Thyroid eye disease can occur without hyperthyroidism
About 90% of patients with thyroid eye disease have Graves hyperthyroidism, but hypothyroidism and euthyroidism can also accompany this condition.1 Eye disease usually develops in patients with hyperthyroidism within the first 1–2 years, but the disease can occur decades later.
Hallmark features of the disease include retraction of the eyelid, exophthalmos and restricted ocular movement
Retraction of the eyelid (Figure 1) is the most common clinical sign, present in 90% of patients with thyroid eye disease. Exophthalmos (60% of patients) and restricted eye movement (40% of patients) are also common.1
Figure 1:
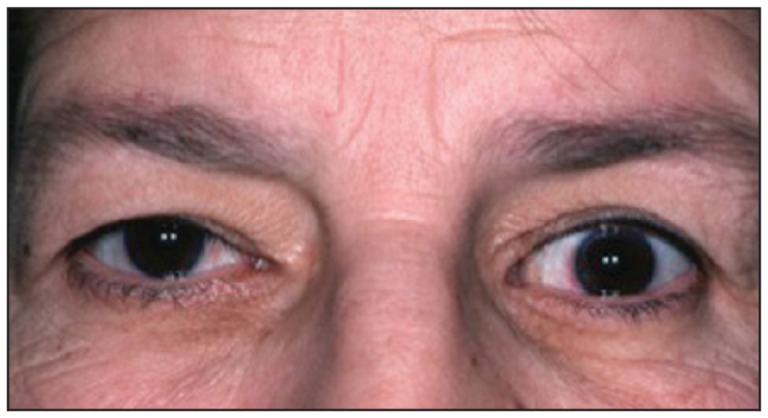
Photograph showing retraction of the left upper eyelid. The upper eyelid normally rests just below the limbus, the lower eyelid at the limbus.
Thyroid eye disease can lead to blindness
Most patients receive conservative treatment — lubrication of the eye to reduce symptoms related to disturbance of the tear film. About 5% of patients will need more aggressive therapy (e.g., systemic corticosteroids, orbital radiation, surgical removal of orbital walls) to prevent vision loss caused by either compression of the optic nerve by enlarging extraocular muscles or corneal ulceration due to exposure.2 Red flags for urgent consultation with an ophthalmologist include reduction in visual acuity or colour vision, relative afferent pupillary defect, swelling of the optic disc, corneal opacity and severe periorbital swelling.
Removal of the thyroid does not cure thyroid eye disease
Thyroid eye disease is driven by autoantigens on orbital fibroblasts that are also expressed by thyroid epithelium.3 The eye disease and systemic disease often have distinct clinical courses. Although supporting evidence is limited, achieving euthyroidism with the assistance of an endocrinologist is recommended, particularly in moderate to severe cases.4 Steroid prophylaxis can prevent the eye disease from worsening after thyroid ablation with radioactive iodine.4 Thyroid removal has little or no additional effect on the natural history of thyroid eye disease.
Smoking is associated with the development, progression and poor response to treatment of thyroid eye disease
Smoking increases the risk of thyroid eye disease (odds ratio 1.9–10.1), and disease progression and poor treatment outcomes are more likely to occur in people who smoke. Thus, smoking cessation is the most important modifiable risk factor.5
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
References
- 1.Bartley GB, Fatourechi V, Kadrmas EF, et al. Clinical features of Graves’ ophthalmopathy in an incidence cohort. Am J Ophthalmol 1996;121: 284–90 [DOI] [PubMed] [Google Scholar]
- 2.Rootman J, Dolman PJ. Thyroid orbitopathy. In: Rootman J, editor. Disease of the orbit: a multidisciplinary approach. 2nd ed Philadelphia (PA): Lippincott Williams & Wilkins; 2003. p. 169–212 [Google Scholar]
- 3.Bahn RS. Graves ophthalmopathy. N Engl J Med 2010;362:726–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hegedüs L, Bonnema SJ, Smith TJ, et al. Treating the thyroid in the presence of Graves’ ophthalmopathy. Best Pract Res Clin Endocrinol Metab 2012;26: 313–24 [DOI] [PubMed] [Google Scholar]
- 5.Thornton J, Kelly SP, Harrison RA, et al. Cigarette smoking and thyroid eye disease: a systematic review. Eye (Lond) 2007;21:1135–45 [DOI] [PubMed] [Google Scholar]


