Abstract
Objectives
To examine the effects of changes in payment and risk adjustment on (1) the annual enrollment and switching behavior of Medicare Advantage (MA) beneficiaries, and (2) the relative costliness of MA enrollees and disenrollees.
Data
From 1999 through 2008 national Medicare claims data from the 5 percent longitudinal sample of Parts A and B expenditures.
Study Design
Retrospective, fixed effects regression analysis of July enrollment and year-long switching into and out of MA. Similar regression analysis of the costliness of those switching into (out of) MA in the 6 months prior to enrollment (after disenrollment) relative to nonswitchers in the same county over the same period.
Findings
Payment generosity and more sophisticated risk adjustment were associated with substantial increases in MA enrollment and decreases in disenrollment. Claims experience of those newly switching into MA was not affected by any of the policy reforms, but disenrollment became increasingly concentrated among high-cost beneficiaries.
Conclusions
Enrollment is very sensitive to payment levels. The use of more sophisticated risk adjustment did not alter favorable selection into MA, but it did affect the costliness of disenrollees.
Keywords: Medicare advantage, payment, risk adjustment, hierarchical condition categories
Medicare began paying managed care plans on a capitated basis in 1985 using the Adjusted Average Per Capita Cost (AAPCC) methodology (Zarabozo 2000). The AAPCC paid managed care plans 95 percent of the county per capita Medicare expenditure, adjusted for the age, gender, and institutional and welfare status of the enrolled beneficiaries. This risk-adjustment methodology provided strong incentives for favorable selection. Newhouse and colleagues (1989) demonstrated that ex ante health status measures, including prior utilization, could be used in conjunction with the AAPCC model to better predict the future expenditures of beneficiaries. Moreover, they suggested that by incorporating more detailed health status measures, the Medicare payment system could dramatically reduce the extent of favorable selection. However, work by Brown and colleagues (2011) argues that plans respond to more extensive risk-adjustment mechanisms by reducing their efforts to select beneficiaries along the characteristics included in the model and increasing their selection efforts along other dimensions.
The Centers for Medicare and Medicaid Services (CMS) developed the Hierarchical Condition Categories (HCCs) approach in response to the Balanced Budget Act (BBA) and phased it in from 2003 to 2007. Although this change is thought to have reduced favorable selection in the Medicare Advantage (MA) program, as Newhouse (2010) notes, there has been no empirical investigation of this issue.
As part of the 1997 BBA reforms and the subsequent Medicare Modernization Act, Congress made a number of changes in the payment levels that apply to MA plans. In the early years, these changes appear to have led to a substantial exit of MA plans from markets (Medicare Payment Advisory Commission [MedPAC] 2002). The erosion was most pronounced among small plans and plans in low-population areas (Glavin et al. 2002/2003). In larger markets, the vast majority of MA participants appear to have joined other MA plans (Schoenman et al. 2005). Later changes sought to stem the losses. Rural counties, for example, were given a higher minimum payment threshold to encourage MA enrollment. Catchment areas larger than a county were established for regional Medicare preferred provider organizations. MA plans were also required to bid on a standard set of covered services. If the bid was below a CMS established benchmark, CMS would retain 25 percent of the difference, and the plan was required to provide enhanced services, reductions in cost sharing, or both to beneficiaries with the remaining 75 percent. These changes in payment policy enhanced the attractiveness of the program (MedPAC 2009).
This study investigates the effects of these reforms on enrollment and favorable selection in the MA program. We do this in a two-phase analysis. First, we estimate the effects of the shift to HCCs and the changes in county-specific payment levels on overall Medicare managed care enrollment over the 1999 through 2008 period. As part of this analysis, we explicitly analyze the effects on both entry into and exit from MA plans.
Second, we follow the literature (Physician Payment Review Commission [PPRC] 1996) in using the 6 months prior claims experience of those who switch into a MA plan, relative to those who stay in traditional Medicare, to estimate the extent to which the CMS-HCCs reduced favorable selection over the 10-year period. Analogously, we use the 6 months post-switch claims experience of those who leave a MA plan relative to those who remained in traditional Medicare to assess the extent to which the CMS-HCCs reduced favorable selection through disenrollment.
We find that higher baseline payments to MA plans were associated with large increases in enrollment and reductions in disenrollment. Overall, a 10 percent increase in payment levels increased enrollment by 9.6 percent. The phase-in of the HCCs also led to increased enrollment in MA plans and reduced disenrollment. We find no statistically significant evidence that new enrollment was less subject to favorable selection. Disenrollment, however, was disproportionately concentrated among the highest cost beneficiaries.
Background
There has been substantial research exploring the extent to which managed care plans, particularly health maintenance organizations (HMOs), attract healthier beneficiaries. Reviews by Luft (1981) and Miller and Luft (1994) firmly established the consensus that HMOs have benefited from favorable selection.
Research on favorable selection in Medicare is challenging because claims data are not available for enrollees in MA plans. See Mello et al. (2003) for a careful review of the Medicare HMO favorable selection literature. The Prospective Payment Review Commission (PPRC 1996) examined favorable selection in the Medicare program from 1989 to 1994 by comparing the claims experience of beneficiaries in the 6-month period before they joined a Medicare HMO and after they left such a plan relative to those who never left. It found that those switching in had claims experience that was only 63 percent as large of those who would remain in the traditional program, and those switching out had claims experience that was 160 percent of beneficiaries in traditional Medicare. Batata (2004) used county-level Medicare enrollment and expenditure data for the period 1990 through 1994. She found that a 1 percent increase in county Medicare HMO enrollment was associated with a $1,033 increase in the average claims experience of those in traditional Medicare.
In the 1990s, CMS undertook development work on alternative MA payment systems that incorporated more sophisticated measures of health status, ultimately adopting the HCCs approach. Compared with a simple age/sex risk adjuster, Pope et al. (2004) found that the HCC model predicted future claims better for each quintile of the claims payment distribution. The HCC reduced the overpayment predicted for the least costly quintile of beneficiaries from 166 percent to only 23 percent, for example, and paid the fifth quintile of beneficiaries at 14 percent under the expenditures that would have been incurred through traditional Medicare compared with the 56 percent underpayment implied by the age/sex model.
The Medicare Modernization Act modified the basic HCC model. Beginning in 2006, MA providers had to “bid” a payment rate for their covered services in each county or other (larger) market area. If the proposed rate was above the “benchmark rate” established by CMS, the plan would receive the benchmark rate. If it was below, CMS would recoup 25 percent of the difference with the plan required to use the other 75 percent to enhance benefits and/or to reduce beneficiary cost sharing. The MedPAC (2006) reported that 95 percent of the bids were below the benchmark in 2006. Once the base payment was established through this bid process, the HCC risk-adjustment mechanism was employed as it had been.
Although much of the recent growth in MA is found in private fee-for-service (PFFS) plans, this does not affect the analysis. These plans need not establish a network of providers. A beneficiary may receive care from any provider willing to accept payment from the PFFS and in the absence of a provider agreement between the PFFS plan and the provider, the provider must be paid at least as much as would be paid by traditional Medicare (Blum, Brown, and Frieder 2007). Thus, PFFS plans have limited ability to control price or utilization through selective contracting or utilization management. They face at least as much risk from an unhealthy draw of enrollees as would a more conventional managed care plan.
Congress established two significant program changes effective in 2006. First, the Medicare Part D prescription drug program began. Under this program, Medicare beneficiaries could purchase subsidized stand-alone drug coverage in addition to Medicare Parts A and B. Part D coverage had ambiguous effects on MA plans. On the one hand, the introduction of Part D increased the available substitutes for MA plans and would likely lead to reduced enrollment in MA plans. On the other hand, the expansion of coverage led seniors to consider all of their prescription drug options and in the process many may have newly considered the MA option.
Second, Congress also mandated that enrollment in MA plans would be limited to an annual open-enrollment period. Before that, Medicare beneficiaries could switch from one MA plan to another—or to traditional Medicare—at any time. From the beneficiary's perspective, this 12-month “lock-in” made it riskier to enroll in a MA plan. This should lead risk-averse individuals to reduce enrollment, ceteris paribus. However, this change also gave plans a greater incentive to attract persistently low utilizers and to exclude/drop potentially high utilizers, to the extent that either of these groups could be identified. Given the simultaneity of the introduction of Part D and the lock-in, we are only able to examine their joint effect.
Data and Methods
Data for this project were drawn largely from the 1999 through 2008 5 percent sample of Medicare enrollees (Buccaneer et al. 2011). This source provides demographic characteristics and comprehensive longitudinal administrative Part A and B claims data on a random sample of Medicare beneficiaries. These data were augmented with annual county-specific CMS payment rates (CMS 2010a,b) and information on the phase-in of the HCCs, and introduction of the open enrollment period obtained from the CMS website (CMS 2005).
The analysis is limited to those persons aged 65 and older and residing in the 50 states and the District of Columbia. The analysis is further limited to those beneficiaries, whether in traditional Medicare or in MA, who have both Parts A and B coverage.
Enrollment and Switching Analysis
First, we examine the effects of changes in base payment levels and the recent policy changes on annual MA enrollment, and the number of individuals switching into and out of MA plans—all defined at the county level. We calculate annual enrollment using MA enrollment status in July of each year of our 1999–2008 study period and switchers-in and -out by aggregating monthly switchers for each year. The data do not allow us to examine switching from one MA plan to another.
We estimate variants of the following equation:
| (1) |
where S is, alternatively, the number of MA enrollees in the county in the year, the number of beneficiaries in the county-year switching into a MA plan, or the number of beneficiaries in the county-year switching out of MA. We also estimate these models separately for each quartile of counties by Medicare population.
“Pay” is the baseline payment rate (in 1999–2005) or the benchmark payment rate (2006–2008) paid to MA plans in the county in each year adjusted to constant 2008 dollars (using the Consumer Price Index, All-Items). We hypothesize that a higher base or benchmark payment will lead to higher enrollment, greater switching-in, and less switching-out. Although beneficiaries are largely unaware of these payment rates, plans are expected to adjust premiums, copays, covered services, and other characteristics of the plan that are relevant to potential enrollees.
“HCC” is a variable reflecting the phase-in of the HCCs methodology. It takes the value “0” in years 1999–2002, “.10” in 2003, “.30” in 2004, “.50” in 2005, “.75” in 2006, and 1 in years 2007 and 2008. These values reflect the proportion of the payment rate that was computed using the HCC methodology. We hypothesize that the phasing-in of the HCC will lead to greater enrollment, more switching-in, and less switching-out. To the extent that the risk adjustment better reflects ex ante risk, plans face lower risk of enrolling any beneficiary and the profitability of any enrollee, while potentially reduced, is expected to still be positive.
“PartD&Lock” is a dichotomous variable equal to 1 in the years (2006–2008) in which Medicare beneficiaries could enroll in stand-alone Part D prescription drug coverage and could only change MA plans during designated annual open enrollment periods, “0” otherwise. Although these policy changes are expected to affect enrollment, the direction of this effect is theoretically ambiguous. “Time” is a linear time trend taking values 1 in 1999 through 10 in 2008. “MPop” is the number of Medicare beneficiaries residing in the county in each year.
The models also include a set of county-fixed effects and are estimated using ordinary least squares with robust standard errors. We also experimented with a count model which yielded results qualitatively similar to the OLS-fixed effects specification. Because these equations are estimated using a 5 percent sample of enrollees, the number of MA enrollees, switchers, and the Medicare population is multiplied by 20 to yield national estimates of the raw estimated effects. We estimate the regressions on each quartile of counties out of concern that the results may differ by county size and that our standard errors may be inflated due to random missing data that would be more problematic in the less populated counties.
Favorable/Adverse Selection Analysis
We use similar models to examine the effect of CMS reforms on favorable or adverse selection into and out of MA. We hypothesize that higher payment levels will lead to less favorable selection; the advent of the HCC program should lead to less favorable selection; and the lock-in & Part D expansion have ambiguous effects. Here, the dependent variable is the ratio of total Medicare expenditures of those who switched relative to those who did not. We construct these variables by identifying all beneficiaries who switch from traditional Medicare to MA in a given county-month-year. We then compute the average claims in the 6 months prior to switching into MA of all those switching in and divide this by the average claims experience of those in the same county-month-year who remained in traditional Medicare. Analogously, we compute the ratio of claims experience in the 6 months following disenrollment from MA relative to those who had remained in traditional Medicare. This allows us to examine the ratio of local claims experience of those switching in from July 1999 through December 2008. For those switching out, we examine the period February 1999 through July 2008.
There are county-months in which only a very few beneficiaries are observed as switchers due either to low MA penetration and/or small numbers resulting from the 5 percent sample. To address this, we estimate weighted regressions, using the total number of MA enrollees in the county as weights.
Results
Enrollment and Switching Analysis
The average county in our analysis, over the entire 10 years of the study, had 97.5 MA enrollees in the 5-percent sample. This implies average county enrollment of 1,950 age 65 plus MA enrollees overall. In the average county, 226.8 people joined MA annually and 149 disenrolled. The average monthly payment in constant 2008 dollars was $656. See Table 1.
Table 1.
Annual July Total Enrollment in Medicare Advantage Total and by County Medicare Population Quartiles, 1999–2008
| Mean | Total | I | II | III | IV | |
|---|---|---|---|---|---|---|
| Base payment | $655.76 ($94.12) | 2.85*** (0.64) | −0.10*** (0.03) | −0.19*** (0.071) | −0.40** (0.20) | 9.47*** (2.38) |
| HCC | 0.37 (0.40) | 998.48*** (76.75) | 60.07*** (4.53) | 186.72*** (11.50) | 499.95*** (26.87) | 3,469.19***(298.94) |
| Part D and lock-in | 0.30 (0.46) | 442.26*** (28.87) | 34.60*** (2.10) | 98.07*** (4.85) | 219.04*** (10.90) | 1,453.76***(111.04) |
| Medicare pop | 10,340 (27,618) | 0.40*** (0.12) | 0.07*** (0.01) | 0.10*** (0.02) | 0.15*** (0.03) | 0.38***(0.12) |
| Time trend | 5.5 (2.9) | −217.60*** (23.81) | −0.64 (0.82) | −6.37*** (2.43) | −24.74*** (6.04) | −804.96***(85.21) |
| Constant | −3,327.96*** (1,399.95) | 10.59 (19.72) | −64.59 (75.81) | −248.99 (175.45) | −9,061.85*(4,870.70) | |
| County-fixed effects | Yes | Yes | Yes | Yes | Yes | |
| Adj. R2 | 0.983 | 0.650 | 0.764 | 0.838 | 0.981 | |
| N | 30,390 | 30,390 | 7,556 | 7,799 | 7,779 | 7,256 |
Mean of annual enrollment = 1,950.0 (10,034.8).
*, **, *** indicate statistical significance at the 90, 95, and 99 percent confidence intervals, respectively.
Standard deviations (column 1) and standard errors are in parentheses.
Table 1 also reports the regression results of the July enrollment analysis. The second column shows the overall estimates and the remaining four contain estimates for each quartile of counties, from those with the fewest Medicare beneficiaries to the most. We find that county-level MA enrollment is highly sensitive to the base payment level. Evaluated at the means, a 10 percent increase in monthly payment levels was associated with a 9.6 percent increase in annual enrollment. This effect is driven entirely by the largest Medicare counties as the coefficients are negative and near zero for the three smallest quartiles of counties.
The annual enrollment effect was achieved both by more beneficiaries switching into MA plans and fewer switching out. These results are shown in Table 2. Our estimates, evaluated at the means, imply that a 10 percent increase in base payment increased switching in by 15.3 percent and decreased switching out by 29.9 percent. Appendix Tables 1 and 2 demonstrate that, again, both of these effects result from disproportionate effects in the largest counties.
Table 2.
Regression Results of the Year-Long Number of Beneficiaries Switching In and Switching Out of Medicare Advantage Plans, 1999–2008
| Switchers-In | Switchers-Out | |
|---|---|---|
| Base payment | 0.53*** (0.11) | −0.68*** (0.17) |
| HCC | 304.60*** (25.75) | −448.26*** (54.41) |
| Part D and lock-in | 152.26*** (10.01) | 183.00*** (16.43) |
| Medicare pop | 0.04* (0.02) | 0.01 (0.02) |
| Time trend | −34.72*** (3.77) | 38.82*** (6.07) |
| Constant | −517.39** (246.55) | 363.44 (232.52) |
| County-fixed effects | Yes | Yes |
| Adj. R2 | 0.751 | 0.472 |
| N | 30,390 | 30,390 |
Means (standard deviations) of the dependent variables: Switchers-In = 226.8 (828.7), Switchers-Out = 149.1 (743.7).
*, **, *** indicate statistical significance at the 90, 95, and 99 percent confidence intervals, respectively.
Standard errors are in parentheses.
The implementation of HCCs resulted in increased MA enrollment (Table 1) and did so by both increasing the number of new enrollees and decreasing the number of disenrollees (Table 2). This is consistent with the view that the more sophisticated payment system encouraged plans to recruit more enrollees and retain existing enrollees. These effects are consistent across counties with differing numbers of Medicare beneficiaries, but much larger for the largest Medicare counties (Appendix Tables).
Requiring Medicare beneficiaries to remain in their chosen plan for a year (locked-in) and opening access to stand-alone Part D drug plans had the net effect of increasing total enrollment by 442 beneficiaries in the average county-year. Our results show that these policy changes were not only associated with increases in the number of beneficiaries switching into MA plans but also with increases in those switching out. Both of these effects were larger in larger markets.
The direct effect of market size on enrollment was positive. It was also larger with respect to switching into MA plans, but there was no meaningful effect of market size on the number of beneficiaries switching out. However, it is clear that the size of the Medicare population in the county was important not due to the effects of size per se, but rather due to the differing effects that the policy variables have in markets of differing sizes.
Finally, the time trend variable yields a negative coefficient estimate suggesting that, other things equal, beneficiaries were choosing MA plans less frequently over time. This was reflected in both fewer people switching in and more people switching out over time. This finding is consistent with the “managed care backlash” reported for managed care plans generally, over the period of our study.
Favorable/Adverse Selection Analysis
Figure 1 shows the 10-year trends in the relative costliness of those who switched into and out of an MA plan relative to those who remained in traditional FFS Medicare. In 1999, the average 6 months prior claims expenditures of those who switched into MA was only 79 percent of that of individuals in the same county in traditional Medicare who did not switch. By 2008, it was 91 percent. For those switching out of MA and returning to traditional Medicare, their claims expenditures in the 6 months after returning was 137 percent of those in the same county who remained in traditional Medicare throughout. By 2008, the relative costliness of those switching out had risen to 151 percent of nonswitchers.
Figure 1.
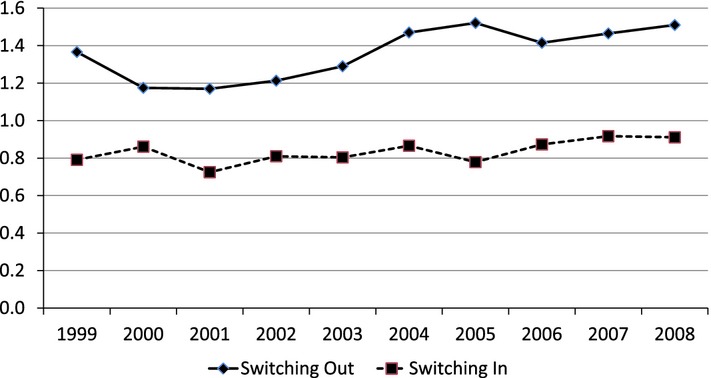
Costliness of Those Switching In and Switching Out of Medicare Advantage Relative to Nonswitchers, 1999–2008
Table 3 reports the weighted regression results for the relative expenditure ratios among switchers into and out of MA plans. The switching-in prior expenditures models reveal no statistically significant effects of the Medicare policy variables. Moreover, the coefficient estimates are generally near zero. The lone exception in the weighted regression is the coefficient on the HCC phase-in. It suggests that the fully phased-in risk-adjustment model resulted in the enrollment of beneficiaries who had prior claims experience 20 percent higher than before implementation. However, we cannot reject the hypothesis that this is simply due to chance.
Table 3.
Regression Results of Relative Claims Expenditure for Medicare Beneficiaries Switching In and Switching Out of Medicare Advantage, 1999–2008
| Switching-In | Switching-Out | |||||||
|---|---|---|---|---|---|---|---|---|
| UnWeighted | Weighted | UnWeighted | Weighted | |||||
| Means | Model | Means | Model | Means | Model | Means | Model | |
| Dependent variable | 0.92 (2.31) | 0.84 (0.76) | 1.27 (2.07) | 1.37 (0.99) | ||||
| Base payment | 703.67 (90.30) | −0.0004 (0.0007) | 769.08 (122.63) | −0.001 (0.0007) | 686.43 (97.95) | −0.0004 (0.0008) | 768.83 (123.43) | 0.00086* (0.00048) |
| HCC | 0.59 (0.40) | −0.066 (0.233) | 0.41 (0.42) | 0.222 (0.189) | 0.45 (0.42) | 0.106 (0.254) | 0.40 (0.42) | 0.639*** (0.153) |
| Part D and lock-in | 0.55 (0.50) | −0.176 (0.105) | 0.36 (0.48) | 0.0004 (0.0600) | 0.41 (0.49) | −0.170 (0.118) | 0.35 (0.48) | −.286*** (0.098) |
| Time trend | 6.94 (2.77) | 0.031 (0.030) | 5.71 (3.06) | 0.008 (0.014) | 6.02 (2.98) | 0.039 (0.027) | 5.64 (3.04) | −0.024* (0.014) |
| Constant | 1.131** (0.442) | 1.504 (0.486) | 1.272*** (0.455) | 0.694** (0.326) | ||||
| Fixed effects | Yes | Yes | Yes | Yes | ||||
| Adj. R2 | 0.419 | 0.286 | 0.053 | 0.236 | ||||
| N | 13,831 | 13,245 | ||||||
Dependent variables: Switching-In: The average claims experience of those who join a Medicare Advantage plan in the 6 months prior to joining divided by the average experience over the same time period of those beneficiaries residing the same county who do not enroll. Switching-Out: The average claims experience of those who disenroll from a Medicare Advantage plan in the 6 months immediately following disenrollment divided by the average experience over the same time period of those beneficiaries residing in the same county who remained in traditional Medicare. Weighted regressions use the number of Medicare Advantage enrollees in the county-year as the weight. Standard deviations are in parentheses below mean values; standard errors are in parentheses below coefficient estimates.
*, **, *** indicate statistical significance at the 90, 95, and 99 percent confidence levels, respectively.
The regression results for the postdisenrollment claims experience of those MA enrollees returning to traditional Medicare tell a very different story. Focusing on the weighted regression results in Table 3, we find that the fully implemented HCC program was associated with a large increase in postdisenrollment claims experience. Claims of returning beneficiaries were nearly 64 percentage points higher than before the HCC program. This result must be put in the context of our earlier findings that the number of beneficiaries switching out of MA declined substantially. This increase in relative claims is likely to disproportionately reflect the very expensive tail of the distribution of beneficiaries whose health status experience was least well modeled by the HCCs.
Finally, our estimate of the net effect of Part D and the lock-in was a 29 percentage point increase in the average relative claims experience of those returning to traditional Medicare. This is consistent with risk-averse less-healthy beneficiaries returning to traditional Medicare to avoid the lock-in and/or to less-healthy beneficiaries returning to traditional Medicare now that valued prescription drug coverage was available through stand-alone plans.
To better understand the nature of MA disenrollment, we divided those switching out of MA in 1999 into quintiles based on the Medicare payments made on their behalf during the first 6 months of their return to traditional Medicare. For the least costly 20 percent of switchers in 1999, Medicare spent $124 or less on their covered care on their return to traditional Medicare. The fortieth percentile was $445, the sixtieth was $1,277, and the eightieth was $5,019.
We then used Medicare's average Parts A and B payments per beneficiary in each year relative to the 1999 value to convert subsequent years' spending into 1999 dollars. This index has the advantage of adjusting for both changes in Medicare prices and in Medicare utilization. We then computed the proportion of switchers-out who had 6 months post-disenrollment expenditures in each quintile.
The results for the lowest, middle, and highest quintiles of expenditures are plotted in Figure 2. By construction, 20 percent of the switchers in 1999 are in each of the five expenditure categories. In the 2000–2002 period, a higher percentage of MA disenrollees were in this low expenditure group. However, the trend reversed in 2003 and by 2008 only 15.1 percent of disenrollees were in this group. The pattern is reversed in the highest expenditure group. In the 2000–2002 period, relatively few disenrollees were in the highest cost group; this trend reversed in 2004 and by 2008 over 22 percent of the disenrollees were in this group. Thus, coincident with the phasing-in of the HCC, those disenrolling from MA were disproportionately “unhealthy.”
Figure 2.
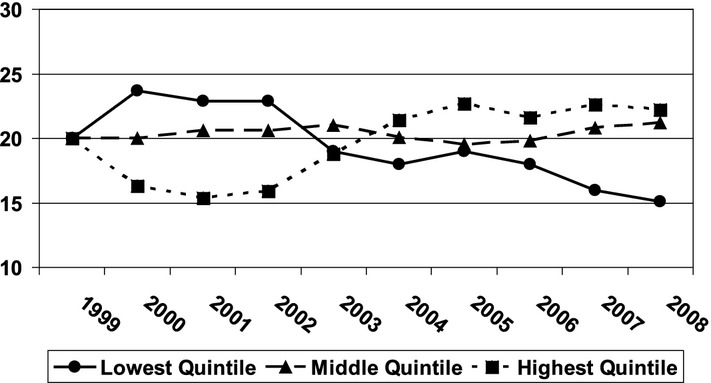
Percentage of Switchers-Out in Each Quintile of Expenditures, 1999–2008
Discussion
This study has examined the effects of changes in Medicare county base payment levels to MA plans and the phase-in of the HCCs approach to adjusting payment for beneficiary health status.
Five findings stand out. First, enrollment in MA plans is sensitive to the county-specific per capita payment level determined by CMS. A 10 percent higher monthly payment was associated with a 9.6 percent increase in county-level enrollment. Disenrollment was particularly sensitive to the payment level; a 10 percent increase reduced county-level disenrollments by over 35 percent. We are unable to examine the mechanisms whereby these changes in enrollment occurred. Certainly, many plans exited their markets in the early years and others entered later in the decade. In addition, lower (higher) payment levels may have led plans to raise (lower) premiums and copays or decrease (increase) supplemental services they provided. These changes would have led some beneficiaries to switch to or from traditional Medicare. Indeed, using 1998 Current Beneficiary Survey data, Atherly, Dowd, and Feldman (2004) found that a 10 percent increase in the premium of an MA plan reduced its market share by .62 percentage points. From the plan's perspective, this implied a premium elasticity of −4.6.
This finding has important implications for the Patient Protection and Accountable Care Act, which reduces payment levels to MA plans. Other things equal, one should anticipate reductions in enrollment that are on a par with the size of the cuts. That is, a 10 percent cut is likely to reduce enrollment by nearly 10 percent. Although the plans will reduce their enrollment of new subscribers, there is likely to be a substantial period of disenrollment when current enrollees return to traditional Medicare.
Second, our findings are driven by the effects in the one quarter of the counties with the largest Medicare population. Although one might expect counties with more potential buyers to see more impact, this was not the case. The population elasticities with respect to enrollment are virtually the same across the four groups of counties. Instead, our results indicate that the effects of the policy variables are substantially different in the largest Medicare counties. This suggests that much of the Medicare managed care market was largely unable to respond to policy changes implemented in the 2000s.
Third, our analysis of the introduction of the HCC approach suggests that the improved risk-adjustment mechanism has substantially affected the MA marketplace. The adoption of the HCC methodology is associated with much greater enrollment in MA plans and large reductions in disenrollment. From the perspective of MA plans, this can be viewed as a success. While we can only speculate, the results are consistent with a view that the new system reduced the uncertainly associated with enrolling Medicare beneficiaries. If a plan enrolled people who, ex post, were found to be less healthy, the payment system did provide higher payments.
However, there was no statistically significant evidence that the HCC led plans to enroll less-healthy beneficiaries; by the end of our analysis period in 2008, the 6 months prior claims experience of new enrollees remained only 91 percent of that of traditional Medicare enrollees in the same county over the same time period. We also found that the average claims experience of those disenrolling relative to those always in traditional Medicare was substantially higher in the last years of our study period. Much of this increase was attributable to the implementation of the HCC. However, as Pope and colleagues (2004) noted in their simulation of the HCC payment algorithm, instead of underpaying for beneficiaries in the fourth quintile of expenditures, the HCC overpaid by 2 percent and instead of underpaying by 56 percent in the top quintile of expenditures, the HCC only underpaid by 14 percent. Thus, it is reasonable to interpret our findings as saying that those in the middle of the expenditure distribution were more likely to remain in MA plans after the introduction of the HCC model. As a result, the post-HCC disenrollees were disproportionately in the costly tail of the expenditure distribution. Our investigation of the distribution of disenrollees by quintile of Medicare expenditures supports this speculation. As such, our findings lend support to the Ellis and McGuire (1993) and Newhouse (1996) proposals to directly pay MA plans for the costs associated with very high cost beneficiaries.
Fourth, we found that the introduction of the Medicare Part D drug program and the annual open enrollment period in which Medicare beneficiaries choose their plans for an entire year had modest and sometimes offsetting effects. On net, they not only increased the number of those switching into MA plans but also increased the number disenrolling by about the same magnitude. One of the traditional advantages of MA plans was the availability of prescription drug coverage. The availability of many stand-alone Part D drug programs may have provided ample substitutes for MA subscribers, leading to substantial disenrollment. However, the net increase in annual enrollment in our data suggests that there is more than just a Part D effect in operation and the introduction of the lock-in of potentially healthier beneficiaries is consistent with our findings.
Finally, this study offers some implications for the exclusion of MA populations from observational studies using Medicare claims data. First, it indicates that the MA population continues to have claims experience that is favorable relative to those in traditional Medicare. One should not generalize from the traditional Medicare population to the MA population nor should one generalize in the other direction. Furthermore, the increasingly higher claims experience of those who do return to traditional Medicare suggests that researchers should consider excluding newly disenrolled beneficiaries from studies, at least for several months because their utilization is much higher than that of those who have remained in traditional Medicare.
There are several limitations to this study. First, some caution must be exercised in interpreting our payment rate effects. Although the baseline rates used in the period 1999 through 2002 were the prices observed by MA plans, the benchmark rates phased-in beginning in 2003 do not reflect actual prices. They are the payment rates for plans submitting bids above the benchmark, but few plans did this. Most bids were below the benchmark. This result meant the plan received a payment rate that was below the benchmark by 25 percent of the difference between the benchmark and its bid. While this problem is likely modest over the phase-in period, it does imply that our payment rate estimates are biased downward.
Second, we only use the 5 percent sample of Medicare beneficiaries. However, we do inflate the country-level values by a factor or 20. Thus, our estimates should be of the correct magnitudes, but our standard errors are likely to be larger than would be the case if we had access to all of the Medicare data. Third, we do not observe the actual claims experience of those enrolled in MA plans; thus, of necessity our findings are inferential, based upon the experience of MA beneficiaries before they enroll in a plan and after they leave. Prior and subsequent claims experience is certainly not perfectly correlated with the claims experience while in the plans. Fifth, much of the growth in MA enrollment came from PFFS plans. While these plans have the same economic incentives as others, it may be that they enrolled a different subset of Medicare beneficiaries. Our data do not allow us to examine this possibility. Finally, we are not able to fully control for other factors affecting enrollment and disenrollment, but we have relied on a time trend and county-level fixed effects with robust standard errors to minimize this problem.
These limitations notwithstanding, this study reflects the first effort to evaluate the effects of the policy changes that have affected MA program since the Balanced Budget Act of 1997.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: Earlier versions of this article were presented at the biennial meeting of the 2011 International Health Economics Association biennial convention, the University of Georgia and Ohio State University. This research is supported by a contract between UAB and Amgen, Inc. Only authors from UAB have access to the Medicare data used. The analysis, presentation, and interpretation of the results are solely the responsibility of the authors.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Table S1: Switchers Into Medicare Advantage Total and by County Medicare Population Quartiles, 1999–2008.
Table S2: Switchers Out of Medicare Advantage Total and by County Medicare Population Quartiles, 1999–2008.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Atherly A, Dowd BE, Feldman R. “The Effects of Benefits, Premiums, and Health Risk on Plan Choice in the Medicare Program”. Health Services Research. 2004;39(4 part 1):847–64. doi: 10.1111/j.1475-6773.2004.00261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batata A. “The Effects of HMOs on Fee-for-Service Health Care Expenditures: Evidence from Medicare Revisited”. Journal of Health Economics. 2004;23:951–63. doi: 10.1016/j.jhealeco.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Blum J, Brown R, Frieder M. Medicare Issue Brief. Menlo Park, CA: Henry J. Kasier Family Foundation; 2007. “An Examination of Medicare Private Fee-for-Service Plans”; pp. 1–17. [Google Scholar]
- Brown J, Duggan M, Kuziemko I, Woolston W. 2011. “How Does Risk Selection Respond to Risk Adjustment? Evidence from the Medicare Advantage Program,” National Bureau of Economic Research working paper 16977. [DOI] [PubMed]
- Buccaneer Data Services, LLC. 2011. [accessed on October 1, 2012]. Available at: http://www.ccwdata.org/cs/groups/public/documents/document/ccw_userguide.pdf.
- Center for Medicare and Medicaid Services (CMS) 2010a. Health Plans, Reports, Files and Data – State County [accessed on October 1, 2012]. Available at: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/HealthPlanRepFileData/SC.html.
- Center for Medicare and Medicaid Services (CMS) 2010b. Medicare Advantage – Rates & Statistics – Ratebooks & Supporting Data. [accessed on October 1, 2012]. Available at: http://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/index.html?redirect=/MedicareAdvtgSpecRateStats/09_Bid_Forms_and_Instructions.asp.
- Centers for Medicare and Medicaid Services (CMS) Chapter 2: Medicare Advantage Enrollment and Disenrollment. Medicare Managed Care Manuel. 2005. [accessed on October 1, 2012]. Available at: http://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/index.html?redirect=/MedicareAdvtgSpecRateStats/09_Bid_Forms_and_Instructions.asp]. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R66MCM.pdf.
- Ellis RJ, McGuire T. “Supply Side and Demand Side Cost Sharing in Health Care”. Journal of Economic Perspectives. 1993;7:135–51. doi: 10.1257/jep.7.4.135. [DOI] [PubMed] [Google Scholar]
- Glavin MPV, Tompkins CP, Wallack SS, Altman SH. “An Examination of Factors in the Withdrawal of Managed Care Plans from the Medicare+Choice Program”. Inquiry. 2002;39:341–54. doi: 10.5034/inquiryjrnl_39.4.341. /2003. [DOI] [PubMed] [Google Scholar]
- Luft HS. Health Maintenance Organizations: Dimensions of Performance. New York: John Wiley and Son; 1981. [Google Scholar]
- Medicare Payment Advisory Commission. Report to the Congress: Medicare Payment Policy. Washington, DC: MedPAC, March; 2002. [Google Scholar]
- Medicare Payment Advisory Commission. Report to the Congress: Increasing the Value of Medicare. Washington, DC: MedPAC, June; 2006. [Google Scholar]
- Medicare Payment Advisory Commission. Report to Congress: Improving Incentives in the Medicare Program. Washington, DC: MedPAC, June; 2009. [Google Scholar]
- Mello MM, Stearns SC, Norton EC, Ricketts TC. “Understanding Biased Selection in Medicare HMOs”. Health Services Research. 2003;38(3):961–92. doi: 10.1111/1475-6773.00156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller RH, Luft HS. “Managed Care Plan Performance Since 1980”. Journal of the American Medical Association. 1994;271(19):1512–9. [PubMed] [Google Scholar]
- Newhouse JP. “Reimbursing Health Plan Providers: Efficiency in Production versus Selection”. Journal of Economic Literature. 1996;34:1236–63. [Google Scholar]
- Newhouse JP. “Assessing Health Reform's Impact on Four Key Groups of Americans”. Health Affairs. 2010;29(9):1–11. doi: 10.1377/hlthaff.2010.0595. [DOI] [PubMed] [Google Scholar]
- Newhouse JP, Manning WG, Keeler EB, Sloss EM. “Adjusting Capitation Rates Using Objective Health Measures and Prior Utilization”. Health Care Financing Review. 1989;10(3):41–54. [PMC free article] [PubMed] [Google Scholar]
- Physician Payment Review Commission. Chapter 15: Risk Selection and Risk Adjustment in Medicare. Washington, DC: PPRC; 1996. pp. 255–79. Annual Report to Congress. [Google Scholar]
- Pope GC, Kautter J, Ellis RP, Ashe AS, Avanian JZ, Izzoni LI, Ingber MJ, Levy JM, Robst J. “Risk Adjustment of Medicare Capitation Payments Using the CMS-HCC Model”. Health Care Financing Review. 2004;25(4):119–41. [PMC free article] [PubMed] [Google Scholar]
- Schoenman JA, Parente ST, Feldman JJ, Shah MM, Evans WN, Finch MD. “Impact of HMO Withdrawals on Vulnerable Medicare Beneficiaries”. Health Care Financing Review. 2005;26(3):5–30. [PMC free article] [PubMed] [Google Scholar]
- Zarabozo C. “Milestones in Medicare Managed Care”. Health Care Financing Review. 2000;22(1):61–7. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


