Abstract
INTRODUCTION
Prevalence of multiple primary malignancies is slowly increasing due to prolonged survival of cancer patients with advances in diagnostic and therapeutic modalities. The reasons may be environmental modifications, genetic predisposition or therapy induced. We describe a case of a 64-year-old woman with three different metachronous primary malignancies managed at our center since 4 years.
PRESENTATION OF CASE
First primary diagnosed in our patient was adenocarcinoma of small intestine which is a rare gastrointestinal malignancy. For this she underwent surgical resection followed by chemotherapy. After 21 months she developed infiltrating duct carcinoma of breast which was managed with modified radical mastectomy and chemotherapy. Again after latent period of 10 months patient had papillary adenocarcinoma of ovary for which she was administered chemotherapy. During follow up tumor was found to be chemoresistant and again she underwent cytoreductive surgery followed by chemotherapy.
DISCUSSION
In present case patient did not have significant risk factors for development of carcinoma of small intestine, breast and ovary. Our patient underwent surgical excision three times and received total 16 chemotherapy cycles of different regimens during management of all three primary malignancies. Development of second and higher order primary malignancy after successful management of previous one should be always kept in mind.
CONCLUSION
Awareness, suspicion of multiple primary malignancy and aggressive diagnostic work up plays crucial role in their detection at earlier stage for better outcome. In addition choice of appropriate chemotherapeutic agents and their regimens remains the cornerstone while managing the patients with multiple primary malignancies.
Keywords: Multiple primary malignancies, Adenocarcinoma of small intestine, Infiltrating duct carcinoma of breast, Papillary adenocarcinoma of ovary
1. Introduction
Multiple primary malignancy (MPM) is defined as occurrence of two or more malignancies in the same individual without any relationship between the tumors either simultaneously or with interval of time. MPM in the same individual was first described by Warren and Gals. Although rare, its reported incidence in clinical and autopsy cases varies from 3 to 5% of all malignancies among which triple tumors are seen in 0.5% of cases.1 Number of cancer survivors is growing by 2% each year with advances in diagnostic modalities, treatment and supportive care.2 An individual may develop MPM in lifetime due to genetic predisposition, environmental exposure to carcinogens, immunodeficiency or as a serious complication of chemotherapy or radiotherapy received for first primary malignancy. National Cancer Institute's Surveillance, Epidemiology, and End Results Program reported that about one in six cancer patients develop second malignant neoplasm in their further lifetime.3
In literature several interesting cases of MPM involving different organs have been reported. But as per our knowledge after extensive search in literature, the case described herein is the first report of triple primary metachronous malignancy involving small intestine, breast and ovary in a postmenopausal woman from India.
2. Presentation of a case
A 64-year-old Indian woman with triple primary malignancy of small bowel followed by carcinoma of breast and then of ovary over last four years was managed successfully at our center. On acquisition of detailed medical history, there was no personal or family history of cancer as well as major risk factor for cancer. She is multiparious woman with age of menarche at 14 years and parity at 21 year. She is menopausal with her last period about 20 years ago. Our patient never received hormone replacement therapy and oral contraceptive pills in her lifetime. She is known to be hypertensive since ten years controlled with antihypertensive drugs.
In July 2009 patient presented with two-month history of vague abdominal pain. Abdominal ultrasound and computer tomography provided a clue suggestive of small bowel tumor of size 4 × 3 cm. Laboratory parameters were within normal limit. Explorative laparotomy revealed an evidence of intestinal obstruction due to stricture with growth at terminal ileum (Fig. 1). So tumor was excised with end to end anastomosis. There was no evidence of any pelvic mass. Histopathology revealed moderately differentiated adenocarcinoma of ileum of stage III (T2N1M0) with evidence of metastasis in mesenteric lymph nodes. Then she received six cycles of adjuvant chemotherapy of regimen Taxenes 260 mg (Paclitaxol), Carboplatin 450 mg every 21 days. Any chemotherapy induced serious adverse events were not reported during and after completion of chemotherapy. This management ceased the progression of disease.
Fig. 1.

Specimen of resected small intestine with growth in terminal ileum.
In April 2011 patient complained of lump in right breast. Physical examination confirmed a palpable mass of size 4 cm × 3 cm in upper outer quadrant without evidence of nipple discharge and ulceration. Fine needle aspiration cytology revealed presence of malignant cells and patient underwent modified radical mastectomy with axillary lymph node dissection. On macroscopic examination size of tumor was 4 cm × 3 cm × 3 cm. Histologically it was well differentiated infiltrated duct carcinoma showing presence of large cells with hyper chromatic pleomorphic nuclei, mitotic figures, nucleoli and scanty cytoplasm (Fig. 2). As per Scarf Bloom scoring system it was grade II tumor. All 9 lymph nodes from level I and II and 3 from level III were free of metastasis. On immunohistochemistry, estrogen receptors were positive in 90% tumor cells with Allred score 8/8. Progesterone receptors were positive in 40% tumor cells with Allred score 6/8. Tumor was negative for Cerb B2 examination. There was no evidence of distant metastasis at that time. Patient received six cycles of adjuvant chemotherapy with Cyclophosphamide 750 mg, Epirubicin 110 mg and 5-fluorouracil 750 mg, on every 21 days. After six months she developed type 2 diabetes mellitus and managed with oral hypoglycemic drugs.
Fig. 2.
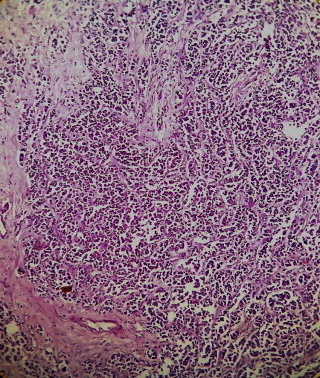
Histopathological features of infiltrated duct carcinoma of breast.
In February 2012, patient complained of pain and bloating sensation in abdomen. Abdominal ultrasound examination revealed bilateral large solid and cystic lesion of size 27 × 15 cm in pelvic region with evidence of ascites and bilateral pleural effusion. Her serum CA 125 was found to be raised to 79.7 U/ml. Ultrasound guided fine needle aspiration cytology showed presence of malignant cells suggesting well differentiated adenocarcinoma of ovary. Because of presence of ascites and large size of tumor she started with chemotherapy regimen of gemcetamine and carboplatin followed by assessment of response to this therapy. Her serum CA 125 was found to be raised to 239.7 U/ml and because of chemoresistant nature of tumor surgeon felt she should be considered for surgical excision of tumor (Fig. 3). Histopathologically it was papillary adenocarcinoma of ovary of grade IV comprised of papillary and gland like structures formed by large cuboidal to columnar cells with large hyper chromatic pleomorphic nuclei and scanty cytoplasm (Fig. 4). Cytoreductive surgical management will improve outcome of patient and response to chemotherapy.
Fig. 3.

Resected specimen of tumor of ovary.
Fig. 4.
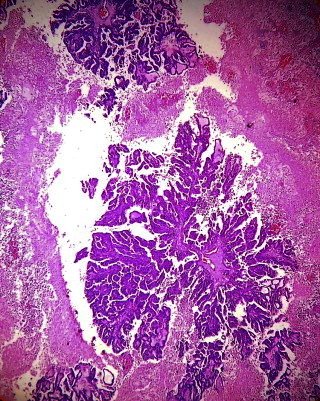
Histopathological features of papillary adenocarcinoma of ovary.
During this period all vital signs and laboratory workup including hematological, renal and liver function tests were within normal limit. Our patient tolerated her treatment with minimal side effects and without complications.
3. Discussion
MPM are categorized into two types (a) synchronous have all malignant lesions at the same time or within six months of first malignancy (b) metachronous in which second or high order malignancies follows in sequence at least six months after previous one.4
Cancer survivors have 20% higher risk of new primary cancer in same or different organ in comparison with general population. Second and higher ordered primary cancers can be therapy induced, syndrome related or by sharing common etiologic factors.5
Multiple metachronous malignancies are often seen with hematological, lung, thyroid, breast, skin and genitourinary malignancies.6 In present case first primary malignancy was adenocarcinoma of small intestine which is a rare condition accounting for 0.1 to 0.3% of all and 2% of gastrointestinal malignancies.7 The patients with familial adenomatous polyposis, Crohn's disease or hereditary nonpolyposis colorectal carcinoma are known to have increased risk of primary adenocarcinoma of small intestine.8 But our patient did not have any such predisposing factor. As per the literature most common site of malignancy in small intestine is duodenum. Brucher et al. found no patient with adenocarcinoma of the ileum in their series.9 Recently, Dabaja et al., reported a 13% incidence of adenocarcinoma in the ileum.10 Sook Hee Hong and colleagues in their retrospective analysis for 53 patients with primary adenocarcinoma of small intestine reported recurrence in 13 of 26 patients after curative resection but not a single case of MPM.11 Amin et al. documented evidence of one third metachronous cancers in patients with small intestine malignancy, but in carcinoid syndromes.12 Antal et al. reported triple primary malignancies in four of 719 cancer patients but involving different combinations of organs.13
Higher incidence of MPM has been observed in embryologically related organs endometrium and ovary. Most frequently involved organ in MPM is breast due to embryological and hormonal factors. Familial carcinoma syndrome is a combination of carcinoma of breast and ovary. But our patient does not have family history of cancer and also no known risk factor for these malignancies. So present case is sporadic occurrence which might be related to polygenic model and environmental modifications.14 Soo-Kyung Noh reported a case of quadruple malignancy involving ovary and endometrium, but after breast and rectal cancer.15
The diagnostic criteria for multiple primary cancers were advocated by Warren and Gates in 1932, namely: (1) Each cancer must be definitively malignant by histopathology, (2) they must be histologically different, and (3) the possibility of metastasis among the cancers must be excluded.16 Our patient fulfilled these criteria and classified as metachronous MPM. Metachronous MPM including adenocarcinoma of small intestine, infiltrating duct carcinoma of breast and papillary adenocarcinoma of ovary has not been reported among Indians. Our patient underwent three surgical procedures and received 16 different cycles of chemotherapy as her general condition was good. But choice of chemotherapeutic agents and regimens was difficult task.
While managing patients of malignancies, risk of developing subsequent malignant lesions of higher order should be always be kept in mind. We learnt from present case that clinician should not only think of recurrence or metastatic lesion during follow up period, but also occurrence of second or higher primary lesions in cancer survivors. This high risk population should be targeted for preventive and interventional strategies.
Challenges faced in management of this case were due to differential diagnosis, difficulty to distinguish between local, distant metastasis, recurrences and diagnosis of onset of new malignant lesion with different histopathology. Aggressive diagnostic approach of a surgeon may overcome these challenges. There are no standard guidelines for management of MPM but type of malignancies, progression of disease, response to therapy and general condition of patients should be always taken into consideration. If primary lesion is curative, clinician should opt for radical therapy otherwise palliative treatment should be considered.
4. Conclusion
Whenever a patient with known malignancy complains of new symptom we tend to correlate it with recurrence of primary one. But one should always keep in mind the possibility of subsequent new malignancy. As a clinician one should always have high index of suspicion for MPM for early detection with improved outcome.
Conflict of interest
None
Funding
None.
Ethical approval
Written informed consent for publishing case report and images is obtained from the patient.
Author contributions
All the authors have contributed to this case report, and to its design. Analysis and interpretation of the data were performed by all the authors.
References
- 1.Hu N.C., Hsiech S.C., Chen T.J., Chang J.Y. Multiple primary malignancies including colon, stomach, lung, breast and liver cancer: a case report and literature review. Chinese Medical Journal. 2009;122:3091–3093. [PubMed] [Google Scholar]
- 2.Cercato M.C., Colella E., Ferraresi V., Diodoro M.G., Tonachella R. Report of two cases of quintuple primary malignancies and review of the literature. Anticancer Research. 2008;28:2953–2958. [PubMed] [Google Scholar]
- 3.Wood M.E., Vogel V., Ng A., Foxhall L., Goodwin P., Travis L.B. Second malignant neoplasms: assessment and strategies for risk reduction. Journal of Clinical Orthodontics: JCO. 2012;30:3734–3745. doi: 10.1200/JCO.2012.41.8681. [DOI] [PubMed] [Google Scholar]
- 4.Moertel C.G. Multiple primary malignant neoplasms: historical perspectives. Cancer. 1977;40(Suppl. 4):1786–1792. doi: 10.1002/1097-0142(197710)40:4+<1786::aid-cncr2820400803>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 5.Travis L.B., Hill D., Dores G.M. Cumulative absolute breast cancer risk for young women treated for Hodgkin lymphoma. Journal of the National Cancer Institute. 2005;97:1428–1437. doi: 10.1093/jnci/dji290. [DOI] [PubMed] [Google Scholar]
- 6.Jayaraman S., Balakrishnan S., Rao D. Multiple metachronous malignancies, one patient with three primary malignancies. Indian Journal of Surgery. 2011;73(5):377–379. doi: 10.1007/s12262-011-0281-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Varghese R., Weedon R. ‘Metachronous’ adenocarcinoma of the small intestine. International Journal of Clinical Practice. 2005;147(Suppl.):106–108. doi: 10.1111/j.1368-504x.2005.00070.x. [DOI] [PubMed] [Google Scholar]
- 8.Chaiyasate K., Jain A.K., Cheung L.Y., Jacobs M.J., Mittal V.K. Prognostic factors in primary adenocarcinoma of the small intestine: 13-year single institution experience. World Journal of Surgical Oncology. 2008;6:12. doi: 10.1186/1477-7819-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brucher B.L.D.M., Stein H.J., Roder J.D., Busch R., Fink U., Werner M., Siewert J.R. New aspects of prognostic factors in adenocarcinomas of the small bowel. Hepato-Gastroenterology. 2001;48:727–732. [PubMed] [Google Scholar]
- 10.Dabaja B.S., Suki D., Pro B., Bonnen M., Ajani J. Adenocarcinoma of the small bowel: presentation, prognostic factors, and outcome of 217 patients. Cancer. 2004;101:518–526. doi: 10.1002/cncr.20404. [DOI] [PubMed] [Google Scholar]
- 11.Hong S.H., Koh Y.H., Rho S.Y., Byun J.H., Oh S.T., Im K.W. Primary adenocarcinoma of the small intestine: presentation, prognostic factors and clinical outcome. Japanese Journal of Clinical Oncology. 2009;39(1):54–61. doi: 10.1093/jjco/hyn122. [DOI] [PubMed] [Google Scholar]
- 12.Amin S., Warner R.R., Itzkowitz Sh, Kim M.K. The risk of metachronous cancers in patients with small-intestinal carcinoid tumors: a US population-based study. Endocrine-Related Cancer. 2012;19(3):381–387. doi: 10.1530/ERC-11-0392. [DOI] [PubMed] [Google Scholar]
- 13.Antal A., Vallent K. Cases of multiple tumors in our clinic. Orvosi Hetilap. 1997;38:1507–1510. [PubMed] [Google Scholar]
- 14.Hemminki K., Aaltonen L., Li X. Subsequent primary malignancies after endometrial arcinoma and ovarian carcinoma. Cancer. 2003;97:2432–2439. doi: 10.1002/cncr.11372. [DOI] [PubMed] [Google Scholar]
- 15.Noh S.-K., Yoon J.Y., Ryoo U.N., Choi C.H., Sungand C.O. A case report of quadruple cancer in a single patient including the breast, rectum, ovary, and endometrium. Journal of Gynecologic Oncology. 2008;19(4):265–269. doi: 10.3802/jgo.2008.19.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Warren S., Gates O. Multiple primary malignant tumors. A survey of the literature and a statistical study. American Journal of Cancer. 1932;16:1358–1414. [Google Scholar]


