Abstract
Left-sided portal hypertension (LSPH) followed by acute pancreatitis is a rare condition with most patients being asymptomatic. In cases where gastrointestinal (GI) bleeding is present, however, the condition is more complicated and the mortality is very high because of the difficulty in diagnosing and selecting optimal treatment. A successfully treated case with severe GI bleeding by transcatheter splenic artery embolization is reported in this article. The patient exhibited severe uncontrollable GI bleeding and was confirmed as gastric varices secondary to LSPH by enhanced computed tomography (CT) scan and CT-angiography. After embolization, the bleeding stopped and stabilized for the entire follow-up period without any severe complications. In conclusion, embolization of the splenic artery is a simple, safe, and effective method of controlling gastric variceal bleeding caused by LSPH in acute pancreatitis.
Keywords: Left-sided portal hypertension (LSPH), Gastric varices, Acute pancreatitis, Gastrointestinal bleeding, Splenic artery embolization (SAE)
1. Introduction
Gastrointestinal (GI) bleeding is the most common cause of death for acute pancreatitis patients. Left-sided portal hypertention (LSPH) is a rare cause of GI bleeding, which is characterized as splenomegaly, isolated gastric varices, and normal liver condition (Moossa and Gadd, 1985; Madsen et al., 1986; Ito et al., 2008). Sixty percent of cases are followed by pancreatitis, specifically chronic pancreatitis, accompanied by splenic venous thrombosis (SVT) (Madsen et al., 1986), and may progress into severe GI bleeding. Despite the development of treatment for acute pancreatitis, the emergent bleeding of gastric varices has a high mortality rate because of its rarity and the poor systemic condition of these patients. It remains a challenge for clinicians to make the right decision on the diagnosis and treatment of this condition (Ou et al., 2005). In the present study, we report a case who suffered from acute pancreatitis with emergent GI bleeding caused by gastric varices associated with LSPH, and was successfully treated with transcatheter splenic artery embolization (SAE) without any severe complications. The clinical presentation and management resulting in a full recovery are described.
2. Case report
The case report and analysis has got the permission of the patient.
A 34-year-old Chinese woman was hospitalized by ambulance in Xinchang People’s Hospital (Zhejiang, China) because of acute epigastric pain accompanied with vomiting yellow fluid. Biochemical analysis revealed a high level of the amylase: 2 090 U/L in urine (normal level 50–600 U/L) and 304 U/L in blood (normal level 20–120 U/L). Enhanced computed tomography (CT) scan showed inflammation of the pancreas with severe effusion of the peripancreatic tissue and splenomegaly. Thus, she was diagnosed as having acute pancreatitis and received standard treatment. Ten days later, severe hematochezia and hematemesis occurred with a hemoglobin level of 67 g/L. Emergency upper GI endoscopy failed to reveal the site of bleeding but noted moderate varices at the fundus of the stomach. She then received two units of packed red blood cells and underwent extensive treatment for three days. The bleeding persisted and she was referred to our hospital and admitted into the Surgery Intensive Care Unit.
She presented no history of hepatitis, gallbladder stones, or hepatic stones. She also has no history of alcohol abuse.
Upon admission, she was fully alert with a blood pressure of 103/62 mmHg, pulse rate of 88 beats/min, and body temperature of 37.4 °C. Physical examination was normal except for a pale conjunctiva and mild tenderness of the upper abdomen and periumbili. No sign of peritonism was observed. She then underwent extensive observation and examination, and received anti-acid, anti-infection, hemostatic, and nutritional support therapy.
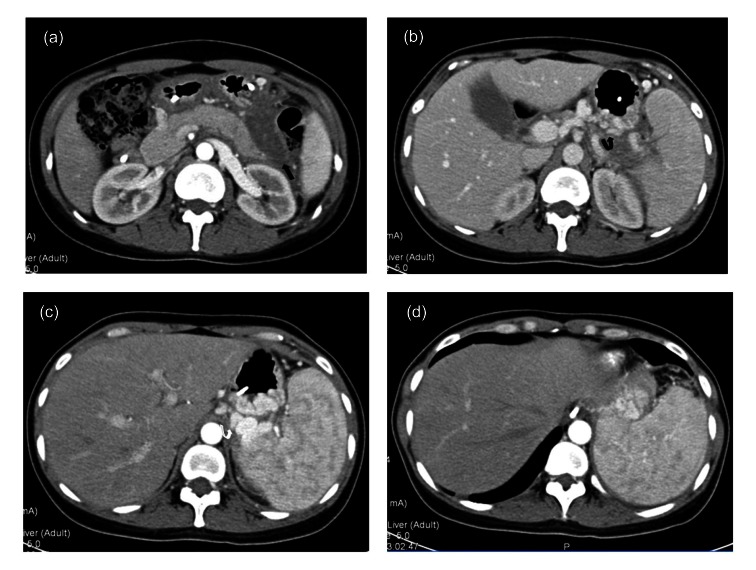
CT scan with contrast showed an edematous area around the pancreas, with peripancreatic effusion, but no pseudocysts or other masses around the pancreas were noted (Fig. 1a). Severe, tortuous gastric and perisplenic varices were presented in Figs. 1b and 1c. The spleen was extremely enlarged but no sign of splenic vein thrombosis (SVT) was noted (Fig. 1d).
Fig. 1.
Enhanced computed tomography (CT) images of the pancreas of the patient
(a) An edematous area around pancreas with peripancreatic fat stranding and fluid (black arrow); (b, c) Severe, tortuous gastric (black curved arrow) and perisplenic varices (white curved arrow) were present; (d) The spleen was extremely enlarged without sign of splenic vein thrombosis (SVT)
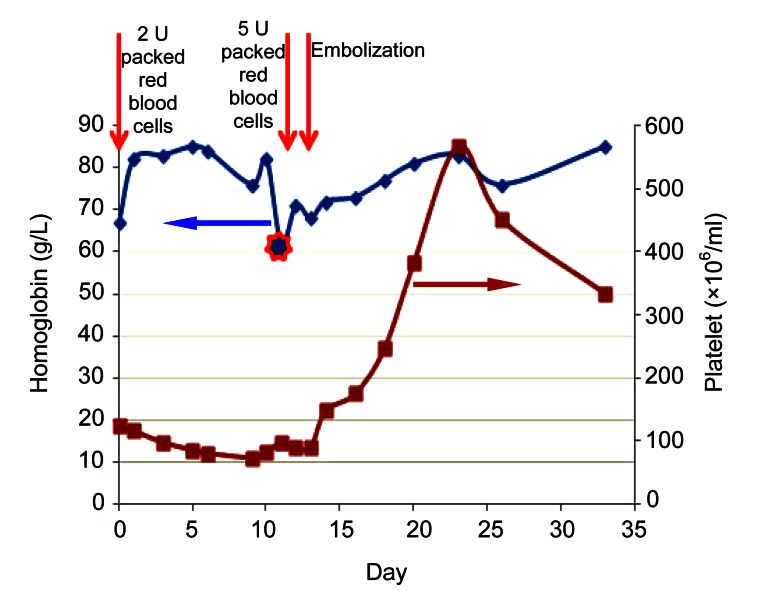
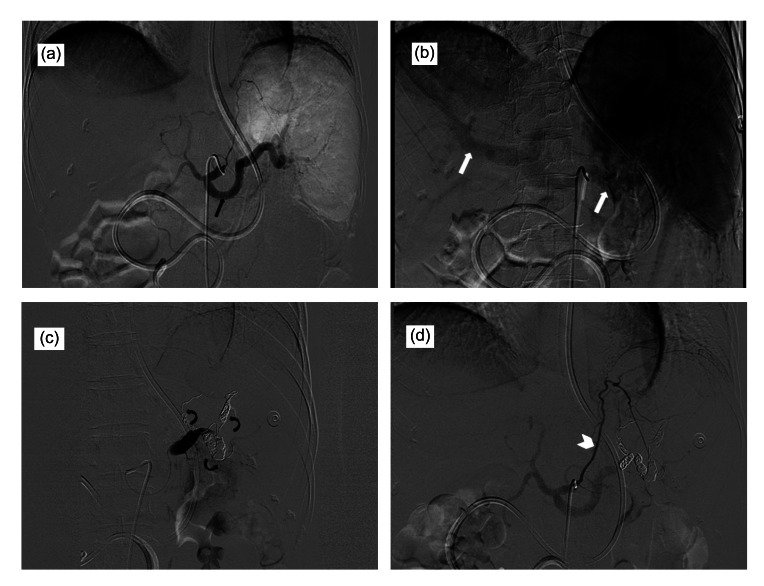
After receiving two units of packed red blood cells, her condition settled on conservative treatment for 10 d with hemoglobin levels fluctuating around 80 g/L (Fig. 2) without hematemesis, but with persistent hematochezia and the platelet count continuously declining. Ten days after admission, she began to vomit blood. Her hemoglobin level fell to 62 g/L and could not rise even after receiving 5 units of packed red blood cells. Emergent digital subtraction angiography (DSA) revealed an enlarged spleen and distorted veins around the spleen, but failed to reveal the site of bleeding (Figs. 3a and 3b). The patient was finally referred for interventional radiologic procedures. To prevent the drop off of the embolization materials, they were injected into the splenic artery and anchored to the branch arteries to completely stop the blood flow (Fig. 3c). After the procedure, though the bypass vessels of gastroduodenal artery to the spleen were still open (Fig. 3d), GI bleeding gradually stopped, and the platelet count increased from 82×106/ml to 568×106/ml in 10 d, which gradually decreased to nearly normal level in 20 d when the patient recovered and discharged from the hospital (Fig. 2). The patient complained of slight pain in her upper abdomen without any fever and other infection symptoms, which was managed by medications and nearly undetecable at the time of discharge.
Fig. 2.
Changes of homoglobin and platelet levels of the patient in the treatment
The patient received two units of packed red blood cells immediately after her arrival to our hospital, as shown by hemoglobin level, her condition settled on conservative treamtment for 10 d. The level of hemoglobin fell to 62 g/L (star) and could not rise even after receiving 5 unit of packed red blood cells at Day 11. The platelet level was fluctuated around 100×106/ml at the beginning. After embolization of splenic artery, the platelet count increased from 82×106/ml to 568×106/ml in 10 d, and decreased to nearly normal at the day of leaving our hospital
Fig. 3.
Emergent digital subtraction angiography (DSA) of the patient
(a) Presented enlarged spleen and artery (black arrow); (b) Presented distorted veins around the spleen (white arrow); (c) Embolization materials were injected into the splenic artery and anchored to the branch arteries for completely stopping the blood flow (black curved arrows); (d) The bypass vessels to the spleen were still open (white arrow head)
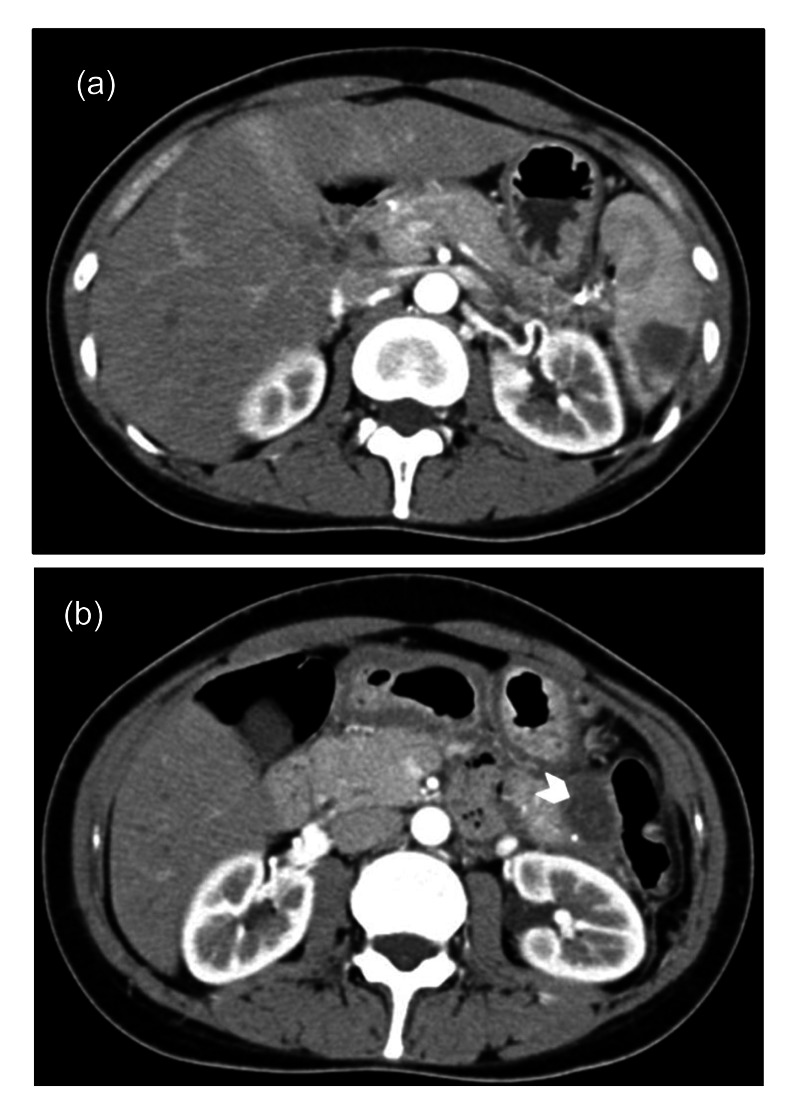
During a five-month follow-up period, enhanced CT scan was carried out. The scan revealed that the patient’s spleen was partially infracted and much smaller compared to her initial hospital admission. The size and number of gastric varices also decreased which was confirmed by GI endoscopy examination. There was an area of encapsulated effusion near the tail of the pancreas which may have been related to the pancreatitis and should be observed for a period (Fig. 4). There was no recurrence of upper GI bleeding or no associated severe complication for more than five months until now.
Fig. 4.
Enhanced CT scan during the follow-up period, three months after her discharge
(a) The pancreas was intact with smooth envelop, and the spleen was partially infracted and was much smaller than that of three months ago. There was no sign of thrombosis in the portal vein. (b) There was encapsulated effusion in the left abdomen near the tail of pancreas (white arrow head)
3. Discussion
LSPH, also known as sinistral or linear portal hypertension, is a rare clinical syndrome characterized by splenomegaly, isolated vein varices, and normal liver condition (Moossa and Gadd, 1985; Madsen et al., 1986; Ito et al., 2008). In most cases, the varices are formed in the fundus of the stomach, while sometimes the esophageal is involved (Weber and Rikkers, 2003), which could lead to severe GI bleeding. Most commonly, LSPH is asymptomatic and is diagnosed occasionally by examinations for other diseases (Bradley, 1986). While in symptomatic cases, GI bleeding is the most common symptom occurring in about 45%–72% of patients with LSPH (Moossa and Gadd, 1985; Madsen et al., 1986). Acute pancreatitis associated upper GI bleeding is the most rapidly fatal complication of acute pancreatitis, with a reported fatal frequency of 1.2%–14.5% (Stabile et al., 1983; Flati et al., 2003). One of the most important reasons for this high mortality is that usually it is difficult to find the location of bleeding in these cases. Arterial erosion or pseudoaneurysms, ischaemic complications, and gastritis are the most common causes for a hemorrhage. Bleeding as a result of LSPH is even more dangerous because of the difficulty of diagnosis, treatment decision, and high recurrence rate (Balthazar, 2002). In the present study, we reported a case of LSPH caused by acute pancreatitis which suffered from fatal GI bleeding because of local gastric varices and failed to respond to medical therapy. It was successfully diagnosed by endoscopy examination, enhanced CT scan, and CT angiography, and treated using SAE with a complete recovery for more than five months.
LSPH is usually caused by SVT following acute or chronic pancreatitis or pancreatic carcinoma, which could alter the venous anatomy, reverse the direction of the gastric venous blood flow, and increase the pressure within the submucosal veins of the gastric fundus (Butler et al., 2011). In the present case, however, according to the CT angiography and enhanced CT scan, no sign of SVT or extrinsic compression was found. They only showed an edematous area around the pancreas with peripancreatic fat stranding and fluid, and the extremely tortuose and dialated splenic vein. Besides, the time between the onset of pancreatitis and bleeding was only 10 d. It implys that local inflammation without SVT or extrinsic compression could also induce severe LSPH and GI bleeding in a short time. According to Evans et al. (1990) and Butler et al. (2011), the incidence of SVT-related LSPH is up to 45% in patients with pancreatitis, with the frequency of GI bleeding ranging from 37%–100% in these studies (Johnston and Myers, 1973; Little and Moossa, 1981; Keith et al., 1982; Evans et al., 1990), while Heider et al. (2004) reported that only 4% of patients with pancreatitis-induced SVT developed clinically evident, gastric variceal bleeding. A recent meta-analysis by Butler et al. (2011), which reviewed 38 articles related to pancreatitis-induced SVT, exhibited that the incidence of SVT in acute pancreatitis was much higher than that in chronic pancreatitis (22.6% vs. 12.4%), but the bleeding rate was similar (6.7% vs. 6.9%). This discrepancy of LSPH incidence and hemorrhage rate may be related to the development and prevalence of CT scan and angiography which made the diagnosis of SVT without severe symptoms much easier (Sakorafas et al., 2000). The enhanced CT scan and angiography were also carried out for our patients, which made it possible for us to accurately diagnose the disease and promptly deliver effective treatment.
According to the collected data, most LSPH patients are asymptomatic, so observing without surgery would be the best choice for them. However, in the situation of gastric variceal bleeding, the mortality rate is as high as 52% at one year (Kim et al., 1997; McCormick and O′Keefe, 2001), which is much higher than other causes of GI bleeding because of the difficulty of endoscopic approach and high recurrence rate. More radical treatment should be recommended in this situation. Until now, optimal therapy remains controversial, with splenectomy being the first-line of treatment (Bernades et al., 1992). Embolization of the splenic artery has been shown as an alternative method which has the same effects as a splenectomy (Shah et al., 1990; Ou et al., 2005). Moreover, it can avoid some severe complications such as postsplenectomy sepsis, or uncontrolled increase of platelet count because of the residual noninfarcted spleen. Koconis et al. (2007) reported that partial splenic embolization made efficacious improvements on the bleeding and hematologic parameters for partial hypertension patients, and the associated morbidity and mortality were acceptable. Petermann et al. (2012) and Gaba et al. (2013) both reported that the overall observed complication rate was around 33%–52%. However, since most of the complications included fever, leukocytosis, abdominal pain, and hydrothorax which have no clinical consequence, we believe that they are best classified as side effects (rather than complications). The most severe procedure-related complications were splenic abscesses and thrombosis of portal vein system. Our patient received emergent CT-guided SAE immediately after the deterioration of GI bleeding. After embolization, the GI bleeding gradually stopped and was stable for more than five months. The platelet count decreased to nearly normal levels at the time discharge. The patient complained only of an appropriate amount of abdominal pain during hospitalization without any severe complications.
4. Conclusions
In summary, LSPH followed by acute pancreatits is a rare condition, which is usually asymptomatic. However, in the cases with GI bleeding, the condition is more complicated and the mortality is very high. Timely and correct diagnosis followed by optimized treatment selection is the key for improving the prognosis. According to our experience of successfully treating an LSPH patient with severe GI bleeding, we concluded that: (1) common enhanced CT scan and angiography provide accurate and timely diagnosis; (2) splenic artery embolization is a simple, safe and effective method of controlling gastric variceal bleeding caused by LSPH in acute pancreatitis.
Footnotes
Project supported by the National Natural Science Foundation of China (No. 30901445), the Zhejiang Provincial Natural Science Foundation (No. Y2100285), and the Specialized Research Fund for the Doctoral Program of Higher Education (No. 20090101120122), China
Compliance with ethics guidelines: Zhi-yu LI, Bin LI, Yu-lian WU, and Qiu-ping XIE declare that they have no conflict of interest.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000(5). Informed consent was obtained from the patient for being included in the study.
References
- 1.Balthazar EJ. Complications of acute pancreatitis: clinical and CT evaluation. Radiol Clin North Am. 2002;40(6):1211–1227. doi: 10.1016/S0033-8389(02)00043-X. [DOI] [PubMed] [Google Scholar]
- 2.Bernades P, Baetz A, Lévy P, Belghiti J, Menu Y, Fékété F. Splenic and portal venous obstruction in chronic pancreatitis. A prospective longitudinal study of a medical-surgical series of 266 patients. Dig Dis Sci. 1992;37(3):340–346. doi: 10.1007/BF01307725. [DOI] [PubMed] [Google Scholar]
- 3.Bradley EL. The natural history of splenic vein thrombosis due to chronic pancreatitis: indications for surgery. Int J Pancreatol. 1986;2(2):87–92. doi: 10.1007/BF03015001. [DOI] [PubMed] [Google Scholar]
- 4.Butler JR, Eckert GJ, Zyromski NJ, Leonardi MJ, Lillemoe KD, Howard TJ. Natural history of pancreatitis-induced splenic vein thrombosis: a systematic review and meta-analysis of its incidence and rate of gastrointestinal bleeding. HPB. 2011;13(12):839–845. doi: 10.1111/j.1477-2574.2011.00375.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Evans GR, Yellin AE, Weaver FA, Stain SC. Sinistral (left-sided) portal hypertension. Am Surg. 1990;56(12):758–763. [PubMed] [Google Scholar]
- 6.Flati G, Andren-Sandberg A, La Pinta M, Porowska B, Carboni M. Potentially fatal bleeding in acute pancreatitis: pathophysiology, prevention, and treatment. Pancreas. 2003;26(1):8–14. doi: 10.1097/00006676-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Gaba RC, Katz JR, Parvinian A, Reich S, Omene BO, Yap FY, Owens CA, Knuttinen MG, Bui JT. Splenic artery embolization: a single center experience on the safety, efficacy, and clinical outcomes. Diagn Interv Radiol. 2013;19(1):49–55. doi: 10.4261/1305-3825.DIR.5895-12.1. [DOI] [PubMed] [Google Scholar]
- 8.Heider TR, Azeem S, Galanko JA, Behrns KE. The natural history of pancreatitis-induced splenic vein thrombosis. Ann Surg. 2004;239(6):876–880. doi: 10.1097/01.sla.0000128685.74686.1e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ito K, Kudo A, Nakamura N, Tanaka S, Teramoto K, Arii S. Left-sided portal hypertension caused by serous cystadenoma of the pancreas: report of a case. Surg Today. 2008;38(2):184–187. doi: 10.1007/s00595-007-3600-y. [DOI] [PubMed] [Google Scholar]
- 10.Johnston FR, Myers RT. Etiologic factors and consequences of splenic vein obstruction. Ann Surg. 1973;177(6):736–739. doi: 10.1097/00000658-197306000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keith RG, Mustard RA, Jr, Saibil EA. Gastric variceal bleeding due to occlusion of splenic vein in pancreatic disease. Can J Surg. 1982;25(3):301–304. [PubMed] [Google Scholar]
- 12.Kim T, Shijo H, Kokawa H, Tokumitsu H, Kubara K, Ota K, Akiyoshi N, Iida T, Yokoyama M, Okumura M. Risk factors for hemorrhage from gastric fundal varices. Hepatology. 1997;25(2):307–312. doi: 10.1002/hep.510250209. [DOI] [PubMed] [Google Scholar]
- 13.Koconis KG, Singh H, Soares G. Partial splenic embolization in the treatment of patients with portal hypertension: a review of the English language literature. J Vasc Interv Radiol. 2007;18(4):463–481. doi: 10.1016/j.jvir.2006.12.734. [DOI] [PubMed] [Google Scholar]
- 14.Little AG, Moossa AR. Gastrointestinal hemorrhage from left-sided portal hypertension. An unappreciated complication of pancreatitis. Am J Surg. 1981;141(1):153–158. doi: 10.1016/0002-9610(81)90029-5. [DOI] [PubMed] [Google Scholar]
- 15.Madsen MS, Petersen TH, Sommer H. Segmental portal hypertension. Ann Surg. 1986;204(1):72–77. doi: 10.1097/00000658-198607000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCormick PA, O′Keefe C. Improving prognosis following a first variceal haemorrhage over four decades. Gut. 2001;49(5):682–685. doi: 10.1136/gut.49.5.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moossa AR, Gadd MA. Isolated splenic vein thrombosis. World J Surg. 1985;9(3):384–390. doi: 10.1007/BF01655272. [DOI] [PubMed] [Google Scholar]
- 18.Ou HY, Huang TL, Chen TY, Tsang LL, Concejero AM, Chen CL, Cheng YF. Emergency splenic arterial embolization for massive variceal bleeding in liver recipient with left-sided portal hypertension. Liver Transpl. 2005;11(9):1136–1139. doi: 10.1002/lt.20543. [DOI] [PubMed] [Google Scholar]
- 19.Petermann A, Chabrot P, Cassagnes L, Dumousset E, Alfidja A, Gageanu C, Ravel A, Abergel A, Boyer L. Hypersplenism due to portal hypertension: retrospective evaluation of 17 patients treated by splenic embolization. Diagn Interv Imaging. 2012;93(1):30–36. doi: 10.1016/j.diii.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 20.Sakorafas GH, Sarr MG, Farley DR, Farnell MB. The significance of sinistral portal hypertension complicating chronic pancreatitis. Am J Surg. 2000;179(2):129–133. doi: 10.1016/S0002-9610(00)00250-6. [DOI] [PubMed] [Google Scholar]
- 21.Shah R, Mahour GH, Ford EG, Stanley P. Partial splenic embolization. An effective alternative to splenectomy for hypersplenism. Am Surg. 1990;56(12):774–777. [PubMed] [Google Scholar]
- 22.Stabile BE, Wilson SE, Debas HT. Reduced mortality from bleeding pseudocysts and pseudoaneurysms caused by pancreatitis. Arch Surg. 1983;118(1):45–51. doi: 10.1001/archsurg.1983.01390010035009. [DOI] [PubMed] [Google Scholar]
- 23.Weber SM, Rikkers LF. Splenic vein thrombosis and gastrointestinal bleeding in chronic pancreatitis. World J Surg. 2003;27(11):1271–1274. doi: 10.1007/s00268-003-7247-6. [DOI] [PubMed] [Google Scholar]