Abstract
Objective
The aim of this study is to demonstrate whether articaine hydrochloride administered alone as a single buccal infiltration in maxillary tooth removal, can provide favourable palatal anesthesia as compared to buccal and palatal injection of lidocaine.
Study Design
The study population consisted of 30 patients who were undergoing orthodontic treatment, and who required bilateral extraction of maxillary permanent premolars as per their orthodontic treatment plan. On the experimental side, 4 % articaine/HCl was injected into the buccal vestibule of the tooth to be extracted. On the control side, 2 % lignocaine HCl was injected both into the buccal and the palatal side of the tooth to be extracted. Following tooth extraction all patients completed a 100-mm visual analogue scale (VAS) and faces pain scale (FPS) to rate the pain on extraction.
Results
According to the VAS and FPS scores, the pain on extraction between buccal infiltration of articaine and the routine buccal and palatal infiltration of lignocaine was statistically insignificant.
Conclusions
The routine use of a palatal injection for the removal of permanent maxillary premolar teeth may not be required when articaine/HCl is used as the local anesthetic.
Keywords: Articaine, Lignocaine, Tooth extraction, Maxillary tooth extraction with buccal infiltration
Introduction
Pain on palatal injection is a very commonly experienced symptom in dentistry and as such is a major concern to dentist. A number of techniques may be used to reduce the discomfort of intra-oral injections [1, 2], the application of topical anesthetic being a well known and frequently used option. However, it is effective only on surface tissues (2–3 mm) and tissues deep to the area of application are poorly anesthetized. Surface anesthesia does allow for atraumatic needle penetration, but because of the density of the palatal soft tissues and their firm adherence to the underlying bone, palatal injection is still painful. It has been claimed that articaine is able to diffuse through soft and hard tissues more reliably than other local anesthetics and that maxillary buccal infiltration of articaine provides palatal soft tissue anesthesia, obviating the need for a palatal injection which in many hands, is traumatic.
This present paper reports a prospective, randomized trial designed to ascertain whether during the extraction of permanent maxillary premolar teeth a single buccal injection of articaine is as effective as the routine use of buccal and palatal injection of lignocaine.
Materials and Methods
A single blind cross-over study was conducted with 30 healthy subjects (19 women and 11 men) ranging in age from 10 to 30 years, who required bilateral extraction of maxillary permanent premolars as per their orthodontic treatment plan. During two separate appointments the subjects randomly received a buccal and palatal infiltration of 2 % lignocaine with 1:100,000 adrenaline and only buccal infiltration of 4 % articaine with 1:100,000 adrenaline. All injections were accomplished by one doctor, with slow injection (approximately 1 ml/min), resulting in greater safety and reduced trauma. None of the subjects were taking any medication that would alter pain perception. The study was approved by the Ethical Committee in Human Research at Pacific Dental College & Hospital, Udaipur; written informed consent was obtained from each subject.
The inclusion criteria were patients with bilateral extraction of permanent maxillary premolar teeth which are indicated for orthodontic extraction under local anesthesia. Exclusion criteria were allergy to sulphites or amide type local anesthetics, severe systemic disease contraindicating tooth extraction and inability to give informed consent.
In all the patients a through history was taken, clinical examination was done and preoperative radiographs were taken. Before administration of the local anesthetic, each patient was explained about visual analogue scale (VAS) [3] and faces pain scale (FPS) [4]. The VAS was composed of an unmarked, continuous, horizontal, 100-mm line, anchored by the end points of “no pain” on the right and “worst pain” on the left.
On the experimental side following test dose administration, the buccal mucosa is dried with cotton gauze. 2 % lidocaine hydrochloride gel is applied to the buccal injection site as topical anesthesia and then 1.7 ml of 4 % articaine hydrochloride with 1:100,000 adrenaline is injected at the buccal site. On the control side a similar protocol is followed except that after topical anesthetic application, 1.75 ml of 2 % lignocaine hydrochloride with 1:100,000 adrenaline is injected at the buccal site and a palatal injection of 0.25 ml is given.
After checking for the objective signs of local anesthesia using a sharp periosteal elevator, the premolars were extracted by using the forceps technique. During extraction patients were periodically questioned about pain. Following extraction all the patients were asked to score the pain experienced during extraction on FPS and a 100 mm VAS.
Results
In this study, a total of 30 patients, aged from 10 to 30 years participated. The mean age of the subjects who participated in this study was 17.73 ± 4.30 years. Three subjects in the articaine group aged 21, 26, and 28 years had slight pain during extraction. All the subjects in the lignocaine group had no pain on extraction (Table 1).
Table 1.
Age wise distribution of subjects
| Age group (years) | No. of subjects | No. of subjects with pain during extraction |
|---|---|---|
| 10–15 | 10 | 0 |
| 16–20 | 15 | 0 |
| 21–25 | 3 | 1 |
| 25–30 | 2 | 2 |
| Total | 30 | 3 |
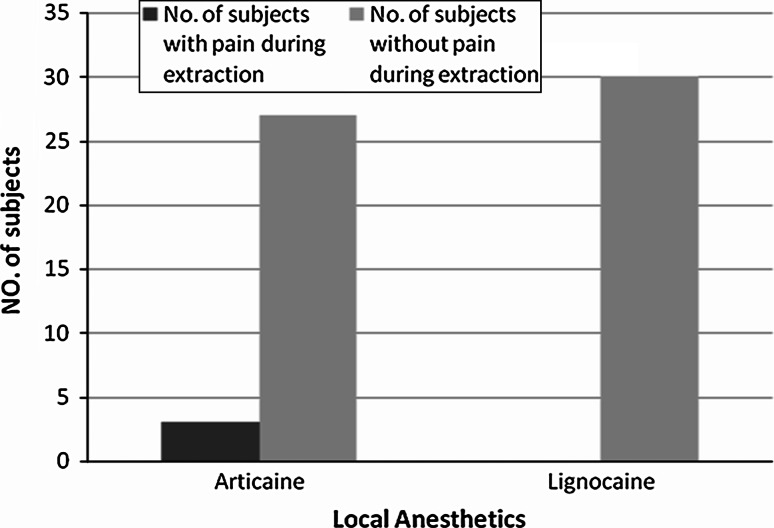
According to VAS and FPS scores (Table 2), three patients in the articaine group had mild pain and all the patients in the lignocaine group had no pain on extraction (Graph 1). When these pain scores were compared statistically by doing a Student t test the difference was statistically insignificant.
Table 2.
Number of patients who had pain according to VAS and FPS
| Groups | VAS | FPS |
|---|---|---|
| Articaine | 3 | 3 |
| Lignocaine | 0 | 0 |
Graph 1.
Comparison of patients with pain and without pain during extraction, in articaine group and lignocaine group
Discussion
Malamed et al. [5] evaluated the safety of 4 % articaine and 1:100,000 epinephrine with that of 2 % lidocaine and 1:100,000 epinephrine in 1,325 patients (882 in the articaine group, 443 in the lidocaine group) aged 4–80 years. Exclusion criteria included pregnancy, allergy or sensitivity to sulphites or amide-type local anesthetics, cardiac or neurologic disease, history of paroxysmal tachycardia, severe untreated hypertension or bronchial asthma, soft tissue infection at the site of injection, intake of analgesics within 24 h before administration of the anesthetic or maxillofacial surgery. The study concluded that Four percent articaine with 1:100,000 epinephrine provides effective anesthesia with a low risk of toxicity in both adults and children.
In this study the statistical analyses showed no significant difference in extraction pain for the visual analogue scale and faces pain scale scores of test and control sites. Hence it can be stated that palatal anesthesia achieved by depositing articaine to the buccal vestibule was as effective as palatal infiltration of lignocaine. This finding is in accordance with the study done by Sina et al. [1], Oertel et al. [6], Grace et al. [7] and Song et al. [8].
Hence permanent maxillary premolars can be extracted by giving only buccal infiltration with 4 % articaine, there by eliminating the need for a palatal injection.The mechanism of reversible nerve conduction block by articaine is similar to that of other amide local anesthetics. However, articaine is unique among them, because it contains a thiophene group, which increases its lipid solubility. Lipid solubility determines to what degree the molecules penetrate nerve membranes. Therefore, articaine diffuses better through soft tissues than do other anesthetics [9], thereby achieving higher intraneural concentration, more extensive longitudinal spreading, and better conduction blockade. This better nerve penetrating property of articaine is because it contains a thiophene ring unlike the benzene ring of lignocaine.
Potocnik et al. [10] in an in vitro study concluded that 2 and 4 % articaine is more effective than 2 % and 4 % lidocaine or 3 % mepivacaine in depressing the compound action potential of the A fibers in the isolated rat sural nerve. In addition, the thiophene derivative (carticaine) blocks ionic channels at lower concentrations than the benzene derivative (lidocaine) [11].
The higher concentration of articaine (4 %) compared to lidocaine (2 %) may also be a reason for adequate diffusional palatal anaesthesia. Oertel et al. [12] determined the concentration of 4 % articaine and 2 % lidocaine in alveolus blood using highperformance liquid chromatography. Blood samples were collected from the alveolus of upper molars 2 to 14 min after submucous injection of 4 % articaine and 2 % lidocaine (2 ml each). They postulated that higher blood levels found for articaine in alveolus blood compared to lidocaine was because of higher concentration of the drug in the injection solution.
In this study it was also noted that none of the younger subjects (below 20 years) in the articaine group had pain on extraction. This can be attributed to the fact that the maxillary bone becomes less porous and more sclerotic as age advances there by decreasing the bone penetrating effect of articaine.
Summary and Conclusion
In this study it can be summarized that the porous thin bone of the maxilla facilitates the diffusion of local anesthetics. Sufficient palatal tissue anesthesia can be provided using articaine as a maxillary buccal infiltration, since articaine diffuses more readily through soft and hard tissues than other local anesthetics. As the maxillary bone becomes more sclerotic with age, the bone penetrating efficacy of articaine may decrease.
References
- 1.Sina U, Dayangac E, Araz K, et al. Is permanent maxillary tooth removal without palatal injection possible? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:733–735. doi: 10.1016/j.tripleo.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 2.Henry H. Topical ice: a precursor to palatal injections. J Endod. 1989;15(1):27–28. doi: 10.1016/S0099-2399(89)80094-9. [DOI] [PubMed] [Google Scholar]
- 3.Amelia W, Barbara H. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14:798–804. doi: 10.1111/j.1365-2702.2005.01121.x. [DOI] [PubMed] [Google Scholar]
- 4.Bosenberg A, Thomas J, Lopez T, et al. Validation of a six-graded faces scale for evaluation of postoperative pain in children. Paediatr Anaesth. 2003;13:708–713. doi: 10.1046/j.1460-9592.2003.01142.x. [DOI] [PubMed] [Google Scholar]
- 5.Malamed SF, Gagnon S, Leblanc D. Articaine hydrochloride: a study of the safety of a new amide local anesthetic. J Am Dent Assoc. 2001;132:177–185. doi: 10.14219/jada.archive.2001.0152. [DOI] [PubMed] [Google Scholar]
- 6.Oertel R, Rahn R, Kirch W. Clinical pharmacokinetics of articaine. Clin Pharmacokinet. 1997;33:417–425. doi: 10.2165/00003088-199733060-00002. [DOI] [PubMed] [Google Scholar]
- 7.Grace E, John N, Melissa D, et al. A prospective, randomized, double-blind comparison of articaine and lidocaine for maxillary infiltrations. J Endod. 2008;34(4):389–393. doi: 10.1016/j.joen.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 8.Song F, Weiliang C, Zhao Y, et al. Comparison of the efficiencies of permanent maxillary tooth removal performed with single buccal infiltration versus routine buccal and palatal injection. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:359–363. doi: 10.1016/j.tripleo.2008.08.025. [DOI] [PubMed] [Google Scholar]
- 9.Tom VB, Gielen MJM. Clinical pharmacology and the use of articaine for local and regional anaesthesia. Best Pract Res Clin Anaesthesiol. 2005;19(2):293–308. doi: 10.1016/j.bpa.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 10.Potocnik I, Tomsic M, Sketelj J, Bajrovic FF. Articaine is more effective than lidocaine or mepivacaine in rat sensory nerve conduction block in vitro. J Dent Res. 2006;85(2):162–166. doi: 10.1177/154405910608500209. [DOI] [PubMed] [Google Scholar]
- 11.Borchard U, Drouin H. Carticaine: action of the local anesthetic on myelinated nerve fibres. Eur J Pharmacol. 1980;62:73–79. doi: 10.1016/0014-2999(80)90482-3. [DOI] [PubMed] [Google Scholar]
- 12.Oertel R, Richter K, Weile K, Gramatte T, Berndt A, Feller K. A simple method for the determination of articaine and its metabolite articainic acid in dentistry: application to a comparison of articaine and lidocaine concentrations in alveolus blood. Methods Find Exp Clin Pharmacol. 1993;15(8):541–547. [PubMed] [Google Scholar]