Abstract
Objective
There is debate concerning the mechanism of Eustachian tube (ET) ventilation. While a mechanism of complete opening has been advocated previously, sequential contraction of the levator veli palatini and medial pterygoid muscles followed by the tensor veli palatini and lateral pterygoid muscles may produce a transient sequential opening mechanism, allowing an air bolus to traverse the ET. This may explain confusion surrounding sonotubometry reports that not every swallow leads to sound passage in normal subjects. We hypothesize that the ET may not need to open completely when ventilating the middle ear; rather, a discrete air bolus can pass through it.
Subjects and Methods
Five normal and five disordered subjects underwent low-radiation dose cine computed tomography (CT) scans of the ET. Sixteen contiguous 2.5 mm slice locations were chosen through a 4 cm area in the nasopharynx that were parallel to and encompassed the entire ET. Twelve images were acquired at each slice over 4.8 seconds during swallowing and other tasks. Serial images were analyzed.
Results
An air bolus was observed passing through the ET in the normal subjects, but not the subject with ET dysfunction. Medial and lateral pterygoid contractions were also observed.
Conclusion
A new hypothetical mechanism of transient sequential ET ventilation is presented. This is not a definitive conclusion, as the number of scans taken and maneuvers used was limited. Improved understanding of ET ventilation may facilitate management of middle ear disease as treatment evolves from ventilatory tube placement to ET manipulation.
Keywords: Eustachian tube ventilation, Eustachian tube dysfunction, patulous Eustachian tube
INTRODUCTION
The Eustachian tube (ET) plays an important role in protection, clearance, and middle ear ventilation. It consists of an osseous posterolateral portion and a fibrocartilaginous anteromedial portion1,2. Opening of the tube during swallowing, yawning, or with mandibular movement allows for ventilation of the middle ear and equilibration of pressure changes between the middle ear and environmental atmosphere.
ET dysfunction, the inability to equalize middle ear and atmospheric pressure, is an important factor in the pathogenesis of middle ear disease3,4. While a specific cause of ET dysfunction is not known, potential etiologies include alteration of mucociliary function5, allergy, laryngopharyngeal reflux, cleft palate, adenoidal hyperplasia, increased compliance or floppy ET6, and primary mucosal inflammatory disease7. If left untreated, ET dysfunction can lead to a lack of middle ear aeration which can cause cholesteatoma, chronic otitis media, hearing loss with language delay in children, chronic tympanic membrane perforations, and tympanic cavity atelectasis8. Patulous ET is characterized by aural fullness, autophony, and hearing one’s own breathing9–11.
Conventional surgical methods of treating middle ear disorders caused by ET dysfunction have utilized a transtympanic approach and insertion of a myringotomy tube. Recently, transnasal endoscopic interventions that address the underlying issue of ET dysfunction have been introduced with promising preliminary results. Laser Eustachian tuboplasty12 and microdebrider tuboplasty7 have both been shown to improve otitis media with effusion. Insertion of an implant to treat a patulous ET has also been performed with promising results13. It is important to reconsider and more precisely define the mechanism of ET opening as these new procedures are popularized in order to maximize treatment benefits.
The specific role of muscles involved in ET ventilation remains controversial14. The contributions of the levator veli palatini muscle (LVPM) and medial pterygoid muscle to ET opening have not been completely defined. The LVPM runs inferior to the ET for its entire cartilaginous portion and forms a sling with fixed insertions at the petrous apex of the temporal bone and at the midline of the soft palate15,16. Finkelstein et al. concluded that the LVPM functions only in closure of the velopharynx, not opening of the ET, since patients with isolated pathology of the LVPM did not exhibit abnormal middle ear pressure. The tensor veli palatini muscle (TVPM) was deemed the sole tubal dilator17. Though the LVPM may not be responsible for ET opening, it may contribute to the shape of the ET lumen18. Sudo et al. proposed that the TVPM may open the posterior cartilaginous portion while the LVPM opens the pharyngeal side of the ET16. This was supported by evidence from Honjo et al., who found that electrically stimulating the LVPM opened the pharyngeal orifice of the ET19. Stimulation did not, however, produce middle ear ventilation. A possible role of the medial pterygoid has been supported by some authors14,20 and disputed by others21,22. Contributions of the TVPM, LVPM, and medial pterygoid may be needed for complete function of the ET, with sequential contraction contributing to a segmental passage of air from the nasopharynx to the middle ear.
Results obtained from ET function testing may also point toward other alternative mechanisms of ET ventilation. Holmquist et al. found adequate aeration but no sound passage during swallowing in 34% of normal subjects undergoing sonotubometry23. This could not be explained by medical history, otoscopy, or tympanometry. Okubo et al. reported that ET opening occurred in only 65% of children during swallowing, concluding that the ET does not necessarily open during swallowing and also that opening depends on the type of swallowing24. While a mechanism of complete opening along the length of the ET may not explain such anomalous findings, alternative mechanisms may provide additional insight. To further investigate the mechanism of ET opening, we performed low-radiation dose sequential (cine) CT scans of the ET during swallowing and additional tasks which trigger ET opening.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board of the University of Wisconsin-Madison and conducted in accordance with the ethical standards set forth by the Declaration of Helsinki. Eight male and two female subjects were recruited to participate. Five subjects had normal ET function, three had ET dysfunction, and two had patulous Eustachian tubes (table 1). One of the normal subjects and one of the subjects with patulous Eustachian tubes could perform auto-ventilation with volitional jaw movement. Subjects in the normal group were without ear disease and provided verbal confirmation that they had no history of Eustachian tube disorders (either ET dysfunction or patulous ET). To confirm normal ET function, tympanometry was performed prior to study participation with the requirement that a type A tympanogram be obtained. Subjects in the ET dysfunction group were under the clinical care of one author (MHM) and had documented difficulty ventilating the middle ear. Some subjects previously underwent myringotomy tube placement to treat the sequelae of ET dysfunction, but all were free of tubes at the time of participation. Subjects in the patulous ET group were under the clinical care of one author (MHM) and had documented symptoms of patulous ET, including aural fullness and autophony. Subjects with patulous ET also had supporting evidence on tympanometry, including a baseline positive pressure and/or a positive sniff test, which evaluates the ability of the ET to protect the middle ear from high pressures in the nasopharynx.25
Table 1.
Subject clinical characteristics.
| Number | Age | Sex | Clinical characteristics |
|---|---|---|---|
| 1 | 23 | M | Normal |
| 2 | 60 | M | Normal |
| 3 | 62 | M | Normal |
| 4 | 21 | M | Normal |
| 5 | 43 | M | Normal |
| 6 | 69 | M |
|
| 7 | 35 | M |
|
| 8 | 39 | F |
|
| 9 | 42 | F |
|
| 10 | 58 | M |
|
Subjects were placed in a supine position on a CT scanning table. Using scout images, the neck was extended so that the ET was perpendicular to the axis of the table such that cine images were acquired parallel to the ET (figure 1). When positioning the subject’s head, we looked for the angle from the floor of the external auditory canal to the pterygoid hamulus. Subjects were instructed to swallow repeatedly while scans were taken. In nine subjects, 16 contiguous 2.5 mm CT slice locations were chosen through a 4 cm area in the nasopharynx that were parallel to and encompassed the entire ET. Twelve cine images were acquired at each slice location over 4.8 seconds (0.4 second images) during swallowing and other tasks designed to elicit ET opening. Serial images were analyzed to determine how air traversed the ET during these actions. Sixty-four 0.625 mm scans over a 4.0 cm area were obtained in one subject. Additional tasks included Valsalva maneuver and volitional jaw movement. A scan field-of-view of 16 cm was used along with a matrix of 512 × 512. This produced a spatial resolution of 0.3 mm.
Figure 1.
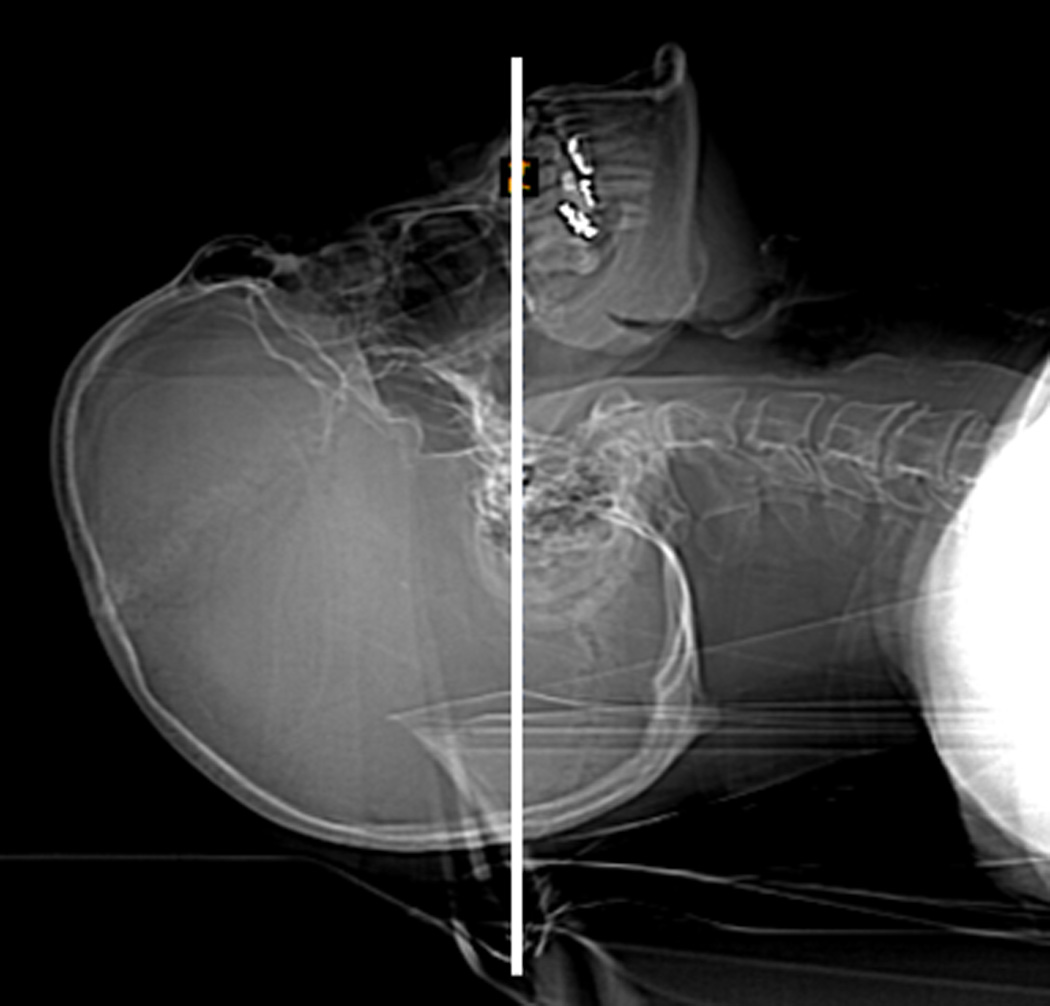
Subject extending his neck so that the Eustachian tube (ET) is perpendicular to the table. Correct positioning was verified using scout images.
RESULTS
Sequential movement of an air bolus could be seen in the images obtained for all subjects. Passage of an air bolus was clearly observed in normal subjects (figure 2; online resources 1, 2). The degree of opening appeared to be enhanced by contraction of the medial and lateral pterygoid muscles (online resource 1). Volitional jaw movement by one normal subject resulted in tensing of the medial and lateral pterygoid muscles, slight condylar movement, and dilation of the ET (figure 3; online resource 3). Swallowing under Valsalva pressure also produced changes in the degree of ET opening, enhancing opening at the pharyngeal orifice.
Figure 2.
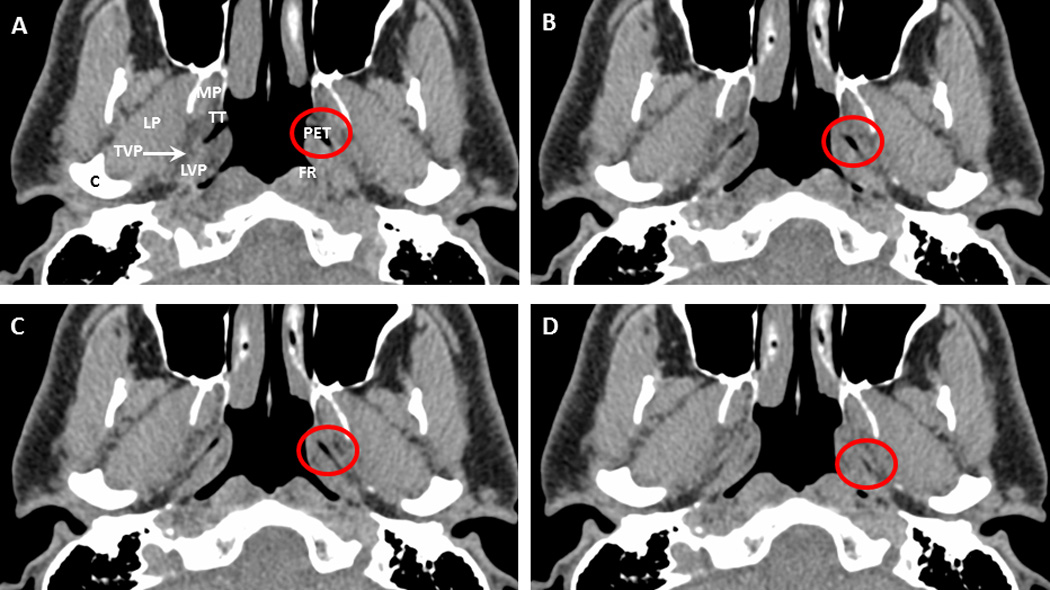
Eustachian tube opening in a normal subject (subject 5). A discrete air bolus (red circle) can be seen. Note that structures occur bilaterally but are labeled unilaterally for clarity. PET = pharyngeal Eustachian tube; MP = medial pterygoid muscle; LP = lateral pterygoid muscle; LVP = levator veli palatini muscle; TVP = tensor veli palatini muscle; TT = torus tubarius; FR = fossa of Rosenmuller; C = condyle.
Figure 3.
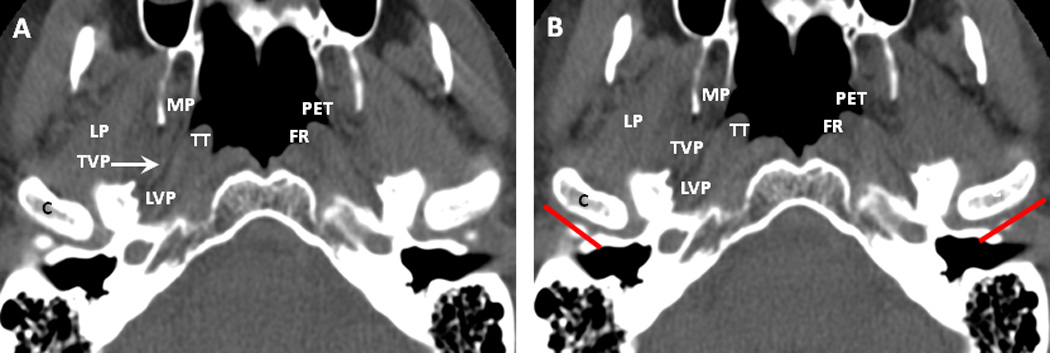
Volitional jaw movement in a normal subject (subject 2), producing condylar movement (C; red lines in figure 3B reflect position of posterior edge of condyle in 3A). Note that structures occur bilaterally but are labeled unilaterally for clarity. PET = pharyngeal Eustachian tube; MP = medial pterygoid muscle; LP = lateral pterygoid muscle; LVP = levator veli palatini muscle; TVP = tensor veli palatini muscle; TT = torus tubarius; FR = fossa of Rosenmuller; C = condyle.
Images obtained from subjects with ET dysfunction displayed several aberrant characteristics (figure 4; online resources 4, 5). First, the size of the air bolus passing through the ET was either discernibly smaller or completely absent. Second, there was little, if any, observable medial pterygoid movement. Opening at the pharyngeal orifice appeared normal. In the subjects with patulous ET, the size of the air bolus appeared larger compared to normal subjects (figure 4; online resource 6).
Figure 4.
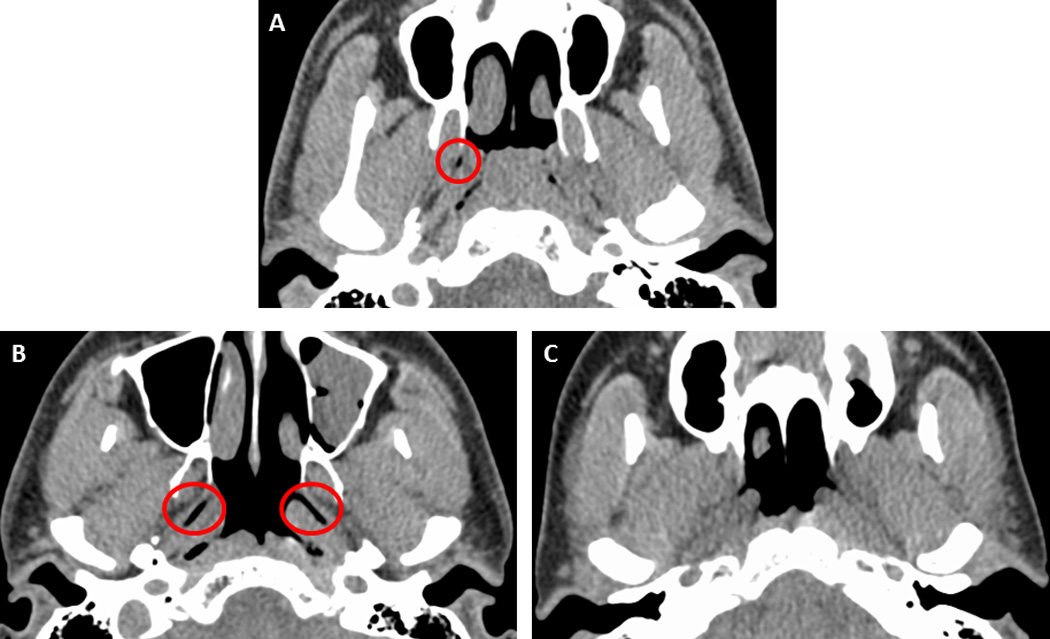
Comparison of air bolus in normal subject (subject 4) (A), subject with patulous Eustachian tubes (subject 7) (B), and subject with Eustachian tube dysfunction (subject 9) (C). Relative to the normal subject, the air bolus is visibly larger in the subject with patulous Eustachian tubes and absent in the subject with Eustachian tube dysfunction.
DISCUSSION
A new mechanism of ET opening is proposed that is supported both by the images obtained in this study as well as previous experiments on ET physiology. An air bolus was visible in all normal subjects as well as the two subjects with patulous ET, but not visible in the three subjects with ET dysfunction. The size of the bolus varied across subjects, but tended to be larger in the two subjects with patulous ET. Due to the relatively low sampling rate used in this study, it is possible that the maximal air bolus volume was not visualized. Sequential peristaltic-like movement of a discrete air bolus through the ET, accompanied by contraction of the TVPM, LVPM, and medial and lateral pterygoid muscles, may explain these findings. This is the first study applying cine CT imaging to visualize the ET. The resolution offered by the scanner combined with the ability to take rapid sequential scans makes this a potentially valuable tool for studying ET physiology. Applying this technique on a larger scale to more subjects and additional disorders could be beneficial.
There are several limitations of this study and these limitations will be the focus of future investigations. There was some difficulty positioning the head. This difficulty could be ameliorated either by placing subjects in an upright sitting position, as in Kikuchi et al.26, or creating a frame which puts the subject’s head at the correct angle for optimal visualization of the ET. While the stages of opening could be observed in our images, they could not be observed during the sequence of a single opening. Increasing the sampling rate of the cine CT may provide additional insight into the mechanism of ET ventilation. We examined subjects in a supine position, but future studies with improvement in CT technology could potentially examine subjects in either an elevated, upright, or prone position. Ingelstedt et al. found that the mean volume of air passing through the ET was reduced by one third when the body was elevated twenty degrees to the horizontal and by two thirds when the body was in the supine position27. Taking cine images of subjects in an upright position may offer a more representative picture of ET function.
A sequential peristaltic-like mechanism potentially resolves several questions arising from ET function testing. The nine-step inflation-deflation test uses a tympanometer to measure the ability of the ET to normalize overpressure, with three swallows typically being required to normalize a relative negative pressure of 300 mmH2O2,28–31. If the ET opened completely along its length, one swallow would likely be sufficient for pressure equalization. Similarly, anomalous poor sound passage on sonotubometry in patients with no history of ear disease and presumably normal ET function2 could be explained by the peristaltic-like mechanism. The ET opening mechanism of those patients exhibiting poor sound passage may be sufficiently slow to dampen the inputted sound. Increasing CT sampling rate, as mentioned previously, may allow for examination of ET opening duration and the effects of slow opening on sonotubometry.
Leuwer et al. used functional 3-D reconstructions to evaluate the effect of the medial pterygoid muscle on ET opening, finding that contraction of it increased the force of the TVPM on the tympanic ET20. The upper portion of the medial pterygoid provides support to the anterior Eustachian tube20–22. Those findings were supported by results from three subjects in this study, including one who used volitional pterygoid movement to open his ET in the absence of swallowing (figure 3). Though a patulous ET resulting from cachectic weight loss has previously been attributed to decreased size of Ostmann’s fat pad, wasting of the muscles which control the ET, including the medial pterygoids, may be the underlying or a contributing cause. The ability to enhance ET opening could be utilized clinically as a conservative approach to address mild ET dysfunction. Training patients how to contract the medial pterygoid could promote ET opening and pressure equalization, potentially preventing the severe complications associated with chronic ET dysfunction. This technique could also be used in patients with dysphagia, for whom swallowing may not result in reliable ET opening. Such a maneuver would likely be of greater benefit to patients with musculoskeletal ET dysfunction than with mucociliary ET dysfunction. Future studies combining electromyography, sonotubometry, and visual assessment of the ET via CT or transnasal endoscopy may further elucidate the effect of medial pterygoid contraction on ET opening and the degree to which it can alleviate ET dysfunction.
In addition to medial pterygoid movement, lateral pterygoid movement was also observed. This occurred not only in the subject performing volitional jaw movement, but also another subject performing normal swallows. While lateral pterygoid contraction would be necessary for a subject to protract the mandible, such movement is not intuitively necessary for swallowing. The lateral pterygoid appears to border and enhance dilation of the tympanic ET, though it is not as closely associated with the ET as the medial pterygoid. To our knowledge, a potential role of the lateral pterygoid in ET ventilation has not been discussed; however, the CT images taken at the level of the ET in this study appear to provide support for such a role. Contraction of the medial and lateral pterygoids may alter the convexity of the anterolateral ET, thus allowing TVPM contraction to have a greater effect. It is important to note that contraction of the pterygoid muscles appears to be neither necessary nor sufficient for ET ventilation; however, it may have an amplificatory role.
Refined knowledge of the ET opening mechanism may lead to a better understanding of ET dysfunction and the development of more directed surgical treatments. In the patients with ET dysfunction, an air bolus was not readily observable (figure 4; online resources 4, 5). There may be a volume at which ET opening can no longer equalize pressure. Determining this volume using cine CT imaging and tympanometry may be helpful when performing ET tuboplasty to allow for minimal damage while still ensuring good outcome. Developing an objective, quantitative method of analyzing these images will be the subject of future studies. At this time, the small size of the air bolus precludes accurate measurement using our standard CT imaging software. Improving measurement accuracy and measuring bolus volume using three-dimensional CT reconstructions could be of clinical and scientific interest. We created a reconstruction from one subject with patulous ET and could see the air bolus in two dimensions (figure 5). Improving temporal resolution to see how this reconstruction changes through time would add further support for the proposed mechanism of ventilation. Decreased pterygoid movement was also observed in the subject with ET dysfunction. While this is likely not the primary underlying cause, it is possible that volitional pterygoid movement may enhance ET dilation and improve middle ear aeration.
Figure 5.
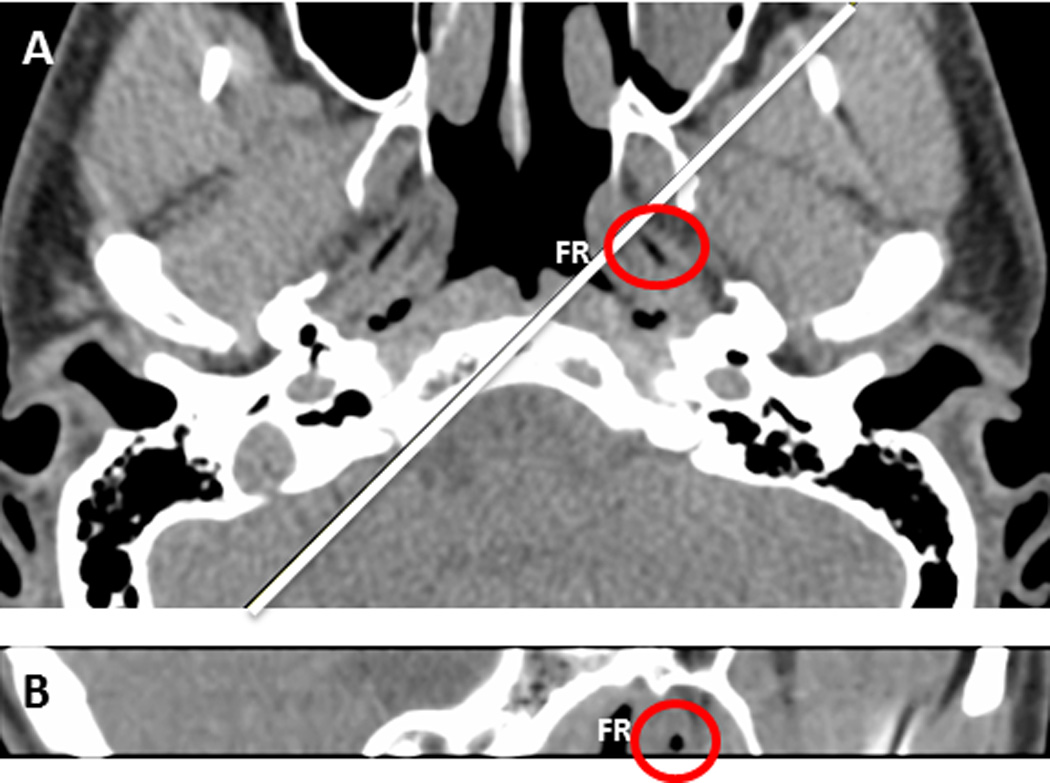
Computed tomography reconstruction in subject with patulous Eustachian tubes (subject 7). The red circle surrounds the air bolus present in the Eustachian tube. The Fossa of Rosenmuller (FR) can also be seen in both planes. The white line in 5A represents the plane shown in 5B.
Opening at the pharyngeal orifice in two of the three subjects with ET dysfunction was not different from that of the normal subjects; dysfunction was only apparent in the tympanic two-thirds of the ET. Poe has reported success in resolving ET dysfunction after ablating the pharyngeal orifice of the ET. As the pharyngeal orifice in the subject in this study appeared normal, it is unclear what benefit pharyngeal ablation would have on his ET dysfunction. Therefore, there may be two types of ET dysfunction: pharyngeal and tympanic. Patients with tympanic ET dysfunction may account for the cases in Poe’s study12 which were not resolved by the laser tuboplasty. These patients may not have difficulty capturing the air bolus in the pharyngeal ET, but the bolus cannot reach the tympanic ET and middle ear. Such patients may benefit from tympanic ET dilation. Compromised medial pterygoid function may be indicative of tympanic ET dysfunction, as the medial pterygoid normally enhances the action of the TVPM20, which acts more posterolaterally than the LVPM. Patients with pharyngeal ET dysfunction may have difficulty capturing the air bolus. Surgical dilation of the pharyngeal orifice may facilitate capturing the air bolus, which can then traverse the ET and reach the middle ear. It would be beneficial to take cine CT images before and after tuboplasty to determine if the procedure facilitated air bolus capture and travel through the ET.
Supplementary Material
Online resource 1. Video demonstrating normal Eustachian tube (ET) ventilation. The red box surrounds the length of the ET. mpeg
Online resource 2. Video demonstrating normal Eustachian tube (ET) ventilation. The red box surrounds the length of the ET. mpeg
Online resource 3. Video demonstrating Eustachian tube (ET) ventilation via volitional jaw movement. The red box surrounds the length of the ET. mpeg
Online resource 4. Video demonstrating inadequate ventilation in a subject with Eustachian tube (ET) dysfunction. The red box surrounds the length of the ET. mpeg
Online resource 5. Video demonstrating inadequate ventilation in a subject with Eustachian tube (ET) dysfunction. The red box surrounds the length of the ET. mpeg
Online resource 6. Video demonstrating large air bolus in subject with patulous Eustachian tubes. The red box surrounds the length of the ET. mpeg
Acknowledgements
This study was funded in part by NIH grant number R01 DC008153 from the National Institute on Deafness and other Communicative Disorders.
Footnotes
Competing interests statement: The authors have no conflicts of interests to declare.
REFERENCES
- 1.Poe DKO. Endoscopic diagnoses of Eustachian tube dysfunction. In: Silverstein R, Poe, editors. Minimally Invasive Surgery of the Ear. 2002. [Google Scholar]
- 2.van der Avoort SJ, van Heerbeek N, Zielhuis GA, et al. Sonotubometry: eustachian tube ventilatory function test: a state-of-the-art review. Otol Neurotol. 2005;26:538–543. doi: 10.1097/01.mao.0000169765.00798.cd. discussion 43. [DOI] [PubMed] [Google Scholar]
- 3.Maroldi R, Farina D, Palvarini L, et al. Computed tomography and magnetic resonance imaging of pathologic conditions of the middle ear. Eur J Radiol. 2001;40:78–93. doi: 10.1016/s0720-048x(01)00376-x. [DOI] [PubMed] [Google Scholar]
- 4.Su CY. Valve section of the eustachian tube. J Laryngol Otol. 1995;109:486–490. doi: 10.1017/s0022215100130531. [DOI] [PubMed] [Google Scholar]
- 5.Bernstein JM. Immunologic aspects of otitis media. Curr Allergy Asthma Rep. 2002;2:309–315. doi: 10.1007/s11882-002-0056-4. [DOI] [PubMed] [Google Scholar]
- 6.Bluestone CD. Impact of evolution on the eustachian tube. Laryngoscope. 2008;118:522–527. doi: 10.1097/MLG.0b013e31815ddaa0. [DOI] [PubMed] [Google Scholar]
- 7.Metson R, Pletcher SD, Poe DS. Microdebrider eustachian tuboplasty: A preliminary report. Otolaryngol Head Neck Surg. 2007;136:422–427. doi: 10.1016/j.otohns.2006.10.031. [DOI] [PubMed] [Google Scholar]
- 8.Linstrom CJ, Silverman CA, Rosen A, et al. Eustachian tube endoscopy in patients with chronic ear disease. Laryngoscope. 2000;110:1884–1889. doi: 10.1097/00005537-200011000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Doherty JK, Slattery WH., 3rd Autologous fat grafting for the refractory patulous eustachian tube. Otolaryngol Head Neck Surg. 2003;128:88–91. doi: 10.1067/mhn.2003.34. [DOI] [PubMed] [Google Scholar]
- 10.O'Connor AF, Shea JJ. Autophony and the patulous eustachian tube. Laryngoscope. 1981;91:1427–1435. doi: 10.1288/00005537-198109000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Ogawa S, Satoh I, Tanaka H. Patulous Eustachian tube. A new treatment with infusion of absorbable gelatin sponge solution. Arch Otolaryngol. 1976;102:276–280. doi: 10.1001/archotol.1976.00780100062006. [DOI] [PubMed] [Google Scholar]
- 12.Poe DS, Metson RB, Kujawski O. Laser eustachian tuboplasty: a preliminary report. Laryngoscope. 2003;113:583–591. doi: 10.1097/00005537-200304000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Poe DS. Diagnosis and management of the patulous eustachian tube. Otol Neurotol. 2007;28:668–677. doi: 10.1097/mao.0b013e31804d4998. [DOI] [PubMed] [Google Scholar]
- 14.Hecht CS, Gannon PJ, Eden AR. Motor innervation of the eustachian tube muscles in the guinea pig. Laryngoscope. 1993;103:1218–1226. doi: 10.1288/00005537-199311000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Graves GE, LF The eustachian tube: review of its descriptive, microscopic, topographic, and clinical anatomy. Arch Otolaryngol. 1944;39:359–397. [Google Scholar]
- 16.Sudo M, Sando I, Suzuki C. Three-dimensional reconstruction and measurement study of human eustachian tube structures: a hypothesis of eustachian tube function. Ann Otol Rhinol Laryngol. 1998;107:547–554. doi: 10.1177/000348949810700701. [DOI] [PubMed] [Google Scholar]
- 17.Finkelstein Y, Talmi YP, Nachmani A, et al. Levator veli palatini muscle and eustachian tube function. Plast Reconstr Surg. 1990;85:684–692. discussion 93-7. [PubMed] [Google Scholar]
- 18.Honjo I. Pharyngeal orifice of eustachian tube in cleft palate. Tokyo, Japan: Springer-Verlag; 1988. [Google Scholar]
- 19.Honjo I, Okazaki N, Kumazawa T. Opening mechanism of the eustachian tube. A clinical and experimental study. Ann Otol Rhinol Laryngol Suppl. 1980;89:25–27. doi: 10.1177/00034894800890s309. [DOI] [PubMed] [Google Scholar]
- 20.Leuwer R, Schubert R, Kucinski T, et al. The muscular compliance of the auditory tube: a model-based survey. Laryngoscope. 2002;112:1791–1795. doi: 10.1097/00005537-200210000-00016. [DOI] [PubMed] [Google Scholar]
- 21.Doyle WR, SR Comparison of the anatomy of the eustachian tube in the rhesus monkey (Macaca mulatta) and man, implications for physiologic modeling. Ann Otol Rhinol Laryngol. 1980;89:49–57. doi: 10.1177/000348948008900112. [DOI] [PubMed] [Google Scholar]
- 22.Cantekin EI, Doyle WJ, Reichert TJ, et al. Dilation of the eustachian tube by electrical stimulation of the mandibular nerve. Ann Otol Rhinol Laryngol. 1979;88:40–51. doi: 10.1177/000348947908800108. [DOI] [PubMed] [Google Scholar]
- 23.Holmquist JBG, Olen L. Measurement of eustachian tube function using sonotubometry. Scand Audiol. 1981;10:33–35. doi: 10.3109/01050398109076159. [DOI] [PubMed] [Google Scholar]
- 24.Okubo J, Watanabe I. Aeration of the tympanomastoid cavity and the Eustachian tube. Acta Otolaryngol Suppl. 1990;471:13–24. doi: 10.3109/00016489009124804. [DOI] [PubMed] [Google Scholar]
- 25.Falk B. Sniff-induced negative middle ear pressure: study of a consecutive series of children with otitis media with effusion. Am J Otolaryngol. 1982;3:155–162. doi: 10.1016/s0196-0709(82)80048-3. [DOI] [PubMed] [Google Scholar]
- 26.Kikuchi T, Oshima T, Ogura M, et al. Three-dimensional computed tomography imaging in the sitting position for the diagnosis of patulous eustachian tube. Otol Neurotol. 2007;28:199–203. doi: 10.1097/01.mao.0000253280.10501.72. [DOI] [PubMed] [Google Scholar]
- 27.Ingelstedt S, Ivarsson, Jonson B. Mechanics of the human middle ear. Pressure regulation in aviation and diving. A non-traumatic method. Acta Otolaryngol. 1967;228(Suppl):1–58. [PubMed] [Google Scholar]
- 28.van Heerbeek N, Ingels KJ, Snik AF, et al. Reliability of manometric eustachian tube function tests in children. Otol Neurotol. 2001;22:183–187. doi: 10.1097/00129492-200103000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Bylander A, Tjernstrom O, Ivarsson A. Pressure opening and closing functions of the Eustachian tube by inflation and deflation in children and adults with normal ears. Acta Otolaryngol. 1983;96:255–268. doi: 10.3109/00016488309132898. [DOI] [PubMed] [Google Scholar]
- 30.Falk B, Magnuson B. Test-retest variability of eustachian tube responses in children with persistent middle ear effusion. Arch Otorhinolaryngol. 1984;240:145–152. doi: 10.1007/BF00453472. [DOI] [PubMed] [Google Scholar]
- 31.Groth P, Ivarsson A, Tjernstrom O. Reliability in tests of the eustachian tube function. Acta Otolaryngol. 1982;93:261–267. doi: 10.3109/00016488209130881. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online resource 1. Video demonstrating normal Eustachian tube (ET) ventilation. The red box surrounds the length of the ET. mpeg
Online resource 2. Video demonstrating normal Eustachian tube (ET) ventilation. The red box surrounds the length of the ET. mpeg
Online resource 3. Video demonstrating Eustachian tube (ET) ventilation via volitional jaw movement. The red box surrounds the length of the ET. mpeg
Online resource 4. Video demonstrating inadequate ventilation in a subject with Eustachian tube (ET) dysfunction. The red box surrounds the length of the ET. mpeg
Online resource 5. Video demonstrating inadequate ventilation in a subject with Eustachian tube (ET) dysfunction. The red box surrounds the length of the ET. mpeg
Online resource 6. Video demonstrating large air bolus in subject with patulous Eustachian tubes. The red box surrounds the length of the ET. mpeg


