ABSTRACT
BACKGROUND
The Department of Veterans Affairs (VA) instituted the VA Women’s Health Fellowship (VAWHF) Program in 1994, to accommodate the health needs of increasing numbers of female veterans and to develop academic leaders in women’s health. Despite the longevity of the program, it has never been formally evaluated.
OBJECTIVE
To describe the training environments of VAWHFs and career outcomes of female graduates.
DESIGN AND PARTICIPANTS
Cross-sectional web-based surveys of current program directors (2010–2011) and VAWHF graduates (1995–2011).
RESULTS
Responses were received from six of seven program directors (86 %) and 42 of 74 graduates (57 %). The mean age of graduates was 41.2 years, and mean time since graduation was 8.5 years. Of the graduates, 97 % were female, 74 % trained in internal medicine, and 64 % obtained an advanced degree. Those with an advanced degree were more likely than those without an advanced degree to pursue an academic career (82 % vs. 60 %; P < 0.01). Of the female graduates, 76 % practice clinical women’s health and spend up to 66 % of their time devoted to women’s health issues. Thirty percent have held a VA faculty position. Seventy–nine percent remain in academics, with 39 % in the tenure stream. Overall, 94 % had given national presentations, 88 % had received grant funding, 79 % had published in peer-reviewed journals, 64 % had developed or evaluated curricula, 51 % had received awards for teaching or research, and 49 % had held major leadership positions. At 11 or more years after graduation, 33 % of the female graduates in academics had been promoted to the rank of associate professor and 33 % to the rank of full professor.
CONCLUSIONS
The VAWHF Program has been successful in training academic leaders in women’s health. Finding ways to retain graduates in the VA system would ensure continued clinical, educational, and research success for the VA women veteran’s healthcare program.
KEY WORDS: VA women’s health, fellowship, academic productivity, female leadership, women in academic medicine
INTRODUCTION
By 2033, women will compose 14.3 % percent of the armed forces, nearly doubling from 7.7 % in 2008. Women veterans have unique healthcare needs, underutilize the Department of Veterans Affairs (VA) health care services, receive fragmented and untimely care, and have higher mental and physical health burden when compared to their male counterparts.1
To address the needs of the expanding number of women veterans, the VA developed the Women’s Health Fellowship Program (VAWHF). Seven fellowship sites were established in 1994 to train physicians in clinical women’s health and academic medicine. Graduates were expected to become leaders in teaching, delivering patient care, and conducting research about health issues affecting women veterans.
Male and female faculty members with fellowship training have greater academic productivity and faster academic promotion than do their counterparts without fellowship training.2,3 However, women in academic medicine tend to have fewer publications, receive less funding, be promoted more slowly, and hold fewer leadership positions at all levels than do men.4–10 While the gender gap in academic medicine has been greatly reduced over the past 10 years, the medical community is still in dire need of female leaders. Women’s health research plays an integral role in developing female leaders, as women’s health interests lie mostly with female clinicians, researchers, and educators. For this reason, continued efforts to develop female leaders are expected to help advance women’s health care.11,12
Despite its longevity, the VAWHF Program has never been formally evaluated. By surveying its graduates and recent program directors, we aimed to identify the program’s curricular strengths and weaknesses, and to describe the graduates’ career paths, experiences, and perceptions about the adequacy of their fellowship training for a career in women veterans’ health and academic medicine.
As of May 2012, there were 25 women’s health fellowships (WHF) in the United States.13 However, there is considerable heterogeneity among the non-VA fellowships in their organization, department affiliation, clinical goals and expected scholarly productivity. Because we are unable to succinctly describe the heterogeneity of all fellowships, we will only evaluate the VAWHF programs in this paper.
METHODS
Study Approval and Participants
With approval from the Institutional Review Board of the VA Pittsburgh Healthcare System, we developed and conducted two cross-sectional surveys. Current program directors (2010–2011) and VAWHF fellows from 1995 to 2011 were surveyed.
Survey Design
Our team consisted of individuals with expertise in survey design, outcomes evaluation, curriculum development, teaching, mentoring, program administration, and women’s health. Surveys were administered online and included multiple-choice, short-answer, agree/disagree, and open-ended questions.
The survey for program directors consisted of 39 items concerning the characteristics of current and former fellows and the characteristics, organization, and evaluation of the fellowship program. Survey items were developed in collaboration with the Veterans Health Administration (VHA) Women Veterans Health Strategic Health Care Group.
The survey for fellows consisted of 60 items concerning four content areas: sociodemographic characteristics; fellowship logistics and training experiences; reflections on the adequacy of fellowship training; and career description and academic productivity. Content areas were identified by conducting a literature search of studies of academic physicians and fellows. Surveys were pilot-tested for clarity and face, content, and construct validity by five current fellows and two current faculty members not associated with the VAWHF program, in the Department of General Internal Medicine at the University of Pittsburgh.
Survey Recruitment, Administration, and Analysis
We obtained contact information for the seven program directors from the VHA Office of Academic Affiliations. Former fellows were identified using the VA national fellowship database. Although we consulted program directors, online search engines, and databases of university and professional societies to obtain the mailing or e-mail addresses of the 87 fellows, we could find contact information for only 77 fellows.
Program directors were invited to participate via e-mail. An embedded link within the e-mail was used to access the survey. Fellows were invited to participate using regular mailing addresses and e-mail addresses. Letters sent by regular mail alerted the fellows to the online survey link. Fellows’ responses were anonymous, while program directors’ responses were confidential but not anonymous. We sent follow-up reminders every 2 weeks. Participant consent was assumed if the directors or fellows accessed the survey link.
Program directors completed their survey during fall 2011 and January 2012. Fellows completed their survey from December 2011 to February 2012.
We used REDCap (Research Electronic Data Capture)14 to collect and manage the survey responses. We used descriptive statistics to report survey responses in terms of mean scores and frequencies, and we used chi-square tests to compare the responses of graduates who did and did not complete additional research training during their fellowship. Slide-rule questions were used to assess “adequacy of fellowship training,” which categorized the agreement with a question stem on a scale of 0–100, “0” representing “strongly disagree” and “100” representing “strongly agree.” The average number for responses per question is denoted as the “mean-agreement score” (MAS). This variable was further categorized into “disagree” (value of < 50), “agree” (50–75) and “strongly agree” (76–100).
RESULTS
Forty-five of 77 (58 %) former fellows and six of seven (86 %) program directors responded. Three respondents had not completed fellowship and the rest of their data were excluded, leaving a total of 74 graduates and a response rate of 57 % (42/74). Characteristics of graduates are represented in Table 1.
Table 1.
Sociodemographic Characteristics of the 42 Graduates of the VA Women’s Health Fellowship (VAWHF) Program
| Characteristic | Number (%) |
|---|---|
| Female (n = 39) | 38 (97) |
| Age, mean (range), years (n = 39) | 41.2 (31–50) |
| Time since completion of the VAWHF Program, mean (range), years (n = 41) | 8.5 (1–15) |
| Area of training (n = 42) | |
| Internal medicine | 31 (74) |
| Obstetrics and gynecology | 8 (19) |
| Other * | 3 (7) |
| Completed additional fellowship (n = 42) | 11 (26) |
| Area of additional fellowship (n = 11) | |
| Internal medicine specialty | 6 (55) |
| Obstetrics specialty | 2 (18) |
| Additional research fellowship | 2 (18) |
| Nonclinical specialty | 1 (9) |
| Main reasons for pursuing the fellowship (n = 39) | |
| Develop research skills | 25 (64) |
| Develop teaching skills | 19 (49) |
| Receive early career mentorship | 19 (49) |
| Become a more competitive applicant for a faculty position | 17 (44) |
| Improve clinical skills in women’s health | 16 (41) |
| Happy with decision to pursue fellowship (n = 39) | 38 (97) |
*Responses include medicine–pediatrics, psychiatry, and radiology
Fellowship Logistics and Training Experiences
Fellowship guidelines expect each fellow to develop an individual learning plan addressing long-term goals and resources to be used. Although the main academic goal identified by most directors was “research,” three of six reported that fellows could choose their own balance between research and educational activities. Fellows spent an average of 50 % of their time on research and scholarly activities, 20 % on clinical work, 20 % on class work, and 10 % on teaching. Eighty-one percent of graduated fellows completed in 2 years while 17 % completed in 3 years.
Sixty-four percent obtained an advanced degree/training during fellowship including Masters in Public/Population Health (33 %), Research (30 %), Education (15 %), and Epidemiology (7 %); 11 % obtained certificates in research and one pursued a PhD in population health science. The ability to pursue an advance degree influenced the decision to apply for fellowship in 55 % of cases and it was a “nice bonus” in an additional 17 %. Of the fellows that obtained an advanced degree/training, 82 % of them stayed in academics, compared to 60 % of those that did not pursue such training (p < 0.01). Five of six programs offer an advanced degree for fellows.
Program directors report a matriculation rate of 80 % of available fellowship slots since 1994. Half of the responding programs were always filled, and half of the responding programs have been underfilled. Chief reasons for unfilled slots were “lack of interest” (50 %) and “lack of qualified applicants” (33 %). Most graduates (55 %) report being recruited for fellowship by “word of mouth,” but some (38 %) sought the training opportunity independently. Directors used various forms of recruitment, including word of mouth (83 %), active recruitment from residency programs (67 %), publicity sent to various institutions (50 %), e-mail correspondence with residency program directors (33 %), and national/regional meetings (17 %). Of note, two of three underfilled programs identify “word-of-mouth” as their only recruitment strategy.
Reflections of VAWHF Graduates on the Adequacy of Fellowship Training
Mean agreement scores (MAS) regarding career outcomes, mentoring, and education, research, and career development skills showed that graduates generally found their VAWHF experiences to be positive (Table 2).
Table 2.
Responses of the 42 Graduates of the VA Women’s Health Fellowship (VAWHF) Program to Survey Items About Career Outcomes, Mentoring, and Adequacy of Fellowship Training
| Item | Response * † | Mean Agreement Score ‡ | ||
|---|---|---|---|---|
| Number (%) Who Disagree | Number (%) Who Agree | Number (%) Who Strongly Agree | ||
| Career outcomes | ||||
| Completing the VAWHF improved my career prospects (n = 40) | 0 (0) | 10 (25) | 30 (75) | 86 |
| I was more competitive for career positions as a result of completing the VAWHF (n = 38) | 1 (3) | 12 (32) | 25 (66) | 85 |
| I feel better trained than peers in academic medicine as a result of completing the VAWHF (n = 37) | 2 (5) | 14 (38) | 21 (57) | 78 |
| I am happy in my current career position (n = 40) | 2 (5) | 7 (18) | 31 (78) | 84 |
| I have encouraged others to apply for a VAWHF (n = 34) | 5 (15) | 4 (12) | 25 (74) | 81 |
| It was easy to find a position that matched my career goals (n = 40) | 5 (13) | 15 (38) | 20 (50) | 73 |
| Mentoring | ||||
| I was adequately mentored during my VAWHF (n = 38) | 3 (8) | 9 (24) | 26 (68) | 81 |
| It was easy for me to identify research mentors (n = 36) | 4 (11) | 12 (33) | 20 (56) | 79 |
| It was easy for me to identify career mentors (n = 39) | 7 (18) | 10 (26) | 22 (56) | 73 |
| Education skills: The VAWHF improved my ability to… | ||||
| Teach in small-group settings (n = 38) | 5 (13) | 15 (39) | 18 (47) | 73 |
| Give lectures (n = 39) | 5 (13) | 14 (36) | 20 (51) | 72 |
| Teach physical examination (n = 38) | 8 (21) | 22 (58) | 8 (21) | 60 |
| Write test questions (n = 30) | 14 (47) | 8 (27) | 8 (27) | 51 |
| Research skills: The VAWHF improved my ability to… | ||||
| Statistically evaluate data (n = 39) | 2 (5) | 11 (28) | 26 (67) | 82 |
| Interpret evidence-based medicine (n = 38) | 2 (5) | 8 (21) | 28 (74) | 81 |
| Present at national meetings (n = 39) | 4 (10) | 10 (26) | 25 (64) | 80 |
| Publish research articles (n = 38) | 4 (11) | 8 (21) | 26 (68) | 80 |
| Devise comprehensive research projects (n = 39) | 5 (13) | 11 (28) | 23 (59) | 75 |
| Apply for research grants (n = 39) | 8 (21) | 12 (31) | 19 (49) | 69 |
| Career development skills: The VAWHF improved my ability to… | ||||
| Mentor peers, junior faculty, residents, and students (n = 35) | 3 (9) | 12 (34) | 20 (57) | 76 |
| Write letters of recommendation (n = 34) | 7 (21) | 13 (38) | 14 (41) | 68 |
| Negotiate job contracts effectively (n = 38) | 17 (45) | 14 (37) | 7 (18) | 51 |
*Survey participants were asked to assign scores from 0 to 100 on a slide-rule scale, with 0 indicating “strongly disagree” and 100 indicating “strongly agree.” Scores were categorized as follows: disagree (< 50), agree (50–75), and strongly agree (76–100)
†Because of rounding, percentages may not total 100
‡The mean score was derived from numerical scores ranging from 0 to 100
Graduates agreed that completing their fellowship improved their career prospects, that they were adequately mentored, and that it was easy for them to identify research and career mentors. When asked about program strengths, 56 % cited mentorship.
Although graduates reported high levels of agreement with five aspects of research skill development, they believed that grant-writing skills were the least well developed during fellowship. On open-ended questions, some cited inadequate training in grant writing as a program weakness.
Graduates reported modest improvements in teaching small-group sessions and giving lectures, but little improvement on their perceived ability to teach physical examination write test questions, or effectively negotiate job contracts.
Career Description and Scholarly Activities of Female VAWHF Graduates
Overall, 76 % of female graduates practice clinical women’s health and 77 % teach women’s health to trainees. Graduates spend up to 66 % of their time devoted to women’s health issues. Most strongly agreed that they were encouraged to pursue careers in women’s health, and that fellowship improved their ability to provide high-quality women’s health care. In open-ended questions, 31 % indicated that didactics in women’s health and clinical opportunities for skill development were weaknesses at their fellowship site.
Career characteristics and scholarly activities of the female graduates are outlined in Table 3. Most graduates in academics identify as clinician-educators (52 %), followed by clinician-researchers (39 %), and clinician-administrators (9 %). On average, clinician-educators spent 33 % of their time on educational activities, clinician-researchers spent 56 % of their time conducting research, and clinician-administrators spent 25 % of their time on administrative duties.
Table 3.
Career Characteristics and Scholarly Activities of Female Graduates of the VA Women’s Health Fellowship (VAWHF) Program
| Career and Scholarly Activities | Number (%) of Female Graduates |
|---|---|
| Career | |
| Am currently holding an academic position (n = 39) | 31 (79) |
| Am in the tenure track (n = 31) | 12 (39) |
| Scholarly activities | |
| Presented one or more abstracts at a national meeting * (n = 36) | 34 (94) |
| Presented one or more workshops at a national meeting † (n = 36) | 22 (61) |
| Presented a plenary session at a national meeting (n = 36) | 5 (14) |
| Developed or evaluated a curriculum (n = 39) | 25 (64) |
| Wrote a grant proposal (n = 39) | 25 (64) |
| Of grant proposals written, at least one major grant was successfully funded (n = 25) | 22 (88) |
| Of successfully funded graduates, type of grant obtained (n = 23) | |
| K award | 10 (43) |
| R01 or R21 award | 7 (30) |
| VA career development award | 2 (9) |
| Institutional grant | 18 (78) |
| Foundation grant | 10 (43) |
| Other major federally funded award ‡ | 7 (30) |
| Published one or more peer-reviewed articles in a medical journal (n = 39) | 31 (79) |
| Won a teaching or research award (n = 39) | 20 (51) |
| Ever held a major leadership position (n = 39) | 19 (49) |
*Average number of abstracts presented = 8
†Average number of workshops presented = 4
‡Responses included Agency for Healthcare Research and Quality, Centers for Disease Control and Prevention, Department of Defense, industry, and VA Transformation–21 funding
Nearly half of female graduates have held a major leadership position (Table 3). Leadership positions included associate dean (1), associate department chair (1), division chief (4), section chief (2), associate chief medical officer (1), clinical medical director (3), director or assistant director of a residency or fellowship program (10), and clerkship director (5).
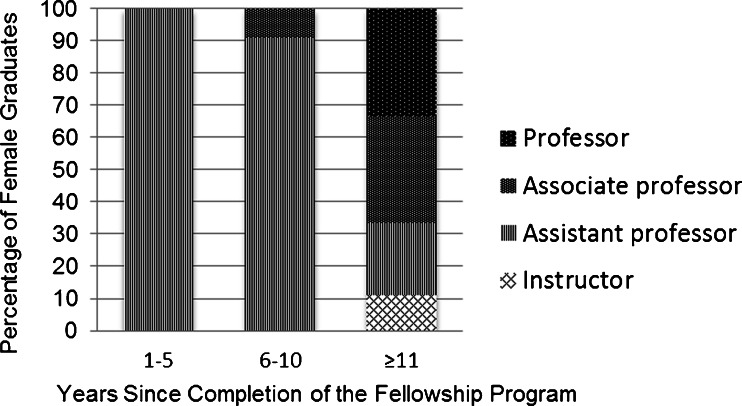
Everyone in academics held assistant professorships 1–5 years after fellowship completion, and the majority remained at this rank 6–10 years after fellowship completion; however, at ≥ 11 years after fellowship completion, 33 % had been promoted to associate professor and 33 % to full professor (Fig. 1).
Figure 1.
Academic rank of female graduates of the VA Women’s Health Fellowship (VAWHF) Program, stratified by years since completion of the program. Responses are shown for 11 graduates at 1–5 years, 11 graduates at 6–10 years, and nine graduates at ≥ 11 years.
Thirty percent of female graduates reported holding a VA faculty position since graduation. Reasons for not pursuing a VA career included lack of a position available for career needs (43 %), not enough clinical women’s health opportunities (13 %), and lack of a teaching or research role (10 %). Most graduates did not feel that they were encouraged to pursue a VA career after their fellowship (MAS = 49).
DISCUSSION
Our study reports the results of the first formal evaluation of training experiences and career outcomes of VAWHF graduates. Although the VAWHF Program has open enrollment for men and women, most graduates have been women, so our findings offer unique insights into the program’s success in developing female academic leaders.
Our data indicate that the overall VAWHF goals of developing leaders in women’s health and academics are being met. Graduates of the VAWHF Program are highly involved in administering, researching, and teaching women’s health, and are holding academic positions in percentages similar to those of other fellowship-trained populations with predominantly male graduates. For example, 79 % of VAWHF fellows, 76 % of pediatrics fellows (47 % of whom are female),15 and 76 % of family medicine fellows (gender % unknown)16 held academic positions after completion of their fellowship.
The data related to VAWHF graduates are particularly impressive, given that women still comprise only 35 % of all academic physicians17 and that during their career, only 26 % of women will be promoted from assistant to associate professor and only 34 % will be promoted from associate to full professor.10 In 1995, while 59 % of women who were in academic medicine for ≥ 11 years had achieved the rank of associate or full professor, only 5 % had become full professors.18 The promotion rates of female VAWHF graduates at ≥ 11 years were considerably higher than these rates, and were also higher than the 26 % professorship rate at ≥ 15 years that was reported for pediatrics fellows (only 47 % female).15 The fact that nearly half of VAWHF female graduates have held major leadership positions is also impressive, given that the average time since fellowship completion was 8.5 years, and that in 2009 women in academia held only 21 % of division and section chief positions, 13 % of department chairs, and 13 % of deanships.17
Two key aspects of fellowship training that contributed strongly to career success are early career mentorship and obtaining an advanced degree. Studies have show that women are less likely than men to have a mentor and that mentoring is associated with publishing, receiving research funds, and overall career success.19,20 All but three VAWHF graduates felt adequately mentored during their fellowship. Graduates found it easier to identify research mentors than career mentors. This could be because both men and women typically serve as research mentors, where as women have a smaller female pool of mentors available for career and professional–personal balance mentorship.21 Our study found that 91 % of graduates agreed that their fellowship improved their ability to mentor others, a skill that will be vital for the next generation of women in academic medicine. Our study also reinforced that an advanced degree earned during fellowship can contribute positively to academic success.2,22 The training environment of the VAWHFs may have helped neutralize the barriers that women typically face when pursuing an academic career, and may explain why the productivity and promotion rates of VAWHF graduates are comparable to those of graduates of male-dominated academic fellowship programs.15,23
All fellowship sites are equipped to provide high-quality primary care for female veterans. VAWHF graduates strongly agreed that their fellowship improved their ability to provide high-quality clinical women’s health for patients. However, in open-ended questions, one-third indicated that didactics in women’s health and clinical opportunities were weaknesses at their fellowship site. Because most VA facilities do not provide obstetrical care for veterans or have fully staffed gynecology services, clinical exposure to reproductive care is difficult. Collaborating with neighboring hospitals and universities to expand clinical training opportunities would be beneficial, as would providing a standardized women’s health clinical curriculum for all VAWHFs
Although more graduates pursued careers as educators than as researchers, they reported that their fellowship did not improve their educational skills as much as it improved their research skills. This reflects the strong research focus of VAWHFs. A major factor that attracts women to academic medicine is an interest in teaching.24 An enhanced focus on training medical educators could improve recruitment of fellows and retention in academics. This is particularly important now, given the continued need for visible female leadership in medicine and the decreasing rate of female matriculants to medical school since 2003.17
Grant-writing skills contribute to funding, publication, and promotion, but training in these skills is often inadequate.25 It is clear from our data that fellows want more dedicated training in grant writing; thus, curricular initiatives in this area should be explored. Suboptimal training in grant writing may help explain why VAWHF graduates are more likely to pursue a career in education than research.
Some programs have struggled with recruitment of VAWHF candidates. This may be due to competition from 18 non-VA WHF programs13 or to the lack of visibility of VAWHFs. It is easier for an institution to recruit from its own residency programs, but only one VAWHF site is affiliated with an institution that offers a dedicated women’s health track for residents. This makes it important for the VAWHF Program to increase its visibility to individuals interested in academic women’s health by tailoring its recruitment efforts at national meetings, advertising in journals, and corresponding with directors of residency programs.
Thirty percent of graduates have held a faculty position at the VA since fellowship. This retention rate for graduates of the VAWHF Program is comparable to the 31 % rate for graduates of the VA National Quality Scholars Fellowship Program.26 Data from our study suggest that graduates were not successful in finding desirable career opportunities within the VA health care system, which in part may be due to lack of clinical or research opportunities in women’s health. Data show that female veterans obtain most of their healthcare outside of the VA Healthcare System.27 Retention of these highly trained fellows in women veterans’ healthcare could be improved by recruitment of female veterans back to the VA via programs that are already in place. These programs provide information to female veterans regarding healthcare eligibility and expansion of women’s health services in deficient areas. There is a growing need for competent women’s health physicians and researchers to accommodate the increasing number of female veterans, and recruitment of graduating fellows should become a priority of the VA Healthcare System.
Our study had several limitations. First, the response rates were 86 % for program directors and 57 % for graduates. The modest rate for graduates was partially attributable to the inability to verify contact information. Second, although the seven VAWHF sites have a common funding source, they differ greatly in program structure and curriculum. We could not account for this variability in our analysis, since the number of graduates who responded from each site ranged from two to 13. Third, we did not verify the graduates’ answers to questions regarding academic productivity, so the results may reflect recall bias. Responder bias is likely, given that the most successful graduates may have been more likely to respond, as Szilagyi and colleagues found when surveying pediatrics fellows.15 However, by using public databases, we were able to determine that three non-responders had first-author publications and other evidence of successful academic careers. Fourth, some fellows graduated more than 15 years ago, making reflections on the fellowship curriculum and training difficult. Lastly, we do not intend to convey that the success of the VAWHF graduates is solely due to the training program, as a large part of academic success may lie within the motivation of the individual; however, there is something exceptional about the training environments of the VAWHFs, as these graduates are surpassing other academic graduates in terms of productivity and academic promotion.
CONCLUSIONS
The VAWHF Program has been successful in training leaders in women’s health while producing exceptional female role models in academic medicine. VAWHF female graduates are likely to stay in academics, practice and teach women’s health, show high academic productivity, and half hold major leadership positions with promotion rates well above that reported in the literature. Opportunities for curricular innovation include better training in clinical women’s health, grant writing, and educational skills. Despite their success, open slots in these fellowships remain available, which may be related to recruitment, lack of interest, and paucity of qualified candidates. Finding ways to retain these graduates in the VA system would ensure continued clinical, educational, and research success for the VA women Veterans’ healthcare program.
Acknowledgements
Contributors
For their support in this project, we are grateful to members of the VHA Women Veterans Health Strategic Health Care Group and, in particular, to Dr. Laure Veet. Please note that the views expressed in this article are of the authors, and do not necessarily reflect the position or policy of the VA Healthcare System, Department of Defense or United States government.
Prior Presentations
These data were presented at the annual meeting of the Society of General Internal Medicine, May 2012, Orlando, Florida.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1."Report of the Under Secretary for Health Workgroup on Provision of Primary Care to Women Veterans." Women Veterans Health Strategic Health Care Group, Office of Public Health and Environmental Hazards; October 2008. Veterans Health Administration, Washington, DC.
- 2.Ferrer RL, Katerndahl DA. Predictors of short-term and long-term scholarly activity by academic faculty: a departmental case study. Fam Med. 2002;34:455–61. [PubMed] [Google Scholar]
- 3.Taylor JS, Friedman RH, Speckman JL, Ash AS, Moskowitz MA, Carr PL. Fellowship training and career outcomes for primary care physician-faculty. Acad Med. 2001;76:366–72. doi: 10.1097/00001888-200104000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Amrein K, Langmann A, Fahrleitner-Pammer A, Pieber TR, Zollner-Schwetz I. Women underrepresented on editorial boards of 60 major medical journals. Gend Med. 2011;8:378–87. doi: 10.1016/j.genm.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Reed DA, Enders F, Lindor R, McClees M, Lindor KD. Gender differences in academic productivity and leadership appointments of physicians throughout academic careers. Acad Med. 2011;86:43–7. doi: 10.1097/ACM.0b013e3181ff9ff2. [DOI] [PubMed] [Google Scholar]
- 6.Morton MS, Sonnad SS. Women on professional society and journal editorial boards. J Natl Med Assoc. 2007;99:764–71. [PMC free article] [PubMed] [Google Scholar]
- 7.Jagsi R, Motomura AR, Griffith KA, Rangarajan S, Ubel PA. Sex differences in attainment of independent funding by career development awardees. Ann Intern Med. 2009;151:804–11. doi: 10.7326/0003-4819-151-11-200912010-00009. [DOI] [PubMed] [Google Scholar]
- 8.Jagsi R, Guancial EA, Worobey CC, et al. The "gender gap" in authorship of academic medical literature–a 35-year perspective. N Engl J Med. 2006;355:281–7. doi: 10.1056/NEJMsa053910. [DOI] [PubMed] [Google Scholar]
- 9.Nonnemaker L. Women physicians in academic medicine: new insights from cohort studies. N Engl J Med. 2000;342:399–405. doi: 10.1056/NEJM200002103420606. [DOI] [PubMed] [Google Scholar]
- 10.Liu CQ AH. Promotion rates for first-time assistant and associate professors appointed from 1967 to 1997. Analysis in Brief, AAMC 2010;9.
- 11.Carnes M, Morrissey C, Geller SE. Women's health and women’s leadership in academic medicine: hitting the same glass ceiling? J Womens Health (Larchmt) 2008;17:1453–62. doi: 10.1089/jwh.2007.0688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Council on Graduate Medical Education Fifth Report. Women and Medicine. 1995. US Department of Health and Human Services PHSHRaSA.
- 13.Directory of Residency and Fellowship Programs in Women's Health Association of Academic Women's Health Programs. J Womens Health (Larchmt) 2012;21:569–608. doi: 10.1089/jwh.2012.DIR6. [DOI] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Szilagyi PG, Haggerty RJ, Baldwin CD, et al. Tracking the careers of academic general pediatric fellowship program graduates: academic productivity and leadership roles. Acad Pediatr. 2011;11:216–23. doi: 10.1016/j.acap.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Anderson WA, Stritter FT, Mygdal WK, Arndt JE, Reid A. Outcomes of three part-time faculty development fellowship programs. Fam Med. 1997;29:204–8. [PubMed] [Google Scholar]
- 17.Leadley J SR. Women in US Academic Medicine: Statistics and Benchmarking Report 2009-2010. Association of American Medical Colleges.
- 18.Tesch BJ, Wood HM, Helwig AL, Nattinger AB. Promotion of women physicians in academic medicine. Glass ceiling or sticky floor? JAMA. 1995;273:1022–5. doi: 10.1001/jama.1995.03520370064038. [DOI] [PubMed] [Google Scholar]
- 19.Stamm M, Buddeberg-Fischer B. The impact of mentoring during postgraduate training on doctors' career success. Med Educ. 2011;45:488–96. doi: 10.1111/j.1365-2923.2010.03857.x. [DOI] [PubMed] [Google Scholar]
- 20.Levine RB, Mechaber HF, Bass EB, Wright SM. The impact of working part-time on measures of academic productivity among general internists. J Womens Health (Larchmt) 2010;19:1995–2000. doi: 10.1089/jwh.2009.1890. [DOI] [PubMed] [Google Scholar]
- 21.Levine RB, Lin F, Kern DE, Wright SM, Carrese J. Stories from early-career women physicians who have left academic medicine: a qualitative study at a single institution. Acad Med. 2011;86:752–8. doi: 10.1097/ACM.0b013e318217e83b. [DOI] [PubMed] [Google Scholar]
- 22.Guttman OR, Lingard L. Credentials as cultural capital: the pursuit of higher degrees among academic medical trainees. Acad Med. 2010;85:S21–4. doi: 10.1097/ACM.0b013e3181ed4097. [DOI] [PubMed] [Google Scholar]
- 23.Simon SR, Shaneyfelt TM, Collins MM, Cook EF, Fletcher RH. Faculty training in general internal medicine: a survey of graduates from a research-intensive fellowship program. Acad Med. 1999;74:1253–5. doi: 10.1097/00001888-199911000-00022. [DOI] [PubMed] [Google Scholar]
- 24.Borges NJ, Navarro AM, Grover AC. Women physicians: choosing a career in academic medicine. Acad Med. 2012;87:105–14. doi: 10.1097/ACM.0b013e31823ab4a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Orlander JD, Callahan CM. Fellowship training in academic general internal medicine: a curriculum survey. J Gen Intern Med. 1991;6:460–5. doi: 10.1007/BF02598172. [DOI] [PubMed] [Google Scholar]
- 26.Splaine ME, Ogrinc G, Gilman SC, et al. The Department of Veterans Affairs National Quality Scholars Fellowship Program: experience from 10 years of training quality scholars. Acad Med. 2009;84:1741–8. doi: 10.1097/ACM.0b013e3181bfdcef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yano EM, Hayes P, Wright S, et al. Integration of women veterans into VA quality improvement research efforts: what researchers need to know. J Gen Intern Med. 2010;25(Suppl 1):56–61. doi: 10.1007/s11606-009-1116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]