Summary
From 1986 to the end of 1998, 482 cases of traumatic carotid-cavernous fistula (TCCF) were treated by means of intravascular embolisation technique. The experience is overviewed in this article.
Many kinds of detachable balloon catheters (including Chinese made detachable balloon catheters), coils and cyano aery late were used as embolic materials. Transcervical, transfemoral, anterior communicating artery, posterior communicating artery approach, or transvenous approach were selected according to conditions. A combination of different approaches or materials was used for complex TCCF.
We found that the special sign, named “bileakage sign”, indicated multileakage of TCCF and was not mentioned before. All 482 cases of TCCF were embolised successfully, of which 405 cases maintained the patency of internal carotid artery (ICA). No death related to the treatment occurred in our group and the symptoms or signs in 462 cases were relieved after embolisation. Emergency embolisation was needed in some conditions such as serious epistaxis, delayed or repeatedly subdural haematoma and rapid visual impairment.
Endovascular treatment of TCCF is a safe and efficient method. The time of operation, approach, and materials for embolisation must be carefully selected in order to obtain the best result.
Key words: carotid-cavernous fistula, embolisation, endovascular treatment
Introduction
Traumatic carotid-cavernous fistula (TCCF) arises from head injury and results in a direct shunt between the internal carotid artery (ICA) and the cavernous sinus, which usually occurs in young men. Symptoms are often abrupt in onset and rapidly progressive, and CCF requires immediate treatment if there is progressive visual impairment, epistaxis or intracranial haemorrhage, etc. The goals of treatment are to eliminate the fistula and maintain the patency of the ICA. The treatment of TCCF has been in continuous and recently rapid evolution. The modern era of endovascular treatment began in 1971, occluding TCCF with non-detachable balloons but requiring the sacrifice of ICA 1. Some authors reported the direct surgical repair of a CCF in 1973 but the operation was technically very difficult2. Detachable balloons had been developed in 1974 and could occluded the fistula and preserve the ICA 3. The detachable balloon catheter has been the predominant method since then. The transvenous technique, embolisation with glue and coils were been developed in recent years to deal with some special situations. It seemed that the technique of treatment of TCCF was flawless, but we found that many special cases were too complex to be treated easily The embolisation of these special cases required abundant experience of intravascular treatment. From 1986 to the end of 1998,482 cases of traumatic carotid-cavernous fistula (TCCF) were treated by means of intravascular embolisation technique. No death related to the embolisation procedures occurred in our group. Self-made detachable balloon catheters, coils and glue were used in this group of cases and good results obtained.
Methods of Treatment
The series comprised 482 patients aged from four to 72 years (mean 30), 368 males and 114 females. The period from injury to hospital admission was from four days to two years. Seven cases were bilateral TCCF.
Catheter and Embolic Material
Many kinds of catheters were used. Most TCCF cases were embolised by balloon catheters (Bait Co. France). In a few cases, Debrun balloon-catheter (Nycomed Co.) and Coaxis system (Cook Co.) were utilized. In 14 cases, Tracker-18 (B.S.C), Transit (Cordis) and Mag 3F/2F catheters were used for injecting coils or glue (cyanoacrylate). In this group, the latex balloon is the most common utilized4,5. Availability of permanent solidifying material, such as hydroxyethyl methacrylate (HEMA) or silicone fluid, were used in our early cases, media contrast was used to inflate the balloon in our later cases.
Embolising Procedure
Mata's test: if the patient could not endure continuous compression of the carotid artery more than 30 minutes, ICA occlusion was not permitted.
Anaesthesia: local anaesthesia was used in almost all patients except children and patients who could not cooperate. 10 mg of dexamisone and 10 mg of diazepam should be intravenously injected just before the procedure and an intravenous drip of heperize saline should be maintained during the operation.
Operative approaches: transcervical and transfemoral approaches were used in 240 and 237 cases respectively (figure 1). Transfemoral vein approach: first the guiding catheter is delivered to the proximal part of the jugular glomus, then the microcatheter is delivered into the cavernous sinus through the superior and inferior petrosal sinus and microcoils or NBCA injected through a microcatheter (figure 2). This approach could only be used in cases in which the ICA had been ligated or occluded and the main direction of drainage of CCF was posterior.
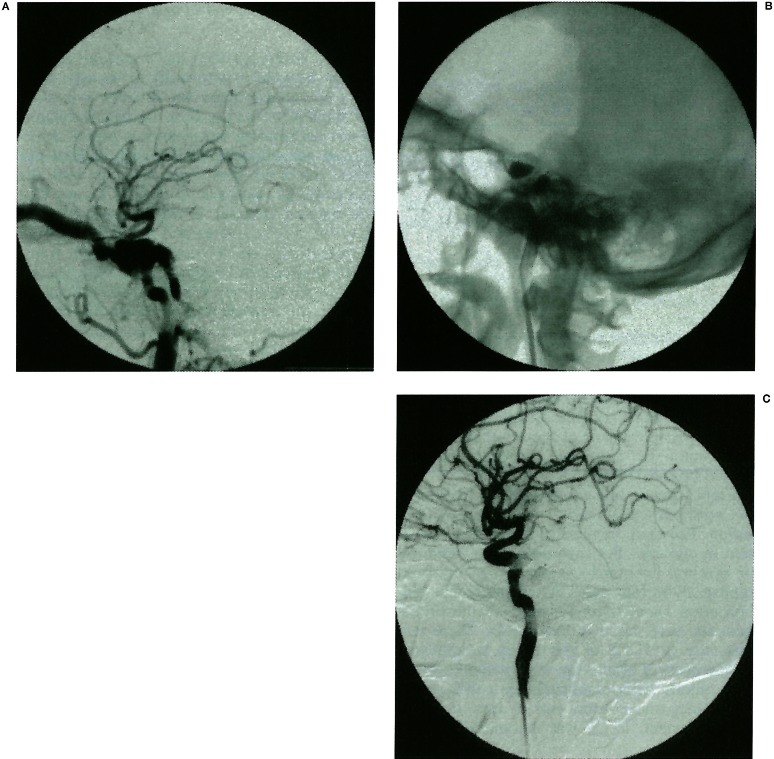
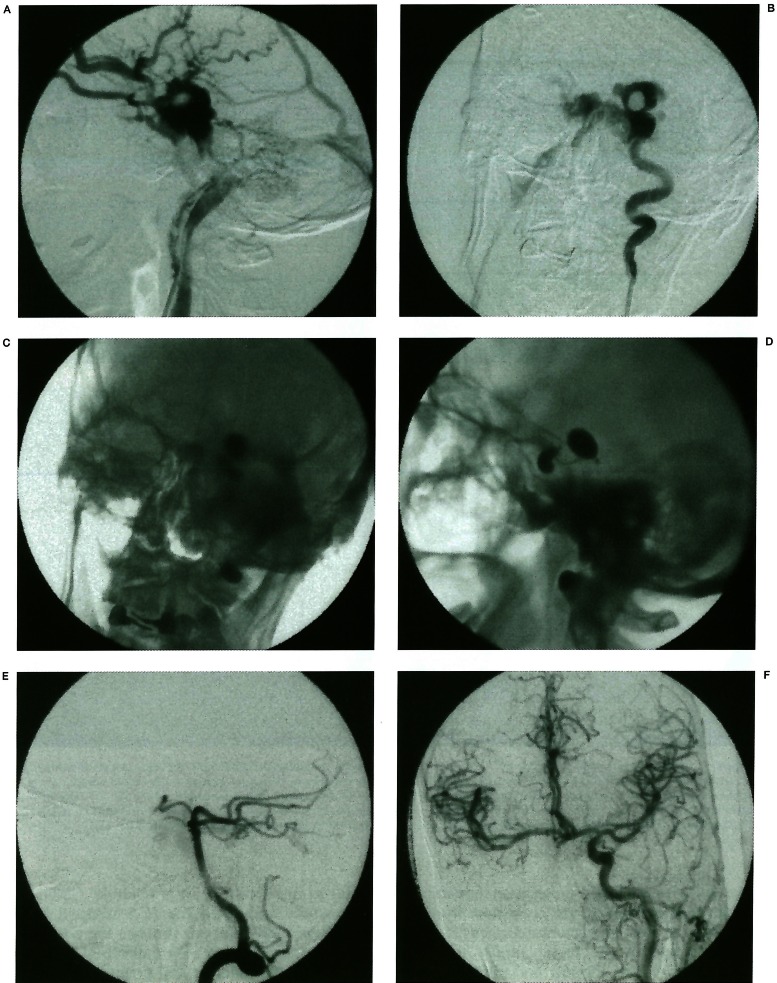
Figure 1.
Thirty-year old male, suffered of TCCF. The fistula was embolised with two balloons by transcervical approach.
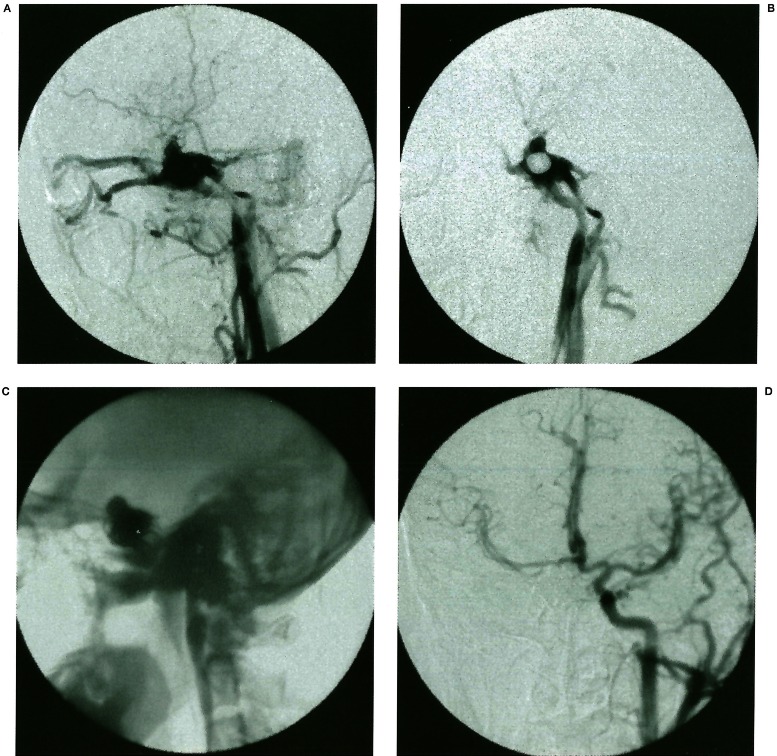
Figure 2.
Thirty-year old male, suffered of TCCF. The fistula could not be occluded completely with balloon. The internal carotid artery was then occluded. But fistula could still be seen by contralateral carotid angiogram. And then we delivered the micro-catheter into cavernous sinus through inferior petrosal. Cavernous sinus was embolised with coils. Finally, fistula was conformed to be embolised by contralateral carotid angiogram.
There were five cases in this group. Transophthalmic vein approach: the superophthalmic vein was punctured directly with a common puncture needle, the needle fixed and then the catheter delivered into the cavernous sinus with a micro wire guide, and NBCA injected or Tungsten coils placed through a microcatheter. Three patients whose ICA had been ligated in other hospitals utilized this approach.
Cautions of Balloon Occlusion
Choose the balloon with a metal mark. Only when the balloon catheter entered the TCCF should the balloon be inflated, this avoids accidental detachment of the balloon. For each procedure the diameter of the inflated balloon should be more than 5 mm, and then angiography should be done with a guiding catheter (5F~8F) to verify the relation between the balloon and leakage.
When the balloon has entered into leakage, the balloon should be placed as near as possible to the leakage. We tried our best to occlude the leakage with one balloon and keep the patency of the ICA.
CCF located on the ventral side of C3 because the leakage of ICA is very close to the anterior wall of cavernous sinus, the inflation of balloon is difficult to stagnate at the leakage, and easy to float to the middle part of the cavernous sinus, it is difficult to occlude the leakage completely with detachable balloons alone. Balloons and microcoils can be used in combination in this situation.
When the balloons were inflated to 0.5 cm in diameter, balloons ruptured suddenly and the contrast media spilled out in five cases in our group. This phenomenon repeatedly verified that the spur of bone fracture could penetrate the balloons. When this phenomenon occurs, the occlusion of ICA with balloons seems difficult to avoid. Microcoils might be used in this situation. In one case, nine balloons were used, and six balloons were ruptured by the spur, so we finally had to occlude the ICA.
Embolisation for the Emergency Treatment of TCCF
Emergency embolisation was necessary in three situations. One was recent severe epistaxis, illustrating that TCCF was combined with pseudoaneurysm (figure 3). Second was rapid visual impairment. Third was repeated occurrence of delayed intracerebral or subdural haematoma, the haematoma commonly located around the cavernous sinus. In our group, 15 cases needed emergency treatment, six cases complicated with severe epistaxis, four cases with delay intracranial haematoma, five cases with rapid visual impairment. All cases were cured.
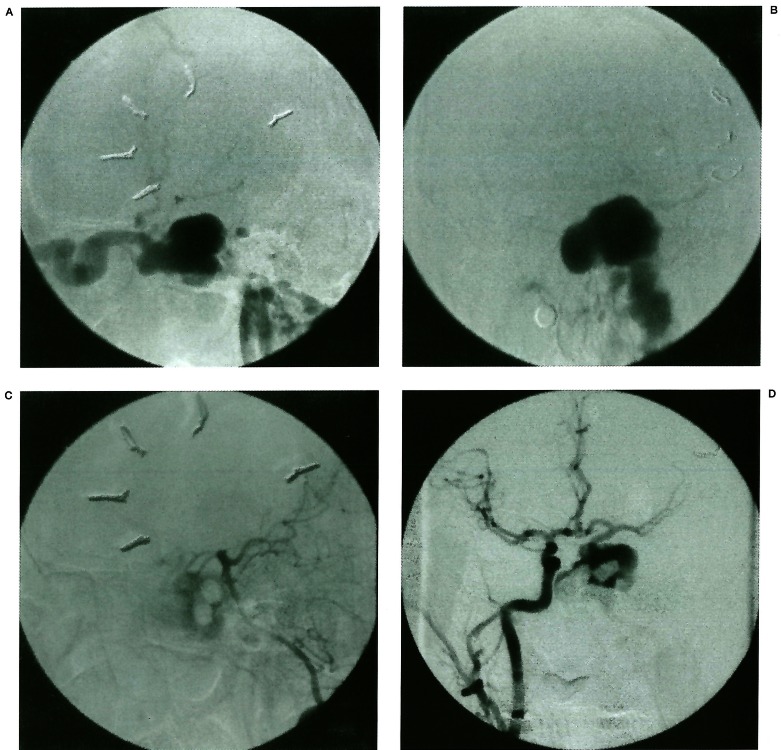
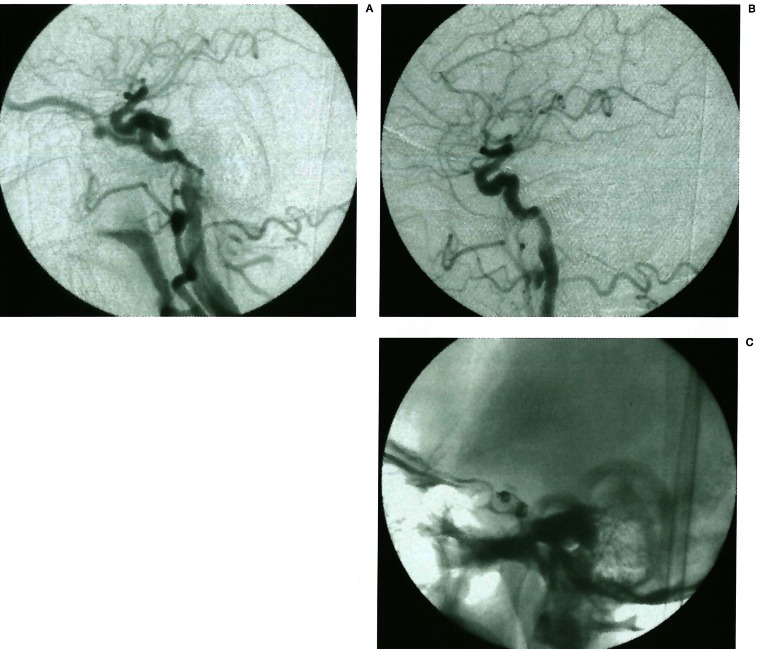
Figure 3.
A 26-year-old male suffered of TCCF with severe epistaxis. Angiogram could show the sign of pseudoaneurysm protruding into sphenoid sinus (A, B). Trying to occlude internal carotid artery could not embolise the fistula completely and epistaxis could not be stopped. Fistula was supported by anterior and posterior communicating artery (C, D). The microcatheter was introduced into fistula through posterior communicating artery. The fistula was totally embolised by MDS (E, F). Contralateral carotid artery and vertebral artery angiogram showed the good result of embolisation (G, H).
Postoperative treatment
Patients who accepted the transfemoral approach should stay in bed for at least eight hours, four hours for other approaches. Violent movement should be avoided for a week.
If the ICA was occluded, heparin should be given within five days after the operation to prevent cerebral ischemia and the nervous condition of patients should be carefully watched.
Results
Among 482 cases of TCCF (including five cases of bilateral TCCF) in our group, 420 cases were embolised successfully with one procedure, 58 with two procedures, three with three procedures and one with four procedures. No death related to the treatment occurred in our group.
Among 482 cases, the ICA were maintained patent in 405 cases (84%) and occluded in 77. Among the 77 ICA-occluded cases, exophthalmus and vessel bruit were alleviated in 16 cases, but did not disappear completely. This was due to the fact that leakage was reversely filled from the distal part of the ICA. We had thought it was feasible to occlude the ICA at the leakage with balloons if the patient could endure Matas test. But we found two cases of cerebral infarction, one case of vision loss, 16 cases of TCCF recurrence by one to three years of follow-up. Therefore, we advocated trying to maintain the patency of the ICA. If TCCF could not be embolised completely in one procedure, retry was attempted after one to two weeks.
The time of disappearance of cavernous sinus syndrome depended on the length of course, seriousness of symptom and degree of complexity.
Intracranial bruit could disappear right away, exophthalmus and orbit bruise could be recovered within one to four weeks. Visual damage could improve obviously within seven days, but diplopia might be recovered within seven to 35 days. If the movement of the ophthalmic muscle cannot be recovered, primary damage should be considered.
Eight cases in our group suffered from serious epistaxis and agreed to emergency embolisation. Epistaxis happened during the operation in one case. Pericavernous sinus, subdural or cerebral haemorrhage with coma occurred repeatedly in four cases. After emergency embolisation, haematoma was gradually absorbed, patients were cured in two weeks. There was one case of TCCF in this group complicated with abscess of brain stem with gradual respiratory failure. After stabilizing the condition by emergency tracheotomy and 20 days of antibiotic treatment, TCCF was embolised successfully.
Discussion
Chinese-made Detachable Balloon Catheter
In most cases, we selected the Chinese-made detachable balloon catheter which has some advantages over common balloon catheters. First, it has a longer 1 F segment, preventing accidental balloon detachment. There were two accidental detachments of balloons with the Bait system, but no accidental detachment with the Chinese-made catheter. Second, the dead cavity of the Chinese-made catheter was much less than in its counterparts.
Selection of Transfemoral or Transcervical Approach
Most authors select the transfemoral approach because it is thought to be safer than the transcervical approach. Besides, it is more convenient for the pre-ICA-occlusion collateral test and finding out if there is post-ICA-occlusion cross-flow to CCF. Nearly half of our cases, admitted first, were treated with the transfemoral approach. It is well known that the balloon catheter is much more resistant than the microcatheter and the arteries of elderly patients are tortuous so that the transfemoral approach to fistula is difficult. The accidental detachment of balloon sometimes occurs. So the transcervical approach has its own advantage due to its short route and fewer accidental detachments.
We selected the transcervical approach on one of the follow conditions. First, the patients were older than 55 years with a tortuous arterial system. Second, the whole cerebral angiographic diagnosis was finished before admission and there was no external carotid arterial supply to the CCF. Third, the history of CCF was no longer than six months to develop a large fistula or complex blood supply. But if it is likely that we have to occlude the fistula together with the ICA, we prefer the transfemoral approach to the transcervical approach. More than half of our cases were embolised by the transcervical approach. The transcervical approach is not much more difficult and dangerous than its counterpart for skilled hands. Some authors reported that the CCF closed following iatrogenic ICA dissection during direct puncture, equivalent to the time-honored, but generally less effective, method of proximal direct ICA ligation5. But in our cases there were only two slight cervical haematomas but no severe complications such as trachea spasm and suffocation. We found that the transcervical approach is suitable for simple fistula and makes the procedure more prompt and efficient.
Occlusion of the Internal Carotid Artery
Since the transarterial detachable balloon became the main therapy for TCCF, a gradual refinement of the technique has led to more than 80% of occlusion of fistula with patency of the ICA6,7,8. We occluded the ICA in 16% ofour cases, in which there were 25 cases initially occluded, 52 cases occluded in additional procedures (figure 4). However, the percentage is unlikely to decrease significantly for several reasons. First, preservation of the ICA is nearly impossible with detachable balloons when there is a large tear or a nearly complete transection of the ICA. Occlusion of the fistula requires occlusion of the ICA as well without the threat of pseudoaneurysm formation or thromboembolism. Second, the balloon may protrude into the lumen of the ICA and create a significant stenosis. Stenosis reduces the flow through the ICA and induces turbulence around the balloon, creating a risk of ischemia. Third, if the main portion of inflated balloon stays in the ICA, the balloon might shift, resulting in ICA occlusion or migration into the distal endovas-culature because of post-embolic gradual spontaneous deflation. Fourth, persistent balloon rupture may be caused by a bony spicule or pressure imbalance.
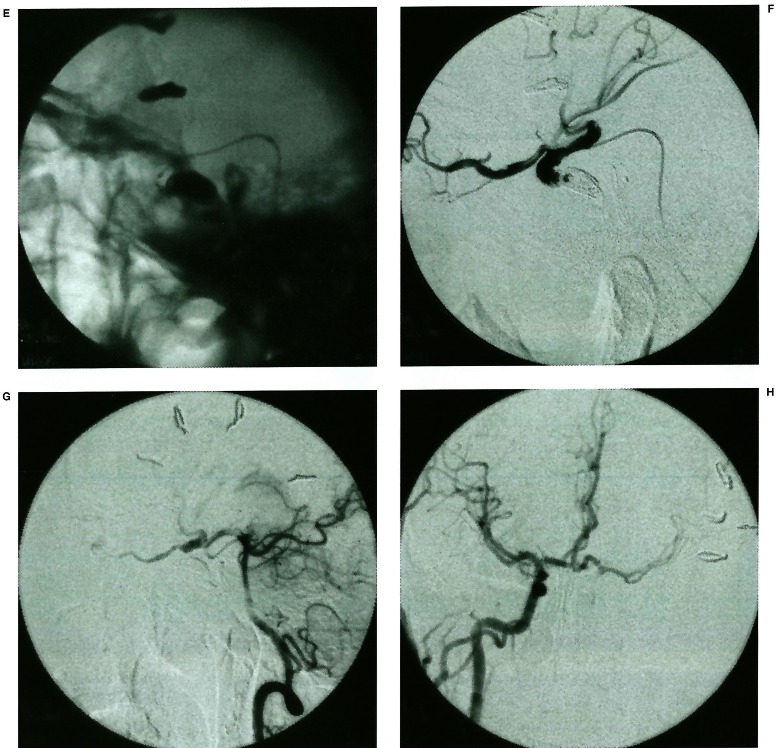
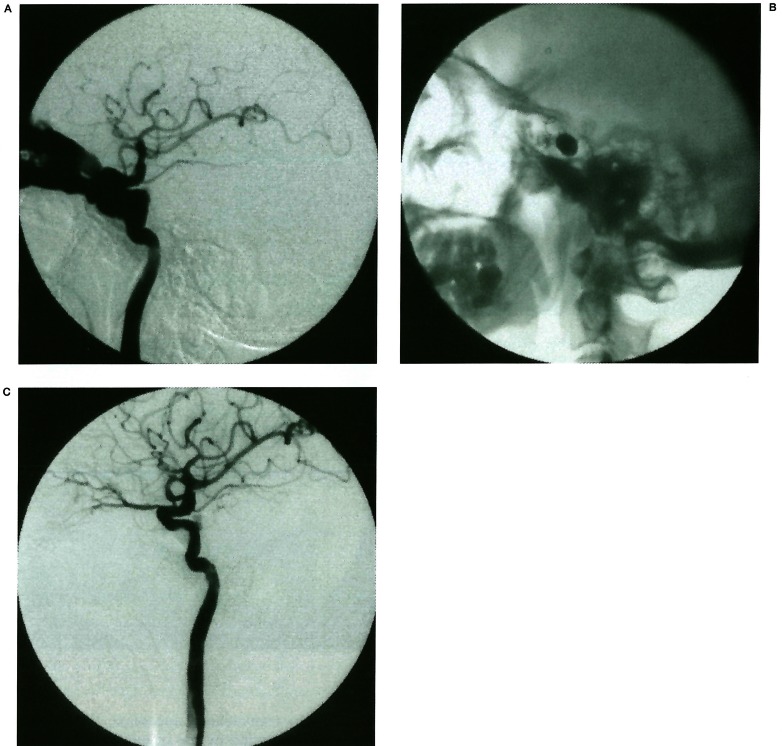
Figure 4.
A 37-year-old male, suffered from left TCCF. The fistula could not be occluded with the patency of ICA (A, B). The ICA had to be occluded together with the fistula (C, D). The angiograms of vertebral artery and contralateral carotid artery showed the compensatory blood supply of the occluded ICA (E, F).
In our early cases, Mata's test, a collateral test, and 30 minute temporary occlusion test were three prerequisites of ICA occlusion. But in some cases with complete or near-complete steal flow, the occlusion of the CCF was could be finished without Mata's test because collateral blood supply is always sufficient by good compensation from cross-flow.
If the ICA is occluded, heparin should be given within five days after the operation to prevent cerebral ischemia, and the nervous condition of patients should be carefully monitored.
Anterior Communicating Artery or Posterior Communicating Artery Approach for TCCF
When the ICA was trapped or a fistula recurred after occlusion of the ICA, catheterization through the anterior or posterior communicating arteries might be another possibility4. If the ICA is trapped, the cross-flow from the anterior or posterior communicating arteries can compensate the blood supply from the trapped ICA. The anterior and posterior communicating artery are always more prominent than that on the common station so that catheterization through the communicating arteries to the fistula point is possible. Cervigon successfully embolised the ICA trapped CCF with detachable balloons through the posterior communicating artery4. We embolised two cases through the anterior and posterior communicating arteries respectively. But we occluded the CCF with coils because the communicating arteries were not large enough for the balloon catheter to go through. These arterial routes might be more feasible than the transvenous approach. But experience in our group or documents is not as much as with the transvenous approach.
Transvenous Approach for TCCF
TCCF may be treated transvenously when the ICA is narrowed or occluded, failed transarterial access or fistula recurrence after trapping. The inferior petrosal sinus or superior ophthalmic vein must be patent to attempt a transvenous approach to the cavernous sinus5. When the CCF is supplied by multiple branches both from the ICA and/or external carotid artery, embolisation through the superior ophthalmic vein might be an alternative method8. Halbach9 also thought that the transvenous approach might be selected when the orifice of the fistula is smaller than the uninflated diameter of the carotid artery. Although arterialization of venous structures can occur in longstanding shunts, the drainage veins and dural sinuses are still thin-walled and can be perforated by catheter and guide wire manipulation.
We selected the transvenous approach when the ICA was ligated with the prominent superior ophthalmic vein or petrosal vein. TCCF supplied by multiple branches was also our indication for the transvenous approach. There were five cases occluded by the transfemoral venous approach and three cases embolised by the superior ophthalmic vein in this group. Four of the eight cases were embolised, two of them were not completely occluded. Catheterization was not successful in two of the cases. Five of the cases were embolised with coils and detachable balloons were utilized in only one case. Coils were used in most cases because it was much more difficult to reach the fistula point with the balloon catheter than with other microcatheters. The tip of the catheter must go as near as possible to the fistula site in order to completely occlude the fistula. The relatively low percentage of success might be caused by partitions within the cavernous sinus which preclude placement of the balloon near the fistula orifice9,10. Besides, the countercurrent and thin wall of the veins might be other causes of failure 8,9.
Although arterialization of venous structures can occur in long-standing shunts, the draining veins and dural sinuses are still thin-walled and can be perforated by catheter and guidewire manipulations. With the increased pressure and flow of the arterialized blood in these structures, small perforations can result in rapidly fatal subarachnoid haemorrhage9. But we did not encounter such a bad situation.
Emergency Treatment of TCCF
The majority of TCCF cases are benign with a good outcome if treated properly. But a minority of cases can lead to sudden death or severe disability. These cases need emergency intracranial embolisation.
TCCF with serious epistaxis is initially mild and brief so that the diagnosis is often elusive and delayed. But subsequent delay could lead to a massive life-threatening attack. A triad of fracture of cranial base (especially orbital fracture), monocular blindness and delayed massive epistaxis is often found in these cases10,11. The reason for epistaxis in TCCF cases is that the wall of cavernous sinus next to the sphenoid sinus ruptures to form a pseudoaneurysm. Massive epistaxis occurs by pulsating impact on the ruptured wall. There were nine cases of TCCF with delayed massive epistaxis one to five weeks after the initial head injury in our group. Five of them suffered from initial monolateral blindness. Two of them had eyesight impaired. Fracture of cranial base was found in all of them. But pseudoaneurysm protruding into sphenoid sinus was the most notable sign which was found in all cases. Packing of the nasal cavity temporarily stopped the massive haemorrhage, but only emergency balloon embolisation to occlude the fistula is the key to saving life6,10. The best result should be complete occlusion of the fistula with patency of the ICA. But fistulas with massive epistaxis are always large or multiple. This made the above best result impossible to achieve. So the embolisation of the ICA together with the fistula was the first choice in seven of our nine cases in order to thoroughly occlude the source of haemorrhage.
Intracranial haemorrhage with TCCF is another fatal condition. Hypertension in cavernous sinus and drainage veins is the premise of intracranial haemorrhage. If the hypertension is combined with rupture of the sinus wall or inverse filling of the cortical veins, intracranial haemorrhage may be induced8,12,13,14,15. There were three cases of intracranial haemorrhage in our group, in which two fistulas were embolised with patency of the ICA; the other one was occluded with sacrifice of the ICA. All three cases were cured. If the fistula is occluded, tension inside cavernous sinus may be decreased and haemorrhage can be stopped. But it is worth noting that removal of the haematoma must be avoided before occlusion of the fistula. Otherwise, fatal haemorrhage may be difficult to control during the operation 12,13,14,15 We suggest that the fistula be embolised be embolised by emergency if there is prominent cortical venous drainage.
Among the cases in our group, the visual impairment progressed slowly in most cases, but rapidly in rare cases. Eyesight loss happened 48 hours after injury in one case and six days after injury in another. This kind of visual impairment could not be reversed. Emergency treatment should be taken when rapid loss of eyesight happens.
Selection of Embolic Material except Detachable Balloons
Detachable balloon is the main method of embolisation of TCCF5,7. Failure may occur because the fistula orifice is too small to allow balloon inflation, or sharp margins of bony fractures or foreign bodies may rupture the balloon during inflation. In some patients who have subtotal occlusion after initial balloon embolisation, navigation of additional balloons into the fistula is unsuccessful owing to the presence of balloons partially blocking the fistula orifice. The use of coils may be an alternative way16,17. Eleven patients with TCCF in our group were embolised with coils because of failure of balloon embolisation (figures 3, 5). Coils were delivered through transvenous route in five and transarterial in six. Nine cases were successful treated and two TCCF were subtotally embolised. In order to avoid the migration of coils, we select the appropriate size of GDC or MDS to be the first and second coils. Additional free coils were delivered into the fistula if they remained empty. But a subtotal occlusion of a fistula may not indicate failure, because progression of thrombosis is likely to occur 16,17. One of two subtotally occluded TCCF with coils was found totally blocked by follow-up. But coils were not suitable to be used in large, high flow fistulas16,17.
Figure 5.
A 45-year-old male, suffered from TCCF. The fistula was too small to pass the balloons. So we had to embolised the fistula with 2 sets of GDC.
Glue such as NBCA or IBCA is rarely used to embolize TCCF. We occluded two cases of TCCF with NBCA. Balloons or coils sometimes cannot embolize all the TCCF because of a large tear of the ICA or part of the special sinus fistula8,9. If the fistula is still not completely embolised, but the flow of shunt was slowed down, NBCA could be tried. NBCA must be highly concentrated so as not to migrate. In two cases good results were obtained because NBCA could disperse more freely than other material and induce thrombosis after solidification (figure 6).
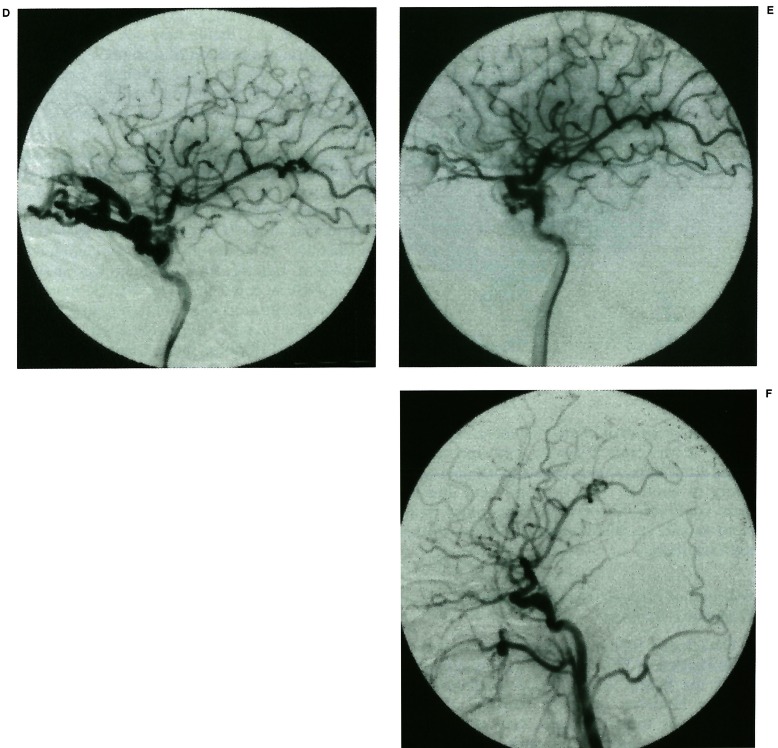
Figure 6.
A 29-year-old male, suffered from TCCF. It was occluded with coils in other hospital, but it reoccurred (A). We re-embolised the fistula with balloon, the coils used by other hospital was also seen (B). But the fistula could not be totally occluded (C). The fistula reoccurred again (D). The fistula was again embolised with NBCA, but it was only partially occluded (E). The fistula was nearly totally occluded 3 days after the NBCA occlusion (F). The patient refused the DSA recheck. But no sign of fistula occurred in 4 years.
Combination Embolisation for Complex TCCE
Most cases of TCCF could be transarterially treated successfully with detachable balloons5,7. But it was not so simple in some complex cases, which included a large tear or transection of the ICA, a large sinus with a long history, complex blood supply from both the ICA and external carotid artery and complex partition of sinus. Occlusion of the ICA cannot resolve all the problems. The combination of transarterial and transvenous approach, combination of balloons, coils and glue may block the fistula step by step. Each approach could be advantageous to embolise one partition of the sinus. Each kind of material could be suitable for some fistula orifice or flow of shunt. Traumatic indirect carotid cavernous fistula is rarely reported18. If the CCF is supplied by a simple branch, treatment is simple. But if the supply vesicle is multiple and small, it is difficult to occlude the CCF in one procedure.
Two cases in our group were embolised by a combination of different approaches and materials, fistula could not be blocked completely and fistula orifices were found to enlarge by follow-up. In one case with delayed repeatedly epistaxis, a laryngoscope was used to block the posterior nasal cavity to successfully stop the haemorrhage. Sometimes a surgical approach may be another alternative way if interventional treatment seams impossible19,20.
Special Balloon Sign in Embolisation of TCCF. “Bileakage Sign”
Recently, when we embolised a case of TCCF with detachable balloons, we found a radiological sign which had not been noticed before, nor reported in documents. We called the special phenomenon the “bileakage sign”. After occluding the ICA near the leakage, we found the balloon filled with media contrast showing two symmetric convexes, like the head of a cobra, we thought that each convex indicated a leakage. This was the special sign of “bileakage”21 (figure 7).
Figure 7.
Bileakage sign.
Besides the special sign, the characteristics of “bileakage” were:
1) It could be seen in sharp hitting and firearm hitting. We had treated a case of firearm induced TCCF, which had bileakage.
2) It could be seen between the C-4 and C-5 segment of the ICA because of the characteristic anatomy.
3) Balloons in the ICA could enter into the cavernous sinus through both ventral and dorsal ICA leakage, but it was difficult to occlude the fistula completely. We considered that the phenomenon indicated the ICA had two leakages.
4) It was difficult to maintain patency of the ICA in some cases.
References
- 1.Prolo DJ, Hanberry JW. Intraluminal occlusion of a carotid cavernous sinus fistula with a balloon catheter: Technical note. J Neurosurg. 1971;35:237–242. doi: 10.3171/jns.1971.35.2.0237. [DOI] [PubMed] [Google Scholar]
- 2.Parkinson D. Carotid cavernous fistula: Direct repair with preservation of the carotid. J Neurosurg. 1973;38:99–106. doi: 10.3171/jns.1973.38.1.0099. [DOI] [PubMed] [Google Scholar]
- 3.Serbinento FA. Balloon catheterization and occlusion of major cerebral vessels. J Neurosurg. 1974;41:125–145. doi: 10.3171/jns.1974.41.2.0125. [DOI] [PubMed] [Google Scholar]
- 4.Cervigon EC, Bien S, et al. Treatment of a recurrent traumatic carotid-cavernous fistula: Vertebro-basilar approach after surgical occlusion of the internal carotid artery. Neuroradiological. 1998;30:355–357. doi: 10.1007/BF00328189. [DOI] [PubMed] [Google Scholar]
- 5.Lewis AL, Tomsick TA, et al. Management of 100 consecutive direct carotid-cavernous fistulas: results of treatment with detachable balloons. Neurosurgery. 1995;36:239–245. doi: 10.1227/00006123-199502000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Tomsick TA. Type A CCF: transarterial balloon occlusion. In: Tomsick TA, editor. Carotid cavernous fistula. Digital Educational Publishing, Inc.; 1997. [Google Scholar]
- 7.Debrun GM, Viñuela F, et al. Indications for treatment and classification of 132 carotid-cavernous fistulas. Neurosurgery. 1988;22:285–289. doi: 10.1227/00006123-198802000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Halbach VV, Higashida RT, et al. Transvenous embolization of direct carotid cavernous fistulas. Am J Neuroradiol. 9:741–747. [PMC free article] [PubMed] [Google Scholar]
- 9.Debrun GM, Lacour P, et al. Treatment of 54 traumatic carotid-cavernous fistulas. J Neurosurg. 1981;55:678–692. doi: 10.3171/jns.1981.55.5.0678. [DOI] [PubMed] [Google Scholar]
- 10.Chen D, Adriane PC, et al. Epistaxis originating from traumatic pseudoaneurysm of the internal carotid artery: diagnosis and endovascular therapy. Laryngoscope. 1998;108(3):327–331. doi: 10.1097/00005537-199803000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Simpson RK, Harper PR, Bryan RN. Emergency balloon occlusion for massive epistaxis due to traumatic carotid-cavernous aneurysm. J Neurosurg. 1988;68:142–144. doi: 10.3171/jns.1988.68.1.0142. [DOI] [PubMed] [Google Scholar]
- 12.Turner DM, Vangilder JC, et al. Spontaneous Intracerebral Hematoma in Carotid-cavernous Fistula. J Neurosurg. 1983;59(10):680–686. doi: 10.3171/jns.1983.59.4.0680. [DOI] [PubMed] [Google Scholar]
- 13.Halbach VV, Hiesshima GB, et al. Carotid-cavernous fistulae: indications for urgent treatment. Am J Radiol. 1987;149(9):587–693. doi: 10.2214/ajr.149.3.587. [DOI] [PubMed] [Google Scholar]
- 14.Lin KT, Chang CN, Wal YY. Spontaneous intracerebral hematoma from occult carotid cavernous fistula during pregnancy and puerperium. J Neurosurg. 1992;76(4):714–717. doi: 10.3171/jns.1992.76.4.0714. [DOI] [PubMed] [Google Scholar]
- 15.Angelo VA, Monte V, et al. Intracerebral venous hemorrhage in “high risk” carotid-cavernous fistula. Surg Neuro. 1988;30:387–390. doi: 10.1016/0090-3019(88)90202-9. [DOI] [PubMed] [Google Scholar]
- 16.Halbach VV, Higashida RT, et al. Transarterial platinum coil embolization of carotid-cavernous fistulas. Am J Neuroradiol. 1991;12:429–433. [PMC free article] [PubMed] [Google Scholar]
- 17.Siniluoto T, Seppanen S, et al. Transarterial embolization of a direct carotid cavernous fistula with Guglielmi Detachable Coils. Am J Neuroradiol. 1997;18:519–523. [PMC free article] [PubMed] [Google Scholar]
- 18.Jacobson BE, Nesbit GM, et al. Traumatic indirect carotid-cavernous fistula: Report of two cases. Neurosurgery. 1996;39:1235–1238. doi: 10.1097/00006123-199612000-00033. [DOI] [PubMed] [Google Scholar]
- 19.Tu YK, Liu HM, Hu SC. Direct surgery of carotid cavernous fistulae and dural arteriovenous malformation of the cavernous sinus. Neurosurgery. 1997;41(4):798–805. doi: 10.1097/00006123-199710000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Krisht AF, Burson T. Combined pretemporal and endovascular approach to the cavernous sinus for the treatment of carotid-cavernous dural fistula: technical case report. Neurosurgery. 1999;44:415–418. doi: 10.1097/00006123-199902000-00113. [DOI] [PubMed] [Google Scholar]
- 21.Higashida R, Halbach V, et al. Interventional neurovascular treatment of traumatic carotid and vertebral artery lesions. Am J Radiol. 1989;153:577–582. doi: 10.2214/ajr.153.3.577. [DOI] [PubMed] [Google Scholar]
- 22.Wu ZX, Wang CC, et al. Endovascular treatment of 260 cases of traumatic carotid-cavernous fistula. Journal of Minimally Invasive Neurosurgery. 1996;1(1):1–3. [Google Scholar]