Abstract
Objective
To determine the proportion of privately insured adults using an out-of-network physician, the prevalence of involuntary out-of-network use, and whether patients experienced problems with cost transparency using out-of-network physicians.
Data Sources
Nationally representative internet panel survey conducted in February 2011.
Study Design
Screener questions identified a sample of 7,812 individuals in private health insurance plans with provider networks who utilized health services within the prior 12 months. Participants reported details of their inpatient and outpatient contacts with out-of-network physicians. An inpatient out-of-network contact was defined as involuntary if: (1) it was due to a medical emergency; (2) the physician's out-of-network status was unknown at the time of the contact; or (3) an attempt was made to find an in-network physician in the hospital but none was available. Outpatient contacts were only defined as involuntary if the physician's out-of-network status was unknown at the time of the contact.
Principal Findings
Eight percent of respondents used an out-of-network physician. Approximately 40 percent of individuals using out-of-network physicians experienced involuntary out-of-network care. Among out-of-network physician contacts, 58 percent of inpatient contacts and 15 percent of outpatient contacts were involuntary. The majority of inpatient involuntary contacts were due to medical emergencies (68 percent). In an additional 31 percent, the physician's out-of-network status was unknown at the time of the contact. Half (52 percent) of individuals using out-of-network services experienced at least one contact with an out-of-network physician where cost was not transparent at the time of care.
Conclusions
The frequency of involuntary out-of-network care is not inconsequential. Policy interventions can increase receipt of cost information prior to using out-of-network physician services, but they may be less helpful when patients have constrained physician choice due to emergent problems or limited in-hospital physician networks.
Keywords: Managed care, out-of-network, balance billing, health reform, cost transparency
Most privately insured individuals are enrolled in private health insurance plans that offer some reimbursement for services provided by out-of-network physicians (Kaiser Family Foundation/Health Research and Educational Trust 2011). These plans allow patients greater physician choice but with higher cost sharing. However, these additional costs may be unexpected if (1) a patient involuntary uses an out-of-network physician or (2) the costs of using an out-of-network physician are not transparent.
Both the voluntary choice and involuntary use of an out-of-network physician are influenced by three domains of factors: patient, encounter, and system (Figure 1). Note that the framework reflects each discrete factor as directly influencing use; however, some factors may interrelate and/or work through mediating factors. Importantly, in contrast with involuntary use, we see voluntary out-of-network use as an active choice by patients. Thus, we expect different factors to affect the decision to voluntarily go out-of-network (factors on left side of the conceptual framework) than those related to involuntary use (factors on right side).
Figure 1.
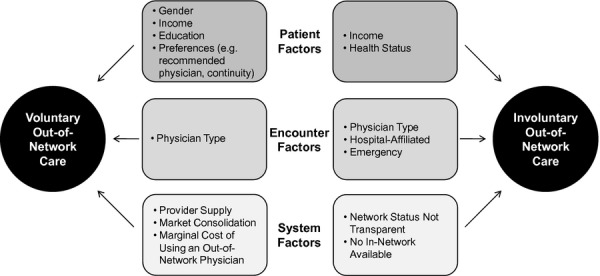
Conceptual Framework: Patient, Encounter, and System Factors Influencing Voluntary and Involuntary Out-of-Network Use
Related to patient factors influencing voluntary use, we expect individuals with higher income will be more likely to use out-of-network providers, and that individual preferences for a recommended physician and physician continuity will affect this choice. Perceived quality of specific out-of-network providers, which may or may not be associated with actual quality, may also lead to voluntary out-of-network health care use. Varying participation by physician type (e.g., primary care, mental health) in insurer networks may influence access to and therefore voluntary use of an out-of-network physician. Considering system characteristics influencing voluntary use, provider shortages and health system concentration may affect network adequacy, which may affect decisions related to out-of-network health care use.
For patient factors influencing involuntary use, we expect those with more contact with the health care system (perhaps due to fair/poor health status) to be more likely to experience involuntary out-of-network care. Of particular interest to policy makers are encounter and system factors that may result in involuntary use: With respect to encounter characteristics, in a medical emergency a patient may be treated at the nearest emergency room regardless of whether it is in-network. Whether a physician is out-of-network may not be disclosed to the patient at the point of care, leaving some patients unaware they have had contact with an out-of-network physician until receiving an unexpectedly high health care bill. Anecdotal evidence suggests that this may be especially problematic for hospital-based services such as anesthesiology or intensive care where the hospital may be in-network, but the assigned physician has chosen not to contract with the insurer (Mathews 2008; Andrews 2011b).
Lack of cost transparency in out-of-network care may relate to a lack of easily accessible information about the amount the physician charges for a specific service (i.e., list price), the level of insurer reimbursement, or patient responsibility with respect to out-of-pocket payments, making the marginal out-of-pocket cost of using an out-of-network physician unknown to the patient when making the decision to go out-of-network. Patients may be aware that out-of-network services are subject to higher coinsurance or higher and separate deductibles but may not be aware that these services are often subject to “balance billing” in which the patient is required to pay the difference between insurer reimbursement and the physician's billed charge.
Involuntary care and lack of cost transparency in out-of-network services have the potential to impact a large number of the privately insured. Although there are no recent national estimates of the prevalence of out-of-network service use, one 2004 study of health care claims suggests that out-of-network care represents 10–13 percent of total charges in point of service or preferred provider organization plans (McDevitt et al. 2007). These issues have also gained priority among policy makers as reflected in provisions in the 2010 Patient Protection and Affordable Care Act and numerous state-level legislative actions. To date, the evidence base for policy efforts has been limited to anecdotal, stakeholder commissioned, or geographically limited data (Mathews 2008; America's Health Insurance Plans 2009; Hoadley, Lucia, and Schwartz 2009; Kolata 2009; Raeburn 2009). We conducted the first nationally representative survey of patient experiences to describe the scope and nature of these issues.
Data and Methods
We sought to estimate (1) the proportion of privately insured adults using an out-of-network physician in the past 12 months, (2) the prevalence of involuntary out-of-network use, (3) the prevalence of voluntary out-of-network use, and (4) whether patients experienced problems with cost transparency using out-of-network physicians. A nationally representative sample of privately insured U.S. adults was surveyed via the internet in February 2011 on details of their out-of-network care experiences. A novel survey (see Supplemental Appendix SA2) was constructed based on existing literature, interviews with key informants, investigator hypotheses, and questions modified from existing surveys (Agency for Healthcare Research and Quality 2009; Center for Studying Health System Change 2009; U.S. Census 2010). Eighteen cognitive interviews using established methods (Willis 2005) were performed to assess relevance of content, as well as language and structure of items. Items for which there was significant respondent confusion during cognitive interviewing, such as those regarding cost sharing and out-of-pocket costs, were removed from the final survey. Respondents had the opportunity to refuse or skip questions for which they were unsure; these were treated as missing data. The reference period for the survey was limited to the past 12 months to reduce recall bias.
The survey was administered via the internet by Knowledge Networks, a private survey research firm. Knowledge Networks' online research panel (KnowledgePanel®) consists of approximately 50,000 U.S. households sampled by random-digit dialing and address-based sampling (KnowledgeNetworks 2011). Self-referred participants are not accepted, and households without internet are provided with necessary equipment and internet access. The probability-based sampling used to construct the panel and its representativeness of the U.S. population have been validated (Baker et al. 2003b), quality standards for recruitment are considered by the Centers for Disease Control and Prevention to be on par with the National Immunization Survey (Centers for Disease Control and Prevention 2010), and Knowledge Networks has become an increasingly common tool for data collection in academic studies (Baker et al. 2003a; Davis and Fant 2005; Bundorf et al. 2006; Barry et al. 2009). Panelists are incentivized to complete weekly surveys through free internet and hardware if needed, raffles for cash and other prizes, and small survey-specific monetary incentives (for this survey, about $1). Poststratification weights were applied to match the sample to the U.S. population based on Current Population Survey data on gender, age, race/ethnicity, education, metropolitan area, census region, and internet access, and to adjust for survey nonresponse and oversampling.
A series of screener questions was sent to 21,754 English-speaking panelists ages 18–64; panelists greater than 64 years old were excluded due to unique Medicare balance billing restrictions. As is typical in internet-based panel surveys, enrollment was closed when a predetermined number of panelists screened in and began the 10-minute survey, resulting in a completion rate of 64 percent (13,900 panelists). The survey had a Household Recruitment Rate of 17.5 percent, Household Profile Rate of 62.0 percent, Household Retention Rate of 37.5 percent, Cumulative Response Rate 1 of 6.9 percent, and Cumulative Response Rate 2 of 2.6 percent (Callegaro and Disogra 2008). There were differences by age and race between respondents and nonrespondents (data not shown). Screener questions identified panelists currently enrolled in a private health insurance plan with a provider network and who had seen either a physician or mental health professional within the last 12 months. Of those initiating the screener, 3,621 (26 percent) were excluded due to lack of private health insurance, 1,126 (8 percent) had private insurance but were not enrolled in a plan with a provider network, 1,095 (8 percent) had no physician use in the last year, and 246 (2 percent) refused or had missing data (see Supplemental Appendix SA3). Panelists who had seen an out-of-network physician or mental health professional completed a 10-minute survey regarding their care experiences.
We limited our survey content to questions about physicians and mental health professionals because cognitive interviewing during survey development revealed respondents consistently defined “health provider” to include providers beyond the scope of this study, including ancillary service personnel and individuals delivering care frequently not covered under health insurance contracts (e.g., massage therapy). We include mental health professionals (e.g., psychologists) because they are frequent providers of out-of-network services (Stein et al. 2007). For this survey, emergency room physicians were considered inpatient because they are hospital affiliated. Respondents were asked to identify how many inpatient and outpatient out-of-network physicians they had contact with in the past 12 months. A representative sample of inpatient and outpatient contacts was then constructed by prompting respondents to relate details on the first and second out-of-network physicians they contacted for first the inpatient and then the outpatient settings. A maximum of three out-of-network contacts were assessed. Because we asked about inpatient experiences first, a small number (4 percent) of respondents were limited to reporting details on only one of their multiple outpatient contacts.
We sought to describe patient, encounter, and system-level factors associated with out-of-network physician use (Figure 1). Apart from overall health status, patient demographic information was available from Knowledge Networks and not reassessed. Respondents were asked a series of questions regarding each out-of-network contact, including the type of physician, whether it was in the setting of a medical emergency, if the hospital was in-network (for inpatient contacts only), and when the out-of-network status of the physician was first known. If it was known that the physician was out-of-network either before or at the time of the contact, the respondent was asked to select from a list of reasons or free text why they decided to use the physician and then select a primary reason. We also included questions regarding the financial burden of out-of-network use and availability of overall cost information.
An inpatient out-of-network contact was defined as involuntary if: (1) it was due to a medical emergency (excluding labor and delivery), (2) the physician's out-of-network status was unknown at the time of the contact (e.g., out-of-network status was not known until receiving the bill), or (3) an attempt was made to find an in-network physician in the hospital but none was available. To determine which of these reasons was most common, we also created a hierarchical categorical variable (in the order noted in the preceding text) which categorized each contact into one of these three reasons. Outpatient contacts were only defined as involuntary if the physician's out-of-network status was unknown at the time of the contact. In some cases, the patient may have been able to obtain this information with further research, but we categorize as involuntary because the provider did not disclose network status at the time of contact. Both inpatient and outpatient contacts were defined as not cost transparent if the respondent answered “No” to the question: “Before you received care from this doctor, did you know how much you would have to pay? This information could have come from the hospital, doctor, or the insurance company.”
All reported analyses are weighted to represent the U.S. population. Reported sample sizes are unweighted. Simple frequencies and Chi-squared tests were used for categorical variables, and logistic regression was used to calculate the odds of any out-of-network use, any involuntary out-of-network use, and any contact with nontransparent costs controlling for age, gender, race/ethnicity, marital status, education, income, residence in a metropolitan area, census region, and self-reported health status. To test whether frequent users of out-of-network physicians might have skewed contact-level results, all analyses were performed with only one inpatient and one outpatient contact per person, with no significant change in results (results not shown). All analyses were performed using SAS statistical software version 9.2 (SAS Institute, Inc., Cary, NC, USA). The Yale University Institutional Review Board approved this study with exemption from committee review. Waiver of consent was obtained because identifying data were not available to the investigators.
Results
Users of Out-of-Network Physicians
The sample included 7,812 respondents enrolled in private health plans with provider networks and with at least one physician or mental health professional contact within the last 12 months. Approximately 8.3 percent (n = 721/7,812) used an out-of-network physician (Table 1, Column 2). A significantly greater proportion of those of female sex, never married, some college, income <$35,000 and >$100,000, and with fair or poor health status had contact with at least one inpatient or outpatient out-of-network physician. In adjusted logistic regression, female sex, never being married, and fair or poor health status were associated with increased odds of using an out-of-network physician; middle-income groups ($35–$59 K and $60–$100 K) had decreased odds (Supplemental Appendix SA4).
Table 1.
Total Sample Characteristics and Out-of-Network Use, Involuntary and Voluntary Out-of-Network Use, and Non-Transparent Out-of-Network Costs by Demographic Characteristics
| Characteristic | Total Sample unwt n (wt % of total sample) | Out-of-Network Use* unwt n (wt % of row characteristic) | p | Voluntary Out-of-Network Use* unwt n (wt % of row characteristic) | p | Involuntary Out-of-Network Use* unwt n (wt % of row characteristic) | p | Non-Transparent Out-of-Network Costs* unwt n (wt % of row characteristic) | p |
|---|---|---|---|---|---|---|---|---|---|
| Total | 7,812 (100) | 721 (8.3) | 546 (6.0) | 247 (3.1) | 364 (4.3) | ||||
| Age | |||||||||
| 18–29 | 531 (18.1) | 59 (10.2) | .06 | 33 (6.4) | .75 | 31 (4.4) | .11 | 32 (5.1) | .12 |
| 30–49 | 2,755 (43.8) | 218 (7.1) | 167 (5.6) | 74 (2.6) | 103 (3.4) | ||||
| 50–64 | 4,526 (38.1) | 444 (8.7) | 346 (6.3) | 142 (3.1) | 229 (4.9) | ||||
| Sex | |||||||||
| Male | 2,055 (43.8) | 154 (6.4) | <.001 | 112 (4.5) | <.001 | 60 (2.6) | .12 | 90 (3.8) | .20 |
| Female | 5,757 (56.2) | 567 (9.7) | 434 (7.2) | 187 (3.6) | 274 (4.7) | ||||
| Race | |||||||||
| White | 6,522 (75.2) | 622 (8.5) | .55 | 475 (6.1) | .70 | 203 (3.1) | .90 | 304 (4.4) | .72 |
| Nonwhite | 1,290 (24.8) | 99 (7.7) | 71 (5.7) | 44 (3.2) | 60 (4.0) | ||||
| Marital status | |||||||||
| Married/living with partner | 5,861 (71.9) | 505 (7.3) | .002 | 390 (5.5) | .06 | 164 (2.4) | .002 | 252 (3.7) | .06 |
| Divorced/separated/widowed | 1,064 (10.6) | 110 (9.6) | 81 (6.2) | 40 (4.4) | 56 (5.4) | ||||
| Never married | 887 (17.5) | 106 (11.6) | 75 (8.0) | 43 (5.3) | 56 (5.8) | ||||
| Education | |||||||||
| High school or less | 885 (26.4) | 53 (6.1) | .03 | 35 (4.1) | .03 | 27 (3.1) | .11 | 31 (3.4) | .31 |
| Some college | 2,765 (31.0) | 244 (9.4) | 168 (6.3) | 106 (4.0) | 133 (4.9) | ||||
| Bachelor's degree or higher | 4,162 (42.6) | 424 (8.8) | 343 (7.0) | 114 (2.5) | 200 (4.4) | ||||
| Income (per year) | |||||||||
| <$35,000 | 825 (14.1) | 80 (12.0) | <.001 | 51 (7.6) | <.001 | 42 (6.6) | <.001 | 44 (7.1) | <.001 |
| $35,000–$59,000 | 1,853 (27.5) | 123 (5.2) | 89 (3.8) | 48 (2.6) | 65 (2.7) | ||||
| $60,000–$100,000 | 2,858 (34.5) | 258 (7.7) | 198 (5.6) | 87 (2.4) | 125 (3.8) | ||||
| >$100,000 | 2,276 (23.9) | 260 (10.5) | 208 (8.3) | 70 (2.8) | 130 (5.1) | ||||
| Residence in metropolitan area | |||||||||
| Yes | 6,820 (86.4) | 640 (8.5) | .16 | 494 (6.2) | .31 | 208 (3.2) | .69 | 313 (4.3) | .86 |
| No | 992 (13.6) | 81 (6.6) | 52 (4.9) | 39 (2.9) | 51 (4.4) | ||||
| Region of country | |||||||||
| Northeast | 1,432 (20.8) | 152 (9.3) | .21 | 123 (6.8) | .14 | 45 (3.1) | .79 | 76 (4.2) | .33 |
| Midwest | 2,298 (24.0) | 169 (6.7) | 119 (4.5) | 68 (2.9) | 100 (4.3) | ||||
| South | 2,284 (33.4) | 220 (8.9) | 162 (6.6) | 83 (3.5) | 119 (5.0) | ||||
| West | 1,798 (21.8) | 180 (8.2) | 142 (6.1) | 51 (2.8) | 69 (3.3) | ||||
| Health status (self-reported) | |||||||||
| Excellent, very good, or good | 7,171 (91.4) | 649 (8.0) | .04 | 495 (5.8) | .18 | 213 (2.8) | .006 | 322 (3.9) | .006 |
| Fair or poor | 627 (8.6) | 72 (11.8) | 51 (8.0) | 34 (6.5) | 42 (8.0) | ||||
Note. Sample includes respondents ages 18–64 in private health plans with provider networks using at least one physician or mental health professional in the last year. For Total Sample, column percentages sum to 100 percent. For Out-of-Network Use, Involuntary and Voluntary Out-of-Network Use, and Out-of-Network Costs, means within category are presented. p-values in bold are significant at <.05.
Outcomes include any inpatient or outpatient contact.
Among inpatient contacts, the most frequent physician type was emergency room (28.7 percent) (Table 2, Column 1). For outpatient out-of-network contacts, 44.7 percent were with specialists, 28.2 percent with mental health professionals, and 27.1 percent with primary care physicians.
Table 2.
Characteristics of Out-of-Network Contacts
| Total Sample | Voluntary Contacts unwt n (wt %) | Involuntary Contacts | p | |
|---|---|---|---|---|
| Inpatient contacts | ||||
| Total | 419 (100) | 173 (42.4) | 246 (57.6) | |
| Physician type* | ||||
| Emergency room | 111 (28.7) | – | – | |
| General practitioner | 75 (19.5) | – | – | |
| Anesthesia/ICU/Radiology | 43 (10.2) | – | – | |
| Mental health | 29 (6.8) | – | – | |
| Surgeon | 31 (6.5) | – | – | |
| Ob/Gyn | 17 (6.3) | – | – | |
| Other specialist | 106 (22.1) | – | – | |
| Nontransparent costs | 249 (57.2) | 60 (31.3) | 189 (75.5) | <.0001 |
| Hospital in-network | ||||
| Yes | 196 (48.9) | 67 (43.0) | 129 (53.1) | .43 |
| No | 119 (29.6) | 55 (33.9) | 64 (26.6) | |
| Unknown | 95 (21.5) | 43 (23.1) | 52 (20.3) | |
| Outpatient contacts | ||||
| Total | 662 (100) | 572 (85.3) | 90 (14.7) | |
| Physician type | ||||
| Specialist | 332 (44.7) | 280 (45.4) | 52 (40.1) | .006 |
| Mental health | 161 (28.2) | 148 (30.4) | 13 (15.8) | |
| Primary care | 162 (27.1) | 138 (24.2) | 24 (44.1) | |
| Nontransparent costs | 246 (39.2) | 172 (31.4) | 74 (84.2) | <.0001 |
Note. n's may not sum due to missing data. Percentages may not total 100 due to rounding.
Unable to report comparison by voluntary and involuntary contacts due to sample size.
Voluntary Out-of-Network Use
Patient Factors
Almost three quarters (72.6 percent, n = 546/721) of individuals using an out-of-network physician reported any (at least one) voluntary out-of-network contact in the last 12 months; this represents 6.0 percent of the total sample (Table 1, Column 3). Patient demographic factors associated with voluntary out-of-network use included female sex, and higher education, and income. In adjusted logistic regression, female sex was associated with significantly increased odds of any voluntary out-of-network use and middle-income groups with decreased odds (Supplemental Appendix SA4). Patient preferences for choosing an out-of-network outpatient physician primarily consisted of continuity with a previously known physician; recommendation of another physician, friend, or family member; or the perceived skill of the out-of-network physician (Table 3).
Table 3.
Reasons for Voluntary Outpatient Out-of-Network Use
| All Reasons Noted* | unwt n (wt %) |
|---|---|
| Total | 566 (100) |
| Continuity with previously known physician | 205 (30.8) |
| Physician skill | 198 (30.1) |
| Recommendation of another doctor, family, or friends | 152 (26.1) |
| Illness that needed care right away | 50 (13.7) |
| Convenient location | 45 (9.6) |
| No in-network physician available in area | 32 (6.5) |
| Could schedule appointment sooner | 25 (4.3) |
| Second opinion | 14 (2.1) |
| Service or specialty not covered by insurance | 14 (2.0) |
| Other | 71 (15.8) |
| Refused | 1 (0.23) |
| Primary Reason† | unwt n (wt %) |
|---|---|
| Total | 566 (100) |
| Continuity with previously known physician | 175 (26.6) |
| Recommendation of another doctor, family, or friends | 111 (19.8) |
| Physician skill | 126 (18.7) |
| Illness that needed care right away | 31 (8.5) |
| No in-network physician available in area | 16 (4.1) |
| Convenient location | 16 (3.8) |
| Service or specialty not covered by insurance | 13 (1.8) |
| Could schedule appointment sooner | 8 (1.6) |
| Second opinion | 7 (0.8) |
| Other | 59 (14.1) |
| Refused | 1 (0.2) |
Note. n's may not sum due to missing data. Percentages may not total 100 due to rounding.
Percents sum to greater than 100 because more than one reason could be noted.
Participants were asked to indicate one main reason why they used an out-of-network physician.
Encounter Factors
For voluntary outpatient contacts, physician type was similar to overall out-of-network use (Table 2, Column 2).
Involuntary Out-of-Network Use
Patient Factors
Approximately 40 percent (37.9 percent, n = 247/721) of individuals using an out-of-network physician reported any (at least one) involuntary out-of-network contact in the last 12 months; this represents 3.1 percent of the total sample (Table 1, Column 4). There was a significantly greater representation of involuntary out-of-network use among those never married, income <$35,000, and fair or poor health status. In adjusted logistic regression, never being married and fair or poor health status were associated with significantly increased odds of any involuntary out-of-network use (Supplemental Appendix SA4).
Encounter and Systems Factors
Fifteen percent (n = 90/662) of outpatient out-of-network contacts were involuntary (Table 2, Column 3). A greater proportion of primary care contacts were involuntary as compared to specialist and mental health contacts (24.2 percent vs. 13.4 and 8.3 percent, respectively, p = .006) (Figure 2a; Data from Table 2 presented as row percent).
Figure 2.
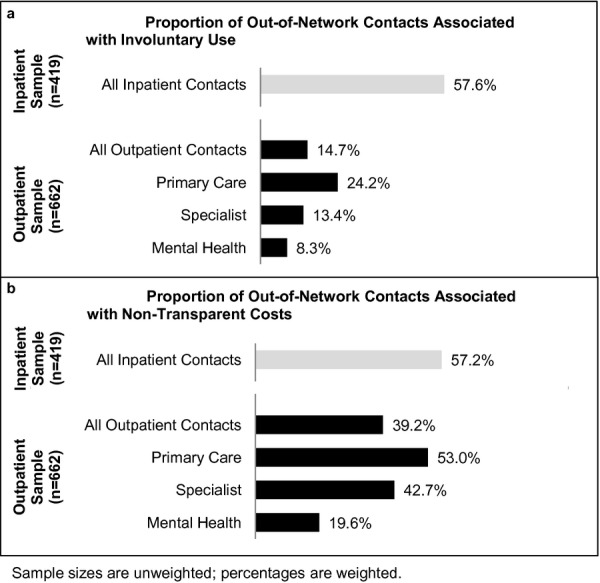
(a) Proportion of Out-of-Network Contacts Associated with Involuntary Use. (b) Proportion of Out-of-Network Contacts Associated with Nontransparent Costs
Over half (57.6 percent, n = 246/419) of inpatient out-of-network contacts were involuntary (Table 2, Column 3). Among involuntary inpatient out-of-network contacts, 68.1 percent occurred in the context of a medical emergency, as compared with 30.6 percent from lack of knowledge of the physician's out-of-network status. For 1.3 percent of contacts, it was known that the physician was out-of-network, but an in-network physician was not available (results not shown). Over half (53.1 percent) of involuntary inpatient out-of-network contacts were at in-network hospitals (Table 2, Column 3).
Lack of Cost Transparency
Approximately half (51.6 percent, n = 364/721) of those using out-of-network services experienced any (at least one) out-of-network contact with nontransparent costs; this represents 4.3 percent of the total sample (Table 1, Column 5). Poor or fair health status was significantly associated with increased odds of experiencing nontransparent costs, whereas middle income ($35,000–$59,000) was associated with decreased odds (Supplemental Appendix SA4).
Over half (57.2 percent) of inpatient out-of-network contacts had nontransparent costs (Figure 2b; Data from Table 2 presented as row percent). Forty percent (39.2 percent) of outpatient out-of-network contacts had nontransparent costs, with a greater proportion among primary care and specialist contacts than mental health (53.0, 42.7, and 19.6 percent, respectively, p < .001). Of those using out-of-network services, when asked, “Do you think you had enough information on the costs of using a doctor not in your insurance network?” 36.3 percent answered, “No.” Approximately 10 percent (9.7 percent) had been contacted by a debt collection agency for an out-of-network bill, and a quarter (25.8 percent) reported financial difficulty paying out-of-network bills in the last year (results not shown).
Discussion
Almost 40 percent of individuals using out-of-network services experienced involuntary out-of-network use. This represents almost 3 million people annually in the United States. We also found a lack of cost transparency for out-of-network services. For over half of inpatient contacts and approximately 40 percent of outpatient contacts, the patient did not know how much they would have to pay before receiving care. One third of individuals using out-of-network services reported not having enough information about the costs of using an out-of-network physician.
Our results suggest that involuntary care and lack of cost transparency in out-of-network physician services are attributable to encounter characteristics and system-level failures rather than individual patient health literacy. Lower educational attainment was not associated with increased involuntary out-of-network use or lack of cost transparency. Involuntary out-of-network use was particularly prevalent in the inpatient setting; almost 60 percent of inpatient out-of-network contacts were involuntary. For these involuntary inpatient contacts, the majority occurred during a medical emergency. The out-of-network option is intended to allow patients the choice of an out-of-network physician at increased cost. However, in a medical emergency, a patient may not have access to an in-network hospital or physician. Those with fair or poor self-reported health status were more likely to use an out-of-network physician and experience involuntary out-of-network care; this may be due to their increased health care system use, especially emergency room visits and hospitalizations.
We found that more than half of involuntary inpatient out-of-network physician contacts were at in-network hospitals. For outpatient care, patients are often aware that it is more expensive to choose an out-of-network physician, and the physician's office may verify insurance plan when an appointment is scheduled. In contrast, patients often do not choose physicians assigned to them in the hospital, and in the case of radiologists or pathologists, may not come in contact with their physician. Patients may incorrectly assume that if a specific hospital is in-network that all physicians treating them at that hospital are also in-network.
The lack of cost transparency for out-of-network services may be more problematic than for in-network services. Out-of-network physicians are not limited to an insurer fee schedule when setting prices and the patient is responsible for any balance billing charges. Balance billing has the potential to increase the patient's out-of-pocket payment significantly. One study found that in California in 2006, among individuals that used any out-of-network services (including inpatient, outpatient, facility, and physician services), the average potential balance bill amount (based on billed charges) for out-of-network services used during the year was $1,289. This was in addition to the average patient copayment or coinsurance of $433 (Hoadley, Lucia, and Schwartz 2009). A 2009 report issued by America's Health Insurance Plans indicated that, at the extremes, physician list prices or charges can be more than 10 times the Medicare fee (America's Health Insurance Plans's 2009). These studies do not provide definitive evidence on the extent of balance billing as some physicians may accept the maximum payment from the insurer, negotiate with the patient for a lower price, or not pursue collections. In this survey, we were unable to assess level of cost sharing or the marginal out-of-pocket cost incurred from using an out-of-network over an in-network physician because cognitive interviewing suggested that self-reports of cost were unreliable. We did find that almost 10 percent of this privately insured population using out-of-network services were contacted by a debt collection agency, and approximately one fourth reported difficulty paying out-of-network bills, although it is impossible to know how this may compare if services were obtained only in-network. The marginal cost of out-of-network care is critical in understanding policy implications and should be addressed in future studies.
The primary limitation of this study is potential for nonresponse bias. Because we used an English-only internet survey and there were some differences between responders and nonresponders, there is some concern that our results may not be representative of the U.S. population. However, the probability-based sampling used by KnowledgeNetworks includes noninternet households and poststratification weights adjusted for internet use. Poststratification weights also adjusted for panel recruitment and attrition and nonresponse to our specific survey using demographic distributions from the most recent data from the Current Population Survey. However, any unmeasured confounders that were associated with both participation in the KnowledgeNetworks panel or our specific survey and outcomes may result in nonrepresentative results.
Second, the survey relied on self-report. We believe that our estimates of out-of-network use are conservative because some respondents may have been unaware that they used an out-of-network physician if it was not known at the time of service and they did not closely examine their health care bill. This may be especially true for hospital-affiliated physician services such as radiology and pathology where the patient may not have contact with the physician. Several measures were taken to mitigate recall bias: the reference period was limited to the last 12 months, cognitive interviewing was used to inform survey development, and hyperlinks to definitions for potentially confusing terms such as “network” or “specialist” were available in the online survey. Although we asked respondents to only share their contacts with physicians, to the extent that respondents could not distinguish between physicians and nurse practitioners or physician assistants, visits with these provider types may be included in the analyses.
Also, while it was possible to obtain a representative sample of out-of-network contacts within the inpatient and the outpatient settings separately, we did not obtain a representative sample of the universe of out-of-network contacts. Therefore, it is not possible from these data to estimate overall involuntary use in out-of-network contacts, or compare the inpatient to outpatient settings. Lack of data on balance billing practices is another limitation of this survey.
Current approaches to protecting patients from involuntary out-of-network charges tend to favor one stakeholder over another: making the insurer liable for the out-of-network charge or limiting provider revenue by prohibiting providers from charging more than the in-network rate. Price transparency measures are a popular solution; for example, both Louisiana and Texas recently passed legislation requiring disclosure of out-of-network status. Texas law also requires out-of-network providers to provide an estimate of charges prior to services (Texas Senate Bill 1731 2007; Louisiana Act No. 354 2009). Disclosure of out-of-network status and price may be sufficient for outpatient care. However, these transparency measures may not be sufficient for the inpatient setting where emergent health issues or lack of an in-network option prevents choice. The Affordable Care Act (ACA) requires that plans not impose higher copayment or coinsurance for out-of-network emergency room providers and regulates the minimum amount insurers must reimburse, although balance billing is allowed (Federal Register 2010). This strategy could be extended to other hospital-based services if it succeeds in protecting patients from unreasonable costs. State variation in the regulatory environment, patient demand for out-of-network providers, network adequacy, and provider competition and incentive to join managed care networks may suggest that the optimal regulatory action may differ by state. Potentially, there may be less need for regulation if accountable care organizations (ACOs) gain greater market share. In these integrated systems, the distinction between payments to hospitals and payments to hospital-based providers may blur, mitigating the problem of unexpected charges from out-of-network providers at in-network hospitals.
The tension between provider choice and health care costs is likely to increase as insurers, employers, and individuals struggle to contain health care costs. A recent PriceWaterhouseCoopers survey found that insurers are increasingly making it more costly for consumers to use out-of-network providers. Many plans are increasing deductibles for out-of-network care; in 2011, 44 percent of plans had a deductible of $1,000 or more for out-of-network care, compared with 29 percent of plans in 2010, while some high-deductible plans may not allow out-of-network costs to contribute toward the deductible (PriceWaterhouseCoopers Health Research Institute 2011). In some markets, employers and individuals are also increasingly interested in the growing number of narrow or limited network plans that exclude premier high-cost hospital systems such as the Harvard teaching hospitals or Mayo Clinic in exchange for lower premiums (Abelson 2010; Andrews 2011a; PriceWaterhouseCoopers Health Research Institute 2011; Snowbeck 2011). If the market shifts toward more restrictive provider networks, purchasers, insurers, and regulators will be forced to consider the relative value of adequate provider payment, increasing premiums, and patient protection from excessive, and often involuntary, out-of-network provider charges.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This study was supported by a grant from the Women's Health Research at Yale Pilot Project Program and funding from the Yale Robert Wood Johnson Foundation Clinical Scholars Program. The sponsors were not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Dr. Kyanko has accepted consulting fees from the Consumers Union, a non-profit organization dedicated to consumer protection, and FAIR Health Inc, an independent, non-profit organization with the mission to ensure fairness of out-of-network reimbursement. These consulting activities are in topic areas outside of the submitted manuscript, but both entities may be perceived to have interest in the manuscript content. Dr. Busch serves on the Scientific Advisory Board of FAIR Health Inc. and has received payment for that service. Dr. Curry has no financial disclosures.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix SA2: Screener and Survey Instruments.
Appendix SA3: Selection of Survey of Respondents.
Appendix SA4: Demographic Predictors of Out-of-Network Use, Involuntary and Voluntary Out-of-Network Use, and Nontransparent Out-of-Network Costs.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Abelson R. “Insurers Push Plans That Limit Choice of Doctor”. The New York Times. 2010 [Google Scholar]
- Agency for Healthcare Research and Quality. 2009. “CAHPS Clinician and Group Survey, Adult Primary Care Questionnaire 1.0, Updated October 8, 2009” [accessed on May 18, 2009]. Available at: https://www.cahps.ahrq.gov/cahpskit/CG/CGChooseQx4P.asp. [DOI] [PubMed]
- America's Health Insurance Plans. 2009. “The Value of Provider Networks and the Role of Out-of-network Charges in Rising Health Care Costs: A Survey of Charges Billed by Out-Of-Network Physicians” [accessed on October 1, 2012]. Available at http://www.ahip.org/Value-of-Provider-Networks-Report/
- Andrews M. “Insurance Trade-Off: Reducing Premiums by Eliminating Expensive Doctors, Hospitals”. Kaiser Health News. 2011a [Google Scholar]
- Andrews M. “Insurers Sometimes Reject Neonatal Intensive Care Costs”. Kaiser Health News. 2011b [Google Scholar]
- Baker L, Wagner TH, Singer S, Bundorf MK. “Use of the Internet and E-mail for Health Care Information: Results from a National Survey”. The Journal of the American Medical Association. 2003a;289(18):2400–6. doi: 10.1001/jama.289.18.2400. [DOI] [PubMed] [Google Scholar]
- Baker LC, Bundorf MK, Singer S, Wagner TH. Validity of the Survey of Health and Internet and Knowledge Network's Panel and Sampling. Stanford, CA: Standford University; 2003b. [Google Scholar]
- Barry CL, Brescoll VL, Brownell KD, Schlesinger M. “Obesity Metaphors: How Beliefs about the Causes of Obesity Affect Support for Public Policy”. The Milbank Quarterly. 2009;87(1):7–47. doi: 10.1111/j.1468-0009.2009.00546.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bundorf MK, Wagner TH, Singer SJ, Baker LC. “Who Searches the Internet for Health Information?”. Health Services Research. 2006;41(3 pt 1):819–36. doi: 10.1111/j.1475-6773.2006.00510.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callegaro M, Disogra C. “Computing Response Metrics for Online Panels”. Public Opinion Quarterly. 2008;72(5):1008–32. [Google Scholar]
- Center for Studying Health System Change. 2009. “2007 Health Tracking Household Survey Public Use File: Codebook” [accessed on May 18, 2009]. Available at: http://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/26001/documentation.
- Centers for Disease Control and Prevention. “Interim Results: Influenza A (H1N1) 2009 Monovalent and Seasonal Influenza Vaccination Coverage among Health-Care Personnel – United States, August 2009–January 2010”. Morbidity and Mortality Weekly Report. 2010;59(12):357–62. [PubMed] [Google Scholar]
- Davis MM, Fant K. “Coverage of Vaccines in Private Health Plans: What Does the Public Prefer?”. Health Affairs (Project Hope) 2005;24(3):770–9. doi: 10.1377/hlthaff.24.3.770. [DOI] [PubMed] [Google Scholar]
- Federal Register. “Rules and Regulation: Patient Protection and Affordable Care Act; Requirements for Group Health Plans and Health Insurance Issuers under the Patient Protection and Affordable Care Act Relating to Preexisting Condition Exclusions, Lifetime and Annual Limits, Rescissions, and Patient Protections; Final Rule and Proposed Rule”. National Archives and Records Administration. 2010 Vol. 75, No. 123. [Google Scholar]
- Hoadley J, Lucia K, Schwartz S. Oakland, CA: California HealthCare Foundation; 2009. “Unexpected Charges: What States Are Doing about Balance Billing.”. [Google Scholar]
- Kaiser Family Foundation/Health Research and Educational Trust. 2011. “2011 Kaiser/HRET Employer Health Benefits Survey. Distribution of Health Plan Enrollment for Covered Workers, by Plan Type, 1988-2011 (Exhibit 5.1)” [accessed on April 30, 2011]. Available at: http://facts.kff.org/chart.aspx?ch=1540.
- KnowledgeNetworks. 2011. “Methodological Papers, Presentations, and Articles on Knowledge Panel “[accessed on July 8, 2011]. Available at: http://www.knowledgenetworks.com/ganp/reviewer-info.html.
- Kolata G. “Tackling the Mystery of How Much It Costs”. The New York Times. 2009 [Google Scholar]
- Louisiana Act No. 354. 2009. “(SB 282) Enacts Revised Statute 22:1879.”.
- Mathews AW. “Surprise Health Bills Make People See Red”. The Wall Street Journal. 2008:1. [Google Scholar]
- McDevitt R, Gabel J, Gandolfo L, Lore R, Pickreign J. “Financial Protection Afforded by Employer-Sponsored Health Insurance: Current Plan Designs and High-Deductible Health Plans”. Medical Care Research and Review. 2007;64(2):212–28. doi: 10.1177/1077558706298292. [DOI] [PubMed] [Google Scholar]
- PriceWaterhouseCoopers Health Research Institute. 2011. “Behind the Numbers: Medical Cost Trends for 2012.”.
- Raeburn P. “Code Blue: Out-Of-Network Charges Can Spur Financial Emergency”. Kaiser Health News. 2009 [Google Scholar]
- Snowbeck C. St. Paul Pioneer Press; 2011. “Some Insurance Companies Pushing Plans with Mayo Clinic Out of Network.”. [Google Scholar]
- Stein BD, Meili R, Tanielian TL, Klein DJ. “Outpatient Mental Health Utilization among Commercially Insured Individuals: In- and Out-of-Network Care”. Medical Care. 2007;45(2):183–6. doi: 10.1097/01.mlr.0000244508.55923.b3. [DOI] [PubMed] [Google Scholar]
- Texas Senate Bill 1731. 2007. “Legislative Session 80(R)”.
- U.S. Census. 2010. “2010 American Community Survey English Questionnaire” [accessed on May 18, 2010]. Available at: http://www.census.gov/acs/www/Downloads/questionnaires/2010/Quest10.pdf.
- Willis GB. Cognitive Interviewing. Thousand Oaks, CA: Sage Publications; 2005. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


