Abstract
INTRODUCTION
Primary adenocarcinoma of the 4th portion of the duodenum is reported less frequently than those other portions of the duodenum. Therefore, few reports discuss the diagnosis and treatment of this malignancy.
PRESENTATION OF CASE
A 54-year-old woman was admitted to our hospital with a complaint of nausea and vomiting after a meal. Upper gastrointestinal examination and a duodenogram revealed a Type 2 tumor of the 4th portion of the duodenum, which was diagnosed as well-differentiated tubular adenocarcinoma by endoscopic biopsy. Partial resection of the duodenum and jejunum was performed on the basis of intraoperative evaluation of negative lymph node metastasis around the pancreas and proximal duodenum with no macroscopic invasion toward the pancreas and proximal duodenal margin. Her postoperative course was uneventful without any sign of recurrence 5 years later.
DISCUSSION
Primary adenocarcinoma in the 4th portion is relatively less common. It is not easy to diagnose this disease. Patients with primary duodenal adenocaricinoma, who are medically fit to undergo surgery, should be given the option of aggressive resection. Duodeno-cephalo-pancreatectomy remains the standard treatment for adenocarcinomas of the 1st and 2nd portion of the duodenum. Partial resection is the preferred surgical method for patients with adenocarcinoma of the 3rd and 4th portions of the duodenum.
CONCLUSION
This report describes a rare case of primary adenocarcinoma of the 4th portion of the duodenum, successfully treated by partial resection of the duodenum and jejunum. However, larger studies are required to clarify the indications for the preferred surgical method for this malignancy.
Keywords: Surgery, Diagnosis, Treatment, Lymph node, Pancreas, Invasion
1. Introduction
Primary adenocarcinoma of the 4th portion of the duodenum is reported less frequently than other portions of the duodenum. Therefore, few reports discuss this malignancy. The diagnosis of primary adenocarcinoma of duodenum (PDA) is often delayed because its symptoms and signs are nonspecific.1 Furthermore, it is not easy to make a diagnosis in the 4th portion of the duodenum. Although, endoscopic treatment has been attempted for early duodenum cancer, surgical treatment should be indicated for more advanced disease.2,3 Here, we report a PDA case of the 4th portion of the duodenum, and relevant literature has been discussed and reviewed.
2. Presentation of case
A 57-year-old woman was admitted to our hospital with a complaint of vomiting after a meal. She had been experiencing nausea following eating since the last 2 months. On admission, the patient was 153 cm tall and weighed 46.2 kg. A physical examination revealed no abdominal mass or tenderness. Her blood pressure was 118/71 mmHg, and her heart rate was 64 bpm. Blood examination revealed a white blood cell count of 9900/mm3 and a hemoglobin concentration of 12.5 g/dl. Her total bilirubin and fasting blood sugar levels were 0.65 mg/dl and 126 mg/dl, respectively. The levels of tumor markers CEA, CA19-9, and AFP were 1.9 ng/ml, 14.8 U/ml, and 2.2 ng/ml, respectively.
Upper gastrointestinal endoscopy revealed a Type 2 tumor with stenosis at the distal portion of the papilla of Vater (Fig. 1), and the endoscopic biopsy specimen showed a well-differentiated tubular adenocarcinoma of the duodenum. The duodenogram revealed a Type 2 tumor at the 4th portion of the duodenum (Fig. 2). Computed tomography of the abdomen revealed an irregular thick wall of the 4th portion of the duodenum and no lymph nodes swollen intra-abdominal cavity (Fig. 3). The patient underwent surgery. Laparotomy did not reveal direct invasion into the pancreas, peritoneal dissemination, or distant metastasis. However, macroscopic examination revealed tumor extension through serosal infiltration. Rapid histological diagnosis during surgery showed no lymph node metastasis around the pancreas. Partial resection of the duodenum and jejunum accompanied with lymph node dissection along the superior mesenteric artery was performed. The inferior pancreaticoduodenal artery and 1st jejunal artery were ligated for lymphadenectomy. Histological examination showed well-differentiated tubular adenocarcinoma partially comprising mucinous adenocarcinoma (Fig. 4) and no lymph node metastasis microscopically. The definitive diagnosis was primary adenocarcinoma of the 4th portion of the duodenum, T4N0M0, Stage II according to the TNM classification of malignant tumors (American Joint committee on Cancer). Postoperative upper gastrointestinal investigation did not show stenosis or leakage. The anastmosis that had obstructed the passage functionally had conservatively improved. The patient started a diet on POD 18 and left the hospital on POD 34. Her postoperative course was uneventful, and she is without any sign of recurrence 5 years later.
Fig. 1.
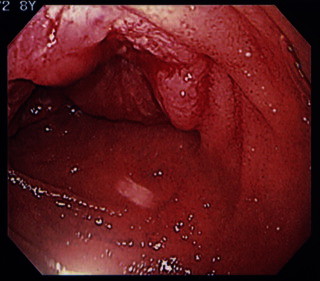
Upper gastrointestinal endoscopy showing a Type 2 tumor around the circumference with stenosis at distal portion of the papilla of Vater. Endoscopic biopsy specimen showing a well-differentiated tubular adenocarcinoma of the duodenum.
Fig. 2.

The duodenogram showing a Type 2 tumor of the 4th portion of the duodenum.
Fig. 3.

Abdominal computed tomography scan showing an irregularly thick wall of the 4th portion of the duodenum. No lymph nodes were found around the pancreas, superior mesenteric artery, or the aorta.
Fig. 4.
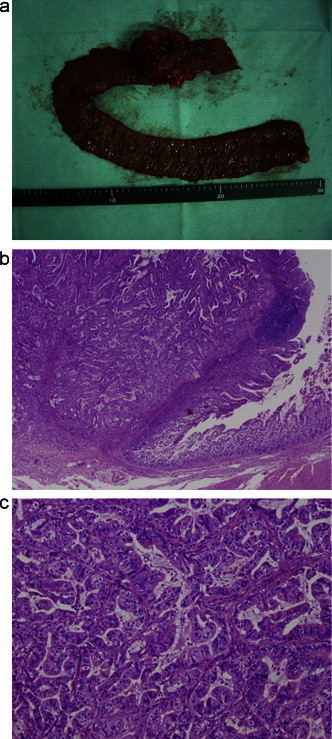
(A) The resected specimen showing a Type 2 tumor at the 4th portion of the duodenum, measuring 50 mm × 45 mm in size. (B) Histological findings of the resected specimen showing a well-differentiated tubular adenocarcinoma (Hemotoxylin Eosin stain, magnification 20×). (C) Histological findings of the resected specimen showing a well-differentiated tubular adenocarcinoma (Hemotoxylin Eosin stain, magnification 100×).
3. Discussion
Primary adenocarcinoma of the duodenum (PDA) is a rare malignant tumor, accounting for 0.3–0.5% of all gastroenteral malignancies.4,5 Approximately 30–50% small intestinal adenocarcinomas occur in the duodenum.6–8 Studies show that 1–15% tumors are located in the 1st portion, 50–75% in the 2nd portion, 14–33% in the 3rd portion, and 5–17% in the 4th portion of the duodenum.9–11 Primary adenocarcinoma in the 2nd portion of the duodenum is most common, whereas that in the 4th portion is relatively less common. There is an average delay of 2–15 months from the onset of symptoms to the time of diagnosis of PDA.12 Upper gastrointestinal endoscopy screening cannot reveal the disease within the horizontal and ascending portions. Examining the entire duodenum using upper gastrointestinal endoscopy is challenging; adenocarcinomas of the 3rd and 4th portions of the duodenum are frequently inaccessible using endoscopy, and most cases require multiple investigations.13 In fact, the 1st endoscopic examination in our patient could not identify the duodenal tumor. A definitive diagnosis of adenocarcinoma was made 2 months after the onset of her symptoms. However, new modalities such as double-balloon enteroscopy or capsule endoscopy can make diagnosis of small bowel or duodenal adenocarcinoma easier.1,14
Some studies have reported that lymph node status, pancreas invasion, duodenum invasion, and tumor size are predicators of prognosis for survival in patients with duodenal adenocarcinoma who underwent surgery.15–18 In contrast, some other studies have reported that tumor size, tumor location within the duodenum, depth of partial penetration, local nodal metastases, tumor differentiation, and invasion of the pancreas were not predictive of prognosis.10,12 There were no clear relationship between tumor differentiation and outcome.2,10,12
Some papers have reported that radical resection offers good long-term results for locally advanced duodenal adenocarcinoma. Resected patients and nonresected patients with PDA had 5-year survival rates of 25–75% and 0% respectively.12,15,19 Five-year survival rates for T4 stage and non-T4 stage patients with PDA were 20% and 40%, respectively.2 It was reported a five-year survival rates in stage I and II of 100% and 52% respectively and 45% and 0% at stage III and IV, respectively.19 It has been reported that life expectancy after resection of the 1st and 2nd portion of the duodenum is longer than that after resection of the 3rd and 4th portions. The median survival time after resection of the 1st and 2nd portions of the duodenum and after resection of the 3rd and 4th portions were 30 months and 46 months, respectively.13 Five-year survival rate for resection of the 3rd and 4th portions of the duodenum was 58%, whereas that of 1st and 4th portions was 32%.16
Early stage duodenal carcinoma should be considered for endoscopic mucosal resection. Advanced stages of PDA require surgical resection for a cure. Patients with PDA, who are medically fit to undergo surgery, should be given the option of aggressive resection.2 Duodeno-cephalo-pancreatectomy (DCP) and segmental resection of the duodenum are employed for treating PDA.20 DCP remains the standard treatment for adenocarcinomas of the 1st and 2nd portion of the duodenum. Patients with locally advanced (N1) tumors (Stage III) can benefit from this aggressive approach with good long-term results.15 Some studies have reported good survival results following segmental duodenectomy despite limited lymph adenectomy occurring during surgical procedure and considerably lower postoperative morbidity.13,16 Segmental duodenectomy is the preferred resection method for patients with adenocarcinoma of the 3rd and 4th portions of the duodenum.13 Our patient had a T4 stage well-differentiated tubular adenocarcinoma without histological lymph node metastases around the pancreas head and no macroscopic invasion of the pancreas or surgical margin. We decided to treat our patient with partial resection of the duodenum and jejunum, and she is doing well without any sign of recurrence five years later.
4. Conclusion
PDA of the 4th potion is rare, and studies have reported this cancer in a small number of patients. The indications for the preferred surgical method require to be clarified by larger studies. This report describes a case of primary adenocarcinoma of the 4th portion of the duodenum, successfully treated by partial resection of the duodenum and jejunum.
Conflicts of interest
The authors report no conflicts of interest.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request. All we authors have to protect the privacy of the patient.
Author contributions
Toru Nakano had made data collection availing help from Kenji Hirau, and written the thesis/paper along with Koh Sugawara. Yutaka Hirano, Masaji Hashimoto, Tsuneo Kaiho and Noriaki Ohuch supervised the entire process.
References
- 1.Safatle-Ribeiro A.V., Franzini T.A., Kuga R., Ishida R.K., Baba E.R., Mendes D.C. Double-balloon enteroscopy in the diagnosis of an adenocarcinoma of the fourth portion of the duodenum: report of a case. Clinics (Sao Paulo) 2007;62(3):353–356. doi: 10.1590/s1807-59322007000300022. Epub 2007/06/26. [DOI] [PubMed] [Google Scholar]
- 2.Hurtuk M.G., Devata S., Brown K.M., Oshima K., Aranha G.V., Pickleman J. Should all patients with duodenal adenocarcinoma be considered for aggressive surgical resection? American Journal of Surgery. 2007;193(3):319–324. doi: 10.1016/j.amjsurg.2006.09.013. discussion 24–5. Epub 2007/02/27. [DOI] [PubMed] [Google Scholar]
- 3.Nakayama Y., Kadowaki K., Nagata N., Itoh H., Hirano Y. Depressed type early duodenal cancer. A case report. Japanese Journal of Gastroenterological Surgery. 2000;33:477–481. [Google Scholar]
- 4.Alwmark A., Andersson A., Lasson A. Primary carcinoma of the duodenum. Annals of Surgery. 1980;191(1):13–18. doi: 10.1097/00000658-198001000-00003. Epub 1980/01/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spira I.A., Ghazi A., Wolff W.I. Primary adenocarcinoma of the duodenum. Cancer. 1977;39(4):1721–1726. doi: 10.1002/1097-0142(197704)39:4<1721::aid-cncr2820390450>3.0.co;2-m. Epub 1977/04/01. [DOI] [PubMed] [Google Scholar]
- 6.Ouriel K., Adams J.T. Adenocarcinoma of the small intestine. American Journal of Surgery. 1984;147(1):66–71. doi: 10.1016/0002-9610(84)90036-9. Epub 1984/01/01. [DOI] [PubMed] [Google Scholar]
- 7.Vincent M.I.N.T. Primary carcinoma of the duodenum. American Surgeon. 1961;27:744–750. [Google Scholar]
- 8.Cunningham J.D., Aleali R., Aleali M., Brower S.T., Aufses A.H. Malignant small bowel neoplasms: histopathologic determinants of recurrence and survival. Annals of Surgery. 1997;225(3):300–306. doi: 10.1097/00000658-199703000-00010. Epub 1997/03/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Delcore R., Thomas J.H., Forster J., Hermreck A.S. Improving resectability and survival in patients with primary duodenal carcinoma. American Journal of Surgery. 1993;166(6):626–630. doi: 10.1016/s0002-9610(05)80668-3. discussion 30–1. Epub 1993/12/01. [DOI] [PubMed] [Google Scholar]
- 10.Pickleman J., Koelsch M., Chejfec G. Node-positive duodenal carcinoma is curable. Archives of Surgery. 1997;132(3):241–244. doi: 10.1001/archsurg.1997.01430270027004. Epub 1997/03/01. [DOI] [PubMed] [Google Scholar]
- 11.Rotman N., Pezet D., Fagniez P.L., Cherqui D., Celicout B., Lointier P. Adenocarcinoma of the duodenum: factors influencing survival. French Association for Surgical Research. British Journal of Surgery. 1994;81(1):83–85. doi: 10.1002/bjs.1800810128. Epub 1994/01/01. [DOI] [PubMed] [Google Scholar]
- 12.Hu J.X., Miao X.Y., Zhong D.W., Dai W.D., Liu W., Hu W. Surgical treatment of primary duodenal adenocarcinoma. Hepato-Gastroenterology. 2006;53(72):858–862. Epub 2006/12/13. [PubMed] [Google Scholar]
- 13.Lowell J.A., Rossi R.L., Munson J.L., Braasch J.W. Primary adenocarcinoma of third and fourth portions of duodenum. Favorable prognosis after resection. Archives of Surgery. 1992;127(5):557–560. doi: 10.1001/archsurg.1992.01420050081010. Epub 1992/05/01. [DOI] [PubMed] [Google Scholar]
- 14.Schwartz G.D., Barkin J.S. Small-bowel tumors detected by wireless capsule endoscopy. Digestive Diseases and Sciences. 2007;52(4):1026–1030. doi: 10.1007/s10620-006-9483-8. Epub 2007/03/24. [DOI] [PubMed] [Google Scholar]
- 15.Bucher P., Gervaz P., Morel P. Long-term results of radical resection for locally advanced duodenal adenocarcinoma. Hepato-Gastroenterology. 2005;52(66):1727–1729. Epub 2005/12/13. [PubMed] [Google Scholar]
- 16.Kaklamanos I.G., Bathe O.F., Franceschi D., Camarda C., Levi J., Livingstone A.S. Extent of resection in the management of duodenal adenocarcinoma. American Journal of Surgery. 2000;179(1):37–41. doi: 10.1016/s0002-9610(99)00269-x. Epub 2000/03/29. [DOI] [PubMed] [Google Scholar]
- 17.Ohigashi H., Ishikawa O., Tamura S., Imaoka S., Sasaki Y., Kameyama M. Pancreatic invasion as the prognostic indicator of duodenal adenocarcinoma treated by pancreatoduodenectomy plus extended lymphadenectomy. Surgery. 1998;124(3):510–515. Epub 1998/09/16. [PubMed] [Google Scholar]
- 18.Ryder N.M., Ko C.Y., Hines O.J., Gloor B., Reber H.A. Primary duodenal adenocarcinoma: a 40-year experience. Archives of Surgery. 2000;135(9):1070–1074. doi: 10.1001/archsurg.135.9.1070. discussion 4–5. Epub 2000/09/12. [DOI] [PubMed] [Google Scholar]
- 19.Santoro E., Sacchi M., Scutari F., Carboni F., Graziano F. Primary adenocarcinoma of the duodenum: treatment and survival in 89 patients. Hepato-Gastroenterology. 1997;44(16):1157–1163. Epub 1997/07/01. [PubMed] [Google Scholar]
- 20.Sista F., Santis G.D., Giuliani A., Cecilia E.M., Piccione F., Lancione L. Adenocarcinoma of the third duodenal portion: case report and review of literature. World Journal of Gastrointestinal Surgery. 2012;4(1):23–26. doi: 10.4240/wjgs.v4.i1.23. Epub 2012/02/22. [DOI] [PMC free article] [PubMed] [Google Scholar]


