Abstract
The purpose of this article is to describe 3 foundational studies and how their results were used to formulate, design, and test a novel partner intervention for implementation in the immediate post-ICD (implantable cardioverter defibrillator) period after returning home. Nursing’s expanding role into chronic illness management in the creation of evidence-based practice is highlighted. A randomized clinical trial comparing 2 intervention programs is being conducted with patients who receive an ICD for the first time and their intimate partners. Primary outcomes are physical functioning, psychological adjustment, relationship impact, and health care utilization.
Keywords: evidence-based practice, implanted defibrillator, intervention, nursing practice, social cognitive theory, sudden cardiac arrest
The use of the implantable cardioverter defibrillator (ICD) for life-threatening ventricular arrhythmias is standard therapy, because of its superiority over medical treatment in preventing recurrent cardiac arrest.1 New ICD indications for heart failure have been proposed to prevent sudden death by a number of clinical trials.2–4 This has resulted in a dramatic increase in the number of ICDs implanted, making relevant the testing and generalizability of intervention programs for both patients and their partners. Post-ICD implantation requires an adaptation period; 13% to 38% of patients experience severe anxiety, 34% to 43% report depression, and 15% develop posttraumatic stress disorder (PTSD) after receiving ICD shocks.5
In recovery from life-threatening cardiac illness, the intimate partners’ experience is known to influence that of the recovering patient.4 In addition, the health status of the intimate partner at the time of the patient’s life threatening event influences the partner’s ability to offer the support needed to make a positive recovery.6 Intimate partners of ICD patients have been adversely affected when the patient receives an ICD shock.7 In the last decade, cardiac surgery techniques, the management of congestive heart failure, and the treatment of cardiac arrhythmias have changed dramatically. These changes have resulted in shorter hospital stays, use of new medications and technological devices, an increasingly older population of cardiac patients, and more complex treatment regimens.8 Attending to the needs of the family after a cardiac illness is important aspect of the nurse’s role because the patient’s psychological adjustment is linked to family function,9 patient adherence to risk factor modification is associated with spousal anxiety and marital function, and caregiver strain and marital quality is related to increased mortality in older caregivers.10,11 Addressing issues that cause distress and increase psychological burden in partners are likely to improve patient outcomes.
Nursing is concerned with the diagnosis and treatment of human responses to health problems, health promotion and optimization, and disease prevention.12 Nurses play a central role in developing interventions to enhance response to illness, adaptation to illness conditions, and the ability to live with chronic illness. In particular, nurse scientists have generated the majority of evidence related to adaptation of patients to sudden cardiac arrest (SCA) and to ICD implantation and recovery. Additionally, nurse scientists have developed and tested behavioral and psychosocial interventions designed to enhance quality of life and improve patient health outcomes after ICD implantation. Now needed in clinical practice are theoretically driven, evidence-based interventions with demonstrated efficacy for improved patient and family outcomes. Yet, to date, there have been no randomized trials testing interventions to assist the partner of patients who receive an ICD, producing dramatic gaps in health care, which nursing is well situated to address. Promoting changes and expansions in nurses’ scope of practice requires nursing leadership in both practice and educational reform.
In our current health care delivery system, nurses provide the greater part of care to patients and families with heart disease in the acute care situation. To a large extent, however, nurses are less involved in chronic illness management at home and in the community. The recent Institute of Medicine Report on “The Future of Nursing: Leading Change Advancing Health” reaffirms the need for nursing’s involvement in managing chronic illness, coordinating care among clinicians and health care agencies, and preventing occurrences of acute care episodes and disease progression resulting in rehospitalization.13 Tagney14 reported that 85% of nurses caring for patients with an ICD in the hospital were not confident that they could prepare patients for living at home with an ICD; 37% did not understand ICD precautions after going home, and 64% were not aware of lifestyle changes required to live successfully with an ICD. In addition, Sears et al15 reported that nurses and physicians understand concerns of patients and families after receiving an ICD, but fewer than 50% of providers had the necessary skills to assist patients in managing anxiety, fear and worry, depression, returning to a sexual relationship, overprotectiveness of the spouse, or daily activities such as driving issues. Therefore, nurses are in a key position to effect important health outcomes for patients and partners after ICD implantation, but they must possess basic knowledge and skills that are common to the first year after receipt of an ICD.
The purpose of this article is to describe 3 foundational studies and how the results were used to formulate, design, and test a novel partner intervention for implementation in the immediate post-ICD implantation period after returning home. First, what is known about partner responses after the patient receives an ICD will be discussed. Then, each study will be discussed in brief, and how the 3 studies were linked together to provide the necessary background and rationale for the design of a new partner intervention will be described. Finally, implications for nursing will be suggested.
In describing partner physical and mental health after the patient received an ICD, 2 recent reports highlight these issues. Spouses of patients participating in the amiodarone versus implantable defibrillator (AVID) trial16 showed a decline in self-reported physical health from baseline ICD insertion to 12 months later, with reduction in depression and anxiety reported over the same period. Physical health was reportedly lower in partners with older age and higher disease burden. Notably, mental health declined in those partners where the patient received an ICD shock. A second report about patient-partner pairs within 30 months of ICD implantation17 found no statistical differences in anxiety or marital adjustment between patients and partners. Partners, however, reported more worry over an ICD shock than the patient.
Overprotectiveness, stress, anxiety, fear, anger, depression, and despair are reported by partners of patients who have experienced cardiac events.6,18,19 Feelings of helplessness, changes in family roles and life patterns, and lack of family support strain the family system making it difficult to meet the care demands needed for successful recovery.18,20–22 Ocampo23 noted that although the patient eventually accepts the device and lifestyle changes, family members appear to have a difficult time doing so. Pycha et al24 reported that within 17 months after ICD implantation, 81% of partners felt that the ICD was a life extender and 66% felt the ICD was a source of security. One third of spouses were concerned that expressing strong emotions might provoke an ICD shock. Even though patients and partners expressed positive perceptions about the ICD, 94% of patients reported increased preoccupation with the heart more than 1 year after ICD implantation. A longer term worry of both patients and partners was the extended functioning of the ICD battery and the availability of experienced providers should they travel.
Reports of the effects of the ICD on intimate relationships suggested that SCA contributed to marital strain and reduced sexual frequency within couples.25 Spouses of ICD patients noticed increased anxiety, anger, irritability, and dependency in their mates after SCA. Both spouses and patients expressed the need for more information from health care professionals concerning the cardiac arrest event and how to make needed adjustments.26,27 Family social support was noted to be especially low throughout the first year after ICD implantation.28 Doolittle and Sauve29 found differences in perceptions about ICD recovery between spouses and patients. Spouses who witnessed the cardiac arrest had a greater degree of protectiveness toward the patient, often creating conflicts between the couple. In addition, 78% of individuals were sexually active before the ICD, with 55% reporting resumption of their sexual relationship after the ICD. Both patients and partners report similar issues about returning to sex: fear in returning to sex by the partner (56%), lack of interest in sex (29%), fear of ICD firing during sex (29%), and fear of cardiac arrest if the ICD did not fire (29%). Importantly, health providers rarely discussed sexual information with patients who received an ICD.30
Investigations demonstrate that surviving cardiac arrest and receiving an ICD results in significant changes in an individual’s physical, social, and psychological functioning during the first year postimplantation.25,31,32 After a patient suffers cardiac arrest and receives an ICD, partners are often responsible for caring for the patient at home with little guidance or assistance from health care providers. Both patients and their partners are anxious about what the ICD will do, how to live with it successfully, what to do if an ICD shock occurs, and how to adapt to living with a serious cardiac diagnosis. Many adjustments need to occur at home in ICD recovery, the patient often requires assistance, and partners are not sure what will be most helpful to the patient. This psychological distress, coupled with demands on the partner to assist the patient with ICD recovery, places the partner at risk for physical and mental health problems.
To address such concerns, we previously developed and tested an intervention to improve patient outcomes following SCA and ICD implantation.33,34 Our earlier intervention study was not designed to intervene with intimate partners of patients who receive an ICD. Rather, the intervention targeted self-management of patient responses that contribute to caregiver burden: anxiety, symptoms, fear of dying, depression, self-efficacy, and ICD shocks. At the conclusion of the study, 72% of patients requested more information about helping their intimate partner adjust to the experience. Because of this identified need and data suggesting that partners of patients who receive ICDs are equally or more distressed than patients,35 we conducted 3 studies that led to the formulation and testing of a new intervention to assist the intimate partner of patients with their own concerns, health, and emotional reactions. This newly developed partner intervention is being formally tested in a randomized clinical trial sponsored by the National Heart, Lung, and Blood Institute (5R01 HL086580, Patient and Partner Intervention to Improve Outcomes after an ICD, NCT01252615). The original patient intervention is combined with the new partner intervention (called patient+partner, ie, P+P intervention) and tested against the patient-only (P-only) intervention. The results of this ongoing investigation will demonstrate if actively involving the partner in the patient’s recovery and addressing the physical and mental health of the partner will result in improved health outcomes and reduced costs for both the partner and patient.
THREE FOUNDATIONAL STUDIES
We conducted 3 investigations to provide the background and rationale to demonstrate the need to test an intervention for intimate partners of patients who receive an ICD. These studies provide information regarding the following: (1) partner domains of concern36 that underpin the content of the partner intervention; (2) the partner’s physical and mental health35 that describes critical partner outcomes in the first year post-ICD implant; and (3) acceptability, feasibility, and projected effect sizes based on pilot test results of the partner intervention. Each preliminary study is described briefly below with key contributions of each study in the design of the partner intervention.
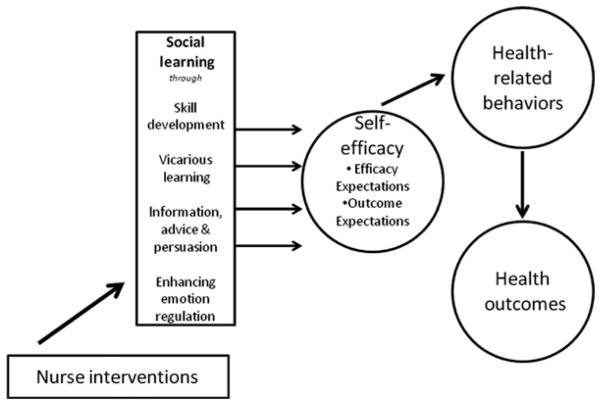
Bandura’s social cognitive theory37 was used to structure the design of the preliminary studies and the partner intervention (see Figure 2). Self-efficacy, a central concept, is a conviction about one’s ability to execute a particular behavior that is required to produce a particular outcome. Behavioral change and maintenance are functions of both expectations about the outcomes that will result from engaging in a behavior (outcome expectations) and expectations about one’s ability to execute the behavior required (efficacy expectations). Self-efficacy influences aspects of behavior, including acquisition of new behaviors, inhibition of existing behaviors, and resumption of behaviors.
Figure 2.
Schematic of key variables in Bandura’s Social Cognitive Theory used to design new post-ICD intervention for partners.38
Efficacy expectations are increased through the following: (1) performance attainment (learning by doing); (2) vicarious experiences (observing others or role models); (3) verbal persuasion from expert sources; and (4) minimizing emotional arousal (emotion regulation, reducing anxiety). Successful performance of difficult tasks results in increased self-efficacy and is the most powerful source of efficacy expectations. Successive mastery of tasks aids development and refinement of coping skills. Observing another person demonstrate mastery over situations that are perceived as difficult or feared can enhance one’s efficacy expectations. Effective modeling, however, must demonstrate mastery over difficult situations through determined effort and the person modeling the behavior must be perceived as similar to the observer (eg, similar in age, gender, or other characteristics). Modeled behaviors that have rewarding and definitive outcomes are more effective than modeling that has neutral or ambiguous outcomes. Verbal persuasion from heath care providers or others viewed as “experts” can aid individuals to change behaviors. Finally, high emotional arousal impairs behavioral performance because people are less attentive to situational cues and more likely to expect failure when emotionally distressed.
Study 1: Partner domains of concern
The purpose of this initial study was to generate a grounded theory of patient and partner recovery during the first year after SCA and ICD insertion. A grounded theory-quantitative research method was used, the details of which have been reported.36,39 Briefly, ICD patients (n = 15) and their intimate partners (n = 15) were followed prospectively from hospitalization through the first year after an ICD implant. The mean age of SCA survivors was 57 ± 11 years, and the mean age of intimate partners was 53 ± 9 years. All SCA survivors experienced primary ventricular fibrillation at the time of SCA and subsequently underwent ICD implantation during hospitalization. Intimate partners were primarily spouses of SCA survivors (13 women and 2 men), although 2 couples were not married but were living together at the beginning of the study. Fourteen couples were Caucasian (83%) and 1 couple was African American. Eight (53%) of the SCA survivors and 6 (40%) of the partners were employed full time at the time of cardiac arrest. Of these, 2 survivors retired from work during the 1-year recovery period.
Data were collected with in-person interviews with each individual and one intimate partner at 5 times: hospital discharge, 1 month, 3 months, 6 months, and 12 months. Interviews were audio-recorded, transcribed, and analyzed using constant comparative analysis and thematic coding. Themes of recovery were constructed and validated for each the patient and the partner groups at each of the 5 time points. The results particularly pertinent to the development of the interventions currently being tested included the following: (1) domains of concern of ICD patients and (2) domains of concern of intimate partners after ICD implantation. Seven domains of concern of ICD patients and 8 domains of concern for partners amenable to change through intervention were derived from the in-depth interviews. The domains of concern for intimate partners form the basis for the content of the current P+P intervention program (Figure 1).
Figure 1.
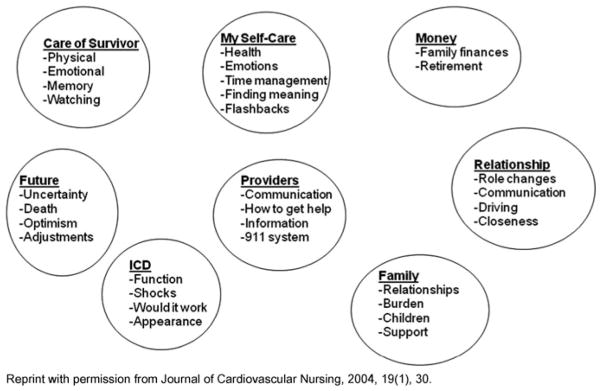
Domains of concern: Partner.
The 8 domains of concern for the intimate partner included the following: Care of the Survivor concerns centered around physical care, emotional care, memory loss, monitoring, and how the survivor had changed. Partner Self-Care concerns focused on meeting their own physical and emotional needs while caring for the survivor, time management, finding meaning in the event, and dealing with flashbacks. The impact of SCA on the intimate Relationship focused on changes in communication, roles, and driving responsibilities between the couple. Financial changes (Money) imposed on the family as a result of the survivor being hospitalized and out of work for a prolonged period of time was a concern during the first 6 months after SCA. Partners had many concerns about the function and maintenance of the ICD, including how to prevent and respond to ICD shocks. An Uncertain Future was produced by the cardiac arrest experience in relation to adjustments needed to make a full recovery, the possibility of recurrent SCA in the patient, and overall prognosis. Dealing with Health Care Providers was a stressful experience for intimate partners in acquiring adequate information to help with recovery at home and in receiving support for themselves. Family concerns of intimate partners encompassed the areas of mobilizing help and support that was needed from the family, communicating what had happened, and dealing with conflicts of past family relationships in the context of illness. These 8 domains of concern, along with evidence about partner health issues, serve as the important content foundation for the partner intervention36 that was pilot tested in study 3.
Study 2: Physical and mental health of partners of patients after an ICD
The purpose of this study was to describe the physical and mental health of intimate partner’s of persons receiving an ICD for the first time35 over a 1-year period. A prospective longitudinal repeated-measures design was used, with data collected at hospital discharge, and at 1, 3, 6, and 12 months after implantation. Key outcome variables representing partners’ physical functioning, psychological adjustment, health care utilization, and relationship impact were collected at each time period. Complete data were available for analysis with 100 intimate partners from 127 of patients who received a first time ICD for secondary prevention reasons. Intimate partners were 60.96 (±12.87) years of age, among whom 82% were female, 96.9% Caucasian, 29.6% college graduates, and 33.3% employed outside the home in clerical or managerial positions. The average annual household income for 44% of the sample was more than $49,999 per year.
Intimate partners had a number of health concerns of their own at the time of ICD implant in the patient. The most common health problems were hypertension in 38%, osteoarthritis in 36%, and thyroid disease in 15% of patients. The average Charlson comorbidity score was 2.27, meaning partners were dealing with an average of 2 chronic health conditions at the time they entered the study. The most common medication being taken by partners was for hypertension. The average number of medications taken was 2.96 ± 2.6 per person.
Intimate partners of ICD patients reported declines in their general physical health (SF-12 physical component score [PCS]) over the 1 year, P = .007. Physical symptom frequency (P = .04) in the partner also declined in the year after cardiac arrest. The decline in SF-12 PCS health averaged 3 points, similar to that reported by Jenkins et al.16 Post-hoc analyses revealed that declines were highly significant at the time periods between baseline to 3 months (P = .002) and baseline to 12 months (P = .002). The top 5 physical symptoms reported by partners included feeling rundown (62%), headaches (36%), low back pain (33%), nausea and upset stomach (28%), and soreness of muscles (26%). Throughout the 12-month period, feeling rundown remained the most commonly reported symptom by partners.
General mental health (SF-12 mental component score [MCS]) in intimate partners improved from hospital discharge throughout 1 year (P = .03). Anxiety and depression in intimate partners decreased during the first year, with anxiety (P = .002) and depression (P = .001) significantly reduced over time. Levels of anxiety reported by intimate partners at hospital discharge were relatively high (M = 39.91 ± 12.81), with a cutoff score of 40 on the state-trait anxiety inventory reflecting severe anxiety. At the end of 12 months, intimate partners still reported elevated anxiety (M = 35.6 ± 12.47). The level of depression reported by intimate partners was not significantly elevated at any time during the first year.
Impact on family functioning after ICD implantation was the greatest at hospital discharge with improvement over time (P = .001). Family functioning was affected the most in the following areas: patient needed to be protected from stress (77%), patient needed help with treatments (69%), worry about the patient responding to therapy (68%), need for greater sensitivity to mood changes in the patient (67%), and need for more emotional support in the patient (64%). At 12 months, the demands on family functioning were reduced in these same areas. Partners no longer reported that the patient needed help in performing medical treatments at home at 12 months.
Behavioral care demands of the patient were the highest at the time of ICD implantation, then declined over the first year (P = .001). The top 5 individual care demands at both baseline and 12 months included preparing meals, having the patient constantly on one’s mind, shopping and making appointments for the patient, checking on the patient during the night, and managing family finances. Of these care demands, 43% were new tasks performed by the intimate partner. These findings were used to guide the essential outcomes measured by the study, timing of intervention delivery, and sequencing of content sessions so that all partner health and caregiving demand issues would be addressed by the new intervention.
In summary, the intimate partners’ physical health, anxiety, symptoms, and depression declined over the first year, the most change was noted from hospital discharge to 3 months. Self-reported physical health declined over the first year. Although anxiety was significantly reduced with time, it remained elevated in partners at 1 year. The impact of ICD implantation on the intimate relationship and care demands was most apparent at hospital discharge. This study demonstrated that both physical and mental health of intimate partners is affected by SCA and ICD implant, most notably between hospital discharge and 3 months after the ICD implant. These findings indicate that an intervention that addresses these important themes had the potential to improve the experience of the intimate partner when the patient requires an ICD.
Study 3: Pilot study of partner interventions after ICD implantation
On the basis of the results of the 2 studies mentioned earlier, we developed a theory-driven, empirically supported partner intervention that focused on addressing partner domains of concern as well as partner physical health, mental health, and caregiving demands after ICD implant.37 We pilot tested this new partner intervention in combination with the patient intervention to determine its feasibility and acceptability. Ten patient-partner pairs were recruited immediately after ICD implant, were enrolled in the pilot study posthospital discharge, and were followed for 3 months. The patient and partner (P+P) intervention was nurse delivered by telephone during the first 3 months. This new partner intervention included 4 components: (1) structural informational booklet for the partner, (2) nursing psychoeducational and counseling telephone protocol focused on partner behaviors that can improve the patient’s recovery outcomes, (3) patient and partner, 24 hour/7 day nurse pager, and (4) partner telephone group (PTG).40 These intervention elements were delivered on the basis of Bandura’s theory. For example, within the nursing telephone protocol, specific issues are addressed with the patient and partner, strategies to deal with the issue are offered, skills are demonstrated in the booklets, and action plans to practice essential skills over the subsequent week are assigned. Baseline outcomes were measured at hospital discharge and at the conclusion of the intervention at 3 months. In addition, at the conclusion of the intervention, we assessed feasibility, acceptability, content, delivery, timing, and willingness to participate using an open-ended exit interview.
Measures of physical health included the short-form health survey (SF-36)41 and the partner concerns assessment adapted from the patient concerns assessment.42 The partner concerns assessment is a new scale that is highlighted in the measures section. Anxiety was measured using the State-Trait Anxiety Inventory43 and depression was assessed using the Geriatric Depression Scale.44 Mental health was measured using the MCS score of the SF-36 general health measure as described earlier. Relationship impact was measured using the Dyadic Adjustment to Illness Scale45 and the Demands of Caregiving Inventory.46 The single group design without a control group prevented concluding that changes were due to the intervention. Rather, our interest focused on change in the outcomes between pre- and postintervention.
Patients with an ICD were an average of 66.9 (±5.74) years old, Caucasian (100%), male (90%), and with a high school education (90%). Patients were employed full- or part-time (60%), with an annual household income of $30 000 to 49 000. Sixty percent of ICD patients received their ICD for secondary prevention of SCA, while the remaining 40% for primary prevention of SCA. Intimate partners were an average of 64.0 (±8.46) years old, Caucasian (90%), female (90%), and with a high school education (100%). Partners were employed full- or part-time (60%).
Physical health
Patients with an ICD reported reductions in symptoms and concerns (Table 1) at 3 months (P = 0.07). The most common patient symptoms during the first month after ICD implantation were difficult sleep, fatigue, low energy, frustration, and memory loss. Partners also reported a reduction in symptoms of weakness, low back pain, fatigue, difficult sleep, and headaches. Significant improvements were noted in the PCS-physical and MCS-mental health component scores of the SF-36 for both patients and partners.
Table 1.
Change Scores for Patients and Partners in Pilot Study (N = 10)
| Outcomea | Hospital Discharge, Mean ± SD | 3 Months, Mean ± SD | Change Score,b Mean ± SD | Wilcoxon Signed Rank Test |
|---|---|---|---|---|
| Physical Functioning | P | |||
| Patient/Partner Concerns | ||||
| Patient | 13.6 ± 10.5 | 8.5 ± 9.65 | − 5.10 ± 9.1 | 0.07 |
| Partner | 7.5 ± 7.6 | 6.4 ± 7.2 | − 1.10 ± 8.3 | 0.57 |
| SF-36 PCS | ||||
| Patient | 40.1 ± 6.6 | 46.83 ± 10.8 | 6.74 ± 8.0 | 0.44 |
| Partner | 49.64 ± 11.7 | 55.88 ± 8.87 | 6.34 ± 9.5 | 0.40 |
| SF-36 MCS | ||||
| Patient | 56.07 ± 6.44 | 60.01 ± 4.46 | 3.94 ± 6.10 | 0.37 |
| Partner | 48.71 ± 13.06 | 53.24 ± 14.9 | 4.52 ± 8.48 | 0.20 |
| Psychological Adjustment | ||||
| State-Trait Anxiety Inventory | ||||
| Patient | 39.89 ± 15.1 | 31.00 ± 8.19 | − 7.89 ± 17.04 | 0.08 |
| Partner | 34.33 ± 11.78 | 31.89 ± 12.94 | − 2.44 ± 12.5 | 0.21 |
| Geriatric Depression Scale | ||||
| Patient | 1.78 ± 2.99 | 0.5 ± 2.4 | − 1.28 ± 2.11 | 0.61 |
| Partner | 2.00 ± 3.52 | 1.83 ± 3.54 | − 0.17 ± 1.17 | 0.75 |
| Relationship impact | ||||
| Dyadic Adjustment Scale | ||||
| Patient | 110.56 + 15.9 | 114.78 ± 13.5 | 4.22 ± 10.97 | 0.26 |
| Partner | 105.67 ± 26.2 | 110.83 ± 26.77 | 4.56 ± 12.87 | 0.39 |
| Caregiving instrumental activities of daily living | ||||
| Partner | 1.82 ±0.25 | 1.76 ± 0.20 | − 0.06 ± 0.17 | 0.33 |
| Self-efficacy | ||||
| SCA self-efficacy | ||||
| Patient | 8.76 + 1.4 | 9.33 +1.33 | 0.57 + 1.6 | 0.77 |
| Partner | 8.5 + 1.52 | 8.00 + 8.8 | 0.40 + 0.90 | 0.36 |
| SCA outcome expect | ||||
| Patient | 4.46 + 0.51 | 4.94 + 0.55 | 0.48 + 0.69 | 0.92 |
| Partner | 4.55 + 0.42 | 4.88 + 0.19 | 0.33 + 0.41 | 0.36 |
| Knowledge | ||||
| Patient | 20.33 + 3.8 | 22.0 + 2.9 | 1.67 + 4.08 | 0.46 |
Patient scores are noted in “Bold” and partner scores in “Italic”.
Change scores calculated: 3 month score minus baseline (posthospital discharge)
Abbreviations: SCA, sudden cardiac arrest; SF-36, short-form health survey-36.
Psychological adjustment
Reductions in patient anxiety and depression were noted, with greater reductions in anxiety than depression for both patients and partners. While reductions in depression for patients and partners were evident, these reductions were relatively small due to low baseline levels of depression.
Relationship impact
Improvements in dyadic adjustment were evident for patients and partners postintervention, with partners reporting slightly less overall dyadic satisfaction than patients. Areas of improvement included dyadic consensus, dyadic cohesion, and affectional expression. Caregiver burden for partners was reduced in both behavioral care demands of the patient and instrumental activities of daily living at 3 months. Tasks that the partner performed on behalf of the patient in instrumental activities of daily living included medication management, making appointments, arranging meals, taking care of finances, running errands, and personal communication.
Self-efficacy
There were noted modest improvements in self-efficacy expectations and outcome expectations in the patient sample, without noted increased self-efficacy expectations in partners. Improvements in patient knowledge postintervention were also noted.
Feasibility and acceptability
From the exit interview, we found evidence that the interventions were both feasible and acceptable. None of the couples who were approached refused to participate. Shorter telephone calls were better tolerated by patients, completing data collection by phone worked exceptionally well and allowed individuals to enter the study earlier, and the materials provided essential information about ICD recovery that was not otherwise available. Patients and partners reported that the timing, sequencing, and format of the nursing telephone protocol were acceptable. Partners who participated thought that the PTG was an essential component of the intervention. During the course of the study, a subset of partners contacted the study nurse independently by phone to talk at a time when the patient was not at home, providing additional support for the need for the PTG. Thus, the pilot study results demonstrated a highly promising (P+P) intervention for improving partner as well as patient outcomes, and warranted clinical testing with a larger sample. Nurses who are caring for new ICD implant patients in the hospital setting possess little information about ICD recovery posthospital stay. This creates a gap between care received in the acute setting and more long-term follow-up needed at home for patients and families to make a successful recovery, prevent complications, and facilitation adaptation.
In summary, we conducted 3 studies that created the foundation for the development and testing of a new partner intervention. The first study outlined the important concerns of partners in the 1 year after the patient suffers a cardiac arrest and receives an ICD. These findings shaped the content of the new partner intervention. The second study demonstrated critical effects on partner health and caregiving demands when a patient receives an ICD. These health concerns became the targets of the intervention, including physical and mental health and caregiving demands. In the third study, we pilot tested the newly developed partner intervention combined with the patient intervention to assess feasibility, acceptability, and potential effects on outcomes. The pilot study demonstrated that the P+P intervention timing, content, and focus demonstrated improvement in outcomes. These 3 foundational studies support the current design and testing of the P+P intervention in a larger scale as described later.
TESTING THE NEW PARTNER INTERVENTION
In our previous investigations, intimate partners expressed interest in participating in the intervention and requested more help and guidance from health care providers than was currently available in general practice. Generally partners do not have access to information about normal recovery processes for ICD patients, are not the focus of education and support interventions, and thus do not understand how to be helpful while maintaining their own health. The intimate partner provides essential physical and psychological support to the ICD patient; thus, it is crucial to maintain the intimate partner’s physical and psychological health so they can attend to the patient caregiving demands. Thus, the central goals for including the intimate partner in the P+P intervention is to actively engage the partner in the patient’s recovery, provide the same information to both persons simultaneously, and provide the partner with skills designed to promote patient recovery and maintain their own health. Actively involving the partner in the patient’s recovery is expected to facilitate implementation of the patient intervention and support the patient in regaining self-care activities. Telephone interactions with partners are designed to provide performance accomplishment opportunities (learning by doing, self-monitoring, and obtaining feedback) and persuasion (learning through information and advice provided by expert).
Research design
The P+P intervention study compares 2 intervention conditions: P+P intervention against the P-only intervention during the first year post-ICD implantation. The design is a 2-group (n = 150, patient-partner pairs/group) blocked randomized clinical trial. The blocking variable is ICD indication for either primary prevention of SCA or secondary prevention of SCA. The study interventions are delivered in the first 3 months after ICD implantation. Data are collected on ICD patients and their intimate partners 5 times: at hospital discharge, and at 1, 3-, 6-, and 12-month post-ICD implantation.
Patient selection
A total of 300 dyads (150/group) will participate in this prospective study. Intimate partner is defined as the spouse, lover, life partner, or significant other involved in a committed relationship with the ICD patient. Participants are identified from acute care institutions. Inclusion criteria include the following: (a) first ICD implantation due to either primary or secondary prevention of SCA in the patient, (b) intimate partner (spouse, lover, or life partner) living at the same residence and willing to participate, (c) able to read, speak, and write English, and (d) access to telephone for 1 year after ICD implantation. Exclusion criteria include the following: (a) clinical comorbidities that severely impair physical functioning at telephone screening, (b) short BLESSED score more than 6, (c) age less than 21 years, (d) AUDIT-C score more than or equal to 4 for alcohol use, and (e) ASSIST 2.0 score more than or equal to 4 for daily nonmedical use of opiates or hallucinogens.
Nurse interventions
The nursing interventions being delivered are designed to be implemented by baccalaureate-prepared nurses with a background in cardiovascular nursing who would undergo training and practice before beginning intervention delivery. Ideally, nurses having knowledge about the technical aspects of the ICD, how it works, and how it will treat recurrent cardiac arrhythmias would be best prepared for this role. Nurses would need ongoing supervision and support from an advanced practice nurse who possessed specialized skills for dealing the ICD-related problems, questions, symptoms, and psychosocial responses. Nurses are in a key position to implement early telephone support for the recognition of impending adverse outcomes and complications, and to intervene before more urgent care is needed.
Two intervention programs (P-only and P+P) are being compared with each other that are delivered by trained cardiovascular nurses. All intervention elements were designed on the basis of social cognitive theory37 and the domains of concern of patients and partners from “Experiences of Recovery Following Sudden Cardiac Arrest.”36,39 The intervention targets all 4 methods for self-efficacy: enhancing performance accomplishments, using vicarious experience and verbal persuasion, and reducing emotional arousal, while assessing the impact on behavior and outcomes.
P-only intervention
The patient-only intervention has been detailed earlier and shown to be effective in improving patient outcomes after an ICD implantation33,34,40,47 Briefly, the intervention goals are to assist with (1) managing physical symptoms and changes, (2) returning to performance of activities of daily living and safe activity, (3) exercising safely with an ICD, (4) managing anxiety and depression, (5) handling ICD shocks, (6) performing preventive ICD care, (7) obtaining information related to ICD care, and (8) learning when to call 911 or the health care provider in emergencies.
P+P intervention
The combined P+P intervention includes the P-only intervention plus integration of the intimate partner into all aspects of the patient intervention, and the addition of the PTG. For this study, we are testing the new partner version of the structural informational booklet, integration of partners into the nursing telephone support (NTS) calls with the patient that include partner assignments, providing partners with access to the on-call nurse via pager, incorporation of strategies for partners to assist in the patient recovery process, and the effectiveness of the partner-only telephone support group (PTG).
Structural Informational booklet (partner version) is a stand-alone booklet containing 2 components: a descriptive component that includes verbatim statements from other partners about first year ICD-recovery experiences, and a management component that discusses successful strategies used by partners in dealing with specific issues of recovery.
NTS protocol (P+P) includes 8 planned telephone home calls made by an expert cardiovascular nurse. The content of the NTS is patient-focused, and partners are asked to read NTS-associated materials, participate in home telephone calls, ask questions, and engage in patient support behaviors.
Nurse pager (partner) is a nationwide, toll free paging system with access to the research nurse 24 hours/day over 7 days/week. The partner can access the study nurse after work hours for questions or concerns that arise between the planned NTS and/or PTG telephone calls.
PTG is a weekly, 4-session telephone conference call group focused on the intimate partner that occurs in conjunction with the P+P nursing support calls. The PTG is held in the evenings with rotating topics; partners can join the PTG at any time when they join the study and remain in the PTG until all topics have been covered. Partners call a toll free telephone conference network on a weekly basis for 4 weeks; a summary or open-ended telephone call is delivered on the 6th and 12th weeks. Topics covered in the PTG are those that were validated with partners in a previous study.36 Each week, a topic of concern is covered in the first 30 minutes, with the remaining 45 minutes for open discussion, sharing for information and strategies, obtaining psychological support, setting goals, action planning, problem solving, and planning for the next PTG. The content of the PTG includes the following: week 1: introduction, group rules, and care of the ICD patient; week 2: partner self-care; week 3: relationship impact and role adjustment; week 4: ICD uncertain future planning for the future; week 6 and week 12: review, questions, and open-ended topics.
Measures
Two sets of variables are being measured: (1) outcome variables that determine the effects of the interventions and (2) mediating variables specified from social cognitive theory (Table 2). Outcomes variables are (a) physical functioning in the ICD patient (ICD shocks, general health, concerns, physical activity) and the partner (general health, concerns, physical activity, return to work); (b) psychological adjustment in the ICD patient and partner (anxiety and depression); (c) health care utilization by the patient and partner (unscheduled outpatient visits, ER visits, hospitalizations); and (d) relationship impact for patient (dyadic adjustment) and partner (dyadic adjustment and caregiver burden). Mediating variables are self-efficacy expectations, outcome expectations, knowledge, and caregiving. The primary time for treatment assessment is the measurement of outcomes at 3 months postintervention, with 6- and 12-month follow-up assessments to determine whether intervention effects are sustained over the year after receipt of the ICD (Table 2).
Table 2.
Outcome and Mediating Variables Used in Ongoing Study
| Variable/Measure | Description | Source | Mode | Reliability Cronbach α |
|---|---|---|---|---|
| Outcome variables | ||||
| Physical functioning | ||||
| Heart rhythm stability/ICD shocks, arrhythmias | ICD shocks/heart rhythm stability based on interrogation reports from ICD device. Variables stored on device: number ICD shocks, antitachycardia pacing, aborted defibrillatory shocks. | Patient only | ICD interrogations | |
| Symptoms and concerns/patient/partner concerns assessment | Assesses physical symptoms and fears common in first months post-ICD.42 Unique disease-specific instrument for ICD patients; sensitive to change over 12 months. Adapted for intimate partner concerns in pilot testing. | Patient and partner | Questionnaire self-report | 0.8242 |
| General health/Short-form health survey | Developed to assess physical and mental health41; measures 8 health domains: physical functioning, physical role functioning, bodily pain, general health, vitality, social functioning, emotional role functioning, mental health. Summary scales: physical (PCS) and mental health (MCS) derived. | Patient and partner | Questionnaire self-report | 0.65–0.9641 |
| Average daily activity/Cyma step watch | Stepwatch 3 Activity Monitor (SAM; OrthoCare Innovations), pager-sized, lightweight, fastens above ankle. SAM is accelerometer that records gait cycles (strides). Accuracy of 98% to 99%.48 Study participants wear during waking hours × 5 days for at least 10 or more hours (600 min). | Patient and partner | Activity monitor | 0.87–0.9248 |
| Employment/Return to work information | Employment, full or part-time employed, # of days off work since the ICD, no. of sick days used during study period, decision to retire due to ICD, reasons for not returning to work and/or retirement. | Patient and partner | Interview | |
| Psychological adjustment | ||||
| Anxiety/State-Trait Anxiety Inventory | “State” anxiety scale used to measure levels of situational anxiety. Extensive normative data available for comparison, as well as established reliability and validity.43 | Patient and partner | Questionnaire | 0.85–0.9643 |
| Depression/Center for Epidemiologic Studies, Depression Scale | Measures depressive symptoms, focus on depressed affect.49 Commonly used in health studies, normative data available for comparison, established reliability, validity with clinical cut points. | Patient and partner | Questionnaire | 0.85–0.9049 |
| Relationship impact | ||||
| Dyadic adjustment/Dyadic Adjustment Scale | Measures relationship adjustment. Normative values available for cardiac arrest samples, married and divorced couples.45 | Patient and partner | Questionnaire | 0.73–0.9645 |
| Caregiving demands/Demands of caregiving | Measures patient care responsibilities for activities of daily living, instrumental activities of daily living, and personal demands.46 | Partner only | Questionnaire | 0.8346 |
| Health care utilization | ||||
| ER visits/Items on interim health history | Summarizes number of emergency room (ER) visits for ICD, cardiac-related illness and other reasons | Patient and partner | Interview/Self-report | |
| Outpatient visits/Interim health history | Summarizes number of unexpected outpatient visits to physicians, mental health providers, cardiac rehabilitation and others | Patient and partner | Interview/Self-report | |
| Hospitalizations/Interim health history and medical records | Summarizes number of hospital admissions & total number hospital days for ICD, cardiac related illness and other reasons | Patient and partner | Interview/Medical records | |
| Mediating variables | ||||
| Efficacy expectations/SCA self-efficacy (SCA-SE) | Measures self-efficacy to perform self-management behaviors, manage illness experience post-ICD implantation.38 | Patient and partner | Questionnaire | 0.8938 |
| Outcome expectations SCA outcome expectations | Measures outcomes expected due to engaging in behaviors relevant to ICD recovery; expectancies and beliefs that engaging in particular behaviors will result in positive outcomes post-ICD.38 | Patient and partner | Questionnaire | 0.8038 |
| Caregiving self-efficacy/SE-caregiving | Assesses self-efficacy in caring for loved one by respite, responding to patient behaviors, controlling negative thoughts, based on social cognitive theory.50 | Partner only | Questionnaire | 0.8350 |
| Knowledge assessment/SCA knowledge assessment | Quantifies knowledge about physical function, ADL, emotional reactions, ICD shocks, partner relationships, safety/precautions living with ICD.38 | Patient and partner | Questionnaire | 0.84–0.8638 |
T1 = baseline data collection prior to randomization to study condition; T2 = follow-up data collection at 3 months post-ICD implantation; T3 = follow-up data collection at 6 months; T4 = follow-up data collection at 12 months.
Abbreviations: ICD, implantable cardioverter defibrillator; SCA, sudden cardiac arrest.
Study progress
Enrollment in the P+P study began on February 1, 2010. We have completed 2 years of recruitment and randomization. Final enrollment will be completed in 2013, with study results available in 2014. Recruitment in the study occurs through site coordinators as patients are admitted to an acute care agency implanting the ICD. Weekly surgery and laboratory schedules are reviewed to identify potential participants. The site coordinator verifies eligibility of potential study participants and determines the presence of an intimate partner. Once it is determined that the individual patient meets the inclusion criteria, the site coordinator informs the person about the study and obtains permission for the research staff to be in contact. Within 24 hours of hospital discharge, patients and partners are telephoned, the study is explained, verbal informed consent is obtained, screening and baseline questionnaires are completed, and written consent is mailed. After written informed consent is completed, couples are randomized to the P+P arm or the P-only arm of the study. Patients who will not be discharged home after hospitalization or who are physically or cognitively compromised are not approached for participation. At the current time, 16 sites are actively participating in subject recruitment.
Study innovation
This intervention study described here is one of the first intervention trials to include both ICD patients and their intimate partners, with elements of the interventions focused specifically on the partner. Included in the study are those who have received an ICD for either primary or secondary prevention of SCA, to determine whether intervention effects are applicable and uniform across these ICD subgroups. In addition, the study uses an innovative telephone small group, conference call approach to deliver the partner intervention. The intervention delivery allows for maximum flexibility in study participation because no in-person visits are required of either the patient or the partner. If the intervention elements are validated and effective, we envision moving toward electronic versions of the intervention, made widely available to a larger number of patients and partners using Internet and telephone technology. The information gleaned from implementation and delivery of this format promises applicability to other partner populations likely to benefit from a group intervention in illness recovery.
DISCUSSION
There is a paucity of information about the impact of SCA and ICD implantation on intimate partners and family members. Descriptive studies suggest that intimate partners experience a decline in physical health, prolonged anxiety, symptoms of stress, and new and additional caregiver demands specifically during the first 3 months after the patient receives an ICD. In addition, research demonstrates that ICD shock events adversely impact partner as well as patient anxiety levels. Yet, even with such compelling evidence, little effort has been directed toward designing or testing a partner-focused intervention. Using a staged approach to intervention development, we sought evidence to create a partner-focused intervention to address partner issues, concerns, and health outcomes and to serve as an adjunct for a patient-focused intervention.
Developing evidence-based practice for nursing at all levels calls for systematic approaches. In our approach to intervention development, we began with a qualitative study to discover the lived experience of patients and partners following cardiac arrest and receipt of ICDs. This initial study highlighted important times and experiences over the 1-year period that would later become the structure, timing, and major content of intervention components. Next, we examined the physical health, mental adjustments, caregiver burden, and health care utilization of partners over a 1-year period after the ICD implantation. This description study provided the necessary background for discerning important health outcomes most likely to be amenable to intervention efforts. Then, integrating findings from these 2 descriptive studies guided by a theoretical framework focused on determinants of behavioral change and outcomes, we designed a nursing intervention to improve partner physical and health outcomes after an ICD. This approach illustrates how nursing advances knowledge regarding a particular phenomenon, pointing to a general process for developing evidence-based interventions for building the science and practice of nursing.
In leading health care change for the future,13 nursing science and practice must be involved in both acute and chronic care settings that extend into homes, long-term care facilities, and communities. Nurses are being called forward to shift the delivery of care for chronic illness in a health care environment where patients leave the hospital early and often have inadequate support or care at home. Envisioning and leading health care change, nurses will need to be prepared for the increasing complexities in care and decision making for populations that are more ill and frail and require sophisticated health care approaches. Care outside the hospital is complex, and nurses are required to coordinate care across care continuums and across the lifespan. To do so effectively, nurses require new knowledge and skills to help patients and their families prepare for living with chronic illness at home. In our research with ICD patients and partners, this means understanding important physical and psychological challenges of the illness, and recognizing the multiple challenges of living with an ICD long term. The knowledge, intervention, and development processes described in this article contribute to the body of knowledge that nurses will need for current and future health care of patients and partners in dealing with life-threatening cardiac conditions, including those living with an ICD.
The intervention currently being tested for partners of patients who have an ICD is structured to be delivered by baccalaureate-prepared nurses in the posthospital care environment. Because this is the first test of intervention efficacy, procedures for translating this evidence into real world practice settings have not been developed but constitute the next set of goals to be accomplished. The challenge of translating empirical results generated from research investigations into practice is a current focus of several national agencies that want to assure that valid and reliable evidence for practice is available to patients and families. Nurses are positioned to play a major role in research translation, particularly those that influence outcomes that target improvements in health. Doctorally prepared nurses in PhD and DNP programs are in excellent positions to lead this charge, particularly in developing and implementing interventions that involve human responses to health conditions. Currently the health care system is not ideally suited for nursing intervention implementation in chronic care or community settings because of unresolved issues of reimbursement and program sustainability. Future health care reform and the Affordable Care Act will address some, but not all of these issues.
CONCLUSIONS
In a series of 3 investigations, we determined major concerns and issues that partners of patients who receive an ICD encounter throughout the first year of recovery from ICD implant. We then designed and are in the testing phase of a social cognitive theory based nursing intervention aimed to effect important outcomes for partners in the first year after the patient receives an ICD. Because nurses play a key role in managing and intervening in chronic illness, evidence-based approaches to guide intervention delivery are essential to effect important health outcomes. This approach to the development of evidence and then the application of evidence to improve clinical nursing practice is a model that can be applied to other health conditions for which nurses have an impact.
Acknowledgments
Pilot study funding has been taken from the Research Intramural Funding Program, University of Washington School of Nursing and intervention study funding from National Institute of Health, R01 HL086580. ClinicalTrials.gov: NCT 01252615.
References
- 1.Glikson M, Friedman P. The implantable cardioverter defibrillator. The Lancet. 2001;357:1107–1117. doi: 10.1016/S0140-6736(00)04263-X. [DOI] [PubMed] [Google Scholar]
- 2.Bardy GH, Lee KL, Mark DB, et al. for SCD-Heft Investigators. Amiodarone or an implantable cardioverter defibrillator for congestive heart failure. New Eng J Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 3.Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. New Engl J Med. 2002;346:877–883. doi: 10.1056/NEJMoa013474. [DOI] [PubMed] [Google Scholar]
- 4.Cleland JG, Ghosh J, Freemantly N, Nasir M, Clerk AL, Cole AP. Clinical trials update and cumulative meta-analyses from the ACC: WATCH, SCD-HeFT, DIMAM, CASINO, STRATUS-US, RIO-Lipids and cardiac resynchronization therapy in heart failure. Eur J Heart Fail. 2003;6(4):501–508. doi: 10.1016/j.ejheart.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 5.Sears SF, Conti JB. Quality of life and psychological functioning of ICD patients. Heart. 2002;87:488–493. doi: 10.1136/heart.87.5.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carlson LE, Bultz BD, Speca M, St Pierre M. Partners of cancer patients: Part II. Current psychosocial interventions and suggestions for improvement. J Psychosoc Oncol. 2000;18(3):33–43. [Google Scholar]
- 7.Dougherty CM. Psychological reactions and family adjustment in shock versus no shock groups after implantation of the internal cardioverter defibrillator. Heart Lung. 1995;24(4):281–291. doi: 10.1016/s0147-9563(05)80071-8. [DOI] [PubMed] [Google Scholar]
- 8.Corbin JM, Strauss A. A Nursing Model for Chronic Illness Management Based on the Trajectory Framework: the Corbin and Strauss Nursing Model. New York, NY: Springer Publishing Co; 1992. pp. 9–28. [Google Scholar]
- 9.Miller PJ, Wikoff R. Spouses psychosocial problems, resources, and marital functioning post-myocardial infarction. Prog Cardiovasc Nurs. 1989;4:71–76. [PubMed] [Google Scholar]
- 10.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the caregiver health effects study. JAMA. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 11.Coyne JC, Rohrbaugh MJ, Shoham V, Sonnega JS, Micklas JM, Cranford JA. Prognostic importance of martial quality for survival of congestive heart failure. Am J Cardiol. 2001;88:526–529. doi: 10.1016/s0002-9149(01)01731-3. [DOI] [PubMed] [Google Scholar]
- 12.American Nurses Association. Nursing’s social policy statement: the essence of the profession. Washington, DC: American Nurses Association; 2010. [Google Scholar]
- 13.Institute of Medicine of the National Academies. The Future of Nursing: Advancing Change, Leading Health, Brief Report. Washington, DC: Institute of Medicine of the National Academies; 2010. [Google Scholar]
- 14.Tagney J. Can nurses in cardiology areas prepare patients for implantable cardioverter defibrillator implant and life at home? Nurs Crit Care. 2004;9(3):104–114. doi: 10.1111/j.1362-1017.2004.00064.x. [DOI] [PubMed] [Google Scholar]
- 15.Sears SF, Todaro JF, Urizar G, et al. Assessing the psychosocial impact of the ICD: a national survey of implantable cardioverter defibrillator health care providers. Pacing Clin Electrophysiol. 2000;23(6):939–945. doi: 10.1111/j.1540-8159.2000.tb00878.x. [DOI] [PubMed] [Google Scholar]
- 16.Jenkins LS, Powell JL, Schron EB, et al. Partner quality of life in the anti-arrhythmics versus implantable defibrillators trial. J Cardiovasc Nurs. 2007;22:472–479. doi: 10.1097/01.JCN.0000297378.98754.06. [DOI] [PubMed] [Google Scholar]
- 17.Sowell LV, Sears SF, Walker RL, Kuhl EA, Conti JB. Anxiety and marital adjustment in patients with implantable cardioverter defibrillators and their spouses. J Cardiopulm Rehabil Prev. 2007;27(1):46–49. doi: 10.1097/01.hcr.0000265027.79649.6a. [DOI] [PubMed] [Google Scholar]
- 18.Van Horn E, Fleury J, Moore S. Family interventions during the trajectory of recovery from cardiac event: an integrative literature review. Heart Lung. 2002;31:186–198. doi: 10.1067/mhl.2002.124342. [DOI] [PubMed] [Google Scholar]
- 19.Gilliss CL. The family dimension of cardiovascular care. Can J Cardiovasc Nurs. 1991;2:1–3. 7. [PubMed] [Google Scholar]
- 20.Dickerson SS, Posluszny M, Kennedy MC. Help seeking in a support group for recipients of implantable cardioverter defibrillators and their support persons. Heart Lung. 2000;29(2):87–96. [PubMed] [Google Scholar]
- 21.Teplitz L, Egenes KJ, Brask L. Life after sudden death: the development of a support group for automatic implantable cardioverter defibrillator patients. J Cardiovasc Nurs. 1990;4(2):20–32. doi: 10.1097/00005082-199002000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Levin RF. Caring for the cardiac spouse. Am J Nurs. 1993;93(11):50–53. [PubMed] [Google Scholar]
- 23.Ocampo CM. Living with an implantable cardioverter defibrillator. Impact on the patients, family, and society. Nurs Clin N Am. 2000;35(4):1019–1031. [PubMed] [Google Scholar]
- 24.Pycha C, Calabrese JR, Gulledge AD, Maloney JD. Patient and spouse acceptance and adaptation to implantable cardioverter defibrillator. Clev Clin J Med. 1990;57(5):441–444. doi: 10.3949/ccjm.57.5.441. [DOI] [PubMed] [Google Scholar]
- 25.Morris PL, Badger J, Chmielewski C, Berger E, Goldberg RJ. Psychiatric morbidity following implantation of the automatic implantable cardioverter defibrillator. Psychosomatics. 1991;32:58–64. doi: 10.1016/S0033-3182(91)72112-9. [DOI] [PubMed] [Google Scholar]
- 26.Vlay SC, Olson LC, Fricchione GL, Friedman R. Anxiety and anger in patients with ventricular tachyarrhythmias: responses after automatic internal cardioverter defibrillator implantation. PACE. 1989;12:366–373. doi: 10.1111/j.1540-8159.1989.tb02670.x. [DOI] [PubMed] [Google Scholar]
- 27.Dunnington C, Johnson M, Finkelmeier B. Patients with heart rhythm disturbances: variables associated with increased psychologic distress. Heart Lung. 1988;17:381–389. [PubMed] [Google Scholar]
- 28.Dougherty CM. Longitudinal recovery following sudden cardiac arrest: patients and their families. Am J Crit Care. 1994;3:145–154. [PubMed] [Google Scholar]
- 29.Doolittle ND, Sauve MJ. Impact of aborted sudden cardiac death on patients and their spouses: the phenomenon of different reference points. Am J Crit Care. 1995;4(5):389–396. [PubMed] [Google Scholar]
- 30.Steinke EE. Sexual concerns of patients and partners after an implantable cardioverter defibrillator. Dimens Crit Care Nurs. 2003;22(2):89–95. doi: 10.1097/00003465-200303000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Sears S, Todaro J, Lewis T, Sotile W, Conti J. Examining the psychosocial impact of implantable cardioverter defibrillators: a literature review. Clin Cardiol. 1999;22:481–489. doi: 10.1002/clc.4960220709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bainger EM, Fernsler JI. Perceived quality of life before and after implantation of an internal cardioverter defibrillator. Am J Crit Care. 1991;4(1):36–43. [PubMed] [Google Scholar]
- 33.Dougherty CM, Lewis FM, Thompson ET, Baer JD, Kim W. Short term efficacy of a telephone intervention after an ICD. PACE. 2004;27:1594–1602. doi: 10.1111/j.1540-8159.2004.00691.x. [DOI] [PubMed] [Google Scholar]
- 34.Dougherty CM, Thompson EA, Lewis FM. Long term outcomes of a nursing intervention after an ICD. Pacing Clin Electrophysiol. 2005;28:1157–1167. doi: 10.1111/j.1540-8159.2005.09500.x. [DOI] [PubMed] [Google Scholar]
- 35.Dougherty CM, Thompson EA. Intimate partner physical and mental health after sudden cardiac arrest and receipt of an implantable cardioverter defibrillator. Res Nurs Health. 2009;32(4):432–442. doi: 10.1002/nur.20330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dougherty CM, Pyper GP, Benoliel JQ. Domains for nursing intervention for intimate partners of sudden cardiac arrest patients. J Cardiovasc Nurs. 2004;19(1):21–31. doi: 10.1097/00005082-200401000-00006. [DOI] [PubMed] [Google Scholar]
- 37.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 38.Dougherty CM, Lewis FM, Johnston SA. Reliability and validity of the self-efficacy expectations and outcome expectations after ICD implantation scales. Appl Nurs Res. 2007;20:116–124. doi: 10.1016/j.apnr.2007.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dougherty CM, Benoliel JQ, Bellin CM. Domains of nursing intervention after sudden cardiac arrest and automatic internal cardioverter defibrillator implantation. Heart Lung. 2000;29(2):79–86. [PubMed] [Google Scholar]
- 40.Dougherty CM, Pyper GP, Frasz HA. Description of a nursing intervention after ICD implantation. Heart Lung. 2004;33(3):183–190. doi: 10.1016/j.hrtlng.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 41.Ware JC, Shelbourne CD. The MOS 36-item short form health survey (SF-36): conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 42.Jenkins LS, Dunbar SB, Hawthorne MH. Patient concerns before and the first 9 months after ICD implantation. Circulation. 1997;96(suppl I):I-134. [Google Scholar]
- 43.Speilberger C, Gorsuch R, Lushene R. Manual for the State-Trait Anxiety Inventory (Self-Evaluation Questionnaire. Palo Alto, CA: Consulting Psychologists; 1970. [Google Scholar]
- 44.Watson LC, Pigone MP. Screening accuracy for late-life depression in primary care: a systematic review. J Fam Pract. 2003;52:956–964. [PubMed] [Google Scholar]
- 45.Spanier GB. Assessing dyadic adjustment: New Scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976;38:15–28. [Google Scholar]
- 46.Wallhagen MI. Caregiving demands: their difficulty and effects on the well-being of elderly caregivers. Sch Inq Nurs Pract. 1992;6(2):111–127. [PubMed] [Google Scholar]
- 47.Dougherty CM, Johnson-Crowley NR, Lewis FM, Thompson EA. Theoretical development of nursing interventions for sudden cardiac arrest survivors using social cognitive theory. Adv Nurs Sci. 2001;24(1):78–86. doi: 10.1097/00012272-200109000-00009. [DOI] [PubMed] [Google Scholar]
- 48.Cavanaugh JT, Coleman KL, Gaines JM, Laing L, Morey MC. Using step activity monitoring to characterize ambulatory activity in community-dwelling older adults. J Am Geriatr Soc. 2007;55(1):120–124. doi: 10.1111/j.1532-5415.2006.00997.x. [DOI] [PubMed] [Google Scholar]
- 49.Radloff LS. The CES-D scale: a self-report of depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 50.Steffen AM, McKibbin C, Zeiss AM, Gallagher-Thompson D, Bandura A. The revised scale for care-giving self-efficacy: reliability and validity studies. J Geront. 2002;57B:74–86. doi: 10.1093/geronb/57.1.p74. [DOI] [PubMed] [Google Scholar]