Abstract
Although thrombotic thrombocytopenic purpura (TTP) is a rare disease, when it develops in a post-cardiac surgery patient, it may have a fatal outcome. Since the frequency of early-onset thrombocytopenia in post-cardiac surgery patients is high, platelet concentrates are commonly transfused during postoperative management. However, when TTP is the likely diagnosis, platelet transfusion is not recommended. We experienced a postoperative TTP in a cardiac surgery patient and discovered the importance of identifying the etiology of postoperative thrombocytopenia. Here, we report the case with a brief review of the literature.
Keywords: Thrombotic thrombocytopenic purpura, Thoracic surgery, Thrombocytopenia
CASE REPORT
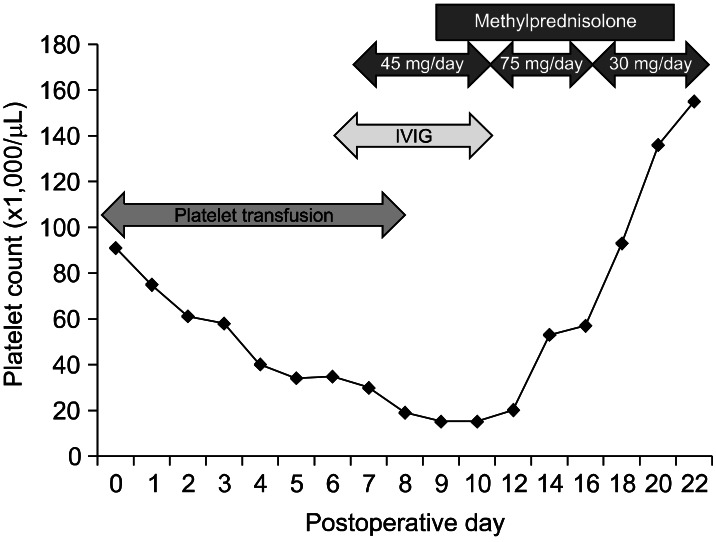
A 62-year-old woman was hospitalized for the further evaluation of her progressive chest discomfort for 10 days. The patient had undergone total thyroidectomy 20 years earlier, and she has been managed for hypothyroidism since then. Seven years prior to admission, she was diagnosed with and managed for angina pectoris, but was not evaluated properly. A month before presentation, she had experienced worsening chest pain with dyspnea on exertion despite medication. She was diagnosed with severe mitral regurgitation by echocardiography at our cardiovascular clinic. When she was hospitalized, she complained that her chest pain and dyspnea had been aggravated with time. Two weeks of medicinal management did not control the symptoms. After dobutamine stress echocardiography, it was determined that the patient should undergo open heart surgery. Mitral valve replacement was performed under extracorporeal circulation. Immediately after surgery, the patient's general condition and laboratory data were found to be stable except for mild thrombocytopenia. Platelet concentrates were transfused to increase the platelet number and prevent unexpected bleeding. A postoperative echocardiogram showed good mitral valve function without para-valvular regurgitation. Since postoperative day 4, she had a fever over 38℃ and the laboratory data showed signs of disseminated intravascular coagulopathy (DIC). Acinetobacter baumannii was cultured in the blood. She was treated with broad spectrum antibiotics for sepsis as well as plasma and platelet transfusion for pulmonary hemorrhage, which occurred on postoperative day 6. Since the thrombocytopenia did not respond to transfusion, intravenous immunoglobulin G was infused and methylprednisolone was administrated intravenously at a dose of 15 mg three times a day. In spite of vigorous treatment, the platelet count did not increase, and even worse, it decreased to a lower count. The lowest platelet count occurred at postoperative day 9. To identify the reason for the refractory response to platelet transfusion, a study for antibody to platelet and additional immune workup were performed on postoperative days 9 and 10. The findings included hemolytic anemia with thrombocytopenia (hemoglobin=7.6 g/dL, platelet=15,000/µL, schistocytosis(+) in a peripheral blood smear), negative direct and indirect Coombs tests, decreased haptoglobin (3 mg/dL), normal ranges of an international normalized ratio (INR 1.13), activated partial thromboplastin time (38.2 seconds) and fibrinogen (287 mg/dL), slightly elevated D-dimer (3.3 µg/mL), hyperbilirubinemia (total bilirubin 3.28 mg/dL, direct bilirubin 1.9 mg/dL), increased lactate dehydrogenase (580 mg/dL), normal serum alanine aminotransferase (10 IU/L) and aspartate aminotransferase (15 IU/L), increased blood urea nitrogen (51 mg/dL), normal creatinine (0.8 mg/dL), microscopic hematuria (red blood cell >30/HPF), negative human immunodeficiency virus antibody, and positive hepatitis B surface antibody. The immune workup results showed decreased complement 3 and 4 levels (lower-most to 51.5/6.9 mg/dL; normal range, 90-180/10-40 mg/dL) and strong positivity in an autoimmune target test (autoimmune cytoplasmic antibody level 4). Antiplatelet antibody was negative. Since postoperative thrombotic thrombocytopenic purpura (TTP) needed to be ruled out at that moment, platelet transfusion was discontinued and the dosage of methylprednisolone was increased to 75 mg/day. Treated with the increased dosage of methylprednisolone, the platelet count steadily increased and maintained within a stable range. The increase in the platelet count and associated dosage of methylprednisolone can be seen in Fig. 1.
Fig. 1.
The change of platelet count with treatments on postoperative days. IVIG, intravenous immunoglobulin.
Since the patient's general condition was stable without thrombocytopenia, or pulmonary bleeding or bleeding from other sites as of postoperative day 18, the tapering of the dosage of methylprednisolone was begun and close observation for bleeding or thrombotic events was maintained. The patient was not given heparin or any other anticoagulation agent until postoperative day 36 due to the above history, but warfarin was given as an anticoagulant since the patient clearly had no risk of bleeding tendency. The patient was discharged on postoperative day 51 after a long period of not only antibiotics treatment for sepsis due to Acinetobacter baumannii but also management and monitoring for ventricular tachycardia. The patient has not complained since of the symptoms of congestive heart failure and has had a normal platelet count for 28 months of follow-up.
DISCUSSION
Thrombocytopenia is a common and intricate problem in an immediate postoperative cardiac surgery patient. When thrombocytopenia persists, its exact etiology is needed but is difficult to determine. Although postoperative TTP is less common than heparin-induced thrombocytopenia, it is associated with high patient morbidity and mortality if the thrombocytopenia persists unresponsive to treatment, especially with thromboembolic events [1].
A distinct feature of postoperative TTP is presence of microangiopathic hemolytic anemia. The classic pentad of thrombocytopenia, hemolytic anemia, fever, renal dysfunction, and neurologic symptoms is present in only a minority of patients. TTP after endothelial injury has been recognized for a long time, but postoperative TTP has only recently been appreciated as a distinct clinical syndrome in the surgical field. Furthermore, an unusual clinical presentation makes TTP diagnosis more difficult [2,3]. The conditions to be identified for differential diagnosis of thrombotic microangiopathies can include TTP, hemolytic uremic syndrome, DIC, severe hypertension, preeclampsia, eclampsia, hemolysis-elevated liver enzymes-low platelet count syndrome, systemic lupus erythematosus, drug-induced TTP, and disseminated malignancy [3]. In our patient, the platelet count immediately after surgery was more than 50% of the preoperative count, unlike the phenomenon by cardiopulmonary bypass itself or heparin-induced thrombocytopenia [4]. As our patient had presented signs and symptoms of DIC and sepsis since postoperative day 4, the thrombocytopenia was considered to be one of their signs and treated by routine management for a bleeding episode through platelet transfusion. However, the decreasing platelet count was aggravated with time and platelet transfusion regardless of the improvement in signs of DIC and sepsis. Once we determined that the etiology of the thrombocytopenia was not only sepsis but also postoperative TTP, platelet transfusion, to which our patient was refractory, was discontinued, and the laboratory work-up for differential diagnosis was performed as we described in the case report. Platelet transfusion has been traditionally associated with worse outcomes, although a recent review of platelet transfusion in patients with TTP suggested that the evidence for this might be uncertain [5].
In postoperative TTP, there might be also an autoimmune-mediated mechanism related to antibodies against a disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13 (ADAMTS-13) [6,7]. In our patient, we did not have a test for the determination of ADAMTS-13 activity or antibodies to ADAMTS-13, but the patient showed a strong positivity to the autoimmune target test. Since the patient had low compliment C3 and C4 levels, we concluded that the thrombocytopenia could not be explained by sepsis alone. Because a strong suspicion of postoperative TTP and its early treatment helps the patient's outcome, we started the treatment with a high dose of corticosteroid. Plasmapheresis is recognized as a primary treatment for TTP patients [3,6-8], but we could not perform plasmapheresis because of the persistently positive results of microorganism cultures in our patient's blood. After 5 days of 75 mg/day treatment with methylprednisolone, the platelet count reached over 50,000/µL. Kessler et al. [3] again emphasized that TTP is a rare but true hematological emergency with fatal consequences, and they recommended that once TTP is considered to be the likely diagnosis, arrangements for emergency plasma exchange should be made and high-dose corticosteroids should be given. Our patient responded to methylprednisolone therapy; the patient did not need other immunosuppressive therapy such as rituximab or cyclosporine.
The patient underwent a long period of antibiotic treatment for sepsis and monitoring for ventricular tachycardia even after the recovery of a normal platelet count, but the patient did not show the symptoms of neurologic or renal complications when she was discharged from the hospital. In conclusion, we recognized that if the postoperative patient has prolonged thrombocytopenia that has not improved with routine management, postoperative TTP, even though it is a rare disorder, should be considered and ruled out.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Marques MB. Thrombotic thrombocytopenic purpura and heparin-induced thrombocytopenia: two unique causes of life-threatening thrombocytopenia. Clin Lab Med. 2009;29:321–338. doi: 10.1016/j.cll.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Sarode R. Atypical presentations of thrombotic thrombocytopenic purpura: a review. J Clin Apher. 2009;24:47–52. doi: 10.1002/jca.20182. [DOI] [PubMed] [Google Scholar]
- 3.Kessler CS, Khan BA, Lai-Miller K. Thrombotic thrombocytopenic purpura: a hematological emergency. J Emerg Med. 2012;43:538–544. doi: 10.1016/j.jemermed.2012.01.027. [DOI] [PubMed] [Google Scholar]
- 4.Gruel Y, Pouplard C. Post-operative platelet count profile: the most reliable tool for identifying patients with true heparin-induced thrombocypenia after cardiac surgery. J Thromb Haemost. 2010;8:27–29. doi: 10.1111/j.1538-7836.2009.03646.x. [DOI] [PubMed] [Google Scholar]
- 5.Swisher KK, Terrell DR, Vesely SK, Kremer Hovinga JA, Lammle B, George JN. Clinical outcomes after platelet transfusions in patients with thrombotic thrombocytopenic purpura. Transfusion. 2009;49:873–887. doi: 10.1111/j.1537-2995.2008.02082.x. [DOI] [PubMed] [Google Scholar]
- 6.Saltzman DJ, Chang JC, Jimenez JC, et al. Postoperative thrombotic thrombocytopenic purpura after open heart operations. Ann Thorac Surg. 2010;89:119–123. doi: 10.1016/j.athoracsur.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 7.Scully M, Hunt BJ, Benjamin S, et al. Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Haematol. 2012;158:323–335. doi: 10.1111/j.1365-2141.2012.09167.x. [DOI] [PubMed] [Google Scholar]
- 8.Schiller O, Ash S, Schonfeld T, et al. Postoperative thrombotic thrombocytopenic purpura in an infant: case report and literature review. J Pediatr Surg. 2011;46:764–766. doi: 10.1016/j.jpedsurg.2011.01.009. [DOI] [PubMed] [Google Scholar]