Abstract
Objective
To assess the impact of endometriosis on health-related quality of life (HRQoL) and work productivity.
Design
Multicenter cross-sectional study with prospective recruitment.
Setting
Sixteen clinical centers in ten countries.
Patient(s)
A total of 1,418 premenopausal women, aged 18–45 years, without a previous surgical diagnosis of endometriosis, having laparoscopy to investigate symptoms or to be sterilized.
Intervention(s)
None.
Main Outcome Measure(s)
Diagnostic delay, HRQoL, and work productivity.
Result(s)
There was a delay of 6.7 years, principally in primary care, between onset of symptoms and a surgical diagnosis of endometriosis, which was longer in centers where women received predominantly state-funded health care (8.3 vs. 5.5 years). Delay was positively associated with the number of pelvic symptoms (chronic pelvic pain, dysmenorrhoea, dyspareunia, and heavy periods) and a higher body mass index. Physical HRQoL was significantly reduced in affected women compared with those with similar symptoms and no endometriosis. Each affected woman lost on average 10.8 hours (SD 12.2) of work weekly, mainly owing to reduced effectiveness while working. Loss of work productivity translated into significant costs per woman/week, from US$4 in Nigeria to US$456 in Italy.
Conclusion(s)
Endometriosis impairs HRQoL and work productivity across countries and ethnicities, yet women continue to experience diagnostic delays in primary care. A higher index of suspicion is needed to expedite specialist assessment of symptomatic women. Future research should seek to clarify pain mechanisms in relation to endometriosis severity.
Keywords: Endometriosis, quality of life, work productivity
Endometriosis (the presence of endometrial-like tissue outside the uterus) is a chronic disease associated with pelvic pain and subfertility (1). Prevalence rates in the general population are unknown, because a definitive diagnosis is established only at laparoscopy. However, based on community prevalence estimates of symptoms (2–4), endometriosis probably affects 10% of all and 30%–50% of symptomatic premenopausal women (5). This represents ~176 million affected women worldwide (6).
The diagnosis may be overlooked in primary care, and patients think that this causes unnecessary suffering and reduced quality of life (7). However, the impact of endometriosis has been poorly researched (8), focusing on highly selected, mainly Western populations with small sample sizes, poorly selected control subjects, and inadequately validated instruments (9–12). Therefore, the influence on quality of life of factors such as disease stage, symptom severity, and care seeking remains unclear (13). In one U.S. study, the direct costs of endometriosis were estimated at US$2,801 per woman (14), but indirect costs were not provided. Few studies have quantified reported absence from work (15, 16); however, these are geographically limited and focused on women who knew their disease status, with potential for recall bias. Furthermore, work absenteeism does not describe the full spectrum of disease-related work productivity loss. To generate meaningful estimates, both presenteeism (reduced productivity while at work) and absenteeism (time lost from work) must be considered (17).
The lack of robust information about the impact of endometriosis world-wide led us to initiate the Global Study of Women’s Health (GSWH) to investigate the care-seeking experience of affected women and to examine in detail the impact of endometriosis on health-related quality of life (HRQoL) and work productivity on a global scale.
METHODS
The methods, reported in detail elsewhere (18), are summarized here.
Recruitment and Study Population
The GSWH is a cross-sectional study in 16 hospitals in 10 countries. Between August 2008 and January 2010, we prospectively recruited consecutive premenopausal women, aged 18–45 years, scheduled for a laparoscopy: 1) to investigate endometriosis-associated pelvic pain (i.e., chronic pelvic pain (CPP), dysmenorrhoea, pain during or after intercourse), and/or subfertility, with or without pelvic mass; or 2) to be sterilized. Women with previous surgical diagnosis of endometriosis were excluded. The Mid and South Buckinghamshire Research Ethics Committee and local Ethics Committees approved the study.
Data Collection
In the week before surgery, women completed a 67-item questionnaire in their own language about presenting complaints and their effect on HRQoL and ability to function, medical history, reproductive factors, and health care resource use (http://www.endometriosisfoundation.org/GSWH-questionnaire-English.pdf). Experienced gynecologists recorded laparoscopic findings in a standard manner (http://www.endometriosisfoundation.org/GSWH-surgical-sheet.pdf). Following European Society of Human Reproduction and Embryology (ESHRE) guidelines, endometriosis was diagnosed on visual evidence alone (1). Disease severity was staged using the revised American Fertility Society (rAFS) classification: I (minimal), II (mild), III (moderate), or IV (severe) (19). Stages I/II and III/IV were amalgamated in analyses, as in earlier studies (20, 21).
Health-Related Quality of Life and Work Impairment
Validated language versions of the Short Form–36 version 2 (SF36v2) questionnaire were used to measure HRQoL (22). A general health version of the Work Productivity and Activity Impairment (WPAI:GH) questionnaire (23) was incorporated to: 1) assess absenteeism and presenteeism in symptomatic employed women; and 2) assess the impact of symptoms on activities. We, as others have (24), used a 4-week assessment period instead of the original 7 days, because the week before surgery may not reflect true work patterns and endometriosis-associated symptoms fluctuate cyclically. Work productivity and other activities were measured on a 0 (“symptoms had no effect on work”) to 10 (“symptoms completely prevented working”) scale.
Analyses
Comparison groups
There were three outcome groups: 1) Women with endometriosis (including disease found at sterilisation); 2) symptomatic control women without endometriosis; and 3) sterilization control women without endometriosis. Comparisons were also made across sites (centers), with those that recruited ≤25 women combined into an “other” center. See Supplemental Material 1 (available online at www.fertstert.org) for methods regarding characteristics of the study population at recruitment and the care-seeking experience.
Endometriosis and HRQoL
For each SF36v2 dimension, item scores were coded, summed, and transformed on a 0–100 (worst to best possible health state) scale; missing data were not substituted. The physical health (PCS) and mental health (MCS) component summaries were calculated, standardized to normative data from the Third Oxford Health and Lifestyles Survey (25) (Supplemental Material 2, available online at www.fertstert.org).
Endometriosis and work productivity
The WPAI:GH dimensions were calculated by recruitment centre and outcome group using standard methods (23) (Supplemental Material 3, available online at www.fertstert.org). Lost hours multiplied by 2007 hourly labour cost (26) produced estimates of the cost of work productivity loss for countries.
Statistical Methods
We used chi-square analyses and Fisher’exact tests to study categoric variables in the Stata program (v.11). We investigated continuous variables using independent-sample t test or nonparametric Mann-Whitney U test as appropriate. Multiple logistic and linear regression analyses were used to study associations between variables and outcomes, adjusting for potential confounders independently associated with exposure and outcome of interest in univariate analysis. P values of <.05 were considered nominally significant.
RESULTS
Study Population and Diagnostic Incidence of Endometriosis
In total, 1,486 (89%) of 1,669 eligible women agreed to participate. Fifty-two had not undergone surgery by the close of recruitment, and 16 did not meet inclusion criteria, leaving complete data for 1,418 women (Supplemental Fig. 1, available online at www.fertstert.org).
Endometriosis was found in 745/1,418 (cumulative diagnostic incidence 52.5%, 95% confidence interval [CI] 49.9%–55.1%), ranging from 34.8% (95% CI 28.3–41.2%) in Oxford to 100% in Siena. Diagnostic incidence was 54.3% (699/1,287, 95% CI 51.6%–57%) among women undergoing laparoscopy for symptoms and 35.1% (46/131, 95% CI 26.9–43.3%) in those being sterilized. Among affected women, 60.5% (95% CI 57%–64%) had moderate/severe disease. Of the 46 affected women undergoing sterilization, 25 (54.3%, 95% CI 40.0%–68.7%) had moderate/severe disease (Supplemental Fig. 2, available online at www.fertstert.org).
Demographic and Clinical Characteristics
Compared with symptomatic control women (Table 1), affected women had higher educational achievement (P=.004) and lower body mass index (BMI; P<.001) and were less likely to be married or cohabiting (P=.002) (Table 1; Supplemental Material 4; Supplemental Table 1).
TABLE 1.
Characteristics of the women at recruitment.
| No endometriosis (n = 673) |
|||||
|---|---|---|---|---|---|
| Characteristic | Endometriosis (n = 745) |
Symptomatic (n = 587) |
P valuea | Laparoscopic sterilization (n = 86) |
P valueb |
| Demographic/personal | |||||
| Age (y) [Mean (SD)] | 32.5 (6.2) | 33.1 (6.4) | .10 | 37.2 (5.0) | <.001 |
| Postsecondary education [% (n)] |
69.9 (521) | 61.7(362) | .004 | 45.3 (39) | <.001 |
| In employment [% (n)] | 78.5 (585) | 73.6 (432) | .054 | 70.9 (61) | .067 |
| Ethnicity [% (n)] | .005 | <.001 | |||
| White | 50.1 (373) | 45.3 (266) | 48.8 (42) | ||
| Asian/Oriental | 32.0 (238) | 35.4 (208) | 8.1 (7) | ||
| Black | 7.0 (52) | 10.6 (62) | 8.1 (7) | ||
| Other/mixed | 9.7 (72) | 6.1 (36) | 33.7 (29) | ||
| Married or living with partner [% (n)] |
73.3 (546) | 80.2 (471) | .002 | 84.9 (73) | .017 |
| Body mass index (kg/m2) [mean (SD)] |
22.5 (4.1) | 23.4 (4.8) | <.001 | 25.2 (4.4) | <.001 |
| Smoked >100 cigarettes in lifetime [% (n)] |
27.2 (203) | 25.6 (150) | .53 | 39.5 (34) | .012 |
| Regular vigorous exercise in past 3 months [% (n) |
27.0 (201) | 25.2 (148) | .86 | 20.9 (18) | .54 |
| Clinical | |||||
| Hormonal contraception in past 3 months [% (n)] |
23.4 (174) | 16.9(99) | .004 | 45.3 (39) | <.001 |
| Reasons for hormonal contraception [% (n)] | .42 | <.001 | |||
| Contraception/other | 58.6 (102) | 63.6 (63) | 97.4 (38) | ||
| Pelvic pain, irregular or heavy periods |
40.2 (70) | 35.4 (35) | 2.6 (1) | ||
| Menstrual cycle length [% (n)] | .041 | .23 | |||
| ≤24 days | 16.2 (121) | 13.8(81) | 20.9 (18) | ||
| 25-32 days | 63.2 (471) | 60.3 (354) | 58.1 (50) | ||
| ≥33 days | 5.4 (40) | 8.5 (50) | 2.3 (2) | ||
| Menstrual duration (days) [mean (SD)] |
4.9 (2.8) | 4.9 (2.3) | .99 | 4.7 (2.4) | .63 |
| Parity [mean (SD)] | 0.2 (0.5) | 0.5(1.0) | <.001 | 1.8 (1.4) | <.001 |
| Gravidity [mean (SD)] | 0.5 (0.9) | 1.0(1.4) | <.001 | 2.3 (1.6) | <.001 |
| Subfertility [% (n)] | 39.6 (295) | 51.8 (304) | <.001 | 18.6 (16) | <.001 |
| Type of symptoms reported [% (n)] | |||||
| Pelvic pain, no subfertility |
42.7 (318) | 29.3 (172) | <.001 | 8.1 (7) | <.001 |
| Pelvic pain and subfertility |
17.7 (132) | 15.2 (89) | .21 | 2.3 (2) | <.001 |
| Subfertility, no pelvic pain |
13.4 (100) | 28.6(168) | <.001 | 4.7 (4) | .02 |
| No pelvic pain, no subfertility |
26.2 (195) | 27.1 (159) | .72 | 84.7 (73) | <.001 |
| No. of symptoms [mean (SD)] | |||||
| “Pelvic” symptoms | 1.5 (1.5) | 1.0 (1.3) | <.001 | 0.3 (0.9) | <.001 |
| “Bowel” symptoms | 0.5 (0.9) | 0.3 (0.6) | <.001 | 0.1 (0.4) | <.001 |
| “Urinary” symptoms | 0.2 (0.5) | 0.1 (0.4) | .015 | 0.0 (0.1) | .005 |
| “Pelvic mass” symptoms |
1.3 (0.8) | 0.9 (0.8) | <.001 | 1.0 (0.4) | .004 |
| Pelvic pain severity NRS 0–10 [mean (SD)] |
5.6 (2.2) | 4.7 (2.2) | <.001 | 5.0 (2.5) | .048 |
| Other pathologies at laparoscopy [% (n)] | |||||
| Nonendometriotic adhesions |
11.0 (82) | 34.2 (201) | <.001 | 10.5 (9) | .89 |
| Nonendometriotic cysts |
10.6(79) | 25.7 (151) | .018 | 4.7 (4) | .81 |
| Fibroids | 16.1 (120) | 21.5 (126) | .015 | 3.5 (3) | .54 |
| Otherc | 2.8 (21) | 8.2 (48) | <.001 | 1.2 (1) | .37 |
| Comorbidity [% (n)]d | |||||
| Cancer | 1.5 (11) | 1.9 (11) | .58 | 2.3 (2) | .55 |
| Autoimmune/atopic conditions |
19.7 (147) | 20.1 (118) | .64 | 14.0 (12) | .20 |
| Other | 76.9 (573) | 60.3 (354) | <.001 | 47.8 (41) | <.001 |
| Any | 82.4 (614) | 66.3 (389) | <.001 | 53.5 (46) | <.001 |
Endometriosis vs. symptomatic control subjects.
Endometriosis vs. laparoscopic sterilization control subjects.
Other pathologies were mainly teratoma and bilateral tubal blockage.
Cancer included breast and ovarian cancer, melanoma and Hodgkin/non-Hodgkin lymphoma; autoimmune/atopic conditions included asthma, eczema, Hashimoto disease, multiple sclerosis, rheumatoid arthritis, Sjogren syndrome, thyroid disease, and systematic lupus erythematosus; Other included chronic fatigue syndrome, deafness, fibromyalgia, depression, diabetes, fibroids, glandular fever, imperforate hymen, migraines, ovarian cysts, polycystic ovarian syndrome, pyloric stenosis, scoliosis, and mitral valve prolapse.
Endometriosis: Care-Seeking Experience
Diagnostic delay was 6.7 years (SD 6.3) in affected women and 5.9 years (SD 6.0) in symptomatic control women (P=.017). This was mainly due to delays in referral from primary care physician to gynecologist, with women reporting an average of seven visits before specialist referral. After adjusting for demographic factors, type of presenting symptoms, severity of pelvic pain, and comorbidity, delay was longer in women with higher BMI (P=.040) and more “pelvic” symptoms (P<.001; Supplemental Table 2, available online at www.fertstert.org).
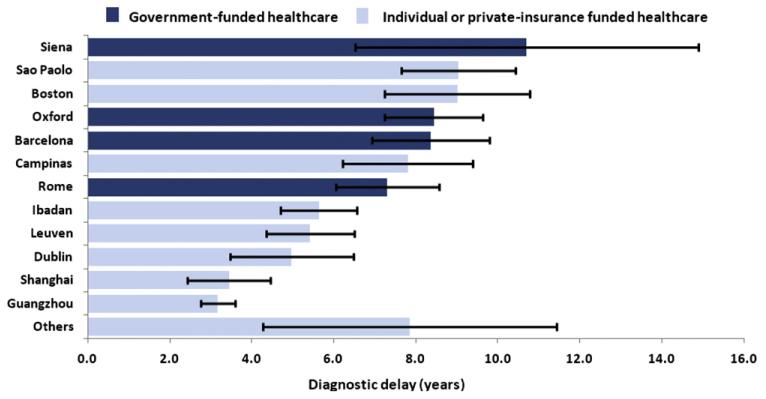
Diagnostic delay varied across centers: 3.3 years (SD 3.6) in Guangzhou to 10.7 years (SD 9.3) in Siena (Fig. 1). After adjustment for potential confounders (site, demographic differences, BMI, symptom type and severity, and comorbidity), it was significantly longer in centers with predominantly state-funded (8.3 years, 95% CI 7.5–9.0) compared with self- or insurance-funded (5.5 years, 95% CI 5.1–5.9) health care (P=.001; Fig. 1).
FIGURE 1.
Diagnostic delay by center of recruitment. Others comprises Buenos Aires, Washington, DC, San Francisco, and Palo Alto.
Endometriosis and Health-Related Quality of Life
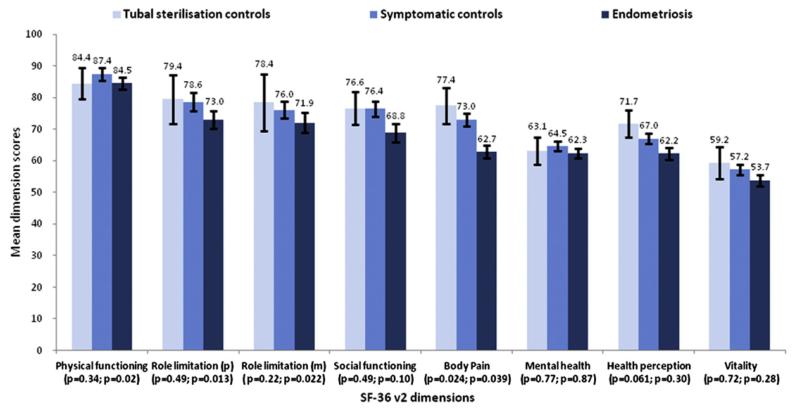
Compared with both symptomatic and sterilization control women, mean HRQoL scores in affected women were poorest in all SF36v2 dimensions except physical functioning. After adjusting for relevant covariates (demographic factors, pelvic pain severity, type and number of presenting symptoms, and comorbidity), affected women had significantly reduced HRQoL compared with symptomatic control women in physical functioning (P=.02), physical (P=.013) and mental (P=.022) role limitation, and bodily pain (P=.039; Fig. 2). Compared with sterilization control women, affected women had significantly poorer HRQoL only in bodily pain (P=.024). Symptomatic control women and affected women had lower PCS scores, and all three outcome groups had lower MCS scores, than the normative population; compared with symptomatic controls, affected women had significantly reduced PCS but not MCS scores (Fig. 2; Supplemental Fig. 3, available online at www.fertstert.org).
FIGURE 2.
Health-related quality of life in women with endometriosis (n = 745), symptomatic control women (n = 587), and laparoscopic sterilization control women (n = 86): SF-36v2 dimension scores with adjusted P valuesb and 95% confidence intervals. A lower score means lower health-related quality of life. P values are presented as (P=x; P=y), x being the P value for comparison of endometriosis and laparoscopic sterilization control subjects and y being the P value for comparison of endometriosis and symptomatic control subjects. P values are adjusted for education, maritalstatus, employment status, pelvic pain severity, type and number of presenting symptoms, and comorbidity.
HRQoL was higher in women whowere in paid or self-employment (P<.001) and who did not report any pelvic pain (P=.017), but lower in those who had more severe pelvic pain (P<.001). After adjusting for site (center), health care funding, pelvic pain, subfertility, severity of pelvic pain, and number of “pelvic” and “bowel” symptoms reported, longer diagnostic delays were associated with reduced physical HRQoL in affected women (P=.047; Supplemental Material 5, available online at www.fertstert.org).
Endometriosis and Work Productivity
See Supplemental Material 6 (available online at www.fertstert.org) for more. Affected women reported greater absenteeism and presenteeism compared with symptomatic control women (Table 2): Overall work productivity loss was 10.8 h/wk (SD 12.2) versus 8.4 h/wk (SD 10.2), respectively (P<.001; Table 2).
TABLE 2.
Work productivity in symptomatic women with and without endometriosis.
| Work and productivity loss variables | Endometriosis (n = 745) |
Symptomatic control (n = 587) |
Unadjusted P value |
Adjusted P valuea |
|---|---|---|---|---|
| General | ||||
| Weekly hours paid to work, mean (SD) | 39.2 (14.0) | 38.6 (12.1) | .44 | .047 |
| Weekly hours actually worked, mean (SD) | 24.9 (16.1) | 28.5 (25.0) | .01 | .32 |
| Work Productivity and Activity Impairment dimensions | ||||
| Absenteeismb | ||||
| %, mean (SD) | 11.2 (21.6) | 8.5 (20.0) | .069 | .58 |
| h/wk, mean (SD) | 4.4 (8.0) | 3.3 (8.4) | .24 | .82 |
| Presenteeismc | ||||
| %, mean (SD) | 25.8 (26.8) | 17.9 (22.1) | <.001 | .26 |
| h/wk, mean (SD) | 6.4 (7.9) | 5.1 (6.7) | .001 | .36 |
| Overall work productivity lossd | ||||
| %, mean (SD) | 32.3 (29.8) | 22.0 (25.1) | <.001 | .045 |
| h/wk, mean (SD) | 10.8 (12.2) | 8.4 (10.2) | <.001 | .032 |
| Activity impairmente | ||||
| %, mean (SD) | 28.5 (26.9) | 19.6 (23.4) | <.001 | .48 |
Variables adjusted for included educational attainment, marital status, type and number of symptoms, severity of pelvic pain, and comorbidity.
Time absent from work owing to symptoms.
Reduced effectiveness while on the job owing to symptoms.
Combination of absenteeism and presenteeism.
Reduced effectiveness while doing non-work-related activities, e.g., child care, exercise, housekeeping, etc.
In multivariate analyses, overall work productivity loss in employed women was greater in those with pelvic pain without subfertility (P=.030) and more severe pelvic pain (P<.001) and less in those who had higher educational attainment (P=.032). After adjusting for educational attainment, marital status, type and number of symptoms, pelvic pain severity, and comorbidity, we found that absenteeism (P=.019), presenteeism (P=.033) and overall work productivity loss (P=.014) increased with increasing disease severity (Supplemental Fig. 4, available online at www.fertstert.org).
Absenteeism-related costs ranged from US$1/wk in Nigeria to US$231/wk in Italy; presenteeism costs ranged from US$3/wk in Nigeria to US$250/wk in the USA (Supplemental Fig. 5, available online at www.fertstert.org).
DISCUSSION
Patient groups have advocated that endometriosis is associated with diagnostic delay, reduced quality of life, and loss of work productivity. However, past studies, mainly in Western countries, are limited by small sample sizes (9, 12), suboptimal control selection (10), lack of geographic spread (11), and potential recall bias. Using robust quantitative methods, the GSWH is the first to demonstrate the substantial impact of endometriosis on women and society across different countries and ethnicities. These data have never been available in most of the participating countries.
We found an average diagnostic delay of 6.7 years (consistent with earlier U.K. and U.S. reports (27–29). Delay was longer in women with more “pelvic” symptoms (e.g., CPP, dysmenorrhoea, and dyspareunia) and a higher BMI, and at centers delivering predominantly state-funded health care. We showed that delays are strongly associated with care-seeking experiences in primary care, as previously suggested (30, 31), but we do not exclude other reasons. For example, women may delay seeking help because of the “discrediting” nature of menstrual irregularities and risk of stigmatization (27, 32).
An association between higher BMI and diagnostic delay is recognized in other diseases (33, 34); in endometriosis it may arise because of difficulty detecting pathology on pelvic examination. The association between diagnostic delay and health care funding in endometriosis is novel, although similar findings are reported in cancer patients (35). Rationing of health care and differences in readiness of clinicians to suggest surgery in private- versus public-funded health care settings are possible explanations but other influences, such as negative experiences of primary care consultations, cannot be excluded (31).
The effect of endometriosis on physical (but not mental) HRQoL of women was substantial, with SF36v2 PCS scores similar to those reported in women with cancer (36). The effect was less if women were employed and free of pelvic pain, and worse with severe pelvic pain and advanced disease. Notably, even after adjusting for covariates, such as pain severity and comorbidity, bodily pain, health perception, and PCS scores were significantly reduced in those with moderate/severe compared with minimal/mild disease.
We demonstrated that pelvic pain and disease severity are the major drivers of work productivity loss in endometriosis. Although reduced effectiveness at work is less frequently assessed and recorded than work absence, it accounted for nearly 60% of total work productivity loss. The annual costs (per employed woman) of endometriosis-associated work productivity loss (varying from US$208 in Nigeria to US$23,712 in Italy), is markedly higher than earlier estimates (direct costs US$2,801 and indirect costs US$1,023 in the U.S.) (14, 15), but those studies only considered absenteeism.
The greater impairment in HRQoL (particularly bodily pain) and work productivity in moderate/severe versus minimal/mild disease, after accounting for pelvic pain severity and comorbid conditions, is intriguing and could have a number of causes. Despite careful adjustment, there might still be residual differences in symptom severity or differential reporting of comorbid conditions in case subjects and symptomatic control subjects, but we would expect these to affect mental as well as physical dimensions, which was not the case. An alternative explanation is the role of central sensitization. This theory, supported by experiments in animals and humans (37–39), suggests that persistent pain stimuli, generated by endometriotic tissue as disease advances, results over time in heightened pain awareness even from regions removed from the tissue itself. If true, such heightened awareness could explain the impact of worsening endometriosis on HRQoL and work productivity.
Although the GSWH was designed to avoid many of the methodologic limitations of earlier studies, it had important potential limitations itself. First, HRQoL and work productivity in the weeks leading up to scheduled surgery may be affected by both the impending surgery and the symptoms themselves. This is perhaps reflected in the reduced SF36v2 summary scores in sterilization control subjects compared with general population standards. However, because women in all groups were undergoing surgery, its effect on comparing results between case and control groups should be negligible. Second, work loss data were self-reported. Although an independent measure of employment would be more reliable, self-reported data compare favorably with more objective data (e.g., employment records) and are an efficient and accurate way to collect data on illness-related work productivity loss (40). Third, we altered the standard 7-day recall period of the WPAI to 4 weeks for the reasons given above. A study that similarly extended the recall period to 4 weeks found that the construct validity of the modified questionnaire was similar to that of the original, though estimates of work productivity impairment were higher (24). Fourth, endometriosis was diagnosed visually, without histologic confirmation, following ESHRE guidelines (1), based on the premise that negative histology does not exclude the presence of disease. Although the hospitals were experienced in diagnosing endometriosis, disease stage might have been inadequately classified. However, combining minimal with mild and moderate with severe stages in analyses minimizes such potential bias. Furthermore, in a post-GSWH validation study, 29 surgeons from 12 of the 16 participating centers viewed nine standardized videos to identify/eliminate and stage endometriosis. Preliminary analysis suggested substantial interrater agreement in disease identification and staging (both Fleiss κ >0.60; unpublished data, by courtesy of Drs C. Becker and K. May, Oxford, U.K.).
The observation that 35.1% of women undergoing sterilization had endometriosis is not surprising, because rates of 3%–45% are reported in such women (41, 42). More surprising is that >50% of them had moderate/severe endometriosis, which may indicate that a relatively large proportion were not asymptomatic. Finally, the variability in both the range of endometriosis prevalence (34.8% in Oxford to 100% in Siena) and the proportion of moderate/severe disease (30%–40% in most centers but nearly 90% in some countries) may relate to a minority of participating centers routinely assessing women with presurgical ultrasound scans and prioritizing surgery in those with evidence of ovarian (endometriotic) cysts, but they may also reflect reality, because the proportion of moderate/severe endometriosis was reported as 63% in Iceland over a 20-year period (43). Although such differences in routine clinical protocols should be borne in mind when interpreting the results, additional adjustment of combined HRQoL and work productivity results according to center showed that key results were unaffected by any such differences.
A key strength of our study was that, to limit information bias, we restricted our study to women undergoing a first laparoscopy for symptoms suggestive of endometriosis or sterilization and collected relevant data before diagnosis. Our results are therefore generalizable to this incident patient group but may underestimate HRQoL and work productivity figures among women who have suffered from the condition for longer.
In conclusion, endometriosis significantly affects women and societies world-wide, but substantial delays in diagnosis exist. Heightened awareness of the disease in primary care should lead to earlier diagnosis, less suffering, and improved work productivity. Future research should address the underlying pain mechanisms in endometriosis and identify symptom control strategies that target those pathways to improve the outlook for affected women.
Supplementary Material
SUPPLEMENTAL FIGURE 1 Participating centers and numbers of women recruited in the Global Study of Women’s Health (n = 1,418).
SUPPLEMENTAL FIGURE 2 Proportions of diagnostic endometriosis incidence and stage by center of recruitment. Others comprises Buenos Aires, Washington, DC, San Francisco, and Palo Alto.
SUPPLEMENTAL FIGURE 3 Health-related quality of life in women with endometriosis (n = 745), symptomatic control women (n = 587), and laparoscopic sterilization control women (n = 86): SF36v2 component summary scores with adjusted P values and 95% confidence intervals. A lower score means lower health-related quality of life. P values are presented as (P=x; P=y), x being the P value for comparison of endometriosis and laparoscopic sterilization control subjects and y being the P value for comparison of endometriosis and symptomatic control subjects. Dashed line represents mean component summary score (50) for normative population. All P values are adjusted for site, education, marital status, employment status, pelvic pain severity, type and number of presenting symptoms, and comorbidity.
SUPPLEMENTAL FIGURE 4 Absenteeism, presenteeism, and overall work productivity loss by endometriosis severity (Revised American Fertility Society classification [rAFS]). Adjusted P values for the association between each work productivity dimension and rAFS disease stage (trend test) are given. Variables adjusted for included educational attainment, marital status, type and number of symptoms, severity of pelvic pain, and comorbidity.
SUPPLEMENTAL FIGURE 5 Monetary loss from endometriosis-associated work absenteeism and presenteeism.
SUPPLEMENTAL TABLE 1 Factors (symptom patterns) and loading symptom variables.
SUPPLEMENTAL TABLE 2 Care-seeking for symptoms, mean (SD).
Acknowledgments
The authors thank all of the women who participated in the GSWH for their valuable contributions. The authors are also grateful to all of the clinical and research assistants at the collaborating centers and thank Andrew Prentice for his contribution to the study protocol and questionnaire design.
Bayer Schering Pharma (BSP) provided a grant to the World Endometriosis Research Foundation (WERF), from which L.H. was paid an honorarium for project management, K.T.Z., F.d.C.N., C.d.C.N., T.d’H., and S.H.K. received institutional grants from WERF as well as the European Union Public Health Programme, K.E.N., K.T.Z., L.H. received support for travel to meetings related the study, K.T.Z. received payment for translation of study questionnaire into Dutch, and C.d.C.N. received payment for translation into Italian. K.T.Z., L.H., S.H.K., and T.d’H. have been consultants for BSP. P.W. has nothing to disclose. C.J. has nothing to disclose.
REFERENCES
- 1.Kennedy S, Bergqvist A, Chapron C, d’Hooghe T, Dunselman G, Greb R, et al. ESHRE guideline for the diagnosis and treatment of endometriosis. Hum Reprod. 2005;20:2698–704. doi: 10.1093/humrep/dei135. [DOI] [PubMed] [Google Scholar]
- 2.Eskenazi B, Warner ML. Epidemiology of endometriosis. Obstet Gynecol Clin North Am. 1997;24:235–58. doi: 10.1016/s0889-8545(05)70302-8. [DOI] [PubMed] [Google Scholar]
- 3.Zondervan KT, Yudkin PL, Vessey MP, Jenkinson CP, Dawes MG, Barlow DH, et al. The community prevalence of chronic pelvic pain in women and associated illness behaviour. Br J Gen Pract. 2001;51(468):541–7. [PMC free article] [PubMed] [Google Scholar]
- 4.Zondervan KT, Cardon LR, Kennedy SH. What makes a good case-control study? Design issues for complex traits such as endometriosis. Hum Reprod. 2002;17:1415–23. doi: 10.1093/humrep/17.6.1415. [DOI] [PubMed] [Google Scholar]
- 5.Rogers PAW, d’Hooghe TM, Fazleabas A, Gargett CE, Giudice LC, Montgomery GW, et al. Priorities for endometriosis research: recommendations from an international consensus workshop. Reprod Sci. 2009;16:335–46. doi: 10.1177/1933719108330568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adamson GD, Kennedy SH, Hummelshoj L. Creating solutions in endometriosis: global collaboration through the World Endometriosis Research Foundation. J Endometriosis. 2010;2:3–6. [Google Scholar]
- 7.Harvey J, Warwick I. Endometriosis. BMJ. 2010;340:c2661. doi: 10.1136/bmj.c2661. [DOI] [PubMed] [Google Scholar]
- 8.Gao X, Yeh YC, Outley J, Simon J, Botteman M, Spalding J. Health-related quality of life burden of women with endometriosis: a literature review. Curr Med Res Opin. 2006;22:1787–97. doi: 10.1185/030079906X121084. [DOI] [PubMed] [Google Scholar]
- 9.Oehmke F, Weyand J, Hackethal A, Konrad L, Omwandho C, Tinneberg HR. Impact of endometriosis on quality of life: a pilot study. Gynecol Endocrinol. 2009;25:722–5. doi: 10.3109/09513590903159607. [DOI] [PubMed] [Google Scholar]
- 10.Petrelluzzi KFS, Garcia MC, Petta CA, Grassi-Kassisse DM, Spadari-Bratfisch RC. Salivary cortisol concentrations, stress and quality of life in women with endometriosis and chronic pelvic pain. Stress. 2008;11:390–7. doi: 10.1080/10253890701840610. [DOI] [PubMed] [Google Scholar]
- 11.Marques A, Bahamondes L, Aldrighi JM, Petta CA. Quality of life in Brazilian women with endometriosis assessed through a medical outcome questionnaire. J Reprod Med. 2004;49:115–20. [PubMed] [Google Scholar]
- 12.Sepulcri RDP, do Amaral VF. Depressive symptoms, anxiety, and quality of life in women with pelvic endometriosis. Eur J Obstet Gynecol Reprod Biol. 2009;142:53–6. doi: 10.1016/j.ejogrb.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Lemaire GS. More than just menstrual cramps: symptoms and uncertainty among women with endometriosis. J Obstet Gynecol Neonatal Nurs. 2004;33:71–9. doi: 10.1177/0884217503261085. [DOI] [PubMed] [Google Scholar]
- 14.Simoens S, Hummelshoj L, d’Hooghe TM. Endometriosis: cost estimates and methodological perspective. Hum Reprod Update. 2007;13:395–404. doi: 10.1093/humupd/dmm010. [DOI] [PubMed] [Google Scholar]
- 15.Mathias SD, Kuppermann M, Liberman RF, Lipschutz RC, Steege JF. Chronic pelvic pain: prevalence, health-related quality of life, and economic correlates. Obstet Gynecol. 1996;87:321–7. doi: 10.1016/0029-7844(95)00458-0. [DOI] [PubMed] [Google Scholar]
- 16.Fourquet J, Gao X, Zavala D, Orengo JC, Abac S, Ruiz A, et al. Patients’ report on how endometriosis affects health, work, and daily life. Fertil Steril. 2010;93:2424–8. doi: 10.1016/j.fertnstert.2009.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hemp P. Presenteeism: at work—but out of it. Harv Bus Rev. 2004;82:49–58. [PubMed] [Google Scholar]
- 18.Nnoaham K, Sivananthan S, Hummelshoj L, Jenkinson C, Webster P, Kennedy S, et al. Multi-center studies of the global impact of endometriosis and the predictive value of associated symptoms. J Endometriosis. 2009;1:36–45. [PMC free article] [PubMed] [Google Scholar]
- 19.American Fertility Society Revised American Fertility Society classification of endometriosis. Fertil Steril. 1985;43:351–2. doi: 10.1016/s0015-0282(16)48430-x. [DOI] [PubMed] [Google Scholar]
- 20.Treloar SA, Hadfield R, Montgomery G, Lambert A, Wicks J, Barlow DH, et al. The International Endogene Study: a collection of families for genetic research in endometriosis. Fertil Steril. 2002;78:679–85. doi: 10.1016/s0015-0282(02)03341-1. [DOI] [PubMed] [Google Scholar]
- 21.Ferrero S, Petrera P, Colombo BM, Navaratnarajah R, Parisi M, Anserini P, et al. Asthma in women with endometriosis. Hum Reprod. 2005;20:3514–7. doi: 10.1093/humrep/dei263. [DOI] [PubMed] [Google Scholar]
- 22.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 23.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4:353–65. doi: 10.2165/00019053-199304050-00006. [DOI] [PubMed] [Google Scholar]
- 24.Fowler JF, Ghosh A, Sung J, Emani S, Chang J, Den E, et al. Impact of chronic hand dermatitis on quality of life, work productivity, activity impairment, and medical costs. J Am Acad Dermatol. 2006;54:448–57. doi: 10.1016/j.jaad.2005.11.1053. [DOI] [PubMed] [Google Scholar]
- 25.Jenkinson C, Stewart-Brown S, Petersen S, Paice C. Assessment of the SF-36 version 2 in the United Kingdom. J Epidemiol Community Health. 1999;53:46–50. doi: 10.1136/jech.53.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Federal Statistics Office of Germany Hourly compensation costs in manufacturing. [Accessed April 5, 2011];2010 Oct 19; Available at: http://www.destatis.de/jetspeed/portal/cms/Sites/destatis/Internet/EN/Content/Statistics/Internatio nales/InternationalStatistics/Topic/Tables/BasicData__LaborCosts,templateId=renderPrint.psml.
- 27.Ballard K, Lowton K, Wright J. What’s the delay? A qualitative study of women’s experiences of reaching a diagnosis of endometriosis. Fertil Steril. 2006;86:1296–301. doi: 10.1016/j.fertnstert.2006.04.054. [DOI] [PubMed] [Google Scholar]
- 28.Husby GK, Haugen RS, Moen MH. Diagnostic delay in women with pain and endometriosis. Acta Obstet Gynecol Scand. 2003;82:649–53. doi: 10.1034/j.1600-0412.2003.00168.x. [DOI] [PubMed] [Google Scholar]
- 29.Hadfield R, Mardon H, Barlow D, Kennedy S. Delay in the diagnosis of endometriosis: a survey of women from the USA and the UK. Hum Reprod. 1996;11:878–80. doi: 10.1093/oxfordjournals.humrep.a019270. [DOI] [PubMed] [Google Scholar]
- 30.Pugsley Z, Ballard K. Management of endometriosis in general practice: the pathway to diagnosis. Br J Gen Pract. 2007;57(539):470–6. [PMC free article] [PubMed] [Google Scholar]
- 31.Denny E, Mann CH. Endometriosis and the primary care consultation. Eur J Obstet Gynecol Reprod Biol. 2008;139:111–5. doi: 10.1016/j.ejogrb.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 32.Seear K. The etiquette of endometriosis: stigmatisation, menstrual concealment and the diagnostic delay. Soc Sci Med. 2009;69:1220–7. doi: 10.1016/j.socscimed.2009.07.023. [DOI] [PubMed] [Google Scholar]
- 33.Marrie RA, Horwitz R, Cutter G, Tyry T, Campagnolo D, Vollmer T. Comorbidity delays diagnosis and increases disability at diagnosis in MS. Neurology. 2009;72:117–24. doi: 10.1212/01.wnl.0000333252.78173.5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arndt V, Stürmer T, Stegmaier C, Ziegler H, Dhom G, Brenner H. Patient delay and stage of diagnosis among breast cancer patients in Germany—a population based study. Br J Cancer. 2002;86:1034–40. doi: 10.1038/sj.bjc.6600209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martin S, Ulrich C, Munsell M, Taylor S, Lange G, Bleyer A. Delays in cancer diagnosis in underinsured young adults and older adolescents. Oncologist. 2007;12:816–24. doi: 10.1634/theoncologist.12-7-816. [DOI] [PubMed] [Google Scholar]
- 36.Surtees PG, Wainwright NWJ, Khaw KT, Day NE. Functional health status, chronic medical conditions and disorders of mood. Br J Psychiatry. 2003;183:299–303. doi: 10.1192/bjp.183.4.299. [DOI] [PubMed] [Google Scholar]
- 37.Bajaj P, Bajaj P, Madsen H, Arendt-Nielsen L. Endometriosis is associated with central sensitization: a psychophysical controlled study. J Pain. 2003;4:372–80. doi: 10.1016/s1526-5900(03)00720-x. [DOI] [PubMed] [Google Scholar]
- 38.Berkley KJ, Rapkin AJ, Papka RE. The pains of endometriosis. Science. 2005;308(5728):1587–9. doi: 10.1126/science.1111445. [DOI] [PubMed] [Google Scholar]
- 39.Neziri AY, Haesler S, Petersen-Felix S, Müller M, Arendt-Nielsen L, Manresa JB, et al. Generalized expansion of nociceptive reflex receptive fields in chronic pain patients. Pain. 2010;151:798–805. doi: 10.1016/j.pain.2010.09.017. [DOI] [PubMed] [Google Scholar]
- 40.Ferrie JE, Kivimäki M, Head J, Shipley MJ, Vahtera J, Marmot MG. A comparison of self-reported sickness absence with absences recorded in employers’ registers: evidence from the Whitehall II study. Occup Environ Med. 2005;62:74–9. doi: 10.1136/oem.2004.013896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.D’Hooghe TM, Debrock S, Hill JA, Meuleman C. Endometriosis and subfertility: is the relationship resolved? Semin Reprod Med. 2003;21:243–54. doi: 10.1055/s-2003-41330. [DOI] [PubMed] [Google Scholar]
- 42.Rawson JM. Prevalence of endometriosis in asymptomatic women. J Reprod Med. 1991;36:513–5. [PubMed] [Google Scholar]
- 43.Gylfason JT, Kristjansson KA, Sverrisdottir G, Jonsdottir K, Rafnsson V, Geirsson RT. Pelvic endometriosis diagnosed in an entire nation over 20 years. Am J Epidemiol. 2010;172:237–43. doi: 10.1093/aje/kwq143. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SUPPLEMENTAL FIGURE 1 Participating centers and numbers of women recruited in the Global Study of Women’s Health (n = 1,418).
SUPPLEMENTAL FIGURE 2 Proportions of diagnostic endometriosis incidence and stage by center of recruitment. Others comprises Buenos Aires, Washington, DC, San Francisco, and Palo Alto.
SUPPLEMENTAL FIGURE 3 Health-related quality of life in women with endometriosis (n = 745), symptomatic control women (n = 587), and laparoscopic sterilization control women (n = 86): SF36v2 component summary scores with adjusted P values and 95% confidence intervals. A lower score means lower health-related quality of life. P values are presented as (P=x; P=y), x being the P value for comparison of endometriosis and laparoscopic sterilization control subjects and y being the P value for comparison of endometriosis and symptomatic control subjects. Dashed line represents mean component summary score (50) for normative population. All P values are adjusted for site, education, marital status, employment status, pelvic pain severity, type and number of presenting symptoms, and comorbidity.
SUPPLEMENTAL FIGURE 4 Absenteeism, presenteeism, and overall work productivity loss by endometriosis severity (Revised American Fertility Society classification [rAFS]). Adjusted P values for the association between each work productivity dimension and rAFS disease stage (trend test) are given. Variables adjusted for included educational attainment, marital status, type and number of symptoms, severity of pelvic pain, and comorbidity.
SUPPLEMENTAL FIGURE 5 Monetary loss from endometriosis-associated work absenteeism and presenteeism.
SUPPLEMENTAL TABLE 1 Factors (symptom patterns) and loading symptom variables.
SUPPLEMENTAL TABLE 2 Care-seeking for symptoms, mean (SD).