Abstract
Aim
Characterize longitudinal patterns of substance use across a large sample of psychiatric patients discharged from inpatient admission, followed for 1-year post-hospitalization.
Design
Prospective cohort study.
Setting
Kansas City, Missouri, USA; Pittsburgh, Pennsylvania, USA; Worcester, Massachusetts, USA.
Participants
Eight hundred one schizophrenia-spectrum (N=204), bipolar (N=137) and depressive disorder (N=460) patients from the MacArthur Violence Risk Assessment Study.
Measurements
Symptoms, functioning, drug/alcohol use assessed by the Brief Psychiatric Rating Scale, the Global Assessment of Functioning, and substance use interviews.
Findings
Patients used alcohol (67.0%; N=540) and cannabis (30.0%; N= 237) more frequently than other substances up to 30 days before admission, and those with depressive and schizophrenia-spectrum used heroin more than individuals with bipolar (p = .023). Post-hospitalization, patients using alcohol (B = −.15, p <.001) and cannabis (B= −.27, p <.001) decreased, but patterns varied across diagnosis and genders. Patients using cannabis decreased at greater rates in depressive and schizophrenia-spectrum compared with bipolar (all p <.05), and more men used alcohol (B = .76, p < .001) and cannabis (B = 1.56, p < .001) than women. Cannabis (B = 1.65, p < .001) and alcohol (B = 1.04, p = .002) were associated with higher symptomatology; cannabis (B = −2.33, p < .001) and alcohol (B = −1.45, p = .012) were associated with lower functioning.
Conclusions
Substance use is frequent and associated with poor recovery in patients with serious mental illness recently discharged from psychiatric hospitalization. Addiction treatments personalized by diagnosis and gender may be effective for improving outcomes in people with serious mental illness.
Keywords: Substance Abuse, Addiction, Serious Mental Illness, Longitudinal Research
Introduction
The reported rates of substance use are higher among persons who experience serious mental illnesses (SMIs) than adults in the general population [1–7], and the use of drugs or alcohol is known to worsen the course of many major mental health conditions [7–17]. To date, epidemiological studies have procured general estimates of substance use among persons with SMIs [1–8], and have documented that substance use disorders (SUDs) are significantly comorbid with schizophrenia-spectrum, bipolar, and depressive disorders [1–8]. Evidence from community-based and clinical investigations also reports a high prevalence of comorbid SUDs among persons who are affected by these conditions [9–35], and that the use of drugs or alcohol by individuals with SMIs can substantially impede their recovery [9–19, 27, 31–35]. Indeed, considerable work has examined substance abuse and SMI [1–35], yet few longitudinal investigations have studied drug and alcohol use heterogeneity across the diverse population of individuals with SMIs.
Differences in demographic, clinical and substance use characteristics are important considerations for the treatment and recovery of persons with SMIs [9–10, 12, 14, 16, 33–35]. For example, a first-episode psychosis (FEP) study showed a greater proportion of males used substances compared to females, and that cannabis use was associated with greater degrees of positive symptomatology [9]. A similar study of FEP patients associated persistent drug/alcohol use with poorer remission rates from substances of abuse [10]. A study of adults with schizophrenia-spectrum disorders showed multiple substances were used in the sample, a greater proportion of males were diagnosed with SUDs, and alcohol use was associated with greater degrees of positive symptomatology [8]. A 10-year investigation of patients with schizophrenia-spectrum and bipolar disorders revealed alcohol use was associated with poorer rates of achieving a 6-month remission status over the follow-up period [14]. However, a three-year study revealed patients generally achieved remission from substances of abuse, with schizophrenia-spectrum disorder patients faring less well in terms of hospital readmission compared to patients with bipolar disorders [12, 16]. An investigation of adults with bipolar disorders associated persistent substance use with poorer functional outcomes [33], and similar research associated alcohol use with increased symptoms of depression for females but not for males [35]. A similar study associated persistent alcohol abuse with chronic course of depressive illness for females but not for males [34]. Indeed, heterogeneity in demographic, clinical and substance use characteristics can have a profound influence on the recovery of persons with different SMIs, which may signal sub-samples of patients at risk for addiction related problems, thus having implications for treatment.
Although previous research has identified characteristics that influence the recovery of persons with SMIs, improving outcomes is challenging [33, 36], and thus an investigation comparing the patterns of drug and alcohol use over time across patients with schizophrenia-spectrum, bipolar and depressive disorders is important. The present study sought to prospectively examine the longitudinal patterns of substance use in terms of recovery across a large and diverse sample of psychiatric patients. Accordingly, we followed 801 patients with schizophrenia-spectrum, bipolar and depressive disorders who participated in the MacArthur Violence Risk Assessment Study [37] for 1-year post-hospitalization, to examine: (1) longitudinal patterns in the proportion of patients using different substances; (2) diagnostic differences in the proportion of patients using substances; (3) associations between substance use, symptoms and functioning; and (4) diagnostic differences in the association between substance use, symptomatology and functional recovery.
Methods
Participants
Data were collected from the MacArthur Violence Risk Assessment Study; the results and methodological details are reported elsewhere [37]. The MacArthur Violence Risk Assessment Study assessed 1136 individuals every 10-weeks for 1-year post-hospitalization. Participants were recruited from consecutive inpatient admissions at: Pittsburgh, Pennsylvania; Kansas City, Missouri; and Worchester, Massachusetts [37]. Descriptions of each site and their sample characteristics can be found elsewhere [37–38]. Inclusion criteria required participants be able to read and comprehend English, be between the ages of 18 and 40, and have a medical chart diagnosis of SMI (e.g., schizophrenia, schizophreniform disorder, schizoaffective disorder, major depression, dysthymia, bipolar disorder, delusional disorder, or a personality disorder), which was verified by the DSM-III-R Checklist [39]. Inclusion criteria required participants be of risk for future violence, which was ascertained from patient self-report, collateral informants’ reports and official records (i.e. hospital and arrest records) [37]. Patients were excluded if they were hospitalized for longer than 145 days or if they had been under commitment for more than 21 days [38]; the median length of hospitalization was 9 days for those who met inclusion criteria [38]. We selected the 801 patients from the MacArthur Violence Risk Assessment Study sample with a psychiatric diagnosis within one of the following major categories of SMI: depressive, schizophrenia-spectrum, or bipolar disorders. These 801 patients comprised our sample, and we examined associations between substance use and recovery outcomes for patients with different SMIs during the 1-year post-hospitalization period.
Measures
Substance Use
Participants were assessed by trained raters via self-reported semi-structured interviews of drug and/or alcohol use when hospitalized and at each follow-up assessment post-hospitalization. Patients were asked to self-report their use of 10 types of illicit drugs (e.g. cannabis, heroin, cocaine, PCP, stimulants, opiates, psychedelics, inhalants, sedatives, other) and alcohol, and indicated (“Yes” = use; “No’ = no use) whether they had used the substance during the period assessed. Participants were rated as using if they admitted to any use (i.e. at least one time) for the period assessed.
Psychopathology
Psychiatric symptomatology and psychopathology were assessed using the Brief Psychiatric Rating Scale [41]. This instrument, consisting of 18-items, was administered by trained clinical raters using face-to-face interviews, and assesses psychopathology across symptom domains including; thought disturbance, suspiciousness/hostility, anergia, activation, and anxiety/depression. Each item is rated on a scale ranging from 1 (not present) to 7 (extremely severe), and corresponds with the degree to which symptoms are endorsed [41]. Ratings are computed by summing across symptom domains; higher scores are indicative of more serious symptomatology (18 = minimum score; 112 = maximum score). The BPRS has an established factor structure with good psychometric properties [42], and has been widely used in psychiatric institutional and community-based research settings.
Functioning
Functional outcomes assessed by raters trained in using the Global Assessment of Functioning scale [43]. The GAF is an established measure of global psychosocial and occupational functioning, and is used to assess functional impairment on Axis-V of the Diagnostic and Statistical Manual of Mental Disorders [43–45]. The GAF has been used to assess functional outcomes in SMI. The GAF consists of a global judgment of psychological, social and occupational functioning, is rated on a scale ranging from 1 to 100 (1 = poor functioning; 100 = superior functioning). Final ratings are based on the rater’s combined impressions that pertain to symptom severity and functional impairment exhibited across occupational, interpersonal and social settings.
Procedures
The 801 participants we selected from the MacArthur Violence Risk Assessment Study were initially assessed, while hospitalized, via face-to-face interviews (100%) by trained raters (PhD or MSW/MA) using the self-report measures of substance use, the BPRS and the GAF, respectively. At hospitalization, data were collected using a 30-day retrospective index to examine the initial levels of symptomatology, functioning, and the proportions of patients using substances [37–38]. Then, the same symptom, functional and substance use assessments were re-administered 5 times (every 10-weeks) via face-to-face (89%) or telephone (11%) interviews by trained raters, during the 1-year post-hospitalization period [37–38, 40]. The findings of the parent MacArthur Violence Risk Assessment Study indicated that patients in the follow-up sample were significantly more likely to have a diagnosis of bipolar disorder, less likely to have a history of drug or alcohol abuse, less likely to have a legal status of grave disability, and less likely to have a documented history of violence toward family members or others [38]. Within our sample of patients diagnosed with schizophrenia-spectrum, bipolar, and depressive disorders we found drug/alcohol use at hospitalization was not associated with study completion, χ2(1) = .72, N = 801, p = .400, failure to complete any follow-up assessments, χ2(1) = .06, N = 801, p = .804, failure to complete the final follow-up assessment, χ2(1) = .01, N = 801, p = .945, or number of follow-up assessments completed (r = −.02, p = .664). Participants provided written informed consent, and this research was reviewed annually by each university’s Institutional Review Board.
Data Analysis
To investigate heterogeneity in longitudinal patterns of substance use and the associations of use with recovery outcomes across a large sample of patients with different SMIs, our analytic approach focused on examining: (1) longitudinal patterns in the proportion of patients using substances; (2) diagnostic differences in these patterns; (3) the longitudinal associations between substance use over 1-year with symptom and functional recovery; and (4) diagnostic differences in the association between substance use and recovery outcomes. These questions were examined by employing a series of mixed-effects growth models, which is a form of hierarchical linear modeling for repeated measures data, where multiple measurement occasions are nested within individuals [46]. Longitudinal patterns in the proportion of individuals using substances over 1-year were examined using generalized linear mixed-effects growth models employing penalized-quasi likelihood estimation for computing parameter estimates of binary outcomes. These analyses began with unconditional growth models predicting substance use from time (coded as 0=baseline; 1=10 weeks, 2=20 weeks, etc.) to examine the overall trajectory of the proportion of the sample using substances throughout the follow-up. Subsequently, conditional growth models were constructed predicting substance use from diagnosis and a diagnosis by time interaction to examine diagnostic differences in longitudinal trajectories of substance use. To examine the association between substance use and functional outcome, general linear mixed-effects models using restricted maximum likelihood estimation were constructed predicting symptom and functioning measures from time and time-varying substance use variables. Diagnostic differences in these relationships were also investigated by examining diagnosis by substance use interactions. Finally, exploratory analyses were conducted to examine the degree to which gender moderated these relationships. All conditional growth models included age, race, and gender, as well as initial levels of the outcome variable that was under study (e.g., baseline substance use/functioning) as potentially confounding covariates. Additionally, level of psychopathology, represented by total BPRS scores, was entered in the alcohol use outcome models due to its observed relation with alcohol use.
Analyses were carried out using R version 2.15.0 [47], and all mixed-effects models included both individual and study site as nested random intercept factors, as well as time as a random slope factor. A first-order autoregressive error structure suitable for longitudinal data was used [46]. Mixed-effects models utilized an intent-to-study approach based on intent-to-treat principles that are commonly employed in longitudinal clinical trials by including all eligible individuals who entered the study, regardless of whether they completed all study assessment periods [48]. This approach was taken because examining only those participants who complete the entire study is well-known to bias parameter estimates in longitudinal studies with attrition [48–50]. Rather than discard partial study completers and potentially bias the final sample of individuals analyzed, the expectation-maximization approach was used to handle missing data during maximum likelihood estimation at the time of analysis [51–52]. This approach to missing data is not imputation-based, but relies on estimating model parameters (e.g., individual trajectories) using all available data (e.g., existing measurement occasions for the individual, overall sample parameter estimates, model covariates), and is currently the standard for handling missing data in longitudinal studies [53–54]. Overall missing data was modest at 23% across the study duration, with the largest proportion of missing observations at week 50 follow-up (see Supplementary Table 1). Complete case (N = 419) sensitivity analyses revealed similar, although less statistically powerful results (see Supplementary Table 2).
Results
Sample Characteristics
Characteristics of the 801 participants at hospitalization are presented in Table 1. A total of 57.4% (N = 460) of patients were diagnosed with depressive disorders, 25.5% (N = 204) with schizophrenia-spectrum disorders, and 17.1% (N = 137) with bipolar disorders. At hospitalization, participant ages ranged between 18 and 40 (M = 29.88, SD = 6.18), most (55.1%) were males; the overall majority (70.9%) were white. Most participants had never been married (58.4%) and were hospitalized (72.3%) voluntarily.
Table 1.
Characteristics of Participants across Psychiatric Diagnosis at Hospital Admission (N = 801).
| Bipolar |
Depressive |
Schizophrenia-Spectrum |
||||
|---|---|---|---|---|---|---|
|
N = 137 |
N = 460 |
N = 204 |
Overall Difference |
|||
| Variable | M (SD) | M (SD) | M (SD) | χ2 | F | pa |
| Age | 29.68 (6.08) | 29.29 (6.13) | 31.34 (6.14) | - | 7.58 | .001 |
| Verbal IQb | 41.36 (14.71) | 37.51 (16.32) | 28.55 (16.78) | - | 26.48 | .001 |
| SES | 56.90 (16.47) | 59.92 (15.31) | 65.37 (12.60) | - | 15.20 | .001 |
| GAF | 28.48 (8.47) | 31.54 (11.35) | 28.89 (9.22) | - | 7.13 | .001 |
| BPRS | 38.60 (9.64) | 36.78 (7.96) | 45.02 (10.87) | - | 58.20 | .001 |
| Sex - N (% male) | 77 (56.2%) | 237 (51.4%) | 127 (62.0%) | 68.75 | - | .001 |
| Race - N (% white) | 123 (89.8%) | 342 (74.4%) | 102 (50.2%) | 69.17 | - | .001 |
| Marital Status - N (% ever married) | 70 (51.1%) | 204 (44.6%) | 58 (28.3%) | 21.70 | - | .001 |
| Hospitalization - N (% involuntary) | 46 (32.8%) | 106 (23.2%) | 71 (35.1%) | 12.02 | - | .003 |
Note. SES = Socioeconomic Status; GAF = Global Assessment of Functioning; BPRS = Brief Psychiatric Rating Scale.
Only overall effects are presented. Analysis of variance tests were computed for continuous variables and χ2 tests were used for categorical variables. Corresponding p-values reflect the overall difference across diagnostic groups in terms of the characteristic observed.
Verbal IQ scores are based on raw values.
Pre-Hospitalization Patterns of Substance Use Across Psychiatric Diagnosis
An examination of the frequency of substance use across the sample indicated that alcohol and cannabis were the two most common substances used 30-days prior to hospitalization, with 540 (67.0%) and 237 (30.0%) patients respectively reporting use of these substances within 30-days of admission (see Table 2). Heroin was used by a small proportion (N = 148, 18.0%) of patients and the use of other substances was minimal. Few differences were observed with regard to the proportion of patients who used substances 30-days prior to hospitalization. Equivalent proportions of patients with bipolar, depressive, and schizophrenia-spectrum disorders reported using alcohol and cannabis (all p < .379). A greater proportion of patients with depressive and schizophrenia-spectrum disorders reported using heroin within 30-days of hospitalization, compared to patients with bipolar disorders (see Table 2).
Table 2.
Substance Use Patterns of Participants by Study Site and across Psychiatric Diagnosis 30-days Prior to Hospitalization (N = 801).
| Bipolar |
Depressive |
Schizophrenia-Spectrum |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
N = 137 |
N = 460 |
N = 204 |
|||||||||||||
| Substance Use by Site |
N N - % |
Substance Use by Site |
N N - % |
Substance Use by Site |
N N - % |
||||||||||
| Variable | KC | PITT | WOC | Total | KC | PITT | WOC | Total | KC | PITT | WOC | Total | χ2 | p | |
| Alcohol | 32 66.7% |
35 74.5% |
25 59.5% |
92 67.0% |
156 75.0% |
119 66.1% |
37 51.4% |
312 68.0% |
66 68.7% |
41 63.1% |
29 67.4% |
136 67.0% |
.09 | .955 | |
| Cannabis | 12 25.0% |
11 23.4% |
14 33.3% |
37 27.0% |
81 38.9% |
49 27.2% |
15 20.8% |
145 32.0% |
26 27.1% |
18 27.7% |
11 25.6% |
55 27.0% |
1.94 | .379 | |
| Stimulants | 3 6.2% |
1 2.1% |
0 0.0% |
4 3.0% |
9 4.3% |
5 2.8% |
1 1.4% |
15 3.0% |
2 2.1% |
2 3.1% |
2 4.6% |
6 3.0% |
.08 | .963 | |
| Sedatives | 3 6.2% |
1 2.1% |
0 0.0% |
4 3.0% |
9 4.3% |
5 2.8% |
1 1.4% |
15 3.0% |
2 2.1% |
2 3.1% |
2 6.9% |
6 3.0% |
.08 | .963 | |
| Cocaine | 1 2.1% |
2 4.2% |
0 0.0% |
3 2.0% |
1 0.4% |
5 2.8% |
2 2.8% |
8 2.0% |
1 1.0% |
2 3.1% |
3 11.7 |
6 3.0% |
.99 | .610 | |
| Heroin | 5 10.4% |
4 8.7% |
5 11.9% |
14 10.0% |
44 21.1% |
42 23.3% |
9 12.5% |
95 21.0% |
22 22.9% |
12 18.5% |
5 11.6% |
39 19.0% |
7.54 | .023 | |
| Opiate | 3 6.2% |
2 4.2% |
0 0.0% |
5 4.0% |
8 3.8% |
12 6.7% |
1 1.4% |
21 5.0% |
1 1.0% |
3 4.6% |
0 0.0% |
4 2.0% |
2.69 | .260 | |
| PCP | 1 2.1% |
1 2.2% |
0 0.0% |
2 1.0% |
1 0.5% |
1 0.5% |
0 0.0% |
2 0.0% |
4 4.2% |
0 0.0% |
0 0.0% |
4 2.0% |
3.78 | .151 | |
| Psychedelic | 3 6.2% |
3 6.3% |
2 4.8 |
8 6.0% |
6 2.9% |
5 2.8% |
2 2.7% |
13 3.0% |
1 1.0% |
0 0.0% |
0 0.0% |
1 0.0% |
8.69 | .013a | |
| Other | 0 0.0% |
1 2.1% |
1 2.4% |
2 1.0% |
2 1.7% |
3 1.7% |
0 0.0% |
5 1.0% |
3 3.1% |
1 0.2% |
0 0.0% |
4 2.0% |
.81 | .668 | |
Note. KC= Kansas City, MO; PITT= Pittsburgh, PA; WOC= Worchester, MA; PCP = Phencydidine; Total= the combined reported use of substances from the three study sites by psychiatric diagnosis; χ2 tests of the significance are based on these combined totals.
The p-value estimates for psychedelic drug use may be incorrect due to small cell sizes.
Longitudinal Post-Hospital Discharge Patterns of Substances Use Across Psychiatric Diagnosis
After finding that few significant diagnostic differences in substance use prior to hospitalization, we investigated the longitudinal patterns for the use of the two most commonly used substances, alcohol and cannabis, over the course of 1-year. As can be seen in Table 3, results of unconditional growth models revealed that the overall proportion of patients using alcohol and cannabis significantly decreased over 1-year. Equivalent proportions of patients reported using alcohol post-hospitalization across diagnostic groups; however, the proportion of schizophrenia-spectrum and depressed patients using cannabis declined at significantly greater rates over the course of the study compared to patients with bipolar disorders who used cannabis.
Table 3.
Longitudinal Predictors of Alcohol and Cannabis Use Among Participants with Severe Mental Illness (N = 801).
| Alcohol Use |
Cannabis Use |
|||||||
|---|---|---|---|---|---|---|---|---|
| Predictor | B | 95% CI | SE | p | B | 95% CI | SE | p |
| Unconditional Growth Model | ||||||||
| Time | −.15 | −.21 to −.09 | .03 | < .001 | −.27 | −.37 to −.18 | .05 | < .001 |
| Conditional Growth Modela | ||||||||
| Age | −.01 | −.05 to .02 | .02 | .420 | −.08 | −.12 to −.04 | .02 | < .001 |
| Male | .76 | .35 to 1.17 | .21 | < .001 | 1.56 | 1.04 to 2.08 | .26 | < .001 |
| White | .22 | −.25 to .69 | .24 | .365 | −.22 | −.80 to .36 | .30 | .459 |
| Schizophreniac | −.18 | −.84 to .48 | .34 | .593 | .17 | −.68 to 1.01 | .43 | .702 |
| Depressionc | .30 | −.26 to .87 | .29 | .295 | .58 | −.13 to 1.30 | .37 | .111 |
| Depressiond | .48 | −.02 to .99 | .26 | .062 | .42 | −.21 to 1.05 | .32 | .193 |
| Time × Age | −.00 | −.01 to .01 | .01 | .818 | −.00 | −.02 to .01 | .01 | .793 |
| Time × Male | −.10 | −.22 to .02 | .06 | .112 | −.22 | −.40 to −.03 | .09 | .020 |
| Time × White | −.04 | −.18 to .10 | .07 | .565 | −.16 | −.37 to .04 | .10 | .111 |
| Time × Schizophreniac | −.11 | −.30 to .09 | .10 | .282 | −.33 | −.63 to −.04 | .15 | .028 |
| Time × Depressionc | −.06 | −.23 to .10 | .09 | .459 | −.26 | −.50 to −.01 | .13 | .042 |
| Time × Depressiond | .04 | −.10 to .19 | .07 | .567 | .08 | −.15 to .30 | .11 | .507 |
| Gender Moderated Conditional Growth Modela,b | ||||||||
| Time × Schizophrenia × Malec | −.09 | −.46 to .29 | .19 | .650 | −.61 | −1.13 to −.09 | .27 | .022 |
| Time × Depression × Malec | .24 | −.09 to .58 | .17 | .152 | −.09 | −.54 to .36 | .23 | .698 |
| Time × Depression × Maled | .33 | .05 to .62 | .15 | .024 | .43 | .04 to .83 | .20 | .033 |
Note. Alcohol use models also adjusted for Brief Psychiatric Rating Scale total scores given the association between psychopathology and alcohol use observed in the sample. Statistically significant effects appear in boldface.
To avoid visual clutter, previous univariate effects are not presented
Only a priori moderator effects of interest are presented
Reference category is bipolar disorder
Reference category is schizophrenia
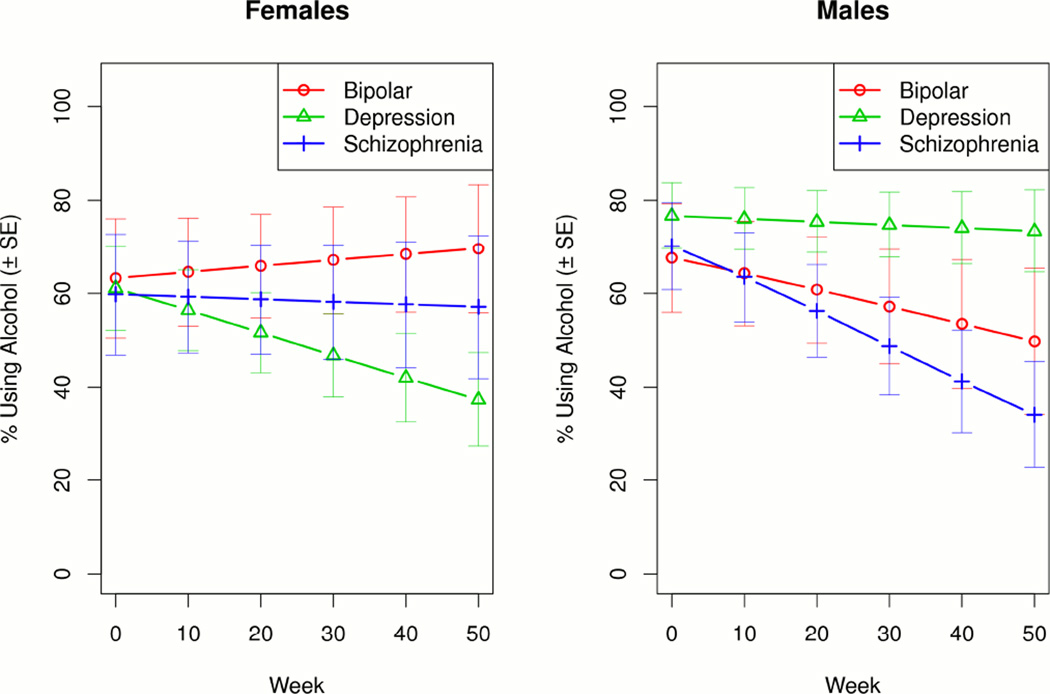
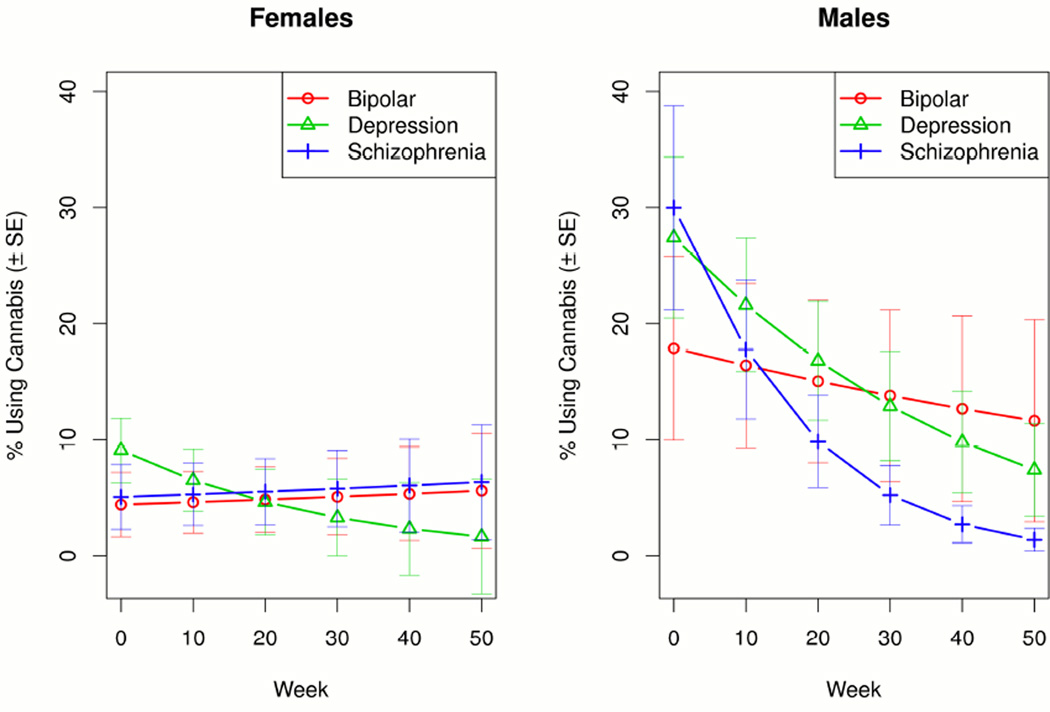
Variability in the longitudinal trajectories of substance use became even more pronounced when examining the moderating effects of gender on cannabis and alcohol use. A significantly greater proportion of men reported using alcohol and cannabis, and the proportion of males who reported using cannabis declined significantly compared to females post-hospitalization (see Table 3). Among women, patients with depressive disorders demonstrated the greatest decline in rates of alcohol use, whereas patients with schizophrenia-spectrum disorders showed the greatest decline in alcohol use among men (see Figure 1). A significantly greater decline in the proportion of men who reported using cannabis was observed in those with schizophrenia-spectrum disorders compared to those with depressive and bipolar disorders (see Figure 2). The proportion of females who reported using cannabis, however, was uniformly low across diagnoses and remained stable throughout the course of the study.
Figure 1.
One-Year Patterns of Alcohol Use Among Men and Women with Schizophrenia-Spectrum, Bipolar, and Depressive Disorders.
Figure 2.
One-Year Patterns of Cannabis Use Among Men and Women with Schizophrenia-Spectrum, Bipolar, and Depressive Disorders.
Longitudinal Impact of Substance Use on Psychopathology and Functional Outcome
Cannabis (B = 1.65 [95% CI = .83 to 2.47], p < .001) and alcohol (B = 1.04 [95% CI = .36 to 1.72], p = .002) use were both associated with consistently higher BPRS scores. Similarly, cannabis (B = −2.33 [95% CI = −3.67 to −.99], p = .001) and alcohol (B = −1.45 [95% CI = −2.59 to −.32], p = .012) use were also associated with poorer functional outcomes. Although no significant differences were observed between diagnostic groups for these outcomes over the follow-up, moderator model results showed significant interactions between diagnostic groups and gender with regard to the associations between alcohol, but not cannabis use and psychopathology and functional outcomes. Females with schizophrenia-spectrum disorders who used alcohol displayed higher levels of psychopathology compared to other diagnostic groups and their male counterparts, F(2, 2561) = 4.27, p = .014. Males with bipolar and depressive disorders who used alcohol exhibited poor functioning compared to their female counterparts, F(2, 2872) = 5.64, p = .004.
Discussion
Substance use by persons with SMI is problematic [7–17], and not many longitudinal investigations have studied the patterns of drug and alcohol use across psychiatric conditions. Therefore, we studied 801 schizophrenia-spectrum, bipolar, and depressive disorder participants in the MacArthur Violence Risk Assessment Study [37] and followed these patients and their recovery and substance use outcomes for 1-year post-hospitalization.
The results of this study showed considerable heterogeneity in the patterns of substance use across the diagnostic groups studied, which became exceedingly apparent after examining the moderating effects of gender. Reported rates of alcohol and cannabis tended to be the highest within 30-days of hospitalization, regardless of diagnosis, and more males continued to use these substances over the follow-up compared to females. Furthermore, patients with bipolar disorder were particularly at risk for continued cannabis use throughout the study, and women with depression were more likely to stop using alcohol whereas men with schizophrenia tended to be the most likely to stop their alcohol use. Regardless, both alcohol and cannabis were associated with poorer symptom and functional outcomes. This study reports results showing substance use is associated with poor outcomes, and that the use of alcohol and cannabis varies by gender and diagnosis, suggesting that personalizing substance use interventions to the psychiatric condition and gender of the patient may be most effective in achieving recovery for individuals with co-occurring conditions.
Several limitations should be noted. First, our measure of substance use was admittedly limited by patients’ self-report [37], and since substance use was not quantified, we are precluded from commenting on the rates of change in terms of drug or alcohol consumption over the follow-up. Given the potential for underreported substance use, our estimates should be interpreted with caution. Second, questions may arise in terms of the applicability of our results because our sample was selected from the MacArthur Violence Risk Assessment Study, which required participants to ‘be at risk for future violence’[37–38]. The investigators of the parent study endorsed their results as ‘fairly representative of the community behaviors of psychiatric patients discharged from acute inpatient facilities’ [37–38], which suggests our findings should be comparatively representative in terms of the sample we selected. Indeed, the MacArthur Violence Risk Assessment Study has not been replicated, and future research will be needed to test these effects in samples more generalizable to the recent literature on substance abuse in SMI. Third, there may be concerns about our use of the DSM-III-R [43]. We found few differences existed between the DSM-III-R and the DSM-IV-TR criteria [43–45]. Given that DSM-III-R criteria were rigorously applied, and confirmed by the DSM-III-R checklist [39], we do not believe that our use of the DSM-III-R has markedly restricted the applicability of this research. It should also be noted that our use of the GAF to assess functional outcomes is limited because of its global focus and its incorporation of symptomatology into the measurement [43]. Since information on treatment and medication compliance were not systematically collected [37], it will be important for future research to examine the potentially confounding effects of these factors. Lastly, we can only comment on the differences observed during the course of 1-year, and future longitudinal research will need to be conducted in this population.
The present study has implications for future research on substance abuse and SMI. Our results indicate that substance use, while a common a prevalent problem in SMI, is not the same for everyone. There appears to be remarkable and complex heterogeneity in substance use patterns by psychiatric diagnosis and genders, signaling sub-groups that may show differences in etiology, maintaining factors and treatment needs. Thus, our findings suggest characterizing the factors associated with poor outcomes may be critical to facilitating effective treatments for substance abuse in this population. Indeed, there is a diagnostic dilemma in terms of whether SMI is associated with primary or induced SUD [36, 55–63], and thus an accurate psychiatric diagnosis is a key component of substance use treatment planning [36]. Delivering treatments for substance abuse presents challenges for mental health professionals [64], and there is seemingly no consensus on a recommended model of intervention to follow in these patients [36], although models employing integrated treatment for co-occurring disorders have a solid evidence base [68–69]. Regardless, the preponderance of the evidence indicates combinations of psychotherapies, behavioral and pharmacological interventions offer effective treatments for this population [65], but how these should be applied in light of such heterogeneity in substance use problems is not well-established. Recent reports suggest that the intensity of substance abuse treatment should be commensurate with the severity of SMI [65], and advise implementing the integrated model due to the favorable results achieved [66, 36]. The integrated model assumes that the patient is cared for by a single team [66–67], and since it already targets the impact of substance use on psychiatric symptomology [66–67], these programs are adaptable to account for sub-group characteristics in terms of treatment needs. The integrated model is expensive and difficult to implement within the current systems of care [36, 68–69], but it will be crucial for efforts to focus on creating cost-effective programs while initiating personalized interventions.
While more research is required to replicate these results, our findings suggest that it will be critical for future efforts to disseminate specialized integrated treatments for persons with SMIs who use drugs and alcohol, and such programs should focus on personalizing interventions by diagnosis and gender, which may help improve outcomes and facilitate recovery.
Supplementary Material
Acknowledgments
The John D. and Catherine T. MacArthur Foundation Research Network on Mental Health and the Law provided the funding support for the MacArthur Violence Risk Assessment Study, which provided the public-access data for this research. This research was also supported by NIH grants DA-30763 (SME) and RR-24154 (SME).
Footnotes
Conflict of Interest: The authors do not have any conflicts of interest requiring disclosure that could inappropriately influence the outcome of this research.
REFERENCES
- 1.Reiger DA, Farmer ME, Rae DS, Locke BZ, Keith SJ. Comorbidity of mental disorders with alcohol and other drug abuse. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- 2.Kessler RC, Nelson CB, McGonagle CA, Edlund MJ, Frank RG, Leaf PJ. The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. Am J Orthopsychiatry. 1996;66:17–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC. The epidemiology of dual diagnosis. Biol Psychiatry. 2004;54:730–737. doi: 10.1016/j.biopsych.2004.06.034. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas K, et al. The epidemiology of major depressive disorder. Results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Wai Tat Chiu AM, Demler O, Walters EE. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- 6.Degenhardt L, Hall W. The association between psychosis and problematic drug use among Australian adults: findings from the National Survey of Mental Health and Well-Being. Psychol Med. 2001;31:659–668. doi: 10.1017/s0033291701003865. [DOI] [PubMed] [Google Scholar]
- 7.Helzer J, Burnam A, McEvoy L. Alcohol abuse and dependence. In: Robins LN, Reiger DA, editors. Psychiatric disorders in America. New York: Free Press; 1991. pp. 81–129. [Google Scholar]
- 8.Kavanagh DJ, Waghorn G, Jenner L, Chant DC, Carr V, Evans M, et al. Demographic and clinical correlates of comorbid substance use disorders in psychosis: Multivariate analyses from an epidemiological sample. Schizophr Res. 2004;66:115–124. doi: 10.1016/s0920-9964(03)00130-0. [DOI] [PubMed] [Google Scholar]
- 9.Addingtion J, Addingtion D. Patterns, predictors and impact of substance use in early psychosis: A longitudinal study. Acta Psychiatr Scand. 2008;115:304–09. doi: 10.1111/j.1600-0447.2006.00900.x. [DOI] [PubMed] [Google Scholar]
- 10.Lambert M, Conus P, Lubman DI, Wade D, Yuen H, Moritz S, et al. The impact of substance use disorders on clinical outcome in 643 patients with first-episode psychosis. Acta Psychiatr Scand. 2005;112:141–148. doi: 10.1111/j.1600-0447.2005.00554.x. [DOI] [PubMed] [Google Scholar]
- 11.Drake RE, Osher EC, Wallach MA. Alcohol use and abuse in schizophrenia: a prospective community study. J Nerv Ment Dis. 1989;177:408–414. doi: 10.1097/00005053-198907000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Drake RE, Xie H, McHugo GJ, Shumway M. Three-year outcomes of long-term patients with co-occurring and bipolar and substance use disorders. Biol Psychiatry. 2004;56:749–756. doi: 10.1016/j.biopsych.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 13.Xie H, Drake RE, McHugo GJ. The 10-year course of substance use disorder among patients with severe mental illness: An analysis of latent class trajectory groups. Psychiatr Serv. 2009;60:804–11. doi: 10.1176/ps.2009.60.6.804. [DOI] [PubMed] [Google Scholar]
- 14.Xie H, Drake RE, McHugo GJ, Xie L, Mohandas L. The 10-year course of remission, abstinence, and recovery in dual diagnosis. J Subst Abuse Treat. 2010;39:132–140. doi: 10.1016/j.jsat.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 15.Mueser KT, Yarnold PR, Levinson DF, Hardeep S, Bellack AS, Morrison K, et al. Prevalence of Substance Abuse in Schizophrenia: Demographic and Clinical Correlates. Schizophr Bull. 1990;16:31–56. doi: 10.1093/schbul/16.1.31. [DOI] [PubMed] [Google Scholar]
- 16.Xie H, McHugo GJ, Helmstetter BS, Drake RE. Three-year recovery outcomes for long-term patients with co-occurring schizophrenic and substance use disorders. Schizophr Res. 2005;75:337–48. doi: 10.1016/j.schres.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 17.Drake RE, Brunette MF. Complications of severe mental illness related to alcohol and other drug use disorders. In: Galanter M, editor. Recent Developments in Alcoholism: Consequences of Alcoholism. Vol. 14. New York: Plenum Publishing Company; 1998. pp. 285–299. [DOI] [PubMed] [Google Scholar]
- 18.Brook JS, Cohen P, Brooke DW. Longitudinal study of co-occurring psychiatric disorders and substance use. J Child Adolesc Psychiatry. 1998;37:322–330. doi: 10.1097/00004583-199803000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Cassidy F, Ahearn E, Carroll B. Substance abuse in bipolar disorder. Bipolar Disorders. 2001;3:181–188. [PubMed] [Google Scholar]
- 20.Alterman AL, Erdlen D, Laporte D, Erdlen F. Effects of illicit drug use in an impatient psychiatric setting. Addict Behav. 1982;7:231–242. doi: 10.1016/0306-4603(82)90050-8. [DOI] [PubMed] [Google Scholar]
- 21.Barbee J, Clark P, Crapanzano M, Heintz G, Kehoe C. Alcohol and substance abuse among schizophrenic patients presenting to an emergency psychiatric service. J Nerv Ment Dis. 1989;177:400–407. doi: 10.1097/00005053-198907000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Frances RL, Hennessy G. Bipolar Disorder and Substance Abuse. Biol Psychiatry. 2004;56:738–748. doi: 10.1016/j.biopsych.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 23.Ramo EB, Schuckit MA. Alcohol dependence and mood disorders. Addict Behav. 1998;23:933–946. doi: 10.1016/s0306-4603(98)00068-9. [DOI] [PubMed] [Google Scholar]
- 24.Swendsen JD, Merikangas KR. The comorbidity of depression and substance use disorders. Clin Psychol Rev. 2000;20:173–189. doi: 10.1016/s0272-7358(99)00026-4. [DOI] [PubMed] [Google Scholar]
- 25.Volkow ND. Substance Use Disorders in Schizophrenia—Clinical Implications of Comorbidity. Schizophr Bull. 2009;35:469–472. doi: 10.1093/schbul/sbp016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Volkow ND. The reality of comorbidity: Depression and drug abuse. Biol Psychiatry. 2004;56:714–717. doi: 10.1016/j.biopsych.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 27.Dixon L. Dual diagnosis of substance abuse in schizophrenia: prevalence and impact on outcomes. Schizophr Res. 1999;35:593–5100. doi: 10.1016/s0920-9964(98)00161-3. [DOI] [PubMed] [Google Scholar]
- 28.Dixon L, Haas G, Weiden P, Frances A. Drug abuse in schizophrenic patients: Clinical correlates and reasons for use. Am J Psychiatry. 1991;148:224–230. doi: 10.1176/ajp.148.2.224. [DOI] [PubMed] [Google Scholar]
- 29.Bennett M, Bellack A, Brown C, DiClemente C. Substance dependence and remission in schizophrenia: A comparison of schizophrenia and affective disorders. Addict Behav. 2009;34:806–814. doi: 10.1016/j.addbeh.2009.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mueser KT, Yarnold PR, Bellack AS. Diagnostic and demographic correlates of substance abuse in schizophrenia and major affective disorder. Acta Psychiatr Scand. 1992;85:48–55. doi: 10.1111/j.1600-0447.1992.tb01441.x. [DOI] [PubMed] [Google Scholar]
- 31.Laudet A, Mogura S, Vogel H. Recovery Challenges among dually diagnosed individuals. J Subst Abuse Treat. 2000;18:321–329. doi: 10.1016/s0740-5472(99)00077-x. [DOI] [PubMed] [Google Scholar]
- 32.Hanson M, Kramer T, Gross W. Outpatient treatment of adults with coexisting substance use and mental disorders. J Subst Abuse Treat. 1990;7:109–116. doi: 10.1016/0740-5472(90)90006-c. [DOI] [PubMed] [Google Scholar]
- 33.Weiss RD, Ostacher MJ, Otto MW, Calabrese JR, Fossey M, Wisniewski SR, et al. Does Recovery From Substance Use Disorder Matter in Patients With Bipolar Disorder? J Clin Psychiatry. 2005;66:705–735. doi: 10.4088/jcp.v66n0609. [DOI] [PubMed] [Google Scholar]
- 34.Salloum I, Cornelius J, Mezzich J. Characterizing female bipolar alcoholic patients presenting for initial evaluation. Addict Behav. 2001;26:341–348. doi: 10.1016/s0306-4603(00)00109-x. [DOI] [PubMed] [Google Scholar]
- 35.Schutte KK, Seable JH, Moos RH. Gender differences in the relations between depressive symptoms and drinking behavior among problem drinkers: A three-wave study. J Consult Clin Psychol. 65:392–404. doi: 10.1037//0022-006x.65.3.392. [DOI] [PubMed] [Google Scholar]
- 36.Roncero C, Barral C, Grau-Lopez L, Barhiller D, Szerman N, Casas M, et al. Protocols of Dual Diagnosis Interventions in Schizophrenia. Addict Disord Their Treatment. 2011;10:131–154. [Google Scholar]
- 37.Monahan J, Steadman HJ, Silver E, Appelbaum PS, Robbins PC, Mulvey EP, et al. Rethinking Risk Assessment: The MacArthur Study of Mental Disorder and Violence. New York: Oxford University Press; 2001. [Google Scholar]
- 38.Steadman H, Mulvey EP, Monahan J, Robbins PC, Appelbaum PS, Grisso T, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. 1998;55:393–401. doi: 10.1001/archpsyc.55.5.393. [DOI] [PubMed] [Google Scholar]
- 39.J’anca A, Helzer J. DSM-III-R criteria checklist. DIS Newsletter. 1990;7:17. [Google Scholar]
- 40.Skeem J, Mulvey E. Psychopahology and Community Violence Among Civil Psychiatric Patients: Results from the MacArthur Violence Risk Assessment Study. J Consult Clin Psych. 2001;69:358–374. [PubMed] [Google Scholar]
- 41.Overall J, Gorham D. The Brief Psychiatric Rating Scale. Psychol Rep. 1962;10:799–812. (1962) [Google Scholar]
- 42.Long J, Brekke J. Longitudinal factor structure of the Brief Psychiatric Rating Scale in schizophrenia. Psychol Assess. 1999;11:498–506. [Google Scholar]
- 43.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Rev. 3rd ed. Washington, DC: Author; 1987. [Google Scholar]
- 44.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- 45.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Text Revision. Washington, DC: Author; 2000. [Google Scholar]
- 46.Raudenbush DSW, Bryk DAS. Hierarchical Linear Models: Applications and data analysis methods. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 47.R Development Core Team R. A language and environment for statistical computing (Version 2.15.0) Computer Software. Vienna Austria: R Foundation for Statistical Computing; [Accessed: 2012-12-22]. 2012-12.22. URL: http://softwaretopic.informer.com/development-core-team-2009/. (Archived by WebCite® at http://www.webcitation.org/6D78fapMs) [Google Scholar]
- 48.Schafer JL, Graham JW. Missing Data: Our View of the State of the Art. Psychol Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- 49.Lachin JM. Statistical Considerations in the Intent-to-Treat Principle. Control Clin Trials. 2000;21:167–189. doi: 10.1016/s0197-2456(00)00046-5. [DOI] [PubMed] [Google Scholar]
- 50.Yau L. Intent-to-Treat Analysis for Longitudinal Studies with Drop Outs. Biometrics. 1996;52:1324–1333. [PubMed] [Google Scholar]
- 51.Dempster AP, Laird NM, Rubin DB. Maximum Likelihood from Incomplete Data via the EM Algorithm. Appl Stat. 1977;39:1–38. [Google Scholar]
- 52.McCulloch C. Maximum Likelihood Algorithms for Generalized Linear Mixed Models. J Am Stat Assoc. 1997;437:162–170. [Google Scholar]
- 53.Gueorguieva R, Krystal JH. Move Over ANOVA Progress in Analyzing Repeated-Measures Data and Its Reflection in Papers Published in the Archives of General Psychiatry. Arch Gen Psychiatry. 2004;61:310–317. doi: 10.1001/archpsyc.61.3.310. [DOI] [PubMed] [Google Scholar]
- 54.Hamer RM, Simpson PM. Last observation carried forward versus mixed models in the analysis of psychiatric clinical trials. Am J Psychiatry. 2009;166:639–641. doi: 10.1176/appi.ajp.2009.09040458. [DOI] [PubMed] [Google Scholar]
- 55.Horsfall J, Cleary M, Hunt G, et al. Psychosocial treatments for people with co-occurring severe mental illnesses and substance use disorders (dual diagnosis): a review of empirical evidence. Harv Rev Psychiatry. 2009;17:24–34. doi: 10.1080/10673220902724599. [DOI] [PubMed] [Google Scholar]
- 56.Mueser K, Drake R, Wallach M. Dual diagnosis: a review of etiological theories. Addict Behav. 1998;23:717–734. [PubMed] [Google Scholar]
- 57.Johnson JG, Cohen P, Pine DS, Klein DE, Kasen S, Brook JS. Association between cigarette smoking and anxiety disorders during adolescence and early childhood. JAMA. 2000;284:2348–2351. doi: 10.1001/jama.284.18.2348. [DOI] [PubMed] [Google Scholar]
- 58.Grant BF, Goldstein RB, Chou SP, Huang B, Stinson ES, Dawson DA, et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the WAVE 2 National Epidemologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zimmerman P, Wittchen HU, Hofler M, Pfister H, Kessler RC, Lieb R. Primary anxiety disorders and the development of subsequent alcohol use disorders: a 4-year community study of adolescents and young adults. Psychol Med. 2003;33:1211–1222. doi: 10.1017/s0033291703008158. [DOI] [PubMed] [Google Scholar]
- 60.Breslau N, Novak SP, Kessler RC. Daily Smoking and the subsequent onset of psychiatric disorders. Psychol Med. 2004;34:323–33. doi: 10.1017/s0033291703008869. [DOI] [PubMed] [Google Scholar]
- 61.Merikangas KR, Herrell R, Swendensen J, Rossler W, Ajdacic-Gross V, Angst J. The specificity of bipolar spectrum in the comorbidity of mood and substance use disorders: results from the Zurich Cohort Study. Arch Gen Psychiatry. 2008;65:47–52. doi: 10.1001/archgenpsychiatry.2007.18. [DOI] [PubMed] [Google Scholar]
- 62.Frisher M, Crome I, Macleod J, Millson D, Croft P. Substance misuse and psychiatric illness: prospective observational study using the general practice research database. J Epidemiol Commun Health. 2005;59:847–850. doi: 10.1136/jech.2004.030833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Swendsen J, Conway KP, Degenhardt L, Glantz M, Jin R, Merikangas, et al. Mental disorders as risk factors for substance use, abuse and dependence: results from the 10-year follow-up of the National Comorbidity Survey. Addiction. 2010;105:1117–1128. doi: 10.1111/j.1360-0443.2010.02902.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bellack AS, Gearon JS. Substance abuse treatment for people with schizophrenia. Addict Behav. 1998;23:749–766. doi: 10.1016/s0306-4603(98)00066-5. [DOI] [PubMed] [Google Scholar]
- 65.Kelly TM, Daley D, Douaihy AB. Treatment of substance abusing patients with comorbid psychiatric disorders. Addict Behav. 2012;37:11–24. doi: 10.1016/j.addbeh.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Green A, Salomon M, Brenner M, et al. Treatment of schizophrenia and comorbid substance use disorder. Curr Drug Targets CNS Neurol Disord. 2002;1:129–139. doi: 10.2174/1568007024606230. [DOI] [PubMed] [Google Scholar]
- 67.Drake RE, Mercer-McFadden C, Mueser KT, McHugo CJ, Bond GR. Review of integrated mental health and substance abuse treatment for patients with dual disorders. Schizophr Bull. 1998;24:589–608. doi: 10.1093/oxfordjournals.schbul.a033351. [DOI] [PubMed] [Google Scholar]
- 68.Drake RE, Wallach MA. Dual diagnosis: 15 years of progress. Psychiatr Serv. 2000;51:1126–1129. doi: 10.1176/appi.ps.51.9.1126. [DOI] [PubMed] [Google Scholar]
- 69.Drake RE, Essock SM, Shaner A, Carey KB, Minkoff K, Kola L, et al. Implementing dual diagnosis services for clients with severe mental illness. Psychiatr Serv. 2001;52:469–476. doi: 10.1176/appi.ps.52.4.469. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.