Abstract
Rapunzel syndrome is a rare type of presentation of trichobezoar, an extension of hair fibers into the small bowel and rarely beyond the ileocecal valve. Its clinical presentation is deceptive ranging from abdominal mass to symptoms of obstruction. We report a 8-year-old girl admitted with a history of abdominal pain and vomiting off and on for a period of 1 year. Ultrasound findings were suggestive of subacute intestinal obstruction. On laparotomy, trichobezoar was found in the stomach extending into small bowel and was removed. Appendix was inflammed hence it was also resected. Microscopic evidence of a hair shaft was seen in the appendix indicating appendicitis was due to luminal obstruction by hair concretions.
Keywords: Rapunzel syndrome, trichobezoar, appendicitis
INTRODUCTION
Rapunzel syndrome is a rare form of trichobezoar.[1] Trichobezoar commonly occurs in patients with psychiatric disturbances who chew and swallow their own hairs. In very rare cases like in this case, hair extends through pylorus into small bowel causing symptom and signs of partial or complete gastric outlet obstruction and presented with appendicitis. Vaughan et al. first described two cases of Rapunzel syndrome in 1968.[1] The literature review performed in 2007 by Naik et al. showed 27 cases of Rapunzel syndrome described between 1968 and 2006.[2] A few other reports on this syndrome were published in the medical literature after this date but presentation of Rapunzel syndrome with appendicitis remains exceedingly rare.[3,4,5]
CASE REPORT
An 8-year-old girl was admitted with history of abdominal pain, nausea, bilious vomiting, weight loss, and constipation. The history was on and off for almost 1 year. She was previously treated in a primary health care center as a case of gastroenteritis and parasitic infestations. Despite treatment she was receiving, there was no improvement in her condition. Physical examination revealed tenderness in right pelvic fossa and abdominal distension. Hematologic investigations show low hemolobin (9.2 gm%) and red cells were microcytic hypochromic. Total leukocyte count was raised (15,500/mm3) and differential leukocyte count reveals neutrophilia (72%). X-ray abdomen showed multiple fluid levels. Ultrasonography reveals impression of subacute intestinal obstruction with dilated bowel loops. The patient underwent an exploratory laparotomy. A huge trichobezoar was identified, which took the shape of stomach. There was a long tail of hair extending through the pylorus into the small bowel [Figure 1]. By this feature diagnosis of Rapunzel syndrome was clear. By gastrotomy and enterotomy procedure, trichobezoar was dislodged and removed. Appendix was inflamed so a decision of appendicectomy was also taken along with. On histopathologic examination hair shaft was seen in the lumen of appendix leading to acute appendicitis [Figure 2].
Figure 1.

Gross appearance of trichobezoar
Figure 2.
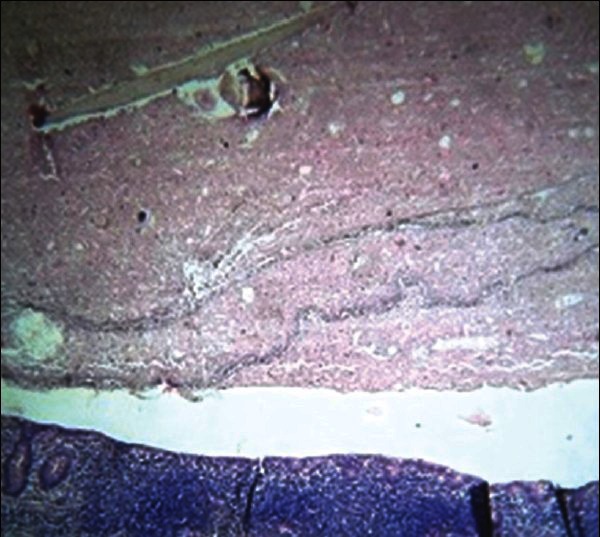
Photomicrograph showing section of appendix revealing hair shaft (H and E, ×200)
DISCUSSION
The common presentation of trichobezoar is in young females usually with an underlying psychiatric disorder. The word “bezoar” is thought to be derived from the Arabic word “badzehr” or “bazahr” for antidose. Bezoar is a tightly packed collection of undigested material, which is unable to exit through the stomach. Formation of trichobezoars occurs when the hair strands are retained in the folds of the gastric mucosa because their slippery surface prevents propulsion by peristalsis. In children, 4 types of bezoars are seen: (1) trichobezoar, which comprises mainly of hairs; (2) phytobezoar, which contains vegetable or fruit fibres; (3) lactobezoar, which is made up of milk; (4) medicinal or food bolus bezoars. Rapunzel syndrome is a rare form of trichobezoar. It is named after a tale written in 1812 by the Brothers Grimm about a young maiden, Rapunzel, with long hairs who lowered her hairs to the ground from the castle in prison tower to permit her young prince to climb up to her window and rescue her.[6,7]
This syndrome was originally described by Voughan et al. in 1968.[1] The commonly accepted definition is that of a gastric trichobezoar with a tail extending to jejunum, ileum, or ileocecal junction. Trichobezoar is usually found in the stomach, but may also be found in the duodenum, ileum, jejunum, colon, or Meckel's diverticulum.[8,9] Appendicitis secondary to trichobezoar has been described only rarely.[10] In our case the presentation is in a very young girl with hairs extending down from the stomach to small bowel, causing symptoms consistent with appendicitis. The presence of microscopic hair shaft in the lumen of appendix was a very rare and unexpected finding. If the appendix was not resected along with the trichobezoar then patient would have presented with acute appendicitis shortly. Complications of Rapunzel syndrome ranges from attacks of incomplete pyloric obstruction to complete obstruction of the bowel perforation, peritonitis, and mortality.[11] Patient with trichotillomania (a psychological condition that involves strong urges to pull out hairs), usually engage in trichophagia and of these only 1% go on to eat their hairs to the extent of requiring surgical removal.[12] Less than half of the patients give a history of trichophagia. Intensive psychiatric follow-up is mandatory to prevent relapses. Our patient was advised to attend psychiatric outpatient department. Symptoms of trichobezoar are nonspecific and may mimic other gastrointestinal conditions. For a long history of gastrointestinal problem, in a pediatric age group with history of trichophagia, endoscopy is recommended. All patients with trichobezoar should be referred for psychiatric evaluation after surgery to avoid recurrence. Also, in cases of Rapunzel syndrome, appendix should be investigated for the extension of the tail of hair, so as to avoid repeated surgeries for the patient.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Vaughan ED, Jr, Sawyers JL, Scott HW., Jr The Rapunzel syndrome. An unusual complication of intestinal bezoar. Surgery. 1968;63:339–43. [PubMed] [Google Scholar]
- 2.Naik S, Gupta V, Naik S, Rangole A, Chaudhary AK, Jain P, et al. Rapunzel syndrome reviewed and redefined. Digest Surg. 2007;24:157–61. doi: 10.1159/000102098. [DOI] [PubMed] [Google Scholar]
- 3.Middleton E, Macksey LF, Phillips JD. Rapunzel syndrome in a pediatric patient: A case report. AANA J. 2012;80:115–9. [PubMed] [Google Scholar]
- 4.Kohler JE, Millie M, Neuger E. Trichobezoar causing pancreatitis: First reported case of Rapunzel syndrome in a boy in North America. J Pediatr Surg. 2012;47:e17–9. doi: 10.1016/j.jpedsurg.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Mehta P, Bhutiani R. The Rapunzel syndrome: Is it an Asian problem? (case report and review of literature) Eur J Gastroenterol Hepatol. 2009;21:937–40. doi: 10.1097/MEG.0b013e3283140ed2. [DOI] [PubMed] [Google Scholar]
- 6.Al Wadan AH, Al Kaff H, Al Senabani J, Al Saadi AS. ‘Rapunzel syndrome’ trichobezoar in a 7-year-old girl: A case report. Cases J. 2008;1:205. doi: 10.1186/1757-1626-1-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Wadan AH, Al-Absi M, Al-Saadi AS, Abdoulgafour M. Rapunzel syndrome. Saudi Med J. 2006;27:1912–4. [PubMed] [Google Scholar]
- 8.DeBakey M, Ochsner A. Bezoars and concretions: A comprehensive review of the literature with analysis of 303 collected cases and a presentation of 8 additional cases. Surgery. 1938;4:934–63. [Google Scholar]
- 9.Vergara Rodríguez J, Sariñana Natera C. [Bezoars in childhood] Bol Med Hosp Infant Mex. 1977;34:1205–13. [PubMed] [Google Scholar]
- 10.Kochar AS. Acute appendicitis associated with a trichobezoar. JAMA. 1984;252:1681–2. doi: 10.1001/jama.1984.03350130013008. [DOI] [PubMed] [Google Scholar]
- 11.Ventura DE, Herbella FA, Schettini ST, Delmonte C. Rapunzel syndrome with a fatal outcome in a neglected child. J Pediatr Surg. 2005;40:1665–7. doi: 10.1016/j.jpedsurg.2005.06.038. [DOI] [PubMed] [Google Scholar]
- 12.Frey AS, McKee M, King RA, Martin A. Hair apparent: Rapunzel syndrome. Am J Psychiatry. 2005;162:242–8. doi: 10.1176/appi.ajp.162.2.242. [DOI] [PubMed] [Google Scholar]


