Abstract
Purpose/Background:
Several examination tests are currently used for diagnosing a supraspinatus lesion. The empty can (EC) test is currently considered the gold standard for testing, but full can (FC) testing is also utilized. Both of these tests do not fully eliminate the deltoid synergistic when resistance is applied. A new diagonal horizontal adduction (DHA) technique has been developed for evaluation of the supraspinatus that has not yet been compared with the existing techniques (EC/FC). Cross‐sectional analysis (CSA) change during contraction as an ultrasonographic means of visualizing and measuring contraction of the supraspinatus has been reported previously.
Objective:
The purpose of this study was to use diagnostic musculoskeletal ultrasound (MSK) to compare CSA of the supraspinatus during the FC, EC, and the DHA tests.
Methods:
The supraspinatus muscle of 37 healthy, uninjured volunteers (21 males and 16 females, mean age of 26.9) were visualized and CSA was captured during 4 randomly assigned test positions (including control) using MSK.
Results:
A one‐way Analysis of Variance with repeated measures of the mean CSA obtained in the testing positions was performed followed by least significant difference (LSD) for post‐hoc analysis. Significant differences (p < 0.05) were found between the mean CSA of the controls and the CSA of each of the three testing procedures analyzed using the MSK. There were no significant differences (p < 0.05) in CSA between any of the three testing procedures.
Conclusions:
In this study, MSK visualized and objectified activity of the supraspinatus muscle as evidenced through increased mean CSA when resisted. All the testing positions (FC, EC, and DHA) demonstrated significantly increased mean CSA of the muscle when isometrically contracted when compared to the resting control. The DHA procedure also elicited significant increase in CSA of the supraspinatus. However, no significant difference was found between the CSA of the DHA when compared to the FC and EC tests.
Level of Evidence:
Level 2
Keywords: Cross‐sectional analysis, supraspinatus testing, ultrasound diagnostics
INTRODUCTION
Rotator cuff disease is one of the most common causes of shoulder pain.1–3 The supraspinatus muscle is usually involved in injuries of the rotator cuff. Jobe and Moynes4 report that the function of the supraspinatus muscle can be isolated and then assessed to some degree with the shoulder near 90° of elevation 20 degrees of horizontal abduction, and full internal rotation, a position they named the empty can test (EC). This has been clarified in muscle testing books as being performed in 90 degrees of elevation in the plane of the scapula with full internal rotation. Assessing isometric strength in this position is commonly referred to as the supraspinatus test. Holtby and Razmjou5 found the sensitivity of the supraspinatus test to be high (88%) for large to massive tears but lower for less severe injuries to the tendon and specificity was less (70% or less) for any injury to the tendon. Hughes et al6, through a systematic review of literature, also reported that the supraspinatus test demonstrated acceptable diagnostic accuracy with full or partial thickness tears.
Several authors have suggested the EC position is painful to perform in many subjects and may recruit unnecessary agonist musculature. Kelly et al7 proposed a resistance test for assessment of the function of the supraspinatus muscle and tendon with the shoulder below 90° of elevation, also in the plane of the scapula, and 45° of external rotation and labeled this the full can test (FC) position. Kelly et al8 suggested the EC position caused subacromial impingement of the shoulder at 90 degrees of elevation and suggested the full can position was less irritating to the supraspinatus as it passes in the subacromial area. These same authors noted that the electromyographic (EMG) activity of the supraspinatus muscle in both the FC and EC tests were similar with the FC test producing less pain during the testing.7 Yasojima et al9 reported EMG activity of the supraspinatus was significantly greater than those of the infraspinatus or teres minor muscles in the FC position at 45‐60 degrees of elevation in the scapular plane when loaded with a set resistance. This 45‐60 degree position was suggested as a better position for both of the test positions in order to reduce impingement and compensatory motions. Escamilla et al10, after reviewing the EMG contractions of the EC and FC tests, suggested the FC test might be the best testing position because it is less likely to cause the impingement that occurs during EC testing yet still results in a significant contraction of the supraspinatus. However, they also acknowledged this test position allowed more assistive activity from the subscapularis and the infraspinatus.
Recording of the actual muscular activity of the supraspinatus is challenging and typically is recorded using fine wire EMG as surface EMG records concurrent with the activity of the upper trapezius. Researchers have attempted to find alternative and less invasive means of measuring activity of this deeper musculature. Takeda et al11 used MRI to measure the change in CSA of the supraspinatus and compared this to EMG activity of the supraspinatus to determine that both the EC and FC exercises were effective in activating the supraspinatus muscle. There has been minimal research reporting on the activity of the muscles of the shoulder assessed with diagnostic musculoskeletal ultrasound (MSK).12
Possible problems with the existing FC and EC tests still exist. Beyond the issue of assistive deltoid activity, both tests do not require the supraspinatus muscle to perform the glenohumeral stabilization or approximation function as described by Longo et al.13 The supraspinatus muscle biomechanically provides stability to the glenohumeral joint (GHJ) and prevents impingement of the supraspinatus in the subacromial arch during arm elevation through approximation of the humeral head into the glenoid fossa during the elevation of the arm.14 Reinold et al demonstrated increased activity of the supraspinatus with distraction of the humerus from the glenoid utilizing measurements obtained via fine wire EMG.15 Abduction of the humerus between 30‐60° increases compression of the humeral head in the glenoid fossa and allows the supraspinatus to hold the humerus tightly in the glenoid fossa.10,15 Using this information, clinicians have developed a technique to examine the ability of the supraspinatus to perform the function of approximation and stabilization of the humerus in the glenoid fossa. This technique places the shoulder in a full horizontally adducted position, in 30 degrees of flexion, with full external rotation. This position distracts the humeral head out of the glenoid fossa and puts the supraspinatus tendon on stretch. The subject/patient is then asked to lift the arm off the chest (horizontally abduct) so the supraspinatus performs it's function of approximation and pulls the humeral head into close approximation with the glenoid fossa. The authors of this study will hereafter refer to this test position as the diagonal horizontal adduction test of DHA test. This new testing technique is hypothesized to isolate the supraspinatus during contraction and focuses on the supraspinatus action of approximation of the humerus into the glenoid fossa. A review of the literature did not produce any studies that have investigated the DHA test. There are also no studies comparing the DHA to the commonly utilized EC and FC tests.
Recently several authors have demonstrated that the supraspinatus can be examined and evaluated using MSK. Boehm et al16 concluded that good intra and inter‐observer reliability is attained in visualization and measurement of the cross section of the supraspinatus through MSK. MSK has been used to increase the efficiency of diagnosing atrophy of the supraspinatus muscle17 and has been found to be as accurate as magnetic resonance imaging (MRI) in assessing tears of the tendon of the supraspinatus because of excellent visualization of this area.17–21 This unique tool is also capable of visualizing contraction of muscle tissue over time (dynamic visualization), which is not available through the use of MRI or other imaging modalities. MSK is an inexpensive alternative to MRI and just as accurate at assessing pathology and activity of muscle and tendon.22
Most previous studies of muscle activity in the supraspinatus have involved the use of fine wire EMG. However, less invasive techniques have been used involving observation of the changes in the cross‐sectional analysis (CSA) of a muscle as an indicator of the activity of the muscle. Zanetti and colleagues23 used CSA of muscle through MRI analysis and determined that this type of measurement could be used in determination of the activity of the muscles of the rotator cuff. Maughan et al24 demonstrated a positive relationship between CSA of a muscle, measured by MRI, and strength. Maughan et al measured resistance and compared the resistance to changes in CSA. Akagi et al25 concluded that muscle CSA can be assessed with diagnostic MSK during maximum voluntary contraction, thus allowing for an easy and practical evaluation of the muscle strength. Two studies have demonstrated MSK provides repeatable and valid measures of a muscle CSA, muscle thickness and moment arm.26,27 Moreover, MSK can detect training‐induced changes in muscle CSA with a comparable degree of precision when compared to MRI.28 Therefore, CSA of the supraspinatus muscle can be measured through the use of ultrasonography and changes in CSA will relate to muscle activity.
The purpose of this study was to use diagnostic MSK to compare CSA of the supraspinatus during the FC, EC, and the DHA tests. The new testing technique proposed is hypothesized to isolate the supraspinatus during contraction and focuses on the supraspinatus action of approximation of the humerus into the glenoid fossa. The hypotheses are that the DHA testing technique will show a similar or larger change in CSA when compared to the FC or EC techniques and that the FC and EC techniques will each have similar changes in CSA when compared to each other.
METHODS
Subjects
The institutional review board of the University of Central Arkansas approved this study. Informed consent was obtained prior to the collection of data on any subject. The subjects for this project were volunteer students and faculty members from a mid‐south physical therapy university educational program without any reported history of injury or pathological condition of the shoulder or upper quarter. There were 37 participants, 21 males and 16 females. The participant's mean age was 26.9 years (range 22‐55). Most of the subjects were right hand dominant (n=34) with only 3 participants being left hand dominant. The subjects all signed an informed consent form.
Equipment
Two researchers with specialty training and several years of experience in diagnostic musculoskeletal ultrasound (MSK) were utilized to collect the CSA data from the participants. The MSK units used in this study were two identical Terason t3200 MSK ultrasound machines (Terason Ultrasound, Division of Teratech Corporation, Burlington, MA) each with a 15L4 linear array transducer head. There were two MSK data collection stations, each with one MSK machine. There were three researchers at each data station: one expert MSK specialist to obtain and optimize the image of the supraspinatus in the sulcus, another researcher who made sure participants were properly aligned to the boards guiding position and resisting during the test positions, and one researcher who operated the computer to capture the images when requested by the MSK specialist. The MSK machine was set up on a table away from the participants so the patient could not see the screen of the unit. An alignment board with predesigned markings at a 60° angle indicating the height of participants' shoulders and the corresponding angle from the vertical. This was also set at 45° of angle from the sagittal axis to maintain proper scapular plane abduction position (Figure 1). The angle was used to gauge the degree to which each participant would raise their arm during the FC and EC methods. The board was at the proper position in front of the subject so that the participant could maintain a proper alignment during all testing and was placed 25 cm in height from the ground (Figure 1).
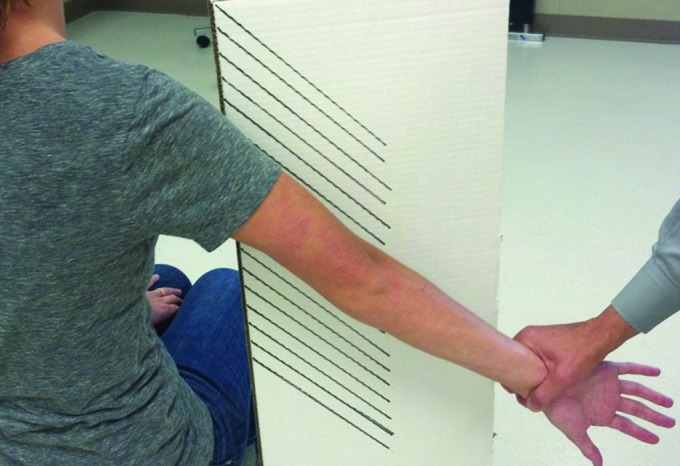
Figure 1.

Stool and marked board used to maintain proper position of the subject's arm at 60 degree elevation and 45 degrees in the sagittal axis.
Testing Protocol
Upon entry to the facility, the subjects read and signed the informed consent document and then were randomly assigned a sequence of testing utilizing the EC, FC, and DHA positions. The subjects assumed the proper state of dress to expose the right shoulder (males removed shirt and females wore sports bra for testing). The height of the stool was adjusted to allow the acromion to be 120 cm from the ground (Figure 1). Proper posture was encouraged throughout the session (upright without protraction, retraction, or slouching). The MSK operator cleaned the area to be visualized with alcohol wipes and placed 4cm of hypoallergenic MSK transduction gel in the area over the supraspinatus muscle. The MSK operator found the tip of acromion and measured three inches medially to locate the supraspinatus. The bony landmark of the scapular notch was the defining landmark that verified to the MSK operator that the muscle being visualized was the supraspinatus and was used in later measurements of CSA (Figure 2). Depending on the muscle thickness of the participants, depth for resolution was set at 4‐7 cm and resolution was set between 10‐17 Hz. A baseline image was captured of the supraspinatus muscle in a neutral relaxed position (the arm resting comfortably at the subject's side) and this was used as the control (Figure 2). The transducer position on the supraspinatus is demonstrated in Figure 3. The subject then was asked to do each of the 3 test positions in the order randomized for their session. Each position was resisted by one of the researchers by applying resistance to the wrist of the subject to the point of failure while the MSK operator captured the image of the contraction at maximum clarity and proper position within this hold time (Figure 4). A rest period of 1 minute was given between each position and contraction. On average, each participant took 5 minutes to complete all the tests.
Figure 2.

Ultrasound transducer position over the supraspinatus.
Figure 3.
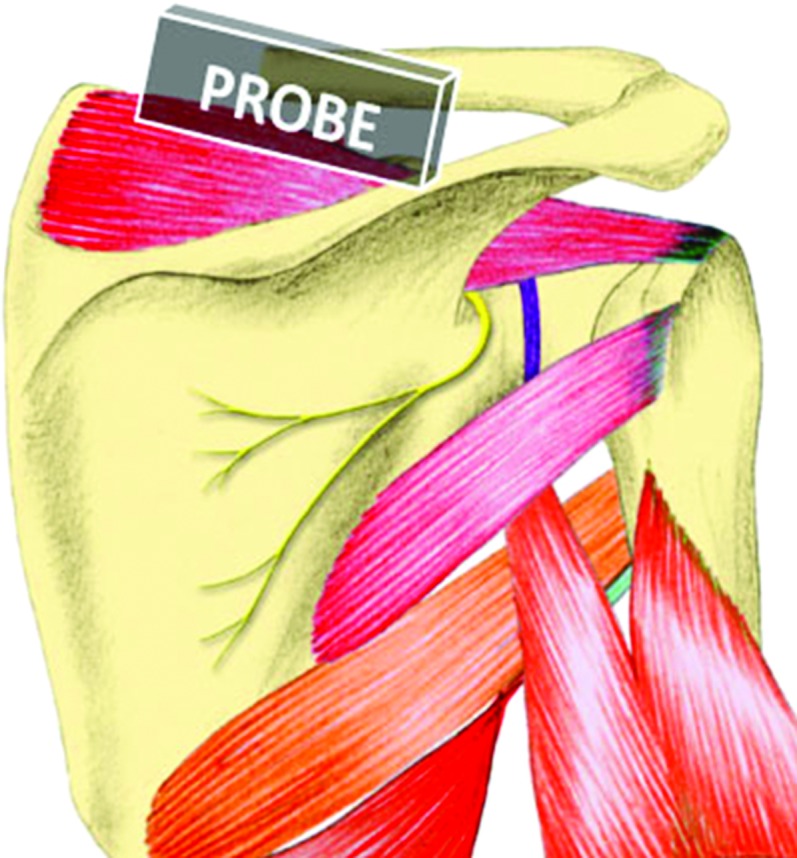
Artist's representation of the position of the ultrasound transducer head position in relation to the supraspinatus.
Figure 4.
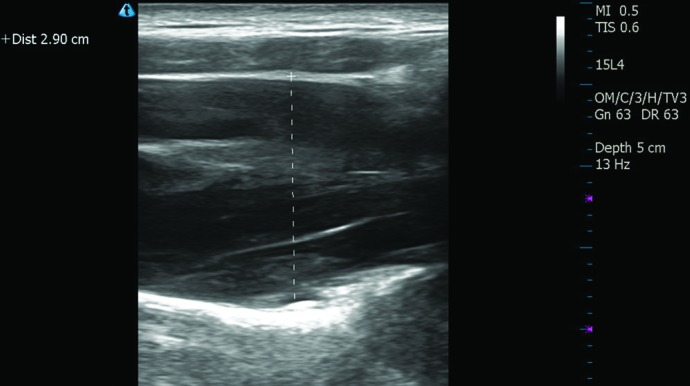
Image captured on ultrasound with cross section marker used for measurement.
The three test positions were:
The EC position: The elbow of the subject was fully extended, the shoulder was in full internal rotation with the thumb facing the ground, the arm was in the scapular plane (approximately 45° horizontally abducted from the sagittal plane) and abducted to 60° (the end of the range of maximal contraction of the supraspinatus according to Escamilla et al10). Resistance occurred as the subject tried to hold the arm in this position while the researcher pushed down toward the ground with resistance given at the wrist. (Figure 5)
The FC position: The elbow of the subject was fully extended, the shoulder was in external rotation so that the thumb pointed to the ceiling, the arm was in the scapular plane (45° horizontally abducted from the sagittal plane) and the arm was abducted to 60°. Resistance occurred as the subject tried to hold the arm in this position while the researcher pushed down toward the ground with resistance given at the wrist. (Figure 6)
The DHA position: The shoulder was in horizontal adduction with the elbow extended and the arm fully externally rotated (thumb pointing toward the ceiling) at 35° of flexion. The arm was placed across the nipple line of the near chest so that the triceps lay across the corner of the chest. Resistance occurred as the subject lifted the arm off the chest and the researcher pushed inward toward the start position. (Figure 7)
Figure 5.
Empty can testing position with applied isometric resistance.
Figure 6.
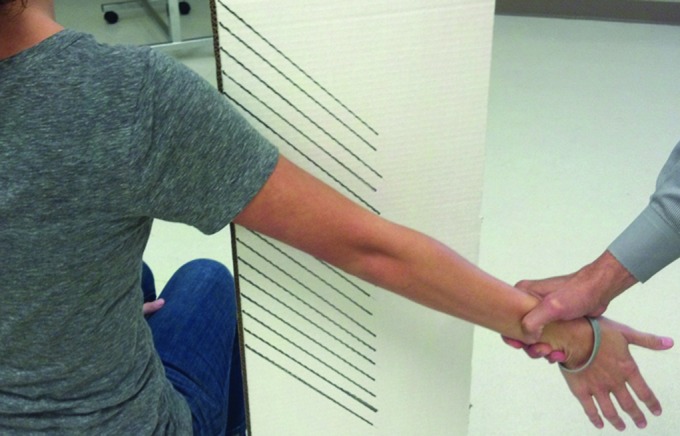
Full can testing position with applied isometric resistance.
Figure 7.
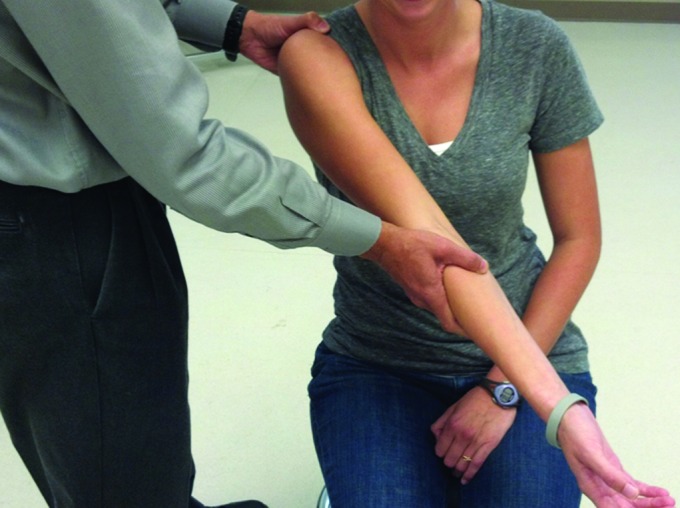
Diagonal horizontal adduction testing position. The arm of the subject is fully externally rotated and adducted across the pectoral area. The subject is asked to lift the arm off the chest against isometric resistance.
In each position, resistance was provided at the wrist to achieve a level of contraction of the supraspinatus just short of failure (inability to maintain position and height of the arm). The subject was encouraged to maintain this contraction for up to 5 seconds or long enough to allow an adequate recording through US.
At the end of the testing, the recordings of supraspinatus muscle for each participant were reviewed and a line was drawn using the suprascapular notch and the fascial layer between the supraspinatus and upper trapezius muscles as endpoints (Figure 2). The length of line drawn between these two landmarks was then measured on the screen and this was labeled as the CSA of the supraspinatus. Differences or change in CSA from the rest position (neutral control) to each of the testing positions and between test positions was compared. Results obtained are shown in the results section.
STATISTICAL METHODS
Statistical analysis was performed using SPSS 14.0 statistical software (SPSS Inc., Chicago, IL). The mean and standard deviation of the CSA measurements obtained in each of the four positions of testing (neutral or control, EC, FC, and DHA) were calculated. A repeated measure one‐way ANOVA was performed for these means and a post‐hoc analysis was completed using pairwise comparisons utilizing least significant difference. A post hoc power analysis was performed and there was a small effect size and there would need 100 subjects to have 80% power to detect a difference at alpha=.05. However, our goal was not to find the smallest difference possible as this analysis would suggest. Results obtained are shown in the results section.
RESULTS
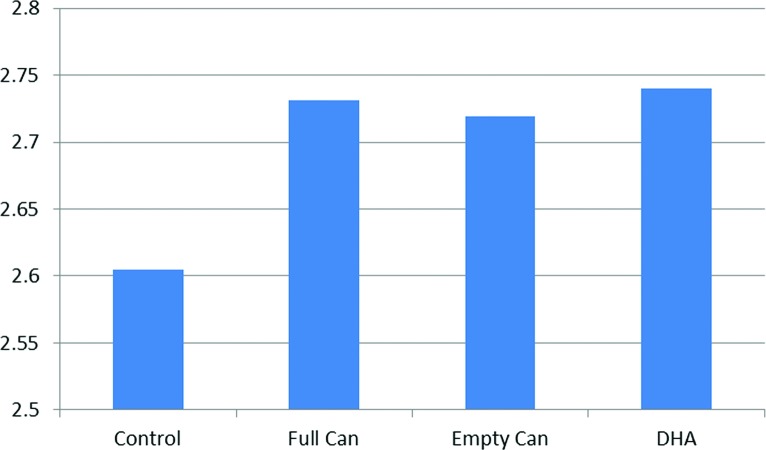
Table 1 and Figure 8 display the mean and standard deviation results for the CSA measurements obtained in the four different testing positions (control, FC, EC, and DHA).
Table 1.
Demographics of Study Participants.
| Testing Group | Mean CSA | SD | N |
| C | 2.605 | 0.442 | 37 |
| FC | 2.732 | 0.484 | 37 |
| EC | 2.719 | 0.460 | 37 |
| DHA | 2.740 | 0.430 | 37 |
CSA: Cross Sectional Area, SD: Standard Deviation, N: Number of Participants C: Control, FC: Full Can, EC: Empty Can, DHA: Diagonal Horizontal Adduction
Figure 8.
Mean cross‐section measurement of each testing position and control. DHA: diagonal horizontal adduction.
A repeated measures one‐way ANOVA revealed a statistically significant difference in the mean CSA of the supraspinatus in the test positions when compared to the control position at p<0.02. A post hoc analysis using pairwise comparisons utilizing least significant difference indicated that the mean change in CSA was significant between the control (relaxed) position and each of the other three positions (p<0.05). However, when the FC, EC, and DHA techniques were compared to each other, the mean change in CSA was not found to be significant (Table 2). Specifically, the DHA position had the largest change in mean CSA measurement when compared to the control and had the least standard deviation but the differences in mean CSA between each of the active test positions was not significant.
Table 2.
Statistical Comparisons of Means and Standard Errors between Test Positions.
| TEST MEANS COMPARED | MEAN DIFFERENCE | STANDARD ERROR | P‐VALUE: SIGNIFICANCE* |
|---|---|---|---|
| C/FC | −0.126 | 0.047 | 0.011* |
| C/EC | −0.114 | 0.045 | 0.017* |
| C/DHA | −0.135 | 0.052 | 0.013* |
| FC/EC | 0.012 | 0.036 | 0.729 |
| FC/DHA | −0.009 | 0.052 | 0.870 |
| EC/DILA | −0.021 | 0.055 | 0.703 |
O Control; FC= Full Can; EC= Empty Can; DHA= Diagonal Horizontal Abduction; *= significant at p<0.05
DISCUSSION
In this study, CSA was the primary measurement taken to define activity through three different positions for testing the supraspinatus muscle, (FC, EC, and DHA testing). All three tests show significant and similar increase in CSA when compared to resting (control). One could surmise that the DHA test might be another means of testing the supraspinatus activity and strength.
The ability to isolate a muscle during contraction is important to help determine activity. The definition of relative isolation does not require maximal activation of the muscle of interest, but rather greater activation of that muscle relative to the mean activation of the other surrounding muscles.29 The supraspinatus muscle not only assists in elevation of the shoulder and approximates the humerus into the glenoid fossa, it also contributes to shoulder external rotation, assisted by the infraspinatus muscle, the teres minor muscle, and the posterior deltoid.10 Reinold et al analyzed the EMG activity of the rotator cuff and deltoid musculature during common shoulder exercises.15 These researchers measured fine wire EMG activity in healthy subjects using different shoulder positions including prone horizontal abduction and standing external rotation at both 45 degrees and zero degrees of abduction. The prone testing position has not been suggested to be a strength test but has been suggested to be used as a strengthening position for the supraspinatus because of lack of isolation of the supraspinatus muscle, and therefore was not utilized in this study.
Any physical examination test for the supraspinatus in isolation does not completely rule in large to massive tears, but it should suggest that a clinician progress to further testing to confirm the diagnosis since a positive finding suggests a fairly significant probability of pathology.15 Calis et al30 concluded that physical examination tests were insufficient for certain diagnoses, but suggested that the tests play an important part in clinical evaluation. Evidence supports the use of both the FC and EC tests for evaluation of supraspinatus activity and strength, but not enough evidence exists to support that these testing positions be used for isolation of the supraspinatus or for strengthening of this muscle after injury. Ure et al31 did not find single tests very helpful and felt that a combination of tests used by an experienced clinician provided more information regarding injury to the supraspinatus tissue, suggesting that the EC, the FC, and other supraspinatus testing procedures (such as the DHA) might be used in combination for best effect.
In the current study there was no attrition between the numbers of subjects recruited and the numbers of subjects participating in the study under consent. Attrition is common with studies involving fine wire EMG. Fine wire EMG is considered to be the best means of determining electrical activity of any accessible muscle group.29 The placement of fine wires is easy to do in the supraspinatus muscle, but obviously is more invasive than US as a measurement tool. Fine wire EMG also reduces “cross‐talk” from muscles surrounding the supraspinatus but, also isolates only a small section of the muscle being tested.32 Reproducing the recorded data is difficult because small variations in the placement of the electrodes produce recordings from a different area of the muscle.32 The volunteer subjects also have less risk of infection and discomfort if a researcher assesses the activity of a muscle without this invasion of the tissue with a fine wire. Subjects may be more eager to participate in studies that utilize non‐invasive methods as demonstrated in this study.
Ultrasonography as a means of defining activity in a muscle may be more acceptable than fine wire EMG and demonstrates sensitivity and specificity when used for identifying changes in morphology of the rotator cuff.20,27,33–38 More research needs to be performed in order to define the parameters needed for accurate measurement of muscle activity using US and should involve some form of measurement of CSA during relaxation and contraction. These definitions and protocols may allow US to be used more frequently in place of fine wire EMG in supraspinatus activity studies.
This data suggests that the resisted EC position does allow a significant contraction of the supraspinatus visualized with US when compared to a resting state of the muscle (p = .011). This data is strongly supported by previous research. The EC test is still considered the standard supraspinatus strength testing procedure.6,10,39 Worrell et al40 demonstrated that the EC position produced the most torque but they also suggested this might be a result of the recruitment of the posterior and middle deltoid. Kelly et al7 expressed concern that impingement positioning may decrease the accuracy of the EC test for muscle testing. Impingement was reduced in this study by keeping the shoulder at less than 60° of elevation during all EC testing.
In this sample of subjects, the resisted FC testing position demonstrated a significant increase in CSA of the supraspinatus muscle when compared to the resting position (p = 0.017). However, this positional test did not have a significant difference when compared to the EC position during resistive testing (p = .729). The full can test is considered a viable alternate test position for the supraspinatus when there might be a possibility of subacromial impingement.7 As impingement can cause a pain response, even in asymptomatic subjects, and this pain response can further decrease the ability to contract the supraspinatus fully, certain authors have suggested the full can test may be a better test of supraspinatus function than the empty can test.7,41 Again, ultrasonography has rarely been used to measure CSA or activity responses in the supraspinatus of normal subjects when performing the FC testing.
The DHA technique was effective in demonstrating a contraction of the supraspinatus when compared to the resting position, and demonstrated the largest descriptive change in mean cross‐sectional area across all subjects, although no significant difference existed between mean CSA during the resisted EC test position, the resisted FC test position, and the resisted DHA test positions. Thus, all were equally effective at creating activity in the supraspinatus (measured by CSA). This testing procedure has been utilized in the clinical situation in evaluation of supraspinatus function, but has not been tested or reviewed in the literature up until this study, to the knowledge of the authors. Additional research is needed comparing the EMG activity of the deltoid musculature and the supraspinatus musculature in each of these three test positions in order to assess relative activity of these two synergistic muscles.
All three tests are effective in soliciting a contraction of the supraspinatus when measuring change in CSA through US. However, the lack of significant difference between the three resisted techniques does not suggest one testing technique is superior for obtaining a contraction of the supraspinatus over the others. The DHA technique can be used in conjunction with the currently used techniques, but should not be used as the only diagnostic test in order to confirm a supraspinatus weakness or injury as there is lack of research on the efficacy of this test. When exploring any new testing technique, multiple investigations need to be performed in order to allow validation of the procedure. Much more investigation needs to be performed, using EMG and other tools, to determine the efficacy of the DHA test. Based on the results of this study, the DHA may compliment the EC and/or FC tests in the evaluation of supraspinatus strength and activation. These tests, if used in combination, may help the clinician determine if supraspinatus pathology exists.
LIMITATIONS
This study has potential limitations. The resistance applied to the subject by the researcher was not measured quantitatively. Because of this, it is possible that each subject did not receive the same resistance during each test position or as the other subjects. Significant and consistent contraction of the muscle tested would be necessary to get optimal change in CSA of that muscle. However, the same researcher was applying the resistance throughout the study and attempted to achieve a maximal contraction (point just short of failure) from the subjects across all conditions. Also, though proper posture was encouraged throughout the testing, many of the subjects had tendencies to slump during the resistive testing procedures. This lack of postural support may influence the values recorded in CSA through US.
The position chosen for the EC test was at 60° of elevation and Jobe and Moyne4 suggested this position should be near 90°. The authors chose this position to eliminate the potential of reduced muscle activity, which has been discussed as a limitation of the EC test. Escamilla et al10 also suggested the best activity of the supraspinatus was at 60° of elevation. The authors realize that this position was different than the original description in the Jobe and Moyne article and understand that this may limit comparisons using the results from this study.
Cross‐sectional measurements of various muscles have been attained in many different ways through the a variety of previous studies. In this study, a straight line from the supraspinatus notch to the fascial line between the deltoid and the supraspinatus was drawn and measured and was used as the CSA measurement. This measurement does not take into account the volume of the entire area of the muscle which is suggested to correlate best to muscle strength.23,24,42–44 There is little literature suggesting a proper measurement of CSA using either MRI or US for the supraspinatus. This needs to be further defined.
FUTURE RESEARCH
Further research on the DHA test is necessary. Any new testing procedure would need to be compared to the gold standard test for the same activity or muscle. In the shoulder, the gold standard tests for the supraspinatus are the FC and EC tests. Even though the DHA had similar results in mean change in CSA when compared to the EC and FC tests using change in CSA through US in normal, healthy subjects, this test has not been performed or analyzed using EMG data and has not been used or tested in the painful or injured population.
CONCLUSION
In this study, US effectively visualized and objectified activity of the supraspinatus muscle as evidenced through increased mean CSA of the muscle when resisted. All the testing positions (FC, EC, and DHA) demonstrated significantly increased mean CSA of the muscle when isometrically contracted, as compared to CSA of the rest position. The DHA procedure elicited significant increase in CSA of the supraspinatus and might be effectively used in conjunction with current tests in diagnosing supraspinatus lesions. Although the data obtained during the DHA test elicits this activity of the supraspinatus, there was no significant difference between the CSA of the supraspinatus during this new test when compared to the CSA's obtained during the FC and EC tests.
REFERENCES
- 1.Murrell GA, Walton JR. Diagnosis of rotator cuff tears. Lancet. Mar 10 2001;357(9258):769–770 [DOI] [PubMed] [Google Scholar]
- 2.Ostergren PO, Hanson BS, Balogh I, et al. Incidence of shoulder and neck pain in a working population: effect modification between mechanical and psychosocial exposures at work? Results from a one year follow up of the Malmo shoulder and neck study cohort. J Epidemiol Community Health. Sep 2005;59(9):721–728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis. Nov 1998;57(11):649–655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jobe FW, Moynes DR. Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries. The American journal of sports medicine. Nov‐Dec 1982;10(6):336–339 [DOI] [PubMed] [Google Scholar]
- 5.Holtby R, Razmjou H. Validity of the supraspinatus test as a single clinical test in diagnosing patients with rotator cuff pathology. The Journal of orthopaedic and sports physical therapy. Apr 2004;34(4):194–200 [DOI] [PubMed] [Google Scholar]
- 6.Hughes PC, Taylor NF, Green RA. Most clinical tests cannot accurately diagnose rotator cuff pathology: a systematic review. Aust J Physiother. 2008;54(3): 159–170 [DOI] [PubMed] [Google Scholar]
- 7.Kelly BT, Kadrmas WR, Speer KP. The manual muscle examination for rotator cuff strength. An electromyographic investigation. The American journal of sports medicine. Sep‐Oct 1996;24(5):581–588 [DOI] [PubMed] [Google Scholar]
- 8.Abdul‐Latif AA. Dropped shoulder syndrome: a cause of lower cervical radiculopathy. J Clin Neurol. Jun 2011;7(2):85–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yasojima T, Kizuka T, Noguchi H, Shiraki H, Mukai N, Miyanaga Y. Differences in EMG activity in scapular plane abduction under variable arm positions and loading conditions. Medicine and science in sports and exercise. Apr 2008;40(4):716–721 [DOI] [PubMed] [Google Scholar]
- 10.Escamilla RF, Yamashiro K, Paulos L, Andrews JR. Shoulder muscle activity and function in common shoulder rehabilitation exercises. Sports medicine. 2009;39(8):663–685 [DOI] [PubMed] [Google Scholar]
- 11.Takeda Y, Kashiwaguchi S, Endo K, Matsuura T, Sasa T. The most effective exercise for strengthening the supraspinatus muscle: evaluation by magnetic resonance imaging. The American journal of sports medicine. May‐Jun 2002;30(3):374–381 [DOI] [PubMed] [Google Scholar]
- 12.Audenaert EA, De Roo PJ, Mahieu P, et al. Deltoid muscle volume estimated from ultrasonography: in vitro validation and correlation with isokinetic abduction strength of the shoulder. Medical & biological engineering & computing. May 2009;47(5):557–563 [DOI] [PubMed] [Google Scholar]
- 13.Longo UG, Berton A, Papapietro N, Maffulli N, Denaro V. Biomechanics of the rotator cuff: European perspective. Med Sport Sci. 2012;57:10–17 [DOI] [PubMed] [Google Scholar]
- 14.Kolber MJ, Beekhuizen KS, Cheng MS, Hellman MA. Shoulder joint and muscle characteristics in the recreational weight training population. J Strength Cond Res. Jan 2009;23(1):148–157 [DOI] [PubMed] [Google Scholar]
- 15.Reinold MM, Macrina LC, Wilk KE, et al. Electromyographic analysis of the supraspinatus and deltoid muscles during 3 common rehabilitation exercises. Journal of athletic training. Oct‐Dec 2007;42(4):464–469 [PMC free article] [PubMed] [Google Scholar]
- 16.Boehm TD, Kirschner S, Mueller T, Sauer U, Gohlke FE. Dynamic ultrasonography of rotator cuff muscles. J Clin Ultrasound. Jun 2005;33(5):207–213 [DOI] [PubMed] [Google Scholar]
- 17.Khoury V, Cardinal E, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscle: sonography versus MRI. AJR Am J Roentgenol. Apr 2008;190(4):1105–1111 [DOI] [PubMed] [Google Scholar]
- 18.Alasaarela E, Takalo R, Tervonen O, Hakala M, Suramo I. Sonography and MRI in the evaluation of painful arthritic shoulder. Br J Rheumatol. Sep 1997;36(9):996–1000 [DOI] [PubMed] [Google Scholar]
- 19.Kelly BT, Williams RJ, Cordasco FA, et al. Differential patterns of muscle activation in patients with symptomatic and asymptomatic rotator cuff tears. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons … [et al.]. Mar‐Apr 2005;14(2):165–171 [DOI] [PubMed] [Google Scholar]
- 20.Naqvi GA, Jadaan M, Harrington P. Accuracy of ultrasonography and magnetic resonance imaging for detection of full thickness rotator cuff tears. Int J Shoulder Surg. Oct 2009;3(4):94–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wall LB, Teefey SA, Middleton WD, et al. Diagnostic performance and reliability of ultrasonography for Fatty degeneration of the rotator cuff muscles. J Bone Joint Surg Am. Jun 20 2012;94(12):e831–839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jacobson JA. Musculoskeletal ultrasound: focused impact on MRI. AJR Am J Roentgenol. Sep 2009;193(3):619–627 [DOI] [PubMed] [Google Scholar]
- 23.Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol. Mar 1998;33(3):163–170 [DOI] [PubMed] [Google Scholar]
- 24.Maughan RJ. Relationship between muscle strength and muscle cross‐sectional area. Implications for training. Sports medicine. Jul‐Aug 1984;1(4):263–269 [DOI] [PubMed] [Google Scholar]
- 25.Akagi R, Takai Y, Kato E, et al. Relationships between muscle strength and indices of muscle cross‐sectional area determined during maximal voluntary contraction in middle‐aged and elderly individuals. J Strength Cond Res. Jul 2009;23(4):1258–1262 [DOI] [PubMed] [Google Scholar]
- 26.Ahtiainen JP, Hoffren M, Hulmi JJ, et al. Panoramic ultrasonography is a valid method to measure changes in skeletal muscle cross‐sectional area. Eur J Appl Physiol. Jan 2010;108(2):273–279 [DOI] [PubMed] [Google Scholar]
- 27.Juul‐Kristensen B, Bojsen‐Moller F, Holst E, Ekdahl C. Comparison of muscle sizes and moment arms of two rotator cuff muscles measured by ultrasono‐graphy and magnetic resonance imaging. Eur J Ultrasound. Jun 2000;11(3):161–173 [DOI] [PubMed] [Google Scholar]
- 28.Sipila S, Suominen H. Quantitative ultrasonography of muscle: detection of adaptations to training in elderly women. Archives of physical medicine and rehabilitation. Nov 1996;77(11):1173–1178 [DOI] [PubMed] [Google Scholar]
- 29.Brookham RL, McLean L, Dickerson CR. Construct validity of muscle force tests of the rotator cuff muscles: an electromyographic investigation. Physical therapy. Apr 2010;90(4):572–580 [DOI] [PubMed] [Google Scholar]
- 30.Calis M, Akgun K, Birtane M, Karacan I, Calis H, Tuzun F. Diagnostic values of clinical diagnostic tests in subacromial impingement syndrome. Ann Rheum Dis. Jan 2000;59(1):44–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ure BM, Tiling T, Kirchner R, Rixen D. [Reliability of clinical examination of the shoulder in comparison with arthroscopy. A prospective study]. Der Unfallchirurg. Jul 1993;96(7):382–386 [PubMed] [Google Scholar]
- 32.Malanga GA, Jenp YN, Growney ES, An KN. EMG analysis of shoulder positioning in testing and strengthening the supraspinatus. Medicine and science in sports and exercise. Jun 1996;28(6):661–664 [DOI] [PubMed] [Google Scholar]
- 33.Brenneke SL, Morgan CJ. Evaluation of ultrasonography as a diagnostic technique in the assessment of rotator cuff tendon tears. The American journal of sports medicine. May‐Jun 1992;20(3):287–289 [DOI] [PubMed] [Google Scholar]
- 34.Bryant L, Shnier R, Bryant C, Murrell GA. A comparison of clinical estimation, ultrasonography, magnetic resonance imaging, and arthroscopy in determining the size of rotator cuff tears. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons … [et al.]. May‐Jun 2002;11(3):219–224 [DOI] [PubMed] [Google Scholar]
- 35.Crass JR, Craig EV, Feinberg SB. Ultrasonography of rotator cuff tears: a review of 500 diagnostic studies. J Clin Ultrasound. Jun 1988;16(5):313–327 [DOI] [PubMed] [Google Scholar]
- 36.Iannotti JP, Ciccone J, Buss DD, et al. Accuracy of office‐based ultrasonography of the shoulder for the diagnosis of rotator cuff tears. J Bone Joint Surg Am. Jun 2005;87(6):1305–1311 [DOI] [PubMed] [Google Scholar]
- 37.Roberts CS, Walker JA, 2nd, Seligson D. Diagnostic capabilities of shoulder ultrasonography in the detection of complete and partial rotator cuff tears. American journal of orthopedics. Feb 2001;30(2): 159–162 [PubMed] [Google Scholar]
- 38.Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff. A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am. Apr 2000;82(4):498–504 [PubMed] [Google Scholar]
- 39.Itoi E, Kido T, Sano A, Urayama M, Sato K. Which is more useful, the “full can test” or the “empty can test,” in detecting the torn supraspinatus tendon? The American journal of sports medicine. Jan‐Feb 1999;27(1):65–68 [DOI] [PubMed] [Google Scholar]
- 40.Worrell TW, Corey BJ, York SL, Santiestaban J. An analysis of supraspinatus EMG activity and shoulder isometric force development. Medicine and science in sports and exercise. Jul 1992;24(7):744–748 [PubMed] [Google Scholar]
- 41.Hertel R, Lambert SM. Supraspinatus rupture at the musculotendinous junction. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons … [et al.]. Jul‐Aug 1998;7(4):432–435 [DOI] [PubMed] [Google Scholar]
- 42.Masuda K, Kikuhara N, Takahashi H, Yamanaka K. The relationship between muscle cross‐sectional area and strength in various isokinetic movements among soccer players. J Sports Sci. Oct 2003;21(10):851–858 [DOI] [PubMed] [Google Scholar]
- 43.Maughan RJ, Watson JS, Weir J. Strength and cross‐sectional area of human skeletal muscle. J Physiol. May 1983;338:37–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maughan RJ, Watson JS, Weir J. Muscle strength and cross‐sectional area in man: a comparison of strength‐trained and untrained subjects. British journal of sports medicine. Sep 1984;18(3):149–157 [DOI] [PMC free article] [PubMed] [Google Scholar]