Abstract
Background
Plants have traditionally been used for treatment of human and livestock ailments in Ethiopia by different ethnic and social groups. However, this valuable source of knowledge is not adequately documented, which impedes their widespread use, evaluation and validation. Here, we recorded indigenous knowledge and standard practices for human and livestock disease control, of three ethnic groups (Aari, Maale and Bena-Tsemay) in South Omo Zone of Southern Nations, Nationalities and Peoples Regional State, Ethiopia.
Methods
A cross-sectional study was carried out using a semi-structured questionnaire to document knowledge of 50 traditional healers (40 male and 10 female) in medicinal plant use for treatment of human and livestock ailments. Descriptive statistics were used to analyze and summarize the ethno-botanical data.
Results
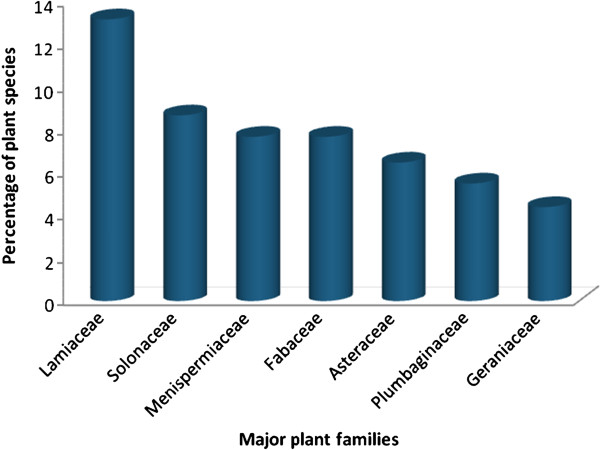
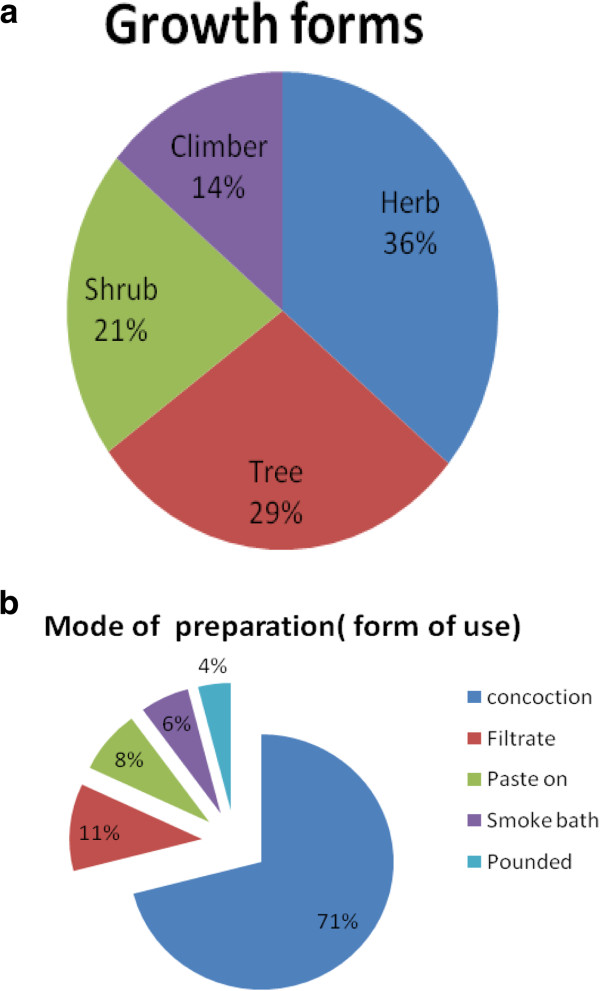
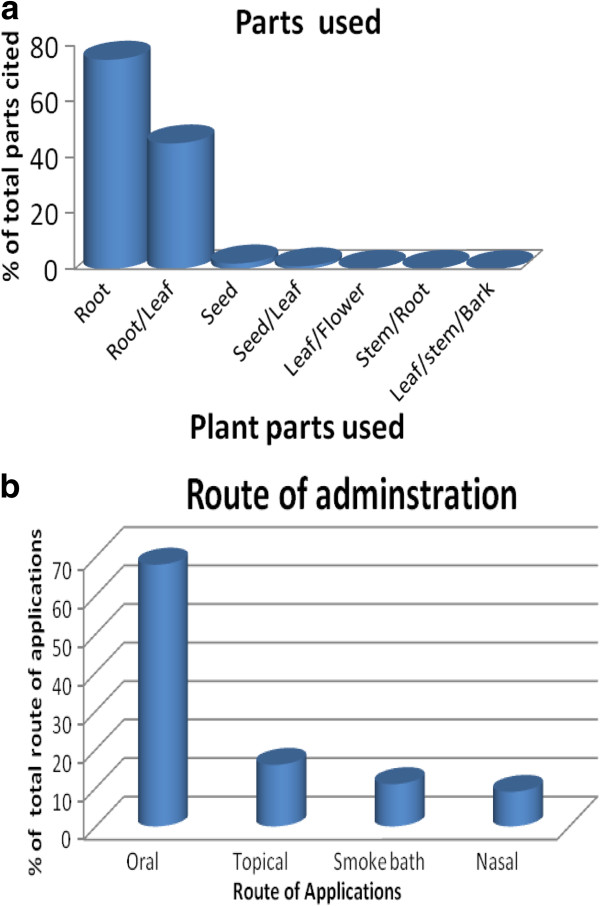
Ninety-one plants, with claimed medicinal properties against a total of 34 human and livestock ailments, were reported and botanically identified as belonging to 57 genera and 33 plant families. Most of the plant species reported belonged to one of seven major families: Lamiaceae, Solanaceae, Menispermiaceae, Fabaceae, Asteraceae, Plumbaginaceae and Geraniaceae. Woody plants (shrubs 21% and trees 29%) were the major growth form used, whilst roots (40%) and leaves (35%) were the major plant parts used in the study areas. Healers mostly practice oral administration of plant preparations (65%). Multiple medicinal plants were cited against particular ailments, and mixing of two or more different medicinal plants (14.3%) against a single ailment was also commonly reported.
Conclusion
This study showed that traditional medicine, mainly involving the use of medicinal plants, is playing a significant role in meeting the primary healthcare needs of the three ethnic groups. Acceptance of traditional medicine and limited access to modern healthcare facilities could be considered as the main factors for the continuation of the practice. Documented knowledge of the traditional healers can be used to support the country’s human and livestock health care system and improve lives and livelihoods. Information generated will be used in future studies to validate bioactivity of selected medicinal plants used by traditional healers, so to increase their acceptability in health care systems both nationally and internationally.
Keywords: Ethnomedicine, Traditional healers, Medicinal plants, South Omo, Ailments, Informants consensus factor
Background
Knowledge can arise from scientific or traditional sources [1]. Traditional knowledge has been described as a cumulative body of knowledge, practice and belief, evolving through adaptive processes and handed over through generations by cultural transmission [2]. Traditional medicine is used throughout the world as it is heavily dependent on locally available plant species and plant-based products and capitalizes on traditional wisdom-repository of knowledge [3]. The wide spread use of traditional medicine could be attributed to cultural acceptability, economic affordability and efficacy against certain type of diseases as compared to modern medicines. Thus, different local communities in countries across the world have indigenous experience in various medicinal plants where they use their perceptions and experience to categorize plants and plant parts to be used when dealing with different ailments [4].
Plants have played a central part in combating many ailments in human and livestock in many indigenous communities, including Africa [5]. Traditional healers, and particularly medicinal plant herbalists, in Africa have a detailed knowledge-base of traditional medicine [6,7], which is transferred orally from one generation to the next through professional healers, knowledgeable elders and/or ordinary people [8].
In Ethiopia, traditional medicine has played a significant role in treating health problems in both livestock and humans [9-12]. Knowledge of medicinal plants of Ethiopia and of their uses provides vital contribution to human and livestock health care needs throughout the country [13]. The plant- based human and livestock health care persists and remains as the main alternative treatment for different ailments in Ethiopia, largely due to shortage of pharmaceutical products, prohibitive distance of the health service stations, unaffordable prices by small holder farmers and pastoralists for conventional drugs, emergence and re-emergence of certain diseases and appearance of drug resistant microbes and/or helminthes [14].
Much of the Ethiopian South Omo population is made up of nomadic pastoralists who depend upon livestock as their main source of livelihood [15]. The traditional medicinal plant lore and potentials of the three ethnic groups have not been investigated to a conspicuous level. Similar to many other rural communities in Ethiopia, the use of traditional medicinal plants plays a vital role in human and livestock health care systems in the pastoral and agro-pastoral communities of the study areas. The three ethnic groups (Aari, Maale and Bena-Tsemay) in South Omo are expected to be custodians of valuable indigenous knowledge on the use of their traditional medicinal plants, which they use for treating of human and livestock ailments. Currently, access to modern health services for both human and livestock is very limited and/or non-existent for some community members of the study areas. This study is basically focusing on a remote and pastoralist areas where the accessibility, affordability and cultural acceptability of the use of medicinal plants for treatment of human and livestock ailments is very significant. The dependence of the plant-based health care system could partly be attributed to underdeveloped infrastructures and modern medical health care system in the general area. Unless the plants are conserved and the ethno-medicinal knowledge is documented, there is a danger that both the valuable medicinal plants and the associated indigenous knowledge of the ethnic groups could vanish forever due to lack of documentation [6] and loss of valuable medicinal plants due to population pressure, agricultural expansion and deforestation [16], as well as due to drought, urbanization and acculturation [17]. Furthermore, pastoral and agro-pastoral communities of these ethnic groups have remained ethno-medicinally unexplored and there is no comprehensive account of the medicinal plant-based practices. Therefore, the objective of this study was to document the indigenous knowledge and practices of the healers in the study areas (the three ethnic societies in the South Omo zone of the Southern Nations, Nationalities and Peoples Region (SNNPR) of Ethiopia) on medicinal plants for human and livestock disease control. Below, we describe the study area, how informants were selected, the type of information we have gathered, and the use of the informant consensus factor to synthesize the information obtained, followed by presenting our findings and discussing them in context of existing literature.
Materials and methods
Description of the study area and the people
The study was conducted in selected areas of the South Omo zone, inhabited by three ethnic groups (Aari, Maale and Bena-Tsemay). The administrative zone is bordered on the south by Kenya, on the west by Bench Maji, on the northwest by Kefa-Sheka, on the north by North Omo, on the northeast by the Derashe and Konso Special Woredas, and on the east by the Oromia Regional State (Figure 1).
Figure 1.
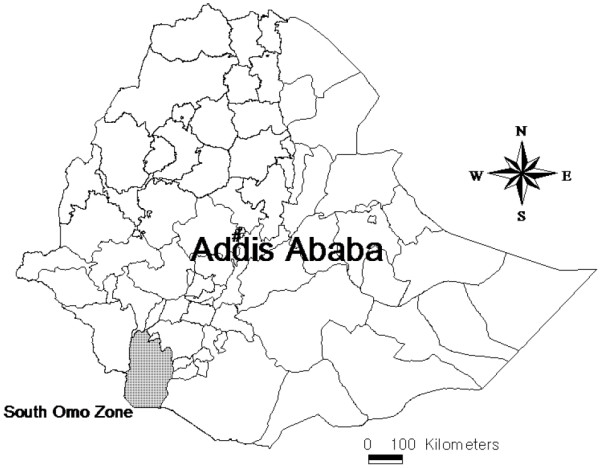
Map of South Omo zone indicated by the shaded region.
The annual average temperature of the area is 28°C with an annual average rainfall of 1190 mm [18]. The 2007 census data revealed that the zone has a total population of 573,435 people (286,607 male and 286,828 female) of which 4.45% are pastoralists and semi-pastoralists. Their culture places highest value on cattle, with relatively less on mixed farming (Central Statistics Agency, 2007). Among the six largest ethnic groups living in the area, Aari, Maale and Hamer-Bena (Bena-Tsemay) comprise 42.9%, 13.5% and 12.9%, respectively. Aari, Maale and Hamer are the major languages spoken by 43.3%, 13.7% and 13% of the people in the area, respectively [19].
Selection of informants
A total of 50 traditional healers, i.e. 24 from the Aari (20 males and 4 females), 16 from the Maale (13 males and 3 females) and 10 from Bena-Tsemay (7 males and 3 females) ethnic groups of different ages (32–81 years) were selected with the help of local elders, agricultural and health extension workers and administrative personnel, and interviewed as key informants. The selected healers were well-known in the community due to their long practice in providing services related to traditional health care to the community. Prior to the interview process, discussion was held with the informants through assistance of local elders to elaborate the objective of the study. This was done to clarify the purpose and build confidence of the respondents to provide reliable information without suspicion. After the discussion, 6 potential informants (2 from Aari, 1 from Maale and 3 from Bena-Tsemay) showed unwillingness to share their medicinal plant knowledge and withdrew from the study. The 50 healers that participated in the study were asked to provide information on plant(s) use against any kind of illness in humans and livestock, and in particular the type of plant (e.g. trees, shrubs, herbs, climbers or others) and the parts used (e.g. roots, leaves, seeds, flowers, stems or others), the methods of remedy preparation (e.g. concoction, filtrate, paste on, smoke bath, pounded or others), the routes of administration (e.g. oral, topical, smoke bath, nasal or others) and the dosage. Specimen of the reported medicinal plants were collected during the interview from the field, coded and sent to the National Herbarium of Addis Ababa University for botanical identification and archiving.
Data collection and analysis
Descriptive statistics were used to analyze and summarize the ethno-botanical data. Based on the information obtained from the informants, the ailments reported were grouped into a total of 12 categories (Table 1). To estimate medicinal plant use variability and to assist prioritizing medicinal plants for further studies, the informant consensus factor (ICF) was calculated [20]. The ICF is calculated using the number of use citations (Nuc) in each category and the number of plant species (Ns) cited through the following formula:
Table 1.
Informant consensus factor (ICF) values of use category of multiple plants claimed as having medicinal values by informants of the three ethnic groups from South Omo zone, southern Ethiopia
| Use category | Plant species | Number of use citation* | % of all citations | ICF value |
|---|---|---|---|---|
| Anthrax |
Dombeya spp. (7), Achyrospremum schimperi (6), Tragia doryodes (5), Geranium aculeolatum (8) |
26 |
6.5 |
0.88 |
| Poisonous plants |
Solanum spp. (5), Oxalis corniculata (7) |
12 |
2.9 |
0.91 |
| Skin infections and external parasites |
Solanum incanum (6), Desmodium dichotomum (7), Laggera tomentosa (8), Geranium arabicum (6), Nicotiana tabacum (6), Premna schimperi (9), Calpurnia aurea (8) |
50 |
12.4 |
0.88 |
| Pain related illnesses |
Senna spp. (4), Tagetes spp. (9), Monsonia parvifolia (8), Plumbago caerulea (4), Desmodium delotum (3) |
28 |
6.9 |
0.85 |
| Malaria and anemia like syndrome with jaundice |
Carphalea glaucescens (5), Cissampeolos mucronata (6), Indigofera arrecta (6), Cissampelos spp. (2), Lantana trifolia (4), Luecas stachydiformis (2), Premna oligotricha (5), Droguetia iners (6), Zornia glochidiata (3), Galinsoga parviflora (3) |
40 |
9.9 |
0.77 |
| Abdominal/stomach disorders and internal parasites |
Pycnostachys meyeri (5), Zornia apiculata (4), Achyranthes aspera (4), Stereospermum kunthianum (7), Cissampelos pariera (6), Cissampelos capensis (3), Lagenaria siceraria (3), Momordica charantia (2), Tagetes minuta (6), Premna spp. (5), Salvia acuminata (4), Echinacea spp. (2), Pelargonium alchemilloides (5), Orthosiphon surmentosus (6), Mucuna melanocarpa (8), Sida spp. (5), Chasmanthera welwitschii (2), Rytigynia spp. (5), Zornia latifolia (3), Centella asiatica (3), Ipomoea eriocarpa (7), Chlaenandra ovata (2) |
97 |
24.1 |
0.78 |
| Snake bite/poisoning |
Alonsoa acutifolia (5), Plumbago pulchella (6), Opericulicarya gummifera (6), Plectranthus globosus (6), Barthlottia madagascariensis (3), Ludwigia abyssinica (6), Claoxylopsis andapensis (8), Carissa carandas (5), Hyparrhenia hirta (4), Verbena officinalis (5) |
54 |
13.4 |
0.83 |
| Mich and Megagna** |
Dobera spp. (6), Droguetia debilis (5), Justica dianthera (4) |
15 |
3.7 |
0.86 |
| Coughing in equines and ruminants |
Justicia diffusa (5), Solanum bellum (5), Datura stramonium (4), Vaccaria hispanica (6), Ozoroa insignis (6) |
26 |
6.5 |
0.84 |
| Removal of retained placenta |
Solanum acaule (2), Solanum acuminatum (3), Dovyalis spp. (5), Galinsoga quadriradiata (6), Colocasia esculenta (4), Plumbago zeylanica (6), Momordica spp. (2) |
28 |
6.9 |
0.78 |
| Evil eye |
Drymaria spp. (4), Plectranthus glabriflorus (3), Cissus quadrangularis (4), Cryptocarpus spp. (3), Colignonia ovalifolia (4), Achyrospermum africanum (5), Drymaria cordata (3), Plumbago auriculata (4), Chelonopsis moschata (2), Withania somnifera (3), Plumbago spp. (2) |
37 |
9.2 |
0.72 |
| Black leg |
Momordica foetida (7), Pentas suswaensis (8), Chasmanthera dependens (3) |
18 |
4.5 |
0.88 |
| Rabies |
Caylusea abyssinica (3) |
3 |
0.7 |
1.00 |
| Improve milk production in cows | Indigofera trita (6) | 6 | 1.4 | 1.00 |
* Numbers in parenthesis indicate the number of citation of that plant by informants (traditional healers and community members) against a particular ailment category.
** Ailment characterized with fever, head ache and sweating.
Thus, ICF values range from 0 to 1, with high values (i.e. close to 1) indicating that relatively few plants are used by a large proportion of informants, while low values (<0.5) indicate that informants do not agree on the plant species to be used to treat a category of ailments.
Results and discussion
Knowledge of informants on medicinal plants
Indigenous people of different localities have their own specific knowledge on plant use, management and conservation [21]. Medicinal plants represent a significant contribution to human and livestock health and it has been suggested that their use is one of the most significant ways in which humans directly reap the benefits provided from biodiversity [22,23]. During the field survey in our study areas, informants reported ethno-medicinal data of 91 species of plants distributed across 33 families and 57 genera as having medicinal properties against 34 ailments (12 in humans, 11 in livestock and 11 in both human and livestock). The 91 plant species that are used by traditional healers among the three ethnic groups interviewed were identified and documented. Among the medicinal plants identified most of them belong to the seven families as shown in Figure 2. The plant family Lamiaceae was most frequently represented amongst the documented useful species, with a total of 12 species out of the 91 plants identified, followed by Solanaceae with a total of 8 species and Menispermiaceae, and Fabaceae with total of 7 species each, and others constitute one up to six plant species per family.
Figure 2.
The percentage of plant species distributed over seven major families.
The informants cited 32 (35.2%), 35 (38.5%) and 24 (26.4%) plants as having medicinal properties against ailments of livestock, humans or both livestock and humans, respectively (Table 2). The informants also reported multiple plant remedies against certain ailments, such as snake bite/poisoning for both humans and livestock. Depending upon the type of illness, the use of two or more parts of medicinal plants was also reported by some healers as common practice. For example, of the total 32 medicinal plants purely claimed for livestock illnesses, eight were used in two-plant combination preparations, and these target three different ailments, i.e. to treat epizootic lymphangitis, removal of fetal membrane, and anemia with jaundice (Table 2).
Table 2.
Medicinal plants, with family, scientific and local name, for selected ailments of human and/or veterinary importance, with parts used and preparations, as claimed by informants of the three ethnic groups from South Omo zone, Southern Ethiopia
| Family | Scientific name | Local name* | Voucher number | Use(s) | Parts used and preparation | Importance |
|---|---|---|---|---|---|---|
| Amaranthaceae |
Achyranthes aspera Linn. |
Busino (M) |
KTG28 |
Abdominal pain and tonsillitis |
Root chopped and mixed with water and taken orally. Leaf chewed and the extract kept near the inflammation area |
Human |
| Lamiaceae |
Achyrospermum africanum Hook.f. ex Baker |
Kebit buda (A) |
KTG54 |
Evil eye |
Leaf and root chopped and soaked with water |
Human |
| |
Achyrospermum schimperi (Hochst. ex Briq.) Perkins |
Abasanga medihanit (A,Amh) |
KTG65 |
Anthrax |
Leaf and flower chopped and soaked with hot water and drenched |
Veterinary |
| Scrophulariaceae |
Alonsoa acutifolia Ruiz & Pav. |
Shosha tesha (M) |
KTG66 |
Snake bite/poison |
Root chopped and mixed with Plectranthus glandulosus in water and the filtrate drenched |
Human and Veterinary |
| |
Barthlottia madagascariensis E.Fisch. |
Unkown (A) |
KTG18 |
Snake bite/poison |
Concoction |
Human and Veterinary |
| Fabaceae |
Calpurnia aurea (Aiton)Benth. |
Kaino(M) |
KTG91 |
Flea and louse infestation |
Freshly chopped or dried and ground leaf mixed with water and applied to the flea and louse infested areas |
Veterinary |
| Apocynaceae |
Carissa carandas L. |
Goiti(B),ebab medihanit (Amh) |
KTG45 |
Snake bite/poison |
The leaf chopped, mixed with water taken orally |
Human and Veterinary |
| Rubiaceae |
Carphalea glaucescens (Hiern) Verdc |
Wariamo (M) |
KTG31 |
Anaemia (known as Airo) |
Leaf powdered mixed with Ipomoea kiwuensis smoked for three days |
Human |
| Recedaceae |
Caylusea abyssinica (fresen.) Fisch. & Mey |
Giesilla (M) |
KTG64 |
Rabies (effective even when clinical signs are present) |
Root chopped and mixed with cold water and drenched |
Human and Veterinary |
| Apiaceae |
Centella asiatica - (L.)Urb. |
Busino (M) |
KTG87 |
Abdominal ache |
Root dried, ground and mixed with cold water when needed (on cup or glass full) |
Human |
| Menispermaceae |
Chasmanthera dependens (Hochst) |
Moshito (M) |
KTG33 |
Black leg |
Root bark and leaf dried and ground and given to emaciate calf as much as possible |
Veterinary |
| |
Chasmanthera welwitschii Troupin |
Heilho (M) |
KTG27 |
Antiamoeba |
Root bark and leaf dried and ground and given to emaciate calf as much as possible |
Veterinary |
| Lamiaceae |
Chelonopsis moschata Miq. |
Kebit buda (A) |
KTG47 |
Evil eye |
Leaf and root chopped and soaked with water |
Human |
| Menispermaceae |
Chlaenandra ovata. Miq. |
Eincht (A) |
KTG73 |
Abdominal ache |
Root chopped and mixed with water and drenched |
Human |
| |
Cissampelos capensis L.f. |
Wontin kanna (A) |
KTG76 |
Abdominal cramp |
Root chopped, powdered, soaked with water, filtered and drenched |
Human |
| |
Cissampelos mucronata A.Rich. |
Kawuro (M) |
KTG37 |
Anaemia with jaundice |
Leaf collected, dried, ground and mixed with hot water and two spoonful taken at once |
Human |
| |
Cissampelos pareira L. |
Shelindo (M) |
KTG70 |
Broad spectrum anti- helminthiasis |
Root ground mixed with large amount of water and drenched. It causes fever diarrhea then animals are cured |
Veterinary |
| |
Cissampelos spp. |
Kawto (M) |
KTG32 |
Anaemia like syndrome with jaundice |
Leaf collected, dried, ground with local mill and mixed with hot water and two spoonful taken at once (bitter) |
Human |
| Vitaceae |
Cissus quadrangularis L. |
Bararo (M) |
KTG20 |
Evil eye |
Tied under belly |
Veterinary |
| Euphorbiaceae |
Claoxylopsis andapensis Radcl.-Sm. |
Dorba (A) |
KTG43 |
Snake bite/poison |
Bark and leaf chopped, soaked in water and drenched |
Human |
| Nyctaginaceae |
Colignonia ovalifoliaHeimerl |
Afesha (A) |
KTG41 |
Evil eye |
Leaf squeezed and inhaled |
Human |
| Araceae |
Colocasia esculenta (L.) Schott |
Haleko (A,M,BT) |
KTG77 |
To detach retained fetal membrane |
Root dried, ground and mixed with powdered root of Momordica spp. and all soaked in warm water and one cupful drenched |
Veterinary |
| Nyctaginaceae |
Cryptocarpus spp. |
Afei tesha (M) |
KTG23 |
Evil eye |
Root chopped and mixed with cold/hot water |
Human |
| Solanaceae |
Datura stramonium L. |
Onidod (A) |
KTG05 |
Coughing (for horses, mules and donkeys) |
Leaf chopped and mixed with cold water and drenched via nose |
Veterinary |
| Papilionaceae |
Desmodium dichotomum (Willd.) DC. |
Muasii (A) |
KTG07 |
Epizootic lymphangitis (tushita) |
Root chopped, mixed with cold water and drenched via nose |
Veterinary |
| |
Desmodium delotum J.F. Macbr. |
Not known (A) |
KTG42 |
Eye illness |
Leaf apex chopped, soaked in water, applied to sick eye |
Human and Veterinary |
| Salvadoraceae |
Dobera spp. |
Mitch medihanit (A, Am) |
KTG89 |
Mitch |
Leaf boiled with water and inhaled |
Human |
| Sterculiaceae |
Dombeya spp. |
Bata (A) |
KTG15 |
Anthrax |
The leaf is chopped and mixed with Tragia doryodes and the filtrate taken orally |
Human and Veterinary |
| Flacortiaceae |
Dovyalis spp. |
Mukale (M) |
KTG85 |
To detach retained placenta |
Leaf chopped and mixed with hot water and given as ad libtum |
Veterinary |
| Urticaceae |
Droguetia debilis Rendle |
Megagna medanit (Amh) |
KTG52 |
Megagna |
Leaf apex chopped and pasted on the pain area |
Human |
| |
Droguetia iners (Forssk.) Schweinf. |
Yewoba medihanit (A) |
KTG61 |
Malaria |
Leaf chopped and mixed with Premna oligotricha and boiled together one glassful drenched |
Human |
| Caryophyllaceae |
Drymaria cordata (L.) Willd. ex Schult. |
Yebuda medihanit (A, Amh) |
KTG59 |
Evil eye in animals |
Leaf and root chopped mixed in water and the filtrate is sprayed on animal body and the sediments are drenched |
Human and Veterinary |
| |
Drymaria spp. |
Unknown (A) |
KTG17 |
Evil eye |
The leaf is chopped and mixed with water and the filtrate taken orally |
Human |
| Asteraceae |
Echinacea spp. |
Unkown |
KTG53 |
Diarrhoea alone |
Root chopped and soaked in warm water taken orally |
Human and Veterinary |
| |
Galinsoga parviflora Cav. |
Midirberbere, (Amh) |
KTG14 |
Anaemia with jaundice |
The flower is chopped and mixed with Monosonia longipes and warmed on and applied of gum of achy tooth |
Human |
| |
Galinsoga quadriradiata Cav. |
Mukala (M) |
KTG74 |
To detach retained fetal membrane and/or placenta |
Leaf chopped and mixed with Plumbango zeylanica and then drenched |
Veterinary |
| Geraniaceae |
Geranium aculeolatum Oliv. |
Abasanga medihanit (A, AM) |
KTG72 |
Anthrax |
Leaf chopped and rubbed on wounded part |
Veterinary |
| |
Geranium arabicum Forssk. |
Tushita (A) |
KTG26 |
Epizootic lymphangitis |
Root chopped and mixed with chopped root of Laggera tomentosa and one bear bottle drenched through left nose of horse. |
Veterinary |
| Poaceae |
Hyparrhenia hirta (L.) Stapf |
Goiti ebab” medihanit (B) |
KTG46 |
Snake bite/poison |
Plant material chopped and soaked in hot water and the filtrate drenched |
Human and Veterinary |
| Fabaceae |
Indigofera arrecta A.Rich. |
Wareami (A) |
KTG80 |
Anaemia with jaundice |
Leaf dried and smoked to patients |
Human |
| |
Indigofera trita L.f. |
Wusis (A) |
KTG01 |
To improve milk production of cows |
Root chopped, mixed with water and drenched |
Veterinary |
| Convolvulaceae |
Ipomoea eriocarpa R. Br. |
Choko (M) |
KTG40 |
Endoparasite |
Root chopped and mixed with water, then the filtrate is drenched and rest sediments are poured on the wound part |
Veterinary |
| Acanthaceae |
Justica dianthera Vell. |
Mitch(A, Amh) |
KTG51 |
Mitch |
The leaf apex boiled with water and the vapor inhaled and/or the filtrate drenched |
Human |
| |
Justicia diffusa Willd. |
Makaiso (A) |
KTG04 |
For coughing of equines |
Leaf chopped and mixed with cold water and drenched via nose |
Veterinary |
| Cucurbitaceae |
Lagenaria siceraria (Molina) Standl. |
Busino (M) |
KTG35 |
Diarrhoea and vomiting |
Leaf chopped and ground and the drench the filtrate |
Human |
| Asteraceae |
Laggera tomentosa Schultz Bip. |
Tushita (A) |
KTG71 |
Epizootic lymphangitis |
Root chopped and mixed with chopped root of Geranium arabicum and one bear bottle drenched through horses nose |
Veterinary |
| Verbenaceae |
Lantana Trifolia L. |
Yewoba medihanit (A) |
KTG55 |
Malaria (shivering type, vivax) |
Root chopped and soaked with water and mixed with local alcoholic drink (Areke) |
Human |
| Lamiaceae |
Leucas stachydiformis (Benth.) Hochst. ex Briq. |
Businae (M) |
KTG19 |
Anaemia with jaundice |
Leaf and bark chopped and drench the filtrate or inhalation |
Human |
| Onagraceae |
Ludwigia abyssinica A.Rich. |
Yechira ebab medihanit (Amh) |
KTG44 |
Snake bite/poison |
Stem and root mixed with other plants and applied orally |
Human |
| Cucurbitaceae |
Momordica foetida Schumach. |
Chekko (M,B) |
KTG03 |
Black leg |
Root chopped, soaked in water for half a day and a filtrate is drenched |
Veterinary |
| |
Momordica charantia L. |
Unknown (A) |
KTG90 |
Diarrhea and vomiting |
Leaf and root ground well and mixed with milk and taken orally |
Human |
| |
Momordica spp. |
Kill (M) |
KTG79 |
To detach fetal membrane |
Root dried, ground and mixed with Colocasia esculenta, all soaked in warm water and one cupful filtrate drenched |
Veterinary |
| Geraniaceae |
Monsonia parvifolia Schinz |
Not known (A) |
KTG58 |
Tooth ache |
Seed and leaf crushed and mixed with salt and Galinsoga parvifolia; made hot on fire with “enset leaf” and applied on gum. |
Human |
| Papilionaceae |
Mucuna melanocarpa Hochst |
Salabano (M) |
KTG86 |
For calf Ascariasis |
Leaf ground and mixed with water and drenched that induces diarrhea |
Veterinary |
| Solanaceae |
Nicotiana tabacum L. |
Bangiso(M) |
KTG78 |
Tick infestation |
Root chopped and mixed with water and dressed to the tick infested area on cow and calf |
Veterinary |
| Anacardiaceae |
Operculicarya gummifera (Sprague) Capuron |
Dorba (M) |
KTG38 |
Snake bite/poison |
Orally taken butt its preparation is not specified due to unwillingness of the respondent |
Human and Veterinary |
| Lamiaceae |
Orthosiphon sarmentosus A.J. Paton & Hedge |
Zititu (A) |
KTG67 |
Ascariasis |
Leaf chopped, soaked in water and a glass full filtrate drunken |
Human |
| Oxalidaceae |
Oxalis corniculata L. |
Dani (M) |
KTG02 |
Toxic |
Root chopped, cooked for two days and more and the paste rubbed on arrow tip to hunt wild animals |
Human and veterinary |
| Anacardiaceae |
Ozoroa insignis Delile |
Bussa (M) |
KTG39 |
For coughing of equines |
Bark dried, powdered and mixed with cold water and the filtrate drenched |
Veterinary |
| Geraniaceae |
Pelargonium alchemilloides (L.) Aiton |
Unkown |
KTG13 |
Constipation |
Root chopped and soaked in warm water taken orally |
Human |
| Rubiaceae |
Pentas suswaensis Verdc. |
Haromato (M) |
KTG63 |
Aba gorba “Black leg” |
Leaf chopped and mixed with boiled water and the filtrate is drenched |
Veterinary |
| Lamiaceae |
Plectranthus glabriflorus P.I.Forst. |
Gullo/Karika (A) |
KTG09 |
Evil eye |
Leaf soaked in hot water and drunken |
Human |
| |
Plectranthus globosus Ryding |
Chambuase (M) |
KTG60 |
Snake bite/poison |
Leaf chopped mixed with Alectra sessiliflora mixed in cold water and taken orally |
Human |
| Plumbaginaceae |
Plumbago auriculata Lam. |
Masilok (M) |
KTG81 |
For animal evil spirit |
Leaf chopped and soaked in water and the filtrated drenched and the remaining sediments pasted on the body |
Human and Veterinary |
| |
Plumbago caerulea Kunth |
Wugat medihanit (Amh) |
KTG68 |
Back and side pain |
Root and seed are chopped and mixed with hot water and onion |
Human |
| |
Plumbago pulchella Boiss. |
Not known (A) |
KTG12 |
Snake bite/poison |
Fresh leaf chopped and mixed with cold water |
Human and Veterinary |
| |
Plumbago spp. |
Misirich (M) |
KTG49 |
Evil eye in animals |
Leaf chopped and soaked in water and the filtrated drenched and the remaining sediments pasted on the body |
Veterinary |
| |
Plumbago zeylanica L. |
Telba (M) |
KTG75 |
To detach retained fetal membrane |
Seed ground by traditional mortar mixed with Galinsoga Parviflora and boiled with water and drenched |
Veterinary |
| Lamiaceae |
Premna oligotricha Baker |
Yewoba medihanit (A) |
KTG34 |
Malaria (non-shivering type, falciparium) |
Leaf collected and ground and mixed with water |
Human |
| |
Premna schimperi Engl. |
Bangizo(M) |
KTG21 |
Dermatophilous and mite infestation |
Root chopped and soaked in warm water over night and filtrate applied topically to treat dermatophytes and tick mite infestations |
Veterinary |
| |
Premna spp. |
Anchiphi (M) |
KTG57 |
Diarrhea in calf |
Leaf powdered and mixed with water and the filtrate drenched |
Veterinary |
| |
Pycnostachys meyeri Gürke ex Engl. |
Unkown (A) |
KTG83 |
Abdominal pain (children) |
Fresh root chopped and mixed with cold water and drenched |
Human |
| Rubiaceae |
Rytigynia spp. |
Golodo (M) |
KTG30 |
Typhoid (Micho) |
Leaf chopped and mixed with water and taken orally |
Human |
| Lamiaceae |
Salvia acuminata Ruiz & Pav. |
Anchino (M) |
KTG48 |
Diarrhoea alone |
Chewing the leaf |
Human |
| Fabaceae |
Senna spp. |
Diko (M) |
KTG84 |
Joint ache and breakage of bones |
Leaf rubbed on affected parts and some leaf chopped and soaked in warm water and drenched |
Human and Veterinary |
| Malvaceae |
Sida spp. |
Moishita (M) |
KTG25 |
Anti-parasitic/ to fatten calf |
Leaf chopped and soaked in water and the filtrate is drenched repeatedly |
Veterinary |
| Solanaceae |
Solanum bellum S. Knapp |
Ondod (M) |
KTG22 |
Coughing of equines(Busa) |
Root chopped and mixed with cold water and the filtrate drenched either by nose or mouth |
Veterinary |
| |
Solanum acaule Bitter |
Mushta (A) |
KTG62 |
Removes retained placenta |
Root chopped and mixed with cold water and the filtrate is applied nasally |
Veterinary |
| |
Solanum acuminatum Ruiz & Pav. |
raki (A) |
KTG82 |
To detach retained placenta |
Root chopped, mixed with cold water and drenched orally |
Human and Veterinary |
| |
Solanum incanum L. |
Garint (A) |
KTG06 |
Epizootic lymphangitis(tushita) |
Root chopped and mixed with cold water and drenched via nose |
Veterinary |
| |
Solanum spp. |
Danni (M) |
KTG50 |
Poisonous to animals |
Root chopped and concoction with water until paste is formed, rubbed on arrow tip & used for hunting |
Human and Veterinary |
| Bignoniaceae |
Stereospermum kunthianum Cham. |
Addi (M) |
KTG29 |
Abdominal pain |
Root chopped and mixed with water/coffee and taken in ad libitum |
Human |
| Asteraceae |
Tagetes spp. |
Businae (A) |
KTG88 |
Muscle cramp and joint pain |
Leaf rubbed well and oils from the leaf are swabbed on areas where pain felt. Fumigation is also possible. Boiled filtrate is drenched |
Human |
| |
Tagetes minuta L. |
Kawato (M) |
KTG36 |
Diarrhea and vomiting |
Leaf chopped and ground and the drench the filtrate |
Human |
| Euphorbiaceae |
Tragia doryodes M.G.Gilbert |
Anderta (A) |
KTG16 |
Anthrax |
The leaf is chopped and mixed with Dombya spp. and the filtrate taken orally |
Veterinary |
| Caryophyllaceae |
Vaccaria hispanica (Mill.) Rauschert |
Sanba tesha (M) |
KTG69 |
For contagious bovine pleuropneumonia and contagious caprine pleuropneumonia |
Root chopped and mixed with large amount of water. It gets bloody color (the bloody color indicates appropriate concentration), then drenched |
Veterinary |
| Verbenaceae |
Verbena officinalis L. |
Guni tesha (A) |
KTG56 |
Snake bite/poison |
Leaf squeezed by hand and mixed with water and drenched by water |
Human and Veterinary |
| Solanaceae |
Withania somnifera (L.) Dunal |
Buto/wogare (M) |
KTG24 |
Night mare |
Roots powdered and children smoked until they cough |
Human |
| Fabaceae |
Zornia apiculata Milne-Redh. |
Medhanit (A) |
KTG10 |
Abdomen ache and vomiting in children |
Fresh root chopped and mixed with cold water and drenched |
Human |
| |
Zornia glochidiata DC. |
Halimi (A) |
KTG11 |
Malaria |
Root bark is chopped and boiled/concoction with local drinks and boiled coffee leaf |
Human |
| Zornia latifolia Sm. | Medihanit (A) | KTG08 | Abdominal pain, vomiting | Fresh leaf chopped and mixed to form filtrate | Human |
*A=Aari; M=Maale; B=Benigna; Amh = Amharic.
This is the first study that documented plants used for disease control by the three ethnic groups in South Ethiopia. Previous studies have documented indigenous knowledge of medicinal plants and medicinal plant practices used in other parts of the country and by other ethnic groups including those in southern Ethiopia [24,25], northern and northwestern Ethiopia [8,26-28], and southwestern Ethiopia [29-31]. Our study thus complements existing studies but also extends them to pastoral areas where the ecology, practices, biodiversity, accessibility and cultural acceptability of medicinal plants are very different from the highlands. The aforementioned reports and our study taken together capture a wide range of different ethnic and social groups, which is a reflection of the richness of knowledge in use of plants for medicinal purposes, and the significance and cultural acceptability of plant based medicinal practice in large parts of Ethiopia. At the same time, this indicates that plant diversity and use of plant based remedies remain decisive for managing human and livestock health in countries like Ethiopia, as is the case for many other countries [7,32-46].
Ailments treated and ICF
Plants were clustered into 12 different groups based on the use citations by the informants and other end users (Table 1) in order to calculate the ICF. In our study, the ICF values range from 0.72 for evil eye and to 1.00 for rabies. Thus, all clusters had an ICF value greater than 0.5 and hence all of them could be considered for validation of bioactivity and isolation and characterization of the active principles by interested and potential researchers in each cluster.
The highest number of plant species were reported to be used for treatment of abdominal/stomach disorders and internal parasites (22 species, 24.2%), followed by evil eye spirit (11 species, 12.1%), malaria and anemia like syndrome with jaundice, and snake bite/poisoning (10 species, 10.9% each), skin conditions (skin infections and ecto-parasites) and removal of retained placenta (7 species, 7.7% each), coughing in equines and ruminants and pain related illness (5 species, 5.5% each), anthrax (4 species, 4.4%), mich and megagna (an ailment characterized with fever, headache and sweating) and black leg (3 species, 3.3% each) and rabies (1 species, 1.1%) as shown in Table 1.
Animal diseases are one of the major reasons for poor livestock performance in Ethiopia [33], and the use of conventional medicine by smallholder livestock owners is constrained by their high prices and inaccessibility. On the other hand, Ethiopia is characterized by having diverse ecology and diverse mix of socio-cultural and linguistic groups, which might have contributed to the existence of rich knowledge in managing and using large numbers of different medicinal plants against both human and livestock ailments [32]. Therefore, in the absence of use of modern medicine to treat livestock diseases in smallholder livestock production systems, the use of traditional medicinal plants will remain a vital component of Ethiopian livestock production for some years to come. For instance, ethnoveterinary uses of the plant species Caylusea abyssinica, Cissampelos mucronata, Cissampelos pariera, Desmodium dichotomum, Ipomoea eriocarpa, Justicia diffusa, Premna schimperi, and Zornia glochidiata are reported by these ethnic groups to be effective against selected ecto- and endo-parasites of livestock. Validation of the later through in vitro and in vivo assessment of their anti-parasitic properties is required to better inform their use by pastoralists and smallholder farmers. Furthermore, bioactivity evaluation of these plant species also help to isolate and purify the active principles by bio-assay guided fractionation for new drug development.
The ICF results could be useful in prioritizing medicinal plants for further scientific validation of plants and plant products [7,8,27,47-49], as pharmacologically effective remedies are expected from plants with higher ICF values [50,51]. Indeed, documentation of inherently rich traditional ethno-medicinal knowledge based on ICF values have provided valuable information on new pharmacological dimensions for better health care of livestock and humans regarding many ailments [50], and also assist conservation and management of rare, gradually vanishing important ethno-medicinal plant species. If validated, the claim for medicinal plants used in traditional medicine for a number of ailments of humans and livestock could provide new applications in supporting health care systems that are urgently needed. In our study, medicinal plant species claimed for anthrax, skin infection and external parasites, pain related illnesses and black leg were cited with the highest ICF values followed by those used to treat coughing in equines and ruminants, malaria and anemia like syndrome with jaundice, abdominal/stomach disorders and internal parasite and retained placenta. The lowest ICF value was recorded for the medicinal plant used to treat evil eye spirit. However, none were below 0.5, which would typically result from plant use to treat rare diseases [27,49], suggesting that our survey addressed medicinal plant species commonly used to treat common human and veterinary ailments in the study areas. Moreover, the highest numbers of plant species were reported to be used for treatment of abdominal/stomach disorders and internal parasites whereas the lowest number of medicinal plant species were reported for the treatment of rabies (Table 1). This implies that stomach disorders and endoparasite infections are likely the more common health problems of human and livestock in the three ethnic groups. Parasite-based health problems in human may be due to domestic hygiene, shared use of water from the same source for themselves and for their livestock, and zoonotic parasite infection. The parasitic health problem in livestock in the study areas could be associated with the ectoparasites particularly ticks and mange mites, increasing the risk for vector born diseases. The internal parasitic health problem in livestock in the study areas are a serious threat during humid season as the condition favors the infection, multiplication and transmission of endoparasites.
Habits of growth
Figure 3a shows that woody plants made up 50% of the growth form of the plants claimed by the healers for having medicinal properties (29% trees and 21% shrubs), followed by herbs (36%) and climbers (14%). The high proportion of woody plants in our survey is likely associated to the ability of trees and shrubs to withstand long dry seasons, thus resulting in their abundance and year round availability in arid and semi-arid areas. This finding is contrary to the general patterns seen in most medicinal plant inventories where herbs are the largest plant growth forms [23,25,27,53]. A high usage of herbs in some studies could be an indication of their abundance, especially in areas receiving year round rainfall. Thus, the variation in parts of medicinal plants used may be related to differences in seasonality though also arise from differences in socio-cultural beliefs, and practices of the healers of different regions or countries.
Figure 3.
Proportions of growth form (a) and form of use (b) of medicinal plants identified in South Omo for treatment of different human and livestock ailments in South Omo zone, southern Ethiopia.
Mode of preparation (form of use)
Concoction, filtrate (a liquid from which insoluble impurities have been removed), paste on (topical), pounded and smoke bath are common use forms or modes of preparations reported in our study, with concoction (71%) and filtrate (11%) as the major use forms of the plants cited (Figure 3b). The remedies are prepared using water (hot or warm), local drinks, boiled coffee or milk as a carrier and taken either orally or through inhalation of the vapor after boiling (smoke bath treatment). Within the total number of claimed medicinal plants, healers used 14 plants (15.4%) by mixing of two plants to treat selected ailments. For instance, Geranium arabicum mixed with Laggera tomentosa is used for the treatment of epizootic lymphangitis in animals; Droguetia iners mixed with Premna oligotricha is used for the treatment of malaria in humans, and Dombeya spp. mixed with Tragia doryodes is used for the treatment of anthrax. The frequent use of concoction and the mixing of two or more plants by healers could be associated with healer’s belief of synergistic effects of certain plant components for healing the illnesses. This finding is consistent with earlier reports [26,54,55] but disagrees with other studies where crushing and squeezing [27,28] and homogenizing and crushing [24] were the main use forms. It is likely that these differences are associated with the differences in culture and knowledge in different socio-cultural groups.
Parts of plant used
Almost all plant parts, including roots, leaves, stem, bark, fruits, young shoots and flowers, were cited for use in preparing the different remedies. However, roots followed by leaves represented the most common parts used (Figure 4a) for treating ailments in humans and livestock, respectively. Roots appeared to be the main plant part commonly used by the healers in the current study area. This could be associated with the fact that roots remain in the soil and are easily available, even during the long dry seasons in arid and semi-arid areas. In addition, the use of plants root could also be associated with early African beliefs in their powerful therapeutic effects. For example, early African diasporas in the Americas and those migrants to Caribbean countries during the colonial period used plant roots to protect against malaria and venereal diseases and to induce abortions, but also to prepare favorite household alcoholic drinks, as roots contributed to alcohol fermentation, color, flavor, and foam formation [20,56,57]. However, the use of medicinal plant roots, either for immediate use of treating ailments or for commercialization purpose to generate income, could also negatively contribute to local biological diversity and conservation because of complete plant removal from its natural habitat. The common use of leaf in the preparation of remedies could partly be due to the relative ease of finding this plant part. In agreement with our study, similar studies in other parts of Ethiopia reported that roots and leaves are indeed the most commonly used medicinal plant parts [27,28].
Figure 4.
Proportion of plant parts used for medicinal purposes (a) and route of administration of plant preparations (b) for treatment of human and livestock ailments in South Omo zone, southern Ethiopia.
Routes of administration and dosage used
Both internal and external applications were reported by the informants in the treatment of various human and livestock ailments in our study. The commonly reported routes of administration are oral (65%), followed by topical (15%), nasal (10%) and smoke bath treatment (10%; Figure 4b). The choice of oral administration may be related to the use of some solvents or additives (milk, butter, alcoholic drinks, boiled coffee, and food) that are commonly believed to serve as a vehicle to transport the remedies. The additives are also important to minimize discomfort, improve the taste and reduce adverse effects such as vomiting and diarrhoea, and enhance the efficacy and healing conditions [31]. Similar findings were reported by many other researchers, indicating the oral route as the most preferred mode of administration [25,28,58-64]. However, there is no consensus on the dosage used and frequency of the medication among healers. For example, the dosage varied according to the type of illness ranging from two spoonfuls (e.g. for treatment of anemia like syndrome with jaundice using concoct prepared from Cissampelos spp.) to a cup or glass full (e.g. for treating “busino” or abdominal pain using decoct from Centella asiatica).
Conclusion
This study showed that traditional medicine, mainly involving the use of medicinal plants, is playing a significant role in meeting the primary healthcare needs of the three ethnic groups. Acceptance of traditional medicine and limited access to modern healthcare facilities could be considered as the main factors for the continuation of the practice.
This field survey has documented 91 plant species distributed across 33 families and 57 genera as having medicinal properties against 34 human and livestock ailments as reported by healers from Aari, Maale and Bena-Tsemay ethnic groups, complementing previous studies from other ethnic groups in Ethiopia. The highest number of plant species was reported to be used for treatment of abdominal/stomach disorders and internal parasites. Woody plants (trees and shrubs) were the main form used, likely related to the long dry seasons typically occurring in the residential area of the ethnic groups studied. Concoction appeared to be the most popular use form in the current study. The most commonly used route of administration is oral. This study contributes to the enormous indigenous knowledge on medicinal plants and plant-based remedies practiced among ethnic groups, and it assists knowledge and practice preservation, which remain mostly with elderly traditional practitioners. Furthermore, the information generated will also inform future validation studies, so as to increase the acceptability of plant-based remedies in human and animal health care systems both nationally and internationally.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
KT, ED and AT carried out field survey and data analysis, ED and KT prepared the initial structure of the draft manuscript and KT, ED and AT revised the manuscript critically to the present form. GG introduced us to the people in the study and was involved in a preliminary survey. SA and JH secured funding for the project, assisted data interpretation, manuscript structuring and provided input to previous drafts resulting in the present form. All authors read the final manuscript and agreed on its submission.
Contributor Information
Ketema Tolossa, Email: ketema_tolossa@yahoo.com.
Etana Debela, Email: etana_debela@yahoo.com.
Spiridoula Athanasiadou, Email: spiridoula.athanasiadou@sruc.ac.uk.
Adugna Tolera, Email: atolera@yahoo.com.
Gebeyehu Ganga, Email: g.ganga2009@gmail.com.
Jos GM Houdijk, Email: jos.houdijk@sruc.ac.uk.
Acknowledgements
This work was supported by the UK Biotechnology and Biological Sciences Research Council (BBRSC), Department for International Development (DFID) and Scottish Government (SG) under the umbrella of their CIDLID initiative (BB/H009299/1). RCBP-NARF provided support for preliminary survey work. We are also thankful to the informants from the three ethnic groups who without reservation shared their medicinal plant knowledge with us, the elders and the local administration for their support in facilitating the interview process. We also thank the staff of the National herbarium of Addis Ababa University for plant identification.
References
- Santos García-Alvarado JS, Verde-Star MJ, Heredia NL. Traditional uses and scientific knowledge of medicinal plants from Mexico and Central America. Journal of Herbs, Spices & Medicinal Plants. 2001;8:37–89. [Google Scholar]
- Berkes F, Colding J, Folke C. Navigating social-ecological systems: building resilience for complexity and change. Cambridge, UK: Cambridge University Press; 2003. [Google Scholar]
- Awas T, Demissew S. In: Proceedings of the 16th International Conference of Ethiopian Studies. Svein E, Harald A, Birhanu T, Shiferaw B, editor. Trondheim, Norway: NTNU-Trykk Press; 2009. Ethnobotanical study of medicinal plants in Kafficho people, southwestern Ethiopia; pp. 711–726. 3. [Google Scholar]
- Omoruyi BE, Bradley G, Afolayan AJ. Ethnomedicinal survey of medicinal plants used for the management of HIV/AIDS infection among local communities of Nkonkobe Municipality, Eastern Cape, South Africa. Journal of Medicinal Plants Research. 2012;6:3603–3608. [Google Scholar]
- Bussmann WR, Swartzinsky P, Worede A, Evangelista P. Plant use in Odo-Bulu and Demaro, Bale region Ethiopia. J Ethnobiol Ethnomed. 2011;7:28. doi: 10.1186/1746-4269-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sindiga I, Nyaigotti-Chacha C, Kanunah MP. Traditional medicine in Africa. Nairobi: East Africa Educational Publishers; 1995. pp. 132–139. [Google Scholar]
- Moshi MJ, Otieno DF, Mbabazi PK, Weisheit A. The Ethnomedicine of the Haya people of Bugabo ward, Kagera Region, north western Tanzania. J Ethnobiol Ethnomed. 2009;5:24. doi: 10.1186/1746-4269-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giday M, Teklehymanot T, Abebe A, Yalemtsehay M. Medicinal plants of the Shinasha, Agew-awe and Amhara peoples in northwest Ethiopia. J Ethnopharmacol. 2007;110:516–525. doi: 10.1016/j.jep.2006.10.011. [DOI] [PubMed] [Google Scholar]
- Abebe D. Traditional medicine in Ethiopia. The attempt being made to promote it for effective and better utilization. SINET: Ethiopian Journal of Science. 1986;9:61–69. [Google Scholar]
- Gebremariam T, Asres K. Applied Research in Medicinal Plants. Addis Ababa: Biodiversity Institute; 1998. (Programme and Abstract of National Workshop on “Biodiversity Conservation and Sustainable Use of Medicinal Plants in Ethiopia”, April 28–May 1). [Google Scholar]
- Debella A, Abebe D, Urga K. Traditional medicine in Ethiopia: perspectives and developmental efforts. Journal of Ethiopian Medical Practice. 2001;1:114–117. [Google Scholar]
- Addis G, Abebe D, Urga K. A survey of traditional medicine in Shirika District, Arsi Zone, Ethiopia. Ethiopian Pharmaceutical Journal. 2001;19:30–47. [Google Scholar]
- Belayneh A, Asfaw Z, Demissew S, Bussa FN. Medicinal plants potential and use by pastoral and agro-pastoral communities in Erer Valley of Babile Woreda, Eastern Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2012;8:12. doi: 10.1186/1746-4269-8-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekele D, Asfaw Z, Petros B, Tekie H. Ethnobotanical study of plants used for protection against insect bite and for the treatment of livestock health problems in rural areas of Akaki District, Eastern Shewa, Ethiopia. Topclass Journal of Herbal Medicine. 2012;1:40–52. [Google Scholar]
- Gebre Michael Y, Hadgu K, Ambaye Z. A report on addressing pastoralist conflict in Ethiopia: The case of the Kuraz and Hamer sub-districts of South Omo zone. 2005. (Africa Peace Forum, Ethiopian Pastoralist Research and Development Association, Interafrica Group, Saferworld, August, 2005).
- Abebe D, Zewdu M, Demissie A. conservation and sustainable use of medicinal plants in Ethiopia Proceeding of the National Workshop on Biodiversity Conservation and Sustainable Use of Medicinal Plants in Ethiopia. Addis Ababa: IBCR; 2002. Biodiversity conservation of medicinal plants: Problem and prospects; pp. 198–203. [Google Scholar]
- Giday M, Asfaw Z, Woldu Z. Medicinal plants of Meinit ethnic group of Ethiopia. An ethnobotanical study. Journal of Ethnopharmacology. 2009;124:513–521. doi: 10.1016/j.jep.2009.05.009. [DOI] [PubMed] [Google Scholar]
- Diress B. Climate change impact and adaptation in South Omo Zone, Ethiopia: MSc thesis. Netherlands: Wageningen University; 2012. [Google Scholar]
- Central Statistics Agency. Administrative Report on 2007 population and housing census of Ethiopia. Addis Ababa, Ethiopia; 2012. [Google Scholar]
- Heinrich M, Ankli A, Frei B, Weimann C, Sticher O. Medicinal plants in Mexico: Healers’ consensus and cultural importance. Soc Sci Med. 1998;47:1859–1871. doi: 10.1016/s0277-9536(98)00181-6. [DOI] [PubMed] [Google Scholar]
- Cotton CM. Ethnobotany: Principles and Applications. New York, USA: John Wiley and Sons; 1996. [Google Scholar]
- Fransworth NR, Soejarto DD. In: The Conservation of medicinal plants. Akerele O, Heywood V, Synge H, editor. Cambridge, UK: Cambridge University press; 1991. Global importance of medicinal plants; pp. 25–51. 8. [Google Scholar]
- Bannister K, Prophet River Ethnobotany. A report on traditional plant knowledge and contemporary concerns of the Prophet River First Nation. Northeastern British Colombia: Prophet River First Nation and Prophet River Contracting Ltd; 2006. pp. 1–53. [Google Scholar]
- Bekalo TH, Wondmatas SD, Woldemariam ZA. An ethno botanical study of medicinal plants used by local people in the low lands of Konta Special Woreda, SNNPR, Ethiopia. J Ethnobiol Ethnomed. 2009;5:26. doi: 10.1186/1746-4269-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesfin F, Demissew S, Teklehymanot T. An ethno botanical study of medicinal plants in Wonago Woreda, SNNPR, Ethiopia. J Ethnobiol Ethnomed. 2009;5:28. doi: 10.1186/1746-4269-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yirga G. Ethnobotanical study of medicinal plants in and around Alamata, southern Tigray, North Ethiopia. Curr Res J Biol Sci. 2010;2:338–344. [Google Scholar]
- Teklehymanot T, Giday M. Ethnobotanical study of medicinal plants used by people in Zegie peninsula, northwestern Ethiopia. J Ethnobiol Ethnomed. 2007;3:12. doi: 10.1186/1746-4269-3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filate T, Gedif T, Asres K, Gebere-Mariam T. Ethnomedical survey of Berta ethnic group Assosa zone, Benishangul-Gumuz regional state, mid-west Ethiopia. J Ethnobiol Ethnomed. 2009;5:14. doi: 10.1186/1746-4269-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yineger H, Yewhalaw D. Traditional medicinal plant knowledge and use by local healers in Sekoru District, Jimma zone, southwestern Ethiopia. J Ethnobiol Ethnomed. 2007;3:24. doi: 10.1186/1746-4269-3-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yineger H, Yewhalaw D, Teketay D. Ethnomedicinal plant knowledge of the Oromo ethnic group in southwestern Ethiopia. Journal of Ethnobotanical and Ethnomedicine. 2008;4:11. doi: 10.1186/1746-4269-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etana B. Ethnobotanical study of traditional medicinal plants of Goma Woreda, Jimma zone of Oromia region. Ethiopia: MSc Thesis, Addis Ababa University; 2010. [Google Scholar]
- Assefa B, Glatzel G, Buchmann C. Ethnomedicinal uses of Hagenia abyssinica (Bruce) J.F. Gmel among rural communities of Ethiopia. J Ethnobiol Ethnomed. 2010;6:20. doi: 10.1186/1746-4269-6-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teshale S, Merga B, Girma A, Ensermu K. Medicinal plants in the ethnoveterinary practice of Borana pastoralists, southern Ethiopia. International Journal of Applied Research and Veterinary Medicine. 2004;2:220–225. [Google Scholar]
- Di Stasi LC, Oliveiraa GP, Carvalhaesa MA, Queiroz-Juniora M, Tiena OS, Kakinamia SH, Reisb MS. Medicinal plants popularly used in the Brazilian Tropical Atlantic Forest. Fitoterapia. 2002;73:69–91. doi: 10.1016/s0367-326x(01)00362-8. [DOI] [PubMed] [Google Scholar]
- Devkota MP. Mistletoes of Khimti forest, Ramechaap district, Nepal. Banko janakari. 1997;7:52–53. [Google Scholar]
- Gerald B, Hammond Irma D, Villegas F, Abraham J, Vaisberg. A survey of traditional medicinal plants from the Callejo’n de Huaylas, Department of Ancash, Peru. J Ethnopharmacol. 1998;61:17–30. doi: 10.1016/s0378-8741(98)00009-9. [DOI] [PubMed] [Google Scholar]
- Oyedemi SO, Bradley G, Afolayan AJ. Ethnobotanical survey of medicinal plants used for the management of diabetes mellitus in the Nkonkobe municipality of South Africa. Journal of Medicinal Plants Research. 2009;3:1040–1044. [Google Scholar]
- Tchacondo T, Karou SD, Batawila K, Agban A, Ouro-Bang’na K, Anani KT, Gbeassor M, Comlan Souza CD. Herbal remedies and their adverse effects in Tem tribe traditional medicine in Togo. African Journal of Traditional Complement Alternative Medicine. 2011;8:45–60. doi: 10.4314/ajtcam.v8i1.60522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qadir S, Dixit AK, Dixit P. Use of medicinal plants to control Haemonchus contortus infection in small ruminants. Veterinary World. 2010;3:515–518. [Google Scholar]
- Githiori JB. Evaluation of anthelmintic properties of ethnoveterinary plant preparations used as livestock dewormers by pastoralists and small holder farmers in Kenya. Doctoral thesis Swedish University of Agricultural Sciences Uppsala; 2004. [Google Scholar]
- Gakuubi MM, Wycliffe W. A survey of plants and plant products traditionally used in livestock health management in Buuri district, Meru County, Kenya. J Ethnobiol Ethnomed. 2012;8:39. doi: 10.1186/1746-4269-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abel C, Kofi K. An exploratory ethnobotanical study of the practice of herbal medicine by the Akan peoples of Ghana. Altern Med Rev. 2005;10:112–122. [PubMed] [Google Scholar]
- Fajimi AK, Taiwo AA. Herbal remedies in animal parasitic diseases in Nigeria. Afr J Biotechnol. 2005;4:303–307. [Google Scholar]
- Ribeiro A, Romeiras MM, Tavares J, Faria MT. Ethnobotanical survey in Canhane village, district of Massingir, Mozambique: medicinal plants and traditional knowledge. J Ethnobiol Ethnomed. 2010;6:33. doi: 10.1186/1746-4269-6-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamoga D. Some pharmacological activities of selected medicinal plant species used for treating cattle diseases in Kabira sub-county. Rakai district: MSc Thesis Makerere University, Tanzania; 2010. [Google Scholar]
- Teng Y, Guo H, Liang Z, Shu Z, Li Z, Wu W. Ethnobotanical survey of medicinal plants and their utilization in Shaanxi Province, China. Journal of Medicinal Plants Research. 2011;5:1762–1778. [Google Scholar]
- Subramanyam R, Steven NG, Murugesan M, Balasubramaniam V, Muneer M. Consensus of the ’Malasars’ traditional aboriginal knowledge of medicinal plants in the Velliangiri holy hills, India. J Ethnobiol Ethnomed. 2008;4:8. doi: 10.1186/1746-4269-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley G, Afolayan AJ. Ethnobotanical survey of medicinal plants used for the management of diabetes mellitus in the Nkonkobe municipality of South Africa. Journal of Medicinal Plants Research. 2009;3:1040–1044. [Google Scholar]
- Tabuti JR, Kukunda CB, Kaweesi D, Kasilo OM. Herbal medicine use in the districts of Nakapiripirit, Pallisa, Kanungu, and Mukono in Uganda. J Ethnobiol Ethnomed. 2012;8:35. doi: 10.1186/1746-4269-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trotter RT, Logan MH. In: plants in Indigenous Medicine and Diet. Etkin NL, editor. Bedford Hill, NY, USA: Redgrave Publishing Company; 1986. Informants consensus: a new approach for identifying potentially effective medicinal plants; pp. 91–112. [Google Scholar]
- Etuk EU, Mohammed BJ. Informant consensus selection method: reliability assessment on medicinal plants used in north western Nigeria for the treatment of diabetes mellitus. African Journal of Pharmacy and Pharmacology. 2009;3:496–500. [Google Scholar]
- Upadhyay B, Singh KP, Kumar A. Ethno-veterinary uses and informants’ consensus factor of medicinal plants of Sariska region, Rajasthan, India. J Ethnopharmacol. 2011;133:14–25. doi: 10.1016/j.jep.2010.08.054. [DOI] [PubMed] [Google Scholar]
- Teklehymanot T, Giday M, Medhin G, Mekonnen Y. Knowledge and use of medicinal plants by people around Debre Libanos monastery in Ethiopia. J Ethnopharmacol. 2007;111:271–283. doi: 10.1016/j.jep.2006.11.019. [DOI] [PubMed] [Google Scholar]
- Abebe D, Ayehu A. Medicinal plants and Enigmatic health practices of Northern Ethiopia. Addis Ababa, Ethiopia: B.S.P.E; 1993. [Google Scholar]
- Lal SD, Yadav BK. Folk medicines of Kurukshetra district (Hrayana), India. Econ Bot. 1983;37:299–305. [Google Scholar]
- VanAndel T, Mitchell S, Volpato G, Vandebroek I, Swier J, Ruysschaer S, Jiménez CAR, Raes N. In search of the perfect aphrodisiac: Parallel use of bitter tonics in West Africa and the Caribbean. J Ethnopharmacol. 2012;143:840–850. doi: 10.1016/j.jep.2012.08.008. [DOI] [PubMed] [Google Scholar]
- Voeks RA. In: Mobility and migration in indigenous Amazonia: contemporary ethnoecological perspectives. Alexiades M, editor. London: Beghahn Books; 2009. Traditions in Transition: African diaspora ethnobotany in Low land South America; pp. 275–294. [Google Scholar]
- Nalule AS, Mbaria JM, Olila D, Kimenju JW. Ethnopharmacological practices in management of livestock helminthes by pastoral communities in the drylands of Uganda. 2011. (Livestock Research for Rural Development Newsletter).
- Bhattarai S, Chaudhary RP, Quave CL, Taylor RS. The use of medicinal plants in the trans-Himalayan arid zone of Mustang district, Nepal. J Ethnobiol Ethnomed. 2010;6:14. doi: 10.1186/1746-4269-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addisie Y, Yared D, Kumar PA, Tomas Z, Awol A. Traditional medicinal plants used by people in Libo-Kemkem district, south Gondar, Ethiopia. Asian Journal of Agricultural Sciences. 2012;4:171–176. [Google Scholar]
- Garcia D, Domingues MV, Rodrigues E. Ethnopharmacological survey among migrants living in the Southeast Atlantic Forest of Diadema, São Paulo, Brazil. J Ethnobiol Ethnomed. 2010;6:29. doi: 10.1186/1746-4269-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lulekal E, Kelbessa E, Bekele T, Yineger H. An ethnobotanical study of medicinal plants in Mana Angetu district, southeastern Ethiopia. J Ethnobiol Ethnomed. 2008;4:10. doi: 10.1186/1746-4269-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panghal M, Vedpriya Arya V, Yadav SS, Kumar S, Yadav JP. Indigenous knowledge of medicinal plants used by Saperas community of Khetawas, Jhajjar district, Haryana, India. J Ethnobiol Ethnomed. 2010;6:4. doi: 10.1186/1746-4269-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otang WM, Grierson DS, Ndip RN. Ethnobotanical survey of medicinal plants used in the management of opportunistic fungal infections in HIV/AIDS patients in the Amathole district of the Eastern Cape Province, South Africa. Journal of Medicinal Plants Research. 2012;6:2071–2080. [Google Scholar]