Abstract
Many human genetic disorders result from unbalanced chromosome abnormalities, in which there is a net gain or loss of genetic material. Such imbalances often disrupt large numbers of dosage-sensitive, developmentally important genes and result in specific and complex phenotypes. Alternately, some chromosomal syndromes may be caused by a deletion or duplication of a single gene with pleiotropic effects. Traditionally, chromosome abnormalities were identified by visual inspection of the chromosomes under a microscope. The use of molecular cytogenetic technologies, such as fluorescence in situ hybridization and microarrays, has allowed for the identification of cryptic or submicroscopic imbalances, which are not visible under the light microscope. Microarrays have allowed for the identification of numerous new syndromes through a genotype-first approach in which patients with the same or overlapping genomic alterations are identified and then the phenotypes are described. Because many chromosomal alterations are large and encompass numerous genes, the ascertainment of individuals with overlapping deletions and varying clinical features may allow researchers to narrow the region in which to search for candidate genes.
Keywords: chromosome, deletion, duplication, telomere, segmental duplication
Introduction
Humans have 23 pairs of chromosomes, ie, one pair of sex chromosomes (X and/or Y) and 22 pairs of autosomes (chromosomes 1–22). Many human genetic disorders result from unbalanced chromosome abnormalities, in which there is a net gain or loss of genetic material. Numeric and structural chromosomal abnormalities occur in approximately 0.6% of live births,1 and often result in dysmorphism, malformations, and/or developmental disabilities. The resulting phenotypes are caused by the imbalance of one or more dosage-sensitive genes in a particular chromosome or chromosomal segment. Such gene imbalances often have devastating consequences and cause 25% of all miscarriages and stillbirths, and 50%–60% of first-trimester miscarriages.2
Numeric abnormalities, or aneuploidies, result from the gain or loss of an entire chromosome. Most aneuploidies result from improper segregation of the chromosome pairs during meiosis. Numeric abnormalities comprise the most common cytogenetic abnormalities. Numeric abnormalities are more tolerated for the sex chromosomes and only certain autosomes. The most common monosomy is that for the X chromosome (45,X) found in Turner syndrome. Trisomy, the presence of three, rather than two, copies of a particular chromosome, causes Down syndrome, or trisomy 21, and occurs in about 1/800 live births. Other common trisomies include trisomy 13 and 18. Mosaicism for a normal cell line and an abnormal cell line may occur in a single individual. Certain trisomies, such as trisomy 8 and 9, rarely occur in all cells and are mostly found in individuals with mosaicism.
In contrast with numeric abnormalities, structural chromosomal abnormalities result from the breakage and subsequent reunion of chromosome arms. Some structural chromosome abnormalities result in gain or loss of material. Deletions involve the loss of a segment of a chromosome and duplications result in a gain of a chromosome segment. Deletions may be terminal or interstitial; a terminal deletion results after one break in the chromosome with loss of the segment distal to the break, whereas an interstitial deletion results after two breaks in the chromosome, with the loss of the intervening segment, and rejoining of the remaining chromosome segments. A duplication is caused by the gain of a copy of a chromosomal segment at the original location on the chromosome. Duplications may be in an inverted orientation or in the original (direct) orientation.
Other structural chromosome abnormalities do not result in gain or loss of any genetic material. Such rearrangements include inversions, which are caused by a two-break event and the end-to-end reversal of the intervening chromosomal segment; translocations, which result from the exchange of chromosome segments between two or more chromosomes; and insertions, which occur when a segment of one chromosome is translocated and inserted into a new region of the same chromosome, the other homolog, or a nonhomologous chromosome. These rearrangements may be pathogenic if a gene(s) is disrupted by a rearrangement breakpoint, a novel fusion gene product is formed, or a position effect is exerted on genes neighboring the rearrangement.
Compared with, for example, single-gene mutations, chromosome abnormalities often disrupt large numbers of developmentally important genes. Such imbalances may alter the dosage of genes expressed within the affected chromosomal segment, resulting in clinical consequences for the individual (see Table 1). Some imbalances result in a contiguous gene syndrome, in which multiple genes within the deleted or duplicated region are affected, each contributing a discrete clinical feature to the phenotype.3 Alternately, some chromosomal syndromes may be caused by a deletion or duplication of a single gene with pleiotropic effects. For most deletion syndromes, deletion causes haploinsufficiency of a gene or genes in the region, in which the remaining intact copy of the gene does not produce sufficient gene product for normal function. Haploinsufficiency for specific genes has been identified in several syndromes, including Williams syndrome, Langer–Giedion syndrome, Miller–Dieker syndrome, and DiGeorge/velocardiofacial syndrome.
Table 1.
| Microdeletion/microduplication syndrome | Common features | OMIM# | Gene/locus | Location | Size of aberration | Detection rate for deletion/duplication by microarray | References |
|---|---|---|---|---|---|---|---|
| 1p36 microdeletion | Dysmorphic facial features (deep-set eyes, flat nasal bridge, asymmetric ears, and pointed chin), seizures, cardiomyopathy, developmental delay, and hearing impairment | 607872 | Multiple | 1p36 | Variable | ~99% have a detectable deletion | Heistedt et al93; Helistedt et al94; Yu et al95 |
| 1q21.1 microdeletion with susceptibility for thrombocytopenia-absent radius | Hypomegakaryocytic thrombocytopenia, upper extremity abnormalities ranging from bilateral absent radii to phocomelia; normal intellect | 274000 | Multiple | 1q21.1 | 500 kb deletion mediated by LCRs | ~99% have a detectable deletion | Klopocki et al96 |
| 1q21.1 microdeletion with susceptibility to mental retardation, autism, or congenital anomalies | Mild to severe mental retardation, microcephaly, occasional congenital heart disease; schizophrenia | 612474 | Multiple | 1q21.1 | 1.5 Mb deletion mediated by LCRs | ~99% have a detectable deletion | International Schizophrenia Consortium;97 Stefansson et al;98 Brunetti-Pierri et al;99 Mefford et al100 |
| 3q29 microdeletion | Mild-to-moderate mental retardation, with only slightly dysmorphic facial features that are similar in most patients: a long and narrow face, short philtrum, and high nasal bridge | 609425 | Multiple | 3q29 | 1.5 Mb deletion mediated by LCRs | ~99% have a detectable deletion | Willatt et al101 |
| 10q22.3q23.2 microdeletion | Learning disabilities, speech and language delay, mild developmental delays, mild dysmorphic features | N/A | Multiple | 10q22.3q23.2 | 7.95 Mb deletion mediated by LCRs | ~99% have a detectable deletion | Baloiuniene et al90,91 |
| 15q11–15q13 microduplication* | Autism, mental retardation, ataxia, and seizures | 608636 | Multiple | 15q11–15q13 | Duplications most commonly occur between BP3B-BP3B and BP4-BP5 | ~99% have interstitial duplications; precise detection rate of markers depends on size of duplicated region | Wang et al102,103 |
| 15q13.3 microdeletion | Mental retardation, epilepsy, and variable dysmorphism of the face and digits | 612001 | Multiple | 15q13.3 | Deletions occur between BP3–BP5, 3.95 Mb; BP4–BP5, 1.6 Mb | ~99% have a detectable deletion | Sharp et al;104,105 Slavotinek106 |
| 15q24 microdeletion | Mild to moderate mental retardation, high anterior, hairline, downslanting palpebral fissures, long philtrum, digital abnormalities, genital abnormalities, loose connective tissue | N/A | Multiple | 15q24.1q24.3 | 1.8 Mb deletion mediated by LCRs | ~99% have a detectable deletion | Klopocki et al13,14 |
| 16p11.2p12.2 microdeletion | Severe developmental delay; hypotonia; flat facies, downslanting palpebral fissures, posteriorly rotated ears | N/A | Multiple | 16p11.2p12.2 | 7.1–8.4 Mb deletions mediated by LCRs | ~99% have a detectable deletion | Ballif et al16 |
| 17q21.31 microdeletion | Mild to severe global developmental delay, childhood hypotonia, long face, tubular, or pear-shaped nose, bulbous nasal tip, friendly/amiable behavior | 610443 | Multiple | 17q21.31 | 700 kb deletion mediated by LCRs | ~99% have a detectable deletion | Koolen et al10–12 |
| 17q23.1q23.2 microdeletion | Speech delay, postnatal growth retardation, heart defects and hand, foot and limb abnormalities | N/A | Multiple | 17q23.1q23.2 | 2.2–2.8 Mb deletions mediated by LCRs | ~99% have a detectable deletion | Ballif et al107 |
| 22q11.2 distal microdeletion | Features mildly suggestive of DGS/VCFS, prematurity, prenatal and postnatal growth delay, developmental delay, and mild skeletal abnormalities | 611867 | Multiple | 22q11.2 | 1.4 Mb–2.1 Mb deletion distal to the common 3Mb deletion of DGS/VCFS | ~99% have a detectable deletion | Ben-Shachar et al108,109 |
| 22q11.21 microduplication | Failure to thrive, marked hypotonia, sleep apnea, and seizure-like episodes in infancy, delay of gross motor development with poor fine motor skills, velopharyngeal insufficiency, and a significant delay in language skills | 608363 | Multiple | 22q11.21 | 3.0 Mb duplication | ~99% have a detectable duplication | Ensenauer et al59,110–112 |
| 22q13.3 microdeletion | Neonatal hypotonia, global developmental delay, normal to accelerated growth, absent to severely delayed speech, autistic behavior, and minor dysmorphic features | 606232 | Multiple | 22q13.3 | 130 kb deletion | ~99% have a detectable deletion | Phelan et al35,113–115 |
| Adrenal hypoplasia congenita | A rare developmental disorder of the human adrenal cortex caused by deletion or mutation of the DAX-1 gene; hypogonadotropic hypogonadism is frequently associated with AHC | 300200 | NR0B1 | Xp21.2 | Generally part of a contiguous gene deletion with Duchenne muscular dystrophy and GK | ~18% have a detectable deletion in isolated AHC; ~99% have a detectable deletion in AHC/GKD or AHC/GKD/DMD | Guo et al116,117 |
| Alagille | Chronic cholestasis caused by intrahepatic biliary hypoplasia, cardiac disease, skeletal abnormalities, and a characteristic facial phenotype | 118450 | JAG1 | 20p12.2 | Variability in deletion size | 3%–7% have a detectable deletion | Krantz et al118,119 |
| Angelman | Mental retardation, movement or balance disorder, characteristic abnormal behaviors, and severe limitations in speech and language | 105830 | UBE3A | 15q11.2 | Deletions spanning the segment between BP1 or BP2 to BP3 have been estimated at 6 Mb, although larger deletions occur | ~70% have a detectable deletion | Magenis et al120,121 |
| Beckwith-Wiedemann, IGF2-related* | Exomphalos, macroglossia, and gigantism in the neonate; an omphalocele or other umbilical abnormalities characteristic at birth | 130650 | IGF2 | 11p15.5 | Duplications of IGF2 have been reported | Majority have paternal isodisomy or mutations not detectable by array CGH | Henri et al122–124 |
| Cat eye | Coloboma of the iris, anal atresia with fistula, downslanting palpebral fissures, preauricular tags and/or pits, frequent occurrence of heart and renal malformations, and normal or near-normal mental development | 115470 | Multiple | 22q11.1 | A small supernumerary chromosome is present, frequently has two centromeres, is bisatellited, and represents an inv dup(22)(q11) | Precise detection rate unknown, although, the supernumerary marker chromosome is detectable by array CGH | Bartsch et al125–127 |
| Charcot-Marie- Tooth Type 1A | Slowly progressive distal muscle wasting, weakness and decreased nerve conduction velocities; the age of onset of symptoms is variable | 118220 | PMP22 | 17p12 | 1.5 Mb duplication mediated by LCRs | Lupski et al43,128,129 | |
| CHARGE | Coloboma of the eye, heart anomaly, atresia, choanal, retardation of mental and somatic development; microphallus; ear abnormalities and/or deafness; facial palsy, cleft palate, and dysphagia are commonly associated | 214800 | CHD7 | 8q12.2 | 2.3 Mb deletion | ~10% have a detectable deletion | Vissers et al130 |
| Cri du chat | High-pitched cat-like cry, microcephaly, round face, hypertelorism, micrognathia, epicanthal folds, low-set ears, hypotonia, and severe psychomotor and mental retardation | 123450 | Multiple | 5p15.2 | Size is variable and may be terminal, interstitial or whole arm deletions | ~99% have a detectable deletion | Church et al131–133 |
| DiGeorge 1/velocardiofacial | Hypocalcemia arising from parathyroid hypoplasia, thymic hypoplasia, and outflow tract defects of the heart; disturbance of cervical neural crest migration into the derivatives of the pharyngeal arches and pouches can account for the phenotype; many patients die due to cardiac complications or poor immune function | 188400 | HIRA TBX1 | 22q11.21 | 3.0 Mb deletion mediated by LCRs | >95% have a detectable deletion | Shaikh et al56,134,135 |
| DiGeorge 2 | Features similar to DiGeorge 1, including mild mental retardation and slight dysmorphic features of the face, head, and skeletal system | 601362 | Multiple | 10p14 | 2.0 Mb and has been reported both terminal and interstitial | <1% have a detectable deletion | Berend et al136,137 |
| Duchenne muscular dystrophy | Progressive proximal muscular dystrophy with characteristic pseudohypertrophy of the calves; massive elevation of creatine kinase levels in the blood, myopathic changes by electromyography, and myofiber degeneration, with fibrosis and fatty infiltration on muscle biopsy, onset usually occurs before age three years, and the victim is usually wheelchairridden by age 12 and dead by age 20 | 310200 | DMD | Xp21.2– p21.1 | Deletions are most often associated with a contiguous gene deletion including AHC and GK | Del Gaudio et al138–140 | |
| Greig cephalopolysyndactyly | Polydactyly, macrocephaly, and hypertelorism; may be associated with cognitive deficits and abnormalities of the corpus callosum | 175700 | GLI3 | 7p14.1 | Contiguous gene deletion with variable sizes from 151 kb to 10.6 Mb | ~30% have a detectable deletion | Johnston et al141 |
| Glycerol kinase deficiency | Mental retardation, growth retardation, elevated urinary glycerol and pseudo-hypertriglyceridemia | 300474 | GK | Xp21.2 | Deletions are most often associated with a contiguous gene deletion including AHC and GK | Deletions uncommon; majority have mutations not detectable by array CGH | Sargent et al142 |
| Hereditary liability to pressure palsies | Recurrent episodes of truncular palsies | 162500 | PMP22 | 17p12 | 1.5 Mb deletion mediated by LCRs | ~99% have detectable deletion | Inoue et al128,143–145 |
| Kallmann 1 | Congenital, isolated, idiopathic hypogonadotropic hypogonadism and anosmia. | 308700 | KAL1 | Xp22.31 | Isolated deletions are rare, often found as a contiguous gene deletion with steroid sulfatase deficiency | 10%–12% have a detectable deletion | Ballabio et al146–148 |
| Langer–Giedion | Multiple dysmorphic facial features including large, laterally protruding ears, a bulbous nose, an elongated upper lip, as well as sparse scalp hair, winged scapulae, multiple cartilaginous exostoses, redundant skin, and mental retardation | 150230 | TRPS1 EXT1 |
8q23.3 8q24.11 |
Contiguous gene deletion including TRPS1 and EXT1 | ~75% have a detectable deletion | Ludecke et al89,149,150 |
| Microphthalmia 7 with linear skin defects | Unilateral or bilateral microphthalmia and linear skin defects limited to the face and neck, consisting of areas of aplastic skin that heal with age to form hyperpigmented areas in affected females and in utero lethality for males | 309801 | Multiple | Xp22.2 | Deletions are variable in size | Precise detection rate unknown, although majority of reported deletions are detectable by array CGH | Kayserili et al151–153 |
| Miller–Dieker/Lissencephaly 1 | Lissencephaly (pachygyria, incomplete or absent gyration of the cerebrum), microcephaly, wrinkled skin over the glabella and frontal suture, prominent occiput, narrow forehead, downward slanting palpebral fissures, small nose and chin, cardiac malformations, hypoplastic male extrenal genitalia, growth retardation, and mental deficiency with seizures and electroencephalographic abnormalities. Life expectancy is grossly reduced, with death most often occurring during early childhood | 247200 | PAFAH1B1 (LIS1) | 17p13.3 | Contiguous gene deletion with a minimum size of 400 Kb | 85%–90% have a detectable deletion | Dobyns et al154,155 |
| Neurofibromatosis 1/MR | Variable facial dysmorphisms, mental retardation, developmental delay, and an excessive number of neurofibromas for age | 162200 | NF1 | 17q11.2 | ~5%–20% of all NF1 patients carry a 1.5 Mb deletion (NF1 and contiguous genes) mediated by LCRs | 5%–20% have a detectable deletion | Cnossen et al156,157 |
| Pelizaeus–Merzbacher | Nystagmus, spastic quadriplegia, ataxia, and developmental delay. | 312080 | PLP1 | Xq22.2 | Duplications are variable in size and deletions have been reported in a few cases | 60%–70% have a detectable duplication | Inoue et al158,159 |
| Potocki–Lupski/17p11.2 microduplication* | Infantile hypotonia, failure to thrive, mental retardation, autistic features, sleep apnea, and structural cardiovascular anomalies | 610883 | Multiple | 17p11.2 | Two categories of duplications: recurrent 3.7 Mb duplication mediated by LCRs and nonrecurrent duplications ranging in size from 1.3 to 15.2 Mb | ~99% have a detectable duplication | Potocki et al58,66 |
| Potocki–Shaffer | Mental retardation, biparietal foramina, minor facial anomalies, and multiple cartilaginous exostoses | 601224 | EXT2 ALX4 |
11p11.2 | 2.1 Mb deletion | ~99% have a detectable deletion | Wakui et al160,161 |
| Prader–Willi | Obesity, muscular hypotonia, mental retardation, short stature, hypogonadotropic hypogonadism, and small hands and feet; the face is characterized by a narrow bifrontal diameter, almond-shaped eyes (often in mild upslanted position), strabismus, full cheeks, and diminished mimic activity due to muscular hypotonia | 176270 | SNRPN | 15q11.2 | Type 1 mediated by LCR, BP1-BP3; Type 2 mediated by BP2 and BP3 | ~70% have a detectable deletion | Magenis et al162,163 |
| Retinoblastoma/MR | Retinoblastoma is an embryonic tumor of the eye; variability in patients with interstitial deletions at 13q14, have been seen and may include retinoblastoma tumor as well as mental retardation, reintoblastoma without mental retardation, and no retinoblastoma | 180200 | RB1 | 13q14.2 | Variable size | 80% have a detectable deletion | Cowell et al164,165 |
| Rubinstein–Taybi | Mental retardation, broad thumbs and toes, and facial abnormalities | 180849 | CREBBP | 16p13.3 | 25% of patients have a deletion encompassing the CREBBP gene | 11% have a detectable deletion | Petrij et al166,167 |
| Smith–Magenis | Broad flat midface with brachycephaly, broad nasal bridge, brachydactyly, speech delay, and hoarse, deep voice; other common features include decreased or absent deep tendon reflexes, pes planus or pes cavus, decreased sensitivity to pain, and decreased leg muscle mass, suggestive of peripheral neuropathy; self-destructive behaviors, primarily onychotillomania and polyembolokoilamania, and significant symptoms of sleep disturbance have been observed | 182290 | RAI1 | 17p11.2 | 3.7 Mb deletion mediated by LCRs | 90%–99% have a detectable deletion | Seranski et al168–171 |
| Sotos | Excessively rapid growth, acromegalic features, and a nonprogressive cerebral disorder with mental retardation; higharched palate and prominent jaw has been noted; bone age is advanced in most | 117550 | NSD1 | 5q35.3 | Some cases are 2 Mb in size mediated by LCRs; however, there are some variable size deletions. | 10%–40% have a detectable deletion depending upon ethnicity | Kurotaki et al50,172–174 |
| Steroid sulfatase deficiency | Steroid sulfatase deficiency causes an X-linked form of ichthyosis, and has a variable presentation characterized by dry, scaly skin, sparse hair and conical teeth in affected males | 308100 | STS | Xp22.31 | interstitial deletions of the STS gene | 80%–90% have a detectable deletion | Ballabio et al175–178 |
| Trichorhinophalangeal Type 1 | Dysmorphic features include sparse scalp hair, a bulbous tip of the nose, a long flat philtrum, a thin upper vermilion border and protruding ears; skeletal abnormalities include cone-shaped epiphyses at the phalanges, hip malformations, and short stature | 190350 | TRPS1 | 8q23.3 | interstitial deletions of TRPS1 gene | <20% have a detectable deletion | Momeni et al179,180 |
| WAGR | Wilms’ tumor, aniridia, genitourinary abnormalities, and mental retardation | 194072 | PAX6 WT1 |
11p13 | Contiguous gene deletion of PAX6 and WT1 | ~66% have a detectable deletion | Crolla et al181 |
| Williams–Beuren | Supravalvular aortic stenosis, multiple peripheral pulmonary arterial stenoses, elfin face, mental and statural deficiency, characteristic dental malformation, and infantile hypercalcemia | 194050 | ELN | 7q11.23 | 1.5 Mb | >95% have a detectable deletion | Nickerson et al52,182 |
| Wilms tumor Type 1 | Wilms tumor 1 is part of a contiguous gene deletion syndrome, WAGR. Wilms tumor is one of the most common solid tumors of childhood, occurring in 1 in 10,000 children and accounting for 8% of childhood cancers | 194070 | WT1 | 11p13 | 25 bp, only detectable by FISH when part of the contiguous gene deletion, WAGR | Rare deletions unless associated with contiguous gene syndrome | Royer-Pokora et al183 |
| Wolf–Hirschhorn | Severe growth retardation and mental defect, microcephaly, “Greek helmet” facies, and closure defects, including cleft lip or palate, coloboma of the eye, and cardiac septal defects | 194190 | Multiple | 4p16.3 | Terminal and interstitial deletions of 4p with a critical region of 750 kb | 95% have a detectable deletion | van Buggenhout et al184–186 |
| X-linked heterotaxy | Randomization of the placement of visceral organs, including the heart, lungs, liver, spleen, and stomach; the organs are oriented randomly with respect to the left-right axis and with respect to one another | 306955 | ZIC3 | Xq26.3 | Deletions detectable by FISH/array CGH are rare | Ferrero et al187,188 |
Abbreviations: BWS, Beckwith-Wiedermann syndrome; LCR, low-copy repeat; AHC, adrenal hypoplasia congenita; GKD, glycerol kinase deficiency; DMD, Duchenne muscular dystrophy; WAGR, Wilms’ tumor, aniridia, genitourinary abnormalities, and mental retardation; DGS/VCFS, DiGeorge/velocardiofacial syndrome; CGH, comparative genomic hybridization.
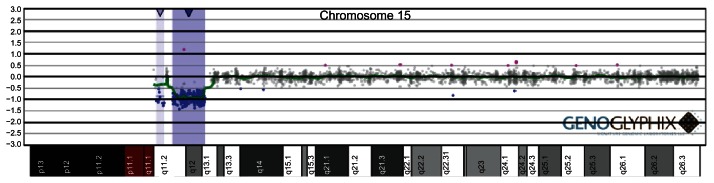
Traditionally, chromosome abnormalities were identified by visual inspection of the chromosomes under a microscope. Each chromosome can be divided into bands, which are sections of a chromosome that can be distinguishable from adjacent sections by lighter or darker variations in intensity following one or more staining methods. The original reports of chromosome rearrangements were made prior to the development of these staining techniques. Thus, any rearrangements recognized under the microscope were either numeric or an altered segment of the chromosome large enough so that the affected homolog could be easily distinguished from the normal homolog based on the overall size of the chromosome.4,5 The development of banding techniques and high-resolution chromosome analysis enabled the detection of subtle rearrangements that affected one or a few chromosome bands. The use of molecular cytogenetic technologies, such as fluorescence in situ hybridization (FISH) and microarrays, has allowed for the identification of cryptic or submicroscopic imbalances, which are not visible under the light microscope (Figure 1). Numerous previously unrecognized microdeletion and microduplication syndromes have been identified by these molecular cytogenetic techniques.6–16
Figure 1.
Identification by oligonucleotide microarray-based comparative genomic hybridization (aCGH) of a single-copy loss of the SNRPN/UBE3A locus at 15q12, deletion of which is found in individuals with Prader–Willi/Angelman syndrome. Probes are ordered on the x axis according to physical mapping positions, with the most proximal chromosome 15 q-arm clones on the left and the most distal chromosome 15 q-arm clones on the right.
In 1986, Schmickel3 first described contiguous gene syndromes (CGS) as involvement of multiple genes located in close proximity to each other on a chromosome. This term has been refined over the years and expanded to include a group of disorders defined by a deletion or duplication of a chromosomal segment spanning more than one disease gene, each affecting the phenotype independently. CGS have been described for many disorders mapping to various chromosomes. Disorders now recognized as CGS often have subtle cytogenetic changes that cannot always be resolved with conventional cytogenetic methods. Molecular cytogenetics, specifically FISH and microarray analysis, has helped to characterize many CGS.
Terminal rearrangements
Of all cytogenetically visible structural abnormalities, the majority occur in the distal telomeric bands of the chromosomes.17 Telomeres are specialized protein-DNA structures at the ends of all linear chromosomes that play numerous important cellular roles, including the prevention of chromosome degradation and end-to-end chromosome fusions,18 as well as the proper pairing, recombination, and segregation of chromosome homologs during meiosis.19 Telomeric DNA consists of tandem repeats of simple G-rich sequences that show remarkable conservation throughout eukaryotic evolution. All human chromosomes terminate with approximately 2–20 kb of the simple tandem repeat (TTAGGG)n.20 Proximal to this telomeric repeat tract is a structurally complex region of subtelomeric DNA that can extend several hundred kb from the end of most chromosomes and has been shown to be highly polymorphic.21–24 Present on all but the short arms of acrocentric chromosomes 13–15 and 21–22, the unique subtelomeric regions have elicited study because they are relatively gene-rich25,26 and are prone to rearrangement by a number of mechanisms.27,28 Thus, rearrangements of the subtelomeric regions have been suggested to represent a high proportion of abnormalities in individuals with idiopathic mental retardation and, because they are gene-rich, to result in more significant clinical consequences than similarly sized imbalances elsewhere in the genome.17,25,29
Several clinically well recognized genetic disorders are associated with terminal deletions, including deletion of distal 5p associated with cri du chat syndrome4 and distal deletion of 4p associated with Wolf–Hirschhorn syndrome.5,30 Deletion of the distal band of the short arm of chromosome 1 (monosomy 1p36) is the most common terminal deletion syndrome, occurring in about 1 in 5000 newborns.7–9
The development of sets of FISH probes for the simultaneous interrogation of all the unique human subtelomeres29,31,32 has allowed for the detection of submicroscopic chromosomal abnormalities in patients with idiopathic mental retardation but without features suggestive of a particular syndrome. The largest study of subtelomeric abnormalities to date examined 11,688 cases with subtelomere FISH and detected pathogenic abnormalities in 2.6%.33 Visible deletions of every telomeric band have been identified.17 Some of these abnormalities have been identified in a sufficiently large number of patients that the abnormality can be conclusively linked to the phenotype, which could in turn be delineated by comparison of clinical features among affected individuals.34,35 Other subtelomeric abnormalities have been identified in only one or a few patients and cannot be considered syndromic until a consistent collection of clinical features is delineated.
Because the distal G-negative bands of the unique chromosome arms are gene-rich,25 deletion or retention of this region may have profound clinical consequences in individuals with telomeric imbalances. Thus, accurate delineation of the nature of the imbalance, either terminal or interstitial, is crucial for diagnosis and prognosis. Recent large-scale prospective studies using microarrays show interstitial deletions are two to three times more frequent than terminal imbalances.36,37 Recently, Ballif et al38 characterized 169 cases with subtelomeric abnormalities identified by microarray analysis. Of these 169 cases, 42 had interstitial deletions. In addition, six (3.5%) individuals had complex rearrangements that showed deletions with duplications or additional deletions. The identification of complex rearrangements suggests chromosome abnormalities are often more complex than what was once thought.
Recurrent abnormalities mediated by underlying genomic architecture
Many recurrent chromosomal abnormalities are caused by nonallelic homologous recombination (NAHR) mediated by flanking segmental duplications.39–42 In NAHR, improper crossing-over between nonallelic, directly repeated, homologous segments (such as low-copy repeats) between sister chromatids (intrachromosomal) or between homologous chromosomes (interchromosomal) produces two reciprocal products, ie, a tandem or direct duplication and a deletion.
Such recurrent syndromes are termed “genomic disorders” and usually meet several criteria, ie, the rearrangement has breakpoints in flanking segmental duplications, the rearrangement is almost always de novo in affected individuals and is rarely seen in controls, and patients with the same rearrangement have similar, consistent phenotypes.40,41 The underlying genomic architecture in each of the genomic disorders identified to date is similar, ie, a stretch of unique sequence (50 kb–10 Mb) flanked by large (>10 kb), highly homologous (>95%) segmental duplications that provide the substrate for NAHR.
NAHR has been implicated in the recurrent rearrangements in Charcot–Marie–Tooth disease,43 hereditary neuropathy with liability to pressure palsies,44 and Prader–Willi,45 Angelman,46 Smith–Magenis,47 DiGeorge/velocardiofacial (DGS/VCFS),48 Williams–Beurens,49 and Sotos50 syndromes (see Table 1). Almost invariably, the abnormalities identified in individuals with the same genomic disorder are of identical size. For example, the common deletion in 7q11.23 found in Williams syndrome is about 1.6 Mb in size51 and is present in greater than 90% of patients.52,53 The common Smith–Magenis syndrome deletion within 17p11.2 is approximately 5 Mb47,54 and is found in the majority of patients.47,55 Approximately 90% of individuals with DGS/ VCFS have an approximately 3 Mb deletion at 22q11.2, and most of the remainder have an alternate distal deletion breakpoint, resulting in a smaller 1.5 Mb deletion, and both deletions are mediated by closely related low copy repeats in the region.56 Atypical breakpoints have been reported for other recurrent rearrangements mediated by segmental duplications. For example, some of the rarer rearrangements of 17p11.2 associated with Smith–Magenis syndrome do not have breakpoints flanked by the typical paired segmental duplications, and are not associated with known genomic architectural features,57 and some of the breakpoints in the recently identified 16p11.2p12.2 microdeletion syndrome are not flanked by segmental duplications.16
Nonallelic homologous recombination predicts that reciprocal duplications of low copy repeat-mediated deletions should occur with equal frequency.40 However, duplications have been reported more rarely than expected.58–62 One explanation is that individuals with duplications usually have milder phenotypes that may not lead to clinical investigation than individuals with deletions.59,61–66 Furthermore, duplications involving segments smaller than 1.5 Mb may be routinely missed, even by FISH of interphase nuclei.67 However, recent large population studies of individuals tested by microarray analysis have shown that the frequency of reciprocal duplications is higher than in previous studies with other cytogenetic technologies.68–71 Duplications of the common Rett syndrome gene MECP2 have been identified in males with developmental delay,72 and the reciprocal duplications of microdeletion syndromes, such as 3q29 microdeletion syndrome,73 Williams–Beuren syndrome,74 and the 22q11.21 microdeletion syndrome,59 have been identified by microarray testing. The clinical significance of some of these reciprocal duplications is not known. For example, only two individuals had de novo microduplications of 3q29, whereas the remaining cases were inherited from a carrier parent. Thus, the clinical significance of these duplications is unclear, and any phenotype may be modulated by an as yet unidentified genetic modifier.
Several new syndromes, including 8p23 duplication75 and 16p12.1 microdeletion,76 can be transmitted from parent to child. The study of 16p12.1 microdeletions presents an interesting case study of the previously underappreciated complexity of genetic disorder pathogenesis. Recurrent microdeletions of 16p12.1 have been identified in individuals referred for genetic testing for idiopathic mental retardation and congenital anomalies, and appear to be enriched in such individuals compared with clinically normal controls.76 Almost all the 16p12.1 microdeletions identified have been inherited from a carrier parent. Carrier parents for the 16p12.1 microdeletion are more likely to exhibit learning disability, bipolar disorder or depression, and seizures than noncarrier parents. The presence of varying degrees of learning disability in the adult family members suggests that some transmitted abnormalities are pathologic and have an underappreciated contribution to the phenotype.76
Deletions of varying size may elucidate causative genes for syndromes
Because many chromosomal alterations are large and encompass numerous genes, the ascertainment of individuals with overlapping deletions and varying clinical features may allow researchers to narrow the region in which to search for candidate genes. For example, varying-sized deletions at Xp21 comprise a contiguous gene syndrome that encompasses seven disorders, ie, adrenal hypoplasia congenita, glycerol kinase, Duchenne muscular dystrophy, McLeod phenotype, chronic granulomatous disease, retinitis pigmentosa, and ornithine transcarbamylase deficiency. The first recognized patient with an Xp21 contiguous gene deletion was diagnosed with Duchenne muscular dystrophy associated with chronic granulomatous disease, retinitis pigmentosa, and McLeod phenotype.77 Molecular studies of subsequent individuals with varyingsized deletions at Xp21 and varying phenotypes allowed for the construction of a disease gene map and the identification of causative genes for each of these disorders.78–81
Such an approach also allowed researchers to delineate the critical regions of trichorhinophalangeal syndrome type 1 and trichorhinophalangeal syndrome type 2, also known as Langer-Giedion syndrome. Langer–Giedion syndrome combines the features of trichorhinophalangeal syndrome type 1 and multiple exostoses type 1. The cytogenetic basis of Langer–Giedion syndrome was unknown until high-resolution banding identified interstitial deletions in the long arm of chromosome 8 in patients with this syndrome,82,83 and the location of the deletion was subsequently determined to be 8q24.1.84,85 Mapping of the deletion breakpoints in a cohort of Langer–Giedion syndrome patients showed that 75% have cytogenetically detectable deletions of 8q24.1.86 The identification of an individual with trichorhinophalangeal syndrome Type 1 but not exostoses and with a partial microdeletion of 8q2387 suggested that Langer–Giedion syndrome was caused by deletion of two or more genes, disruption of one of which results in trichorhinophalangeal syndrome Type 1 and disruption of the other of which results in multiple exostoses. Buhler et al88 concluded that the Langer–Giedion syndrome is due to a deletion extending from 8q24.11 to 8q24.13, whereas trichorhinophalangeal syndrome Type 1 is caused by an even smaller deleted segment, namely, 8q24.12. Thus, it was determined that Langer–Giedion syndrome, which combines features of trichorhinophalangeal syndrome Type 1 and multiple exostoses, is a contiguous gene syndrome caused by haploinsufficiency of both TRPS1 and EXT1.89
Genotype-first approach to diagnosis
Many of the recently identified syndromes have been identified through a genotype-first approach, rather than a typical phenotype-first approach.6 In the phenotype-first approach, the astute clinician would gather patients based on clinical presentation. This approach took many years to observe several rare individuals and develop a syndrome. The resulting syndromes had very consistent phenotypes among patients. In contrast, the genotype-first approach identifies patients with the same or overlapping genomic alterations and then describes the phenotypes observed. In this latter approach, the patients often display varying features, and in hindsight would not have been grouped based on clinical presentation alone.
Recently, microarrays designed to interrogate known segmental duplication “hotspots” of the genome have identified several previously unrecognized genomic disorders. Recurrent microdeletions of chromosome 10q22.3q23.3,90,91 15q24,13–15 16p11.2p12.2,16 17q21.31,10–12 and 17q23.1q23.292 have been identified in such a manner. In all cases, the majority of patients identified met the classical definition of a recurrent genomic disorder. The deletions were flanked by segmental duplications, the deletions were always apparently de novo in origin, and the patients had similar clinical features.41 However, the clinical features of these syndromes do not usually evoke a diagnostic Gestalt, which demonstrates the utility of the genotype-first approach in the absence of striking clinical features.
The genotype-first approach may also enable the identification of small deletions or duplications that reveal the causative genes for specific clinical features, which can aid diagnosis and prognosis. For example, researchers recently identified what is likely to be the causative gene for features of 2q32q33 microdeletion syndrome.92 Individuals with the syndrome have severe mental retardation, growth retardation, dysmorphic facial features, thin and sparse hair, feeding difficulties, and cleft or high palate. Although deletions of varying sizes have been reported, the smallest region deleted in all patients contains at least seven genes. One of these genes, SATB2, is a DNA-binding protein that regulates how genes are expressed. Deletion of SATB2 has been suggested to cause the cleft or high palate of individuals with 2q32q33 microdeletion syndrome. The recent study identified three individuals with small deletions of this region, all of which spanned part of SATB2. Common clinical features among these individuals included severe developmental delay, behavioral problems, and tooth abnormalities. Interestingly, only one of the individuals had a cleft palate. Because the individuals had a portion of only one gene missing and the presence of many of the features associated with the larger microdeletion syndrome, the study authors suggested deletion of SATB2 was sufficient to cause several of the clinical features associated with 2q32q33 microdeletion syndrome.92
Summary
Chromosomal disorders are the most frequent cause of mental retardation and developmental disabilities in our population. The phenotypes are often complex, and the result of a gain or loss of multiple, dosage-sensitive genes in the altered segments. The characterization of these complex phenotypes with overlapping deletions has allowed for the identification of genes causing particular features of the syndrome. The use of high-resolution technologies, such as microarrays, has allowed for the identification of new syndromes through a genotype-first approach at an unprecedented frequency never before imagined through the light microscope. Cytogenetics is no longer in its infancy, and has emerged a “new” genome science that, with the use of new technologies, has established the causes of mental retardation, developmental disabilities, and birth defects in our population.
Footnotes
Disclosure
A Theisen and LG Shaffer are employees of Signature Genomic Laboratories, a subsidiary of PerkinElmer.
References
- 1.Shaffer LG, Lupski JR. Molecular mechanisms for constitutional chromosomal rearrangements in humans. Annu Rev Genet. 2000;34:297–329. doi: 10.1146/annurev.genet.34.1.297. [DOI] [PubMed] [Google Scholar]
- 2.Hassold T, Chen N, Funkhouser J, et al. A cytogenetic study of 1000 spontaneous abortions. Ann Hum Genet. 1980;44(Pt 2):151–178. doi: 10.1111/j.1469-1809.1980.tb00955.x. [DOI] [PubMed] [Google Scholar]
- 3.Schmickel RD. Contiguous gene syndromes: a component of recognizable syndromes. J Pediatr. 1986;109(2):231–241. doi: 10.1016/s0022-3476(86)80377-8. [DOI] [PubMed] [Google Scholar]
- 4.Lejeune L, Lafourcade J, de Grouchy J, et al. Partial deletion of the short arm of chromosome 5. Individualization of a new morbid state. Sem Hop Paris. 1964;18:1069–1079. [PubMed] [Google Scholar]
- 5.Wolf U, Reinwein H, Porsch R, Schroter R, Baitsch H. Deficiency on the short arms of a chromosome No. 4. Humangenetik. 1965;1:397–413. [PubMed] [Google Scholar]
- 6.Shaffer LG, Theisen A, Bejjani BA, et al. The discovery of microdeletion syndromes in the post-genomic era: review of the methodology and characterization of a new 1q41q42 microdeletion syndrome. Genet Med. 2007;9(9):607–616. doi: 10.1097/gim.0b013e3181484b49. [DOI] [PubMed] [Google Scholar]
- 7.Gajecka M, Mackay KL, Shaffer LG. Monosomy 1p36 deletion syndrome. Am J Med Genet C Semin Med Genet. 2007;145C(4):346–356. doi: 10.1002/ajmg.c.30154. [DOI] [PubMed] [Google Scholar]
- 8.Shapira SK, McCaskill C, Northrup H, et al. Chromosome 1p36 deletions: the clinical phenotype and molecular characterization of a common newly delineated syndrome. Am J Hum Genet. 1997;61(3):642–650. doi: 10.1086/515520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Slavotinek A, Shaffer LG, Shapira SK. Monosomy 1p36. J Med Genet. 1999;36(9):657–663. [PMC free article] [PubMed] [Google Scholar]
- 10.Koolen DA, Vissers LE, Pfundt R, et al. A new chromosome 17q21.31 microdeletion syndrome associated with a common inversion polymorphism. Nat Genet. 2006;38(9):999–1001. doi: 10.1038/ng1853. [DOI] [PubMed] [Google Scholar]
- 11.Sharp AJ, Hansen S, Selzer RR, et al. Discovery of previously unidentified genomic disorders from the duplication architecture of the human genome. Nat Genet. 2006;38(9):1038–1042. doi: 10.1038/ng1862. [DOI] [PubMed] [Google Scholar]
- 12.Shaw-Smith C, Pittman AM, Willatt L, et al. Microdeletion encompassing MAPT at chromosome 17q21.3 is associated with developmental delay and learning disability. Nat Genet. 2006;38(9):1032–1037. doi: 10.1038/ng1858. [DOI] [PubMed] [Google Scholar]
- 13.Klopocki E, Graul-Neumann LM, Grieben U, et al. A further case of the recurrent 15q24 microdeletion syndrome, detected by array CGH. Eur J Pediatr. 2008;167(8):903–908. doi: 10.1007/s00431-007-0616-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharp AJ, Selzer RR, Veltman JA, et al. Characterization of a recurrent 15q24 microdeletion syndrome. Hum Mol Genet. 2007;16(5):567–572. doi: 10.1093/hmg/ddm016. [DOI] [PubMed] [Google Scholar]
- 15.Marshall CR, Noor A, Vincent JB, et al. Structural variation of chromosomes in autism spectrum disorder. Am J Hum Genet. 2008;82(2):477–488. doi: 10.1016/j.ajhg.2007.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ballif BC, Hornor SA, Jenkins E, et al. Discovery of a previously unrecognized microdeletion syndrome of 16p11.2–16p12.2. Nat Genet. 2007;39(9):1071–1073. doi: 10.1038/ng2107. [DOI] [PubMed] [Google Scholar]
- 17.Borgaonkar DS. Chromosomal Variation in Man. A Catalog of Chromosomal Variants and Anomalies. 4th ed. New York, NY: Alan R. Liss, Inc; 1984. [Google Scholar]
- 18.McClintock B. The stability of broken ends of chromosomes in Zea mays. Genetics. 1941;26:234–282. doi: 10.1093/genetics/26.2.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cooper JP. Telomere transitions in yeast: the end of the chromosome as we know it. Curr Opin Genet Dev. 2000;10(2):169–177. doi: 10.1016/s0959-437x(00)00070-8. [DOI] [PubMed] [Google Scholar]
- 20.Moyzis RK, Buckingham JM, Cram LS, et al. A highly conserved repetitive DNA sequence, (TTAGGG)n, present at the telomeres of human chromosomes. Proc Natl Acad Sci U S A. 1988;85(18):6622–6626. doi: 10.1073/pnas.85.18.6622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown WR, MacKinnon PJ, Villasante A, Spurr N, Buckle VJ, Dobson MJ. Structure and polymorphism of human telomere-associated DNA. Cell. 1990;63(1):119–132. doi: 10.1016/0092-8674(90)90293-n. [DOI] [PubMed] [Google Scholar]
- 22.Cross SH, Allshire RC, McKay SJ, McGill NI, Cooke HJ. Cloning of human telomeres by complementation in yeast. Nature. 1989;338(6218):771–774. doi: 10.1038/338771a0. [DOI] [PubMed] [Google Scholar]
- 23.Flint J, Bates GP, Clark K, et al. Sequence comparison of human and yeast telomeres identifies structurally distinct subtelomeric domains. Hum Mol Genet. 1997;6(8):1305–1313. doi: 10.1093/hmg/6.8.1305. [DOI] [PubMed] [Google Scholar]
- 24.Riethman H, Ambrosini A, Castaneda C, et al. Mapping and initial analysis of human subtelomeric sequence assemblies. Genome Res. 2004;14(1):18–28. doi: 10.1101/gr.1245004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saccone S, de Sario A, Della Valle G, Bernardi G. The highest gene concentrations in the human genome are in telomeric bands of metaphase chromosomes. Proc Natl Acad Sci U S A. 1992;89(11):4913–4917. doi: 10.1073/pnas.89.11.4913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saccone S, de Sario A, Wiegant J, Raap AK, Della Valle G, Bernardi G. Correlations between isochores and chromosomal bands in the human genome. Proc Natl Acad Sci U S A. 1993;90(24):11929–11933. doi: 10.1073/pnas.90.24.11929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ballif BC, Wakui K, Gajecka M, Shaffer LG. Translocation breakpoint mapping and sequence analysis in three monosomy 1p36 subjects with der(1)t(1;1)(p36;q44) suggest mechanisms for telomere capture in stabilizing de novo terminal rearrangements. Hum Genet. 2004;114(2):198–206. doi: 10.1007/s00439-003-1029-y. [DOI] [PubMed] [Google Scholar]
- 28.Ballif BC, Yu W, Shaw CA, Kashork CD, Shaffer LG. Monosomy 1p36 breakpoint junctions suggest pre-meiotic breakage-fusion-bridge cycles are involved in generating terminal deletions. Hum Mol Genet. 2003;12(17):2153–2165. doi: 10.1093/hmg/ddg231. [DOI] [PubMed] [Google Scholar]
- 29.A complete set of human telomeric probes and their clinical application. National Institutes of Health and Institute of Molecular Medicine collaboration. Nat Genet. 1996;14(1):86–89. doi: 10.1038/ng0996-86. [DOI] [PubMed] [Google Scholar]
- 30.Hirschhorn K, Cooper HL, Firschein IL. Deletion of short arms of chromosomes 4–5 in a child with defects of midline fusion. Humangenetik. 1965;1:479–482. doi: 10.1007/BF00279124. [DOI] [PubMed] [Google Scholar]
- 31.Flint J, Wilkie AO, Buckle VJ, Winter RM, Holland AJ, McDermid HE. The detection of subtelomeric chromosomal rearrangements in idiopathic mental retardation. Nat Genet. 1995;9(2):132–140. doi: 10.1038/ng0295-132. [DOI] [PubMed] [Google Scholar]
- 32.Knight SJ, Horsley SW, Regan R, et al. Development and clinical application of an innovative fluorescence in situ hybridization technique which detects submicroscopic rearrangements involving telomeres. Eur J Hum Genet. 1997;5(1):1–8. [PubMed] [Google Scholar]
- 33.Ravnan JB, Tepperberg JH, Papenhausen P, et al. Subtelomere FISH analysis of 11 688 cases: an evaluation of the frequency and pattern of subtelomere rearrangements in individuals with developmental disabilities. J Med Genet. 2006;43(6):478–489. doi: 10.1136/jmg.2005.036350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ning Y, Rosenberg M, Biesecker LG, Ledbetter DH. Isolation of the human chromosome 22q telomere and its application to detection of cryptic chromosomal abnormalities. Hum Genet. 1996;97(6):765–769. doi: 10.1007/BF02346187. [DOI] [PubMed] [Google Scholar]
- 35.Phelan MC, Rogers RC, Saul RA, et al. 22q13 deletion syndrome. Am J Med Genet. 2001;101(2):91–99. doi: 10.1002/1096-8628(20010615)101:2<91::aid-ajmg1340>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 36.Shaw-Smith C, Redon R, Rickman L, et al. Microarray based comparative genomic hybridisation (array-CGH) detects submicroscopic chromosomal deletions and duplications in patients with learning disability/mental retardation and dysmorphic features. J Med Genet. 2004;41(4):241–248. doi: 10.1136/jmg.2003.017731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vissers LE, de Vries BB, Osoegawa K, et al. Array-based comparative genomic hybridization for the genomewide detection of submicroscopic chromosomal abnormalities. Am J Hum Genet. 2003;73(6):1261–1270. doi: 10.1086/379977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ballif BC, Sulpizio SG, Lloyd RM, et al. The clinical utility of enhanced subtelomeric coverage in array CGH. Am J Med Genet A. 2007;143A(16):1850–1857. doi: 10.1002/ajmg.a.31842. [DOI] [PubMed] [Google Scholar]
- 39.Shaffer LG, Ledbetter DH, Lupski JR. Molecular cytogenetics of contiguous gene syndromes: mechanisms and consequences of gene dosage imbalance. In: Scriver CR, Beaudet AL, Sly WS, et al., editors. Metabolic and Molecular Basis of Inherited Disease. 8th ed. Vol. 1. New York, NY: McGraw Hill; 2001. pp. 1291–1324. [Google Scholar]
- 40.Lupski JR. Genomic disorders: structural features of the genome can lead to DNA rearrangements and human disease traits. Trends Genet. 1998;14(10):417–422. doi: 10.1016/s0168-9525(98)01555-8. [DOI] [PubMed] [Google Scholar]
- 41.Mefford HC, Eichler EE. Duplication hotspots, rare genomic disorders, and common disease. Curr Opin Genet Dev. 2009;19(3):196–204. doi: 10.1016/j.gde.2009.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stankiewicz P, Lupski JR. Genome architecture, rearrangements and genomic disorders. Trends Genet. 2002;18(2):74–82. doi: 10.1016/s0168-9525(02)02592-1. [DOI] [PubMed] [Google Scholar]
- 43.Lupski JR, de Oca-Luna RM, Slaugenhaupt S, et al. DNA duplication associated with Charcot-Marie-Tooth disease type 1A. Cell. 1991;66(2):219–232. doi: 10.1016/0092-8674(91)90613-4. [DOI] [PubMed] [Google Scholar]
- 44.Chance PF, Alderson MK, Leppig KA, et al. DNA deletion associated with hereditary neuropathy with liability to pressure palsies. Cell. 1993;72(1):143–151. doi: 10.1016/0092-8674(93)90058-x. [DOI] [PubMed] [Google Scholar]
- 45.Carrozzo R, Rossi E, Christian SL, et al. Inter- and intrachromosomal rearrangements are both involved in the origin of 15q11–15q13 deletions in Prader-Willi syndrome. Am J Hum Genet. 1997;61(1):228–231. doi: 10.1086/513907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Amos-Landgraf JM, Ji Y, Gottlieb W, et al. Chromosome breakage in the Prader-Willi and Angelman syndromes involves recombination between large, transcribed repeats at proximal and distal breakpoints. Am J Hum Genet. 1999;65(2):370–386. doi: 10.1086/302510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen KS, Manian P, Koeuth T, et al. Homologous recombination of a flanking repeat gene cluster is a mechanism for a common contiguous gene deletion syndrome. Nat Genet. 1997;17(2):154–163. doi: 10.1038/ng1097-154. [DOI] [PubMed] [Google Scholar]
- 48.Edelmann L, Pandita RK, Spiteri E, et al. A common molecular basis for rearrangement disorders on chromosome 22q11. Hum Mol Genet. 1999;8(7):1157–1167. doi: 10.1093/hmg/8.7.1157. [DOI] [PubMed] [Google Scholar]
- 49.Perez Jurado LA, Wang YK, Peoples R, Coloma A, Cruces J, Francke U. A duplicated gene in the breakpoint regions of the 7q11.23 Williams- Beuren syndrome deletion encodes the initiator binding protein TFII-I and BAP-135, a phosphorylation target of BTK. Hum Mol Genet. 1998;7(3):325–334. doi: 10.1093/hmg/7.3.325. [DOI] [PubMed] [Google Scholar]
- 50.Kurotaki N, Harada N, Shimokawa O, et al. Fifty microdeletions among 112 cases of Sotos syndrome: low copy repeats possibly mediate the common deletion. Hum Mutat. 2003;22(5):378–387. doi: 10.1002/humu.10270. [DOI] [PubMed] [Google Scholar]
- 51.Peoples R, Franke Y, Wang YK, et al. A physical map, including a BAC/ PAC clone contig, of the Williams-Beuren syndrome – deletion region at 7q11.23. Am J Hum Genet. 2000;66(1):47–68. doi: 10.1086/302722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nickerson E, Greenberg F, Keating MT, McCaskill C, Shaffer LG. Deletions of the elastin gene at 7q11.23 occur in approximately 90% of patients with Williams syndrome. Am J Hum Genet. 1995;56(5):1156–1161. [PMC free article] [PubMed] [Google Scholar]
- 53.Wu YQ, Nickerson E, Shaffer LG, Keppler-Noreuil K, Muilenburg A. A case of Williams syndrome with a large, visible cytogenetic deletion. J Med Genet. 1999;36(12):928–932. [PMC free article] [PubMed] [Google Scholar]
- 54.Trask BJ, Mefford H, van den Engh G, et al. Quantification by flow cytometry of chromosome-17 deletions in Smith-Magenis syndrome patients. Hum Genet. 1996;98(6):710–718. doi: 10.1007/s004390050291. [DOI] [PubMed] [Google Scholar]
- 55.Juyal RC, Figuera LE, Hauge X, et al. Molecular analyses of 17p11.2 deletions in 62 Smith-Magenis syndrome patients. Am J Hum Genet. 1996;58(5):998–1007. [PMC free article] [PubMed] [Google Scholar]
- 56.Shaikh TH, Kurahashi H, Saitta SC, et al. Chromosome 22-specific low copy repeats and the 22q11.2 deletion syndrome: genomic organization and deletion endpoint analysis. Hum Mol Genet. 2000;9(4):489–501. doi: 10.1093/hmg/9.4.489. [DOI] [PubMed] [Google Scholar]
- 57.Stankiewicz P, Shaw CJ, Dapper JD, et al. Genome architecture catalyzes nonrecurrent chromosomal rearrangements. Am J Hum Genet. 2003;72(5):1101–1116. doi: 10.1086/374385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Potocki L, Chen KS, Park SS, et al. Molecular mechanism for duplication 17p11.2- the homologous recombination reciprocal of the Smith- Magenis microdeletion. Nat Genet. 2000;24(1):84–87. doi: 10.1038/71743. [DOI] [PubMed] [Google Scholar]
- 59.Ensenauer RE, Adeyinka A, Flynn HC, et al. Microduplication 22q11.2, an emerging syndrome: clinical, cytogenetic, and molecular analysis of thirteen patients. Am J Hum Genet. 2003;73(5):1027–1040. doi: 10.1086/378818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hassed SJ, Hopcus-Niccum D, Zhang L, Li S, Mulvihill JJ. A new genomic duplication syndrome complementary to the velocardiofacial (22q11 deletion) syndrome. Clin Genet. 2004;65(5):400–404. doi: 10.1111/j.0009-9163.2004.0212.x. [DOI] [PubMed] [Google Scholar]
- 61.Yobb TM, Somerville MJ, Willatt L, et al. Microduplication and triplication of 22q11.2: a highly variable syndrome. Am J Hum Genet. 2005;76(5):865–876. doi: 10.1086/429841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Somerville MJ, Mervis CB, Young EJ, et al. Severe expressive-language delay related to duplication of the Williams-Beuren locus. N Engl J Med. 2005;353(16):1694–1701. doi: 10.1056/NEJMoa051962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brewer C, Holloway S, Zawalnyski P, Schinzel A, FitzPatrick D. A chromosomal deletion map of human malformations. Am J Hum Genet. 1998;63(4):1153–1159. doi: 10.1086/302041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Brewer C, Holloway S, Zawalnyski P, Schinzel A, FitzPatrick D. A chromosomal duplication map of malformations: regions of suspected haplo- and triplolethality – and tolerance of segmental aneuploidy – in humans. Am J Hum Genet. 1999;64(6):1702–1708. doi: 10.1086/302410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Berg JS, Brunetti-Pierri N, Peters SU, et al. Speech delay and autism spectrum behaviors are frequently associated with duplication of the 7q11.23 Williams-Beuren syndrome region. Genet Med. 2007;9(7):427–441. doi: 10.1097/gim.0b013e3180986192. [DOI] [PubMed] [Google Scholar]
- 66.Potocki L, Bi W, Treadwell-Deering D, et al. Characterization of Potocki-Lupski syndrome (dup(17)(p11.2p11.2)) and delineation of a dosage-sensitive critical interval that can convey an autism phenotype. Am J Hum Genet. 2007;80(4):633–649. doi: 10.1086/512864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shaffer LG, Kennedy GM, Spikes AS, Lupski JR. Diagnosis of CMT1A duplications and HNPP deletions by interphase FISH: implications for testing in the cytogenetics laboratory. Am J Med Genet. 1997;69(3):325–331. [PubMed] [Google Scholar]
- 68.Shaffer LG, Bejjani BA, Torchia B, Kirkpatrick S, Coppinger J, Ballif BC. The identification of microdeletion syndromes and other chromosome abnormalities: Cytogenetic methods of the past, new technologies for the future. Am J Med Genet C Semin Med Genet. 2007;145C(4):335–345. doi: 10.1002/ajmg.c.30152. [DOI] [PubMed] [Google Scholar]
- 69.Shaffer LG, Kashork CD, Saleki R, et al. Targeted genomic microarray analysis for identification of chromosome abnormalities in 1500 consecutive clinical cases. J Pediatr. 2006;149(1):98–102. doi: 10.1016/j.jpeds.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 70.Lu X, Shaw CA, Patel A, et al. Clinical implementation of chromosomal microarray analysis: summary of 2513 postnatal cases. PLoS ONE. 2007;2(3):e327. doi: 10.1371/journal.pone.0000327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.de Vries BB, Pfundt R, Leisink M, et al. Diagnostic genome profiling in mental retardation. Am J Hum Genet. 2005;77(4):606–616. doi: 10.1086/491719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.del Gaudio D, Fang P, Scaglia F, et al. Increased MECP2 gene copy number as the result of genomic duplication in neurodevelopmentally delayed males. Genet Med. 2006;8(12):784–792. doi: 10.1097/01.gim.0000250502.28516.3c. [DOI] [PubMed] [Google Scholar]
- 73.Ballif BC, Theisen A, Coppinger J, et al. Expanding the clinical phenotype of the 3q29 microdeletion syndrome and characterization of the reciprocal microduplication. Mol Cytogenet. 2008;1(1):8. doi: 10.1186/1755-8166-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kriek M, White SJ, Szuhai K, et al. Copy number variation in regions flanked (or unflanked) by duplicons among patients with developmental delay and/or congenital malformations; detection of reciprocal and partial Williams-Beuren duplications. Eur J Hum Genet. 2006;14(2):180–189. doi: 10.1038/sj.ejhg.5201540. [DOI] [PubMed] [Google Scholar]
- 75.Barber JC, Maloney VK, Huang S, et al. 8p23.1 duplication syndrome; a novel genomic condition with unexpected complexity revealed by array CGH. Eur J Hum Genet. 2008;16(1):18–27. doi: 10.1038/sj.ejhg.5201932. [DOI] [PubMed] [Google Scholar]
- 76.Girirajan S, Rosenfeld JA, Cooper GM, et al. A recurrent 16p12.1 microdeletion supports a two-hit model for severe developmental delay. Nat Genet. 2010;42(3):203–209. doi: 10.1038/ng.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Francke U, Ochs HD, de Martinville B, et al. Minor Xp21 chromosome deletion in a male associated with expression of Duchenne muscular dystrophy, chronic granulomatous disease, retinitis pigmentosa, and McLeod syndrome. Am J Hum Genet. 1985;37(2):250–267. [PMC free article] [PubMed] [Google Scholar]
- 78.Lindgren V, de Martinville B, Horwich AL, Rosenberg LE, Francke U. Human ornithine transcarbamylase locus mapped to band Xp21.1 near the Duchenne muscular dystrophy locus. Science. 1984;226(4675):698–700. doi: 10.1126/science.6494904. [DOI] [PubMed] [Google Scholar]
- 79.Monaco AP, Neve RL, Colletti-Feener C, Bertelson CJ, Kurnit DM, Kunkel LM. Isolation of candidate cDNAs for portions of the Duchenne muscular dystrophy gene. Nature. 1986;323(6089):646–650. doi: 10.1038/323646a0. [DOI] [PubMed] [Google Scholar]
- 80.Royer-Pokora B, Kunkel LM, Monaco AP, et al. Cloning the gene for an inherited human disorder – chronic granulomatous disease – on the basis of its chromosomal location. Nature. 1986;322(6074):32–38. doi: 10.1038/322032a0. [DOI] [PubMed] [Google Scholar]
- 81.Sargent CA, Affara NA, Bentley E, et al. Cloning of the X-linked glycerol kinase deficiency gene and its identification by sequence comparison to the Bacillus subtilis homologue. Hum Mol Genet. 1993;2(2):97–106. doi: 10.1093/hmg/2.2.97. [DOI] [PubMed] [Google Scholar]
- 82.Buhler EM, Buhler UK, Stalder GR, Jani L, Jurik LP. Chromosome deletion and multiple cartilaginous exostoses. Eur J Pediatr. 1980;133(2):163–166. doi: 10.1007/BF00441586. [DOI] [PubMed] [Google Scholar]
- 83.Pfeiffer RA. Langer-Giedion syndrome and additional congenital malformations with interstitial deletion of the long arm of chromosome 8 46, XY, del 8 (q 13–22) Clin Genet. 1980;18(2):142–146. doi: 10.1111/j.1399-0004.1980.tb01025.x. [DOI] [PubMed] [Google Scholar]
- 84.Langer LO, Jr, Krassikoff N, Laxova R, et al. The tricho-rhino-phalangeal syndrome with exostoses (or Langer-Giedion syndrome): four additional patients without mental retardation and review of the literature. Am J Med Genet. 1984;19(1):81–112. doi: 10.1002/ajmg.1320190110. [DOI] [PubMed] [Google Scholar]
- 85.Bowen P, Biederman B, Hoo JJ. The critical segment for the Langer- Giedion syndrome: 8q24.11–8q24.12. Ann Genet. 1985;28(4):224–227. [PubMed] [Google Scholar]
- 86.Ludecke HJ, Johnson C, Wagner MJ, et al. Molecular definition of the shortest region of deletion overlap in the Langer-Giedion syndrome. Am J Hum Genet. 1991;49(6):1197–1206. [PMC free article] [PubMed] [Google Scholar]
- 87.Goldblatt J, Smart RD. Tricho-rhino-phalangeal syndrome without exostoses, wih an interstitial deletion of 8q23. Clin Genet. 1986;29(5):434–438. doi: 10.1111/j.1399-0004.1986.tb00517.x. [DOI] [PubMed] [Google Scholar]
- 88.Buhler EM, Buhler UK, Beutler C, Fessler R. A final word on the tricho-rhino-phalangeal syndromes. Clin Genet. 1987;31(4):273–275. doi: 10.1111/j.1399-0004.1987.tb02806.x. [DOI] [PubMed] [Google Scholar]
- 89.Ludecke HJ, Wagner MJ, Nardmann J, et al. Molecular dissection of a contiguous gene syndrome: localization of the genes involved in the Langer-Giedion syndrome. Hum Mol Genet. 1995;4(1):31–36. doi: 10.1093/hmg/4.1.31. [DOI] [PubMed] [Google Scholar]
- 90.Alliman S, Coppinger J, Marcadier J, et al. Clinical and molecular characterization of individuals with recurrent genomic disorder at 10q22.3q23.2. Clin Genet. 2010 doi: 10.1111/j.1399-0004.2010.01373.x. [DOI] [PubMed] [Google Scholar]
- 91.Balciuniene J, Feng N, Iyadurai K, et al. Recurrent 10q22–10q23 Deletions: A Genomic Disorder on 10q Associated with Cognitive and Behavioral Abnormalities. Am J Hum Genet. 2007;80(5):938–947. doi: 10.1086/513607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rosenfeld JA, Ballif BC, Lucas A, et al. Small deletions of SATB2 cause some of the clinical features of the 2q33.1 microdeletion syndrome. PLoS One. 2009;4(8):e6568. doi: 10.1371/journal.pone.0006568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Heilstedt HA, Ballif BC, Howard LA, et al. Physical map of 1p36, placement of breakpoints in monosomy 1p36, and clinical characterization of the syndrome. Am J Hum Genet. 2003;72(5):1200–1212. doi: 10.1086/375179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Heilstedt HA, Ballif BC, Howard LA, Kashork CD, Shaffer LG. Population data suggest that deletions of 1p36 are a relatively common chromosome abnormality. Clin Genet. 2003;64(4):310–316. doi: 10.1034/j.1399-0004.2003.00126.x. [DOI] [PubMed] [Google Scholar]
- 95.Yu W, Ballif BC, Kashork CD, et al. Development of a comparative genomic hybridization microarray and demonstration of its utility with 25 well-characterized 1p36 deletions. Hum Mol Genet. 2003;12(17):2145–2152. doi: 10.1093/hmg/ddg230. [DOI] [PubMed] [Google Scholar]
- 96.Klopocki E, Schulze H, Strauss G, et al. Complex inheritance pattern resembling autosomal recessive inheritance involving a microdeletion in thrombocytopenia-absent radius syndrome. Am J Hum Genet. 2007;80(2):232–240. doi: 10.1086/510919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Rare chromosomal deletions and duplications increase risk of schizophrenia. Nature. 2008;455(7210):237–241. doi: 10.1038/nature07239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Stefansson H, Rujescu D, Cichon S, et al. Large recurrent microdeletions associated with schizophrenia. Nature. 2008;455(7210):232–236. doi: 10.1038/nature07229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Brunetti-Pierri N, Berg JS, Scaglia F, et al. Recurrent reciprocal 1q21.1 deletions and duplications associated with microcephaly or macrocephaly and developmental and behavioral abnormalities. Nat Genet. 2008;40(12):1466–1471. doi: 10.1038/ng.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mefford HC, Sharp AJ, Baker C, et al. Recurrent rearrangements of chromosome 1q21.1 and variable pediatric phenotypes. N Engl J Med. 2008;359(16):1685–1699. doi: 10.1056/NEJMoa0805384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Willatt L, Cox J, Barber J, et al. 3q29 microdeletion syndrome: clinical and molecular characterization of a new syndrome. Am J Hum Genet. 2005;77(1):154–160. doi: 10.1086/431653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wang NJ, Liu D, Parokonny AS, Schanen NC. High-resolution molecular characterization of 15q11–15q13 rearrangements by array comparative genomic hybridization (array CGH) with detection of gene dosage. Am J Hum Genet. 2004;75(2):267–281. doi: 10.1086/422854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cook EH, Jr, Lindgren V, Leventhal BL, et al. Autism or atypical autism in maternally but not paternally derived proximal 15q duplication. Am J Hum Genet. 1997;60(4):928–934. [PMC free article] [PubMed] [Google Scholar]
- 104.Sharp AJ, Mefford HC, Li K, et al. A recurrent 15q13.3 microdeletion syndrome associated with mental retardation and seizures. Nat Genet. 2008;40(3):322–328. doi: 10.1038/ng.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Miller DT, Shen Y, Weiss LA, et al. Microdeletion/duplication at 15q13.2q13.3 among individuals with features of autism and other neuropsychiatric disorders. J Med Genet. 2009;46(4):242–248. doi: 10.1136/jmg.2008.059907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Slavotinek AM. Novel microdeletion syndromes detected by chromosome microarrays. Hum Genet. 2008;124(1):1–17. doi: 10.1007/s00439-008-0513-9. [DOI] [PubMed] [Google Scholar]
- 107.Ballif BC, Theisen A, Rosenfeld JA, et al. Identification of a recurrent microdeletion at 17q23.1q23.2 flanked by segmental duplications associated with heart defects and limb abnormalities. Am J Hum Genet. 2010;86(3):454–461. doi: 10.1016/j.ajhg.2010.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ben-Shachar S, Ou Z, Shaw CA, et al. 22q11.2 distal deletion: a recurrent genomic disorder distinct from DiGeorge syndrome and velocardiofacial syndrome. Am J Hum Genet. 2008;82(1):214–221. doi: 10.1016/j.ajhg.2007.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rauch A, Zink S, Zweier C, et al. Systematic assessment of atypical deletions reveals genotype-phenotype correlation in 22q11.2. J Med Genet. 2005;42(11):871–876. doi: 10.1136/jmg.2004.030619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wentzel C, Fernstrom M, Ohrner Y, Anneren G, Thuresson AC. Clinical variability of the 22q11.2 duplication syndrome. Eur J Med Genet. 2008;51(6):501–510. doi: 10.1016/j.ejmg.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 111.Alberti A, Romano C, Falco M, et al. 1.5 Mb de novo 22q11.21 microduplication in a patient with cognitive deficits and dysmorphic facial features. Clin Genet. 2007;71(2):177–182. doi: 10.1111/j.1399-0004.2007.00750.x. [DOI] [PubMed] [Google Scholar]
- 112.Torres-Juan L, Rosell J, Morla M, et al. Mutations in TBX1 genocopy the 22q11.2 deletion and duplication syndromes: a new susceptibility factor for mental retardation. Eur J Hum Genet. 2007;15(6):658–663. doi: 10.1038/sj.ejhg.5201819. [DOI] [PubMed] [Google Scholar]
- 113.Anderlid BM, Schoumans J, Anneren G, et al. FISH-mapping of a 100-kb terminal 22q13 deletion. Hum Genet. 2002;110(5):439–443. doi: 10.1007/s00439-002-0713-7. [DOI] [PubMed] [Google Scholar]
- 114.Luciani JJ, de Mas P, Depetris D, et al. Telomeric 22q13 deletions resulting from rings, simple deletions, and translocations: cytogenetic, molecular, and clinical analyses of 32 new observations. J Med Genet. 2003;40(9):690–696. doi: 10.1136/jmg.40.9.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Okamoto N, Kubota T, Nakamura Y, et al. 22q13 Microduplication in two patients with common clinical manifestations: a recognizable syndrome? Am J Med Genet A. 2007;143A(23):2804–2809. doi: 10.1002/ajmg.a.31771. [DOI] [PubMed] [Google Scholar]
- 116.Guo W, Mason JS, Stone CG, Jr, et al. Diagnosis of X-linked adrenal hypoplasia congenita by mutation analysis of the DAX1 gene. JAMA. 1995;274(4):324–330. [PubMed] [Google Scholar]
- 117.Peter M, Viemann M, Partsch CJ, Sippell WG. Congenital adrenal hypoplasia: clinical spectrum, experience with hormonal diagnosis, and report on new point mutations of the DAX-1 gene. J Clin Endocrinol Metab. 1998;83(8):2666–2674. doi: 10.1210/jcem.83.8.5027. [DOI] [PubMed] [Google Scholar]
- 118.Krantz ID, Colliton RP, Genin A, et al. Spectrum and frequency of jagged1 (JAG1) mutations in Alagille syndrome patients and their families. Am J Hum Genet. 1998;62(6):1361–1369. doi: 10.1086/301875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Spinner NB, Colliton RP, Crosnier C, Krantz ID, Hadchouel M, Meunier-Rotival M. Jagged1 mutations in alagille syndrome. Hum Mutat. 2001;17(1):18–33. doi: 10.1002/1098-1004(2001)17:1<18::AID-HUMU3>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 120.Magenis RE, Brown MG, Lacy DA, Budden S, LaFranchi S. Is Angelman syndrome an alternate result of del(15)(q11q13)? Am J Med Genet. 1987;28(4):829–838. doi: 10.1002/ajmg.1320280407. [DOI] [PubMed] [Google Scholar]
- 121.Zackowski JL, Nicholls RD, Gray BA, et al. Cytogenetic and molecular analysis in Angelman syndrome. Am J Med Genet. 1993;46(1):7–11. doi: 10.1002/ajmg.1320460104. [DOI] [PubMed] [Google Scholar]
- 122.Henry I, Puech A, Riesewijk A, et al. Somatic mosaicism for partial paternal isodisomy in Wiedemann-Beckwith syndrome: a post-fertilization event. Eur J Hum Genet. 1993;1(1):19–29. doi: 10.1159/000472384. [DOI] [PubMed] [Google Scholar]
- 123.Li M, Squire JA, Weksberg R. Molecular genetics of Wiedemann- Beckwith syndrome. Am J Med Genet. 1998;79(4):253–259. [PubMed] [Google Scholar]
- 124.Slavotinek A, Gaunt L, Donnai D. Paternally inherited duplications of 11p15.5 and Beckwith-Wiedemann syndrome. J Med Genet. 1997;34(10):819–826. doi: 10.1136/jmg.34.10.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bartsch O, Rasi S, Hoffmann K, Blin N. FISH of supernumerary marker chromosomes (SMCs) identifies six diagnostically relevant intervals on chromosome 22q and a novel type of bisatellited SMC(22) Eur J Hum Genet. 2005;13(5):592–598. doi: 10.1038/sj.ejhg.5201378. [DOI] [PubMed] [Google Scholar]
- 126.Johnson A, Minoshima S, Asakawa S, et al. A 1.5-Mb contig within the cat eye syndrome critical region at human chromosome 22q11.2. Genomics. 1999;57(2):306–309. doi: 10.1006/geno.1999.5757. [DOI] [PubMed] [Google Scholar]
- 127.Rosias PR, Sijstermans JM, Theunissen PM, et al. Phenotypic variability of the cat eye syndrome. Case report and review of the literature. Genet Couns. 2001;12(3):273–282. [PubMed] [Google Scholar]
- 128.Inoue K, Dewar K, Katsanis N, et al. The 1.4-Mb CMT1A duplication/ HNPP deletion genomic region reveals unique genome architectural features and provides insights into the recent evolution of new genes. Genome Res. 2001;11(6):1018–1033. doi: 10.1101/gr.180401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Blair IP, Nash J, Gordon MJ, Nicholson GA. Prevalence and origin of de novo duplications in Charcot-Marie-Tooth disease type 1A: first report of a de novo duplication with a maternal origin. Am J Hum Genet. 1996;58(3):472–476. [PMC free article] [PubMed] [Google Scholar]
- 130.Vissers LE, van Ravenswaaij CM, Admiraal R, et al. Mutations in a new member of the chromodomain gene family cause CHARGE syndrome. Nat Genet. 2004;36(9):955–957. doi: 10.1038/ng1407. [DOI] [PubMed] [Google Scholar]
- 131.Church DM, Yang J, Bocian M, Shiang R, Wasmuth JJ. A high-resolution physical and transcript map of the Cri du chat region of human chromosome 5p. Genome Res. 1997;7(8):787–801. doi: 10.1101/gr.7.8.787. [DOI] [PubMed] [Google Scholar]
- 132.Mainardi PC, Perfumo C, Cali A, et al. Clinical and molecular characterisation of 80 patients with 5p deletion: genotype-phenotype correlation. J Med Genet. 2001;38(3):151–158. doi: 10.1136/jmg.38.3.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zhang X, Snijders A, Segraves R, et al. High-resolution mapping of genotype-phenotype relationships in cri du chat syndrome using array comparative genomic hybridization. Am J Hum Genet. 2005;76(2):312–326. doi: 10.1086/427762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mantripragada KK, Tapia-Paez I, Blennow E, Nilsson P, Wedell A, Dumanski JP. DNA copy-number analysis of the 22q11 deletion-syndrome region using array-CGH with genomic and PCR-based targets. Int J Mol Med. 2004;13(2):273–279. [PubMed] [Google Scholar]
- 135.Yagi H, Furutani Y, Hamada H, et al. Role of TBX1 in human del22q11.2 syndrome. Lancet. 2003;362(9393):1366–1373. doi: 10.1016/s0140-6736(03)14632-6. [DOI] [PubMed] [Google Scholar]
- 136.Berend SA, Spikes AS, Kashork CD, et al. Dual-probe fluorescence in situ hybridization assay for detecting deletions associated with VCFS/ DiGeorge syndrome I and DiGeorge syndrome II loci. Am J Med Genet. 2000;91(4):313–317. [PubMed] [Google Scholar]
- 137.van Esch H, Groenen P, Daw S, et al. Partial DiGeorge syndrome in two patients with a 10p rearrangement. Clin Genet. 1999;55(4):269–276. doi: 10.1034/j.1399-0004.1999.550410.x. [DOI] [PubMed] [Google Scholar]
- 138.del Gaudio D, Yang Y, Boggs BA, et al. Molecular diagnosis of Duchenne/Becker muscular dystrophy: enhanced detection of dystrophin gene rearrangements by oligonucleotide array-comparative genomic hybridization. Hum Mutat. 2008;29(9):1100–1107. doi: 10.1002/humu.20841. [DOI] [PubMed] [Google Scholar]
- 139.Bovolenta M, Neri M, Fini S, et al. A novel custom high density-comparative genomic hybridization array detects common rearrangements as well as deep intronic mutations in dystrophinopathies. BMC Genomics. 2008;9:572. doi: 10.1186/1471-2164-9-572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Srour M, Bejjani BA, Rorem EA, Hall N, Shaffer LG, Shevell MI. An instructive case of an 8-year-old boy with intellectual disability. Semin Pediatr Neurol. 2008;15(4):154–155. doi: 10.1016/j.spen.2008.09.002. discussion 155–156. [DOI] [PubMed] [Google Scholar]
- 141.Johnston JJ, Olivos-Glander I, Turner J, et al. Clinical and molecular delineation of the Greig cephalopolysyndactyly contiguous gene deletion syndrome and its distinction from acrocallosal syndrome. Am J Med Genet A. 2003;123A(3):236–242. doi: 10.1002/ajmg.a.20318. [DOI] [PubMed] [Google Scholar]
- 142.Sargent CA, Kidd A, Moore S, Dean J, Besley GT, Affara NA. Five cases of isolated glycerol kinase deficiency, including two families: failure to find genotype:phenotype correlation. J Med Genet. 2000;37(6):434–441. doi: 10.1136/jmg.37.6.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Lenssen PP, Gabreels-Festen AA, Valentijn LJ, et al. Hereditary neuropathy with liability to pressure palsies. Phenotypic differences between patients with the common deletion and a PMP22 frame shift mutation. Brain. 1998;121(Pt 8):1451–1458. doi: 10.1093/brain/121.8.1451. [DOI] [PubMed] [Google Scholar]
- 144.Lopes J, Tardieu S, Silander K, et al. Homologous DNA exchanges in humans can be explained by the yeast double-strand break repair model: a study of 17p11.2 rearrangements associated with CMT1A and HNPP. Hum Mol Genet. 1999;8(12):2285–2292. doi: 10.1093/hmg/8.12.2285. [DOI] [PubMed] [Google Scholar]
- 145.Le Guern E, Sturtz F, Gugenheim M, et al. Detection of deletion within 17p11.2 in 7 French families with hereditary neuropathy with liability to pressure palsies (HNPP) Cytogenet Cell Genet. 1994;65(4):261–264. doi: 10.1159/000133643. [DOI] [PubMed] [Google Scholar]
- 146.Ballabio A, Parenti G, Tippett P, et al. X-linked ichthyosis, due to steroid sulphatase deficiency, associated with Kallmann syndrome (hypogonadotropic hypogonadism and anosmia): linkage relationships with Xg and cloned DNA sequences from the distal short arm of the X chromosome. Hum Genet. 1986;72(3):237–240. doi: 10.1007/BF00291885. [DOI] [PubMed] [Google Scholar]
- 147.Hardelin JP, Levilliers J, Young J, et al. Xp22.3 deletions in isolated familial Kallmann’s syndrome. J Clin Endocrinol Metab. 1993;76(4):827–831. doi: 10.1210/jcem.76.4.8473391. [DOI] [PubMed] [Google Scholar]
- 148.Sato N, Katsumata N, Kagami M, et al. Clinical assessment and mutation analysis of Kallmann syndrome 1 (KAL1) and fibroblast growth factor receptor 1 (FGFR1, or KAL2) in five families and 18 sporadic patients. J Clin Endocrinol Metab. 2004;89(3):1079–1088. doi: 10.1210/jc.2003-030476. [DOI] [PubMed] [Google Scholar]
- 149.Ahn J, Ludecke HJ, Lindow S, et al. Cloning of the putative tumour suppressor gene for hereditary multiple exostoses (EXT1) Nat Genet. 1995;11(2):137–143. doi: 10.1038/ng1095-137. [DOI] [PubMed] [Google Scholar]
- 150.Nardmann J, Tranebjaerg L, Horsthemke B, Ludecke HJ. The tricho-rhino-phalangeal syndromes: frequency and parental origin of 8q deletions. Hum Genet. 1997;99(5):638–643. doi: 10.1007/s004390050420. [DOI] [PubMed] [Google Scholar]
- 151.Kayserili H, Cox TC, Cox LL, et al. Molecular characterisation of a new case of microphthalmia with linear skin defects (MLS) J Med Genet. 2001;38(6):411–417. doi: 10.1136/jmg.38.6.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Prakash SK, Cormier TA, McCall AE, et al. Loss of holocytochrome c-type synthetase causes the male lethality of X-linked dominant microphthalmia with linear skin defects (MLS) syndrome. Hum Mol Genet. 2002;11(25):3237–3248. doi: 10.1093/hmg/11.25.3237. [DOI] [PubMed] [Google Scholar]
- 153.Zvulunov A, Kachko L, Manor E, Shinwell E, Carmi R. Reticulolinear aplasia cutis congenita of the face and neck: a distinctive cutaneous manifestation in several syndromes linked to Xp22. Br J Dermatol. 1998;138(6):1046–1052. doi: 10.1046/j.1365-2133.1998.02277.x. [DOI] [PubMed] [Google Scholar]
- 154.Dobyns WB, Curry CJ, Hoyme HE, Turlington L, Ledbetter DH. Clinical and molecular diagnosis of Miller-Dieker syndrome. Am J Hum Genet. 1991;48(3):584–594. [PMC free article] [PubMed] [Google Scholar]
- 155.Ledbetter SA, Kuwano A, Dobyns WB, Ledbetter DH. Microdeletions of chromosome 17p13 as a cause of isolated lissencephaly. Am J Hum Genet. 1992;50(1):182–189. [PMC free article] [PubMed] [Google Scholar]
- 156.Cnossen MH, van der Est MN, Breuning MH, et al. Deletions spanning the neurofibromatosis type 1 gene: implications for genotype-phenotype correlations in neurofibromatosis type 1? Hum Mutat. 1997;9(5):458–464. doi: 10.1002/(SICI)1098-1004(1997)9:5<458::AID-HUMU13>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 157.Upadhyaya M, Ruggieri M, Maynard J, et al. Gross deletions of the neurofibromatosis type 1 (NF1) gene are predominantly of maternal origin and commonly associated with a learning disability, dysmorphic features and developmental delay. Hum Genet. 1998;102(5):591–597. doi: 10.1007/s004390050746. [DOI] [PubMed] [Google Scholar]
- 158.Inoue K, Osaka H, Imaizumi K, et al. Proteolipid protein gene duplications causing Pelizaeus-Merzbacher disease: molecular mechanism and phenotypic manifestations. Ann Neurol. 1999;45(5):624–632. [PubMed] [Google Scholar]
- 159.Woodward K, Kendall E, Vetrie D, Malcolm S. Pelizaeus-Merzbacher disease: identification of Xq22 proteolipid-protein duplications and characterization of breakpoints by interphase FISH. Am J Hum Genet. 1998;63(1):207–217. doi: 10.1086/301933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Wakui K, Gregato G, Ballif BC, et al. Construction of a natural panel of 11p11.2 deletions and further delineation of the critical region involved in Potocki-Shaffer syndrome. Eur J Hum Genet. 2005;13(5):528–540. doi: 10.1038/sj.ejhg.5201366. [DOI] [PubMed] [Google Scholar]
- 161.Potocki L, Shaffer LG. Interstitial deletion of 11(p11.2p12): a newly described contiguous gene deletion syndrome involving the gene for hereditary multiple exostoses (EXT2) Am J Med Genet. 1996;62(3):319–325. doi: 10.1002/(SICI)1096-8628(19960329)62:3<319::AID-AJMG22>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 162.Magenis RE, Toth-Fejel S, Allen LJ, et al. Comparison of the 15q deletions in Prader-Willi and Angelman syndromes: specific regions, extent of deletions, parental origin, and clinical consequences. Am J Med Genet. 1990;35(3):333–349. doi: 10.1002/ajmg.1320350307. [DOI] [PubMed] [Google Scholar]
- 163.Kuwano A, Mutirangura A, Dittrich B, et al. Molecular dissection of the Prader-Willi/Angelman syndrome region (15q11–13) by YAC cloning and FISH analysis. Hum Mol Genet. 1992;1(6):417–425. doi: 10.1093/hmg/1.6.417. [DOI] [PubMed] [Google Scholar]
- 164.Cowell JK, Hungerford J, Rutland P, Jay M. Genetic and cytogenetic analysis of patients showing reduced esterase-D levels and mental retardation from a survey of 500 individuals with retinoblastoma. Ophthalmic Paediatr Genet. 1989;10(2):117–127. doi: 10.3109/13816818909088352. [DOI] [PubMed] [Google Scholar]
- 165.Richter S, Vandezande K, Chen N, et al. Sensitive and efficient detection of RB1 gene mutations enhances care for families with retinoblastoma. Am J Hum Genet. 2003;72(2):253–269. doi: 10.1086/345651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Petrij F, Dauwerse HG, Blough RI, et al. Diagnostic analysis of the Rubinstein-Taybi syndrome: five cosmids should be used for microdeletion detection and low number of protein truncating mutations. J Med Genet. 2000;37(3):168–176. doi: 10.1136/jmg.37.3.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Taine L, Goizet C, Wen ZQ, et al. Submicroscopic deletion of chromosome 16p13.3 in patients with Rubinstein-Taybi syndrome. Am J Med Genet. 1998;78(3):267–270. [PubMed] [Google Scholar]
- 168.Seranski P, Heiss NS, Dhorne-Pollet S, et al. Transcription mapping in a medulloblastoma breakpoint interval and Smith-Magenis syndrome candidate region: identification of 53 transcriptional units and new candidate genes. Genomics. 1999;56(1):1–11. doi: 10.1006/geno.1998.5647. [DOI] [PubMed] [Google Scholar]
- 169.Greenberg F, Guzzetta V, Montes de Oca-Luna R, et al. Molecular analysis of the Smith-Magenis syndrome: a possible contiguous-gene syndrome associated with del(17)(p11.2) Am J Hum Genet. 1991;49(6):1207–1218. [PMC free article] [PubMed] [Google Scholar]
- 170.Slager RE, Newton TL, Vlangos CN, Finucane B, Elsea SH. Mutations in RAI1 associated with Smith-Magenis syndrome. Nat Genet. 2003;33(4):466–468. doi: 10.1038/ng1126. [DOI] [PubMed] [Google Scholar]
- 171.Vlangos CN, Yim DK, Elsea SH. Refinement of the Smith-Magenis syndrome critical region to approximately 950kb and assessment of 17p11.2 deletions. Are all deletions created equally? Mol Genet Metab. 2003;79(2):134–141. doi: 10.1016/s1096-7192(03)00048-9. [DOI] [PubMed] [Google Scholar]
- 172.Waggoner DJ, Raca G, Welch K, et al. NSD1 analysis for Sotos syndrome: insights and perspectives from the clinical laboratory. Genet Med. 2005;7(8):524–533. doi: 10.1097/01.GIM.0000178503.15559.d3. [DOI] [PubMed] [Google Scholar]
- 173.Tatton-Brown K, Douglas J, Coleman K, et al. Multiple mechanisms are implicated in the generation of 5q35 microdeletions in Sotos syndrome. J Med Genet. 2005;42(4):307–313. doi: 10.1136/jmg.2004.027755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Turkmen S, Gillessen-Kaesbach G, Meinecke P, et al. Mutations in NSD1 are responsible for Sotos syndrome, but are not a frequent finding in other overgrowth phenotypes. Eur J Hum Genet. 2003;11(11):858–865. doi: 10.1038/sj.ejhg.5201050. [DOI] [PubMed] [Google Scholar]
- 175.Ballabio A, Carrozzo R, Parenti G, et al. Molecular heterogeneity of steroid sulfatase deficiency: a multicenter study on 57 unrelated patients, at DNA and protein levels. Genomics. 1989;4(1):36–40. doi: 10.1016/0888-7543(89)90311-x. [DOI] [PubMed] [Google Scholar]
- 176.Conary JT, Lorkowski G, Schmidt B, et al. Genetic heterogeneity of steroid sulfatase deficiency revealed with cDNA for human steroid sulfatase. Biochem Biophys Res Commun. 1987;144(2):1010–1017. doi: 10.1016/s0006-291x(87)80064-5. [DOI] [PubMed] [Google Scholar]
- 177.Kashork CD, Sutton VR, Fonda Allen JS, et al. Low or absent unconjugated estriol in pregnancy: an indicator for steroid sulfatase deficiency detectable by fluorescence in situ hybridization and biochemical analysis. Prenat Diagn. 2002;22(11):1028–1032. doi: 10.1002/pd.466. [DOI] [PubMed] [Google Scholar]
- 178.Shapiro LJ, Yen P, Pomerantz D, Martin E, Rolewic L, Mohandas T. Molecular studies of deletions at the human steroid sulfatase locus. Proc Natl Acad Sci U S A. 1989;86(21):8477–8481. doi: 10.1073/pnas.86.21.8477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Momeni P, Glockner G, Schmidt O, et al. Mutations in a new gene, encoding a zinc-finger protein, cause tricho-rhino-phalangeal syndrome type I. Nat Genet. 2000;24(1):71–74. doi: 10.1038/71717. [DOI] [PubMed] [Google Scholar]
- 180.Ludecke HJ, Schaper J, Meinecke P, et al. Genotypic and phenotypic spectrum in tricho-rhino-phalangeal syndrome types I and III. Am J Hum Genet. 2001;68(1):81–91. doi: 10.1086/316926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Crolla JA, van Heyningen V. Frequent chromosome aberrations revealed by molecular cytogenetic studies in patients with aniridia. Am J Hum Genet. 2002;71(5):1138–1149. doi: 10.1086/344396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Lowery MC, Morris CA, Ewart A, et al. Strong correlation of elastin deletions, detected by FISH, with Williams syndrome: evaluation of 235 patients. Am J Hum Genet. 1995;57(1):49–53. [PMC free article] [PubMed] [Google Scholar]
- 183.Royer-Pokora B, Beier M, Henzler M, et al. Twenty-four new cases of WT1 germline mutations and review of the literature: genotype/ phenotype correlations for Wilms tumor development. Am J Med Genet A. 2004;127A(3):249–257. doi: 10.1002/ajmg.a.30015. [DOI] [PubMed] [Google Scholar]
- 184.van Buggenhout G, Melotte C, Dutta B, et al. Mild Wolf-Hirschhorn syndrome: micro-array CGH analysis of atypical 4p16.3 deletions enables refinement of the genotype-phenotype map. J Med Genet. 2004;41(9):691–698. doi: 10.1136/jmg.2003.016865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Altherr MR, Wright TJ, Denison K, Perez-Castro AV, Johnson VP. Delimiting the Wolf-Hirschhorn syndrome critical region to 750 kilobase pairs. Am J Med Genet. 1997;71(1):47–53. doi: 10.1002/(sici)1096-8628(19970711)71:1<47::aid-ajmg9>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 186.Battaglia A, Carey JC, Wright TJ. Wolf-Hirschhorn (4p-) syndrome. Adv Pediatr. 2001;48:75–113. [PubMed] [Google Scholar]
- 187.Ferrero GB, Gebbia M, Pilia G, et al. A submicroscopic deletion in Xq26 associated with familial situs ambiguus. Am J Hum Genet. 1997;61(2):395–401. doi: 10.1086/514857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Ware SM, Peng J, Zhu L, et al. Identification and functional analysis of ZIC3 mutations in heterotaxy and related congenital heart defects. Am J Hum Genet. 2004;74(1):93–105. doi: 10.1086/380998. [DOI] [PMC free article] [PubMed] [Google Scholar]