Abstract
Within the field of breast reconstruction there is increasing focus on patient-reported outcomes related to satisfaction, body image, and quality of life. These outcomes are deemed highly relevant because the primary goal of breast reconstruction is to recreate the appearance of a breast (or breasts) that is satisfying to the patient. Prominent researchers have suggested the need to develop improved standards for outcome evaluation which can ultimately benefit patients as well as physicians. The purpose of this article is to summarize key findings in the area of patient-reported outcomes for breast reconstruction and introduce a theoretical framework for advancing research in this field. We conducted an extensive literature review of outcome studies for breast reconstruction focusing on patient-reported results. We developed a theoretical framework illustrating core patient-reported outcomes related to breast reconstruction and factors associated with these outcomes. Our theoretical model highlights domains and distinguishing features of patient satisfaction, body image, and quality of life outcomes for women undergoing breast reconstruction. This model further identifies a broad range of variables (e.g., historical/premorbid influences, disease and treatment-related factors) that have been found to influence patient-reported outcomes and need to be taken into consideration when designing future research in this area. Additional attention is given to examining the relationship between patient reported outcomes and outside evaluation of breast reconstruction. Our proposed theoretical framework suggests key opportunities to expand research in this area with the goal of optimizing body image adjustment, satisfaction, and psychosocial outcomes for the individual patient.
Keywords: breast reconstruction, body image, patient satisfaction, quality of life
Assessing patient-reported outcomes in women undergoing breast reconstruction is highly relevant considering that the primary goal of this treatment is to recreate the appearance of a breast (or breasts) that is satisfying to the patient. Within this field, considerable attention has been given to evaluating the patient’s perspective as evidenced by the number of systematic reviews on patient-reported outcome measures1–6 and continued development and refinement of these tools.7–12
A significant challenge in reviewing this research is the variety and breadth of patient-reported outcomes pertinent to breast reconstruction, and inherent limitations in existing tools being used. These limitations include issues relevant to the content of questionnaires (i.e., degree to which they address disease- and treatment-specific variables) as well as psychometric properties (i.e., reliability, validity, and sensitivity to change). Others have suggested the need to transform the field to develop improved standards for outcome evaluation that will ultimately benefit patients and physicians.13 The goals of this article are to provide an overview of key findings related to patient-reported outcomes for breast reconstruction and introduce a theoretical framework for advancing research in this field.
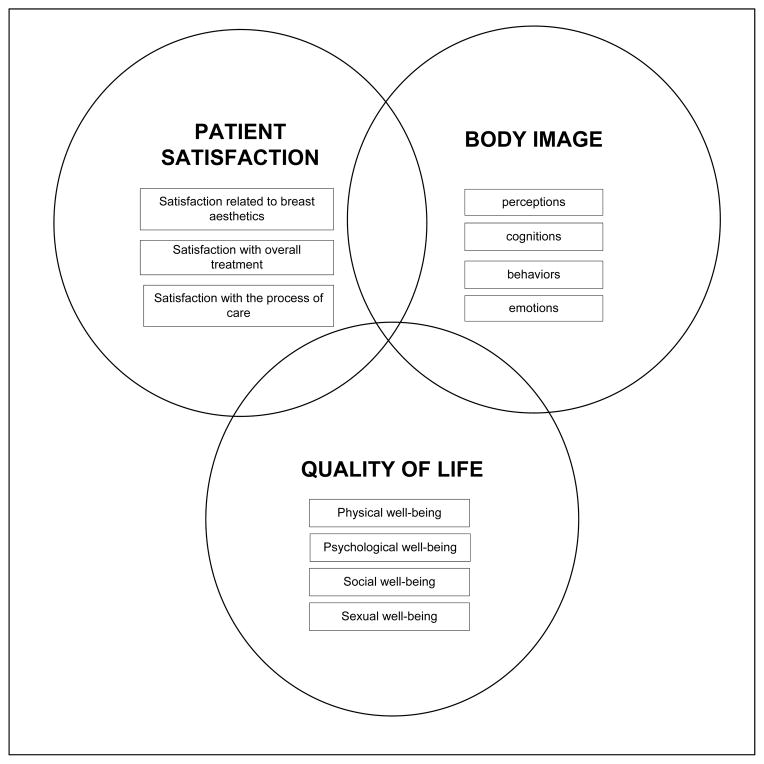
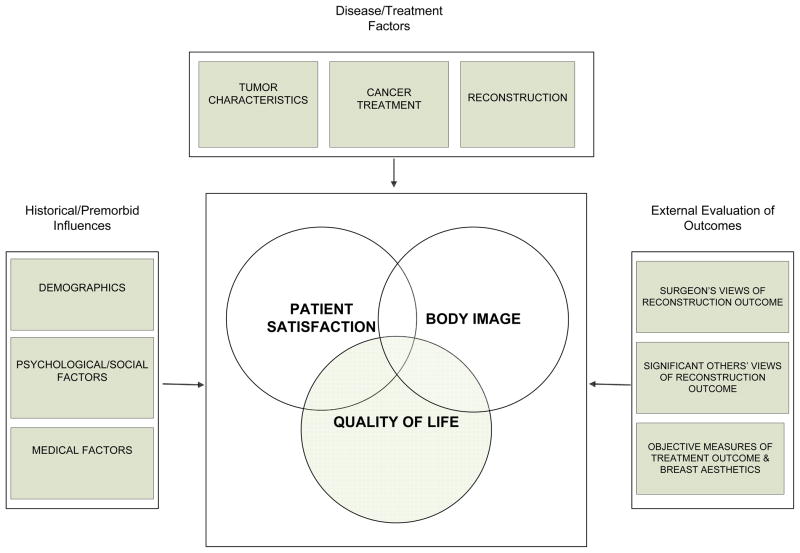
Our proposed theoretical framework is based on a biopsychosocial model which considers biological, psychological, and social factors and their complex interaction in understanding health, illness and healthcare delivery14,15 This approach recognizes that the relationship between mental and physical aspects of health is complex and considers it essential to evaluate the patient’s subjective experience alongside objective biomedical data. At the core of our framework are three central constructs considered essential for evaluating outcomes from breast reconstruction: patient satisfaction, body image, and quality of life. We initially focus on the primary role that patient satisfaction measures have played in outcomes research relevant to breast reconstruction. Although the construct of patient satisfaction is recognized as difficult to define,16,17 it is considered a basic source of feedback on the patient’s views of her treatment outcome as well as a broad indicator of quality of care. Body image is a multifaceted construct that refers to perceptions, thoughts, and feelings about the body and its functioning.18 We examine body image as a central factor in the evaluation of breast reconstruction, and discuss how body image measures can be used to facilitate psychosocial care. Finally, we consider quality of life which can be defined as the patient’s appraisal and perception of her overall health status.19 Quality of life has been extensively studied in women with breast cancer with consistent attention to aspects of psychosocial, physical, and sexual well-being.1,4,20
Developing an appreciation of the relationships among patient satisfaction, body image, and quality of life requires careful attention to the definition and distinguishing features of these constructs. There are significant challenges with reviewing the vast array of literature in this area, as relevant findings and basic information on the definition of these constructs span across multiple fields which include but are not limited to psychology, psychosocial oncology, nursing, public health, plastic surgery, and general medicine. Not surprisingly, there are numerous definitions offered which contributes to confusion and uncertainty regarding how to best distinguish these constructs from one another. Our theoretical framework is grounded by the notion that while these constructs overlap from a conceptual standpoint, each has multiple distinct dimensions which can be derived from the literature. Table 1 provides concise and commonly-accepted definitions for these constructs and identifies important distinguishing features of each construct. Figure 1 further outlines unique dimensions of patient satisfaction, body image, and quality life which are reviewed below. In this paper, we build upon this framework by delineating key variables associated with these patient-reported outcomes. Ultimately, we believe there are significant opportunities to expand research in this area with the goal of maximizing body image adjustment, patient satisfaction, and psychosocial outcomes for the individual patient.
Table 1.
Definitions and distinguishing features of patient satisfaction, body image, and quality of life outcomes.
| Construct | Definition | Issues Specific to Breast Reconstruction | Distinguishing Features |
|---|---|---|---|
| Patient Satisfaction | The patient’s overall evaluation of the quality of health care services received and degree to which treatment expectations were met | Efforts have been made to distinguish between satisfaction with aesthetic outcomes of the breast, with overall treatment outcome, and with the process of care | Focused on evaluating experiences tied specifically to health care Can serve as a broad indicator of quality of care as perceived by the patient |
| Body Image | A multifaceted construct that refers to the patient’s perceptions, cognitions, behaviors, and emotions related to the entire body and its functioning | Encompasses the range of bodily changes a woman with breast cancer may undergo prior to, during, and following reconstructive treatment | Focused exclusively on experiences tied to the body and its functioning Provides insight into the process of adaptation to bodily changes and identifies specific targets to guide psychosocial treatment |
| Quality of Life | The patient’s appraisal and perception of overall health status; basic elements of quality of life include evaluation of the patient’s perspective with regards to physical, psychological, and social well-being | Incorporates symptoms specific to breast cancer, cancer treatment, and reconstructive surgery that affect all domains of quality of life Sexual well-being is often incorporated as an added domain in disease-specific quality of life instruments for breast cancer patients |
The most wide-ranging patient reported outcome; encompasses nearly all aspects of a patient’s well-being |
Figure 1.
Conceptual Framework Illustrating Dimensions of Patient Satisfaction, Body Image and Quality of Life Outcomes for Women Undergoing Breast Reconstruction
Patient Satisfaction
Patient satisfaction is recognized as a legitimate and important healthcare goal, an integral part of high quality healthcare, and a necessary condition of effective care.21 Patient satisfaction measures have also been touted as a primary and useful source of feedback about healthcare services. Advantages of utilizing these measures include minimal cost, ease of administration, and ability to provide rapid feedback about the fulfillment of expectations related to treatment. An expanding knowledge base recognizes that many distinct dimensions of satisfaction can be defined.22,23 Within the field of breast reconstruction, efforts have been made to distinguish between satisfaction with outcome and satisfaction with care. The value of evaluating satisfaction related to overall outcome and satisfaction with specific breast features (e.g., size, shape, symmetry) has also been recognized.20 Additional research supports evaluating how patient-reported outcomes are influenced by satisfaction with various aspects of care during breast cancer treatment. Variables found to affect a wide range of patient-reported outcomes include degree of surgeon specialization, patient’s trust in their provider, and patient’s perceived involvement in the treatment decision making process.20,24–26
A number of problems have been identified with the use of, and overreliance on, patient satisfaction measures. Methodological issues involving uniformly high levels of satisfaction and limited variability in outcomes have led many researchers to criticize the sensitivity of these instruments and ability to provide useful information to remedy dissatisfaction.22,27,28 Significant concerns have also been raised about potential influences of social desirability, recall bias and response bias.21,22,29 Studies have indicated that wording of questions and timing of satisfaction surveys can differentially impact responses. Considerable differences have been found in satisfaction outcomes when utilizing negative descriptive statements as compared to positive statements,30 qualitative versus quantitative study designs23 or using unstructured compared with more direct questions22. With regards to the timing of surveys, outcomes are influenced by the time lag between use of services and evaluation of satisfaction.22
Body Image
Body image is a multidimensional construct that extends beyond the evaluation of an individual’s appearance,31 and encompasses a wide range of experiences tied to an individual’s body. This includes perceptions, cognitions, behaviors, and emotions related to the body and its functioning. It is widely accepted that body image experiences are entirely subjective, and as such are not necessarily reflective of objective reality. Many have argued that body image is strongly influenced by the degree to which an individual is invested in or places a high degree of importance on physical attributes (i.e., body image investment).32–34
It is important to recognize the range of bodily changes that a woman with breast cancer may undergo prior to, during the process of, and following treatment that can affect her psychosocial functioning.35. Body image tools can provide valuable and extremely useful information about the process of adaptation to bodily changes from breast reconstruction. More specifically, knowledge about the patient’s perceptions, thoughts, feelings, and behaviors tied to her appearance and bodily changes can be used as targets for psychosocial treatment to ameliorate dissatisfaction with treatment outcome and improve quality of life. Fingeret36 has reviewed a variety of empirically-supported treatment strategies for treating body image difficulties of cancer patients.
Within the oncology setting, a key barrier to conducting conceptually driven research in the area of body image has been the use of inconsistent, unclear or simplistic definitions of this construct.32,37 As discussed elsewhere, body image cannot be adequately captured with a single-item measure and extends well beyond satisfaction with appearance.32,36 Few body image instruments are specific to oncology populations, though many of these were developed for women with breast cancer or included breast cancer patients in their validation studies. Unfortunately, significant limitations with regards to the psychometric properties of many existing tools have been identified.31,32,37
Quality of Life
Our discussion of patient-reported outcomes relevant to breast reconstruction would not be complete without considering the broad construct of quality of life. Similar to patient satisfaction and body image, quality of life is recognized to be multidimensional in nature and entirely subjective. Quality of life outcomes, however, are extremely wide-ranging, and have been described as encompassing nearly all aspects of a patient’s well-being.38 Cella has argued that basic elements of quality of life assessment include evaluation of the patient’s perspective with regards to physical, psychological, and social well-being.19
Health-related quality of life refers more specifically to the extent to which one’s physical, emotional, and social well-being are affected by a medical condition or its treatment.39 The benefits of incorporating disease and treatment-related factors as part of an assessment of quality of life in medical populations have been widely recognized. In breast cancer patients, another aspect of quality of life routinely considered is sexual well-being. Difficulties with sexual functioning have been reported to be among the most common and distressing symptoms experienced by breast cancer survivors.35,40,41 Furthermore, problems with sexual functioning are less likely to resolve compared to other side effects of cancer treatment, persisting and potentially worsening into survivorship.35
Overview of Patient-Reported Outcomes Research in Breast Reconstruction
Considerable attention has been given to evaluating patient-reported outcomes based on the type of ablative breast surgery as well as timing and method of reconstruction. When comparing outcomes among treatment with breast conservation therapy (BCT), mastectomy, and mastectomy plus reconstruction, BCT patients generally report the highest levels of satisfaction with cosmetic results.42–44 Some research, however, suggests that those undergoing reconstructive procedures rate their cosmetic outcomes better than BCT45,46. When considering quality of life only, findings suggest women undergoing BCT may have comparable long-term outcomes to those undergoing mastectomy with immediate reconstruction.47 A more comprehensive review found limited differences between those with mastectomy versus mastectomy with reconstruction across a broad array of studies on measures of body image, sexuality, and quality of life.3
With regards to the timing of reconstruction, both immediate and delayed procedures have been found to provide substantial and lasting psychosocial benefits.48–50 Some research indicates that overall satisfaction and psychosocial well-being are higher among those with immediate as compared to delayed reconstruction.51 Many studies have found that method of reconstruction has a limited effect on psychosocial outcomes especially when this is considered over time and following completion of the reconstructive process.48,50,52 However, there are numerous reports of significant associations between procedure type and satisfaction rates, with autologous tissue-based procedures tending to have higher satisfaction rates than implant-based procedures.53–55
Other evaluations of patient-reported outcomes with breast reconstruction have focused on disease- and treatment-related factors such as the influence of concomitant therapies, complications, and the stage of reconstruction. Patients undergoing adjuvant radiation therapy tend to report significantly higher rates of reconstructive failure and complications and lower levels of satisfaction.56–58 Colakoglu et al59 found that although the development of a complication increased the overall odds of aesthetic dissatisfaction, patients undergoing prophylactic mastectomy and reconstruction were the most likely to be dissatisfied when complications occurred. Not surprisingly, satisfaction rates are also significantly affected by the stage of completion with the reconstructive process. Buck et al.60 found lower satisfaction with cosmesis during the initial stages of tissue-expander breast reconstruction, whereas maximal satisfaction was achieved after addition of the nipple and areola.
A considerable amount of research has examined the influence of obesity on reconstruction outcomes and resulting patient satisfaction. Obese patients present challenges with obtaining optimal cosmetic results following reconstruction due to well documented risks of higher complication rates as well as the general involvement of larger breast volumes and greater degree of ptosis.61,62 Although there have been few studies to date evaluating patient-reported outcomes based upon BMI, some research suggests there may be limited differences for obese patients as compared to normal-weight patients. Kulkarni et al found that patient satisfaction with surgical outcomes were similar across BMI categories, with obese patients more likely to receive an autologous reconstruction compared to an implant-based reconstruction.61 Similarly, Atisha et al found no differences in general satisfaction with outcome for either expander/implant or TRAM flap based on BMI.63 However, obese patients were found to have lower levels of aesthetic satisfaction with implant-based reconstruction as compared to normal weight patients
Variables outside the healthcare system, such as demographics, personality, and psychological traits also influence adjustment, satisfaction, and quality of life.23,64 Among demographic variables age is the most frequently considered and evaluated, with mixed findings. Alderman et al54 found that age was not significantly associated with overall or aesthetic satisfaction one year following reconstruction. In their retrospective study, Colakoglu et al59 found older age predicted dissatisfaction with reconstruction. By contrast, Harcourt et al65 found that younger age predicted declines in body image at 6 and 12 months after surgery among a mixed sample of women undergoing mastectomy with and without reconstruction.
With regards to psychological functioning, difficulties involving depressed mood, distress, and anxiety have been found to be predictive of decreased satisfaction with reconstructive outcomes.66,67 Associations among psychological functioning, body image outcomes, and patient-perceived aesthetic outcomes have also been demonstrated. For example, Harcourt et al found that higher levels of anxiety and depression predicted poorer body image scores at 6 months and 12 months after surgery.65 Nicholson et al found lower levels of depression and reduced self-consciousness about appearance were significantly related to cosmesis scores as rated by patients.45
Theoretical Framework to Facilitate Understanding of Patient-Reported Outcomes
Figure 2 expands our theoretical framework to highlight core patient-reported outcomes in the field of breast reconstruction and identifies numerous factors associated with these outcomes. This framework is intended to enhance understanding of the complex array of variables that can impact a patient’s psychosocial adjustment to breast reconstruction, and involves consideration of historical/premorbid influences, disease/treatment related factors, and external evaluation of outcomes. Further attention is given to delineating key variables within these broad categories that have been found to influence outcomes involving patient satisfaction, body image, and quality of life (see Table 2) Findings related to many of these key variables have been discussed above.
Figure 2.
Conceptual framework illustrating core patient-outcomes related to breast reconstruction and factors associated with these outcomes
Table 2.
Key Variables that May Influence Patient-Reported Outcomes Related to Breast Reconstruction
| Historical/Premorbid Influences | Disease/Treatment Related Factors |
|---|---|
| Demographics | Tumor Characteristics |
| Age | Cancer type |
| Socioeconomic status | Tumor stage |
| Ethnicity | Biomedical markers (BRCA) |
| Race | |
| Marital status | |
| Psychological/Social Factors | Cancer Treatment |
| Personality traits | Prophylaxis |
| Depression | Mastectomy |
| Anxiety | Radiation therapy |
| Social support | Chemotherapy |
| Coping style | Other |
| Medical factors | Reconstruction |
| Body mass index | Preoperative expectations |
| Comorbidities | Type of reconstruction |
| Smoking status | Timing of reconstruction |
| History of cosmetic procedures | Laterality |
| Previous breast surgery | Time point in process |
| Other | |
| Complications | |
| Pain |
Historical/Premorbid Influences
Historical factors and premorbid influences refer to attributes and past events that have a strong potential to influence how a women responds and adapts to bodily changes resulting from breast reconstruction. These influences can be considered within three broad subcategories reflecting demographic variables, psychological/social factors, and medical factors. With regards to demographic variables, numerous studies identify unique psychosocial experiences and challenges for women with breast cancer based upon age.68–71 A growing body of literature is focused on “the ethnic divide in breast reconstruction”.72 This work highlights issues with access to care based upon socioeconomic status and other demographic variables.72–74 Marital status and relationship satisfaction have been included in our model because of research identifying these as strong predictors of sexual functioning and psychological adjustment for women with breast cancer.40,69
Medical factors relevant to our model include body mass index (BMI), smoking status, comorbidities, and history of cosmetic procedures including previous breast surgery. BMI and smoking status were included based on research demonstrating that both significantly increase the odds of experiencing a complication with reconstruction.75–77 There is also a large body of literature linking BMI, smoking, and cosmetic surgery to body image outcomes in the general population.78 Further work reveals unique issues to consider when performing breast reconstruction in patients who have previously undergone augmentation.79 We have thus included previous breast surgery along with history of cosmetic procedures as potentially important variables for further study.
More recent attention has been given to identifying personality features that are significantly associated with quality of life in women undergoing breast reconstruction as well as psychological issues to consider for this patient population. Personality dimensions related to temperament and interpersonal style have been found to predict quality of life outcomes for women undergoing breast reconstruction.80 As previously discussed, there is a growing body of research dedicated to examining the psychological impact of breast reconstruction.45,65–67,81 This includes work demonstrating the significant influence that complications can have on psychological outcomes82 which further reinforces the importance of being able to provide psychological support and counseling to patients undergoing breast reconstruction. Two final psychosocial variables we consider are social support and coping style, due to a vast array of literature demonstrating the influential role of these variables on psychosocial adjustment to cancer83 and other disfiguring conditions.84,85 Coping styles are dynamic cognitive, emotional, and behavioral strategies to manage threats that are appraised as stressful.86 Within the context of breast cancer, various coping styles have been shown to predict outcomes such as psychological and physical adjustment87 and posttraumatic growth88.
Disease/Treatment Factors
Previous research suggests that when evaluated individually, certain disease and treatment-related factors may not have a strong relationship with patient-reported outcomes. However, findings are equivocal and one must consider the complex interplay between these factors and effects they may have on different dimensions of patient satisfaction, body image, and quality of life outcomes. Our proposed framework delineates a broad array of disease- and treatment-related variables that may impact a woman’s psychosocial adjustment to breast cancer (see Table 2). Cancer treatment and reconstruction factors given the most attention in the literature on patient-reported outcomes include type of ablative surgery (BCT versus total mastectomy), type and timing of reconstruction, stage of reconstruction, complications and radiation therapy as already discussed above. Additional research supporting the inclusion of other disease/treatment factors include studies demonstrating that nipple sparing mastectomy89,90, prophylactic procedures59,91,92, type of implant used57,93, laterality of reconstruction94, and expectations of surgery95 can significantly affect patient-reported outcomes. Although limited attention has been given to studying the effects of tumor characteristics on patient-reported outcomes, research suggests that patient education and counseling needs to be more targeted to enhance communication and alleviate unnecessary confusion and distress regarding prognosis.96
External Evaluation of Reconstruction Outcomes
Our theoretical framework further identifies the importance of considering the relationship between patient reported outcomes and external evaluation of breast reconstruction outcomes. This component reflects a key aspect of the biopsychosocial model in recognizing the benefit of evaluating the patient’s subjective experience alongside external data from experts, other observers, and objective outcomes. Numerous studies have found that patient’s assessments of aesthetic outcomes following breast reconstruction differ significantly from clinician’s assessments.97,98 Current methods used by physicians or other observers to assess breast reconstruction outcome typically involve rating breast aesthetics from photographs, digital images, or direct viewing of the patient. These methods are widely used in the field of breast reconstruction though they have been criticized for demonstrating low interrater and intrarater reliability and being susceptible to observer bias.98–100 Additionally, substantial variability has been found across studies with regards to what aspects of breast aesthetics are being evaluated.100 There is growing interest and attention to incorporating objective measures of reconstructive outcome, which typically involve conducting physical measurements of breast features. We found numerous studies reviewing information on developing technologies for quantifying surgical outcomes in the field of breast reconstruction.98,101–104 The growth of literature in this area is promising and reflects considerable opportunities for future research to develop a more sophisticated understanding of the relationship between patient’s subjective assessment of her reconstructive outcome as compared an external evaluation.
Discussion
Within the field of breast reconstruction, evaluating the patient’s perspective of her treatment outcome is of paramount importance. However, current approaches to examining patient-reported outcomes have been widely criticized as being of limited benefit and value.13,100 Three particular issues raised repeatedly in the literature are the lack of prospective randomized trials, lack of uniformity with regards to outcome measures being used, and poor quality of measures in terms of psychometric properties. In this paper, we synthesized research findings across the fields of plastic surgery, psychology, and psychosocial oncology, and presented a conceptual model to facilitate future advancements in the field of breast reconstruction pertinent to patient-reported outcomes. We consider this to be an introductory model that will benefit from further development and refinement with additional research. At the heart of our model are three fundamental constructs: patient satisfaction, body image and quality of life. Each of these is recognized to play a valuable and unique role in evaluating outcomes of breast reconstruction. Particular emphasis was placed on delineating clear and concise definitions of these constructs, discussing distinguishing features, and identifying additional issues with these constructs that are specific to the field of breast reconstruction (see Table 1). We believe this can provide a useful guide to reconstructive surgeons and others conducting research in this field who may not be as familiar with psychosocial outcomes.
When considering patient-reported outcomes for women undergoing breast reconstruction, it is of ultimate interest and value to understand how the patient adapts to bodily changes resulting from reconstructive treatment. This underscores the need to highlight and emphasize body image as a core outcome alongside patient satisfaction and quality of life. As seen in Table 1, a distinguishing feature of body image is that it is focused exclusively on experiences tied to the body and its functioning. The significance of body image has at times been overlooked in the breast reconstruction literature with some research failing to draw distinctions between body image and patient satisfaction outcomes, and other work only considering body image within the broader umbrella of quality of life outcomes. Body image tools have distinct advantages in providing information on how women adapt to bodily changes resulting from breast reconstruction. They can also provide specific targets to ameliorate dissatisfaction with treatment outcome. We seek to draw further attention to a rich and robust literature within the field of psychology illustrating the complex nature of body image and identifying particular attitudes, behaviors, emotions, and coping strategies which contribute to body image disturbance31,78 Research in this area encompasses medical populations with disfiguring conditions and attends to concepts involving body image investment (i.e., degree of importance placed on appearance)32,34 somatic/sensory awareness (i.e, attentiveness to bodily sensations),31 and bodily integrity (i.e., valuing one’s body as an intact and functional entity).105
Our conceptual framework illustrates significant overlap and interrelationships among patient satisfaction, body image, and quality of life. One way this model can be used in practice is to evaluate the nature of associations among these constructs to clarify the degree of overlap and establish empirically that each plays a unique role in evaluating outcomes of breast reconstruction. This will help to resolve any controversy as to whether body image stands alone or should be subsumed by the broader construct of quality of life. We offer preliminary evidence from work conducted with other cancer patients that associations between quality of life and body image outcomes are indeed significant (rs between −0.32 and −0.54) but not of a magnitude to indicate that are entirely overlapping.106 When considering key findings in the area of patient-reported outcomes for breast reconstruction, it is clear that a myriad of factors have been shown to influence a patient’s perspective on her reconstructive outcome and warrant consideration in future studies.. While many of these factors are tied specifically to breast cancer treatment and the reconstructive surgery process, others fall well outside this scope such as demographic characteristics and underlying personality/psychological features. Our conceptual framework is designed to raise awareness about the complex interplay of factors that can impact a patient’s psychosocial adjustment to breast reconstruction and facilitate further research to maximize adjustment. We offer a variety of different ways this framework could be used in a practical manner to help advance the field. Further work is needed to better understand which patients are at greatest risk for being dissatisfied with reconstructive outcome and experiencing poor body image and quality of life during and following treatment. One could also argue the need to consider which factors protect against adverse outcomes thereby promoting optimal psychosocial adjustment. The proposed framework can be used to aid in selection of variables to study/consider and has the benefit of providing greater structure and organization to research in this area. We fully intend for this model to evolve over time as future research is conducted. Specific attention must be paid to variables that are potentially modifiable and may therefore constitute the components of an intervention to improve outcomes. Additional focus should be given to factors that are unmodifiable as some of these may be indicators of patients who are more likely to benefit from particular types of intervention and support.
This framework can also be used to facilitate studies involving the development, delivery and effectiveness of interventions to facilitate psychosocial adjustment to breast reconstruction. Specific attention must be paid to determining the optimal timing of intervention delivery and to evaluating whether and how body image, patient satisfaction and quality of life may change throughout the course of reconstructive treatment. A key variable addressing this issue is time point in the reconstructive process. It would be particularly value to determine the degree to which this model is dynamic, and to understand how relationships among variables of interest change during the course of treatment and into long-term survivorship. Further work can investigate the tailoring of interventions based on factors in the model, and developing and testing novel intervention strategies targeting modifiable factors in the model.
Our framework also suggests a need to enhance research examining the relationship between patient-reported outcomes and objective evaluation of breast reconstruction. We currently do not have an adequate understanding of the potential disconnect between how a patient evaluates her outcome compared to how others view her reconstructive outcome. This disconnect has been studied more specifically between patients and healthcare providers, but there would be significant value to evaluating concordance between patient’s views and significant others’ views as this has implications for intimacy and marital functioning. Work is also needed to understand how the opinions and coping mechanisms of the significant other contribute in a positive or negative way to the patient satisfaction, body image, and quality of life. Future work must also entail examination of factors that impact the relationship between a patient’s views of her reconstructive outcome and more objective measures of reconstructive outcome. Further advancements in the field of quantifying oncologic surgical outcomes cannot be made unless these outcomes are examined in conjunction with the patient’s perspective
It is important to acknowledge and consider other conceptual models recognized in the literature that are of relevance to women’s psychosocial adjustment to breast reconstruction. Rumsey and colleagues have produced an extensive report of findings designed to investigate psychosocial factors and processes contributing to successful adjustment to disfiguring conditions.85 They present a conceptual model to explain the complex and multivariate nature of adjustment that can be applied to individuals with a range of disfiguring conditions, including cancer. Our framework is unique in that it specific to cancer patients undergoing breast reconstruction and incorporates a large number of disease and treatment-related variables. This Rumsey model shares many similar features with our conceptual framework with its inclusion of age and social support and its considerable focus on personality and psychological factors. The Rumsey model, however, offers insight into social and cognitive processes that help to explain adjustment to a broad spectrum of disfiguring conditions. Their findings reveal that optimism, feelings of social acceptance, satisfaction with social support, concerns about negative evaluation by others, salience and valence afforded to appearance-related information, and social comparison all play a strong and significant role in predicting adjustment to disfigurement. These are all variables to be considered in future research specifically with women undergoing breast reconstruction.
There are other conceptual models reported in the literature that contributed more directly to our framework, due to their exclusive focus on one of our main constructs of interest. These include Cash’s cognitive behavioral model of body image development,34 White’s heuristic cognitive behavioural model of body image disturbance among cancer patients,32 and Klassen and colleagues conceptual model of patient satisfaction and quality of life in breast surgery patients.20 Our model has distinct advantages of bringing together patient satisfaction, body image, and quality of life and delineating a wide range of additional factors that have been found to influence outcomes specifically for women undergoing breast reconstruction.
A key variable we include that is receiving increasing attention in the literature involves patient expectations for breast reconstruction. One group of researchers has conducted several qualitative studies to further examine the informational needs and expectations of patients undergoing different forms of breast surgery. Spector et al described many aspects of the postsurgical experience women felt they were not adequately prepared for by their healthcare providers which related to unexpected postoperative physical sensations and unanticipated outcomes.107 This study also identified specific information found helpful and unhelpful by women, and provides useful recommendations for healthcare providers with regards to preparing women both before and after breast surgery. Snell and colleagues used a similar study design to investigate preoperative expectations for women undergoing implant-based reconstruction.108 Comparable findings were reported such that patients often had unclear expectations regarding physical outcomes of the reconstructed breast. They also found more specific concerns regarding appearance outcomes with inaccurate expectations corresponding to dissatisfaction with final cosmetic results. Pusic and colleagues have developed a preliminary conceptual framework of patient expectations in breast reconstruction that identifies specific concerns of patients deemed important to address and further evaluate, which include appearance and outcome of the breasts, psychosocial impact, physical impact, and process of care and recovery.109 This work clearly identifies the importance of understanding and managing patient expectations for breast reconstruction, and recognizes the value of evaluating the relationship between expectations and patient-reported outcomes.
Conclusions
There are considerable opportunities to expand and improve research with patient-reported outcomes in the field of breast reconstruction. We introduce a theoretical framework based upon an extensive literature review of findings that span across the fields of psychology, psychosocial oncology, and plastic/reconstructive surgery. This framework is rooted in a biopsychosocial model highlighting the importance of the patient’s perspective of her outcomes and recognizes that the relationship between mental and physical aspects of heath is complex. Our framework has a number of advantages in that it is specific to breast reconstruction and can be used to help guide and structure multidisciplinary research. We offer a number of ways our framework can be used in practice. We did not specifically address the broader methodological issues in the field as many other review articles have focused on these problems and offered guidance in this arena.1–3,5,100 Ultimately, we believe our framework has important implications for developing and delivering psychosocial interventions to maximize satisfaction, body image, and quality of life. These interventions may be of particular value prior to beginning reconstruction to set and manage appropriate expectations for aesthetic outcome. However, targeted interventions to facilitate psychosocial adjustment during reconstructive treatment and into survivorship are also needed.
Acknowledgments
This research is supported in part by the MD Anderson Cancer Center Support Grant CA016672
Footnotes
Portions of this paper were presented at the Appearance Matters 5 Conference, Bristol, England, July 4, 2012
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Michelle Cororve Fingeret, Email: mcfinger@mdanderson.org, The University of Texas MD Anderson Cancer Center, 1515 Holcombe Blvd, Houston, TX 77030 (713) 563-8032 (phone), (713)794-4730 (fax)
Summer Nipomnick, Email: sumnip@yahoo.com, The University of Texas MD Anderson Cancer Center 1515 Holcombe Blvd, Houston, TX 77030 (713) 563-2605 (phone), (713)794-4730 (fax)
Melissa A. Crosby, Email: macrosby@mdanderson.org, The University of Texas MD Anderson Cancer Center, 1515 Holcombe Blvd, Houston, TX, 77030 (713) 794-1247 (phone), (713) 794-5492 (fax)
Gregory P. Reece, Email: greece@mdanderson.org, The University of Texas MD Anderson Cancer Center, 1515 Holcombe Blvd, Houston, TX, 77030 (713) 794-1247 (phone) (713) 794-5492 (fax)
References
- 1.Chen CM, Cano SJ, Klassen AF, et al. Measuring quality of life in oncologic breast surgery: a systematic review of patient-reported outcome measures. The breast journal. 2010;16:587–97. doi: 10.1111/j.1524-4741.2010.00983.x. [DOI] [PubMed] [Google Scholar]
- 2.Ching S, Thoma A, McCabe RE, Antony MM. Measuring outcomes in aesthetic surgery: a comprehensive review of the literature. Plast Reconstr Surg. 2003;111:469–80. doi: 10.1097/01.PRS.0000036041.67101.48. discussion 81–2. [DOI] [PubMed] [Google Scholar]
- 3.Lee C, Sunu C, Pignone M. Patient-reported outcomes of breast reconstruction after mastectomy: a systematic review. Journal of the American College of Surgeons. 2009;209:123–33. doi: 10.1016/j.jamcollsurg.2009.02.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pockaj BA, Degnim AC, Boughey JC, et al. Quality of life after breast cancer surgery: What have we learned and where should we go next? J Surg Oncol. 2009;99:447–55. doi: 10.1002/jso.21151. [DOI] [PubMed] [Google Scholar]
- 5.Pusic AL, Chen CM, Cano S, et al. Measuring quality of life in cosmetic and reconstructive breast surgery: a systematic review of patient-reported outcomes instruments. Plast Reconstr Surg. 2007;120:823–37. doi: 10.1097/01.prs.0000278162.82906.81. discussion 38–9. [DOI] [PubMed] [Google Scholar]
- 6.Winters ZE, Benson JR, Pusic AL. A systematic review of the clinical evidence to guide treatment recommendations in breast reconstruction based on patient- reported outcome measures and health-related quality of life. Ann Surg. 2010;252:929–42. doi: 10.1097/SLA.0b013e3181e623db. [DOI] [PubMed] [Google Scholar]
- 7.Anderson RC, Cunningham B, Tafesse E, Lenderking WR. Validation of the breast evaluation questionnaire for use with breast surgery patients. Plast Reconstr Surg. 2006;118:597–602. doi: 10.1097/01.prs.0000233040.82665.15. [DOI] [PubMed] [Google Scholar]
- 8.Baxter NN, Goodwin PJ, McLeod RS, Dion R, Devins G, Bombardier C. Reliability and validity of the body image after breast cancer questionnaire. The breast journal. 2006;12:221–32. doi: 10.1111/j.1075-122X.2006.00246.x. [DOI] [PubMed] [Google Scholar]
- 9.Dalton EJ, Rasmussen VN, Classen CC, et al. Sexual Adjustment and Body Image Scale (SABIS): a new measure for breast cancer patients. The breast journal. 2009;15:287–90. doi: 10.1111/j.1524-4741.2009.00718.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hopwood P, Fletcher I, Lee A, Al Ghazal S. A body image scale for use with cancer patients. Eur J Cancer. 2001;37:189–97. doi: 10.1016/s0959-8049(00)00353-1. [DOI] [PubMed] [Google Scholar]
- 11.Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, Cano SJ. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124:345–53. doi: 10.1097/PRS.0b013e3181aee807. [DOI] [PubMed] [Google Scholar]
- 12.Temple CL, Cook EF, Ross DC, Bettger-Hahn M, MacDermid J. Development of a breast reconstruction satisfaction questionnaire (BRECON): dimensionality and clinical importance of breast symptoms, donor site issues, patient expectations, and relationships. J Surg Oncol. 2010;101:209–16. doi: 10.1002/jso.21477. [DOI] [PubMed] [Google Scholar]
- 13.Morrow M, Pusic AL. Time for a new era in outcomes reporting for breast reconstruction. J Natl Cancer Inst. 2011;103:5–7. doi: 10.1093/jnci/djq471. [DOI] [PubMed] [Google Scholar]
- 14.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196:129–36. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 15.Borrell-Carrio F, Suchman AL, Epstein RM. The biopsychosocial model 25 years later: principles, practice, and scientific inquiry. Ann Fam Med. 2004;2:576–82. doi: 10.1370/afm.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Linder-Pelz SU. Toward a theory of patient satisfaction. Soc Sci Med. 1982;16:577–82. doi: 10.1016/0277-9536(82)90311-2. [DOI] [PubMed] [Google Scholar]
- 17.Sitzia J, Wood N. Patient satisfaction: a review of issues and concepts. Soc Sci Med. 1997;45:1829–43. doi: 10.1016/s0277-9536(97)00128-7. [DOI] [PubMed] [Google Scholar]
- 18.Pruzinsky T, Cash TF. Integrative themes in body-image development, deviance and change. In: Cash TF, Pruzinsky T, editors. Body Images: Development, Deviance and Change. New York: Guilford Press; 1990. [Google Scholar]
- 19.Cella D. Quality-of-life measurement in oncology. In: Baum A, Andersen BL, editors. Psychosocial Intervnetions for Cancer. Washington, D.C: American Psychological Association; 2001. pp. 57–76. [Google Scholar]
- 20.Klassen AF, Pusic AL, Scott A, Klok J, Cano SJ. Satisfaction and quality of life in women who undergo breast surgery: a qualitative study. BMC Womens Health. 2009;9:11. doi: 10.1186/1472-6874-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Avis M, Bond M, Arthur A. Satisfying solutions? A review of some unresolved issues in the measurement of patient satisfaction. Journal of advanced nursing. 1995;22:316–22. doi: 10.1046/j.1365-2648.1995.22020316.x. [DOI] [PubMed] [Google Scholar]
- 22.Carr-Hill RA. The measurement of patient satisfaction. J Public Health Med. 1992;14:236–49. [PubMed] [Google Scholar]
- 23.Williams B. Patient satisfaction: a valid concept? Soc Sci Med. 1994;38:509–16. doi: 10.1016/0277-9536(94)90247-x. [DOI] [PubMed] [Google Scholar]
- 24.Contant CM, van Wersch AM, Wiggers T, Wai RT, van Geel AN. Motivations, satisfaction, and information of immediate breast reconstruction following mastectomy. Patient Educ Couns. 2000;40:201–8. doi: 10.1016/s0738-3991(99)00078-6. [DOI] [PubMed] [Google Scholar]
- 25.Waljee JF, Hawley S, Alderman AK, Morrow M, Katz SJ. Patient satisfaction with treatment of breast cancer: does surgeon specialization matter? J Clin Oncol. 2007;25:3694–8. doi: 10.1200/JCO.2007.10.9272. [DOI] [PubMed] [Google Scholar]
- 26.Waljee JF, Hu ES, Newman LA, Alderman AK. Correlates of patient satisfaction and provider trust after breast-conserving surgery. Cancer. 2008;112:1679–87. doi: 10.1002/cncr.23351. [DOI] [PubMed] [Google Scholar]
- 27.Avis M, Bond M, Arthur A. Questioning patient satisfaction: An empirical investigation in two outpatient clinics. Social Science & Medicine. 1997;44:85–92. [Google Scholar]
- 28.Williams B, Coyle J, Healy D. The meaning of patient satisfaction: an explanation of high reported levels. Soc Sci Med. 1998;47:1351–9. doi: 10.1016/s0277-9536(98)00213-5. [DOI] [PubMed] [Google Scholar]
- 29.Mazor KM, Clauser BE, Field T, Yood RA, Gurwitz JH. A demonstration of the impact of response bias on the results of patient satisfaction surveys. Health Serv Res. 2002;37:1403–17. doi: 10.1111/1475-6773.11194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cohen G, Forbes J, Garraway M. Can different patient satisfaction survey methods yield consistent results? Comparison of three surveys BMJ. 1996;313:841–4. doi: 10.1136/bmj.313.7061.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pruzinsky T. Enhancing quality of life in medical populations: A vision for body image assessment and rehabilitation as standards of care. Body Image: An International Journal of Research. 2004;1:71–81. doi: 10.1016/S1740-1445(03)00010-X. [DOI] [PubMed] [Google Scholar]
- 32.White CA. Body image dimensions and cancer: a heuristic cognitive behavioural model. Psychooncology. 2000;9:183–92. doi: 10.1002/1099-1611(200005/06)9:3<183::aid-pon446>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 33.Cash TF, Labarge AS. Development of the Appearance Schemas Inventory: A new cognitive body-image assessment. Cognitive Therapy and Research. 1996;20:37–50. [Google Scholar]
- 34.Cash TF. Cognitive-behavioral perspectives on body image. In: Cash TF, Smolak L, editors. Body Image: A Handbook of Theory, Research, and Clinical Practice. New York: The Guilford Press; 2011. pp. 39–47. [Google Scholar]
- 35.Fingeret MC. Psychosocial Impact of Breast Cancer Treatment. In: Babiera G, FE, Skoracki R, editors. Advanced Therapy of Breast Disease. 3. Shelton, CT: People’s Medical Publishing House, USA; 2012. pp. 1289–304. [Google Scholar]
- 36.Fingeret MC. Body image and disfigurement. In: Duffy J, Valentine A, editors. MD Anderson Manual of Psychosocial Oncology. New York: McGraw Hill; 2010. pp. 271–88. [Google Scholar]
- 37.Annunziata MA, Giovannini L, Muzzatti B. Assessing the body image: relevance, application and instruments for oncological settings. Support Care Cancer. 2012;20:901–7. doi: 10.1007/s00520-011-1339-x. [DOI] [PubMed] [Google Scholar]
- 38.Velikova G, Stark D, Selby P. Quality of life instruments in oncology. Eur J Cancer. 1999;35:1571–80. doi: 10.1016/s0959-8049(99)00193-8. [DOI] [PubMed] [Google Scholar]
- 39.Cella DF. Measuring quality of life in palliative care. Semin Oncol. 1995;22:73–81. [PubMed] [Google Scholar]
- 40.Schover LR. The impact of breast cancer on sexuality, body image, and intimate relationships. CA Cancer J Clin. 1991;41:112–20. doi: 10.3322/canjclin.41.2.112. [DOI] [PubMed] [Google Scholar]
- 41.Ussher JM, Perz J, Gilbert E. Changes to Sexual Well-Being and Intimacy After Breast Cancer. Cancer Nurs. 2012 doi: 10.1097/NCC.0b013e3182395401. [DOI] [PubMed] [Google Scholar]
- 42.Al-Ghazal SK, Fallowfield L, Blamey RW. Comparison of psychological aspects and patient satisfaction following breast conserving surgery, simple mastectomy and breast reconstruction. Eur J Cancer. 2000;36:1938–43. doi: 10.1016/s0959-8049(00)00197-0. [DOI] [PubMed] [Google Scholar]
- 43.Hartl K, Janni W, Kastner R, et al. Impact of medical and demographic factors on long-term quality of life and body image of breast cancer patients. Ann Oncol. 2003;14:1064–71. doi: 10.1093/annonc/mdg289. [DOI] [PubMed] [Google Scholar]
- 44.Han J, Grothuesmann D, Neises M, Hille U, Hillemanns P. Quality of life and satisfaction after breast cancer operation. Arch Gynecol Obstet. 2010;282:75–82. doi: 10.1007/s00404-009-1302-y. [DOI] [PubMed] [Google Scholar]
- 45.Nicholson RM, Leinster S, Sassoon EM. A comparison of the cosmetic and psychological outcome of breast reconstruction, breast conserving surgery and mastectomy without reconstruction. Breast. 2007;16:396–410. doi: 10.1016/j.breast.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 46.Cocquyt VF, Blondeel PN, Depypere HT, et al. Better cosmetic results and comparable quality of life after skin-sparing mastectomy and immediate autologous breast reconstruction compared to breast conservative treatment. Br J Plast Surg. 2003;56:462–70. doi: 10.1016/s0007-1226(03)00198-x. [DOI] [PubMed] [Google Scholar]
- 47.Heneghan HM, Prichard RS, Lyons R, et al. Quality of life after immediate breast reconstruction and skin-sparing mastectomy - a comparison with patients undergoing breast conserving surgery. Eur J Surg Oncol. 2011;37:937–43. doi: 10.1016/j.ejso.2011.08.126. [DOI] [PubMed] [Google Scholar]
- 48.Atisha D, Alderman AK, Lowery JC, Kuhn LE, Davis J, Wilkins EG. Prospective analysis of long-term psychosocial outcomes in breast reconstruction: two-year postoperative results from the Michigan Breast Reconstruction Outcomes Study. Ann Surg. 2008;247:1019–28. doi: 10.1097/SLA.0b013e3181728a5c. [DOI] [PubMed] [Google Scholar]
- 49.Elder EE, Brandberg Y, Bjorklund T, et al. Quality of life and patient satisfaction in breast cancer patients after immediate breast reconstruction: a prospective study. Breast. 2005;14:201–8. doi: 10.1016/j.breast.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 50.Wilkins EG, Cederna PS, Lowery JC, et al. Prospective analysis of psychosocial outcomes in breast reconstruction: one-year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2000;106:1014–25. doi: 10.1097/00006534-200010000-00010. discussion 26–7. [DOI] [PubMed] [Google Scholar]
- 51.Al-Ghazal SK, Sully L, Fallowfield L, Blamey RW. The psychological impact of immediate rather than delayed breast reconstruction. Eur J Surg Oncol. 2000;26:17–9. doi: 10.1053/ejso.1999.0733. [DOI] [PubMed] [Google Scholar]
- 52.Nano MT, Gill PG, Kollias J, Bochner MA, Carter N, Winefield HR. Qualitative assessment of breast reconstruction in a specialist breast unit. ANZ J Surg. 2005;75:445–53. doi: 10.1111/j.1445-2197.2005.03388.x. discussion 371–2. [DOI] [PubMed] [Google Scholar]
- 53.Alderman AK, Kuhn LE, Lowery JC, Wilkins EG. Does patient satisfaction with breast reconstruction change over time? Two-year results of the Michigan Breast Reconstruction Outcomes Study. Journal of the American College of Surgeons. 2007;204:7–12. doi: 10.1016/j.jamcollsurg.2006.09.022. [DOI] [PubMed] [Google Scholar]
- 54.Alderman AK, Wilkins EG, Lowery JC, Kim M, Davis JA. Determinants of patient satisfaction in postmastectomy breast reconstruction. Plast Reconstr Surg. 2000;106:769–76. doi: 10.1097/00006534-200009040-00003. [DOI] [PubMed] [Google Scholar]
- 55.Saulis AS, Mustoe TA, Fine NA. A retrospective analysis of patient satisfaction with immediate postmastectomy breast reconstruction: comparison of three common procedures. Plast Reconstr Surg. 2007;119:1669–76. doi: 10.1097/01.prs.0000258827.21635.84. discussion 77–8. [DOI] [PubMed] [Google Scholar]
- 56.Cordeiro PG, Pusic AL, Disa JJ, McCormick B, VanZee K. Irradiation after immediate tissue expander/implant breast reconstruction: outcomes, complications, aesthetic results, and satisfaction among 156 patients. Plast Reconstr Surg. 2004;113:877–81. doi: 10.1097/01.prs.0000105689.84930.e5. [DOI] [PubMed] [Google Scholar]
- 57.McCarthy CM, Klassen AF, Cano SJ, et al. Patient satisfaction with postmastectomy breast reconstruction: a comparison of saline and silicone implants. Cancer. 2010;116:5584–91. doi: 10.1002/cncr.25552. [DOI] [PubMed] [Google Scholar]
- 58.Nava MB, Pennati AE, Lozza L, Spano A, Zambetti M, Catanuto G. Outcome of different timings of radiotherapy in implant-based breast reconstructions. Plast Reconstr Surg. 2011;128:353–9. doi: 10.1097/PRS.0b013e31821e6c10. [DOI] [PubMed] [Google Scholar]
- 59.Colakoglu S, Khansa I, Curtis MS, et al. Impact of complications on patient satisfaction in breast reconstruction. Plast Reconstr Surg. 2011;127:1428–36. doi: 10.1097/PRS.0b013e318208d0d4. [DOI] [PubMed] [Google Scholar]
- 60.Buck DW, 2nd, Shenaq D, Heyer K, Kato C, Kim JY. Patient-subjective cosmetic outcomes following the varying stages of tissue expander breast reconstruction: the importance of completion. Breast. 2010;19:521–6. doi: 10.1016/j.breast.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 61.Kulkarni AR, Katz S, Hamilton AS, Graff JJ, Alderman AK. Patterns of Use and Patient Satisfaction with Breast Reconstruction among Obese Patients: Results from a Population-Based Study. Plast Reconstr Surg. 2012;130:263–70. doi: 10.1097/PRS.0b013e3182589af7. [DOI] [PubMed] [Google Scholar]
- 62.Momeni A, Ahdoot MA, Kim RY, Leroux E, Galaiya DJ, Lee GK. Should we continue to consider obesity a relative contraindication for autologous microsurgical breast reconstruction? J Plast Reconstr Aesthet Surg. 2012;65:420–5. doi: 10.1016/j.bjps.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 63.Atisha DM, Alderman AK, Kuhn LE, Wilkins EG. The impact of obesity on patient satisfaction with breast reconstruction. Plast Reconstr Surg. 2008;121:1893–9. doi: 10.1097/PRS.0b013e3181715198. [DOI] [PubMed] [Google Scholar]
- 64.Sitzia J. How valid and reliable are patient satisfaction data? An analysis of 195 studies. Int J Qual Health Care. 1999;11:319–28. doi: 10.1093/intqhc/11.4.319. [DOI] [PubMed] [Google Scholar]
- 65.Harcourt DM, Rumsey NJ, Ambler NR, et al. The psychological effect of mastectomy with or without breast reconstruction: a prospective, multicenter study. Plast Reconstr Surg. 2003;111:1060–8. doi: 10.1097/01.PRS.0000046249.33122.76. [DOI] [PubMed] [Google Scholar]
- 66.Roth RS, Lowery JC, Davis J, Wilkins EG. Psychological factors predict patient satisfaction with postmastectomy breast reconstruction. Plast Reconstr Surg. 2007;119:2008–15. doi: 10.1097/01.prs.0000260584.09371.99. discussion 16–7. [DOI] [PubMed] [Google Scholar]
- 67.Brunault P, Suzanne I, Trzepidur-Edom M, et al. Depression is associated with some patient-perceived cosmetic changes, but not with radiotherapy-induced late toxicity, in long-term breast cancer survivors. Psychooncology. 2012 doi: 10.1002/pon.3038. [DOI] [PubMed] [Google Scholar]
- 68.Baucom DH, Porter LS, Kirby JS, Gremore TM, Keefe FJ. Psychosocial issues confronting young women with breast cancer. Breast disease. 2005;23:103–13. doi: 10.3233/bd-2006-23114. [DOI] [PubMed] [Google Scholar]
- 69.Fobair P, Stewart SL, Chang S, D’Onofrio C, Banks PJ, Bloom JR. Body image and sexual problems in young women with breast cancer. Psychooncology. 2006;15:579–94. doi: 10.1002/pon.991. [DOI] [PubMed] [Google Scholar]
- 70.Girotto JA, Schreiber J, Nahabedian MY. Breast reconstruction in the elderly: preserving excellent quality of life. Ann Plast Surg. 2003;50:572–8. doi: 10.1097/01.SAP.0000069064.68579.19. [DOI] [PubMed] [Google Scholar]
- 71.Ellsworth WA, Bass BL, Skoracki RJ, Heller L. Breast reconstruction in women under 30: a 10-year experience. The breast journal. 2011;17:18–23. doi: 10.1111/j.1524-4741.2010.01020.x. [DOI] [PubMed] [Google Scholar]
- 72.Nelson JA, Nelson P, Tchou J, Serletti JM, Wu LC. The ethnic divide in breast reconstruction: A review of the current literature and directions for future research. Cancer treatment reviews. 2012;38:362–7. doi: 10.1016/j.ctrv.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 73.Christian CK, Niland J, Edge SB, et al. A multi-institutional analysis of the socioeconomic determinants of breast reconstruction: a study of the National Comprehensive Cancer Network. Ann Surg. 2006;243:241–9. doi: 10.1097/01.sla.0000197738.63512.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chen JY, Malin J, Ganz PA, et al. Variation in physician-patient discussion of breast reconstruction. J Gen Intern Med. 2009;24:99–104. doi: 10.1007/s11606-008-0855-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chen CL, Shore AD, Johns R, Clark JM, Manahan M, Makary MA. The impact of obesity on breast surgery complications. Plast Reconstr Surg. 2011;128:395e–402e. doi: 10.1097/PRS.0b013e3182284c05. [DOI] [PubMed] [Google Scholar]
- 76.Chang DW, Reece GP, Wang B, et al. Effect of smoking on complications in patients undergoing free TRAM flap breast reconstruction. Plast Reconstr Surg. 2000;105:2374–80. doi: 10.1097/00006534-200006000-00010. [DOI] [PubMed] [Google Scholar]
- 77.Gritz ER, Fingeret MC, Vidrine DJ, Lazev AB, Mehta NV, Reece GP. Successes and failures of the teachable moment: smoking cessation in cancer patients. Cancer. 2006;106:17–27. doi: 10.1002/cncr.21598. [DOI] [PubMed] [Google Scholar]
- 78.Cash TF, Smolak L. Body image: A handbook of theory, research, & clinical practice. 2. New York: The Guilford Press; 2011. [Google Scholar]
- 79.Salgarello M, Rochira D, Barone-Adesi L, Farallo E. Immediate Breast Reconstruction After Skin- or Nipple-Sparing Mastectomy for Previously Augmented Patients: A Personal Technique. Aesthetic plastic surgery. 2011 doi: 10.1007/s00266-011-9809-6. [DOI] [PubMed] [Google Scholar]
- 80.Bellino S, Fenocchio M, Zizza M, Rocca G, Bogetti P, Bogetto F. Quality of life of patients who undergo breast reconstruction after mastectomy: effects of personality characteristics. Plast Reconstr Surg. 2011;127:10–7. doi: 10.1097/PRS.0b013e3181f956c0. [DOI] [PubMed] [Google Scholar]
- 81.Shridharani SM, Magarakis M, Manson PN, Rodriguez ED. Psychology of plastic and reconstructive surgery: a systematic clinical review. Plast Reconstr Surg. 2010;126:2243–51. doi: 10.1097/PRS.0b013e3181f445ae. [DOI] [PubMed] [Google Scholar]
- 82.Gopie JP, Timman R, Hilhorst MT, Hofer SO, Mureau MA, Tibben A. The short-term psychological impact of complications after breast reconstruction. Psychooncology. 2011 doi: 10.1002/pon.2089. [DOI] [PubMed] [Google Scholar]
- 83.Krishnasamy M. Social support and the patient with cancer: a consideration of the literature. Journal of advanced nursing. 1996;23:757–62. doi: 10.1111/j.1365-2648.1996.tb00048.x. [DOI] [PubMed] [Google Scholar]
- 84.Rumsey N, Harcourt D. The Psychology of Appearance. Berkshire: Open University Press; 2005. [Google Scholar]
- 85.Rumsey N, Byron-Daniel J, Charlton R, et al. Identifying the psychosocial factors and processes contributing to successful adjustment to disfiguring conditions. Bristol, England: Appearance Research Collaboration; 2008. [Google Scholar]
- 86.Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer Publishing Company; 1984. [Google Scholar]
- 87.Stanton AL, Danoff-Burg S, Cameron CL, et al. Emotionally expressive coping predicts psychological and physical adjustment to breast cancer. J Consult Clin Psychol. 2000;68:875–82. [PubMed] [Google Scholar]
- 88.Schroevers MJ, Teo I. The report of posttraumatic growth in Malaysian cancer patients: relationships with psychological distress and coping strategies. Psychooncology. 2008;17:1239–46. doi: 10.1002/pon.1366. [DOI] [PubMed] [Google Scholar]
- 89.Ueda S, Tamaki Y, Yano K, et al. Cosmetic outcome and patient satisfaction after skin-sparing mastectomy for breast cancer with immediate reconstruction of the breast. Surgery. 2008;143:414–25. doi: 10.1016/j.surg.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 90.Didier F, Radice D, Gandini S, et al. Does nipple preservation in mastectomy improve satisfaction with cosmetic results, psychological adjustment, body image and sexuality? Breast Cancer Res Treat. 2009;118:623–33. doi: 10.1007/s10549-008-0238-4. [DOI] [PubMed] [Google Scholar]
- 91.Fuller S, Anderson RC. Adjustment issues related to bilateral prophylactic mastectomy in women at elevated risk of developing breast cancer. Plast Surg Nurs. 2009;29:33–8. doi: 10.1097/PSN.0b013e31819970cc. [DOI] [PubMed] [Google Scholar]
- 92.den Heijer M, Seynaeve C, Timman R, et al. Body image and psychological distress after prophylactic mastectomy and breast reconstruction in genetically predisposed women: a prospective long-term follow-up study. Eur J Cancer. 2012;48:1263–8. doi: 10.1016/j.ejca.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 93.Macadam SA, Ho AL, Cook EF, Jr, Lennox PA, Pusic AL. Patient satisfaction and health-related quality of life following breast reconstruction: patient-reported outcomes among saline and silicone implant recipients. Plast Reconstr Surg. 2010;125:761–71. doi: 10.1097/PRS.0b013e3181cb5cf8. [DOI] [PubMed] [Google Scholar]
- 94.Craft RO, Colakoglu S, Curtis MS, et al. Patient satisfaction in unilateral and bilateral breast reconstruction [outcomes article] Plast Reconstr Surg. 2011;127:1417–24. doi: 10.1097/PRS.0b013e318208d12a. [DOI] [PubMed] [Google Scholar]
- 95.Abu-Nab Z, Grunfeld EA. Satisfaction with outcome and attitudes towards scarring among women undergoing breast reconstructive surgery. Patient Educ Couns. 2007;66:243–9. doi: 10.1016/j.pec.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 96.De Morgan S, Redman S, D’Este C, Rogers K. Knowledge, satisfaction with information, decisional conflict and psychological morbidity amongst women diagnosed with ductal carcinoma in situ (DCIS) Patient Educ Couns. 2011;84:62–8. doi: 10.1016/j.pec.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 97.Thomson HJ, Potter S, Greenwood RJ, et al. A prospective longitudinal study of cosmetic outcome in immediate latissimus dorsi breast reconstruction and the influence of radiotherapy. Ann Surg Oncol. 2008;15:1081–91. doi: 10.1245/s10434-007-9772-2. [DOI] [PubMed] [Google Scholar]
- 98.Kim MS, Sbalchiero JC, Reece GP, Miller MJ, Beahm EK, Markey MK. Assessment of breast aesthetics. Plast Reconstr Surg. 2008;121:186e–94e. doi: 10.1097/01.prs.0000304593.74672.b8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lowery JC, Wilkins EG, Kuzon WM, Davis JA. Evaluations of aesthetic results in breast reconstruction: an analysis of reliability. Ann Plast Surg. 1996;36:601–6. doi: 10.1097/00000637-199606000-00007. discussion 7. [DOI] [PubMed] [Google Scholar]
- 100.Potter S, Harcourt D, Cawthorn S, et al. Assessment of cosmesis after breast reconstruction surgery: a systematic review. Ann Surg Oncol. 2011;18:813–23. doi: 10.1245/s10434-010-1368-6. [DOI] [PubMed] [Google Scholar]
- 101.Dabeer M, Fingeret MC, Merchant F, Reece GP, Beahm EK, Markey MK. A research agenda for appearance changes due to breast cancer treatment. Breast Cancer: Basic and Clinical Research. 2008;2:1–3. doi: 10.4137/bcbcr.s784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Galdino GM, Nahabedian M, Chiaramonte M, Geng JZ, Klatsky S, Manson P. Clinical applications of three-dimensional photography in breast surgery. Plast Reconstr Surg. 2002;110:58–70. doi: 10.1097/00006534-200207000-00012. [DOI] [PubMed] [Google Scholar]
- 103.Liu C, Luan J, Mu L, Ji K. The role of three-dimensional scanning technique in evaluation of breast asymmetry in breast augmentation: a 100-case study. Plast Reconstr Surg. 2010;126:2125–32. doi: 10.1097/PRS.0b013e3181f46ec6. [DOI] [PubMed] [Google Scholar]
- 104.Udpa N, Sampat MP, Kim MS, Reece GP, Markey MK. Objective assessment of the aesthetic outcomes of breast cancer treatment: toward automatic localization of fiducial points on digital photographs. Proc SPIE. 2007:6514651420. [Google Scholar]
- 105.White CA. Body images in oncology. In: Cash TF, Pruzinsky T, editors. Body image: A handbook of theory, research & clinical practice. New York: The Guilford Press; 2002. pp. 379–86. [Google Scholar]
- 106.Fingeret MC, Yuan Y, Urbauer D, Weston J, Nipomnick S, Weber R. The nature and extent of body image concerns among surgically treated patients with head and neck cancer. Psychooncology. 2012;21:836–44. doi: 10.1002/pon.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Spector D, Mayer DK, Knafl K, Pusic A. Not what I expected: informational needs of women undergoing breast surgery. Plast Surg Nurs. 2010;30:70–4. doi: 10.1097/PSN.0b013e3181dee9a4. quiz 5–6. [DOI] [PubMed] [Google Scholar]
- 108.Snell L, McCarthy C, Klassen A, et al. Clarifying the expectations of patients undergoing implant breast reconstruction: a qualitative study. Plast Reconstr Surg. 2010;126:1825–30. doi: 10.1097/PRS.0b013e3181f44580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Pusic AL, Klassen AF, Snell L, et al. Measuring and managing patient expectations for breast reconstruction: impact on quality of life and patient satisfaction. Expert Rev Pharmacoecon Outcomes Res. 2012;12:149–58. doi: 10.1586/erp.11.105. [DOI] [PMC free article] [PubMed] [Google Scholar]