Abstract
Chronic rhinosinusitis (CRS) is an inflammation of the nose and paranasal sinuses lasting for ≥12 weeks. Endoscopic sinus surgery (ESS) is considered during difficult to treat CRS. The minimally invasive technique focuses on the transition areas rather than on the ostia. The aim of this study was to evaluate symptoms, the number of acute sinusitis episodes, and satisfaction after ESS with either preservation or enlargement of the maxillary sinus ostium. Thirty patients with moderate nonpolypous CRS were enrolled. Uncinectomy only and additional middle meatal antrostomy were randomized for each side of each patient and performed single blindly. The symptoms questionnaires were filled at four time intervals. Significant symptom reduction was achieved independently of operation technique. The number of acute sinusitis episodes indicating the exacerbation rate decreased significantly at 9 and, on average, 68 months postoperatively. However, the exacerbation rate began to increase after 9 months postoperatively. Three revisions were performed on the side with uncinectomy only and one on the side with additional antrostomy. Most patients reported good satisfaction with both procedures. There was a trend for patients with asthma and/or job exposure to report insignificantly more frequently no satisfaction with surgery, especially with the uncinectomy-only procedure. Both procedures seem to be efficient in providing symptom relief and satisfaction. More studies are needed to evaluate if patients with risk factors benefit more from an ostium-enlarging procedure.
Keywords: Antrostomy, chronic sinusitis, endoscopic sinus surgery, ethmoidectomy, maxillary sinus, minimally invasive technique, mucosa, outcomes, quality of life, symptoms
Chronic rhinosinusitis (CRS) is a versatile, multifactorial disease of the nose and paranasal sinuses with a prevalence of ∼10%.1,2 Several diseases coexist with CRS by partly unknown mechanisms: asthma, aspirin sensitivity, atopy, chronic rhinitis, depression, anxiety, and fatigue.3 It is known that biological and chemical agents associate with work-related asthma, and occupational exposure causes 10–20% of adult-onset asthma.4–6 However, only few studies address the influence of occupational exposure on CRS.7–9 Primary management of CRS is conservative. It is composed of nasal saline irrigations and corticosteroids. Depending on the comorbidities and hyperinflammatory or infective exacerbations, additional treatment might be used. Quality of life (QoL) questionnaires are not able to estimate exacerbations, e.g., to what extent CRS is under control.10 Even so, only few studies have observed the influence of CRS management on the exacerbation rate.
Endoscopic sinus surgery (ESS) is considered during recalcitrant and difficult-to-treat CRS.2 It is based on the theory that obstruction of the ostium leads to chronic inflammation and eventually to pathological alterations of the maxillary sinus mucosa. Others have shown that ostiomeatal complex obstruction does not correlate with adjacent sinus status in CRS with nasal polyps.11 Nevertheless, it seems that surgical opening of the ostium improves drainage and ventilation of the sinus and thus might restore the normal mucosa during CRS without nasal polyps.11–13 Ragab et al. were not able to prove ESS to be superior to conservative therapy in controlled studies.14 Uncontrolled studies have shown QoL improvement after ESS, also in CRS patients with high age, acetylsalicylic acid intolerance, depression, fibromyalgia, and chronic fatigue syndrome.3,15–19 However, ESS seems to, at least partially, provide symptom relief and/or decrease inflammatory findings.20–24
Despite the fact that the ostium is considered to be the most important area in the pathogenesis of CRS, few studies have addressed the extent of sinus surgery on the ostiomeatal area. Other studies have previously indicated that removal of the uncinate process alone might be enough to restore the ventilation of the maxillary sinus.25–28 There is also evidence that the effect of minimally invasive ESS is comparable with invasive ESS.26,28–33 On the other hand, uncontrolled studies suggest that the presence of biofilms, osteomyelitis, and other factors favor invasive approaches toward the osteomeatal unit.34–39 Our aim was to evaluate symptoms, exacerbation rate, and satisfaction after ESS with either the ostium-preserving or the ostium-enlarging technique.
MATERIALS AND METHODS
Subjects
This study was performed at the Department of Otorhinolaryngology, Tampere University Hospital, Finland, and Mikkeli Central Hospital, Mikkeli, Finland. The study was approved by the Institutional Review Boards of the Tampere University Hospital and Mikkeli Central Hospital. J.P. Myller and A.T. Luukkainen contributed equally to this work. Informed consent was obtained from all patients. Thirty patients with CRS were enrolled in this study. Characteristics of groups of patients can be seen in Table 1 and in a previous publication.40 Inclusion criteria were moderate to severe sinus-related symptoms, according to patient interview, during at least 12 weeks, despite maximal medical treatment and a Lund-McKay sinus computed tomography score41 of at least 6/24 but no more than 18/24. Exclusion criteria were age <18 years; oral corticosteroid treatment during the last 2 months before surgery; previous sinonasal surgery; a history or physical examination suggestive of severe nasal septal deviation (that causes only unilateral nasal obstruction and/or requires septoplasty before ESS can be performed), unilateral sinusitis, nasal polyposis of more than grade 142, aspirin sensitivity, chronic bronchitis, cystic fibrosis, or a tumor or a disease with a severe impact on general immunity; and mild sinus-related symptoms. Dropouts from the study included one patient who died accidentally before the last postoperative control. Three additional patients missed the last follow-up (68 months postoperatively); we were unable to contact them by telephone.
Table 1.
Characteristics of the study population
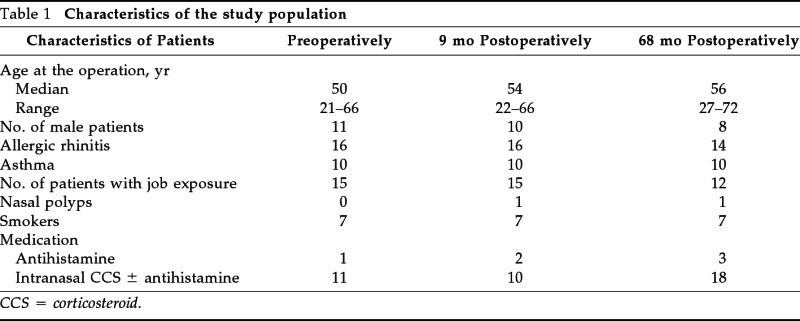
CCS = corticosteroid.
Job exposure was evaluated according to reported current occupation and characterization of workplace. The positive job exposure group was determined according to international categorization of high-risk occupations.4,6 The substances causing job exposure were bioaerosols (four patients), flour (four patients), mites (three patients), wood dust (two patients), reactive chemicals/metalwork (two patients), molds (one patient), and agricultural organic particles (one patient). The determination of the patients' other comorbidities was based on medical records, interview, and medical examination as previously described.40
Sinus Surgery
ESS was performed by two authors (Myller and Torkkeli) as previously described.40,43,44 Both procedures were standardized. Briefly, the uncinectomy was performed on both sides, in which the lower two-thirds of the uncinate process was removed. Additional middle meatal antrostomy was randomized on either the right or the left side of each patient. Randomization was performed by allotment. Two identical pieces of paper, one with the caption “sinistrum” and the other with the caption “dextrum,” were placed in an envelope. Each time a new patient was recruited, the operating surgeon pulled out a piece of paper. Additional meatal antrostomy was performed on the side of the pulled caption. If mucosa blocked the maxillary sinus ostium on the uncinectomy-only side, as little as possible was carefully removed from it, without disturbing the bony ostium. On the additional middle meatal antrostomy side, the diameter of the ostium was duplicated in the posterior direction with cutting forceps. If necessary, a large ethmoid bulla was opened on both ostium-preserving and -enlarging sides (Table 1).
Questionnaires
Patients filled the symptom questionnaire 1–77 days (mean ± SD, 26 ± 23 days) preoperatively. The same questionnaire was filled during a control visit to the operating surgeon 9 months postoperatively, and later on, based on patients' answers during telephone calls made, blindly at 56–86 months (mean ± SD, 68 ± 6.5 months) postoperatively. During the telephone call, if the patient had undergone revision surgery, he/she was asked to answer the questions according to the situation before revision surgery was performed. The following questions were asked preoperatively, and at 9 and, on average, 68 months postoperatively: the number of acute bacterial sinusitis episodes diagnosed or suspected by a doctor during the previous year and the existence of the symptoms of facial pain/pressure, nasal obstruction, nasal discharge, postnasal drip, and decreased sense of smell (no = 0, mild or moderate = 1, and severe = 2). In addition, lacrimation (none = 0, mild = 1, moderate = 2, severe = 3) and postoperative bleeding (absent = 0, mild or moderate = 1, and severe = 2) were asked during the debridement follow-up visit at 7–30 days (mean ± SD, 16 ± 5 days) postoperatively and at 9 months postoperatively. Satisfaction with the operation was scored according to two questions asked at 9 and 68 months postoperatively on each side separately: “How is the situation in the maxillary sinuses now compared with the situation before the operation” (no symptoms, clearly decreased symptoms, slightly decreased symptoms, no change, or more symptoms) and “If you could choose, would you now be willing for a similar operation?” (yes, maybe, or no, and reason why if no). The satisfaction was scored in the following way: 0 = good, patient benefited clearly from the operation; 1 = moderate, patient experienced only slight benefit from the operation and is unsure about the willingness for a similar operation if it was performed now; 2 = poor, patient experienced no change or worsening after the operation and is unwilling/unsure for a similar operation.
Statistical Analysis
Statistics were performed with SPSS Base 11.0 Statistical Software Package (SPSS, Chicago, IL). Data are expressed as medians and interquartile ranges. The nonparametric Wilcoxon test was used for comparison of matched pairs. Mann-Whitney U tests were used for comparisons of two groups. Spearman rank correlation test was used for correlations. For comparisons of dichotomous data in matched pairs, McNemar's test was used. A two-tailed value of p < 0.05 was considered significant in all tests.
RESULTS
Results were analyzed on an intent-to-treat basis and each patient was analyzed according to the randomly allocated treatment.
Symptoms during the Debridement Visit
During the debridement visit at 7–30 days (mean ± SD, 16 ± 5 days) postoperatively, the patients were asked about symptoms during immediate postoperative recovery: pain, bleeding, lacrimation, and nasal obstruction. There were no significant differences between the operation techniques in the median values of each of these four symptoms (p > 0.05; Wilcoxon test; data not shown). The median sum of these four symptoms as well as the median points of pain, obstruction, and bleeding decreased on both sides between the debridement visit and a visit at 9 months postoperatively, indicating good recovery on both sides (p < 0.001; Wilcoxon test; data not shown). Lacrimation remained at the same low level on both sides; thus, there was no a significant difference in the medians at 16 days and 9 months postoperatively (p > 0.05; Wilcoxon test; data not shown).
Long-Term Outcomes
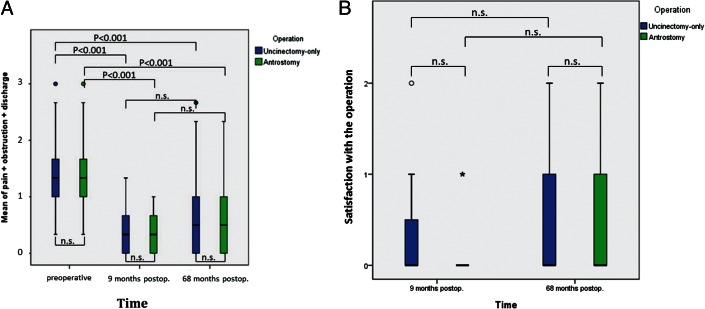
When comparing preoperative and postoperative (9 and 68 months) symptoms, facial pain, nasal obstruction, and discharge values and the mean of these three values, a significant reduction on both the ostium -preserving and the -enlarging sides was observed (p < 0.001, by Wilcoxon test; data partly shown in Fig. 1 A). There was no significant difference between the operation techniques in these values (p > 0.05, by Wilcoxon test; data partly shown in Fig. 1 A). Moreover, the delta-values indicating the change of these three symptoms before and after the operation did not differ between the operation techniques at the 9 and, on average, 68 months postoperative values (p > 0.05, by Wilcoxon test; data not shown). Symptom values for reduced sense of smell and postnasal drip could not be compared between the sides; however, they declined significantly when comparing preoperative and postoperative (9 and 68 months) values (p < 0.001, by Wilcoxon test; data not shown).
Figure 1.
Comparisons of medians indicating (A) mean value of pain + obstruction + discharge scores and (B) satisfaction (0 = yes, 1 = partly, and 2 = no) between the operation techniques and the time points. The p values by Wilcoxon test (n.s. = not significant). Horizontal lines represent medians; upper and lower vertical bars represent the 75th and 25th percentile ranges; vertical lines represent the 99th percentile range.
When observing satisfaction with the operation at 9 and, on average, 68 months postoperatively, the majority of patients expressed good/moderate satisfaction and there were no differences between operative techniques in the reported satisfaction (p > 0.05, by Wilcoxon test; Fig. 1 B).
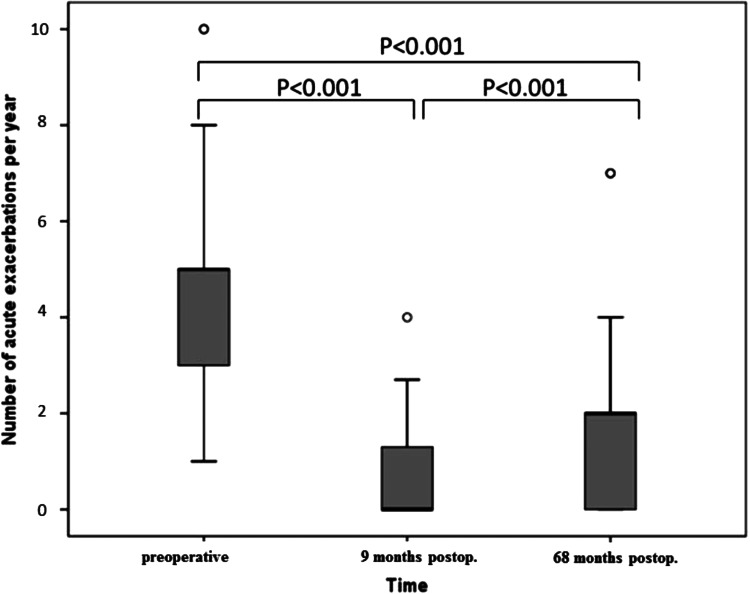
The exacerbation rate could not be compared between sides. When comparing preoperative and postoperative (9 and 68 months) exacerbation rates, e.g., the numbers of reported antibiotic courses for doctor-diagnosed sinusitis during the last year, the number decreased significantly (p < 0.001, by Wilcoxon test; Fig. 2). Interestingly, the number of acute sinusitis per year increased slightly but significantly between 9 and 68 months postoperatively (p < 0.001, by Wilcoxon test; Fig. 2).
Figure 2.
The patient-reported number of acute exacerbations, e.g., prescribed antibiotic courses for doctor-diagnosed sinusitis, per year. At 9 months postoperatively the patients reported the number of antibiotics prescribed during the postoperative follow-up time period (9 months). Thus, this value was multiplied by 12/9 = 1.33 for the analysis and the presentation in the figure. The P values by Wilcoxon test. Horizontal lines represent medians; upper and lower vertical bars represent the 75th and 25th percentile ranges; vertical lines represent the 99th percentile range.
Revision surgery was performed on one antrostomy side and three uncinectomy-only sides for 3 of 26 patients during the observation period; however, this difference between the sides remained statistically insignificant (p > 0.05, McNemar test; data not shown). The two patients (one man and one woman) that underwent revision surgery only on the uncinectomy side had complaints solely on this side before revision antrostomy was performed. Of the three patients that underwent revision surgery, all were nonsmokers and had allergic rhinitis but not asthma. The patient with bilateral revision surgery, additionally, had job exposure (for case report see Fig. 4).
Figure 4.
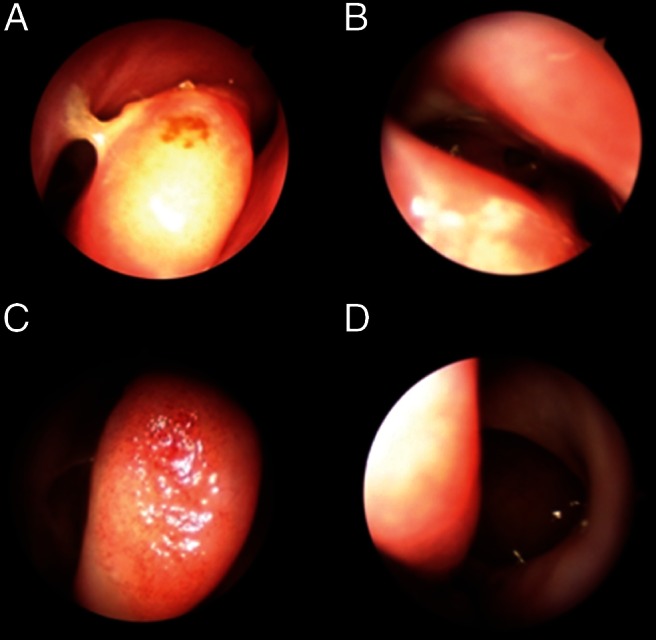
Two cases at 6 years postoperatively. The first patient was a 50-year-old nonsmoking woman with allergic rhinitis and job exposure (cold storage room worker). She had undergone (A) uncinectomy only on the right side and (B) additional middle meatal antrostomy on the left side. However, she underwent revision surgery on both sides 19 months after the primary operation because of the continuation of the symptoms and exacerbations. At 73 months postoperatively, there was a continuation of symptoms, e.g., the mean score of pain + obstruction + discharge was 2.33 on both sides. However, the number of acute exacerbations was 0 during the past 12 months, and she expressed good satisfaction with both techniques. Endoscopy at 79 months postoperatively showed that both sides were open narrowly. The second patient was a 53-year old nonsmoking woman with allergic rhinitis, asthma, and job exposure (nurse). She had undergone (C) uncinectomy only on the right side and (D) additional middle meatal antrostomy on the left side. At 69 months postoperatively, the mean score of pain + obstruction + discharge was 1 on both sides, indicating good recovery. However, she reported that the number of acute exacerbations was 4 during the past 12 months, and she expressed no satisfaction with either technique. Endoscopy at 75 months postoperatively showed that the uncinectomy side was not open and the antrostomy side was widely open.
The Influence of Patient History
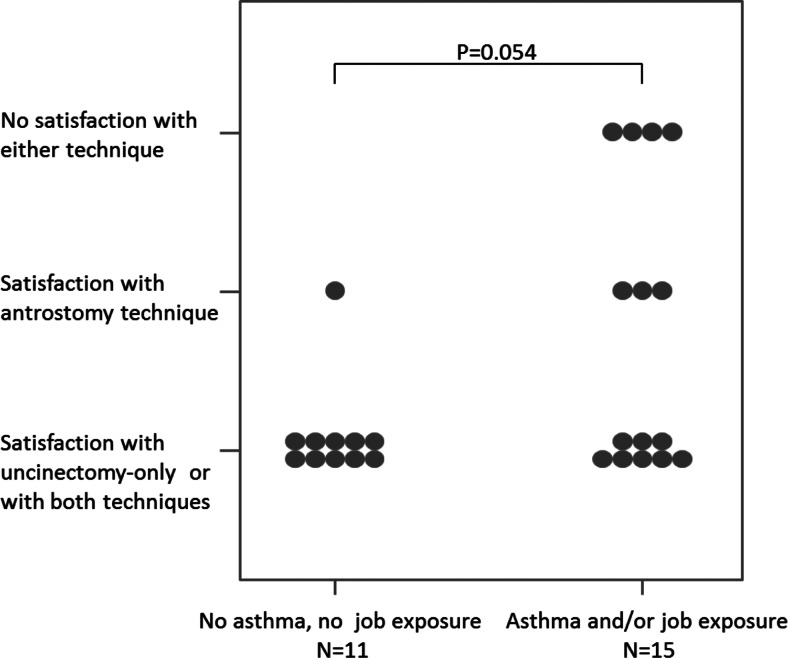
When analyzing the median values of pre- or postoperative symptoms and satisfaction for either ostium-preserving or -enlarging sides, there was no association to sex, allergic rhinitis, and/or asthma; smoking; job exposure; or intranasal corticosteroid and/or antihistamine medication (p > 0.05, Mann-Whitney U test; data not shown). Moreover, these symptom and satisfaction values did not correlate with age or the number of acute sinusitis/year (p > 0.05, Spearman rank correlation test; data not shown). Interestingly, there was a trend that patients with asthma and/or job exposure expressed more frequently satisfaction only on the side with antrostomy or neither technique provided them satisfaction (p = 0.054, Mann-Whitney U test; Fig. 3). The unsatisfied patients had the possibility to come for an extra control visit with nasal endoscopy at, on average, 68 months postoperatively (Fig. 4).
Figure 3.
Observation of two patient groups: the one without asthma or job exposure, and the other one with asthma and/or job exposure. Comparison of the operation technique with which the patient experienced greater satisfaction, between the patient groups, on average at 68 months postoperatively. The p value by Mann Whitney U test.
DISCUSSION
Our aim was to evaluate symptoms, exacerbation rate, and satisfaction after ESS with either the ostium-preserving or the ostium-enlarging technique at 9 and, on average, 68 months postoperatively. Only a few studies have previously addressed the long-term outcomes of ESS. We showed that all asked sinonasal symptoms decreased significantly postoperatively. The reduction of the symptoms that the patient was able to compare between sides, e.g., facial pain, nasal obstruction, and discharge, were similar both on the uncinectomy-only and the additional middle meatal antrostomy sides. However, three revision surgeries were required during the observation time on the uncinectomy side and one on the antrostomy side. Moreover, patients with asthma and/or job exposure frequently expressed more satisfaction only on the side with antrostomy or neither technique provided them satisfaction. Thus, uncinectomy may not be sufficient in providing lasting symptom relief, especially in patients with risk factors, such as asthma and/or job exposure. Irritant exposure has been less investigated in CRS, whereas, it is known to influence asthma onset and exacerbations.4,5,8 Chronic infection, biofilms, or other factors might play a role in CRS pathogenesis, especially in patients with asthma and/or occupational exposure. These patients could benefit more from an ostium-enlarging approach. This hypothesis requires additional studies to be proven. Others have shown that two-thirds of patients with recalcitrant CRS have biofilms in the sinonasal mucosa, but their influence on disease or ESS outcomes still needs to be elucidated.34,36–39,45 Zhang et al. showed that both asthma and biofilm-forming bacteria were associated with revision ESS after adjustment for other CRS risk factors; however, neither asthma nor biofilms modified each other's association with revision ESS.46 Other studies suggest that CRS patients with asthma might have different bacterial colonization and different responses to bacteria colonizing the sinuses, thus putatively leading to or worsening sinonasal inflammation.7,47,48
The number of reported antibiotic courses for doctor-diagnosed sinusitis during the last year was used in this study as a sign of exacerbation rate. It decreased significantly at 9 months postoperatively, indicating good recovery with both procedures. What is interesting is that exacerbations began to increase after the 9-month postoperative follow-up time. We suggest that as in asthma, these episodes would seem to point at uncontrolled disease and/or poor patient compliance with CRS treatment. It has been shown that patients with Samter's triad suffer usually from difficult-to-treat CRS.49 Although we did not observe this patient group, this could partly explain our finding that patients with CRS and asthma or job exposure were less satisfied after ESS with either technique or with the uncinectomy-only technique. Asthma patients or those with job exposure might have mucosal changes that might lead to poor CRS prognosis.49 More studies of ESS with long-term follow-up and with observations of both QoL and exacerbation rate are needed.
Albu et al. did not find differences in subjective outcomes after performing a large (>16 mm) or small (<16 mm) middle meatal antrostomy, which is in accordance with the findings of our study.26,28,50 We have previously indicated within these patients that at 9 months postoperatively, there was a good and relatively similar recovery of the maxillary sinus mucosa, radiologically evaluated; however, the maxillary sinus mucociliary clearance remained poor on both sides.40,44 Moreover, six obstructed maxillary sinus ostia were found endoscopically on the uncinectomy-only side in contrast to four on the antrostomy side.51
CONCLUSION
The exacerbation rate began to increase between the 9- and, on average, 68-month period postoperatively, whereas the reduction in sinonasal symptoms remained the same during this period. There were no significant differences between uncinectomy with additional antrostomy and uncinectomy-only sides in terms of satisfaction with the operation, facial pain, nasal obstruction, and discharge values. It seems that patients with asthma or job exposure might experience less satisfaction with any procedure or might benefit more from maxillary sinus surgery with the ostium-enlarging than the ostium-preserving technique, compared with patients without these risk factors. Moreover, additional middle meatal antrostomy might be slightly superior to uncinectomy only in terms of the need for revision operations.
ACKNOWLEDGMENTS
The authors thank Irina Kosunen, M.D., and research nurse Marja-Leena Oksanen for excellent assistance.
Footnotes
Funded in part by research grants from the Competitive Research Fund of Pirkanmaa Hospital District, the Finnish Anti-Tuberculosis Association, the Finnish Society of Allergology and Immunology, the Finnish Society of Otorhinolaryngology, the Medical Research Fund of Paijat-Hame Central Hospital, the Ahokas Foundation, and the Tampere Tuberculosis Foundation
The authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Hastan D, Fokkens WJ, Bachert C, et al. Chronic rhinosinusitis in Europe—An underestimated disease. A GA(2)LEN study. Allergy 66:1216–1223, 2011 [DOI] [PubMed] [Google Scholar]
- 2. Fokkens W, Lund V, Mullol J; European Position Paper on Rhinosinusitis and Nasal Polyps group European position paper on rhinosinusitis and nasal polyps 2007. Rhinol Suppl 20:1–136, 2007 [PubMed] [Google Scholar]
- 3. Rudmik L, Soler ZM, Orlandi RR, et al. Early postoperative care following endoscopic sinus surgery: An evidence-based review with recommendations. Int Forum Allergy Rhinol 1:417–430, 2011 [DOI] [PubMed] [Google Scholar]
- 4. Kogevinas M, Zock JP, Jarvis D, et al. Exposure to substances in the workplace and new-onset asthma: An international prospective population-based study (ECRHS-II). Lancet 370:336–341, 2007 [DOI] [PubMed] [Google Scholar]
- 5. Syamlal G, Mazurek JM, Bang KM. Prevalence of lifetime asthma and current asthma attacks in U.S. working adults: An analysis of the 1997–2004 National Health Interview Survey data. J Occup Environ Med 51:1066–1074, 2009 [DOI] [PubMed] [Google Scholar]
- 6. Butland BK, Ghosh R, Strachan DP, et al. Job choice and the influence of prior asthma and hay fever. Occup Environ Med 68:494–501, 2011 [DOI] [PubMed] [Google Scholar]
- 7. Hox V, Delrue S, Scheers H, et al. Negative impact of occupational exposure on surgical outcome in patients with rhinosinusitis. Allergy 67:560–565, 2012 [DOI] [PubMed] [Google Scholar]
- 8. Cummings KJ, Gaughan DM, Kullman GJ, et al. Adverse respiratory outcomes associated with occupational exposures at a soy processing plant. Eur Respir J 36:1007–1015, 2010 [DOI] [PubMed] [Google Scholar]
- 9. Hamilos DL. Chronic rhinosinusitis: Epidemiology and medical management. J Allergy Clin Immunol 128:693–707, 2011 [DOI] [PubMed] [Google Scholar]
- 10. Scadding G, Hellings P, Alobid I, et al. Diagnostic tools in Rhinology EAACI position paper. Clin Trans Allergy 1:2, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Leung RM, Kern RC, Conley DB, et al. Osteomeatal complex obstruction is not associated with adjacent sinus disease in chronic rhinosinusitis with polyps. Am J Rhinol Allergy 25:401–403, 2011 [DOI] [PubMed] [Google Scholar]
- 12. Baroody FM. Interfacing medical and surgical management for chronic rhinosinusitis with and without nasal polyps. Clin Allergy Immunol 20:321–336, 2007 [PubMed] [Google Scholar]
- 13. Miwa M, Miwa M, Watanabe K. Changes in intramaxillary sinus pressure following antrostomy, draining tubes, and YAMIK procedures in 25 patients treated for chronic paranasal sinusitis. Ear Nose Throat J 90:368–381, 2011 [DOI] [PubMed] [Google Scholar]
- 14. Ragab SM, Lund VJ, Scadding G, et al. Impact of chronic rhinosinusitis therapy on quality of life: A prospective randomized controlled trial. Rhinology 48:305–311, 2010 [DOI] [PubMed] [Google Scholar]
- 15. Mace J, Michael YL, Carlson NE, et al. Effects of depression on quality of life improvement after endoscopic sinus surgery. Laryngoscope 118:528–534, 2008 [DOI] [PubMed] [Google Scholar]
- 16. Robinson JL, Griest S, James KE, Smith TL. Impact of aspirin intolerance on outcomes of sinus surgery. Laryngoscope 117:825–830, 2007 [DOI] [PubMed] [Google Scholar]
- 17. Litvack JR, Griest S, James KE, Smith TL. Endoscopic and quality-of-life outcomes after revision endoscopic sinus surgery. Laryngoscope 117:2233–2238, 2007 [DOI] [PubMed] [Google Scholar]
- 18. Das S, Khichi SS, Perakis H, et al. Effects of smoking on quality of life following sinus surgery: 4-Year follow-up. Laryngoscope 119:2284–2287, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mendolia-Loffredo S, Laud PW, Sparapani R, et al. Sex differences in outcomes of sinus surgery. Laryngoscope 116:1199–1203, 2006 [DOI] [PubMed] [Google Scholar]
- 20. Tan BK, Lane AP. Endoscopic sinus surgery in the management of nasal obstruction. Otolaryngol Clin North Am 42:227–240, 2009 [DOI] [PubMed] [Google Scholar]
- 21. Soler ZM, Sauer DA, Mace J, Smith TL. Relationship between clinical measures and histopathologic findings in chronic rhinosinusitis. Otolaryngol Head Neck Surg 141:454–461, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Snidvongs K, Lam M, Sacks R, et al. Structured histopathology profiling of chronic rhinosinusitis in routine practice. Int Forum Allergy Rhinol 2:376–385, 2012 [DOI] [PubMed] [Google Scholar]
- 23. Becker AM, Das S, Xia Z, et al. Serum inflammatory protein profiles in patients with chronic rhinosinusitis undergoing sinus surgery: A preliminary analysis. Am J Rhinol 22:139–143, 2008 [DOI] [PubMed] [Google Scholar]
- 24. Daines SM, Wang Y, Orlandi RR. Periostin and osteopontin are overexpressed in chronically inflamed sinuses. Int Forum Allergy Rhinol 1:101–105, 2011 [DOI] [PubMed] [Google Scholar]
- 25. Myller J, Dastidar P, Torkkeli T, et al. Computed tomography findings after endoscopic sinus surgery with preserving or enlarging maxillary sinus ostium surgery. Rhinology 49:438–444, 2011 [DOI] [PubMed] [Google Scholar]
- 26. Wadwongtham W, Aeumjaturapat S. Large middle meatal antrostomy vs undisturbed maxillary ostium in the endoscopic sinus surgery of nasal polyposis. J Med Assoc Thai 86(suppl 2):S373–S378, 2003 [PubMed] [Google Scholar]
- 27. Kutluhan A, Salviz M, Bozdemir K, et al. The effects of uncinectomy and natural ostial dilatation on maxillary sinus ventilation: A clinical experimental study. Eur Arch Otorhinolaryngol 268:569–573, 2011 [DOI] [PubMed] [Google Scholar]
- 28. Albu S, Tomescu E. Small and large middle meatus antrostomies in the treatment of chronic maxillary sinusitis. Otolaryngol Head Neck Surg 131:542–547, 2004 [DOI] [PubMed] [Google Scholar]
- 29. Welch KC, Stankiewicz JA. A contemporary review of endoscopic sinus surgery: Techniques, tools, and outcomes. Laryngoscope 119:2258–2268, 2009 [DOI] [PubMed] [Google Scholar]
- 30. Kuehnemund M, Lopatin A, Amedee RG, Mann WJ. Endonasal sinus surgery: Extended versus limited approach. Am J Rhinol 16:187–192, 2002 [PubMed] [Google Scholar]
- 31. Salama N, Oakley RJ, Skilbeck CJ, et al. Benefit from the minimally invasive sinus technique. J Laryngol Otol 123:186–190, 2009 [DOI] [PubMed] [Google Scholar]
- 32. Catalano P, Roffman E. Outcome in patients with chronic sinusitis after the minimally invasive sinus technique. Am J Rhinol 17:17–22, 2003 [PubMed] [Google Scholar]
- 33. Welch KC, Stankiewicz JA. Application of minimally invasive endoscopic sinus surgery techniques. Otolaryngol Clin North Am 43:565, 578,, ix, 2010 [DOI] [PubMed] [Google Scholar]
- 34. Foreman A, Jervis-Bardy J, Wormald PJ. Do biofilms contribute to the initiation and recalcitrance of chronic rhinosinusitis? Laryngoscope 121:1085–1091, 2011 [DOI] [PubMed] [Google Scholar]
- 35. Larson DA, Han JK. Microbiology of sinusitis: Does allergy or endoscopic sinus surgery affect the microbiologic flora? Curr Opin Otolaryngol Head Neck Surg 19:199–203, 2011 [DOI] [PubMed] [Google Scholar]
- 36. Singhal D, Psaltis AJ, Foreman A, Wormald PJ. The impact of biofilms on outcomes after endoscopic sinus surgery. Am J Rhinol Allergy 24:169–174, 2010 [DOI] [PubMed] [Google Scholar]
- 37. Bendouah Z, Barbeau J, Hamad WA, Desrosiers M. Biofilm formation by Staphylococcus aureus and Pseudomonas aeruginosa is associated with an unfavorable evolution after surgery for chronic sinusitis and nasal polyposis. Otolaryngol Head Neck Surg 134:991–996, 2006 [DOI] [PubMed] [Google Scholar]
- 38. Suh JD, Ramakrishnan V, Palmer JN. Biofilms. Otolaryngol Clin North Am 43:521, 530,, viii, 2010 [DOI] [PubMed] [Google Scholar]
- 39. Psaltis AJ, Weitzel EK, Ha KR, Wormald PJ. The effect of bacterial biofilms on post-sinus surgical outcomes. Am J Rhinol 22:1–6, 2008 [DOI] [PubMed] [Google Scholar]
- 40. Myller JP, Toppila-Salmi SK, Toppila EM, et al. Mucosal eosinophils and l-selectin ligands are associated with invasive and noninvasive sinus surgery outcomes. Am J Rhinol Allergy 23:21–27, 2009 [DOI] [PubMed] [Google Scholar]
- 41. Lund VJ, Kennedy DW. Quantification for staging sinusitis. The Staging and Therapy Group. Ann Otol Rhinol Laryngol Suppl 167:17–21, 1995 [PubMed] [Google Scholar]
- 42. Lund VJ, Mackay IS. Staging in rhinosinusitus. Rhinology 31:183–184, 1993 [PubMed] [Google Scholar]
- 43. Toppila-Salmi SK, Myller JP, Torkkeli TV, et al. Endothelial L-selectin ligands in sinus mucosa during chronic maxillary rhinosinusitis. Am J Respir Crit Care Med 171:1350–1357, 2005 [DOI] [PubMed] [Google Scholar]
- 44. Myller J, Toppila-Salmi S, Torkkeli T, et al. Effect of endoscopic sinus surgery on antral mucociliary clearance. Rhinology 44:193–196, 2006 [PubMed] [Google Scholar]
- 45. Hai PV, Lidstone C, Wallwork B. The effect of endoscopic sinus surgery on bacterial biofilms in chronic rhinosinusitis. Otolaryngol Head Neck Surg 142:S27–S32, 2010 [DOI] [PubMed] [Google Scholar]
- 46. Zhang Z, Linkin DR, Finkelman BS, et al. Asthma and biofilm-forming bacteria are independently associated with revision sinus surgeries for chronic rhinosinusitis. J Allergy Clin Immunol 128:221–223, 2011 [DOI] [PubMed] [Google Scholar]
- 47. Ragab A, Clement P, Vincken W. Bacterial cultures of the middle meatus and bronchoalveolar lavage in chronic rhinosinusitis. ORL J Otorhinolaryngol Relat Spec 69:85–91, 2007 [DOI] [PubMed] [Google Scholar]
- 48. Zurak K, Vagic D, Drvis P, et al. Bacterial colonization and granulocyte activation in chronic maxillary sinusitis in asthmatics and non-asthmatics. J Med Microbiol 58:1231–1235, 2009 [DOI] [PubMed] [Google Scholar]
- 49. Mendelsohn D, Jeremic G, Wright ED, Rotenberg BW. Revision rates after endoscopic sinus surgery: A recurrence analysis. Ann Otol Rhinol Laryngol 120:162–166, 2011 [DOI] [PubMed] [Google Scholar]
- 50. Catalano PJ. Minimally invasive sinus technique: What is it? Should we consider it? Curr Opin Otolaryngol Head Neck Surg 12:34–37, 2004 [DOI] [PubMed] [Google Scholar]
- 51. Luukkainen A, Myller J, Torkkeli T, et al. Endoscopic sinus surgery with antrostomy has better earlier endoscopic recovery in comparison to the ostium-preserving technique. ISRN Otolaryngol 2012. (Article ID 189383, DOI:10.5402/2012/189383.) [DOI] [PMC free article] [PubMed] [Google Scholar]