaction effects models, age×time had a significant effect on course for PD and GAD, but not for SP, in that older age was associated with lower PSRs over time.
Conclusions
The present findings suggest that the severity of anxiety disorders declines over time, although this decline is modest and depends on the specific disorder being assessed. Older individuals with PD and GAD have a better prognosis than their younger counterparts, as their course is characterized by a steeper decline in severity. The present findings provide important information about the course of anxiety disorders in mid-life.
Keywords: Anxiety disorders, longitudinal studies, panic disorder, phobic disorders, prospective studies
Introduction
Anxiety disorders are the most common class of psychiatric disorders in the United States, affecting as many as 28.8% of Americans over their lifetime (Kessler et al. 2005). The estimated cost associated with these disorders is between $42.3 and $46.6 billion annually (Dupont et al. 1996; Greenberg et al. 1999). Substantial research has been done on anxiety disorders in the past three decades. However, there is still much about the long-term course of anxiety disorders that is unknown. While a clearer picture is emerging with regard to age of onset of anxiety disorders (Christie et al. 1988; Battaglia et al. 1995; Kessler et al. 2005), fewer data are available regarding the trajectory of anxiety disorders during the transition from middle into older adulthood and beyond. Given the rapid ageing of the US population, in which one out of five people will be over 65 by the year 2030 (US Census Bureau, 2004), improved understanding of the effects of age on course of mental disorders is an important public health issue.
Most cross-sectional studies have found a decrease in anxiety symptoms and/or anxiety disorders in older age groups (Regier et al. 1988; Henderson et al. 1998; Jorm, 2000; Schaub & Linden, 2000; Sheikh et al. 2004; Kessler et al. 2005), although other studies have found no reduction or an increase in prevalence in older age groups (Eaton et al. 1989; Beekman et al. 1998). While these cross-sectional studies provide a rich ‘snapshot’ of anxiety in various age groups at a single point in time, this approach does not preclude the possibility of a cohort effect (i.e. differences in prevalence of anxiety disorders among different birth cohorts). In addition, cross-sectional designs reveal little about the course of anxiety disorders; longitudinal studies are needed to answer these questions. In the few existing longitudinal investigations of anxiety course in the literature, anxiety status has typically been assessed at baseline and long-term follow-up (e.g. intake and 5-year follow-up) (Goenjian et al. 2000; Carpiniello et al. 2002; Schuurmans et al. 2005). This design is informative regarding long-term outcome of anxiety disorders, but it does not take into account the symptomatology that occurs in the long periods between assessment points. In addition, many previous studies have used a categorical approach to anxiety diagnosis (Regier et al. 1988; Beekman et al. 1998; Kessler et al. 2005), which does not identify those individuals who do not meet full criteria, but remain symptomatic. Attention to full-criteria diagnoses only may underestimate the true prevalence of individuals who are experiencing impairment due to anxiety symptoms. Neither cross-sectional investigations nor long-term follow-up studies, particularly those that only examine full-criteria anxiety diagnoses, provide a comprehensive picture of the longitudinal course of anxiety disorders. Longitudinal designs that use short-interval assessment periods, and that take the full range of anxiety symptom severity into account, are another approach for addressing these questions, particularly with regard to assessing interactions between age and course in anxiety disorders.
The present study utilizes the naturalistic, prospective, longitudinal design of the Harvard–Brown Anxiety Research Program (HARP) to elucidate the course of anxiety disorders in a sample composed largely of middle-aged adults. Participants were evaluated using structured interviews administered at short intervals (every 6–12 months) over a 14-year span, providing a unique opportunity to gather information on severity of anxiety disorders as participants age. Both full and subcriteria anxiety symptoms were tracked at each follow-up interview in order to describe course even in the absence of a full criteria disorder. The aims of the current investigation are to examine: (1) how the longitudinal course of anxiety changes over time in individuals with panic disorder with (PDA) or without (PD) agoraphobia, social phobia (SP) and generalized anxiety disorder (GAD) over a 14-year period; (2) the impact of age on the course of PD/A, SP and GAD; (3) whether there is an interaction of age and time on anxiety course.
Method
Recruitment
This study was conducted using data from HARP, a longitudinal, prospective, study of adults with a current or past history of anxiety disorders. From 1989–1991, 711 participants entered the HARP study from 11 different New England area out-patient clinical treatment facilities ranging from psychiatric clinics to primary care settings. These methods are described in detail elsewhere (Massion et al. 1993). HARP inclusion criteria included a past or current full-criteria diagnosis of the following at intake : PD/A, SP or GAD. Insufficient for inclusion, but often seen as co-morbid conditions, were diagnoses of simple phobia, posttraumatic stress disorder, obsessive–compulsive disorder, or anxiety disorder not otherwise specified. Participants were at least 18 years of age at intake, were willing to participate in the study, and signed a written consent form. Exclusion criteria consisted of the presence of an organic brain disorder or a history of schizophrenia, or current psychosis at intake. All other co-morbidity was allowed.
Diagnostic assessment
The initial comprehensive evaluation assessed lifetime history using the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (DSM)-III-R Non-Affective Disorders – Patient Version (SCID-P; Spitzer et al. 1988) and the Research Diagnostic Criteria (RDC) Schedule for Affective Disorders – Lifetime (SADS-L; Endicott & Spitzer, 1978). Items on the SCID-P and SADS-L were combined to create the SCALUP, a structured interview used to assess diagnoses at intake. The instrument yielded both present and past RDC diagnoses for affective disorders and DSM-III-R diagnoses for non-affective (including anxiety) disorders. Interviews were conducted by bachelor’s- or master’s-level clinical interviewers and usually took place in single sessions lasting 2–4 h.
Follow-up interviews were conducted at 6- to 12-month intervals as follows: every 6 months for the first 2 years, annually for years 3–6, every 6 months in years 7–13, and annually thereafter. These interviews utilized the Longitudinal Interval Follow-up Evaluation-Upjohn (LIFE-UP; Keller et al. 1987), which assesses the weekly course of axis I disorders with psychiatric status ratings (PSRs) ranging from 1 to 6. Weekly PSRs are assigned for each disorder by clinical interviewers at each follow-up point, for all weeks since last follow-up, based on the participant’s report of his or her symptoms during the reporting interval. For the current study, only the highest weekly PSR in the 4-week period preceding each follow-up interview was examined. The greatest severity of illness, a PSR of 6, requires full DSM-III-R criteria in addition to severely disrupted functioning. A PSR of 3 or 4 indicates moderate to major symptoms related to the disorder, but fewer symptoms than necessary for a full criteria diagnosis. A PSR of 1 indicates an absence of symptoms and full remission of a given disorder. As an illustration, an individual with SP who receives a PSR of 4 would meet full DSM-III-R criteria for SP with the exception of criterion E (impairment in functioning or marked distress about phobic fears). Table 1 displays the general PSR scale used by the study; specific PSR scales for individual diagnoses can be found elsewhere (Warshaw et al. 2001; Yonkers et al. 2001).
Table 1.
Weekly psychiatric status rating scale
| Code | Term | Criteria |
|---|---|---|
| 6 | Full criteria, severe | Meets DSM-III-R or Research Diagnostic Criteria for definite disorder, has severe symptoms, and has extreme impairment in functioning |
| 5 | Full criteria | Meets criteria for definite disorder but has no extreme impairment in functioning |
| 4 | Marked | Does not meet the criteria for the disorder but has major symptoms of impairment resulting from this disorder (for example, a participant with a depressive episode who only meets four of the DSM-III-R criteria for major depressive episode but is not able to work) |
| 3 | Partial recovery | Considerably less psychopathologic impairment than full criteria and no more than moderate impairment in functioning, but still has obvious evidence of disorder (this category may represent worsening or improvement in a participant’s prior status; for example, the participant may experience limited symptom panic attacks) |
| 2 | Residual | Either participant claims not to be completely his/her self, or rater notes presence of symptoms of no more than a mild degree (for example, mild anxiety in agoraphobic situations) |
| 1 | Usual self | Participant is returned to his/her usual self, without any residual symptoms of this disorder (the participant may have significant symptoms from some other condition or disorder; if so, a psychiatric status rating should be recorded under that condition or disorder) |
DSM-III-R, Diagnostic and Statistical Manual of Mental Disorders – III (Revised).
Inter-rater reliability studies conducted on the LIFE-UP found good to excellent agreement on PSR scores. Intra-class correlation coefficients for each of the disorders were as follows: 0.67–0.88 for PD, 0.78–0.86 for GAD, 0.75–0.86 for SP and 0.73–0.74 for major depressive disorder (MDD) (Warshaw et al. 1994). Long-term test–retest of patients’ recall over 1 year also found very good to excellent reliability for the anxiety disorders and for MDD. A more recent examination of inter-rater reliability within the HARP sample also yielded similar results in the very good to excellent range (Warshaw et al. 2001). Good concurrent and discriminant validity was found in a separate external validity assessment comparing PSRs with other psychosocial measures (Warshaw et al. 1994).
Sample characteristics
Of the total of 711 participants who completed a baseline interview, 84% (n=594) met criteria for one or more of PD/A, GAD or SP diagnoses at baseline, and 76% of 594 (n=453) had sufficient follow-up data to be included in the current analyses, which comprised the first 14 years of the study period. Specifically, participants with SP and GAD at baseline were included in the current analyses if they completed at least two follow-up interviews. Given the more episodic nature of PD (Bruce et al. 2005), completion of at least three follow-up interviews was necessary for individuals with PD at baseline to be included in the analyses. This inclusion method resulted in 43 participants (24% of all participants with SP at baseline) being excluded from the final SP sample for the current analyses, 37 participants (21% of all participants with GAD at baseline) being excluded from the final GAD sample, and 122 participants (28% of all participants with PD at baseline) being excluded from the final PD sample. Relative to the 141 participants who had insufficient follow-up data to be included in any of the three final diagnostic samples, those included in the current analyses were more likely to be married (53.4 v. 42.6%, χ2=5.08, p=0.024), less likely to have co-morbid MDD at intake (27.4% v. 36.9%, χ2=4.66, p=0.031) and had higher general functioning on average as measured by the global assessment of functioning (GAF) [t(591)=2.16, p=0.031]. There were no other differences between excluded participants and the final sample on any demographic or clinical indices.
Table 2 lists descriptive characteristics for the analytic sample at baseline, including mean number of data points (i.e. follow-up interviews) per participant, according to diagnostic group. The total of these three groups exceeds 453 because the diagnostic groups are not mutually exclusive; 27% of the 453 participants in the current sample met criteria for more than one disorder at intake. The total number of participants per diagnostic group is also listed in Table 2. The number of participants for whom data were available at each time point varied considerably; for the PD analyses, available data per year ranged from n=111 to n=269 (median=173.5); available data for GAD ranged from n=49 to n=123 (median=68.5); and for SP from n=37 to n=111 (median=57.5).
Table 2.
Descriptive characteristics for analytic sample by diagnostic group at baseline
| Variable | PD (n=317) | GAD (n=142) | SP (n=133) |
|---|---|---|---|
| Female (%) | 69.1 | 71.8 | 57.9 |
| Age, years (S.D.) | 40.3 (11.3) | 40.5 (12.2) | 40.1 (11.1) |
| Age range (years) | 17.8–73.7 | 19.0–72.9 | 18.0–68.1 |
| Married (%) | 55.2 | 51.4 | 48.9 |
| At least some college (%) | 66.9 | 67.6 | 65.4 |
| Low socio-economic status (%) | 27.7 | 24.1 | 27.1 |
| Agoraphobia (PD only) (%) | 83.0 | ||
| MDD (%) | 22.1 | 37.3 | 33.8 |
| PD (%) | 52.1 | 44.4 | |
| GAD (%) | 19.9 | 33.8 | |
| SP (%) | 15.5 | 32.4 | |
| GAF (S.D.) | 60.7 (10.5) | 56.8 (11.1) | 56.3 (10.6) |
| Years with diagnosis (S.D.) | 12.5 (11.8) | 19.2 (14.0) | 24.9 (13.5) |
| Number of follow-up interviews (S.D.) | 7.9 (3.0) | 7.3 (3.6) | 6.8 (3.4) |
PD, Panic disorder; GAD, generalized anxiety disorder, SP, social phobia; S.D., standard deviation; MDD, major depressive disorder; GAF, global assessment of functioning.
Analytic approach
We examined the course of PD, GAD and SP over the first 14 years of the study period using separate longitudinal growth models estimated with SAS version 9.1 (SAS Institute, Inc., Cary, NC, USA). The growth modeling framework is a flexible and useful way to examine anxiety disorder course as a continuous linear function that is characterized by an intercept and a slope. This parameterization has a clear interpretation for growth parameters (intercept is starting point, slope is rate of change), and other parameters in the model are also clear to interpret. Main effects are effects on starting point, whereas associations between covariates and course over time can be examined through interaction terms with the slope.
For each disorder, severity was operationalized as the highest weekly PSR in the 4-week period preceding each follow-up interview. We chose this method of operationalizing severity as a way to gauge maximum severity related to the anxiety diagnosis in question proximal to each follow-up point, while covering a relatively brief period (4 weeks prior to interview) in order to keep any bias related to retrospective recall to a minimum. For all disorders, two growth models were estimated, a main effects model with time and age as predictors of PSR growth over time, and an interaction model that included the time×age interaction term. All models included a random effect for study site, and the following intake data as covariates based on previous research (Warshaw et al. 1997; Zlotnick et al. 2001; Yonkers et al. 2003; Bruce et al. 2005): demographic variables including education, gender, marital status and socio-economic status (based on Hollingshead ratings); co-morbid conditions including MDD, SP (for GAD and PD groups), GAD (for SP and PD groups) and agoraphobia (for PD group only); and general severity variables including GAF, and length of time since the onset of the anxiety disorder (according to participants’ retrospective report).
Results
Main effects
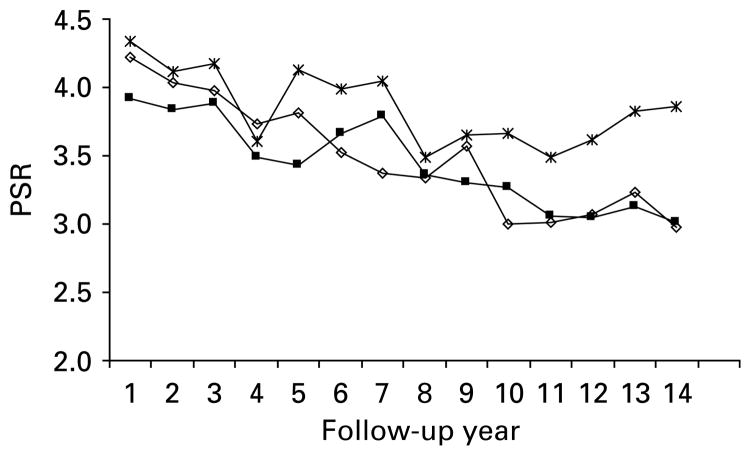
In the main effects models, time had a significant effect on anxiety course in the PD, GAD and SP models, respectively. Specifically, PSRs decreased significantly over the 14-year study period for all three disorders (see Table 3). Fig. 1 displays the PSR values for PD, GAD and SP from follow-up years 1–14. Although direct statistical comparison of these trends for the three disorders is not possible because the diagnostic groups are not mutually exclusive, the curves for PD and GAD appear to both have steeper downward slopes and lower mean PSRs at year 14 compared with SP.
Table 3.
Parameter estimates for PSR growth factors and covariates : main effects models
| Variable | PD (n=317) | GAD (n=142) | SP (n=133) |
|---|---|---|---|
| Intercept | 6.573 (0.648)*** | 3.665 (1.219)** | 6.613 (1.108)*** |
| Gender | 0.154 (0.142) | 0.003 (0.256) | 0.164 (0.238) |
| Marital status | −0.174 (0.133) | −0.366 (0.234) | −0.287 (0.247) |
| At least some college | −0.459 (0.155)** | 0.195 (0.280) | −0.113 (0.289) |
| Socio-economic status | −0.121 (0.162) | −0.073 (0.288) | 0.102 (0.293) |
| Agoraphobia (PD only) | 0.223 (0.181) | ||
| MDD | 0.005 (0.169) | 0.160 (0.251) | −0.325 (0.264) |
| PD | 0.423 (0.335) | −0.223 (0.361) | |
| GAD | −0.086 (0.165) | −0.016 (0.240) | |
| SP | −0.261 (0.183) | 0.367 (0.242) | |
| GAF | −0.035 (0.007)*** | −0.016 (0.011) | −0.031 (0.012)** |
| Length of time since disorder onset | 0.014 (0.007)* | 0.015 (0.009)† | −0.004 (0.013) |
| Age | −0.015 (0.007)* | 0.009 (0.011) | −0.004 (0.017) |
| Time | −0.076 (0.006)*** | −0.094 (0.009)*** | −0.054 (0.008)*** |
PSR, Psychiatric status rating; PD, panic disorder; GAD, generalized anxiety disorder, SP, social phobia; MDD, major depressive disorder; GAF, global assessment of functioning.
Values are given as mean (standard error).
p<0.1,
p<0.05,
p<0.01,
p<0.001.
Fig. 1.
Mean panic disorder (■), social phobia (×) and generalized anxiety disorder (◇) psychiatric status ratings (PSRs) over the 14-year study period.
In the main effects model for PD, the covariates education, GAF, length of intake episode, and age all significantly predicted PD severity at year 1. Specifically, participants with less education, lower GAF scores, longer length of time since disorder onset, and younger age tended to have higher year 1 PSRs. In the GAD model, none of the covariates significantly predicted year 1 severity, although the effect of length of time since disorder onset approached significance (p<0.1). In the SP model, lower GAF scores at intake were associated with greater year 1 severity.
Interaction effects
In the interaction effects models, age×time had a significant effect on course for PD and GAD, but not for SP (Table 4). Specifically, older age was associated with lower PSRs (a steeper downward slope in the growth curve) over time in both PD and GAD. There was no significant age×time interaction for SP.
Table 4.
Parameter estimates for PSR growth factors and covariates : age×time interaction effects model
| Variable | PD (n=317) | GAD (n=142) | SP (n=133) |
|---|---|---|---|
| Intercept | 6.236 (0.663)*** | 3.120 (1.236)* | 6.341 (1.121)*** |
| Gender | 0.150 (0.142) | 0.009 (0.258) | 0.169 (0.238) |
| Marital status | −0.174 (0.133) | −0.369 (0.234) | −0.290 (0.246) |
| At least some college | −0.461 (0.155)** | 0.280 (0.280) | −0.127 (0.289) |
| Socio-economic status | −0.112 (0.162) | −0.086 (0.288) | 0.108 (0.293) |
| Agoraphobia (PD only) | 0.222 (0.181) | ||
| MDD | 0.009 (0.169) | 0.163 (0.251) | −0.320 (0.264) |
| PD | 0.430 (0.336) | −0.219 (0.361) | |
| GAD | −0.083 (0.165) | −0.011 (0.239) | |
| SP | −0.262 (0.183) | 0.375 (0.242) | |
| GAF | −0.035 (0.007)*** | −0.016 (0.011) | −0.031 (0.012)† |
| Length of time since disorder onset | 0.014 (0.007)* | 0.015 (0.009)† | 0.004 (0.013) |
| Age | −0.006 (0.008) | 0.021 (0.012)† | −0.002 (0.017) |
| Time | −0.021 (0.023) | −0.008 (0.031) | −0.008 (0.031) |
| Age×time | −0.001 (0.001)* | −0.002 (0.001)** | 0.001 (0.001) |
PSR, Psychiatric status rating; PD, panic disorder; GAD, generalized anxiety disorder; SP, social phobia; MDD, major depressive disorder; GAF, global assessment of functioning.
Values are given as mean (standard error).
p<0.1,
p<0.05,
p<0.01,
p<0.001.
In the interaction effects model for PD, less education, lower GAF scores, and longer length of time since disorder onset continued to be significantly associated with higher year 1 PSRs, although age and time were no longer significant. In the GAD model, length of time since disorder onset and age were marginally significant (p<0.1). In the SP model, GAF scores were marginally significant in predicting year 1 severity.
Discussion
The current study examined semi-annual and annual anxiety disorder severity ratings over 14 years of follow- up in order to assess how the longitudinal course of anxiety disorders changes over time, adjusting for baseline demographic and clinical factors. The HARP study involves the assignment of weekly psychiatric severity ratings (PSRs) for PD, SP and GAD obtained at prospectively observed time points across the entire study period. In order to adequately gauge anxiety-related impairment during the 14-year study period examined, taking into account the frequent symptom fluctuations that individuals with anxiety disorders experience, the most severe weekly PSR assigned in the 4 weeks prior to each follow-up interview was selected for the current analysis. We limited our inquiry to the 4 weeks prior to each follow-up point in order to minimize bias related to retrospective recall. The current investigation’s methodology represents a departure from other studies in the anxiety literature (Regier et al. 1988; Beekman et al. 1998; Kessler et al. 2005), including some of our own previous work (Yonkers et al. 1998, 2003; Bruce et al. 2005), which have typically examined either the presence/absence of full-criteria diagnoses at a particular point in time, or the probability of relapse or recurrence of full-criteria episodes in a given year. The current study instead examined the full range of anxiety severity ratings, allowing a detailed assessment of anxiety symptoms and related impairment across 14 years of follow-up. We believe this approach represents a novel examination of the course of anxiety disorders and offers different and complementary information on longitudinal course, compared with that provided by previous studies.
The main finding of the current study is that, on average, the severity of anxiety symptoms during episodes of anxiety disorders decreased over time for each of the anxiety disorders examined – PD, GAD and SP. These findings add to the limited empirical data available on the long-term course of anxiety disorders, particularly the course of anxiety disorders in middle-aged and older adults (Weisberg et al. 2002; Lenze et al. 2005; Schuurmans et al. 2005). Most previous, largely cross-sectional studies have suggested that the prevalence of anxiety disorders and symptoms decrease over time or with advancing age. The current study has several strengths that add weight to previous findings. First, the HARP study makes use of a structured diagnostic interview to assess anxiety symptoms, instead of relying exclusively on self-report measures. Second, the current study uses a short-interval (6–12 months) follow-up design that takes into account anxiety symptoms that occur between follow-up points, in contrast to previous studies in which follow-up periods typically average several years. A third strength of the current study is the 14-year follow-up period covered. We were unable to find other studies with comparably long periods during which adult participants with anxiety disorders were continuously followed. Fourth, the current study tracked both categorical (full-criteria) and dimensional anxiety ratings, thus capturing data that would otherwise be lost. In our study, if only full-criteria anxiety diagnoses (e.g. PSR 5 or 6) were tracked, it would appear that most participants had remitted over 14 years, when in fact many participants continue to experience significant impairment without meeting full criteria for the anxiety disorder in question. Thus, this method reveals a far more chronic course of anxiety disorders than would be uncovered with categorical anxiety diagnoses tracking alone.
The decrease in severity appeared to be relatively modest for all three disorders assessed, as all disorders decreased at a rate of about 1 PSR over the 14-year period. Therefore, while most individuals in each diagnostic group no longer met full criteria for that disorder by the end of the follow-up period, it is important to note that the majority were still symptomatic and experiencing at least moderate impairment related to that disorder 14 years later. These findings suggest that the natural course of anxiety disorders is characterized by remarkable persistence over time. One possible reason for continuing persistence of symptoms and impairment may be due to the fact that many participants in our sample are not receiving sufficient treatment, whether in the form of psychotropic medication or evidence-based psychotherapies (Goisman et al. 1999; Vasile et al. 2005). Another possibility, although somewhat speculative, is that individuals with anxiety disorders make changes in their lives such that their anxiety symptoms becoming less impairing over time. For example, an individual with SP may pick a profession in which they do not have to confront the social fears which they found unavoidable, and thus more impairing and distressing, in college. In another scenario, a person with PDA may make life-style modifications, such as taking public transportation instead of driving, which lead to a decrease in panic attacks and associated impairment. This chronic avoidance may lead to a partial remission of their diagnosis, although such behavioral changes may not lead to a complete resolution of anxiety symptoms and impairment. We also know from previous HARP findings that subcriteria symptoms are a risk factor for relapse (Weisberg et al. 2002), suggesting that the individuals in our sample who no longer meet full criteria for an anxiety diagnosis but remain symptomatic are at continued risk for a return to full-criteria diagnoses in the future.
The current finding of anxiety persistence over 14 years of follow-up is notable given that our final sample may represent individuals with a less severe course than those participants excluded from the current analysis. Specifically, the final sample was more likely to be married, had less co-morbid MDD, and had higher GAF scores at baseline, relative to those participants not included in the current analyses. We have previously found each of these factors to be associated with worse course of anxiety disorders within the HARP sample (Yonkers et al. 2000; Bruce et al. 2001, 2005; Zlotnick et al. 2001). Thus, it is possible that participants lost to follow-up and/or not included in the current analysis may be experiencing even greater persistence of anxiety symptoms. Consequently, it is possible that the current findings actually underestimate the chronicity of anxiety course.
Direct statistical comparison of the growth curves for the three disorders was not possible because the participant groups were not mutually exclusive. Consequently, we were unable to determine conclusively whether each disorder was associated with a distinct trajectory over the study period. In the present study, the growth curves for PD and GAD appeared to have somewhat steeper downward slopes than that for SP. This could suggest a more pronounced decrease in symptom severity over time for PD and GAD, while SP may decrease more slowly. The SP group also had a higher mean severity rating at year 14 than either GAD or PD. The possibility of an attenuated decline in symptoms and higher severity in year 14 observed in SP may suggest a worse course compared with GAD and PD, which would be consistent with previous findings (Bruce et al. 2005). However, definite conclusions about the greater chronicity of SP relative to other anxiety disorders must await further empirical investigation.
In the interaction effects model, an age×time interaction emerged for PD and GAD, although this was not true for SP. These findings suggest that course of PD and GAD progress differentially according to age, with older adults experiencing a steeper decline in severity over time versus younger adults. Although the panic sample was much larger than that of the two other diagnostic groups, possibly allowing more findings to emerge in the PD analyses, it is possible that these findings reveal true differences in the course of the different anxiety disorders. For example, it has been suggested that PD ‘burns out’ with age such that elderly adults have fewer panic attacks due to physiological and neurological changes associated with ageing (Sheikh et al. 1991). The current study may support this assumption, although our sample was mostly middle-aged, and thus did not provide a direct test of the ‘burnout’ hypothesis as it applies to older adults. While the findings of the current study may accurately describe the course of anxiety during mid-life, it is unknown whether these findings would hold true for anxiety severity in other age groups, or over longer follow-up periods. For example, a recent study using a cross-sectional sample of adults aged 18–90 years found a non-linear pattern of anxiety course, suggesting an increase in anxiety symptoms until early adulthood, followed by a decrease in symptoms during middle-age into old age, and an increase again during the eighth decade of life (Teachman, 2006).
The current study has several important limitations. First, the current findings may not be representative of individuals with anxiety disorders in the general population for several reasons: some participants were excluded from the current analyses due to insufficient data, all participants were receiving treatment at baseline and many continued to do so throughout the study, and individuals with anxiety disorders seeking treatment today may differ from participants in the current sample, who first enrolled in the current study in 1989–1991. As discussed earlier, individuals in our final sample may have less severe course versus those participants who were excluded. As for treatment, although all participants were treatment-seeking at baseline, we have not found treatment utilization to be a significant predictor of course in our sample (Bruce et al. 2003; Vasile et al. 2005). It is unclear how course of anxiety disorders in non-treatment-seeking individuals would compare with that in the current sample, although one recent study found that individuals with more severe cases of SP were less likely to seek treatment than those with milder cases (Ruscio et al. 2008). While the fact that participants enrolled in the current study almost 20 years ago may reduce our ability to extrapolate to individuals with anxiety disorders today, this is one of the necessary limitations of longitudinal designs. All of these limitations on generalizability should be taken into account when considering the current findings.
In addition to generalizability, there are several additional limitations to the current findings. First, the current study employed DSM-III-R criteria. While there are some differences between DSM-III-R and DSM-IV criteria for the anxiety disorders examined here, most notably for GAD and PD, previous research has found that the vast majority of individuals with these diagnoses classified according to DSM-III-R criteria would also meet DSM-IV criteria (Abel & Borkovec, 1995; Fyer et al. 1996). Second, those diagnosed with PD with and without agoraphobia were considered together in the current analysis. This may obscure differences between PD and PDA, as other research has suggested differences in course for these two groups (Keller et al. 1994; Warshaw et al. 1997). Third, the current findings may be informative about the general trajectory of each of the anxiety disorders examined, but less relevant for individuals with these anxiety disorders, since the current analysis focuses on the interindividual average of all intra-individual trajectories. Fourth, the course of co-morbid conditions was not examined in the current analysis, which further impacts the relevance of the current findings for individuals. For example, while our PD group’s panic diagnoses may have improved over time, we did not examine what was happening to their other diagnoses, or whether they experienced the onset of new conditions over time. Finally, we chose to operationalize anxiety disorder severity for each participant as the highest weekly severity rating (PSR) assigned in the 4-week period prior to each follow-up interview – investigators using different methods may obtain different results. Despite these notable limitations, we believe that the current study contributes a significant ‘piece ’ to the larger puzzle of understanding long-term prognosis in anxiety disorders.
In conclusion, the current study adds a novel contribution to the existing literature on course of anxiety disorders by examining the range of full and subcriteria anxiety severity ratings over time, controlling for several baseline demographic and clinical variables. The present findings suggest that anxiety severity declines over time, although this decline is modest and may partially depend on the disorder being assessed. In addition, older individuals with PD and GAD appear to have a better prognosis than their younger counterparts, in that their course is characterized by a steeper decline in severity. The present findings may be particularly relevant to the course of anxiety in middle-aged, treatment-seeking adults. Future investigators employing similar, naturalistic, prospective designs should examine the trajectory of anxiety disorders in adults over age 65 years, and should assess the impact of additional risk factors (e.g. psychosocial stressors, medical co-morbidity) on course of anxiety disorders.
Acknowledgments
This research was supported by National Institute of Mental Health (NIMH) grant MH-51415. SCALUP, a structured interview used to assess diagnoses at intake, is available from M.B.K. upon request.
Footnotes
Declaration of Interest
None.
References
- Abel JL, Borkovec TD. Generalizability of DSM-III-R generalized anxiety disorders to proposed DSM-IV criteria and cross-validation of proposed changes. Journal of Anxiety Disorders. 1995;9:303–315. [Google Scholar]
- Battaglia M, Bertella S, Politi E, Bernardeschi L, Perna G, Gabriele A, Bellodi L. Age at onset of panic disorder – influence of familial liability to the disease and of childhood separation anxiety disorder. American Journal of Psychiatry. 1995;152:1362–1364. doi: 10.1176/ajp.152.9.1362. [DOI] [PubMed] [Google Scholar]
- Beekman ATF, Bremmer MA, Deeg DJH, van Balkom AJLM, Smit JH, de Beurs E, van Dyck R, van Tilburg W. Anxiety disorders in later life : a report from the longitudinal aging study Amsterdam. International Journal of Geriatric Psychiatry. 1998;13:717–726. doi: 10.1002/(sici)1099-1166(1998100)13:10<717::aid-gps857>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Bruce SE, Machan JT, Dyck I, Keller MB. Infrequency of ‘pure’ GAD: impact of psychiatric comorbidity on clinical course. Depression and Anxiety. 2001;14:219–225. doi: 10.1002/da.1070. [DOI] [PubMed] [Google Scholar]
- Bruce SE, Vasile RG, Goisman RM, Salzman C, Spencer M, Machan JT, Keller MB. Are benzodilazepines still the medication of choice for patients with panic disorder with or without agoraphobia ? American Journal of Psychiatry. 2003;160:1432–1438. doi: 10.1176/appi.ajp.160.8.1432. [DOI] [PubMed] [Google Scholar]
- Bruce SE, Yonkers KA, Otto MW, Eisen JL, Weisberg RB, Pagano M, Shea MT, Keller MB. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder : a 12-year prospective study. American Journal of Psychiatry. 2005;162:1179–1187. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpiniello B, Baita A, Carta MG, Sitzia R, Macciardi AM, Murgia S, Altamura AC. Clinical and psychosocial outcome of patients affected by panic disorder with or without agoraphobia : results from a naturalistic follow-up study. European Psychiatry. 2002;17:394–398. doi: 10.1016/s0924-9338(02)00701-0. [DOI] [PubMed] [Google Scholar]
- Christie KA, Burke JD, Regier DA, Rae DS, Boyd JH, Locke BZ. Epidemiologic evidence for early onset of mental disorders and higher risk of drug abuse in young adults. American Journal of Psychiatry. 1988;145:971–975. doi: 10.1176/ajp.145.8.971. [DOI] [PubMed] [Google Scholar]
- Dupont RL, Rice DP, Miller LS, Shiraki SS, Rowland CR, Harwood HJ. Economic costs of anxiety disorders. Anxiety. 1996;2:167–172. doi: 10.1002/(SICI)1522-7154(1996)2:4<167::AID-ANXI2>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Eaton WW, Kramer M, Anthony JC, Dryman A, Shapiro S, Locke BZ. The Incidence of specific DIS/DSM-III mental disorders : data from the NIMH Epidemiologic Catchment Area Program. Acta Psychiatrica Scandinavica. 1989;79:163–178. doi: 10.1111/j.1600-0447.1989.tb08584.x. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview : the Schedule for Affective Disorders and Schizophrenia (SADS-L) Archives of General Psychiatry. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- Fyer AJ, Katon W, Hollifield M, Rassnick H, Mannuzza S, Chapman T, Ballenger JC. The DSM-IV panic disorder field trial : panic attack frequency and functional disability. Anxiety. 1996;2:157–166. doi: 10.1002/(SICI)1522-7154(1996)2:4<157::AID-ANXI1>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Goenjian AK, Steinberg AM, Najarian LM, Fairbanks LA, Tashjian M, Pynoos RS. Prospective study of posttraumatic stress, anxiety, and depressive reactions after earthquake and political violence. American Journal of Psychiatry. 2000;157:911–916. doi: 10.1176/appi.ajp.157.6.911. [DOI] [PubMed] [Google Scholar]
- Goisman RM, Warshaw MG, Keller MB. Psychosocial treatment prescriptions for generalized anxiety disorder, panic disorder, and social phobia, 1991–1996. American Journal of Psychiatry. 1999;156:1819–1821. doi: 10.1176/ajp.156.11.1819. [DOI] [PubMed] [Google Scholar]
- Greenberg PE, Sisitsky T, Kessler RC, Finkelstein SN, Berndt ER, Davidson JRT, Ballenger JC, Fyer AJ. The economic burden of anxiety disorders in the 1990s. Journal of Clinical Psychiatry. 1999;60:427–435. doi: 10.4088/jcp.v60n0702. [DOI] [PubMed] [Google Scholar]
- Henderson AS, Jorm AF, Korten AE, Jacomb P, Christensen H, Rodgers B. Symptoms of depression and anxiety during adult life : evidence for a decline in prevalence with age. Psychological Medicine. 1998;28:1321–1328. doi: 10.1017/s0033291798007570. [DOI] [PubMed] [Google Scholar]
- Jorm AF. Does old age reduce the risk of anxiety and depression ? A review of epidemiological studies across the adult life span. Psychological Medicine. 2000;30:11–22. doi: 10.1017/s0033291799001452. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, Mcdonaldscott P, Andreasen NC. The Longitudinal Interval Follow-up Evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Keller MB, Yonkers KA, Warshaw MG, Pratt LA, Gollan JK, Massion AO, White K, Swartz AR, Reich J, Lavori PW. Remission and relapse in subjects with panic disorder and panic with agoraphobia : a prospective short-interval naturalistic follow-up. Journal of Nervous and Mental Disease. 1994;182:290–296. doi: 10.1097/00005053-199405000-00007. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Walters EE. Lifetime prevalence and age-of-onset distributions’ of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Mulsant BH, Mohlman J, Shear MK, Dew MA, Schulz R, Miller MD, Tracey B, Reynolds CF., 3rd Generalized anxiety disorder in late life : lifetime course and comorbidity with major depressive disorder. American Journal of Geriatric Psychiatry. 2005;13:77–80. doi: 10.1176/appi.ajgp.13.1.77. [DOI] [PubMed] [Google Scholar]
- Massion AO, Warshaw MG, Keller MB. Quality of life and psychiatric morbidity in panic disorder and generalized anxiety disorder. American Journal of Psychiatry. 1993;150:600–607. doi: 10.1176/ajp.150.4.600. [DOI] [PubMed] [Google Scholar]
- Regier DA, Boyd JH, Burke JD, Rae DS, Myers JK, Kramer M, Robins LN, George LK, Karno M, Locke BZ. One-month prevalence of mental disorders in the United States. Based on five Epidemiologic Catchment Area sites. Archives of General Psychiatry. 1988;45:977–986. doi: 10.1001/archpsyc.1988.01800350011002. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, Kessler RC. Social fears and social phobia in the USA: results from the National Comorbidity Survey Replication. Psychological Medicine. 2008;38:15–28. doi: 10.1017/S0033291707001699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaub RT, Linden M. Anxiety and anxiety disorders in the old and very old – results from the Berlin Aging Study (BASE) Comprehensive Psychiatry. 2000;41:48–54. doi: 10.1016/s0010-440x(00)80008-5. [DOI] [PubMed] [Google Scholar]
- Schuurmans J, Comijs HC, Beekman ATF, de Beurs E, Deeg DJH, Emmelkamp PMG, van Dyck R. The outcome of anxiety disorders in older people at 6-year follow-up : results from the Longitudinal Aging Study Amsterdam. Acta Psychiatrica Scandinavica. 2005;111:420–428. doi: 10.1111/j.1600-0447.2005.00531.x. [DOI] [PubMed] [Google Scholar]
- Sheikh JI, King RJ, Taylor CB. Comparative phenomenology of early-onset versus late-onset panic attacks : a pilot survey. American Journal of Psychiatry. 1991;148:1231–1233. doi: 10.1176/ajp.148.9.1231. [DOI] [PubMed] [Google Scholar]
- Sheikh JI, Swales PJ, Carlson EB, Lindley SE. Aging and panic disorder : phenomenology, comorbidity, and risk factors. American Journal of Geriatric Psychiatry. 2004;12:102–109. [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R – Patient Version (SCID-P) New York State Psychiatric Institute; New York: 1988. [Google Scholar]
- Teachman BA. Aging and negative affect : the rise and fall and rise of anxiety and depression symptoms. Psychology and Aging. 2006;21:201–207. doi: 10.1037/0882-7974.21.1.201. [DOI] [PubMed] [Google Scholar]
- US Census Bureau. [Accessed 20 May 2008];US interim projections by age, sex, race and Hispanic origin. 2004 ( http://www.census.gov/ipc/www/usinterimproj/)
- Vasile RG, Bruce SE, Goisman RM, Pagano M, Keller MB. Results of a naturalistic longitudinal study of benzodiazepine and SSRI use in the treatment of generalized anxiety disorder and social phobia. Depression and Anxiety. 2005;22:59–67. doi: 10.1002/da.20089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warshaw MG, Dyck I, Allsworth J, Stout RL, Keller MB. Maintaining reliability in a long-term psychiatric study : an ongoing inter-rater reliability monitoring program using the longitudinal interval follow-up evaluation. Journal of Psychiatric Research. 2001;35:297–305. doi: 10.1016/s0022-3956(01)00030-9. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Keller MB, Stout RL. Reliability and validity of the longitudinal interval follow-up evaluation for assessing outcome of anxiety disorders. Journal of Psychiatric Research. 1994;28:531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Massion AO, Shea MT, Allsworth J, Keller MB. Predictors of remission in patients with panic with and without agoraphobia: prospective 5-year follow-up data. Journal of Nervous and Mental Disease. 1997;185:517–519. doi: 10.1097/00005053-199708000-00007. [DOI] [PubMed] [Google Scholar]
- Weisberg RB, Machan JT, Dyck IR, Keller MB. Do panic symptoms during periods of remission predict relapse of panic disorder ? Journal of Nervous and Mental Disease. 2002;190:190–197. doi: 10.1097/00005053-200203000-00008. [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Bruce SE, Dyck IR, Keller MB. Chronicity, relapse, and illness – course of panic disorder, social phobia, and generalized anxiety disorder : findings in men and women from 8 years of follow-up. Depression and Anxiety. 2003;17:173–179. doi: 10.1002/da.10106. [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Dyck IR, Keller MB. An eight-year longitudinal comparison of clinical course and characteristics of social phobia among men and women. Psychiatric Services. 2001;52:637–643. doi: 10.1176/appi.ps.52.5.637. [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Dyck IR, Warshaw M, Keller MB. Factors predicting the clinical course of generalised anxiety disorder. British Journal of Psychiatry. 2000;176:544–549. doi: 10.1192/bjp.176.6.544. [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Zlotnick C, Allsworth J, Warshaw M, Shea T, Keller MB. Is the course of panic disorder the same in women and men? American Journal of Psychiatry. 1998;155:596–602. doi: 10.1176/ajp.155.5.596. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Bruce SE, Shea MT, Keller MB. Delayed posttraumatic stress disorder (PTSD) and predictors of first onset of PTSD in patients with anxiety disorders. Journal of Nervous and Mental Disease. 2001;189:404–406. doi: 10.1097/00005053-200106000-00011. [DOI] [PubMed] [Google Scholar]