Abstract
Background
Rhodococcus equi is an important pathogen of foals. Enteral administration of live, virulent R. equi during early life has been documented to protect against subsequent intrabronchial challenge with R. equi, indicating that enteral mucosal immunization may be protective. Evidence exists that mucosal immune responses develop against both live and inactivated micro-organisms. The extent to which live or inactivated R. equi might alter the intestinal microbiome of foals is unknown. This is an important question because the intestinal microbiome of neonates of other species is known to change over time and to influence host development. To our knowledge, changes in the intestinal microbiome of foals during early life have not been reported. Thus, the purpose of this study was to determine whether age (during the first month of life) or administration of either live virulent R. equi (at a dose reported to protect foals against subsequent intrabronchial challenge, viz., 1×1010 colony forming units [CFU]) or inactivated virulent R. equi (at higher doses, viz., 2×1010 and 1×1011 [CFU]) altered the fecal microbiome of foals.
Methodology/Principal Findings
Fecal swab samples from 42 healthy foals after vaccination with low-dose inactivated R. equi (n = 9), high-dose inactivated R. equi (n = 10), live R. equi (n = 6), control with cholera toxin B (CTB, n = 9), and control without CTB (n = 8) were evaluated by 454-pyrosequencing of the 16S rRNA gene and by qPCR. No impact of treatment was observed among vaccinated foals; however, marked and significant differences in microbial communities and diversity were observed between foals at 30 days of age relative to 2 days of age.
Conclusions
The results suggest age-related changes in the fecal microbial population of healthy foals do occur, however, mucosal vaccination does not result in major changes of the fecal microbiome in foals.
Introduction
Rhodococcus equi is a facultative intracellular pathogen that primarily infects macrophages [1]. Although human beings may be infected (primarily those who are immunocompromised by HIV infection or immunosuppressive treatments), R. equi is most commonly recognized clinically as a leading cause of severe pneumonia in foals [1]–[4]. The disease occurs among foals worldwide [1]–[4]. Isolates that are virulent in foals bear a plasmid that encodes for a pathogenicity island, which includes the gene for the virulence-associated protein A (vapA); vapA is necessary but not sufficient to cause disease [5], [6].
Despite the global importance of the disease, an effective vaccine is lacking for control and prevention of R. equi pneumonia in foals. The lack of an effective vaccine is likely attributable to the complexity of immunity to R. equi [7]–[9], and the finding that foals appear to be infected very early in life [10], [11], when immune responses are naïve or deficient. It is generally accepted that a vaccine must be able to provide foals with protection against infection with R. equi during early life [5].
To date, the only vaccination strategy that has been demonstrated repeatedly to be effective for protecting against experimental intrabronchial challenge with virulent R. equi has been oral administration of live, virulent R. equi [12]–[14]. Protection against respiratory pathogens induced by oral vaccination also has been documented in mice [15]–[17], and evidence exists that bacillus Calmette-Guerin (BCG) administered orally is protective against tuberculosis in people and animals [18]–[20]. Moreover, inactivated bacteria and viruses also can elicit protective immune responses against systemic infections, including those of the respiratory tract [21]–[24]. Despite the success of oral administration of live organisms to protect foals against experimental challenge, very limited information is available regarding immune and other biological responses to the enteral route of vaccination.
One issue of importance with regard to enteral vaccination with live organisms is the impact of enteral administration of bacteria on the intestinal microbiome. This question might be particularly important for neonates. Although the microbiome of foals has not been systematically evaluated, evidence exists in other species, including humans, that the intestinal microbiome of neonates develops with age [25]–[27], and is linked to the functional development of the gut and gut immunity [25]–[29]. Thus, the purpose of the study reported here was to determine whether age-related changes in the microbiome occur in foals and whether age-associated changes are impacted by administration of either live virulent R. equi at a dose documented to protect foals against experimental challenge or 2 doses of inactivated virulent R. equi higher than the dose of live R. equi.
Materials and Methods
Ethics statement
All procedures for this study, including collection of rectal swab samples and enteral treatments/vaccinations, were reviewed and approved by the Texas A&M University Institutional Animal Care and Use Committee (protocol number AUP # 2011-124) and the Texas A&M University Institutional Biosafety Committee (permit number 20110183-Cohen). The foals used in this study are owned by Texas A&M University, and permission for their use was provided in compliance with the Institutional Animal Care and Use Committee procedures.
Animals and housing
Forty-two healthy Quarter Horse foals were used for this study. All foals were born healthy and had age-appropriate results of complete blood count (CBC) on day 2 of life, and adequate transfer of passive immunity as assessed by a commercially-available qualitative immunoassay for serum concentration of total IgG (SNAP Foal IgG test; IDEXX, Inc., Westbrook, ME). The foals were assigned into 1 of 5 experimental groups prior to birth (please see section on Vaccine Preparation and Treatment Groups below). All foals were monitored daily by Texas A&M University Horse Center staff for clinical signs of disease, and inspected at least twice weekly by a veterinarian for clinical signs of disease. All foals remained free of clinical signs of disease and in good health throughout the study.
Mare Diet
The respective dams were fed 6.4 kg per horse per day of a 13% horse pellet (crude protein: 13.5%; crude fat: 4.5%; crude fiber: 10%). Also, the foals and their mares were allowed free access to coastal Bermuda grass hay, plus grazing of pastures at the Texas A&M University Horse Center where the mares were maintained.
Vaccine Preparation and Treatment Groups
Rhodococcus equi strain EIDL 5-331, obtained from a Texas foal confirmed to have R. equi pneumonia, was used to prepare live and inactivated vaccines used for this project. Physiological saline (NaCl 0.9%) was used as a diluent to achieve the specified concentration of all vaccine preparations, as well as for the negative control. The vaccine was produced by inoculating blood agar plates with 1 colony forming unit (CFU) of R. equi strain 5-331 and incubating at 37°C for 48 hours. One colony from this pure culture was selected and used to inoculate 1,000 ml of brain heart infusion (BHI, Bacto™Brain Heart Infusion, BD Diagnostic Systems, Sparks, MD) broth. The flask with inoculated broth was placed on an orbital shaker (VWR OS-500, VWR, Radnor, PA) at 200 rpm for 24h at 37°C to allow bacterial growth. Isolates were repeatedly tested by PCR for the vapA gene to confirm that the isolates were virulent [30]. The bacterial culture was inactivated by electron-beam irradiation (irradiation dose between 3.5 and 5 kGy). After inactivation, the irradiated bacterial cells were plated out on BHI agar plates and incubated for 2 weeks at 37°C to confirm inactivation.
The number of foals in each group was determined a priori, and foals were assigned randomly to each of the groups. The study groups were as follows: 1) low-dose inactivated virulent R. equi group (n = 9), receiving 2×1010 CFUs of inactivated R. equi combined with 100 µg of cholera toxin subunit B (CTB, List Biological Laboratories, Campbell, CA) as a mucosal adjuvant, diluted in 100 ml of saline administered via nasogastric intubation; 2) high-dose inactivated virulent R. equi group (n = 10), receiving 1×1011 CFUs of inactivated R. equi with 100 µg of CTB diluted in 100 ml of saline via nasogastric intubation; 3) live virulent R. equi group (n = 6), receiving 1×1010 CFUs of live R. equi diluted in 100 ml of saline administered via nasogastric intubation; 4) control with CTB group (n = 9), receiving 100 µg of CTB diluted in 100 ml of saline via nasogastric intubation; and, 5) control without CTB group (n = 8), receiving 100 ml of saline via nasogastric intubation. Treatments (i.e., live bacteria, inactivated bacteria, and negative controls) were administered by nasogastric intubation to foals at 2, 9, 16, and 23 days of age.
Fecal swabbing
Rectal swabs were collected by inserting a 16-inch, cotton-tipped swab that was pre-moistened with 3 ml of sterile saline approximately 2 to 3 inches into the rectum, and swabbing the rectal mucosa circumferentially by rotating the swab. Once the cotton swab was removed, the cotton tip was separated from the handle using scissors and the tip was placed inside the barrel of a 35-ml catheter-tip syringe; the syringe plunger was used to squeeze the liquid from the swab tip, and the liquid was collected into a sterile tube. Fecal swab samples were collected on days 2 and 30 of life from foals in all groups. For 2 foals in the control group without CTB, fecal swab samples were collected on days 2, 9, 16, 23, 30, and 56 following birth. All fecal solutions were frozen at -80°C until processed.
Fecal DNA extraction
DNA was extracted by a bead-beating method using the ZR Fecal DNA MiniPrep Kit (Zymo Research Corporation) per the manufacturer’s instructions. The bead-beating step was performed using a homogenizer (FastPrep-24, MP Biomedicals) for 60 s at speed of 4 m/s.
Microbiome analysis
Bacterial tag-encoded FLX-titanium amplicon pyrosequencing (bTEFAP) was performed as described previously [31] based upon the V4-V6 region (E. coli position 530 – 1100) of the 16S rRNA gene, with primers forward 530F: GTGCCAGCMGCNGCGG and reverse 1100R: GGGTTNCGNTCGTTR.
Raw sequence data were screened, trimmed, filtered, de-noised, and chimera-depleted with default settings using the QIIME pipeline version 1.6.0 (http://qiime.sourceforge.net) and with USEARCH using the OTU pipeline (www.drive5.com). Operational taxonomic units (OTUs) were defined as sequences with at least 97% similarity using QIIME. For classification of sequences on a genus level the naïve Bayesian classifier within the Ribosomal Database Project (RDP, v10.28) was used [31].
The obtained data were compiled to determine the relative proportions of bacteria for each individual sample. The subsequent analysis was performed on a randomly selected subset of 1,300 sequences per sample to account for unequal sequencing depth across samples. Alpha diversity and beta diversity measures were calculated and plotted using QIIME. To determine differences in microbiota composition between the animal groups, the analysis of similarities (ANOSIM) function in the statistical software package PRIMER 6 (PRIMER-E Ltd., Lutton, UK) was used on the unweighted Unifrac distances matrices. This analysis measures the phylogenetic distance among bacterial communities in a phylogenetic tree, and thereby provides a measure of similarity among microbial communities present in different biological samples. The linear discriminant analysis (LDA) effect size (LEfSe) method was used to represent taxonomic relevant age-related differences in foal fecal swabs [32].
qPCR
To validate the pyrosequencing results, quantitative PCR (qPCR) assays were performed as described previously [33]. Briefly, EvaGreen-based reaction mixtures (total 10 µL) contained 5 µL of SsoFast™ EvaGreen® supermix (Biorad Laboratories), 2.2 µL of water, 0.4 µL of each primer (final concentration: 400 nM), and 2 µL of DNA (normalized to 5 ng/ul)). PCR conditions were 98°C for 2 min, and 40 cycles at 98°C 5 s, and 5 s at the optimized annealing temperature (Table 1). A melt curve analysis was performed for under the following conditions: beginning at 65°C, gradually increasing 0.5°C/5 s to 95°C with acquisition data every 5 s. The qPCR data was expressed as log amount of DNA (fg) for each particular bacterial group per 10 ng of isolated total DNA [34].
Table 1. Oligonucleotide primers/probes used for this study.
| qPCR primers/probe | Sequence (5′- 3′) | Target | Annealing (°C) | Reference |
| CFB555f | CCGGAWTYATTGGGTTTAAAGGG | Bacteroidetes | 60 | 56 |
| CFB968r | GGTAAGGTTCCTCGCGTA | |||
| Fuso-F | KGGGCTCAACMCMGTATTGCGT | Fusobacteria | 51 | 26 |
| Fuso-R | TCGCGTTAGCTTGGGCGCTG | |||
| 341-F | CCTACGGGAGGCAGCAGT | Universal Bacteria | 59 | 57 |
| 518-R | ATTACCGCGGCTGCTGG | |||
| EntF | CCCTTATTGTTAGTTGCCATCATT | Enterococcus | 61 | 58 |
| EntR | ACTCGTTGTACTTCCCATTGT | |||
| EcolRT_F | GTTAATACCTTTGCTCATTGA | E. coli | 55 | 59 |
| EcolRT R | ACCAGGGTATCTAATCCTGTT |
Data analysis
Pairwise comparisons between ages 2 days and 30 days were made at the levels of phylum, class, order, and family of bacteria for 2 outcomes: the observed percentage of sequences of bacteria at a given level, and the proportion of foals in which any amount of a given sequence for a given level was observed (i.e., the dichotomous outcome of whether or not a specific phylum [or class or order or family] was represented). The paired differences in percentages were compared using a Wilcoxon sign-rank test, and the paired proportions were compared using McNemar’s test. Because of the multiplicity of comparisons, P values at a given level (e.g., order) were adjusted using the method of Hochberg [35]. An adjusted P value <0.05 was considered significant for these analyses. Analyses were conducted using S-PLUS (Version 8.0; Insightful, Inc.) and R (Version 2.12.1; R Statistical Project). To assess the diversity of the GI microbiota, the Shannon-Weaver [36] and Chao 1 [37] diversity indices were calculated in QIIME.
Results
Sequence analysis
The 454-pyrosequencing pipeline yielded 499,419 quality sequences for the 42 samples analyzed. For technical reasons attributed to random error, 5 foals (2 foals from the control group without CTB, and 3 foals from the live R. equi group) did not generate sufficient sequences (cut-off value of 1,300 sequences) in at least 1 sample from 1 sampling time-point (either 2 or 30 days) by 454-pyrosequencing. Those foals were included in the descriptive analysis (Figures PCoA and rarefaction). For comparing age-related changes of the microbiome, however, the analysis was restricted to 37 foals with samples available from both collection time-points (2 and 30 days).
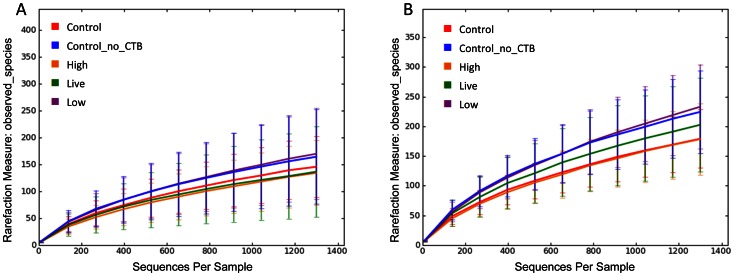
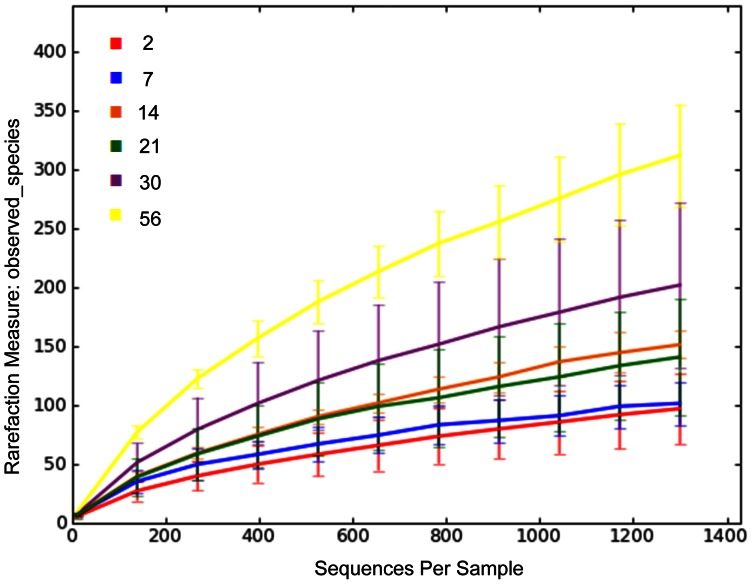
Across all vaccination groups and ages, sequences were classified into 18 phyla (Table 2 and 3). For the rarefaction curves of all vaccination groups (Figure 1A and 1B) and age groups (Figure 2), 1,300 sequences per sample yielded stable estimates of sample diversity.
Table 2. Median and range percentages of sequences represented in the fecal DNA of rectal swab samples from foals (Phylum, class, order, and family).
| Microbial Phylum/Class/Order/Family | 2-day-old foals (N = 37) | 30-day-old foals(N = 37) | P* | |||
| Archaea.Euryarchaeota | 0% (0%) | 0% (0 to 0.6%) | 0.0048 | |||
| Methanobacteria | 0% (0%) | 0% (0 to 0.3%) | 0.0280 | |||
| Methanobacteriales | 0% (0%) | 0% (0 to 0.3%) | 0.0924 | |||
| Methanobacteriacae | 0% (0%) | 0% (0 to 0.3%) | 0.1932 | |||
| Methanomicrobia | 0% (0%) | 0% (0 to 0.6%) | 0.1341 | |||
| Methanomicrobiales | 0% (0%) | 0% (0 to 0.6%) | 0.4321 | |||
| Methanocorpusculaceae | 0% (0%) | 0% (0 to 0.6%) | 0.9089 | |||
| Bacteria.Acidobacteria | 0% (0%) | 0% (0 to 0.2%) | 0.9515 | |||
| Acidobacteria | 0% (0%) | 0% (0 to 0.2%) | 1.0000 | |||
| Acidobacteriales | 0% (0%) | 0% (0 to 0.2%) | 1.0000 | |||
| Acidobacteriaceae | 0% (0%) | 0% (0 to 0.2%) | 1.0000 | |||
| Bacteria.Actinobacteria | 0.2% (0 to 4.1%) | 1.2% (0 to 4.3%) | 0.0048 | |||
| Actinobacteria | 0.2% (0 to 4.1%) | 1.2% (0 to 4.3%) | 0.0280 | |||
| Actinomycetales | 0.1% (0 to 3.4%) | 0.3% (0 to 2.8%) | 0.3904 | |||
| Bifidobacteriales | 0% (0 to 0.2%) | 0% (0 to 0.2%) | 1.0000 | |||
| Other | 0% (0 to 0.7%) | 0% (0 to 1.5%) | 1.0000 | |||
| Coriobacteridae (subclass) | 0% (0 to 1.5%) | 0.2% (0 to 2.7%) | <0.0001 | |||
| Coriobacteriales | 0% (0 to 1.5%) | 0.2% (0 to 2.7%) | 0.0080 | |||
| Rubrobacteridae (subclass) | 0% (0 to 0.7%) | 0% (0%) | 0.9515 | |||
| Rubrobacterales | 0% (0 to 0.7%) | 0% (0%) | 1.0000 | |||
| Other order | 0% (0%) | 0% (0 to 0.8%) | 0.0578 | |||
| Other family | 0% (0%) | 0% (0 to 0.8%) | 0.1190 | |||
| Bacteria.Bacteroidetes | 16.7% (0 to 85.5%) | 40.6% (0.2 to 87.8%) | 0.0066 | |||
| Bacteroidetes | 16.7% (0 to 85.4%) | 25.3% (0.1 to 80.5%) | 0.5376 | |||
| Bacteroidales | 16.7% (0 to 85.4%) | 25.3% (0.2 to 80.5%) | 0.9515 | |||
| Bacteroidieacae | 16.7% (0 to 85.3%) | 5.2% (0 to 53.3%) | 1.0000 | |||
| Porphyromonadaceae | 0% (0 to 9.0%) | 0.4% (0 to 16.4%) | 0.0080 | |||
| Prevotellaceae | 0% (0 to 1.5%) | 2.8% (0 to 63.1%) | <0.0001 | |||
| Rikenellaceae | 0% (0 to 10.2%) | 0% (0 to 5.8%) | 0.2108 | |||
| Other | 0% (0 to 0.2%) | 4.0% (0 to 18.0%) | <0.0001 | |||
| Flavobacteria | 0% (0 to 1.2%) | 0% (0 to 2.3%) | 0.8167 | |||
| Flavobacteriales | 0% (0 to 1.2%) | 0% (0 to 2.3%) | 1.0000 | |||
| Flavobacteriaceae | 0% (0 to 1.2%) | 0% (0 to 2.3%) | 1.0000 | |||
| Sphingobacteria | 0% (0 to 0.2%) | 0% (0 to 0.1%) | 0.8167 | |||
| Sphingobacteriales | 0% (0 to 0.2%) | 0% (0 to 0.1%) | 0.9515 | |||
| Crenotrichaceae | 0% (0 to 0.1%) | 0% (0%) | 1.0000 | |||
| Flexibacteriaceae | 0% (0%) | 0% (0 to 0.1%) | 1.0000 | |||
| Sphingobacteriaceae | 0% (0 to 0.2%) | 0% (0%) | 1.0000 | |||
| Other class | 0% (0 to 1.7%) | 5.5% (0 to 48.1%) | <0.0001 | |||
| Other order | 0% (0 to 1.7%) | 5.5% (0 to 48.1%) | <0.0001 | |||
| Other family | 0% (0 to 1.7%) | 5.5% (0 to 48.1%) | <0.0001 | |||
| Bacteria.Chlamydiae | 0% (0%) | 0% (0 to 30.1%) | <0.0001 | |||
| Chlamydiae | 0% (0%) | 0% (0 to 30.1%) | <0.0001 | |||
| Chlamydiales | 0% (0%) | 0% (0 to 30.1%) | <0.0001 | |||
| Chlamydiaceae | 0% (0%) | 0.1% (0 to 30.1%) | <0.0001 | |||
| Parachlamydiaceae | 0% (0%) | 0% (0 to 0.1%) | 1.0000 | |||
| Bacteria.Chloroflexi | 0% (0%) | 0% (0 to 0.2%) | 0.0441 | |||
| Anaerolineae | 0% (0%) | 0% (0 to 0.2%) | 0.2254 | |||
| Caldilineae | 0% (0%) | 0% (0 to 0.2%) | 0.9515 | |||
| Caldilineales | 0% (0%) | 0% (0 to 0.2%) | 1.0000 | |||
| Other | 0% (0%) | 0% (0 to 0.2%) | 0.2635 | |||
| Other family | 0% (0%) | 0% (0 to 0.2%) | 0.5355 | |||
| Bacteria.Cyanobacteria | 0% (0%) | 0% (0 to 0.1%) | 0.9515 | |||
| Cyanobacteria | 0% (0%) | 0% (0 to 0.1%) | 1.0000 | |||
| Other order | 0% (0%) | 0% (0 to 0.1%) | 1.0000 | |||
| Other family | 0% (0%) | 0% (0 to 0.1%) | 1.0000 | |||
| Bacteria.Deferribacteres | 0% (0% to 0.2%) | 0% (0 to 0.2%) | 0.9515 | |||
| Deferribacteres | 0% (0% to 0.2%) | 0% (0 to 0.2%) | 1.0000 | |||
| Deferribacterales | 0% (0% to 0.2%) | 0% (0 to 0.2%) | 1.0000 | |||
| Deferribacteraceae | 0% (0%) | 0% (0%) | NP | |||
| Incertae sedis 3 | 0% (0 to 0.2%) | 0% (0 to 0.2%) | 1.0000 | |||
| Bacteria.Fibrobacteres | 0% (0%) | 0% (0 to 0.7%) | 0.2104 | |||
| Fibrobacteres | 0% (0% to 0.2%) | 0% (0 to 0.7%) | 0.4698 | |||
| Fibrobacterales | 0% (0% to 0.2%) | 0% (0 to 0.7%) | 0.9515 | |||
| Fibrobacteraceae | 0% (0% to 0.2%) | 0% (0 to 0.7%) | 1.0000 | |||
| Bacteria.Firmicutes | 40.4% (5.8 to 69.2%) | 23.3% (4.4 to 95.2%) | 0.9515 | |||
| Bacilli | 4.8% (0.5 to 32.2%) | 2.4% (0.1 to 78.8%) | 0.2254 | |||
| Lactobacillales | 4.8% (0.5 to 32.2%) | 2.2% (0.1 to 69.8%) | 0.6264 | |||
| Aerococcaceae | 0% (0 to 1.6%) | 0% (0 to 1.1%) | 1.0000 | |||
| Carnobacteriaceae | 0% (0 to 0.2%) | 0% (0 to 0.1%) | 1.0000 | |||
| Enterococcaceae | 1.2% (0 to 14.5%) | 0% (0 to 65.0%) | 0.0080 | |||
| Lactobacillaceae | 0% (0 to 7.9%) | 0% (0 to 5.6%) | 0.0281 | |||
| Leuconostocaceae | 0% (0 to 0.2%) | 0% (0%) | 1.0000 | |||
| Streptococcaceae | 2.1% (0 to 31.2%) | 1.6% (0 to 20.8%) | 1.0000 | |||
| Other | 0.2% (0 to 1.7%) | 0% (0 to 3.8%) | 0.0234 | |||
| Bacillales | 0% (0 to 0.3%) | 0% (0 to 0.8%) | 0.9515 | |||
| Paenibacillaceae | 0% (0 to 0.2%) | 0% (0 to 0.2%) | 1.0000 | |||
| Staphylococcaceae | 0% (0 to 2.5%) | 0.1% (0 to 8.2%) | 1.0000 | |||
| Bacillaceae | 0% (0 to 0.3%) | 0% (0 to 0.1%) | 1.0000 | |||
| Incertae Sedis XI | 0% (0 to 0.2%) | 0% (0 to 0.1%) | 1.0000 | |||
| Planococcaceae | 0% (0%) | 0% (0 to 0.2%) | 1.0000 | |||
| Other | 0% (0 to 0.2%) | 0% (0 to 0.2%) | 1.0000 | |||
| Other order | 0% (0 to 0.1%) | 0% (0 to 0.5%) | 0.9515 | |||
| Other family | 0% (0 to 0.1%) | 0% (0 to 0.5%) | 1.0000 | |||
| Clostridia | 30.1% (3.4 to 64.5%) | 18.8% (3.6 to 82.5%) | 0.1314 | |||
| Clostridiales | 30.1% (3.4 to 64.5%) | 29.5% (3.4 to 64.5%) | 0.9515 | |||
| Eubacteriaceae | 0% (0 to 2.2%) | 0% (0 to 1.2%) | 0.3839 | |||
| Lachnospiraceae | 3.7% (0 to 55.5%) | 5.6% (0.7 to 76.7%) | 1.0000 | |||
| Peptostreptococcaceae | 3.4% (0 to 20.1%) | 0% (0 to 12.4%) | <0.0001 | |||
| Ruminococcaceae | 0.2% (0 to 4.6%) | 1.5% (0.1 to 18.5%) | <0.0001 | |||
| Clostridiaceae | 7.1% (0.1 to 45.2%) | 5.4% (0 to 19.0%) | 0.0080 | |||
| Incertae Sedis XI | 0% (0 to 1.1%) | 1.2% (0 to 14.0%) | <0.0001 | |||
| Incertae Sedis XIII | 0% (0 to 0.8%) | 0.1% (0 to 5.8%) | 0.0080 | |||
| Peptococcaceae | 0% (0%) | 0% (0 to 2.5%) | 0.0438 | |||
| Veillonellaceae | 0% (0 to 8.3%) | 0.9% (0 to 3.5%) | <0.0001 | |||
| Other | 3.1% (0.1 to 13.7%) | 2.0% (0 to 16.5%) | 1.0000 | |||
| Other order | 0% (0 to 0.4%) | 0.2% (0 to 23.5%) | 0.0190 | |||
| Other family | 0% (0 to 0.4%) | 0.2% (0 to 23.5%) | 0.0375 | |||
| Erysipelotrichi | 0.1% (0 to 1.0%) | 0.1% (0 to 2%) | 0.5376 | |||
| Erysipelotrichales | 0.1% (0 to 1.0%) | 0.1% (0 to 2%) | 0.4844 | |||
| Erysipelotrichiaceae | 0.1% (0 to 1.0%) | 0.1% (0 to 2%) | 1.0000 | |||
| Other class | 0% (0 to 0.5%) | 0.3% (0 to 6.5%) | <0.0001 | |||
| Other order | 0% (0 to 0.5%) | 0.3% (0 to 6.5%) | <0.0001 | |||
| Other family | 0% (0 to 0.5%) | 0.3% (0 to 6.5%) | <0.0001 | |||
| Bacteria.Fusobacteria | 0.8% (0 to 45.5%) | 0.8% (0 to 42.5%) | 0.9510 | |||
| Fusobacteria | 0.8% (0 to 45.5%) | 0.8% (0 to 42.2%) | 1.0000 | |||
| Fusobacteriales | 0.8% (0 to 45.5%) | 0.8% (0 to 42.2%) | 1.0000 | |||
| Fusobacteriaceae | 0.4% (0 to 45.3%) | 0.8% (0 to 42.2%) | 1.0000 | |||
| Incertae sedis 11 | 0% (0 to 0.2%) | 0% (0%) | 1.0000 | |||
| Other | 0% (0 to 16.1%) | 0% (0 to 1.0%) | 1.0000 | |||
| Bacteria.Lentisphaerae | 0% (0%) | 0% (0%) | NP | |||
| Lentisphaerae | 0% (0%) | 0% (0%) | NP | |||
| Victivallales | 0% (0%) | 0% (0%) | NP | |||
| Victivallaceae | 0% (0%) | 0% (0%) | NP | |||
| Bacteria. Other | 0.2% (0 to 8.1%) | 4.6% (0.2 to 68.5%) | <0.0001 | |||
| Bacteria. Other Class | 0.2% (0 to 8.1%) | 4.6% (0.2 to 68.5%) | <0.0001 | |||
| Other Order | 0.2% (0 to 8.1%) | 4.6% (0.2 to 68.5%) | <0.0001 | |||
| Other family | 0.2% (0 to 8.1%) | 4.6% (0.2 to 68.5%) | <0.0001 | |||
| Bacteria.Planctomycetes | 0% (0 to 0.1%) | 0% (0 to 1.4%) | 0.0015 | |||
| Planctomycetacia | 0% (0 to 0.1%) | 0% (0 to 1.4%) | 0.0322 | |||
| Planctomycetales | 0% (0 to 0.1%) | 0% (0 to 1.4%) | 0.0047 | |||
| Planctomycetaceae | 0% (0 to 0.1%) | 0% (0 to 1.4%) | 0.0080 | |||
| Bacteria.Proteobacteria | 36.3% (0.5 to 85.8%) | 2.7% (0 to 40.9%) | <0.0001 | |||
| Alphaproteobacteria | 0% (0 to 0.3%) | 0% (0 to 0.3%) | 0.8167 | |||
| Caulobacterales | 0% (0 to 0.2%) | 0% (0) | 0.9515 | |||
| Caulobacteriaceae | 0% (0 to 0.2%) | 0% (0) | 1.0000 | |||
| Rhizobiales | 0% (0 to 0.2%) | 0% (0 to 0.2%) | 0.9515 | |||
| Hyphomicrobiaceae | 0% (0%) | 0% (0 to 0.1%) | 1.0000 | |||
| Methylobacteriaceae | 0% (0 to 0.1%) | 0% (0 to 0.1%) | 1.0000 | |||
| Other | 0% (0 to 0.2%) | 0% (0 to 0.3%) | 1.0000 | |||
| Rhodobacteriales | 0% (0 to 0.2%) | 0% (0 to 0.1%) | 0.9515 | |||
| Rhodobacteriaceae | 0% (0 to 0.2%) | 0% (0 to 0.1%) | 1.0000 | |||
| Rhodospirales | 0% (0%) | 0% (0%) | NP | |||
| Other | 0% (0%) | 0% (0%) | NP | |||
| Other order | 0% (0%) | 0% (0 to 0.1%) | 0.9515 | |||
| Other family | 0% (0%) | 0% (0 to 0.1%) | 1.0000 | |||
| Betaproteobacteria | 0% (0 to 0.2%) | 0% (0 to 0.5%) | 0.4698 | |||
| Burkholderiales | 0% (0 to 0.2%) | 0% (0 to 0.5%) | 0.9230 | |||
| Alcaligenaceae | 0% (0 to 0.1%) | 0% (0 to 0.1%) | 1.0000 | |||
| Comamonadacea | 0% (0 to 0.1%) | 0% (0 to 0.1%) | 1.0000 | |||
| Other | 0% (0 to 0.1%) | 0% (0 to 0.5%) | 1.0000 | |||
| Other order | 0% (0 to 0.1%) | 0% (0 to 0.1%) | 0.9515 | |||
| Other family | 0% (0 to 0.1%) | 0% (0 to 0.1%) | 1.0000 | |||
| Deltaproteobacteria | 0% (0 to 0.4%) | 0% (0 to 1.1%) | 0.0084 | |||
| Desulfovibrionales | 0% (0 to 0.4%) | 0% (0 to 0.5%) | 0.0385 | |||
| Desulfovibrionaceae | 0% (0 to 0.4%) | 0% (0 to 0.5%) | 0.1136 | |||
| Other | 0% (0 to 0.1%) | 0% (0 to 0.2%) | 1.0000 | |||
| Myxococcales | 0% (0%) | 0% (0 to 1.1%) | 0.9515 | |||
| Nannocystineae | 0% (0%) | 0% (0 to 1.0%) | 1.0000 | |||
| Other | 0% (0%) | 0% (0 to 0.1%) | 1.0000 | |||
| Epsilonproteobacteria | 0% (0 to 0.1%) | 0.3% (0 to 16.4%) | <0.0001 | |||
| Campylobacterales | 0% (0 to 0.1%) | 0.3% (0 to 16.4%) | <0.0001 | |||
| Campylobacteriaceae | 0% (0 to 0.1%) | 0.2% (0 to 4.7%) | <0.0001 | |||
| Helicobacteraceae | 0% (%) | 0% (0 to 15.9%) | 0.0080 | |||
| Gamma proteobacteria | 36.3% (0 to 85.8%) | 0.5% (0 to 40.9%) | <0.0001 | |||
| Aeromonadales | 0% (0 to 3.2%) | 0% (0 to 4.2%) | 0.9515 | |||
| Aeromonadaceae | 0% (0 to 3.2%) | 0% (0%) | 0.3234 | |||
| Succinivibrionaceae | 0% (0%) | 0% (0 to 4.2%) | 0.0080 | |||
| Enterobacteriales | 36.2% (0 to 85.8%) | 0.1% (0 to 39.8%) | <0.0001 | |||
| Enterobacteriaceae | 36.2% (0 to 85.8%) | 0.1% (0 to 39.8%) | <0.0001 | |||
| Legionellales | 0% (0%) | 0% (0 to 0.2%) | 0.9515 | |||
| Coxiellaceae | 0% (0%) | 0% (0 to 0.1%) | 1.0000 | |||
| Legionellaceae | 0% (0%) | 0% (0 to 0.2%) | 1.0000 | |||
| Oceanospirillales | 0% (0 to 0.1%) | 0% (0%) | 0.9515 | |||
| Halomonadaceae | 0% (0 to 0.1%) | 0% (0%) | 1.0000 | |||
| Pasteurellales | 0% (0 to 3.6%) | 0% (0 to 1.2%) | 0.9515 | |||
| Pasteurellaceae | 0% (0 to 3.6%) | 0% (0 to 1.2%) | 1.0000 | |||
| Pseudomonadales | 0% (0 to 1.5%) | 0% (0 to 1.1%) | 0.9515 | |||
| Moraxellaceae | 0% (0 to 0.3%) | 0% (0 to 0.7%) | 1.0000 | |||
| Pseudomonadaceae | 0% (0 to 1.2%) | 0% (0 to 0.4%) | 1.0000 | |||
| Xanthomonadales | 0% (0%) | 0% (0 to 0.1%) | 0.9515 | |||
| Xanthomonadaceae | 0% (0%) | 0% (0 to 0.1%) | 1.0000 | |||
| Other order | 0% (0 to 0.5%) | 0% (0%) | 0.3278 | |||
| Other family | 0% (0 to 0.5%) | 0% (0%) | 1.0000 | |||
| Other class | 0% (0 to 0.2%) | 0% (0 to 23.7%) | 0.0099 | |||
| Other order | 0% (0 to 0.2%) | 0% (0 to 23.7%) | 0.0333 | |||
| Other family | 0% (0 to 0.2%) | 0% (0 to 23.7%) | 0.9089 | |||
| Bacteria.Spirochaetes | 0% (0%) | 0% (0 to 2.1%) | 0.0100 | |||
| Spirochaetes | 0% (0%) | 0% (0 to 2.1%) | 0.0375 | |||
| Spirochaetales | 0% (0%) | 0% (0 to 2.1%) | 0.0360 | |||
| Spirochaetaceae | 0% (0%) | 0% (0 to 2.1%) | 0.0720 | |||
| Other | 0% (0%) | 0% (0 to 0.2%) | 1.0000 | |||
| Bacteria.TM7 | 0% (0%) | 0% (0 to 1.8%) | 0.0048 | |||
| TM7 genera incertae sedis | 0% (0%) | 0% (0 to 1.8%) | 0.0280 | |||
| Other order | 0% (0%) | 0% (0 to 1.8%) | 0.0156 | |||
| Other family | 0% (0%) | 0% (0 to 1.8%) | 0.0308 | |||
| Bacteria.Tenericutes | 0% (0%) | 0% (0 to 0.1%) | 0.9515 | |||
| Mollicutes | 0% (0%) | 0% (0 to 0.1%) | 1.0000 | |||
| Anaeroplasmatales | 0% (0%) | 0% (0 to 0.1%) | 1.0000 | |||
| Anaeroplasmataceae | 0% (0%) | 0% (0 to 0.1%) | 1.0000 | |||
| Bacteria.Verrucomicrobia | 0% (0 to 42.5%) | 1.0% (0.4 to 48.7%) | 0.0015 | |||
| Verrucomicrobiae | 0% (0 to 42.5%) | 1.0% (0.4 to 48.7%) | 0.0322 | |||
| Verrucomicrobiales | 0% (0 to 42.5%) | 1.0% (0.4 to 48.7%) | 0.0040 | |||
| Other | 0% (0%) | 0% (0 to 0.2%) | 1.0000 | |||
| Subdivision 5 | 0% (0 to 0.2%) | 0.3% (0 to 25.4%) | 0.0000 | |||
| Verrucomicrobiaceae | 0% (0 to 42.5%) | 0.6% (0 to 48.6%) | 0.0158 | |||
| Xiphinematobacteriaceae | 0% (0%) | 0% (0 to 0.2%) | 1.0000 | |||
| Other Kingdom, Other phylum | 0% (0 to 1.1%) | 0% (0 to 0.3%) | 0.9515 | |||
| Other class | 0% (0 to 1.1%) | 0% (0 to 0.3%) | 1.0000 | |||
| Other order | 0% (0 to 1.1%) | 0% (0 to 0.3%) | 1.0000 | |||
| Other family | 0% (0 to 1.1%) | 0% (0 to 0.3%) | 1.0000 | |||
Fecal swab samples were collected from 37 Quarter Horse foals on days 2 and 30 of life. *P values represent the results of Wilcoxon sign-rank tests for paired differences, adjusted by the method of Hochberg. NP = Not Performed.
Table 3. Median and range proportion of foals with sequences detected in the fecal DNA of rectal swab samples (Phylum, class, order, and family).
| Microbial Family | 2-day-old foals (N = 37) | 30-day-old foals (N = 37) | P* | |||
| Archaea.Euryarchaeota | 0% (0/37) | 35% (13/37) | 0.0117 | |||
| Methanobacteria | 0% (0/37) | 24% (9/37) | 0.0770 | |||
| Methanobacteriales | 0% (0/37) | 24% (9/37) | 0.1925 | |||
| Methanobacteriacae | 0% (0/37) | 24% (9/37) | 0.4851 | |||
| Methanomicrobia | 0% (0/37) | 16% (6/37) | 0.3708 | |||
| Methanomicrobiales | 0% (0/37) | 16% (6/37) | 0.9064 | |||
| Methanocorpusculaceae | 0% (0/37) | 16% (6/37) | 1.0000 | |||
| Bacteria.Acidobacteria | 0% (0/37) | 3% (1/37) | 0.9999 | |||
| Acidobacteria | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Acidobacteriales | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Acidobacteriaceae | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Bacteria.Actinobacteria | 73% (27/37) | 97% (36/37) | 0.1590 | |||
| Actinobacteria | 73% (27/37) | 97% (36/37) | 0.1925 | |||
| Actinomycetales (order) | 62% (23/37) | 73% (27/37) | 1.0000 | |||
| Bifidobacteriales (order) | 3% (1/37) | 8% (3/37) | 1.0000 | |||
| Other | 14% (5/37) | 8% (3/37) | 1.0000 | |||
| Coriobacteridae (subclass) | 24% (9/37) | 76% (28/37) | 0.0041 | |||
| Coriobacteriales | 24% (9/37) | 76% (28/37) | 0.0221 | |||
| Rubrobacteridae (subclass) | 3% (1/37) | 0% (0/37) | 1.0000 | |||
| Rubrobacterales | 3% (1/37) | 0% (0/37) | 1.0000 | |||
| Other order | 0% (0/37) | 27% (10/37) | 0.1452 | |||
| Other family | 0% (0/37) | 27% (10/37) | 0.2944 | |||
| Bacteria.Bacteroidetes | 92% (34/37) | 100% (37/37) | 0.5152 | |||
| Bacteroidetes | 89% (33/37) | 100% (37/37) | 1.0000 | |||
| Bacteroidales | 89% (33/37) | 100% (37/37) | 1.0000 | |||
| Bacteroidieacae | 86% (32/37) | 95% (35/37) | 1.0000 | |||
| Porphyromonadaceae | 30% (11/37) | 89% (33/37) | <0.0001 | |||
| Prevotellaceae | 8% (3/37) | 95% (35/37) | <0.0001 | |||
| Rikenellaceae | 11% (4/37) | 49% (18/37) | 0.1496 | |||
| Other | 11% (4/37) | 95% (35/37) | <0.0001 | |||
| Flavobacteria | 16% (6/37) | 11% (4/37) | 1.0000 | |||
| Flavobacteriales | 16% (6/37) | 11% (4/37) | 1.0000 | |||
| Flavobacteriaceae | 16% (6/37) | 11% (4/37) | 1.0000 | |||
| Sphingobacteria | 5% (2/37) | 3% (1/37) | 1.0000 | |||
| Sphingobacteriales | 5% (2/37) | 3% (1/37) | 1.0000 | |||
| Crenotrichaceae | 3% (1/37) | 0% (0/37) | 1.0000 | |||
| Flexibacteriaceae | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Sphingobacteriaceae | 3% (1/37) | 0% (0/37) | 1.0000 | |||
| Other class | 27% (10/37) | 95% (35/37) | <0.0001 | |||
| Other order | 27% (10/37) | 95% (35/37) | <0.0001 | |||
| Other family | 27% (10/37) | 95% (35/37) | <0.0001 | |||
| Bacteria.Chlamydiae | 0% (0/37) | 51% (19/37) | <0.0001 | |||
| Chlamydiae | 0% (0/37) | 51% (19/37) | <0.0001 | |||
| Chlamydiales | 0% (0%) | 51% (19/37) | <0.0001 | |||
| Chlamydiaceae | 0% (0%) | 51% (19/37) | <0.0001 | |||
| Parachlamydiaceae | 0% (0%) | 3% (1/37) | 1.0000 | |||
| Bacteria.Chloroflexi | 0% (0/37) | 22% (8/37) | 0.1463 | |||
| Anaerolineae | 0% (0/37) | 22% (8/37) | 0.1173 | |||
| Caldilineae | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Caldilineales | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Other | 0% (0/37) | 19% (7/37) | 0.7223 | |||
| Other family | 0% (0/37) | 19% (7/37) | 1.0000 | |||
| Bacteria.Cyanobacteria | 0% (0/37) | 3% (1/37) | 0.9999 | |||
| Cyanobacteria | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Other order | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Other family | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Bacteria.Deferribacteres | 3% (1/37) | 5% (2/37) | 0.9999 | |||
| Deferribacteres | 3% (1/37) | 5% (2/37) | 1.0000 | |||
| Deferribacterales | 3% (1/37) | 5% (2/37) | 1.0000 | |||
| Deferribacteraceae | 0% (0%) | 0% (0%) | NP | |||
| Incertae sedis 3 | 3% (1/37) | 5% (2/37) | 1.0000 | |||
| Bacteria.Fibrobacteres | 0% (0/37) | 14% (5/37) | 0.5152 | |||
| Fibrobacteres | 0% (0/37) | 14% (5/37) | 0.4698 | |||
| Fibrobacterales | 0% (0/37) | 14% (5/37) | 0.9515 | |||
| Fibrobacteraceae | 0% (0/37) | 14% (5/37) | 1.0000 | |||
| Bacteria.Firmicutes | 100% (37/37) | 100% (37/37) | NP | |||
| Bacilli | 100% (37/37) | 100% (37/37) | NP | |||
| Lactobacillales | 100% (37/37) | 100% (37/37) | NP | |||
| Aerococcaceae | 27% (10/37) | 14% (5/37) | 1.0000 | |||
| Carnobacteriaceae | 14% (5/37) | 3% (1/37) | 1.0000 | |||
| Enterococcaceae | 95% (35/37) | 41% (15/37) | 0.0078 | |||
| Lactobacillaceae | 27% (10/37) | 70% (26/37) | 0.2944 | |||
| Leuconostocaceae | 8% (3/37) | 0% (0/37) | 1.0000 | |||
| Streptococcaceae | 97% (36/37) | 97%(36/37) | 1.0000 | |||
| Other | 78% (29/37) | 22% (8/37) | <0.0001 | |||
| Bacillales | 46% (17/37) | 70% (26/37) | 1.0000 | |||
| Paenibacillaceae | 3% (1/37) | 5% (2/37) | 1.0000 | |||
| Staphylococcaceae | 32% (12/37) | 62% (23/37) | 1.0000 | |||
| Bacillaceae | 14% (5/37) | 14% (5/37) | 1.0000 | |||
| Incertae Sedis XI | 11% (4/37) | 3% (1/37) | 1.0000 | |||
| Planococcaceae | 3% (1/37) | 11% (4/37) | 1.0000 | |||
| Other | 0% (0/37) | 8% (3/37) | 1.0000 | |||
| Other order | 30% (11/37) | 11% (4/37) | 1.0000 | |||
| Other family | 30% (11/37) | 11% (4/37) | 1.0000 | |||
| Clostridia | 100% (37/37) | 100% (37/37) | NP | |||
| Clostridiales | 100% (37/37) | 100% (37/37) | NP | |||
| Eubacteriaceae | 5% (2/37) | 35% (13/37) | 0.6076 | |||
| Lachnospiraceae | 89% (33/37) | 100% (37/37) | 1.0000 | |||
| Peptostreptococcaceae | 43% (16/37) | 0.0150 | ||||
| Ruminococcaceae | 70% (26/37) | 100% (37/37) | 0.1716 | |||
| Clostridiaceae | 100% (37/37) | 78% (29/37) | 0.7980 | |||
| Incertae Sedis XI | 11% (4/37) | 78% (29/37) | <0.0001 | |||
| Incertae Sedis XIII | 5% (2/37) | 57% (21/37) | 0.0154 | |||
| Peptococcaceae | 0% (0/37) | 32% (12/37) | 0.1065 | |||
| Veillonellaceae | 16% (6/37) | 95% (35/37) | <0.0001 | |||
| Other | 100% (37/37) | 97% (36/37) | 1.0000 | |||
| Other order | 32% (12/37) | 59% (22/37) | 0.8136 | |||
| Other family | 32% (12/37) | 59% (22/37) | 1.0000 | |||
| Erysipelotrichi | 62% (23/37) | 70% (26/37) | 1.0000 | |||
| Erysipelotrichales | 62% (23/37) | 70% (26/37) | 1.0000 | |||
| Erysipelotrichiaceae | 62% (23/37) | 70% (26/37) | 1.0000 | |||
| Other class | 49% (18/37) | 86% (32/37) | 0.0242 | |||
| Other order | 49% (18/37) | 86% (32/37) | 0.0594 | |||
| Other family | 49% (18/37) | 86% (32/37) | 1.0000 | |||
| Bacteria.Fusobacteria | 62% (23/37) | 84% (31/37) | 0.5152 | |||
| Fusobacteria | 62% (23/37) | 84% (31/37) | 1.0000 | |||
| Fusobacteriales | 62% (23/37) | 84% (31/37) | 1.0000 | |||
| Fusobacteriaceae | 62% (23/37) | 81% (30/37) | 1.0000 | |||
| Incertae sedis 11 | 5% (2/37) | 0% (0/37) | 1.0000 | |||
| Other | 32% (12/37) | 43% (16/37) | 1.0000 | |||
| Bacteria.Lentisphaerae | 0% (0/37) | 0% (0/37) | NP | |||
| Lentisphaerae | 0% (0/37) | 0% (0/37) | NP | |||
| Victivallales | 0% (0/37) | 0% (0/37) | NP | |||
| Victivallaceae | 0% (0/37) | 0% (0/37) | NP | |||
| Bacteria.Other | 86% (32/37) | 100% (37/37) | 0.5152 | |||
| Bacteria. Other Class | 86% (32/37) | 100% (37/37) | 1.0000 | |||
| Other Order | 86% (32/37) | 100% (37/37) | 1.0000 | |||
| Other family | 86% (32/37) | 100% (37/37) | 1.0000 | |||
| Bacteria.Planctomycetes | 3% (1/37) | 43% (16/37) | 0.0045 | |||
| Planctomycetacia | 3% (1/37%) | 43% (16/37) | 0.0377 | |||
| Planctomycetales | 3% (1/37) | 43% (16/37) | 0.0120 | |||
| Planctomycetaceae | 3% (1/37) | 43% (16/37) | 0.0003 | |||
| Bacteria.Proteobacteria | 100% (37/37) | 97% (36/37) | 0.9999 | |||
| Alphaproteobacteria | 11% (4/37) | 14% (5/37) | 1.0000 | |||
| Caulobacterales | 3% (1/37) | 0% (0/37) | 1.0000 | |||
| Caulobacteriaceae | 3% (1/37) | 0% (0/37) | 1.0000 | |||
| Rhizobiales | 5% (2/37) | 8% (3/37) | 1.0000 | |||
| Hyphomicrobiaceae | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Methylobacteriaceae | 3% (1/37) | 3% (1/37) | 1.0000 | |||
| Other | 3% (1/37) | 3% (1/37) | 1.0000 | |||
| Rhodobacteriales | 5% (2/37) | 3% (1/37) | 1.0000 | |||
| Rhodobacteriaceae | 5% (2/37) | 3% (1/37) | 1.0000 | |||
| Rhodospirales | 0% (0%) | 0% (0%) | NP | |||
| Other | 0% (0%) | 0% (0%) | NP | |||
| Other order | 0% (0%) | 3% (1/37) | 1.0000 | |||
| Other family | 0% (0%) | 3% (1/37) | 1.0000 | |||
| Betaproteobacteria | 11% (4/37) | 27% (10/37) | 1.0000 | |||
| Burkholderiales | 8% (3/37) | 24% (9/37%) | 1.0000 | |||
| Alcaligenaceae | 3% (1/37) | 3% (1/37) | 1.0000 | |||
| Comamonadacea | 3% (1/37) | 8% (3/37) | 1.0000 | |||
| Other | 3% (1/37) | 14% (5/37) | 1.0000 | |||
| Other order | 5% (2/37) | 3% (1/37) | 1.0000 | |||
| Other family | 5% (2/37) | 3% (1/37) | 1.0000 | |||
| Deltaproteobacteria | 5% (2/37) | 49% (18/37) | 0.0104 | |||
| Desulfovibrionales | 5% (2/37) | 46% (17/37) | 0.0377 | |||
| Desulfovibrionaceae | 5% (2/37) | 43% (16/37) | 0.1496 | |||
| Other | 3% (1/37) | 14% (5/37) | 1.0000 | |||
| Myxococcales | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Nannocystineae | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Other | 0% (0/37) | 0% (0/37) | NP | |||
| Epsilonproteobacteria | 3% (1/37) | 73% (27/37) | <0.0001 | |||
| Campylobacterales | 3% (1/37) | 73% (27/37) | <0.0001 | |||
| Campylobacteriaceae | 3% (1/37) | 65% (24/37) | <0.0001 | |||
| Helicobacteraceae | 0% (0/37) | 43% (16/37) | 0.0154 | |||
| Gamma proteobacteria | 97% (36/37) | 89% (33/37) | 1.0000 | |||
| Aeromonadales | 22% (8/37) | 41% (15/37) | 1.0000 | |||
| Aeromonadaceae | 22% (8/37) | 0% (0/37) | 0.7980 | |||
| Succinivibrionaceae | 0% (0/37) | 41% (15/37) | 0.0219 | |||
| Enterobacteriales | 95% (35/37) | 62% (23/37) | 0.0858 | |||
| Enterobacteriaceae | 95% (35/37) | 62% (23/37) | 0.2145 | |||
| Legionellales | 0% (0/37) | 5% (2/37) | 1.0000 | |||
| Coxiellaceae | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Legionellaceae | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Oceanospirillales | 3% (1/37) | 0% (0/37) | 1.0000 | |||
| Halomonadaceae | 3% (1/37) | 0% (0/37) | 1.0000 | |||
| Pasteurellales | 32% (12/37) | 38% (14/37) | 1.0000 | |||
| Pasteurellaceae | 32% (12/37) | 38% (14/37) | 1.0000 | |||
| Pseudomonadales | 14% (5/37) | 11% (4/37) | 1.0000 | |||
| Moraxellaceae | 14% (5/37) | 11% (4/37) | 1.0000 | |||
| Pseudomonadaceae | 5% (2/37) | 3% (1/37) | 1.0000 | |||
| Xanthomonadales | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Xanthomonadaceae | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Other order | 16% (6/37) | 0% (0/37) | 0.9064 | |||
| Other family | 16% (6/37) | 0% (0/37) | 1.0000 | |||
| Other class | 5% (2/37) | 43% (16/37) | 0.0242 | |||
| Other order | 5% (2/37) | 43% (16/37) | 0.0594 | |||
| Other family | 5% (2/37) | 43% (16/37) | 0.1496 | |||
| Bacteria.Spirochaetes | 0% (0/37) | 30% (11/37) | 0.0312 | |||
| Spirochaetes | 0% (0/37) | 30% (11/37) | 0.0439 | |||
| Spirochaetales | 0% (0/37) | 30% (11/37) | 0.0910 | |||
| Spirochaetaceae | 0% (0/37) | 30% (11/37) | 0.1716 | |||
| Other | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Bacteria.TM7 | 0% (0/37) | 35% (13/37) | 0.0117 | |||
| TM7 genera incertae sedis | 0% (0/37) | 35% (13/37) | 0.0218 | |||
| Other order | 0% (0/37) | 35% (13/37) | 0.0351 | |||
| Other family | 0% (0/37) | 35% (13/37) | 0.0648 | |||
| Bacteria.Tenericutes | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Mollicutes | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Anaeroplasmatales | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Anaeroplasmataceae | 0% (0/37) | 3% (1/37) | 1.0000 | |||
| Bacteria.Verrucomicrobia | 24% (9/37) | 89% (33/37) | <0.0001 | |||
| Verrucomicrobiae | 24% (9/37) | 89% (33/37) | <0.0001 | |||
| Verrucomicrobiales | 24% (9/37) | 89% (33/37) | <0.0001 | |||
| Other | 0% (0%) | 5% (2/37) | 1.0000 | |||
| Subdivision 5 | 8% (3/37) | 76% (28/37) | <0.0001 | |||
| Verrucomicrobiaceae | 16% (6/37) | 78% (29/37) | <0.0001 | |||
| Xiphinematobacteriaceae | 0% (0%) | 3% (1/37) | 1.0000 | |||
| Other Kingdom, Other phylum | 19% (7/37) | 22% (8/37) | 0.9999 | |||
| Other class | 19% (7/37) | 22% (8/37) | 1.0000 | |||
| Other order | 19% (7/37) | 22% (8/37) | 1.0000 | |||
| Other family | 19% (7/37) | 22% (8/37) | 1.0000 | |||
Fecal swab samples collected from 37 Quarter Horse foals on days 2 and 30 of life. *P values represent the results of McNemar’s test for paired dichotomous data, adjusted by the method of Hochberg. NP = Not Performed.
Figure 1. Rarefaction analysis of 16 S rRNA gene sequences obtained from fecal swabs from foals.
Lines represent the average of each vaccination group at all ages (panel A) or at 30 days only (panel B), while the error bars represent the standard deviations. The analysis was performed on a randomly selected subset of 1,300 sequences per sample and included samples from 42 foals. Note that both the greatest and least number of species observed occurred among foals that received no enteral bacteria (live or inactivated), indicating an absence of evidence of treatment effect. Control = control plus CTB group; Control_no_CTO = control without CTB group; High = high-dose inactivated R. equi group; Live = live R. equi group; Low = low-dose inactivated R. equi group.
Figure 2. Rarefaction analysis of 16 S rRNA gene sequences obtained from fecal swabs from foals.
Lines represent the average numbers obtained at each age (legend numbers refer to the age in days), while the error bars represent the standard deviations. The analysis was performed on a randomly selected subset of 1,300 sequences per sample and included samples from 42 foals. Note the progressive increase in observed species (representing microbial diversity) with sequential age. The numbers for the legend represent age (in days).
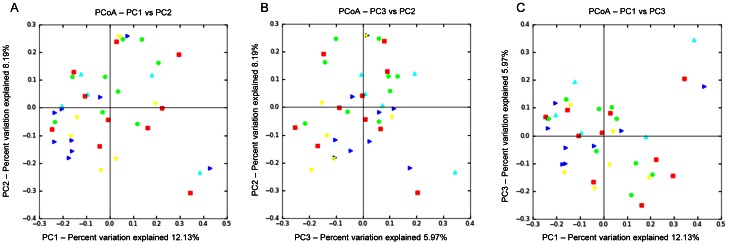
Microbial communities in control and vaccinated foals
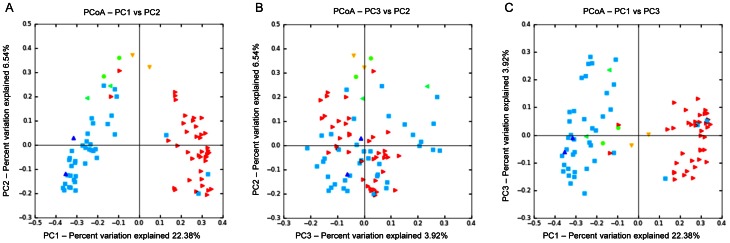
No differences in microbial composition were observed among animals from control, live and inactivated treatment/vaccination groups (Figures 1A, 1B, and 3). The rarefaction curves for the treatment groups revealed no clear pattern of greater number of observed species (i.e., diversity) among foals receiving either live or inactivated R. equi, or those foals in the 3 control groups that did not receive R. equi (Figure 1A). Because the samples at age 2 days were not affected by treatment (because treatment was administered after sample collection on day 2), we also performed analysis restricting data to samples collected at age 30 days (Figure 1B). Once again, there was no pattern of differences in the rarefaction curves among treatment groups receiving either live or inactivated R. equi or the control groups. Using PCoA (Figures 3 and 4), there was no qualitative evidence of differences among groups; the clustering observed in Figure 3 panel A was attributable to effects of age (please see next section). When considering only the data from foals at 30 days of age (because samples on day 2 were collected prior to treatment administration), the PCoA plots revealed no clustering by group and the ANOSIM test statistic for differences among groups was not significant (P = 0.494).
Figure 3. Principal coordinates analysis (PCoA) of unweighted UniFrac distances of 16 S rRNA genes.
Analysis for 42 foals in groups control with CTB (red square), control without CTB (yellow triangle), low-dose inactivated R. equi (dark blue triangle), high-dose inactivated R. equi 2 (green dot), and live R. equi (light blue triangle) at 2 and 30 days of age (ANOSIM, P = 0.236). The 3 panels represent the comparison of the first 2 principal components (A), the second and third principal components (B), and the first and third principal components (C). The pattern in the panel A is attributable to effects of age (please see Figures 4 and 5).
Figure 4. Principal coordinates analysis (PCoA) of unweighted UniFrac distances of 16 S rRNA genes.
Analysis for 42 foals in groups control with CTB (red square), control without CTB (yellow triangle), low-dose inactivated R. equi (dark blue triangle), high-dose inactivated R. equi 2 (green dot), and live R. equi (light blue triangle) at 30 days of age only. Differences among groups were not significant (ANOSIM, P = 0.449). The 3 panels represent the comparison of the first 2 principal components (A), the second and third principal components (B), and the first and third principal components (C).
Age-related changes in microbial communities in foals
There were strong and significant differences in the fecal microbiome of foals associated with age. The rarefaction curves demonstrated a pattern of increasing number of species (diversity) with increasing age (Figure 2). These results should be interpreted with caution because there were only 2 foals for which data for ages other than 2 days and 30 days were available. The PCoA plots by age revealed an obvious separation of samples by age, attributable to differences between the time-points of days 2 and 30 (Figure 5); the ANOSIM test statistic for differences between day 2 and day 30 was significant (P = 0.0010).
Figure 5. Principal coordinates analysis (PCoA) of unweighted UniFrac distances of 16 S rRNA genes.
Analysis for 42 foals at 2 (red triangle), 7 days old (yellow triangle), 14 (green dot), 21 (green triangle), 30 (light blue square), and 56 days of age (dark blue triangle). The 3 panels represent the comparison of the first 2 principal components (A), the second and third principal components (B), and the first and third principal components (C). Strong effects of age can be seen in panels A and C, and differences among age groups were significant (ANOSIM, P = 0.0010).
Significant differences in the number of OTUs, the Shannon index, and the Chao1 metric were observed between the age groups (Table 4). The median number of OTUs for 2day-old foals (92 OTUs; range, 50 to 195 OTUs) was significantly (P<0.0001) lower than that for 30-day-old foals (201 OTUs; range, 94 to 318 OTUs). The Shannon Index for the foals studied also increased significantly (P<0.0001) from 2 days of life (median, 2.37; range, 1.24 to 3.97) to 30 days of life (median, 3.7; range, 1.90 to 4.80). Similarly, there was a significant (P<0.0001) age-related increase in Chao 1 values between 2-day-old foals (median, 206.54; range, 128.16 to 415.70) and 30-day-old foals (median, 362.38; range, 197.42 to 581.43).
Table 4. Summary of alpha diversity measures.
| Index | 2 day-old | 30 day-old | P |
| Chao 1 (median, range) | 206.54 (128.16 to 415.70) | 362.38 (197.42 to 581.43) | <0.0001 |
| OTUs (median, range) | 92 (50 to 195) | 201 (94 to 318) | <0.0001 |
| Shannon H (median, range) | 2.37 (1.24 to 3.97) | 3.7 (1.90 to 4.80) | <0.0001 |
Because of the apparent differences of the microbiota between age groups, we also compared the distribution of bacteria by phylum, class, order, and family between foals aged 2 days and 30 days. In total, 18 phyla were detected in fecal samples from foals (Table 2). Of those, Bacteroidetes (40.6%, day 30), Firmicutes (40.4%, day 2), and Proteobacteria (36.6%, day 2) had the highest percentages of sequences reported. Proteobacteria and Firmicutes were detected in all samples from 2-day-old foals, followed by Bacteroidetes (92%) and Actinobacteria (73%) (Table 3). Among 30-day-old foals, Bacteroidetes and Firmicutes were detected in all fecal samples, followed by Actinobacteria (97%) and Proteobacteria (97%), Verrucomicrobia (89%), and Fusobacteria (84%) (Table 3). The following phyla increased significantly with age (i.e, from 2 days to 30 days of age): Euryarchaeota, Actinobacteria, Bacteroidetes, Chlamydiae, Chloroflexi, Planctomycetes, Spirochaetes, TM7, and Verrucomicrobia. Proteobacteria was the only phylum that decreased significantly with age. Other classes, orders, and families also showed statistically significant age-related changes (Table 2 and Figure 6).
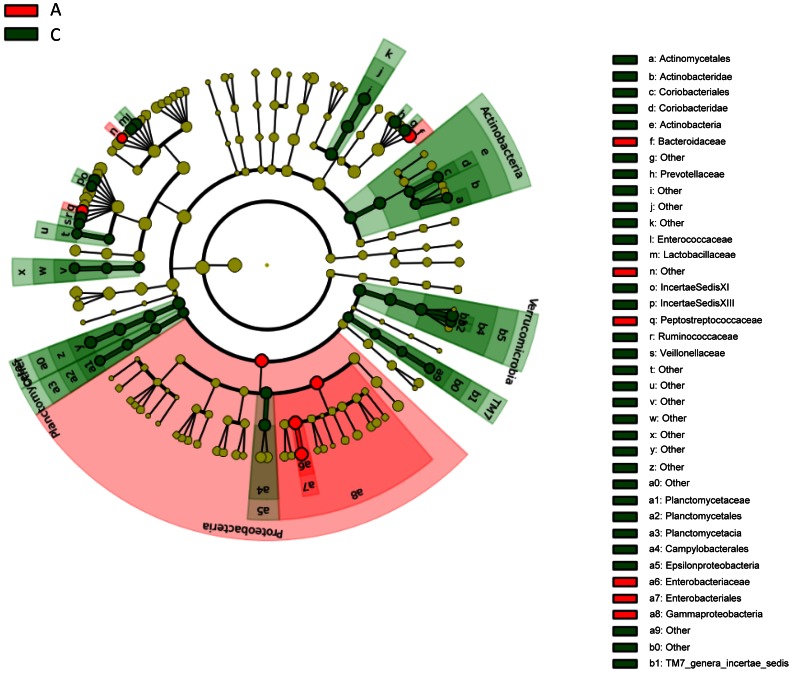
Figure 6. LEfSe results on foal microbiome.
Rotary phylogenetic representation of the predominate microbial composition of fecal samples from foals at 2 days of age (A, red) and 30 days of age (C, green) [32].
Within the phylum Proteobacteria, the class Gammaproteobacteria (P<0.0001) and the family Enterobacteriaceae (P<0.0001) decreased significantly with age. Other classes of Proteobacteria, such as Deltaproteobacteria (P = 0.0084) and Epsilonproteobacteria (P<0.0001) significantly increased with age (Table 2).
To confirm results of pyrosequencing, we also performed real-time quantitative PCR. Significant differences were observed in specific microbial communities between the 2 age groups based on qPCR analysis, with age-related decreases for Escherichia coli (P<0.0001) and for Enterococcus (P<0.0001). These data were consistent with genus-level results observed by pyrosequencing (Table 5) for Enterococcus (P = 0.0009) and for Escherichia (P<0.0001). We also found agreement for a lack of evidence of a significant difference between the pyrosequencing and the qPCR results for Bacteroidetes (P = 0.9519 by qPCR and P = 0.5376 by pyrosequencing) and Fusobacteria (P = 0.1051 on qPCR and P = 0.1000 on pyrosequencing).
Table 5. Results of qPCR analysis.
| Medians (min-max) log DNA (qPCR) | |||
| 2 day-old | 30 day-old | P* | |
| Universal | 13.2 (11.0 to 14.5) | 12.3 (9.3 to 14.2) | 0.0108 |
| Bacteroidetes | 11.4 (8.4 to 12.9) | 11.2 (9.3 to 12.4) | 0.9519 |
| Enterococcus | 7.9 (6.5 to 9.3) | 5.7 (4.1 to 7.3) | <0.0001 |
| Escherichia | 8.2 (4. 3 to 8.9) | 5.3 (2.8 to 6.5) | <0.0001 |
| Fusobacteria | 8.6 (6.0 to 10.4) | 7.8 (6.4 to 9.7) | 0.1051 |
Median (range) of log DNA. *P value for Wilcoxon rank-sum test comparing differences between ages day 30 and day 2, adjusted by the method of Hochberg.
Discussion
In this study, our first objective was to evaluate changes in the microbiome of foals following vaccination with both live and inactivated R. equi. Although the number of CFUs administered were as high (for the live R. equi group) or higher than the number of CFU documented to protect foals against intrabronchial challenge with virulent R. equi (viz., 1×1010 CFU), no apparent differences in microbial communities were observed among vaccinated groups (Figures 1A and 3). Because all but 2 foals had samples collected only on days 2 and 30, and because fecal samples on day 2 were not influenced by treatment (because they were collected immediately prior to treatment), the effect of group also was examined among only samples collected at 30 days of age. Results restricted to 30 days of age also revealed no pattern distinguishing vaccinated and non-vaccinated foals (Figures 1B and 4). Thus, we failed to detect evidence of a significant effect of enteral administration of either live or inactivated R. equi on microbial populations in neonatal foals. These results are consistent with reports in which probiotics (administered at similar or higher numbers of CFUs) have failed to alter the intestinal/fecal microbiome [38]–[40]. Our results should be interpreted with caution because of the relatively small number of foals, particularly in the live R. equi group. For technical reasons attributed to random error, pyrosequencing failed for samples from 3 foals from the live R. equi group and 2 foals from the control group without CTB group; therefore, only 3 foals from the live R. equi group and 6 from the controls without CTB group were included in the analysis.
A significant difference between the fecal microbial populations between day 2 and day 30 of age was observed (Table 2 and 3; Figures 2, 5, and 6). For descriptive purposes, we included the results from the 2 foals from which we had data at other ages (these data were not included in the statistical analysis comparing ages). The resident intestinal or fecal microbiota has been described for neonates of other species, such as cats [41], [42], dogs [43], and humans [25]–[27], [44]. To the authors’ knowledge, this is the first report of age-related changes of the fecal microbiome in foals. Significant changes in the number of OTUs, the Shannon index, and the Chao1 metric were observed between the age groups (Table 4), showing clear evidence of strong diversification of bacterial populations between 2 and 30 days of age.
Firmicutes were detected in 100% of foals at both 2 and 30 days of age, with reported median sequences of 40% in 2-day-old foals decreasing (albeit not significantly) to 23% in 30-day-old foals. In 2 previous studies using fecal samples from adult horses, Firmicutes represented 44% [45] and 72% [46] of the bacteria. Within the Firmicutes, the family Enterococcaceae significantly decreased with age (P = 0.0080), which was likely attributable at least in part to decreases in the genus Enterococcus that were observed to decrease significantly by qPCR (P<0.0001) and by pyrosequencing (Table 5). Proteobacteria were detected in the feces of all 2-day-old foals and 97% of 30-day-old foals, a difference that was not significant; however, the median percentage of sequences decreased significantly (P<0.0001) between day 2 (median, 36.3%; range, 0.5 to 85.8%) and day 30 (median, 2.7%; range, 0 to 40.9%). In adult horses, Proteobacteria have been reported to represent 6% [45] and 12% [47] of fecal sequences. These results from adult horses are interesting in light of our findings, particularly our observation that the family Enterobacteriaceae decreased with age, a finding substantiated by our qPCR results with a significant decrease in the amount of E. coli (P<0.0001) between ages 2 and 30 days.
The sterile GI tract of newborn puppies and kittens is presumably colonized by bacteria present in the birth canal and from the environment [48], and human neonates appear to become colonized by these sources as well as through the intestinal microbiota of the mother [25], [49]. In humans, the initial microbes colonizing infants are facultative anaerobic bacteria, such as E. coli and Streptococcus spp. [49], which was also observed in 2-day old foals by the presence of Enterobacteriaceae (E. coli) and Streptococcaceae families (Streptococcus spp.). We observed a significant decrease in both these families by 30 days of age, suggesting that a similar phenomenon might happen in foals. In human beings, after the initial colonization by facultative anaerobic bacteria, colonization occurs by Staphylococcus-, Enterococcus-, and Lactobacillus-like species, and this change might contribute to generating an anaerobic environment [44]. The development during the first month of life in foals of an anaerobic environment is supported by the age-related increase in the detection of the phylum of Bacteroidetes (P = 0.0066), which is also a common constituent of the gut microbiota of dogs and cats [48]. However, we also observed a significant decrease in the Enterococcaceae family (P = 0.0080) and Enterococcus spp. by qPCR (P<0.0001), as well as the Lactobacillaceae family (P = 0.0281).
Our study has a number of important limitations. One limitation is the use of fecal swab samples for analysis, because feces might not be representative of other compartments of the gut. In humans, the composition of the mucosal-surface microbiota is distinct from that recovered in the feces [50]. The situation is probably similar in the horse, because of the complexity of the equine gastrointestinal tract. For example, the microbial population of adult horse fecal samples is likely to represent that of the right dorsal colon, but not that of the cecum [51].
A second limitation of our study is the small number of foals enrolled. Our sample size was limited both by financial considerations and the number of foals available to us during the study period. Because of the small sample size, we were only able to observe large changes in fecal microbial populations. Nevertheless, our results provide useful data for those exploring enteral vaccination of foals [14], [52]. It is worth noting that there were significant differences in immune responses that were detectable among these groups of foals despite the small sample size (data not shown). Also, we were able to detect significant age-related differences in the microbiome of foals, irrespective of the treatment groups.
Another limitation of our study is that we only characterized age-related changes at 2 ages during the first month of life. Although our data from 2 foals with more frequent sampling appears to demonstrate a progressive diversification of microbial flora with age (Figure 5), further studies using more foals with more frequent sampling times are needed to better characterize microbial diversification. Our focus on the first month of life was based on current understanding that vaccination of foals against R. equi will have to occur during early life [53].
In conclusion, no differences were observed in the fecal microbiome of foals following enteral vaccination with either live or inactivated R. equi. These results demonstrate that administration of the doses of bacteria used in this study does not likely cause an alteration of the fecal microbiome of foals. More notably, the results indicate significant age-related changes in the microbiome composition of foals during the first month of life.
Acknowledgments
The authors wish to thank Ms. Courtney Brake, Ms. Kristin Knabe, Ms. Michele Batista, Dr. Michelle Coleman, Dr. Jessica Bourquin, Ms. Krissy Johnson Schroeder, and Mr. Dave Golden for their help during the animal phase of this study. The authors would also like to thank Drs. Charles Love, David McMurray and Waithaka Mwangi for consultation and reviewing this manuscript.
Funding Statement
This work was supported by the Link Equine Research Endowment at Texas A&M University with additional support provided by the Gastrointestinal Laboratory at Texas A&M University and Boehringer-Ingelheim Vetmedica. Dr. Bordin was supported by a fellowship from Fort Dodge Animal Health/Pfizer Animal Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Meijer WG, Prescott JF (2004) Rhodococcus equi . Veterinary Research 35: 383–396. [DOI] [PubMed] [Google Scholar]
- 2. Muscatello G, Leadon DP, Klayt M, Ocampo-Sosa A, Lewis DA, et al. (2007) Rhodococcus equi infection in foals: the science of 'rattles'. Equine Vet J 39: 470–478. [DOI] [PubMed] [Google Scholar]
- 3. Prescott JF (1991) Rhodococcus equi: an animal and human pathogen. Clin Microbiol Rev 4: 20–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Takai S (1997) Epidemiology of Rhodococcus equi infections: a review. Vet Microbiol 56: 167–176. [DOI] [PubMed] [Google Scholar]
- 5. Giguère S, Cohen ND, Chaffin MK, Hines SA, Hondalus MK, et al. (2011) Rhodococcus equi: clinical manifestations, virulence, and immunity. Journal of Veterinary Internal Medicine 25: 1221–1230. [DOI] [PubMed] [Google Scholar]
- 6. Jain S, Bloom BR, Hondalus MK (2003) Deletion of vapA encoding Virulence Associated Protein A attenuates the intracellular actinomycete Rhodococcus equi . Mol Microbiol 50: 115–128. [DOI] [PubMed] [Google Scholar]
- 7. Dawson TR, Horohov DW, Meijer WG, Muscatello G (2010) Current understanding of the equine immune response to Rhodococcus equi. An immunological review of R. equi pneumonia. Vet Immunol Immunopathol 135: 1–11. [DOI] [PubMed] [Google Scholar]
- 8. Harris SP, Fujiwara N, Mealey RH, Alperin DC, Naka T, et al. (2010) Identification of Rhodococcus equi lipids recognized by host cytotoxic T lymphocytes. Microbiology 156: 1836–1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Patton KM, McGuire TC, Hines MT, Mealey RH, Hines SA (2005) Rhodococcus equi-specific cytotoxic T lymphocytes in immune horses and development in asymptomatic foals. Infection and Immunity 73: 2083–2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Horowitz ML, Cohen ND, Takai S, Becu T, Chaffin MK, et al. (2001) Application of Sartwell's model (lognormal distribution of incubation periods) to age at onset and age at death of foals with Rhodococcus equi pneumonia as evidence of perinatal infection. Journal of Veterinary Internal Medicine 15: 171–175. [DOI] [PubMed] [Google Scholar]
- 11. Chaffin MK, Cohen ND, Martens RJ (2008) Chemoprophylactic effects of azithromycin against Rhodococcus equi-induced pneumonia among foals at equine breeding farms with endemic infections. Journal of the American Veterinary Medical Association 232: 1035–1047. [DOI] [PubMed] [Google Scholar]
- 12. Chirino-Trejo JM, Prescott JF, Yager JA (1987) Protection of foals against experimental Rhodococcus equi pneumonia by oral immunization. Can J Vet Res 51: 444–447. [PMC free article] [PubMed] [Google Scholar]
- 13. Hooper-McGrevy KE, Wilkie BN, Prescott JF (2005) Virulence-associated protein-specific serum immunoglobulin G-isotype expression in young foals protected against Rhodococcus equi pneumonia by oral immunization with virulent R. equi . Vaccine 23: 5760–5767. [DOI] [PubMed] [Google Scholar]
- 14. van der Geize R, Grommen AW, Hessels GI, Jacobs AA, Dijkhuizen L (2011) The steroid catabolic pathway of the intracellular pathogen Rhodococcus equi is important for pathogenesis and a target for vaccine development. PLoS Pathogens 7: e1002181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Arnold H, Bumann D, Felies M, Gewecke B, Sorensen M, et al. (2004) Enhanced immunogenicity in the murine airway mucosa with an attenuated Salmonella live vaccine expressing OprF-OprI from Pseudomonas aeruginosa. Infection and Immunity 72: 6546–6553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Villena J, Medina M, Raya R, Alvarez S (2008) Oral immunization with recombinant Lactococcus lactis confers protection against respiratory pneumococcal infection. Canadian Journal of Microbiology 54: 845–853. [DOI] [PubMed] [Google Scholar]
- 17. KuoLee R, Harris G, Conlan JW, Chen W (2007) Oral immunization of mice with the live vaccine strain (LVS) of Francisella tularensis protects mice against respiratory challenge with virulent type A F. tularensis. Vaccine 25: 3781–3791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Clark SO, Kelly DL, Badell E, Castello-Branco LR, Aldwell F, et al. (2010) Oral delivery of BCG Moreau Rio de Janeiro gives equivalent protection against tuberculosis but with reduced pathology compared to parenteral BCG Danish vaccination. Vaccine 28: 7109–7116. [DOI] [PubMed] [Google Scholar]
- 19. Tompkins DM, Buddle BM, Whitford J, Cross ML, Yates GF, et al. (2013) Sustained protection against tuberculosis conferred to a wildlife host by single dose oral vaccination. Vaccine 31: 893–899. [DOI] [PubMed] [Google Scholar]
- 20. Ancelet LR, Aldwell FE, Rich FJ, Kirman JR (2012) Oral vaccination with lipid-formulated BCG induces a long-lived, multifunctional CD4(+) T cell memory immune response. PLoS ONE 7: e45888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Garrido JM, Sevilla IA, Beltran-Beck B, Minguijon E, Ballesteros C, et al. (2011) Protection against tuberculosis in Eurasian wild boar vaccinated with heat-inactivated Mycobacterium bovis. PLoS ONE 6: e24905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Quan FS, Compans RW, Kang SM (2012) Oral vaccination with inactivated influenza vaccine induces cross-protective immunity. Vaccine 30: 180–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sealy R, Webby RJ, Crumpton JC, Hurwitz JL (2012) Differential localization and function of antibody-forming cells responsive to inactivated or live-attenuated influenza virus vaccines. Int Immunol. [DOI] [PMC free article] [PubMed]
- 24. Paillot R, Prowse L, Montesso F, Huang CM, Barnes H, et al. (2013) Whole inactivated equine influenza vaccine: Efficacy against a representative clade 2 equine influenza virus, IFNgamma synthesis and duration of humoral immunity. Vet Microbiol 162: 396–407. [DOI] [PubMed] [Google Scholar]
- 25. Mshvildadze M, Neu J (2010) The infant intestinal microbiome: friend or foe? Early Human Development 86 Suppl 167–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Murgas Torrazza R, Neu J (2011) The developing intestinal microbiome and its relationship to health and disease in the neonate. Journal of Perinatology 31 Suppl 1S29–34. [DOI] [PubMed] [Google Scholar]
- 27. Palmer C, Bik EM, DiGiulio DB, Relman DA, Brown PO (2007) Development of the human infant intestinal microbiota. PLoS Biology 5: e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Inman CF, Laycock GM, Mitchard L, Harley R, Warwick J, et al. (2012) Neonatal colonisation expands a specific intestinal antigen-presenting cell subset prior to CD4 T-cell expansion, without altering T-cell repertoire. PLoS ONE 7: e33707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Willing BP, Van Kessel AG (2007) Enterocyte proliferation and apoptosis in the caudal small intestine is influenced by the composition of colonizing commensal bacteria in the neonatal gnotobiotic pig. Journal of Animal Science 85: 3256–3266. [DOI] [PubMed] [Google Scholar]
- 30. Halbert ND, Reitzel RA, Martens RJ, Cohen ND (2005) Evaluation of a multiplex polymerase chain reaction assay for simultaneous detection of Rhodococcus equi and the vapA gene. American Journal of Veterinary Research 66: 1380–1385. [DOI] [PubMed] [Google Scholar]
- 31.Mashoof S, Goodroe A, Du CC, Eubanks JO, Jacobs N, et al.. (2012) Ancient T-independence of mucosal IgX/A: gut microbiota unaffected by larval thymectomy in Xenopus laevis. Mucosal Immunology. [DOI] [PMC free article] [PubMed]
- 32. Segata N, Izard J, Waldron L, Gevers D, Miropolsky L, et al. (2011) Metagenomic biomarker discovery and explanation. Genome Biol 12: R60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Garcia-Mazcorro JF, Dowd SE, Poulsen J, Steiner JM, Suchodolski JS (2012) Abundance and short-term temporal variability of fecal microbiota in healthy dogs. Microbiologyopen 1: 340–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Suchodolski JS, Markel ME, Garcia-Mazcorro JF, Unterer S, Heilmann RM, et al. (2012) The fecal microbiome in dogs with acute diarrhea and idiopathic inflammatory bowel disease. PLoS ONE 7: e51907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hochberg Y (1988) A sharper Bonferroni procedure for multiple tests of significance. Biometrika 75: 800–802. [Google Scholar]
- 36.Shannon CE, Weaver W (1963) The mathematical theory of communication. Urbana, IL: University of Illinois Press.
- 37. Chao A (1987) Estimating the population size for capture-recapture data with unequal catchability. Biometrics 43: 783–791. [PubMed] [Google Scholar]
- 38. Garcia-Mazcorro JF, Lanerie DJ, Dowd SE, Paddock CG, Grutzner N, et al. (2011) Effect of a multi-species synbiotic formulation on fecal bacterial microbiota of healthy cats and dogs as evaluated by pyrosequencing. FEMS Microbiol Ecol 78: 542–554. [DOI] [PubMed] [Google Scholar]
- 39. Venturi A, Gionchetti P, Rizzello F, Johansson R, Zucconi E, et al. (1999) Impact on the composition of the faecal flora by a new probiotic preparation: preliminary data on maintenance treatment of patients with ulcerative colitis. Aliment Pharmacol Ther 13: 1103–1108. [DOI] [PubMed] [Google Scholar]
- 40. Vitali B, Ndagijimana M, Cruciani F, Carnevali P, Candela M, et al. (2010) Impact of a synbiotic food on the gut microbial ecology and metabolic profiles. BMC Microbiol 10: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Jia J, Frantz N, Khoo C, Gibson GR, Rastall RA, et al. (2011) Investigation of the faecal microbiota of kittens: monitoring bacterial succession and effect of diet. FEMS Microbiol Ecol 78: 395–404. [DOI] [PubMed] [Google Scholar]
- 42. Minamoto Y, Hooda S, Swanson KS, Suchodolski JS (2012) Feline gastrointestinal microbiota. Animal Health Research Reviews 13: 64–77. [DOI] [PubMed] [Google Scholar]
- 43. Buddington RK (2003) Postnatal changes in bacterial populations in the gastrointestinal tract of dogs. Am J Vet Res 64: 646–651. [DOI] [PubMed] [Google Scholar]
- 44. Scholtens PA, Oozeer R, Martin R, Amor KB, Knol J (2012) The early settlers: intestinal microbiology in early life. Annu Rev Food Sci Technol 3: 425–447. [DOI] [PubMed] [Google Scholar]
- 45. Shepherd ML, Swecker WS Jr, Jensen RV, Ponder MA (2012) Characterization of the fecal bacteria communities of forage-fed horses by pyrosequencing of 16S rRNA V4 gene amplicons. FEMS Microbiology Letters 326: 62–68. [DOI] [PubMed] [Google Scholar]
- 46. Daly K, Stewart CS, Flint HJ, Shirazi-Beechey SP (2001) Bacterial diversity within the equine large intestine as revealed by molecular analysis of cloned 16S rRNA genes. FEMS Microbiology Ecology 38: 141–151. [Google Scholar]
- 47.Costa M, Sturgeon A, Arroyo LG, Staempfli H, Weese JS. The horse's 2nd genome; metagenomic investigation of the equine intestinal microbiome; 2011; Denver, Colorado.
- 48. Suchodolski JS (2011) Companion animals symposium: microbes and gastrointestinal health of dogs and cats. Journal of Animal Science 89: 1520–1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fanaro S, Chierici R, Guerrini P, Vigi V (2003) Intestinal microflora in early infancy: composition and development. Acta Paediatrica Supplement 91: 48–55. [DOI] [PubMed]
- 50.Smith P, MacDonald TT, Blumerg RS (2013) Principles of Mucosal Immunology. New York, NY: Garland Science. 529 p.
- 51. Dougal K, Harris PA, Edwards A, Pachebat JA, Blackmore TM, et al. (2012) A comparison of the microbiome and the metabolome of different regions of the equine hindgut. FEMS Microbiol Ecol 82: 642–652. [DOI] [PubMed] [Google Scholar]
- 52. Whitehead AE, Parreira VR, Hewson J, Watson JL, Prescott JF (2012) Development of a live, attenuated, potential vaccine strain of R. equi expressing vapA and the virR operon, and virulence assessment in the mouse. Vet Immunol Immunopathol 145: 479–484. [DOI] [PubMed] [Google Scholar]
- 53. Giguère S, Cohen ND, Chaffin MK, Slovis NM, Hondalus MK, et al. (2011) Diagnosis, treatment, control, and prevention of infections caused by Rhodococcus equi in foals. Journal of Veterinary Internal Medicine 25: 1209–1220. [DOI] [PubMed] [Google Scholar]