Abstract
The burden of mental illness is profound and growing. Coupled with large gaps in extant psychiatric services, this mental health burden has often forced emergency departments (EDs) to become the de facto primary and acute care provider of mental health care in the United States. An expanded emergency medical and mental health research agenda is required to meet the need for improved education, screening, surveillance, and ED-initiated interventions for mental health problems. As an increasing fraction of undiagnosed and untreated psychiatric patients passes through the revolving doors of U.S. EDs, the opportunities for improving the art and science of acute mental health care have never been greater. These opportunities span macroepidemiologic surveillance research to intervention studies with individual patients. Feasible screening, intervention, and referral programs for mental health patients presenting to general EDs are needed. Additional research is needed to improve the quality of care, including the attitudes, abilities, interests, and virtues of ED providers. Research that optimizes provider education and training can help academic settings validate psychosocial issues as core components and responsibilities of emergency medicine. Transdisciplinary research with federal partners and investigators in neuropsychiatry and related fields can improve the mechanistic understanding of acute mental health problems. To have lasting impact, however, advances in ED mental health care must be translated into real-world policies and sustainable program enhancements to assure the uptake of best practices for ED screening, treatment, and management of mental disorders and psychosocial problems.
Keywords: mental health, emergency medicine, psychiatry, psychobehavioral emergencies, consensus conference
The burden of mental illness is profound and growing.1,2 Psychiatric disorders rank second only to cardiovascular disease as a leading cause of lost productivity in the United States.3,4 Each year, almost one in three adults in the noninstitutionalized community has a diagnosable mental or addictive disorder,1,5 and this figure climbs to approximately 40% among ED patients.6 Mental disorders are the fastest growing component of emergency medical practice.3,7–12 In 2006, 4.7 million patients presented to American EDs with a primary psychiatric diagnosis, a rate of approximately 20 visits per 100 adults.13 The Emergency Medical Treatment and Active Labor Act (EMTALA) legislation and mental health insurance carveouts, as well as changes in the mental health infrastructure including fewer psychiatric inpatient beds, fewer psychiatrists, and deinstitutionalization, mean that EDs have become the de facto primary and acute care providers for mental health patients in the United States.7,14–16 While many of those who present to EDs with mental health problems are uninsured, underinsured, homeless, and of racial and ethnic minorities who have no easy access to health care, the largest increase in mental health visits in the past decade comes from those who are insured.3 As the health care system becomes inaccessible to an increasing fraction of the American population, the 15% increase in ED psychiatric visits observed between 1992 and 2001 will likely rise still further.3,17,18
As a result of these trends, emergency medicine (EM) is being forced to assume an increasing responsibility for providing both primary and acute mental health care.3,7,17,19 Indeed, from substance abuse to suicide attempts, EM has long provided expertise in the art and science of clinical toxicology and acute psychiatric stabilization.17,20,21 Recent fragmentation in psychiatric and primary care services, however, suggests that emergency physicians (EPs) must increase their psychosocial research armamentarium if they are to meaningfully improve EM practice.15 To this end, a research agenda is needed. This article addresses this need by reviewing trends in the psychoepidemiology of U.S. ED visits, advocating for increased resources for EM-based mental health research and training, and developing recommendations for an improved behavioral science/EM research agenda that promotes screening, surveillance, best practice guidelines, and ED-initiated interventions for the acute management of mental health problems.
EPIDEMIOLOGY
Overall, from 1992 to 2001, 53 million visits to U.S. EDs were made primarily for mental health–related reasons.3 The most prevalent diagnoses were substance-related disorders (30%), mood disorders (23%), and anxiety disorders (21%).3,8 Psychoses constituted 10%, and suicide attempts 7%, of all documented mental health–related visits.7,9 Rates of presentation to EDs for the most serious mental health problem (suicidal behavior) increased almost 50% from 1992 to 2001, and this trend shows no sign of declining.7 As well as suicidal behavior, increased rates of visits were significant for all of the most prevalent disorders (mood, substance use, and anxiety disorders), but not for psychoses, which may reflect the results of recent substantial investment in early intervention and intensive case management in this field.9
These five major classifications of disorders (mood/substance/anxiety/suicide/psychoses) accounted for almost 80% of all mental health–related ED visits.3 In addition, a significant fraction of those who present to EDs for non–mental health reasons may have occult or silent mental health problems, often neither inquired about nor detected in the ED. It has been estimated that as many as one-third of ED patients have silent or frank depression, and up to 13% have frank or occult suicidal ideation.22 The true number of visits for mental health reasons may be far higher than these estimates, because a substantial fraction of visits are currently coded as “ill-defined conditions,”3 and patients commonly present to EDs for physical conditions with undetected or unrecorded anxiety and depressive symptoms.8,23 Other mental health conditions seen in ED patients, but less commonly diagnosed, include posttraumatic stress disorder (PTSD), conduct disorder, antisocial personality disorder, antisocial behavior, borderline personality disorder, somatization, conversion, Munchausen's syndrome, factitious disorders, and hypochondriasis. Dual diagnoses are common in ED patients (for example, depression and substance abuse,24 psychosis and substance abuse,25 and PTSD and depression26), and such patients tend to have higher levels of severity of both mental health and social problems, to be more difficult to treat, and to be frequent users of EDs.27,28
These epidemiologic data suggest that mental health patients are the fastest growing group of ED patients and reflect EM's increasing burden of responsibility for their care. Of critical importance is that fact that there are approximately 4,000 general EDs in the United States (American Hospitals Association, personal communication, 2009), but only 146 psychiatric EDs (American Association for Emergency Psychiatry, personal communication, 2009). Based on these figures, any initiatives designed to screen for mental health problems, engage patients, and initiate treatment must focus on solutions that will be feasible in busy, general hospital EDs. To date, traditional models of outpatient psychiatric care have failed. New models of psychiatric care that are appropriate, feasible, and sustainable in increasingly busy, pressured, and underresourced EDs are needed. Moreover, given increased volumes of patients and costs of care, ED mental health solutions must decrease crowding and lower recidivism and be cost-effective. We set out below a series of recommendations for a research and development agenda to address the needs and realities of 21st-century acute mental health care in U.S. EDs.
SURVEILLANCE
Emergency medicine offers unique prospects for conducting surveillance studies relevant to a range of mental health issues. While untimely, the Centers for Disease Control and Prevention National Violent Death Reporting System, state and national databases,24,29 large data registries such as the Health Care Cost and Utilization Project, and the National Hospital Ambulatory Medical Care are available to EM researchers to monitor trends in ED and emergency medical services (EMS) care of mental health patients.3,30,31 In disasters and terrorist attacks, EDs are a central data capture site for individuals likely to be most at risk of developing mental health problems.32 Geospatial mapping can be employed to detect clusters of suicide attempts and of suicides from ED admission data. The ED also provides exclusive opportunities to monitor the incidence, clinical effects, and impact of both therapeutic drugs and drugs of abuse. While illicit and prescription drug abuse is an ever-changing scene, users of these substances who suffer from drug-induced illness often seek care in an ED, rendering EDs sentinel sites for observing changes in street and leisure drugs.33 Studies of both prescribed and illicit drug use may be conducted collaboratively by ED toxicologists working with regional and national poison control centers, and databases such as the national Toxic Exposure Surveillance System and the Researched Abuse, Diversion, and Addiction Related Surveillance system.21,34,35
Emergency departments are potentially important sites at which to establish mental health registries. Multisite, state, and national psychiatric registries could encourage: standardization of screening and diagnosis of mental health problems in ED patients; monitor the changing epidemiology of ED mental health presentations; provide more timely data capture; facilitate interdisciplinary research efforts; monitor mental health high users of ED services, track substance abusing and substance seeking patients; and legitimize and facilitate efforts to engage ED staff in screening, intervention, and referral of psychiatric patients to treatment. Models for such registries exist for cancer and for cardiovascular disease, and the feasibility of developing multisite ED registries explicitly for suicide attempt patients is currently being explored in the Department of Veterans Affairs hospitals and other sites.
Recommendation 1: Establish the burden of illness and track prevalence of comorbid mental health and substance abuse problems in patients presenting to general EDs. Integrate ED data systems with other data sources, including poison centers, vital statistics, EMS, and other federal and state records systems.
SCREENING
Patients with mental health problems may present to EDs with psychiatric problems as their primary complaint. However, many present with chief complaints of medical problems, injury or trauma, somatic complaints, psychosocial problems, or behavioral problems. Mental health problems may be obvious and frankly admitted by some patients but occult, denied, undiagnosed, or underdiagnosed in others. ED patients are not routinely screened for mental health problems. Research studies that have screened for psychiatric disorders find that up to one-half of ED patients may have a substance use disorder,36 more than one-third may meet diagnostic criteria for depression,12 and 13% may have occult suicidal ideation.22
The goals of ED screening for mental health problems would be to identify patients with mental health or substance use disorders that require psychiatric treatment or psychosocial support, that might compromise treatment of medical conditions, or that mean that the patient cannot safely be discharged. No mental health screening tool is currently widely accepted or recommended for ED use. In contrast, a 20-year-long, multi-million dollar investment in developing ED-based screening instruments for hazardous alcohol use has resulted in a suite of well-established, widely used tools such as Alcohol Use Disorders Identification Test (AUDIT), Alcohol, Smoking and Substance Involvement Screening Test (ASSIST), and Drug Abuse Screening Test (DAST).37,38 The use of these tools can be extrapolated more broadly to screen for mental health problems, including, in particular, depression, anxiety, and suicide. However, EDs demand pragmatic solutions: screening instruments in the ED must be not only brief, easily understood by patients, available in multiple languages, readily administered in busy general hospital settings, and capable of generating rapidly available responses for review by ED staff, but also able to detect, with a minimum of questions, a range of mental health problems in the patient groups outlined above.
A series of candidate broad mental health and specific depression and suicide screening tools exist that could be used, abbreviated, and / or adapted for use with adolescent, adult, and elder populations.12,39–56 In considering how these tools might be modified and used in the ED setting, there are a number of issues to be considered: the minimum questions required to optimally screen for mental health problems; the mode of questioning to best elicit valid responses to sensitive questions; the methods of screening that are feasible, acceptable to staff and patients, and cost-effective; ways to convey screening results to clinicians so that appropriate referrals and care are instituted; and the extent to which screening generates risk-stratified results that assist physician decision-making for referral and disposition. Cost-benefit analyses are required to determine the extent to which investment in screening and subsequent referral for psychiatric treatment or psychosocial support reduce both morbidity and repeat ED visits.37,57
Recommendation 2: Develop a brief, feasible, acceptable, and cost-effective screening / case-finding program for mental health problems for patients presenting to general EDs. Examine scalability and applicability to young, old, and special populations.
INTERVENTIONS
Emergency department management of patients with mental health problems has tended to follow a traditional model based on referral to psychiatric ED, inpatient, or outpatient services. However, changes in mental health infrastructure mean that this model is outmoded. There are now compelling reasons to conduct or initiate interventions in the ED to address some fraction of identified mental health problems, overcome problems of poor patient engagement and adherence with outpatient care, reduce imminent risk of death (for suicidal patients), and capitalize on a “teachable moment” or a possible “window of opportunity.”58 Effective ED interventions could minimize subsequent repeat visits to overcrowded EDs.
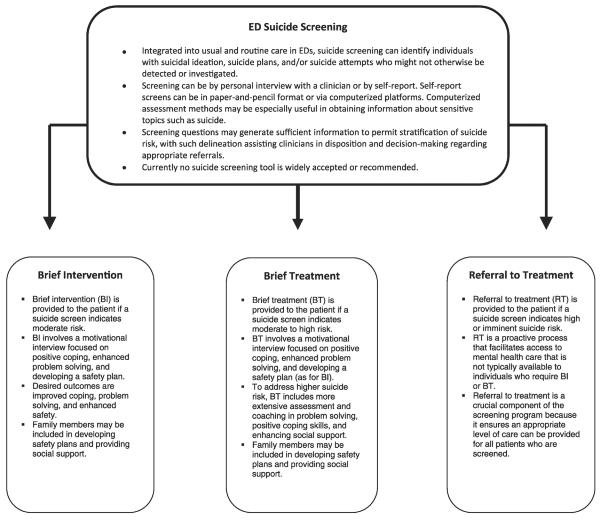
However, there are few evidence-based ED interventions for mental health patients. The experiences of ED-based practitioners in developing and delivering brief interventions (BIs) for patients with substance use disorders provides a model for the development of similar interventions for people with mental health problems. ED staff have been trained to screen quickly for the presence and extent of hazardous substance use and to deliver BIs using motivational interviewing techniques to increase patient awareness and motivation to change their substance use behaviors. Staff are also trained to deliver brief treatments that involve a more comprehensive approach than BI alone, incorporating assessment and patient education, teaching problem solving and coping skills, and encouraging the patient to develop a supportive social environment. In addition to BIs and treatments, ED staff facilitate patient referrals to longer-term care and social support. This approach has been effective in reducing hazardous alcohol, heroin, and cocaine use and tobacco smoking, justifying trials of similar strategies for mental health problems.36,37,59–61 To illustrate the potential transferability of this approach, we adapted the screening, brief intervention, and referral to treatment (SBIRT) model and applied it (theoretically) to an expanded SBIRT for suicidal behavior (Figure 1).
Figure 1.
Expanded screening, brief intervention, brief treatment, and referral to treatment for suicide risk. Adapted from: http://www.sbirt.samhsa.gov/care_comp/index.htm.
In addition to the SBIRT model, research is needed to develop, deliver, and evaluate a series of promising psychotherapeutic interventions and treatments for subgroups of mental health patients. A number of these interventions may be delivered or initiated in ED settings by clinicians. Table 1 lists candidate interventions using suicidal behavior as an example,62–65 because suicidal behavior has potentially the most serious outcome of ED mental health presentations.
Table 1.
Promising Psychotherapeutic Interventions for ED Patients With Mental Health Problems
| Psychopharmacology |
| Safety plans |
| Cognitive behavioral therapy (CBT)—individual, family62 |
| Home-based family intervention |
| Group therapy |
| Dialectical behavioral therapy (DBT) |
| Multisystemic therapy (MST) |
| Combination of medication and CBT |
| Increasing social support networks63 |
| Intensive case management |
| Chain of care–linked services |
| Postcards or “friendly lette”64 |
| Telephone follow-up65 |
| Restricting access to means of harm |
| Problem solving therapy (PST), coping skills, self-soothing skills |
| Social work support |
| Sitters, minders |
In addition to being a novel setting in which to conduct brief, tailored, psychosocial intervention research, the ED is also an ideal location to study brief psychopharmacologic interventions for mood states and psychosis. New, long-acting neuroleptics and even rapid-onset antidepressants can ideally be studied in the ED setting. For example, Zarate and colleagues66 have demonstrated robust and rapid (within 2 hours) antidepressant effects of a single dose of ketamine (0.5 mg / kg, IV infusion over 40 minutes), which was sustained in refractory depression patients for over 1 week. Beyond ketamine, the number of candidate psychopharmacologic compounds worthy of ED study could occupy an entire research career.
Mental health interfaces with EM for a series of special populations including immigrants, the homeless, those with serious mental illness, adolescents, and elders. We discuss one group here—adolescents—to illustrate the ways in which the ED provides a unique opportunity to intervene with a vulnerable group. Adolescents present to EDs with a wide range of mental health and substance abuse problems, perhaps reflecting the fact that adolescents often do not seek mental health services on their own until a crisis arises. Many adolescents seen in the ED do not have regular contact with primary care providers67 and are thus less likely to receive either intervention or prevention services. The salience of an alcohol-related event may increase an adolescent's sense of vulnerability and thereby increase receptivity to an intervention. Because a parent often accompanies a teen to the ED, the ED also represents a situation in which parents may be engaged and encouraged to take steps to better address their teen's mental health and substance use issues.
The ED is the most common site for the evaluation and treatment of adolescents with medically serious suicide attempts.68 The primary task for the EP evaluating a suicidal adolescent is to assess current emotional / behavioral status, which in turn helps determine the appropriate discharge disposition.69,70 Empirical guidelines for making clinical determinations are not standardized, and clinical research addressing this area is needed. For example, algorithms for disposition decisions based on adolescent measures of current state and parent measures of psychiatric history might be tested and disseminated.
Once the decision has been made to discharge a suicidal adolescent to outpatient care, the EP must be cognizant of the fact that follow-through with outpatient treatment is problematic.71 None of the approaches thus far (crisis interventions, postdischarge phone calls, motivating families) have been shown to definitively improve follow-through with outpatient care. Studies examining the coordination of ED care and community mental health clinic care are sorely needed, given that the breakdown in follow-through with outpatient care often occurs at a systems level.72
The prevalence estimate for adolescents with a positive blood alcohol level being treated in the ED is approximately 5%.73 Research designed to better understand which interventions are indicated based on ED presentation and history, as well as the best way to deliver these interventions, is necessary.73 In addition, studies designed to see whether these interventions can be delivered effectively by health care professionals, rather than research staff, will also be important in future research.
Recommendation 3: Develop feasible, acceptable, and cost-effective ED-initiated interventions for patients with mental health problems that enhance mental health service linkages, as well as improve patient safety and self-management skills; increase adherence to medical treatments, recommendations, and appointment-keeping; and minimize ED recidivism.
WORKFORCE ENRICHMENT/EDUCATION
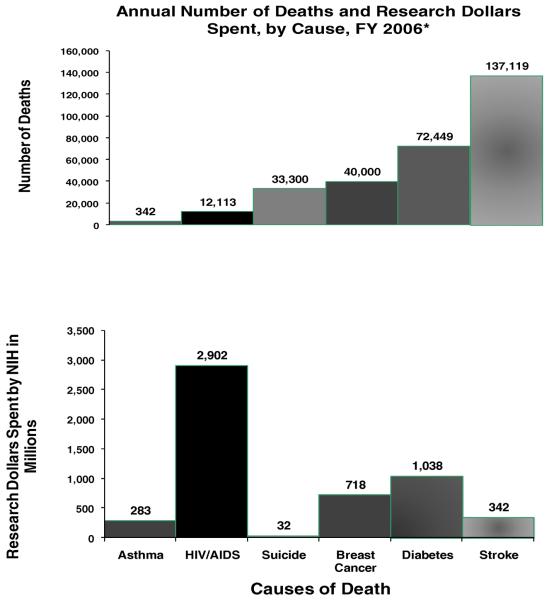
Despite EDs becoming an increasingly common site for psychiatric disorders to first present to health care professionals, these disorders are often undetected, in part due to a lack of appreciation by staff. Indeed, EM residencies offer minimal formal education in the diagnosis and management of mental illness.74 Currently neither the Accreditation Council for Graduate Medical Education (ACGME) nor the American Board of Emergency Medicine specifies a well-defined core curriculum relating to psychiatric disorders, and the core content dedicated to mental health is incommensurate with the large volume of psychiatric-related ED visits occurring annually (Figure 2). A 2003 survey of North American EM program directors found that 67% did not require their residents to undertake, nor provided, formal training in treating acute psychiatric emergencies.75
Figure 2.
Comparison of mortality, and research funding, by cause of death. National Center for Health Statistics (NCHS), National Vital Statistics System. *http://www.nih.gov/news/fundingresearchareas.htm#1.
Emergency medicine curricula would be improved by more formal teaching about psychopharmacology, mood disorders and suicidal behavior, substance abuse, and the safe use of chemical and physical restraints for dangerously agitated patients.76 Applying the ACGME core competencies (patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice) to an expanded psychiatric portion of the EM residency curriculum would further validate its place as core content.77 In addition, the development of emergency psychiatry fellowships for EM-trained physicians is both logical and practical.
Psychiatric patients often are regarded by health care staff as difficult to treat, and staff report that they do not enjoy treating them.78,79 Negative attitudes toward patients and their detrimental impact on patient care have been recognized for decades.80 Careful selection and education of students, residents, and physicians, and attention to staff “burnout,” could both reduce stigmatization and ensure provision of professional and compassionate care. Research is needed to explore the extent to which selecting and training residents and other ED providers specifically for attitudes, abilities, interests, and virtues that are sympathetic to patients with mental health issues can enhance identification of mental health problems and result in more professional, compassionate care and attention to patients' psychiatric and psychosocial issues. Similar research is needed to assess the impact on patient care of promoting ED provider virtues outlined in the American College of Emergency Physicians Code of Ethics (prudence, courage, justice, vigilance, unconditional positive regard, charity, trustworthiness, and resilience).81 The use of simulation as both a research and a training tool could be leveraged to promote new pedagogic advances in training EM residents in the care of the mentally unwell.
Recommendation 4: Develop and evaluate core educational programs for medical students and EM residents and physicians that validate career selection and the incorporation of mental/psychosocial issues as core components and responsibilities of EPs. Study educational simulation, communication science, and training initiatives that ensure providers recognize and treat mental health patients with competence, professionalism, sensitivity, and compassion.
RESEARCH FUNDING AND INFRASTRUCTURE
Mental health research in the ED faces several barriers. Mental health research in general is underfunded relative to the annual burden of deaths (Figure 2) and underfunded specifically in ED research relative to the ED burden of cardiopulmonary arrest, trauma, chest pain, and pneumonia. In addition, EM has traditionally been reluctant to embrace mental health in either research or education. Further, these vulnerable psychiatric patients are not readily able to advocate for themselves and their own health care needs. To overcome these challenges, an adequately funded research agenda for EM and mental health research is required. In addition to the specific research proposals and agenda outlined in this paper, increased EM researcher networking with EM peers (including mental health, public health, and injury prevention researchers), and the establishment of ED-based research networks are needed to address ED-relevant policy-level mental health issues. Opportunities to work with federal mental health partners regarding grants and study sections are needed. Increased collaboration between departments of EM and psychiatry, increased EM research focus on mental health topics, and increased funding for this work from an institutional to the federal level could all help ultimately to provide better patient care.
Recommendation 5: Increase quality of EM mental health research training, and increase EM researcher networking with EM peers and with federal mental health partners, behavioral science researchers, neuroscientists, and psychiatrists. Develop more formal EM and mental health research fellowships. Advocate for enhanced research funding and support locally and nationally.
RESEARCH TO PRACTICE
The most well-funded and carefully executed research program amounts to relatively little if the fruits of such academic labor are not translated into improvement in policy and practice. The science of knowledge translation informs this process of evidence uptake and includes attending to the goals and values of a wide range of interested stakeholders (Table 2).82 Particular attention needs to be paid to advocating for mental health research, screening, and intervention to be incorporated and funded as part of EM. Research programs in EM mental health need to be conducted in parallel with education, training, and continuing audits at both local and national levels to generate and inform evidence-based practice. Researchers must promote feasible and cost-effective solutions and be responsible stewards of resources. The most elegant solutions will never change practice if they are not feasible in the real world. Indeed, getting evidence used is as important as its generation, a critical link in the EM and behavioral health research agenda.
Table 2.
Stakeholders in Mental Health Knowledge Translation in EM
| Patients and parents/families |
| Providers and provider groups |
| Peers and peer networks |
| Professional organizations |
| Public health/public schools |
| Policy makers/politicians |
| Payers/insurers |
| Private sector/nongovernmental organizations/private schools |
| Press/mass media/radio/television/Internet |
| Populace/general public |
Recommendation 6: Increase the interface between EM, mental health, public health, and injury prevention researchers to address ED-relevant policy-level mental health issues. Enhance knowledge translation and uptake of best practices for ED screening, interventions, and management of mental disorders and psychosocial issues among all stakeholders (including patients, providers, funders, researchers).
CONCLUSIONS
The intersection of EM and acute mental health provides opportunities for researchers and clinicians to develop effective interventions, education and training, policies, and programs for a vulnerable and challenging population. Recent developments in research methodology (improved statistical methods and information systems, geospatial mapping tools, the capacity to conduct large multisite studies), advances in biologic science, psychopharmacology, the behavioral social sciences, and the promise of pharmacogenomics offer unparalleled opportunities to advance acute mental health care in ED settings. The research agenda and recommendations (Table 3) addressing these issues range from macro-level screening, to individual level application of new therapeutics and novel health care–based psychosocial interventions, and should be conducted in parallel with efforts to generate a body of best practices for ED-based acute psychiatric care.
Table 3.
Mental Health and EM: Summary of Recommendations
| Priority Areas | Recommendations |
|---|---|
| 1. Surveillance | Establish the burden of illness and track prevalence of comorbid mental health problems in patients presenting to general EDs. Integrate ED data systems with other data sources, including poison centers, vital statistics, EMS, and other federal and state records systems. |
| 2. Screening | Develop a brief, feasible, acceptable, and cost-effective screening program for mental health problems for patients presenting to general EDs, and encourage consistent national use. Examine scalability and applicability to young, elder, and special populations. |
| 3. Interventions | Develop feasible, acceptable, and cost-effective ED-initiated interventions for patients with mental health problems that enhance patient safety, self-management skills, adherence to medical treatments, recommendations, and appointment-keeping and minimize recidivism. Improve ED-based mental health disposition and referral practices and processes that expand access, enhance service linkages, and reduce ED recidivism. |
| 4. Workforce | Develop and evaluate core educational programs for medical students and EM residents and physicians that validate career selection and mental/psychosocial issues as core components and responsibilities of EPs. Impart training that ensures providers communicate optimally, treating mental health patients with professionalism, sensitivity, and compassion. |
| 5. Research infrastructure | Increase quality of EM mental health research training, and increase EM researcher networking with EM peers and with federal mental health partners, behavioral science researchers, neuroscientists, and psychiatrists regarding grants and study sections. Develop EM and mental health research fellowships. Advocate for enhanced research funding and support locally and nationally |
| 6. Knowledge translation | Increase the interface between EM, mental health, public health, and injury prevention researchers to address ED-relevant policy-level mental health issues; enhance knowledge translation and uptake of best practices for ED screening, interventions, and management of mental disorders and psychosocial issues among all stakeholders (including patients, providers, funders, researchers). |
References
- 1.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 2.Murray C, Lopez A. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability From Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Vol 1. Harvard University Press; Boston, MA: 1996. [Google Scholar]
- 3.Larkin GL, Claassen CA, Emond JA, Pelletier AJ, Camargo CA., Jr. Trends in U.S. emergency department visits for mental health conditions, 1992 to 2001. Psychiatr Serv. 2005;56:671–7. doi: 10.1176/appi.ps.56.6.671. [DOI] [PubMed] [Google Scholar]
- 4.Kunen S, Niederhauser R, Smith PO, Morris JA, Marx BD. Race disparities in psychiatric rates in emergency departments. J Consult Clin Psychol. 2005;73:116–26. doi: 10.1037/0022-006X.73.1.116. [DOI] [PubMed] [Google Scholar]
- 5.Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK. The de facto US mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993;50:85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- 6.Marchesi C, Brusamonti E, Giannini A, et al. Psychiatric disorders in patients admitted to emergency department wards. Stress Health. 2001;17:47–53. [Google Scholar]
- 7.Larkin GL, Smith RP, Beautrais AL. Trends in US emergency department visits for suicide attempts, 1992–2001. Crisis. 2008;29:73–80. doi: 10.1027/0227-5910.29.2.73. [DOI] [PubMed] [Google Scholar]
- 8.Smith RP, Larkin GL, Southwick SM. Trends in U.S. emergency department visits for anxiety-related mental health conditions, 1992–2001. J Clin Psychiatry. 2008;69:286–94. doi: 10.4088/jcp.v69n0215. [DOI] [PubMed] [Google Scholar]
- 9.Pandya A, Larkin G, Randles R, Beautrais A, Smith RP. Epidemiological trends in psychosis-related emergency department visits in the United States, 1992–2001. Schizophr Res. 2009;110:28–32. doi: 10.1016/j.schres.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 10.Hazlett SB, McCarthy ML, Londner MS, Onyike CU. Epidemiology of adult psychiatric visits to US emergency departments. Acad Emerg Med. 2004;11:193–5. [PubMed] [Google Scholar]
- 11.Walsh P, Currier G, Shah MN, Lyness JM, Friedman B. Psychiatric emergency services for the US elderly: 2008 and beyond. Am J Geriatr Psychiatry. 2008;16:706–17. doi: 10.1097/JGP.0b013e31817e73c7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boudreaux ED, Clark S, Camargo CA., Jr. Mood disorder screening among adult emergency department patients: a multicenter study of prevalence, associations and interest in treatment. Gen Hosp Psychiatry. 2008;30:4–13. doi: 10.1016/j.genhosppsych.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 13.Downey LVA, Zun LS, Gonzales SJ. Utilization of emergency department by psychiatric patients. Prim Psychiatry. 2009;16:60–64. [Google Scholar]
- 14.Norquist GS, Regier DA. The epidemiology of psychiatric disorders and the de facto mental health care system. Annu Rev Med. 1996;47:473–9. doi: 10.1146/annurev.med.47.1.473. [DOI] [PubMed] [Google Scholar]
- 15.IOM Committee on the Future of Emergency Care in the United States Health System . Hospital-Based Emergency Care at the Breaking Point. National Academies Press; Washington, DC: 2007. [Google Scholar]
- 16.Tai-Seale M, McGuire T, Colenda C, Rosen D, Cook MA. Two-minute mental health care for elderly patients: inside primary care visits. J Am Geriatr Soc. 2007;55:1903–11. doi: 10.1111/j.1532-5415.2007.01467.x. [DOI] [PubMed] [Google Scholar]
- 17.Kreismann E, Gang M, Goldfrank LR. The interface: ethical decision making, medical toxicology, and emergency medicine. Emerg Med Clin North Am. 2006;24:769–84. doi: 10.1016/j.emc.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 18.Rhodes KV, Vieth TL, Kushner H, Levy H, Asplin BR. Referral without access: for psychiatric services, wait for the beep. Ann Emerg Med. 2008;54:272–8. doi: 10.1016/j.annemergmed.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 19.Zink BJ. Anyone, Anything, Anytime: A History of Emergency Medicine. Elsevier Mosby; Philadelphia, PA: 2006. [Google Scholar]
- 20.Goldfrank L. Emergency medicine and medical toxicology: past, present and future: A very personal view. Keynote address. Isr J Emerg Med. 2005;5:10–15. [Google Scholar]
- 21.Hughes AA, Bogdan GM, Dart RC. Active surveillance of abused and misused prescription opioids using poison center data: a pilot study and descriptive comparison. Clin Toxicol (Phila) 2007;45:144–51. doi: 10.1080/15563650600981137. [DOI] [PubMed] [Google Scholar]
- 22.Claassen CA, Larkin GL. Occult suicidality in an emergency department population. Br J Psychiatry. 2005;186:352–3. doi: 10.1192/bjp.186.4.352. [DOI] [PubMed] [Google Scholar]
- 23.Currier GW, Allen M. Organization and function of academic psychiatric emergency services. Gen Hosp Psychiatry. 2003;25:124–9. doi: 10.1016/s0163-8343(02)00287-6. [DOI] [PubMed] [Google Scholar]
- 24.The New DAWN Report. Emergency department visits involving patients with co-occurring disorders. 2006;15:1–4. [Google Scholar]
- 25.Schanzer BM, First MB, Dominguez B, Hasin DS, Caton CLM. Diagnosing psychotic disorders in the emergency department in the context of substanceuse. Psychiatr Serv. 2006;57:1468–73. doi: 10.1176/ps.2006.57.10.1468. [DOI] [PubMed] [Google Scholar]
- 26.Lipsky S, Field CA, Caetano R, Larkin GL. Posttraumatic stress disorder symptomatology and comorbid depressive symptoms among abused women referred from emergency department care. Violence Vict. 2005;20:645–59. [PubMed] [Google Scholar]
- 27.Lejoyeux M, Boulenguiez S, Fichelle A, McLoughlin M, Claudon M, Adès J. Alcohol dependence among patients admitted to psychiatric emergency services. Gen Hosp Psychiatry. 2000;22:206–12. doi: 10.1016/s0163-8343(00)00056-6. [DOI] [PubMed] [Google Scholar]
- 28.Curran GM, Sullivan G, Williams K, et al. Emergency department use of persons with comorbid psychiatric and substance abuse disorders. Ann Emerg Med. 2003;41:659–67. doi: 10.1067/mem.2003.154. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention Surveillance for Violent Deaths– National Violent Death Reporting System, 16 States, 2005. MMWR Surv Summ. 2008;57(SS03):1–45. [PubMed] [Google Scholar]
- 30.McCaig LF, Nawar EW. National Hospital Ambulatory Medical Care Survey: 2004 emergency department summary. Adv Data. 2006;372:1–29. [PubMed] [Google Scholar]
- 31.Larkin GL, Claassen CA, Pelletier AJ, Camargo CA., Jr. National study of ambulance transports to United States emergency departments: importance of mental health problems. Prehosp Disaster Med. 2006;21(2 Suppl 2):82–90. doi: 10.1017/s1049023x0000340x. [DOI] [PubMed] [Google Scholar]
- 32.Larkin GL. Ethical issues in emergency and disaster medicine. Lijec Vjesn. 2007;129(Suppl 5):107–18. [PubMed] [Google Scholar]
- 33.National Institute on Drug Abuse. National Institutes of Health. U.S. Department of Health and Human Services [Accessed Aug 9, 2009];Hospital Visits: NIDA. 2005 Available at: http://www.drugabuse.gov/pdf/infofacts/HospitalVisits08.pdf.
- 34.Cicero TJ, Dart RC, Inciardi JA, Woody GE, Schnoll S, Munoz A. The development of a comprehensive risk-management program for prescription opioid analgesics: researched abuse, diversion and addiction-related surveillance (RADARS) Pain Med. 2007;8:157–70. doi: 10.1111/j.1526-4637.2006.00259.x. [DOI] [PubMed] [Google Scholar]
- 35.Hoffman RS, Kirrane BM, Marcus SM. A descriptive study of an outbreak of clenbuterol-containing heroin. Ann Emerg Med. 2008;52:548–53. doi: 10.1016/j.annemergmed.2008.04.026. [DOI] [PubMed] [Google Scholar]
- 36.D'Onofrio G, Degutis LC. Screening and brief intervention in the emergency department. Alcohol Res Health. 2004;28:63–72. 2004–2005. [PMC free article] [PubMed] [Google Scholar]
- 37.Academic ED SBIRT Collaborative. Bernstein E, Bernstein J, et al. An evidence based alcohol screening, brief intervention and referral to treatment (SBIRT) curriculum for emergency department (ED) providers improves skills and utilization. Subst Abus. 2007;28:79–92. doi: 10.1300/J465v28n04_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Babor TF. We shape our tools, and thereafter our tools shape us: psychiatric epidemiology and the alcohol dependence syndrome concept. Addiction. 2007;102:1534–5. doi: 10.1111/j.1360-0443.2007.01990.x. [DOI] [PubMed] [Google Scholar]
- 39.Asarnow JR, Emslie G, Clarke G, et al. Treatment of selective serotonin reuptake inhibitor-resistant depression in adolescents: predictors and moderators of treatment response. J Am Acad Child Adolesc Psychiatry. 2009;48:330–9. doi: 10.1097/CHI.0b013e3181977476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brown GK. [Accessed Mar 19 2009];A review of suicide assessment measures for intervention research with adults and older adults. Available at: http://sbisrvntweb.uqac.ca/archivage/15290520.pdf.
- 41.Cooper J, Kapur N, Dunning J, Guthrie E, Appleby L, Mackway-Jones K. A clinical tool for assessing risk after self-harm. Ann Emerg Med. 2006;48:459–66. doi: 10.1016/j.annemergmed.2006.07.944. [DOI] [PubMed] [Google Scholar]
- 42.Copelan RI, Messer MA, Ashley DJ. Adolescent violence screening in the ED. Am J Emerg Med. 2006;24:582–94. doi: 10.1016/j.ajem.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 43.Folse VN, Eich KN, Hall AM, Ruppman JB. Detecting suicide risk in adolescents and adults in an emergency department: a pilot study. J Psychosoc Nurs Ment Health Serv. 2006;44:22–9. doi: 10.3928/02793695-20060301-08. [DOI] [PubMed] [Google Scholar]
- 44.Healy DJ, Barry K, Blow F, Welsh D, Milner KK. Routine use of the Beck Scale for Suicide Ideation in a psychiatric emergency department. Gen Hosp Psychiatry. 2006;28:323–9. doi: 10.1016/j.genhosppsych.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 45.Horowitz LM, Wang PS, Koocher GP, et al. Detecting suicide risk in a pediatric emergency department: development of a brief screening tool. Pediatrics. 2001;107:1133–7. doi: 10.1542/peds.107.5.1133. [DOI] [PubMed] [Google Scholar]
- 46.Larzelere RE, Andersen JJ, Ringle JL, Jorgensen DD. The child suicide risk assessment: a screening measure of suicide risk in pre-adolescents. Death Stud. 2004;28:809–27. doi: 10.1080/07481180490490861. [DOI] [PubMed] [Google Scholar]
- 47.Meneese WB, Yutrzenka BA. Correlates of suicidal ideation among rural adolescents. Suicide Life Threat Behav. 1990;20:206–12. [PubMed] [Google Scholar]
- 48.New South Wales Department of Health [Accessed Aug 9, 2009];Framework for suicide risk assessment and management for New South Wales health staff. Available at: http://www.health.nsw.gov.au/pubs/2005/pdf/suicide_risk.pdf.
- 49.Olfson M, Weissman MM, Leon AC, Sheehan DV, Farber L. Suicidal ideation in primary care. J Gen Intern Med. 1996;11:447–53. doi: 10.1007/BF02599038. [DOI] [PubMed] [Google Scholar]
- 50.Patel AS, Harrison A, Bruce-Jones W. Evaluation of the risk assessment matrix: a mental health triage tool. Emerg Med J. 2009;26:11–14. doi: 10.1136/emj.2007.058388. [DOI] [PubMed] [Google Scholar]
- 51.Paykel ES, Myers JK, Lindenthal JJ, Tanner J. Suicidal feelings in the general population: a prevalence study. Br J Psychiatry. 1974;124:460–9. doi: 10.1192/bjp.124.5.460. [DOI] [PubMed] [Google Scholar]
- 52.Posner K, Oquendo MA, Gould M, Stanley B, Davies M. Columbia classification algorithm of suicide assessment (C-CASA): classification of suicidal events in the FDA's pediatric suicidal risk analysis of antidepressants. Am J Psychiatry. 2007;164:1035–43. doi: 10.1176/appi.ajp.164.7.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shedler J. The Shedler Quick Diagnostics Panel (QPD Panel): A psychiatric “lab test” for primary care. In: Maruish M, editor. Handbook of Psychological Assessment in Primary Care Settings. Lawrence Erlbaum Associates; Mahwah, NJ: 2000. [Google Scholar]
- 54.Shedler J, Beck A, Bensen S. Practical mental health assessment in primary care: validity and utility of the Quick Diagnostics Panel. J Fam Pract. 2000;49:614–21. [PubMed] [Google Scholar]
- 55.Skoog I, Aevarsson O, Beskow J, et al. Suicidal feelings in a population sample of nondemented 85-year-olds. Am J Psychiatry. 1996;153:1015–20. doi: 10.1176/ajp.153.8.1015. [DOI] [PubMed] [Google Scholar]
- 56.Tishler CL, Reiss NS, Rhodes AR. Suicidal behavior in children younger than twelve: a diagnostic challenge for emergency department personnel. Acad Emerg Med. 2007;14:810–8. doi: 10.1197/j.aem.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 57.Babor T, Higgins-Biddle J, Saunders J, Monteiro M. The Alcohol Use Disorders Identification Test: guidelines for use in primary care. World Health Organization; Geneva: 2001. [Google Scholar]
- 58.Barnett NP, Lebeau-Craven R, O'Leary TA, et al. Predictors of motivation to change after medical treatment for drinking-related events in adolescents. Psychol Addict Behav. 2002;16:106–12. [PubMed] [Google Scholar]
- 59.Bernstein E, Bernstein J, Levenson S. Project ASSERT: an ED-based intervention to increase access to primary care, preventive services, and the substance abuse treatment system. Ann Emerg Med. 1997;30:181–9. doi: 10.1016/s0196-0644(97)70140-9. [DOI] [PubMed] [Google Scholar]
- 60.Bernstein SL, Boudreaux ED, Cydulka RK, et al. Tobacco control interventions in the emergency department: a joint statement of emergency medicine organizations. Ann Emerg Med. 2006;48:e417–26. doi: 10.1016/j.annemergmed.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 61.Academic ED SBIRT Collaborative The impact of screening, brief intervention, and referral for treatment on emergency department patients' alcohol use. Ann Emerg Med. 2007;50:699–710. doi: 10.1016/j.annemergmed.2007.06.486. [DOI] [PubMed] [Google Scholar]
- 62.Brown GK, Ten Have T, Henriques GR, et al. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294:563–70. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- 63.King CA, Kramer A, Preuss L, Kerr DCR, Weisse L, Venkataraman S. Youth-nominated support team for suicidal adolescents (version 1): a randomized controlled trial. J Consulting Clin Psychol. 2006;74:199–206. doi: 10.1037/0022-006X.74.1.199. [DOI] [PubMed] [Google Scholar]
- 64.Carter G, Clover K, Whyte IM, Dawson AH, D'Este C. Postcards from the EDge: 24-month outcomes of a randomised controlled trial for hospital-treated self-poisoning. Br J Psychiatry. 2007;191:548–53. doi: 10.1192/bjp.bp.107.038406. [DOI] [PubMed] [Google Scholar]
- 65.Vaiva G, Vaiva G, Ducrocq F, et al. Effect of telephone contact on further suicide attempts in patients discharged from an emergency department: randomised controlled study. BMJ. 2006;332:1241–5. doi: 10.1136/bmj.332.7552.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zarate CA, Jr, Singh JB, Carlson PJ, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry. 2006;63:856–64. doi: 10.1001/archpsyc.63.8.856. [DOI] [PubMed] [Google Scholar]
- 67.Elixhauser A, Machlin SR, Zodet MW, et al. Health care for children and youth in the United States: 2001 annual report on access, utilization, quality, and expenditures. Ambul Pediatr. 2002;2:419–37. doi: 10.1367/1539-4409(2002)002<0419:hcfcay>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 68.Centers for Disease Control and Prevention Suicide trends among youths and young adults aged 10–24 years–United States, 1990–2004. MMWR Morb Mortal Wkly Rep. 2007;56:905–8. [PubMed] [Google Scholar]
- 69.Spirito A, Monti PM, Barnett NP, et al. A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. J Pediatr. 2004;145:396–402. doi: 10.1016/j.jpeds.2004.04.057. [DOI] [PubMed] [Google Scholar]
- 70.Spirito A, Brown L, Overholser J, Fritz G, Bond A. The use of the Risk-Rescue Scale with adolescents: a cautionary note. Death Stud. 1991;15:269–80. [Google Scholar]
- 71.Boergers J, Spirito A. Follow-up Outcome of Adolescent Suicide Attempters. Cambridge University Press; London, UK: 2003. [Google Scholar]
- 72.Spirito A, Boergers J, Donaldson D, Bishop D, Lewander W. An intervention trial to improve adherence to community treatment by adolescents after a suicide attempt. J Am Acad Child Adolesc Psychiatry. 2002;41:435–42. doi: 10.1097/00004583-200204000-00016. [DOI] [PubMed] [Google Scholar]
- 73.Sindelar HA, Abrantes AM, Hart C, Lewander W, Spirito A. Motivational interviewing in pediatric practice. Curr Probl Pediatr Adolesc Health Care. 2004;34:322–39. doi: 10.1016/j.cppeds.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 74.MacLean TA, Bourgeois JA, Hamilton GC, Kay J. Objectives to direct the training of emergency medicine residents on off-service rotations: psychiatry. J Emerg Med. 1995;13:545–51. doi: 10.1016/0736-4679(95)80019-0. [DOI] [PubMed] [Google Scholar]
- 75.Santucci KA, Sather J, Baker MD. Emergency medicine training programs' educational requirements in the management of psychiatric emergencies: current perspective. Pediatr Emerg Care. 2003;19:154–6. doi: 10.1097/01.pec.0000081235.20228.7a. [DOI] [PubMed] [Google Scholar]
- 76.Lukens TW, Wolf SJ, Edlow JA, et al. Clinical policy: critical issues in the diagnosis and management of the adult psychiatric patient in the emergency department. Ann Emerg Med. 2006;47:79–99. doi: 10.1016/j.annemergmed.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 77.Larkin GL, Iserson K, Kassutto Z, et al. Virtue in emergency medicine. Acad Emerg Med. 2009;16:51–5. doi: 10.1111/j.1553-2712.2008.00315.x. [DOI] [PubMed] [Google Scholar]
- 78.Dressler DM, Prusoff B, Mark HAL, Shapiro D. Clinician attitudes toward the suicide attempter. J Nerv Ment Dis. 1975;160:146–55. doi: 10.1097/00005053-197502000-00009. [DOI] [PubMed] [Google Scholar]
- 79.Goldney RD, Bottrill A. Attitudes to patients who attempt suicide. Med J Aust. 1980;2:717–20. [PubMed] [Google Scholar]
- 80.Friedman T, Newton C, Coggan C, et al. Predictors of A&E staff attitudes to self-harm patients who use self-laceration: influence of previous training and experience. J Psychosom Res. 2006;60:273–7. doi: 10.1016/j.jpsychores.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 81.ACEP Ethics Committee Code of ethics for emergency physicians. Ann Emerg Med. 2008;52:581–90. doi: 10.1016/j.annemergmed.2008.07.041. [DOI] [PubMed] [Google Scholar]
- 82.Larkin GL, Claassen C. Trends in emergency department use of gastric lavage for poisoning events in the United States, 1993–2003. Clin Toxicol (Phila) 2007;45:164–8. doi: 10.1080/15563650601155038. [DOI] [PubMed] [Google Scholar]