Abstract
Purpose
Adequate training and support are critical for community health workers (promotoras de salud in Spanish) to work effectively. Current literature on promotora training is limited by a focus on promotoras' knowledge and satisfaction immediately after training. The relevance of training to subsequent work performance and the need for ongoing training are rarely addressed. This paper describes the training and evaluation components of a promotora intervention focused on diabetes self management.
Training Methods
Project MATCH (the Mexican American Trial of Community Health Workers) is a clinical trial designed to test the effectiveness of an intensive, promotora-based intervention to improve disease self-management for Mexican-Americans with diabetes. The MATCH investigators designed a multi-component promotora training program that provided both initial and ongoing training. The investigators used multiple methods to determine promotoras' knowledge levels, initial competency in intervention delivery, and changes in this competency over time.
Evaluation Methods and Results
The evaluation results show that while the initial training provided a solid knowledge and skills base for the promotoras, the ongoing training was critical in helping them deal with both intervention-related and personal challenges.
Conclusions
The experiences of the MATCH study suggest that in addition to strong initial training, promotora interventions benefit from ongoing training and evaluation to ensure success.
Introduction
Community health workers (promotoras de salud in Spanish) are lay people who receive training to educate and assist members of their community in maintaining and improving their health.1, 2 Promotoras have been a part of health promotion and disease prevention efforts in US communities for several decades. The intent of promotora programs is to address the health needs of under-served populations by training members of these communities, who can reach their community effectively, to provide health promotion and disease prevention interventions3, 4, 5.
While an increasing number of studies are showing effectiveness of promotora interventions to improve health outcomes6–8, the mechanism for how promotora interventions actually change health outcomes remains unclear. The primary theory underlying promotoras is that, by virtue of being of the target community, they can empower community members to identify their own needs and implement their own solutions, leading to improved personal and community self-efficacy1, 2, 4, 9. To begin to understand how these interventions work, researchers need to define the specific skills necessary for an effective promotora intervention, and then identify the necessary support and training for the acquisition of these skills. The current promotora training literature is primarily descriptive in nature and focuses on promotora knowledge, satisfaction and self efficacy after training6, 10–13. One study documents a trainer observation scale to evaluate promotora skills, but beyond this there has been little published on the process of promotora training and monitoring over time.10
The Mexican-American Trial of Community Health Workers (MATCH) is a randomized clinical trial testing the effectiveness of a promotora intervention to help Latinos with diabetes to improve their disease self-management skills. After training in diabetes and self management, promotoras make home visits to participants over a two year period, to help model and encourage self-management and action planning for participants in relation to their diabetes, including behaviors such as glucose testing, diet control, exercise, medication regime adherence and visits to a health care provider. The four year study is ongoing and when completed, outcomes will include physiologic measures, and measures of self-efficacy and self-management behaviors.
The MATCH investigators used a multi-component training and evaluation approach to teach the promotoras the intervention skills. Investigators wanted to assess promotora knowledge as a result of the training, but more importantly they wanted to look at the impact of training on the ability of the promotoras to deliver the intervention. This paper describes the initial and ongoing training components of the MATCH program, the impact of training on promotora knowledge and skills, and measurement of promotora intervention competency after the initial training and again at six and 12 months into the intervention.
Training Methods
Promotora Selection
The MATCH study investigators partnered with a Community Based Organization (CBO) that trained promotoras for health promotion projects in the target communities. The study investigators negotiated an agreement with this CBO to train ten promotoras in diabetes knowledge and the MATCH self-management intervention skills. Under this agreement, the MATCH investigators would then select 3–5 of these promotoras to work with the MATCH intervention. This arrangement was mutually agreeable because the CBO was interested in additional training for their staff and the investigators sought the most capable promotoras to deliver the intervention. At the completion of the training, five promotoras (2.75 full-time equivalents) were selected to work on the MATCH project by two methods: 1) recommendation by the leadership of the CBO, and 2) performance during training as assessed by the investigators. Six months into the MATCH intervention, the CBO reorganized their promotora staff and two of the MATCH promotoras went to work on other projects, leaving three MATCH promotoras to cover the same amount of hours.
Promotora Training
The MATCH self-management intervention is delivered by promotoras over two years in the home of each participant. In anticipation of the challenges of such a highly intense, personal intervention, promotoras received 90 hours of initial training, followed by on-going supervision and training14. Of the original ten promotoras who participated in the MATCH training, eight of them were experienced promotoras, who had received training in the CBO around specific health and community issues, and had worked doing outreach and group education initiatives for anywhere from 6 months to ten years prior to MATCH. None of the promotoras had diabetes themselves, but all had some familiarity with the disease from families, friends, or prior community projects.
Initial Training
The initial MATCH promotora training consisted of a brief review of promotora practice, formal training on diabetes knowledge, and project-specific training on self-management and home visiting. The promotora practice training was not extensive, as most of those being trained had several years experience as promotoras. Table 1 lists the topics covered in the initial training.
Table 1.
MATCH Promotora Initial Training
| TOPIC | HOURS |
|---|---|
|
| |
| Midwest Latino Institute Diabetes Self Management Curriculum | 24 |
| Promotora Role | 9 |
| Relationships | 3 |
| Assessing Participants | 3 |
| Teaching Participants | 3 |
| Understanding Diabetes | 3 |
| Self Monitoring | 6 |
| Environmental Restructuring | 3 |
| Working with the Health Care Team: Medication Adherence | 3 |
| Social Support | 3 |
| Cognitive Skills | 6 |
| Overview of the Intervention; Curriculum review | 3 |
| Documentation and Supervision | 3 |
| Stress Management | 3 |
| Teaching the MATCH Intervention in the Home | 3 |
| Challenges in the Field: Problem Clients | 3 |
| Review | 3 |
| Role Play With Feedback From Group | 3 |
| Competency Evaluation | 3 |
|
| |
| TOTAL Initial Training Hours | 90 |
The diabetes education component of the curriculum was developed and taught by staff of the Midwest Latino Health Research, Training and Policy Center of the University of Illinois at Chicago. This training was based on the Diabetes Self Management Education Curriculum (Programa de Educación y Desarrollo de Destrezas sobre Diabetes [DEEP]), funded by the Division of Diabetes Translation of the Centers for Disease Control15, and was specifically designed for training promotoras. This curriculum, offered in Spanish, required 24 hours of face-to-face training, and culminated in a written test assessing knowledge of diabetes self-management. The curriculum was based upon the American Diabetes Association recommended elements for continuing care of diabetes. Promotoras were taught to use a home glucose monitor, interpret results, and understand the relationship between results and actions required based on results. All of the promotoras successfully completed the DEEP post-test prior to proceeding to the next phase of training.
All additional training was delivered by the MATCH research team which consisted of two physicians, a nurse, and a clinical psychologist. This training was conducted in Spanish, the native language of the promotoras and the majority of participants in the MATCH study. This initial training was based on adult learning theory16 and Freirean educational methods.17 Paulo Freire was the 20th century Brazilian educator credited with new methods of teaching and learning, or popular education. Key aspects of Freire's work include an emphasis on teaching and learning as an ongoing dialogue between the teacher and the learner. According to Freire, this dialogue involves respect and does not mean one person acting on another, but rather people working with each other. Second, Freire was concerned with praxis – informed action. For Freire, education is about deepening understanding, but also about making a difference in the world. Third, Freire defined the term conscientization, that is, to aim to have learners develop consciousness that has the power to transform reality. Fourth, Freire focused on situating educational activity in the lived experience of participants.17 For the instructors, this meant ongoing assessment of the promotoras' current knowledge and learning needs, and subsequent tailoring of the training to meet these needs. The training was designed to build on the life experiences of the promotoras in a way that was meaningful to them, with frequent bi-directional feedback between trainers and promotoras.
The MATCH-specific training was divided into morning and afternoon sessions. The mornings focused on application of diabetes information, and the afternoons focused on the self-management skills. A training manual provided written materials to accompany the didactic sessions. Promotoras were evaluated via post-tests for adequate level of knowledge, and an assessment of competence via role play, which documented increased skills, as well as areas for further training.
The self-management skills' training was based on work by Kate Lorig and colleagues, incorporating disease information (“what to do”) with skills (“how to do it”), which Lorig and colleagues contend is what distinguishes a traditional health promotion program from an effective self-management intervention18. The following section further describes Lorig's model as the basis for the MATCH self-management intervention.
Self-Management Program for Training
Lorig's Chronic Disease Self-Management Program (CDSMP)19 was influenced by the work of Corbin & Strauss20 who outlined three steps necessary for managing chronic illness: 1.) medical/behavioral management (e.g., regular use of glucometer, medication compliance), 2.) role management (e.g., adapting to limitations from illness, reassessing priorities), and 3.) emotional management (e.g., coping with depression, anger, fear of future). Lorig and colleagues argue that traditional health promotion programs may focus on one or two of these steps, but not all three concurrently18. Therefore, in order to systematically cover all three steps, Lorig proposed a model that includes five core self-management skills: problem solving, decision making, resource utilization, patient/doctor partnership, and taking action19. Learning techniques for applying these five core skills is the heart of Lorig's program. There is substantial evidence that supports the effectiveness of Lorig's model with use in people with arthritis21–27, asthma28, chronic pain29, diabetes30–31, and multiple chronic illnesses32–35. Evidence includes support for use in diverse cultures21,22,27, including use with Spanish speakers26, 30–31.
Lorig's model is based on the concept of self-efficacy37,39, the core component through which self-management skills are executed, leading to desired health outcomes. Self-efficacy is a cognitive behavioral concept that, in terms of self-management, is the individual's perception of confidence and ability to change a targeted behavior or behaviors for a specified goal, such as improved health. Lorig and colleagues argue that techniques used to teach the five core self-management skills in turn enhance an individual's self-efficacy. While it is most likely that there are other mechanisms involved, evidence supports the idea that self-efficacy is at least one mechanism related to self-management success and health outcomes25,36.
MATCH used a modified version of Lorig's five core self-management skills to enhance participants' self efficacy, with the goal of improving their diabetes self-management. The self-management skills used in MATCH included self-monitoring, environmental restructuring, social support, problem-solving/decision making, and stress management. MATCH investigators believed that self-efficacy needed to be enhanced in the promotoras themselves in order for them to be able to enhance self-efficacy in participants. Therefore, the training incorporated four components of self-efficacy enhancement39: interpretation of symptoms, modeling, social persuasion, and performance mastery.
Interpretation of symptoms begins first with knowledge of symptoms, followed by monitoring changes in those symptoms (self-monitoring), then interpreting and reinterpreting causes of symptoms, leading to the self-management skills of problem solving and decision-making. An example of the use of the skills of self-monitoring, problem solving and decision making used in training was that of a promotora trying to help a participant make healthier food decisions and thus recommending that he reduce the amount of tortillas consumed daily. The promotora teaches the participant to monitor how many tortillas he consumes in one day, as a baseline. The promotora then encourages the participant to set a goal of reducing tortilla intake by 1 or 2 a day in order to make the change a gradual one.
Another component to increase self-efficacy is modeling39. In the MATCH training, modeling was accomplished through a peer-trainer format. Training techniques included modeling the use of exploratory and guided discovery approaches, facilitating group discussions and self-reflection. Promotoras self-evaluated their work, their approach, etc., especially during the role plays where they were given the opportunity to observe peers modeling the use of self-management skills and then discuss feedback with the group.
A third component of self-efficacy enhancement is performance mastery39. When a person feels as though he/she accomplishes a goal, a sense of mastery is experienced. The more goals are accomplished, the greater the sense of mastery and subsequent self-efficacy. To obtain performance mastery, the investigators' trained the promotoras on the use of action planning. Action plans involve identifying one behavior the person would like to change, and developing a very specific plan to accomplish that change. Action plans are not the goal, but, rather, small steps towards that goal. Therefore, in order to increase the sense of mastery, action plans need to be specific, something the person wants to do, and small enough to be realistic and achievable within a short time-frame. After making the action plan, a self-efficacy question is used: “How confident are you that you can complete this action plan?” On a scale of 1 – 10, a rating of 7 and below indicates that the action plan is unrealistic and needs to be narrowed down to something feasible. Problem-solving and decision-making are the relevant self-management skills taught and reinforced with action planning.
The final component in self-efficacy enhancement is social persuasion39. The idea that a group can influence an individual is definitely not a new one, yet social support is often times not emphasized enough. In the case of the promotoras' training, group discussions on beliefs and values of health promotion and practice were an essential part of group cohesion. This cohesion fostered a group identity that, as a result of self-exploration, reflection, and commitment to their work, increased motivation to promote the self-management skills of social support and stress management for participants.
Ongoing Training
Ongoing training uses group and individual supervision. Every two weeks, promotoras and the MATCH research team meet for two hours to review the intervention protocol, answer promotora questions, and discuss specific participant/case issues. The group format allows promotoras to provide each other with practical and social support. In addition, the psychologist provides bimonthly individual consultation and supervision to each promotora, to reinforce the self-management skills.
Audio recordings of MATCH home visits have been conducted to document intervention fidelity and enhance the consistency of intervention delivery. The team psychologist reviews audio tapes in order to determine areas requiring additional support or training. Both group and individual sessions are facilitated using the exploratory and guided discovery approach for problem solving challenges, ranging from specific participant cases to personal promotora challenges impacting intervention implementation. When natural teaching opportunities occur, whether in group sessions focusing on specific participant cases or in individual sessions focusing on promotora-specific challenges, the clinical psychologist models and encourages use of self-management skills.
Evaluation Methods and Results
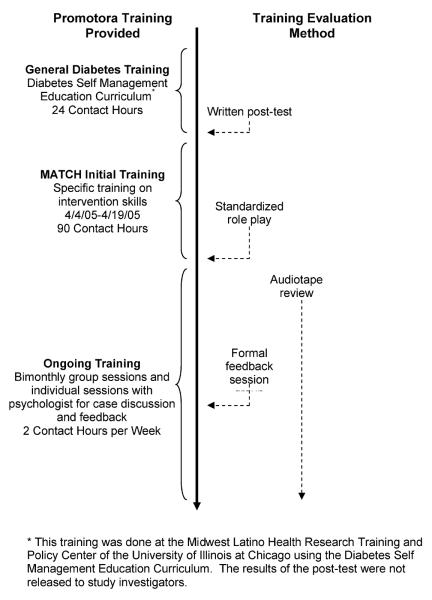
Study investigators evaluated the training process at three time points: during the initial training, immediately after the initial training, and during the ongoing training (the intervention phase) as shown in Figure 1. The evaluation methods were used to determine if desired outcomes were achieved, as well as to determine areas for improvement. While knowledge was evaluated in the specific diabetes training, the focus of the results presented here is on evaluating the acquisition and maintenance of skills for improving disease self-management in MATCH participants.
Figure 1.
Training and Evaluation Summary
At the completion of the initial training, promotora skill acquisition was evaluated by an assessment of competence via a standardized role play, which documented developing skills, as well as areas for further training. For this role play competence assessment, each promotora was given the same information about the client (played by one of the instructors.) The promotoras individually simulated a home visit with the client while other instructors watched. Promotora skills were evaluated by instructors using a 9-item review form (scores for each ranging from 1-lowest to 5-highest), based on the self management content and skills used in the intervention: accuracy of content, clarity of content, openness to participant questions, individualizing the content and process to participants, modeling and guiding self management skills for participants, checking for participant understanding of materials, encouraging participant action planning, asking for participant feedback, and overall interpersonal effectiveness.
The mean score on the role play evaluations for the promotoras after the initial training was 3.62 (range 2.44–4.27) with 5 being the highest score possible and 1 being the lowest. As shown in Table 2, at the conclusion of training the promotoras were skilled at interpersonal interaction and content accuracy, but needed further development in the areas of modeling and promoting participant self-management and action planning, and assessing participant understanding via asking for feedback.
Table 2.
Role Play Assessment of Promotora Competencies at the Completion of Initial Training, possible score range is 1 (lowest) to 5 (highest)
| Training Competencies | Mean* | Range |
|---|---|---|
| Accuracy of content | 3.8 | 2.8–4.8 |
| Clarity of content | 3.8 | 2.5–4.5 |
| Openness to questions | 3.7 | 2–4.5 |
| Individualizing the content and process | 3.7 | 2.5–4.5 |
| Model and guide | 3.3 | 2–4.3 |
| Check for participant understanding of material | 3.6 | 2.5–4.3 |
| Action | 3.3 | 2–4 |
| Asked for feedback | 3.3 | 2.3–4 |
| Interpersonal effectiveness | 4.3 | 2.8–4.8 |
| Promotora Total Score | 3.7 | 2.5–4.3 |
10 promotoras total
The study investigators moderated a formal feedback session with the remaining 3 study promotoras 18 months after the start of the intervention to ask about the usefulness of the initial training. Promotoras reported that the training was challenging and involved more material than they had ever had before. However, they indicated that they felt this was valuable. Promotora 1: “For me it was a lot of new information, information more professional than we had had.” They also said they refer back to the manual from the training frequently. Promotora 1: “…they are good for confirming certain topics like the “hook”. We can see it and it helps explain more clearly, with an example.” Promotora 3: “I read the parts about the medicines. I use the parts from Dr. Steve, I make copies to use.”
The self-management training was a new and challenging skill set for them. They felt the role plays were very useful. Promotora 2: “I remember a lot the role plays with the doctor.” Promotora 1 agreed that “Those helped a lot. Practicing was more important than a lot of information.” Over time, the promotoras expressed they found the action plan to be a useful tool. “Action plan is a word we never had before. We heard it a lot in the training. In reality, it is the correct word.” They said the training on self-management and diabetes made them feel more “professional”. They weren't just trained in general and then sent out to begin the intervention. They were given steps to use, and therefore felt more organized and confident.
Promotoras were asked what they thought about the usefulness of the supervision and bimonthly meetings. Demonstrating an increase in self-efficacy, Promotora 2 said “I didn't like idea of supervision at first, I felt there would be too much control over the visits, but then I saw usefulness from the feedback and not imposition from the supervision. For example, I was afraid at first to do prayers on the tape, but then when I got reassurance from [my supervisor], it helped me to feel more confident in what I do, in my work, rather than feel criticized.” Commenting on the usefulness of repetition and consistency, Promotora 1 said “I like that we review things we learned before” and Promotora 3 said “Continual connection with someone allowed for maintenance of visits and productivity.” Reflecting on their emotional needs and the personal intensity of the work, Promotora 2 commented “The meetings are a form of therapy.” Overall, the promotoras expressed that they found the training useful, and appreciated the ongoing review and assistance with problem solving with challenging clients.
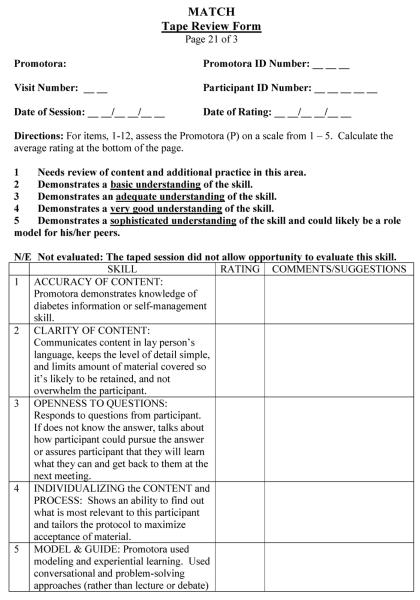
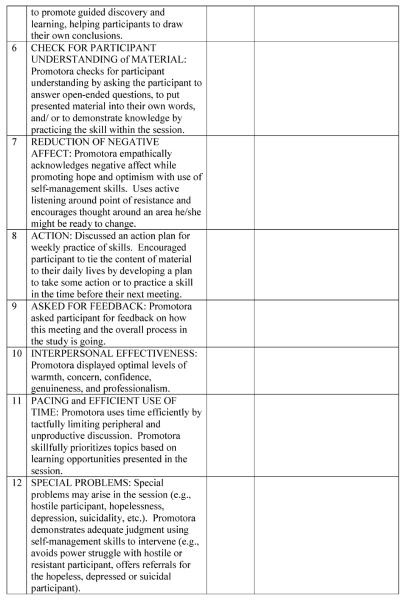
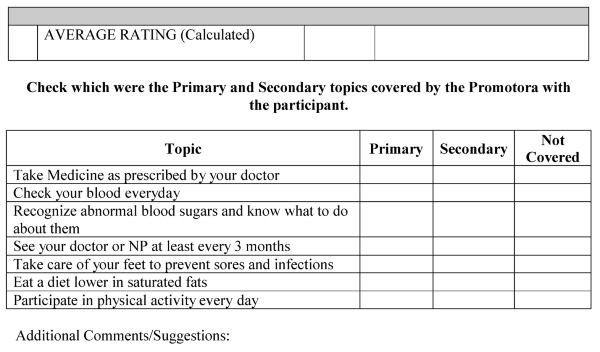
To ensure that promotoras maintained or improved intervention skills over time, promotora performance was assessed by the MATCH clinical psychologist for each promotora during a randomly selected 6-month and 12-month home visit, and compared to the promotora's first home visit using a modified version of the review form developed to evaluate the initial training role play performance. (Figure 2) Figure 3 shows outcomes in four of the key areas of assessment for the Promotora home visits: accuracy of content, individualizing content/intervention to participant, modeling and guiding of participants, and action planning with participants. These areas were identified by the research team as most critical to the intervention and in need of improvement based on the post-training role play assessment. In addition to presenting the changes in overall skill level for each promotora, these data assisted the psychologist in planning for the bimonthly educational sessions by indicating which skills need further development for the group as a whole, and for each individual promotora. Overall, the promotoras improved their performance on these intervention skills by 16–80% over the 12 month period.
Figure 2.
Role Play Evaluation Form
Figure 3.
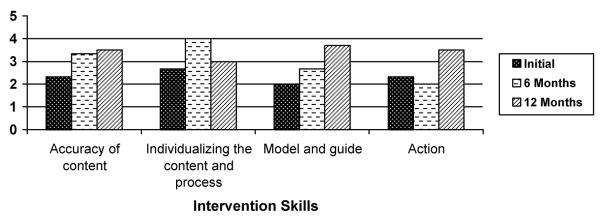
Promotora Improvements in Intervention Skills over Time as Assessed by Audiotape Review
Note: Scores of 3 promotoras are averaged for each value.
Discussion
Effectiveness of Overall Training
The initial promotora training for MATCH promoted effective intervention delivery. Promotoras completed the initial training with basic knowledge about diabetes and self-management, a manual as a resource, and opportunities to practice and improve the skills to be used in the MATCH intervention. The material in the training was at the correct level of difficulty, based on the promotoras self-report and evidence of their knowledge and skill mastery from the role play and audiotape reviews. It is worth noting that these were experienced promotoras who had functioned in other roles in their community (primarily as group education leaders). New trainees might need additional time to become comfortable with the promotora role, and develop confidence in working with community residents on health promotion and disease prevention strategies.
The ongoing training component of the MATCH project, although time intensive, has proven particularly useful. Continued instruction, supervision, and evaluation of promotora work are crucial to the success of promotora programs, but supervision linked to the continuing evaluation of promotora on-the-job performance has often been the most neglected phase of these programs.9,39 The bimonthly group and individual sessions with the promotoras, MATCH study investigators and team psychologist allow for assessment of intervention fidelity and help the promotoras further refine and practice their intervention delivery skills. The ongoing training provides the promotoras the opportunity to process the intervention experiences and address challenges as they arise. In addition, these sessions provide investigators an exclusive window into the actual intervention which allows them to hear the perceived challenges of participants and how the promotoras address them. This information will be essential to design and implement future promotora trainings and interventions.
Previous studies have shown that promotora interventions that incorporate self-management can improve diabetes outcomes, 40–42 yet there is no literature on how to train promotoras to teach these critical skills. The self-management material was a new skill set for these promotoras, which required additional time and practice to master. One of the challenges in the training was the translation of the self-management terms into Spanish. This translation was done jointly by the bilingual instructors and the promotoras, which ensured that the terms were being translated correctly in cultural terms, and gave the promotoras additional time to understand and become comfortable with each term, as they struggled to find the most appropriate translation. The same can be said for having the promotoras develop and share their own action plans, as a way of practicing and demonstrating knowledge of a critical skill they would use in the intervention. Finding ways to have the promotoras work with the skills and concepts throughout the training helped them to learn and implement the complex psychological concept of self-management. In addition, we note that the MATCH training involved a small number of promotoras. Study replication would be useful to see if training results can be replicated with a larger group.
The MATCH team also notes that the final evaluation of the MATCH training will be the impact of the promotora intervention on the MATCH participants. At this point in the study, we have data on promotora intervention delivery as judged by observation and role play. The MATCH study outcomes will document whether these promotora skills are effective at helping study participants better manage their diabetes.
Training Instructors
The inclusive design of the MATCH study allowed for there to be a variety of professionals involved in the training, both in development and implementation. The MATCH instructors included physicians, a nurse and a clinical psychologist. During the initial training, there were always two instructors in the class, and all training and role plays were done in Spanish. Two instructors at all times was a practice that had numerous positive consequences for the training outcomes, and the authors recommend this model for future trainings involving non-native English speakers. This staffing level allowed the instructors to assist each other with interpretation, language, content and assessment of skills. Training in the primary language was also a best practice for this group as concepts key to the training would have been very challenging to translate.
The diabetes content of the training was at a level that can be appropriately taught by a variety of health professionals. The promotora skills content needed a teacher with familiarity with the promotora model and their overall roles in the community. Similarly, the self-management content required someone very skilled in this area, and with experience teaching and modeling action planning to lay people. The clinical psychologist served this role both in the initial training and in the ongoing training where she currently is the direct supervisor of the promotoras. She continues to use every opportunity to reinforce and model the action plan technique and the overall self management skills.
The use of a psychologist to supervise the promotoras is expensive and unconventional—typically it is project coordinators who assist with documentation, scheduling, and job support. In MATCH however, the promotoras often brought personal concerns to the ongoing training sessions where the psychologist expressed empathy but also modeled self management and action planning methods for problem solving. Because the psychologist was so effective in using promotora questions as opportunities for learning, it is unclear whether the same level of promotora role competency would have been observed if they interacted primarily with a project coordinator to manage the intervention.
Implications
Several issues that arose during the MATCH intervention suggest additional training components for future work. In general, promotoras de salud are chosen to work with underserved and hard to reach populations because they live in the same communities and are familiar with the concerns of their neighbors 4–5. This definition, however, means that many promotoras face the same daily life challenges as their neighbors. These challenges make it difficult to concentrate on work when income, housing, legal status or other such issues loom in their lives. In MATCH, these issues were used to help the promotoras practice and fully understand the self-management skills they were teaching the study participants. While such training proved very valuable, both to the promotoras personally and to the MATCH intervention skills they developed, this process is time consuming.
A recent national survey44 of promotora training confirmed that promotora programs were becoming formalized across the country with training conducted both on the job and at the community college level, and several states have developed mechanisms for promotora certification. Promotoras have specific training and support needs that must be recognized40 as the profession grows and gains visibility. To improve the quality of the promotora performance and the initial training from which it stems, continual evaluation of promotoras must be built into the promotora program from the start.14 Overall, the MATCH experience confirmed for the investigators the importance of careful, documented training; and ongoing opportunities for assessment and improvement of skills, to ensure adherence to the intervention. Promotora programs and studies need to plan for a high level of training and support for the workers. Further study is needed on the cost of this support relative to the benefits of effective promotora interventions.
Acknowledgements
MATCH, and the work described here, would not have been possible without the efforts of promotoras Pilar Gonzalez, Susana Leon, Maria Sanchez, and the staff of Centro San Bonifacio.
This work was partially supported by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), #R01dk061289
References
- 1.Berman PA, Gwatkin DR, Burger SE. Community-based health workers: Head start or false start towards health for all? Soc Science Med. 1987;25(5):443–59. doi: 10.1016/0277-9536(87)90168-7. [DOI] [PubMed] [Google Scholar]
- 2.Center for Policy Alternatives . Community health workers – A leadership brief on preventive health programs. Nov, 1998. [Google Scholar]
- 3.Swider SM. Outcome effectiveness of community health workers: An integrative literature review. Public Health Nursing. 2002 Jan-Feb;19(1):11–20. doi: 10.1046/j.1525-1446.2002.19003.x. [DOI] [PubMed] [Google Scholar]
- 4.Rosenthal EL. The final report of the national community health advisor study. Annie E. Casey Foundation; Baltimore, MD: 1998. [Google Scholar]
- 5.U.S. Department of Health and Human Services Community health workers national workforce study. 2007
- 6.Han HR, Kim KB, Kim MT. Evaluation of the training of Korean community health workers for chronic disease management. Health Education Research. 2007 Aug;22(4):513–21. doi: 10.1093/her/cyl112. [DOI] [PubMed] [Google Scholar]
- 7.Kuhajda MC, Cornell CE, Brownstein JN, Littleton MA, Stalker VG, Bittner VA, Lewis CE, Raczynski JM. Training community health workers to reduce health disparities in Alabama's black belt: The pine apple heart disease and stroke project. Family Community Health. 2006 Apr-Jun;29(2):89–102. doi: 10.1097/00003727-200604000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Perez LM, Martinez J. Community health workers: Social justice and policy advocates for community health and well-being. Am J Public Health. 2008 Jan;98(1):11–4. doi: 10.2105/AJPH.2006.100842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hill-Briggs F, Batts-Turner M, Gary T, Brancati F, Hill M, Levine D, Bone L. Training Community Health Workers as Diabetes Educators for Urban African-Americans: Value Added Using Participatory Methods. Progress in Community Health Partnerships: Research, Education and Action. 2007 Summer;1.2:185–194. doi: 10.1353/cpr.2007.0008. [DOI] [PubMed] [Google Scholar]
- 10.Perez M, Findley SE, Mejia M, Martinez J. The impact of community health workers training and programs in New York City. Journal of Health Care for the Poor and Underserved. 2006;17:26. doi: 10.1353/hpu.2006.0011. [DOI] [PubMed] [Google Scholar]
- 11.Lewin SA, Dick J, Pond P, Zwarenstein M, Aja G, van Wyk B, Bosch-Capblanch X, Patrick M. Lay health workers in primary and community health care. Cochrane Database Syst Rev. 2005 Jan 25;1(1):CD004015. doi: 10.1002/14651858.CD004015.pub2. [DOI] [PubMed] [Google Scholar]
- 12.Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: A qualitative systematic review. American Journal of Preventive Med. 2007 Nov;33(5):418–27. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 13.Witmer A, Seifer SD, Finocchio L, Leslie J, O'Neil EH. Community health workers: Integral members of the health care work force. American Journal of Public Health. 1995 Aug;85(8 Pt 1):1055–8. doi: 10.2105/ajph.85.8_pt_1.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li VC, Goethals PR, Dorfman S. A global review of training of community health workers, 1983–84. International Quarterly of Community Health Education. 2006 – 2007;27(3):181–218. doi: 10.2190/IQ.27.3.b. [DOI] [PubMed] [Google Scholar]
- 15.Midwest Latino Health Research, Training and Policy Center . Diabetes Education Empowerment Program. University of Illinois at Chicago; Chicago, IL: 2002. [Google Scholar]
- 16.Knowles Malcolm S., Holton Elwood F., III, Swanson Richard A. The adult learner. the definitive classic in adult education and human resource development. 5th Edition ed. Gulf Publishing Company, Book Division; Houston, TX: 1998. [Google Scholar]
- 17.Freire P. Pedagogy of the oppressed. Continuum Books; New York: 2000. [Google Scholar]
- 18.Lorig K, Holman H. Self-management education: History, definition, outcomes, and mechanisms. Annals of Behavioral Medicine. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 19.Lorig K, Sobel D, Stewart A, Brown BW, Bandura A, Ritter P, Gonzalez V, Laurent D, Holman H. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: A randomized trial. Medical Care. 1999;37:5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Corbin J, Strauss A. Unending work and care: Managing chronic illness at home. Jossey-Bass; San Francisco: 1988. [Google Scholar]
- 21.Barlow J, Williams B, Wright C. Patient education for people with arthritis in rural communities: The UK experience. Patient Education Counsel. 2000;1451:1–10. doi: 10.1016/s0738-3991(00)00196-8. [DOI] [PubMed] [Google Scholar]
- 22.Chui D, Poon P, Lee E, Lau J. Self-management programme for rheumatoid arthritis in Hong Kong. British Journal of Therapy Rehabilitation 1998. 5:477–481. [Google Scholar]
- 23.Goeppinger J, Arthur M, Baglioni AJ, Brunk S, Brunner C. A re-examination of the effectiveness of self-care education for persons with arthritis. Arthritis & Rheumatism. 1989;32:706–716. doi: 10.1002/anr.1780320608. [DOI] [PubMed] [Google Scholar]
- 24.Lorig K, Lubeck D, Kraines R, Seleznick M, Holman H. Outcomes of self-help education for patients with arthritis. Arthritis and Rheumatism. 1985;28:680–685. doi: 10.1002/art.1780280612. [DOI] [PubMed] [Google Scholar]
- 25.Lorig K, Mazonson P, Holman H. Evidence suggesting that health education for self-management in patients with chronic arthritis has sustained health benefits while reducing health care costs. Arthritis & Rheumatism. 1983;36:439–446. doi: 10.1002/art.1780360403. [DOI] [PubMed] [Google Scholar]
- 26.Lorig K, Gonzalez V, Ritter P. Community-based Spanish language arthritis education program. A randomized trial. Medical Care. 1999;37:957–963. doi: 10.1097/00005650-199909000-00011. [DOI] [PubMed] [Google Scholar]
- 27.McGowan P, Green L. Arthritis self-management in native populations of British Columbia: An application of health promotion and participatory research principles in chronic disease control. Canadian Journal of Aging. 1995;14:201–212. [Google Scholar]
- 28.Gibson P, Powell H, Coughlan J, Wilson A, Abramson M, Haywood P, Bauman A, Hensley M, Walters E. Self-management education and regular practitioner review for adults with asthma. Cochrane Database of Systematic Reviews. 2003;1 doi: 10.1002/14651858.CD001117. [DOI] [PubMed] [Google Scholar]
- 29.Von Korff M, Moore J, Lorig K, Cherkin D, Saunders K, Gonzalez V, Laurent D, Rutter C, Comite F. A randomized trial of a lay person-led self-management group intervention for back pain patients in primary care. Spine. 1998;23:2608–2615. doi: 10.1097/00007632-199812010-00016. [DOI] [PubMed] [Google Scholar]
- 30.Lorig K, Ritter P, Jacquez A. Outcomes of border health Spanish/English chronic disease self-management programs. The Diabetes Educator. 2005;31:401–409. doi: 10.1177/0145721705276574. [DOI] [PubMed] [Google Scholar]
- 31.Lorig K, Ritter P, Villa F, Piette J. Spanish diabetes self-management with and without automated telephone reinforcement: Two randomized trials. Diabetes Care. 2008;31(3):408–414. doi: 10.2337/dc07-1313. [DOI] [PubMed] [Google Scholar]
- 32.Jerant A, Moore M, Lorig K, Franks P. Perceived control moderated the self-efficacy-enhancing effects of a chronic illness self-management intervention. Chronic Illness. 2008;4:173–182. doi: 10.1177/1742395308089057. [DOI] [PubMed] [Google Scholar]
- 33.Lorig K, Laurin J, Holman H. Arthritis self-management: a study of the effectiveness of patient education for the elderly. Gerontologist. 1984;24:455–457. doi: 10.1093/geront/24.5.455. [DOI] [PubMed] [Google Scholar]
- 34.Marks R, Allegrante J. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: Implications for health education practice (Part II) Health Promotion Practice. 2005;6(2):148–156. doi: 10.1177/1524839904266792. [DOI] [PubMed] [Google Scholar]
- 35.Marks R, Allegrante J, Lorig K. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: Implications for health education practice (Part I) Health Promotion Practice. 2005;6(1):37–43. doi: 10.1177/1524839904266790. [DOI] [PubMed] [Google Scholar]
- 36.Lorig K, Ung E, Chastain R, Shoor S, Holman H. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis & Rheumatism. 1989;32:37–44. doi: 10.1002/anr.1780320107. [DOI] [PubMed] [Google Scholar]
- 37.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychology Review. 1977 Mar;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 38.Bandura A. Social foundations of thought and action: A social cognitive theory. Prentice Hall; Englewood Cliffs, NJ: 1996. [Google Scholar]
- 39.Bandura A. Self-efficacy: The exercise of control. Freeman; New York: 1997. [Google Scholar]
- 40.McElmurry BJ, McCreary LL, Park CG, Ramos L, Martinez E, Parikh R, Kozik K, Fogelfeld L. Implementation, outcomes, and lessons learned from a collaborative primary health care program to improve diabetes care among urban Latino populations. Health Promotion Pract. 2008 Mar 14; doi: 10.1177/1524839907306406. [DOI] [PubMed] [Google Scholar]
- 41.Davis KL, O'Toole ML, Brownson CA, Llanos P, Fisher EB. Teaching how, not what: The contributions of community health workers to diabetes self-management. Diabetes Educator. 2007 Jun;33(Suppl 6):208S–15S. doi: 10.1177/0145721707304133. [DOI] [PubMed] [Google Scholar]
- 42.Liebman J, Heffernan D, Sarvela P. Establishing diabetes self-management in a community health center serving low-income Latinos. Diabetes Educator. 2007 Jun;33(Suppl 6):132S–8S. doi: 10.1177/0145721707304075. [DOI] [PubMed] [Google Scholar]
- 43.Thompson JR, Horton C, Flores C. Advancing diabetes self-management in the Mexican American population: A community health worker model in a primary care setting. Diabetes Educator. 2007 Jun;33(Suppl 6):159S–65S. doi: 10.1177/0145721707304077. [DOI] [PubMed] [Google Scholar]
- 44.Kash BA, May ML, Tai-Seale M. Community health worker training and certification programs in the United States: Findings from a national survey. Health Policy. 2007 Jan;80(1):32–42. doi: 10.1016/j.healthpol.2006.02.010. [DOI] [PubMed] [Google Scholar]