Abstract
Objective:
To find the effect of neonatal hyperbilirubinemia on neurobehavior of term infants.
Materials and Methods:
This study was undertaken in the neonatal unit of our tertiary care hospital. Term neonates who developed jaundice with serum bilirubin value of above 15 mg/dl within 1st week of life were enrolled in the study. Peak total serum bilirubin (PSB) levels of cases were recorded. Age and sex matched normal controls were assigned to every case. Both the groups were assessed by Brazelton′s neurobehavioral assessment scale (NBAS) and the scores of the individual clusters were compared.
Results:
Habituation, range of state, autonomic regulation and regulation of state clusters were significantly altered in the case group, while motor organization cluster was mainly affected in neonates with severe jaundice (PSB > 25 mg/dl). No differences were noted in the reflex and orientation NBAS clusters.
Conclusion:
Neonatal hyperbilirubinemia causes definite alteration in the neonatal neurobehavior.
Keywords: Brazelton′s neurobehavioral assessment scale, hyperbilirubinemia, neonates, neurobehavior
Introduction
Neonatal jaundice is a leading cause of preventable brain damage in infants. In most infants, unconjugated hyperbilirubinemia reflects a normal transitional phenomenon. It is known that once advanced phases of acute bilirubin encephalopathy develop (levels above 30 mg/dl), irreversible neurologic damage is probable and likely associated with adverse neurobehavior and neurodevelopment.[1] It is still not clear whether neonatal jaundice falling short of developing “acute bilirubin encephalopathy” has any effect on neurobehavior and future development. It is still a matter of debate and research. This has led to a considerable debate whether aggressive treatment is required for less severe jaundice.[2–4] This study was conducted to find out the effects of moderate rise in bilirubin levels on neonatal neurobehavior.
Materials and Methods
The present study was conducted over a 2 year period at a tertiary care teaching hospital located in South India. All the term neonates who developed jaundice with at least one serum bilirubin value of above 15 mg/dl within 1st week of life were enrolled in the study. Neonates with major congenital anomalies, prematurity (<37 weeks), intra uterine growth retardation, birth asphyxia, convulsions or any other disease process which could possibly affect the neurobehavior were excluded from the study. Bilirubin estimation was done by spectrophotometry. A detailed antenatal history, gestational age, birth weight, sex, ethnicity and treatment history were noted. Age and sex matched normal controls were assigned to every case. The controls were normal neonates of same post natal age as cases with no apparent jaundice on clinical inspection. Bilirubin estimation was not done in controls due to ethical concerns.
Both the groups were assessed by Brazelton′s neurobehavioral assessment scale (NBAS) within 24 h of serum bilirubin estimation. The examination consists of 27 behavioral items and 20 elicited responses. The neurobehavioral items from the scale were reduced to seven clusters namely habituation, orientation, motor organization, range of state, autonomic stability, regulation of state and reflex derived conceptionally based on neurophysiology.[5] The sample size in order to achieve 80% power to detect a difference of 25% in behavioral response, at the 5% level of significance between the two groups was found to be 34 in each group. Institute ethics committee approval was obtained before starting the study. Data entry and analysis were done using SPSS for Windows Version SPSS 16.0 (SPSS Inc, Chicago, IL, USA). The mean ± SD scores of the cases group and controls were compared using unpaired t test and Welch′s corrected t test.
Results
A total of 66 neonates completed the study with 33 each in case and control group [Figure 1]. The general characteristics of case and control groups are shown in Table 1. The case group was subdivided based on the severity of peak total serum bilirubin (PSB) as mild, moderate and severe groups when the PSB value was between 15 mg% and 20 mg%, 20 mg% and 25 mg% and >25 mg% respectively.
Figure 1.
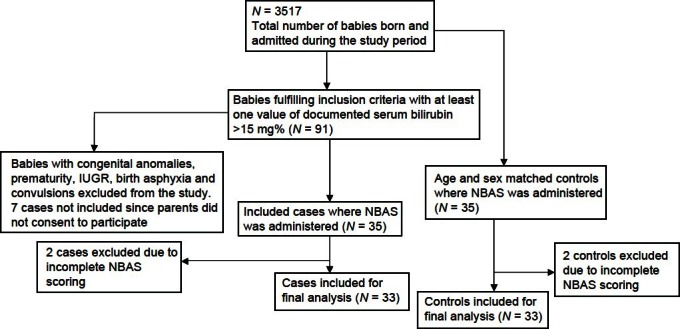
Study flow diagram
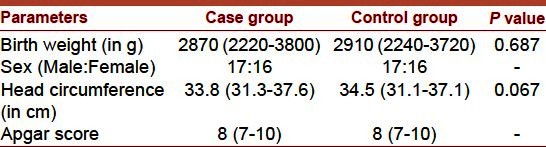
Table 1.
Characteristics of case and control groups
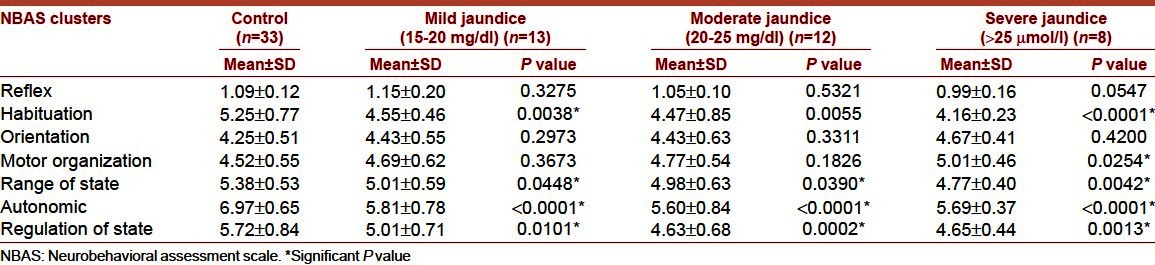
The comparison of NBAS between case groups and controls is shown in Table 2. There was a significant difference in habituation, range of state, autonomic regulation and regulation of state scores of the cases when compared with controls. The motor organization scores were significantly altered in the severe jaundice group (PSB > 25 mg/dl) when compared to controls. No significant differences in neurobehavior were noted between the case groups.
Table 2.
Comparison of neurobehavioral assessment scale clusters between mild, moderate and severe neonatal jaundice and control group
Discussion
The neurobehavioral scoring looks inward at the newborn′s capacities to maintain physiological homeostasis, to organize their states of consciousness and defend themselves against disruptions by external stimuli. The scoring also looks outward at the newborn′s capacities to engage the environment and the effect that the newborn′s form of engagement have on the environment.
The qualitative and quantitative behavioral changes are proportionately related to the severity of jaundice. The peak level of total serum bilirubin attained correlates closely with the neurologic outcome.[6] We found that habituation, range of state, autonomic regulation, and regulation of state scores were significantly altered in neonates with PSB > 15 mg/dl. Habituation is the ability not to respond to an environmental stimulus that is either disrupting the newborn′s state organization or has no functional significance to the newborn. The habituation cluster scores the behavior characterized by shut down of body movements, diminution of blinks and respiratory changes following visual, auditory or tactile stimuli. This capacity to shut down disturbing visual, auditory or tactile stimuli serves the infants who are confronted with a continuous stream of intense animate and inanimate stimulation. PSB > 15 mg/dl significantly affects the habituation center from adapting to the demands of a stimulation rich environment.
The neonatal infant displays a rich variety of behavioral states. The interplay of these states, their transition, and variety presented by the newborn is similar to examining the “higher mental functions” of the adult. The range of state cluster measures infant′s cuddliness, consolability, peak of excitement, defensive movements, irritability, activity, tremulousness, and startle responses. In our study, the neonates with jaundice were found to be drowsier during the initial state and if stimulated they became more irritable and difficult to console. In autonomic regulation cluster, the infant′s lability of skin color to various stimuli and lability of states were assessed. We observed that the neonates with jaundice had poor autonomic responses and less swings between states when compared to the controls. The regulation of state cluster, which checks the self-quieting activity, hand to mouth facility and smile of infants was also affected significantly by jaundice. Paludetto et al. observed that self-quieting abilities of neonates were affected when total bilirubin levels >13.2 mg/dl.[4]
No significant difference was noted in the reflex cluster where primitive reflexes are elicited to check the brainstem integrity of infants. Another similar study documented significant differences in habituation, orientation, motor performance, regulation of state, and autonomic stability clusters in neonates with PSB levels between 11.6 mg/dl and 14.6 mg/dl when compared to normal controls.[7]
We noted that motor organization score which measures alertness, tone, spontaneous limb movements, and infant′s response to pull to sit, was significantly altered only in neonates with severe jaundice (PSB > 25 mg/dl), suggesting that motor organization is affected with high PSB levels. The motor organization is a way of infant′s communication to indicate their preference for the type and kind of handling they need to stabilize their physiological state. In a similar study by Paludetto et al., in motor organization cluster, motor maturity and response to pull to sit were significantly poor in the group with total bilirubin levels between 13.2 mg/dl and 20 mg/dl.[4] They also observed that these cases had excessive limb movements and were not able to voluntarily shut down the unwanted excessive limb movements. However, unlike our study, the total serum bilirubin levels were assessed at the time of observation itself.
Soorani-Lunsing et al. also have observed minor motor dysfunctions in neonates with PSB of 13.6–26 mg/dl.[6] They noted that the degree of neurologic dysfunction at 12 months was proportional to the levels of bilirubin in the neonatal period especially when >20 mg/dl.[6]
The pattern of behavioral alterations that we describe has intriguing similarities with the central nervous system (CNS) involvement seen in higher bilirubin levels. Hyperbilirubinemia show extrapyramidal and sensorial involvement while other cortical functions are relatively spared. This is attributable to the predominant effect of bilirubin on basal ganglia and mesencephalic formations.[8]
Reflex responses of newborns are involuntary, neuromuscular acts that provide primitive protection against harm. Since reflexes directly mirror adaptive functioning of the very young nervous system, they can be used to determine the localization of nervous system abnormalities and the integrity of peripheral nerves. Reflex responses also provide a basis for the development of mature, purposeful movements, and postural changes. Therefore, assessment of reflexes can be particularly useful in the ongoing developmental description of infants′ movements and postures. In the present study, the reflex scores were not affected in neonates with jaundice.
Orientation is the ability to focus and process information from the environment. Infants can look, listen, smell, touch, and taste effectively. Infants can make coordinated head and eye movements and visually locate and discriminate among different targets. They can turn their heads and localize a sound. They can discriminate their mother′s milk from others with taste and odor. The orientation score is based on the responses to visual and auditory stimuli with animate and inanimate objects. The visual stimulus checks the infant′s abilities to brighten, focus, still and follow the stimulus by smooth head turning. The auditory stimulus checks the infant′s ability to quieten, still, brighten and shifting of eyes and head in search of stimuli. The neonates with jaundice were well oriented similar to the control group. However, in a similar study, increased bilirubin concentrations have been found to significantly impair orientation and state range clusters.[9] Paludetto et al. also noted impaired orientation skills with total bilirubin levels of 13.2–20 mg/dl.[4] They also repeated the NBAS at discharge among the same sets of infants who had initial abnormal neurobehavioral findings, and found only minor differences indicating the fact that the effects of bilirubin levels on brain is probably transient with no long-term sequelae.[4] Low levels of hyperbilirubinemia causes an apparently reversible alteration in the neonatal behavior due to transient involvement of the same CNS centers that will be severely affected by higher bilirubin concentrations.[4] Other investigators, studying neonates with lesser degrees of hyperbilirubinemia, have considered similar findings to be transient on the basis of short term follow-up.
The limitations of the study include assigning controls without clinical jaundice based on visual inspection alone which may not be accurate. Also, the phototherapy used for treating hyperbilirubinemia can be a significant confounding factor affecting the neurobehavior of these infants.
Conclusion
PSB levels of more than 15 mg/dl are associated with a definite alteration in the neonatal neurobehavior. Habituation, range of state, autonomic regulation, and regulation of state were significantly altered in neonates with bilirubin levels of above 15 mg/dl irrespective of the severity of jaundice. Motor organization was affected by increasing PSB levels but most strikingly in neonates with severe jaundice (PSB > 25 mg/dl). Long-term, rigorous, targeted studies are required to understand the effect of abnormal neurobehavior on neurodevelopment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Hansen TW, Nietsch L, Norman E, Bjerre JV, Hascoet JM, Mreihil K, et al. Reversibility of acute intermediate phase bilirubin encephalopathy. Acta Paediatr. 2009;98:1689–94. doi: 10.1111/j.1651-2227.2009.01409.x. [DOI] [PubMed] [Google Scholar]
- 2.Vohr BR, Lester B, Rapisardi G, O’Dea C, Brown L, Peucker M, et al. Abnormal brain-stem function (brain-stem auditory evoked response) correlates with acoustic cry features in term infants with hyperbilirubinemia. J Pediatr. 1989;115:303–8. doi: 10.1016/s0022-3476(89)80090-3. [DOI] [PubMed] [Google Scholar]
- 3.Paludetto R, Mansi G, Rinaldi P, Ariola P, Cascioli CF. Moderate hyperbilirubinemia does not influence the behavior of jaundiced infants. Biol Neonate. 1986;50:43–7. doi: 10.1159/000242560. [DOI] [PubMed] [Google Scholar]
- 4.Paludetto R, Mansi G, Raimondi F, Romano A, Crivaro V, Bussi M, et al. Moderate hyperbilirubinemia induces a transient alteration of neonatal behavior. Pediatrics. 2002;110:e50. doi: 10.1542/peds.110.4.e50. [DOI] [PubMed] [Google Scholar]
- 5.Brazelton TB, Nugent KJ. Clinics in development medicine. In: Brazelton TB, Nugent KJ, editors. Neonatal Behavioral Assessment Scales. 3rd ed. London: SIMP; 1995. p. 137. [Google Scholar]
- 6.Soorani-Lunsing I, Woltil HA, Hadders-Algra M. Are moderate degrees of hyperbilirubinemia in healthy term neonates really safe for the brain? Pediatr Res. 2001;50:701–5. doi: 10.1203/00006450-200112000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Escher-Gräub DC, Fricker HS. Jaundice and behavioral organization in the full-term neonate. Helv Paediatr Acta. 1986;41:425–35. [PubMed] [Google Scholar]
- 8.Volpe JJ. Bilirubin and brain injury. In: Volpe JJ, editor. Neurology of the Newborn. Philadelphia, PA: Saunders; 2001. pp. 521–46. [Google Scholar]
- 9.Vohr BR, Karp D, O’Dea C, Darrow D, Coll CG, Lester BM, et al. Behavioral changes correlated with brain-stem auditory evoked responses in term infants with moderate hyperbilirubinemia. J Pediatr. 1990;117:288–91. doi: 10.1016/s0022-3476(05)80549-9. [DOI] [PubMed] [Google Scholar]


