Abstract
Background:
With growing interest in global health, surgeons have created outreach missions to improve health care disparities in less developed countries. These efforts are mainly episodic with visiting surgeons performing the operations and minimal investment in local surgeon education. To create real and durable advancement in surgical services in disciplines that require urgent patient care, such as pediatric neurosurgery, improving the surgical armamentarium of the local surgeons must be the priority.
Methods:
We propose a strategic design for extending surgical education missions throughout the Western Hemisphere in order to transfer modern surgical skills to local neurosurgeons. A selection criteria and structure for targeted missions is a derivative of logistical and pedagogical lessons ascertained from previous missions by our teams in Peru and Ukraine.
Results:
Outreach programs should be applied to hospitals in capital cities to serve as a central referral center for maximal impact with fiscal efficiency. The host country should fulfill several criteria, including demonstration of geopolitical stability in combination with lack of modern neurosurgical care and equipment. The mission strategy is outlined as three to four 1-week visits with an initial site evaluation to establish a relationship with the hospital administration and host surgeons. Each visit should be characterized by collaboration between visiting and host surgeons on increasingly complex cases, with progressive transfer of skills over time.
Conclusion:
A strategic approach for surgical outreach missions should be built on collaboration and camaraderie between visiting and local neurosurgeons, with the mutual objective of cost-effective targeted renovation of their surgical equipment and skill repertoire.
Keywords: Central and South America, missions, neurosurgery, pediatric neurosurgery, targeted renovation
INTRODUCTION
Global health, defined as “an area for study, research and practice that places priority on improving health and achieving equity in health for all people,” is an increasing focus of political organizations, governmental bodies, and American medical education. Various models of medical outreach have demonstrated the ability to deliver care that creates sustained improvement, such as immunization for disease prevention, improvement of infection treatment, and water purification.[1,12,16] Surgical outreach missions do deliver care that benefits citizens of the host country, but because of the sophistication of skills and equipment needed, their impact is often episodic rather than sustained.[16]
It is estimated that the richest 30% of the world's population receives 73-76% of all surgical procedures while the poorest third receives only 3-5%. Given that the incidence of surgical disease burden is similar between rich and poor countries, surgical care in less developed countries represents a significant unmet clinical need.[2,3] As initiatives to improve surgical care in poorer countries move forward, disparate strategies have evolved.
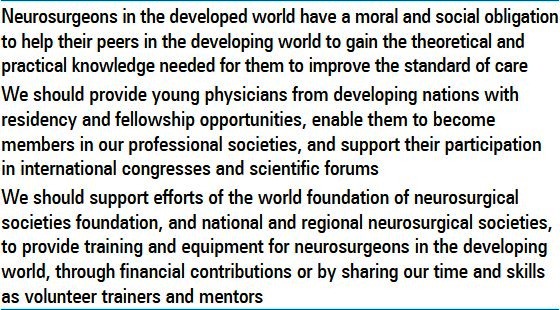
The potential to create sustainable improvements in pediatric neurosurgical care exists and is a worthwhile humanitarian goal[4,13,22] [Table 1]. However, numerous challenges exist. Since pediatric neurosurgery is a highly technical field with a limited number of surgeons, its practice often depends on advanced technology with operations that cannot be performed on an elective basis.[18,19] Therefore, if sustained improvement is the goal, educating and equipping local surgeons must become a priority. Even when this occurs, the transfer of newly acquired skills by neurosurgical teams in charity hospitals is difficult due to the lack of adequate equipment needed for assistants, students, and residents to learn the surgical steps undertaken. Accordingly, the less developed nations in the Western Hemisphere face a double challenge when providing neurosurgical care to their citizens. First, to varying degrees, they lack the basic equipment needed to provide modern care. Second, when valuable new skills are acquired or introduced, the surgeons are not equipped to teach the techniques to colleagues and students for perpetuation of surgical skills.
Table 1.
Narrowing the gap-neurosurgery in the developed and developing world
With finite resources available and many other philanthropic needs competing for the limited funds, the prospect of achieving real and sustained improvements in pediatric neurosurgical care requires a strategic design. This design must take advantage of academic neurosurgeons interested in being part of the process, and be structured so that efforts can target countries that are both interested in and committed to sustainable improvements.[1,21]
STRATEGIC APPROACH AND RATIONAL DESIGN
The great majority of described non-neurosurgical missions focus on performance of elective surgery with minimal investment on surgical education. One challenge from a public health perspective is that most existing surgical missions tackle elective nonfatal conditions that are amenable to yearly scheduling. However, the majority of the preventable surgical deaths result from injuries, obstetrics, and other surgical emergencies.[16] Neurosurgery missions require the transfer of operative skill in order to effectively manage pediatric neurological pathology that typically necessitates urgent intervention. Accordingly, the optimal model for neurosurgical outreach must have at its core the goal to teach surgical skills such that local providers can continue to perform operations after the mission is completed.[1,9,20]
To achieve this goal at a global level, it will require the careful selection and deployment of effective mission teams, with a continual focus on careful spending of limited funds. Indeed, existing organizations performing elective plastic and reconstructive surgery have been criticized for suboptimal utilization of millions of dollars.[7] Also, not every underserved region presents an educational opportunity. Differences in the medical needs of populations, the skills of local health care providers, and the level of interest in international collaboration present additional challenges.[14,21] We believe that the key to success for fiscally responsible and effective operative skill transfer is to collaborate with academic neurosurgeons in capital cities who can perpetuate the newly acquired techniques to surgeons in training as well as deliver the needed care to their citizens.[8,4,22]
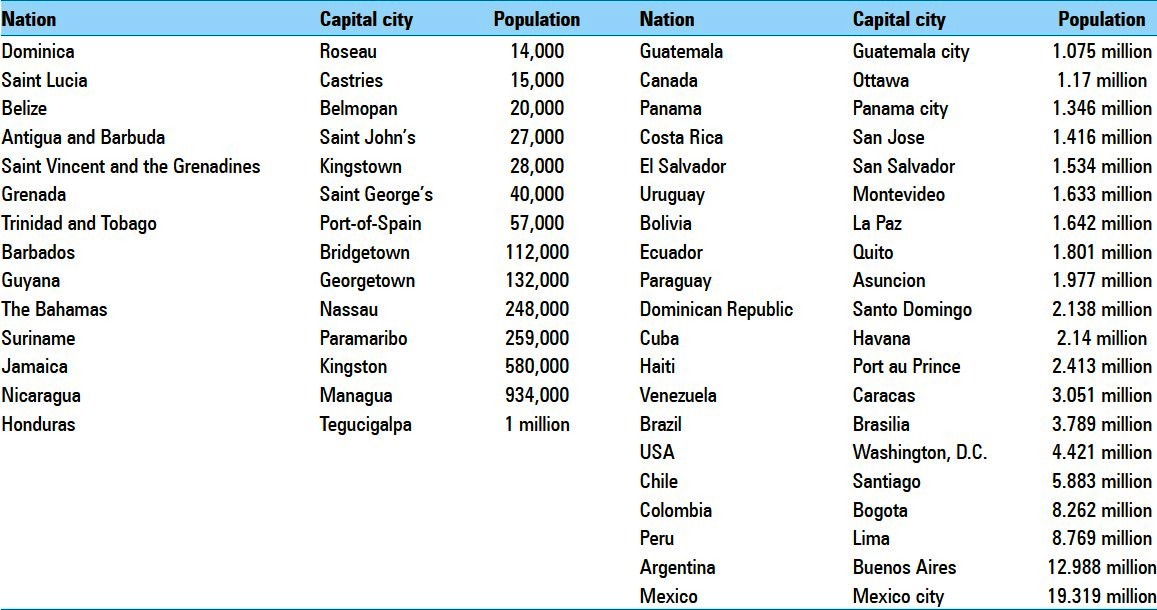
To improve pediatric neurosurgical care via targeted programs throughout the western hemisphere, upfront decisions regarding the countries that should be included and excluded need to be made. Inclusion criteria should be based on rational decision-making that is strategic in achieving its goal, but also flexible enough for changes to be made as the program grows and evolves [Table 2]. Charity hospitals in capital cities are the primary target. Often, the medical care provided in less industrialized nations in the Western Hemisphere is dichotomized. Private clinics exist for wealthy patients who can afford to purchase good medical and surgical care. In contrast, government hospitals provide care for poorer citizens, but are underfunded due to political influence and/or the relative poverty of the country.[15] Although pediatric neurosurgical care is also provided in non-capital cities, the referral centers are located predominantly in capitals where improvements in health care would have the best potential to impact the wider population. Our experience has shown that various states and municipalities often guide indigent patients to the central referral centers located in the capitals.[2] As a consequence of the limited resources available to most mission teams, western hemisphere nations with less than 1 million residents in their capitals will not be prioritized [Table 3].[5] Often countries with smaller populations rely on neighboring nations that are larger and more cosmopolitan for complex surgical care. The need for improved pediatric neurosurgical care is an obvious inclusion criterion, but the determination of “need” is complex and difficult because it is nation, city, and hospital dependent.[3] Nevertheless, certain countries can be excluded if it is established that they have modern facilities, equipment, and adequate care. Others, however, will require an onsite evaluation to evaluate the “need” criteria, which is the lack of modern pediatric neurosurgical care and lack of basic neurosurgical equipment.
Table 2.
Inclusion criteria for potential countries
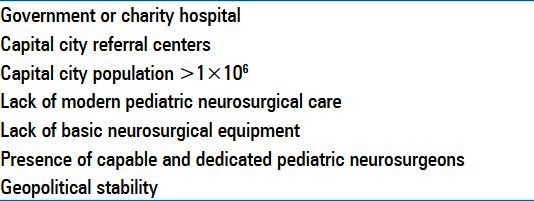
Table 3.
Western hemisphere capital city population densities
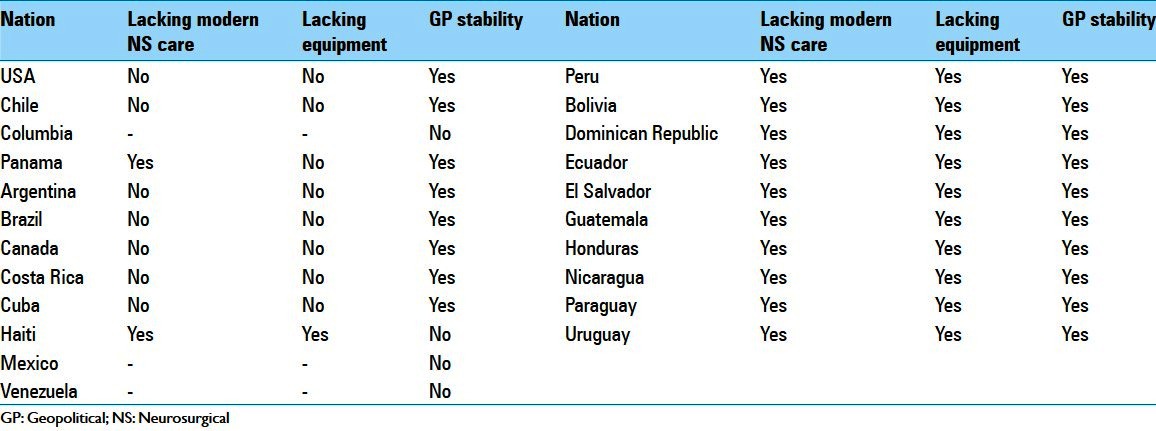
Although some hospitals are in obvious need, they must still meet the other criteria of the strategic design including but not limited to: population density, dedicated neurosurgeons willing and able to host missions, and geopolitical stability. Geopolitical stability is based on the opinions of the visiting neurosurgeons and the general travel advisory. As expected, obtaining commitments from volunteer neurosurgeons to participate in surgical missions they perceived to be dangerous is difficult. Based on all of the aforementioned inclusion criteria, the countries for potential in-person site evaluation have been selected [Table 4].[5]
Table 4.
Application of inclusion criteria
SITE EVALUATION
An in-person site evaluation is a key step for determining if the perceived “need” is in fact real and if a successful mission can be undertaken. The information obtained from digital and telephone communication needs to be verified in person prior to sending a mission group to educate and equip neurosurgeons in the selected hospitals. There are also ethical considerations for both the visiting and host teams.[23] Specifically, the site evaluation must evaluate the genuine commitment of the host neurosurgical team to improving the welfare of the indigent citizens they treat at the government or charity hospitals. Some anecdotal reports indicate that the surgical equipment donated by the surgical missions has been misappropriated for use in the private clinics.[20]
The site evaluation is also the ideal time to meet not only with the host neurosurgeons, but also with the hospital administration that must permit and promote the mission effort [Figure 1]. To complete a week of a dedicated neurosurgical mission with multiple operation dates, administrative support is critical for the cooperation of other surgeons in relinquishing operating days and preparing nurses for the increased case volume and postoperative nursing requirements. Ultimately, the on-site evaluation and face-to-face meeting allow assessment of personal and logistical elements.
Figure 1.

Photograph of meeting with administration to discuss feasibility of potential surgical missions during a site evaluation in Kiev, Ukraine 2004
MISSION DESIGN
Mission objective
The objective is to develop a strategic model for missions to provide sustainable improvements in neurosurgical care for underserved populations. The creation of a collaborative relationship in which long-term follow up data is obtainable is a priority to determine mission effectiveness. The total number of missions would be limited to three to four 1-week visits, not including the site evaluation.[6]
Pedagogical approach
The first (inaugural) visit establishes the mission foundation and demonstrates the host team's ability to successfully coordinate and execute the logistics of patient selection, operating schedules, and postoperative care – including obtaining hospital administrative support for anesthesia, nursing, and beds. The inaugural visit focuses primarily on less complicated neurosurgical cases, with the visiting team performing operations interspersed with grand-round style case presentation and discussion. Although the host team will prepare the potential operative cases, the mission week should begin with a joint clinic to evaluate patients together and come to a mutual agreement about which operations will be performed [Figure 2].[14] The second mission is more collaborative, focusing on the transfer of skills and expertise. The host neurosurgeon and visiting faculty are paired as primary and assistant surgeon for the duration of the trip [Figure 3]. Host surgeons should take an increasingly important role in operative cases and begin to function as the primary surgeon on some, in accordance with his/her level of skill. On the third mission, the host team members should be the primary surgeons on most cases [Figure 4]. Throughout the three to four 1-week missions, there should be a gradual increase in the complexity of the cases and an increasing role of host surgeons during the operations.
Figure 2.
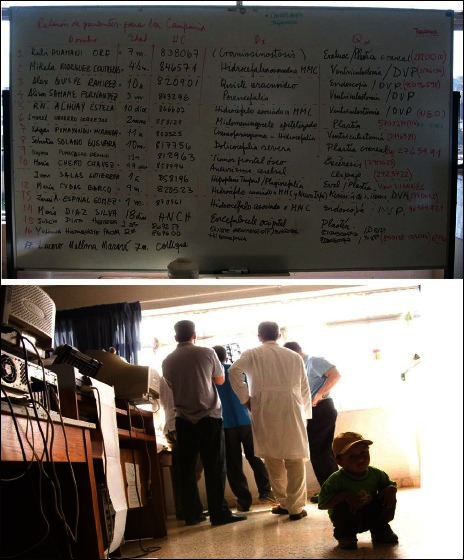
Photograph of potential case list prepared by host surgeons during inaugural mission in Lima, Peru 2003. Patients that were considered were evaluated in clinic and discussed during day one of the inaugural mission to collectively decide indications and process for undertaking planned surgical intervention
Figure 3.
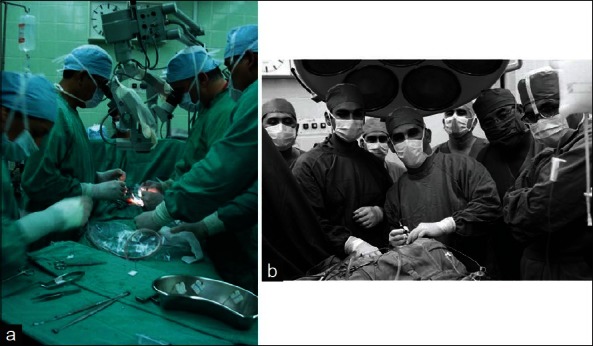
(a) Photograph of visiting surgeon and host surgeon cooperating with donated microscope. (b) Photograph of visiting surgeon assisting host surgeon during second surgical mission. Host surgeon is driving endoscope
Figure 4.

Photograph taken during last surgical mission of visiting surgeon standing un-scrubbed in corner of operating theater with primary and assist surgical roles undertaken entirely by host neurosurgeons
EFFICACY ASSESMENT AND LONG-TERM FOLLOW UP
A critical appraisal of operative skill transfer is an essential feature of sustainable, global surgical care improvement.[17,20,22] To ascertain if the collaborating teams have acquired effective technical skills, a straightforward assessment is made by the surgeons involved. However, this does not evaluate the ability of newly trained surgeons to manage complications related to newly learned operations.[20] Digital correspondence is one method by which complication management can be mutually performed. Long-term patient follow up is another limitation. Based on the population served, regular visits and follow up remain a challenge and much of the care is provided with little long-term follow-up. Despite the inability of some to return to the center in which their operation was performed, one possibility for improving data acquisition is to take advantage of the nearly ubiquitous cell-phone technology for basic patient follow up data acquisition. To improve both these limitations of current surgical missions, the dialogue should begin during the site evaluation and efforts to gather information and provide guidance must persist after completion of the mission.
CONCLUSION AND FUTURE DIRECTIONS
Effective transfer of modern operative skills to neurosurgeons can be accomplished by limited international team visits using a targeted approach to minimize expenditures on personnel and capital. By prioritizing the teaching of operative techniques as opposed to perennially performing operations, the mission team can achieve improved surgical care that is sustained after the missions officially conclude. Our experience with charity hospitals in the capital cities of Lima, Peru and Kiev, Ukraine provide a platform that can be used to effectively renovate other programs in need.[10] In both Lima and Kiev, the priority was teaching of an operative technique, as opposed to perennially performing operations by a visiting mission team, sustainable surgical care was achieved and perpetuated after missions officially concluded. Five year data from both sites demonstrate that surgeons continued to perform newly learned operations after cessation of mission trips.[10,24,25] Ultimately, this human endeavor rests on the academic collaboration between the mission and host teams. This bi-directional relationship between visiting and host neurosurgeons is best served by yearly missions over 3-4 years, thereby avoiding the pitfalls of sporadic missions.[8,11,20] Based on the model proposed here, we hypothesize that the strategic renovation of charity hospitals in the Western Hemisphere is an achievable goal.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2013/4/1/62/111092
Contributor Information
Amanda Hambrecht, Email: achambrecht@gmail.com.
Matthew J. Duenas, Email: mduenas@coh.org.
Edward J. Hahn, Email: edjhahn@gmail.com.
Henry E. Aryan, Email: DrAryan@DrAryan.com.
Samuel A. Hughes, Email: samuel.a.hughes@gmail.com.
Dawn Waters, Email: j.dawn.waters@gmail.com.
Michael L. Levy, Email: mlevy@rchsd.org.
Rahul Jandial, Email: rjandial@coh.org.
REFERENCES
- 1.Anderson F, Wansom T. Beyond medical tourism: Authentic engagement in global health. Am Med Assoc J Ethics. 2009;11:506–10. doi: 10.1001/virtualmentor.2009.11.7.medu1-0907. [DOI] [PubMed] [Google Scholar]
- 2.Azzie G, Bickler S, Farmer D, Beasley S. Partnerships for developing pediatric surgical care in low-income countries. J Pediatr Surg. 2008;43:2273–4. doi: 10.1016/j.jpedsurg.2008.08.062. [DOI] [PubMed] [Google Scholar]
- 3.Bickler S, Ozgediz D, Gosselin R, Weiser T, Spiegel D, Hsia R, et al. Key concepts for estimating the burden of surgical conditions and the unmet need for surgical care. World J Surg. 2010;34:374–80. doi: 10.1007/s00268-009-0261-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blankstein U, Dakurah T, Bagan M, Hodaie M. Structured online neurosurgical education as a novel method of education delivery in the developing world. World Neurosurg. 2011;76:224–30. doi: 10.1016/j.wneu.2011.02.041. [DOI] [PubMed] [Google Scholar]
- 5.The World Factbook. CIA, June 1997. [Last accessed on 10 May 2012]. Available from: https://www.cia.gov/library/publications/the-world-factbook/
- 6.Duenas VJ, Hahn EJ, Aryan HE, Levy MV, Jandial R. Targeted neurosurgical outreach: 5-year follow-up of operative skill transfer and sustainable care in Lima, Peru. Childs Nerv Syst. 2012;28:1227–31. doi: 10.1007/s00381-012-1771-3. [DOI] [PubMed] [Google Scholar]
- 7.Dupuis CC. Humanitarian missions in the third world: A polite dissent. Plast Reconstr Surg. 2004;113:433–5. doi: 10.1097/01.PRS.0000097680.73556.A3. [DOI] [PubMed] [Google Scholar]
- 8.Fisher QA, Nichols D, Stewart FC, Finley GA, Magee WP, Jr, Nelson K. Assessing pediatric anesthesia practices for volunteer medical services abroad. Anesthesiology. 2001;95:1315–22. doi: 10.1097/00000542-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Gosselin RA, Gyamfi YA, Contini S. Challenges of meeting surgical needs in the developing world. World J Surg. 2011;35:258–61. doi: 10.1007/s00268-010-0863-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hayden MG, Hughes S, Hahn EJ, Aryan HE, Levy ML, Jandial R. Maria Auxiliadora Hospital in Lima, Peru as a model for neurosurgical outreach to international charity hospitals. Childs Nervous Syst. 2011;27:145–8. doi: 10.1007/s00381-010-1170-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jesus JE. Ethical challenges and considerations of short-term international medical initiatives: An excursion to Ghana as a case study. Ann Emerg Med. 2010;55:17–22. doi: 10.1016/j.annemergmed.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 12.Koplan JP, Bond TC, Merson MH, Reddy KS, Rodriguez MH, Sewankambo NK, et al. Towards a common definition of global health. Lancet. 2009;373:1993–5. doi: 10.1016/S0140-6736(09)60332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mainthia R, Tye GW, Shapiro J, Doppenberg EM, Ward JD. A model for neurosurgical humanitarian aid based on 12 years of medical trips to South and Central America. J Neurosurg Pediatr. 2009;4:4–9. doi: 10.3171/2009.1.PEDS08193. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell KB, Balumuka D, Kotecha V, Said SA, Chandika A. Short-term surgical missions: Joining hands with local providers to ensure sustainability. S Afr J Surg. 2012;50:2. [PubMed] [Google Scholar]
- 15.Ozgediz D, Jamison D, Cherian M, McQueen K. The burden of surgical conditions and access to surgical care in low- and middle-income countries. Bull World Health Organ. 2008;86:646–7. doi: 10.2471/BLT.07.050435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Riviello R, Lipnick MS, Ozgediz D. Medical missions, surgical education, and capacity building. J Am Coll Surg. 2011;213:572–4. doi: 10.1016/j.jamcollsurg.2011.06.420. [DOI] [PubMed] [Google Scholar]
- 17.Suchdev P, Ahrens K, Click E, Macklin L, Evangelista D, Graham E. A model for sustainable short-term international medical trips. Ambul Pediatr. 2007;7:317–20. doi: 10.1016/j.ambp.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 18.Warf BC, Alkire BC, Bhai S, Hughes C, Schiff SJ, Vincent JR, et al. Costs and benefits of neurosurgical intervention for infant hydrocephalus in sub-Saharan Africa. J Neurosurg Pediatr. 2011;8:509–21. doi: 10.3171/2011.8.PEDS11163. [DOI] [PubMed] [Google Scholar]
- 19.Warf BC, Dagi AR, Kaaya BN, Schiff SJ. Five-year survival and outcome of treatment for postinfectious hydrocephalus in Ugandan infants. J Neurosurg Pediatr. 2011;8:502–8. doi: 10.3171/2011.8.PEDS11221. [DOI] [PubMed] [Google Scholar]
- 20.Welling DR, Ryan JM, Burris DG, Rich NM. Seven sins of humanitarian medicine. World J Surg. 2010;34:466–70. doi: 10.1007/s00268-009-0373-z. [DOI] [PubMed] [Google Scholar]
- 21.Wolfberg AJ. Volunteering overseas:Lessons from surgical brigades. N Engl J Med. 2006;354:443–5. doi: 10.1056/NEJMp058220. [DOI] [PubMed] [Google Scholar]
- 22.Zeitler DM. Education paramount in surgical missions to developing countries. Otolaryngol Head Neck Surg. 2011;144:298–9. doi: 10.1177/0194599810392494. [DOI] [PubMed] [Google Scholar]
- 23.Huges SA, Jandial R. Ethical considerations in targeted paediatric neurosurgery missions. J Med Ethics. 2013;39:51–4. doi: 10.1136/medethics-2012-100610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levy ML, Duenas VJ, Hambrecht AC, Hahn EJ, Aryan HE, Jandial R. Pediatric neurosurgery outreach: sustainability appraisal of a targeted teaching model in Kiev, Ukraine. J Surg Educ. 2012;69:611–6. doi: 10.1016/j.jsurg.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 25.Duenas VJ, Hahn EJ, Aryan HE, Jandial R. Targeted neurosurgical outreach: 5-year follow-up of operative skill transfer and sustainable care in Lima, Peru. Childs Nerv Syst. 2012;28:1227–31. doi: 10.1007/s00381-012-1771-3. [DOI] [PubMed] [Google Scholar]


