Abstract
OBJECTIVE
To reach consensus on key issues for clinical practice and future research in active surveillance and focal therapy in managing localized prostate cancer.
PATIENTS AND METHODS
A group of expert urologists, oncologists, radiologists, pathologists and computer scientists from North America and Europe met to discuss issues in patient population, interventions, comparators and outcome measures to use in both tissue-preserving strategies of active surveillance and focal therapy.
Break-out sessions were formed to provide agreement or highlight areas of disagreement on individual topics which were then collated by a writing group into statements that formed the basis of this report and agreed upon by the whole Transatlantic Consensus Group.
RESULTS
The Transatlantic group propose that emerging diagnostic tools such as precision imaging and transperineal prostate mapping biopsy can improve prostate cancer care. These tools should be integrated into prostate cancer management and research so that better risk stratification and more effective treatment allocation can be applied.
The group envisaged a process of care in which active surveillance, focal therapy, and radical treatments lie on a continuum of complementary therapies for men with a range of disease grades and burdens, rather than being applied in the mutually exclusive and competitive way they are now.
CONCLUSION
The changing landscape of prostate cancer epidemiology requires the medical community to re-evaluate the entire prostate cancer diagnostic and treatment pathway in order to minimize harms resulting from over-diagnosis and over-treatment. Precise risk stratification at every point in this pathway is required alongside paradigm shifts in our thinking about what constitutes cancer in the prostate.
Keywords: focal therapy, active surveillance, multi-parametric MRI, template prostate mapping biopsies, risk stratification, trial design
INTRODUCTION
The management of men with prostate cancer is set to become one of the most challenging public health issues in coming years if the current pathway of care is left unchecked. This article presents the findings of a transatlantic consensus group, which was convened in May 2010 to deliberate on the problems of the current care pathway and suggest research strategies for moving the field forward.
The problems associated with the diagnosis and management of prostate cancer have been widely presented and debated. They include over-diagnosis, over-treatment, treatment-related toxicity and escalating, unsustainable costs [1,2]. There are several reasons why prostate cancer poses such challenges.
First, many prostate cancers are clinically insignificant when first detected, in the sense that they will not affect the individual in any way if left undiagnosed and untreated. The lifetime risk of having prostate cancer is high, but the lifetime risk of dying of prostate cancer is only ≈3% [3]. Second, the current diagnostic process, which has inherent random and systematic errors related to the biopsy technique, underestimates the true cancer grade in as many as one quarter and the cancer burden in as many as one half of men diagnosed with low-risk disease [4]. Third, and as a result of these errors, localization of individual tumours within the prostate is poor.
The management of prostate cancer reflects these diagnostic uncertainties. For example, the use of active surveillance reflects our inability to give an accurate prognosis in individual patients. If we knew which cancers were harmless at the time of diagnosis, we could confidently leave them alone without the need for close monitoring. When we do use radical treatments, such as radiotherapy or surgery, those treatments are directed at the entire organ, because we are not able to accurately localize tumours within the prostate. Whole-gland therapies risk damage to neighboring structures such as the bladder neck, external urinary sphincter, neurovascular bundles, and rectum. Such damage can result in significant urinary incontinence requiring pads, erectile dysfunction, and rectal toxicity (proctitis, bleeding, and diarrhoea).
The transatlantic consensus group met to consider the potential roles of emerging diagnostic tools such as precision imaging and transperineal prostate mapping biopsy in improving prostate cancer care. In the present article, we propose that integrating these tools into prostate cancer research and management could lead to better risk stratification and more effective treatment allocation than we have at present. We envisage a process of care in which active surveillance, focal therapy, and radical surgery or radiotherapy lie on a continuum of complementary therapies for men with a range of disease grades and burdens, rather than being applied in the mutually exclusive and competitive way they are now [5,6].
IMPROVING DETECTION AND CHARACTERIZATION OF PROSTATE CANCER
The optimal prostate cancer diagnostic strategy would reliably identify cancers that could harm the patient, would have low morbidity, and be inexpensive. It would also avoid unnecessary biopsy in patients who do not have harmful cancers and reduce the number of biopsy cores taken in those who do need biopsy.
IMAGING WITH PRECISION
At present, MRI is the only clinically available imaging method that depicts the zonal anatomy of the prostate in detail. Furthermore, anatomical MRI can be combined with functional and metabolic MR techniques such as dynamic contrast enhancement, diffusion-weighting, and MR spectroscopy to facilitate better tumour detection and characterization and to obtain quantitative predictive and prognostic biomarkers [7] (Figs 1 and 2).
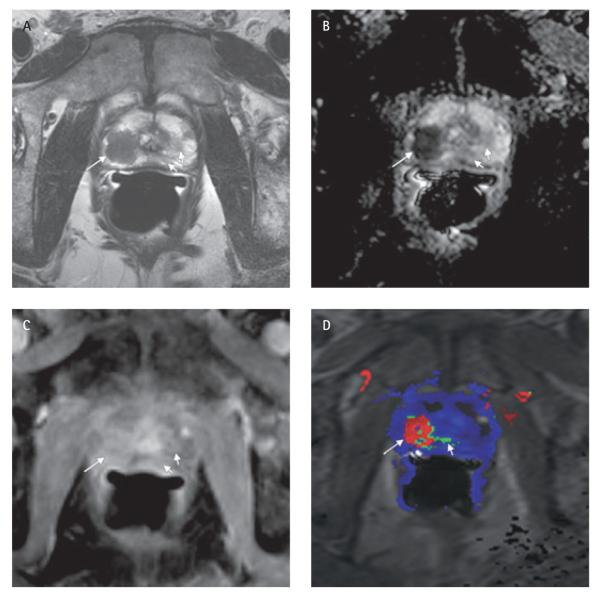
FIG. 1.
Images showing the value of multi-parametric MRI for identifying the dominant lesion in a 58-year-old man with a preoperative PSA level of 11.9 ng/mL, in whom surgical pathology showed pT2b prostate cancer of Gleason score 8 (4 + 4). (A) T2-weighted image; (B) apparent diffusion coefficient (ADC) map; (C) dynamic contrast-enhanced T1-weighted image; and (D) colour-coded map showing peak enhancement. Marked differences in T2 signal, ADC values, and contrast enhancement can be seen between the dominant lesion (Gleason score 8; long arrows) at the right apex and a smaller lesion (Gleason score 6; short arrows) on the left side.
FIG. 2.
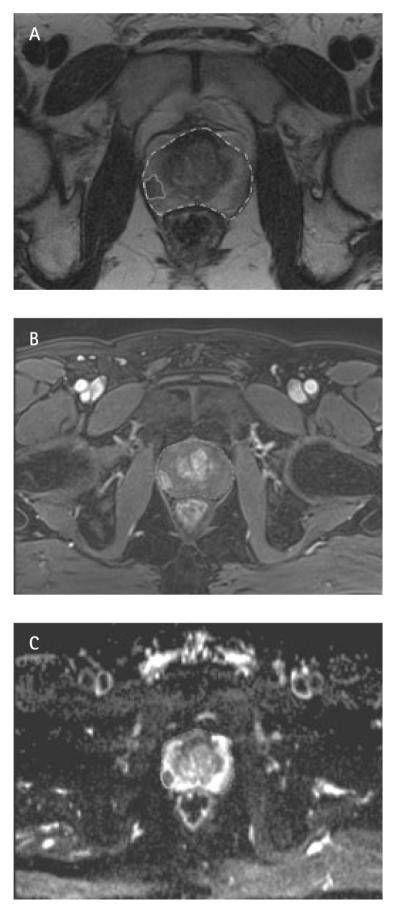
In a 57-year-old man with a PSA level of 4.87 ng/mL diagnosed with low-risk prostate cancer (Gleason 3 + 3, 1/12 cores positive), multi-parametric MRI showed a clinically significant lesion: a 1 × 1 × 0.6-cm (0.5-mL by planimetry) focal area of low T2-signal intensity (A) within the right peripheral zone at the mid-gland level, abutting the lateral aspect of the prostatic capsule for a length of 1 cm without evidence of extracapsular extension. The lesion shows early arterial enhancement (B) and markedly restricted diffusion (C) in keeping with a carcinoma. No other clinically significant lesions are seen on MRI.
PATIENT SELECTION FOR BIOPSY
Patient selection for prostate biopsy has, in the past, been largely based on serum PSA levels. The 2000 AUA guidelines describe a PSA level of ≥4.0 ng/mL as sufficient to trigger consultation of a urologist for prostate biopsy [8]. However, ≈70% of prostate biopsies prompted by an elevated PSA level do not show any evidence of cancer, which suggests that many of them are unnecessary [9]. Furthermore, many, if not most, prostate cancers detected using PSA screening are clinically insignificant, such that between 12 and 48 men need to be treated to extend the life of one man over the course of ≈10 years. The screening and biopsy burden is many-fold higher [10]. Others have shown that the PSA threshold may need to be lowered [11].
To minimize the problems of over-diagnosis and over-treatment, PSA threshold-based selection for biopsy is being replaced by a risk-based selection process, now recommended by the AUA [12]. Several risk calculators have been published that can be used to estimate an individual’s risk of high-grade prostate cancer on biopsy [13–16]. These calculators use factors such as PSA level, DRE findings, age, ethnicity, family history, and previous biopsy history to estimate risk. Using such a model has been shown to reduce the number of unnecessary biopsies, with little, if any, impact on the detection of significant cases. For example, Vickers et al. [17] found that using DRE findings, age, and a kallikrein panel (total PSA, free PSA, intact PSA and kallikrein-related peptidase 2) to predict the probability of a positive biopsy, and applying a threshold of 20% probability as the criterion for biopsy, would lead to 362 fewer biopsies per 1000 men with elevated PSA; they estimated that 43 cancers would be missed, of which only four would be high grade.
MRI could potentially be incorporated in the risk analysis and used as a triage tool to further improve patient selection for prostate biopsy, as it has shown promise as a means to distinguish between clinically insignificant and significant prostate cancer [18]. Those men considered at increased risk of clinically significant prostate cancer, according to a risk calculator could undergo prostate imaging. If a normal prostate imaging result could reliably exclude significant prostate cancer, men with normal imaging could avoid unnecessary biopsy [7]. Used in this way, non-invasive imaging could contribute to preventing the harms associated with prostate biopsy, not least the harm of being diagnosed and treated for a cancer that will have no impact on a man’s life, other than to cause him and his family anxiety. Furthermore, performance of MRI before biopsy would avoid post-biopsy artifact caused by haemorrhage and allow more accurate local staging and determination of disease burden than is possible with post-biopsy MRI.
BIOPSY TECHNIQUE
Standard practice is to use TRUS guidance to take 10–12 transrectal needle biopsies from different parts of the prostate in a systematic fashion. TRUS is used to locate the prostate gland itself but otherwise plays little part in guiding the biopsy procedure. Consequently, random error occurs, as the operator has no knowledge of where the cancerous areas may be. In addition, systematic error occurs because only the posterior peripheral zone is sampled, and sampling of the anterior peripheral and transition zones and apex is inadequate. Although routine acquisition of 4–6 mid-lobar anterior cores has been recommended to detect anterior cancers in glands >50 mL [19], it has been associated with low detection rates [20]. Thus, significant cancers in these areas go undetected during the initial biopsy [21]. TRUS-guided biopsy has a substantial false-negative rate, with cancer being found in ≈20% of repeat biopsies [22].
The use of imaging for targeting biopsies would bring prostate cancer diagnosis into line with the biopsy technique used for the detection of almost all other solid tumours, relying on measurable disease that can be visualized and targeted. The strategy of targeting biopsies to areas suspicious on MRI could potentially improve the detection of significant cancers and the assessment of tumour grade and burden (Fig. 3) [23–25].
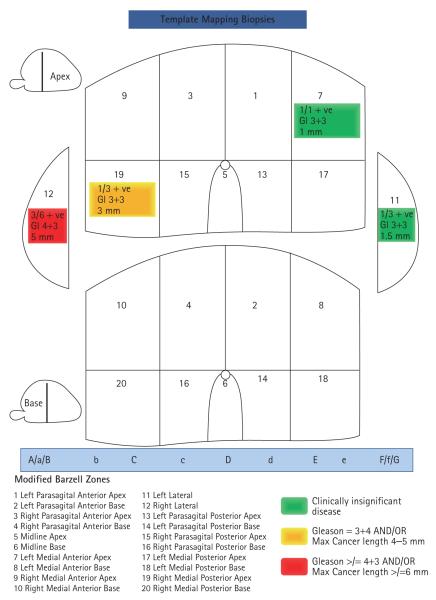
FIG. 3.
The same man shown in Fig. 2 underwent 3-D TPM biopsy, with a total of 69 biopsies taken from 20 zones. Clinically significant cancer was confirmed in the right peripheral zone as shown on multiparametric MRI. Two smaller low-grade areas found in the contralateral lobe did not show enhancement or diffusion patterns that are associated with clinically significant cancer on MRI.
Multi-parametric MRI with gadolinium injection has been shown to be very sensitive for both anterior and posterior cancer detection [26–29], and recent published data support the concept of MRI-targeted biopsy. Anterior cancers are medially located, anterior to the urethra and, because of this, their detection by systematic anterior biopsy is minimal in comparison with their detection by targeted biopsies to MRI-suspicious areas [28]. After negative TRUS-guided biopsy, MRI-guided biopsy can detect cancer with fewer biopsy cores than are obtained in the recommended (14-core) systematic biopsy. For example, in a study of patients with negative first biopsy, the detection rate with MRI guidance was 59% (40 of 68 cases) using a median of 4 cores [24]. The detection rate with MRI-guided biopsy was significantly higher than that with TRUS-guided prostate biopsy in all patient subgroups in a matching population (P < 0.01) except those with PSA levels of >20 ng/mL, prostate volume >65 mL and PSA density >0.5 ng/mL/mL [24]. Furthermore, 93% of cases detected by MRI-guided biopsy were thought to represent clinically significant disease. The use of multi-parametric MRI (as compared with standard T2-weighted MRI) to identify suspicious lesions before MRI-targeted biopsy, increases cancer detection and can provide an indication of cancer aggressiveness [23–25].
ASSESSMENT OF THE RISK OF DISEASE PROGRESSION OR RECURRENCE
Several variables, e.g. PSA level, clinical stage, and Gleason score are typically used to stratify patients into low-, intermediate-, or high-risk disease categories that indicate the likelihood of recurrence after therapy. However, these variables suffer from some substantial limitations. For instance, PSA may not be strongly expressed by high-grade cancers. Assessment of clinical stage is operator dependent and most tumours are impalpable in the modern era. The biopsy Gleason score may not be representative of radical prostatectomy (RP)-based pathology [30,31]. Tumour volume (often assessed by the number of positive biopsy cores or the percentage involvement of biopsy cores) is not precisely known or easily incorporated into predictive tables. In addition, pathological reporting for prostate biopsy has not been standardized to routinely include variables that may affect outcome such as tertiary Gleason patterns, perineural invasion, lymphovascular invasion, extracapsular extension, and tumour volume.
The current risk stratification algorithms also have limitations. Often, variables are categorical (D’Amico stratification, Partin Tables) and not continuous, especially for low-risk patients [32,33]. Finally, nearly all of the outcomes predicted by current risk-stratification approaches assume destruction or resection of the entire prostate and therefore do not apply to understanding the biology of the cancer within the gland in situ.
Risk stratification in the future will need to incorporate new, more reliable biomarkers that can distinguish between clinically insignificant prostate cancers and those that are locally aggressive not only among men, but also among different lesions in the same man [34]. This will require increased knowledge of prostate tumour biology and embedding evaluation of molecular markers into trials assessing imaging methods and focal therapy studies incorporating index lesion ablation [35,36].
Historically, imaging tests have been used to contribute little other than anatomical information about the location and extent of the cancer to aid loco-regional staging. Increasingly, functional imaging techniques provide information not just about tumour location, but also about cancer behaviour. For example, numerous early studies have documented correlations between apparent diffusion coefficient (ADC) values obtained with diffusion-weighted MRI and Gleason scores [37–43]. Significant differences between the ADC values of low- and intermediate-risk prostate cancer have been found [25,44], and in a cohort of patients on active surveillance, the baseline ADC value was an independent predictor of both adverse repeat biopsy findings and time to radical treatment [45]. Preliminary results have also suggested a correlation between Gleason scores and spectral patterns obtained by MR spectroscopic imaging [46]. By providing prognostic markers, diffusion-weighted MRI and MR spectroscopy could potentially aid in the choice between active treatment on the one hand and surveillance on the other. Indeed, it is possible that functional and metabolic imaging data could also be predictive, for example, by identifying cancers better suited to radiotherapy or surgery.
TRANSPERINEAL PROSTATE MAPPING BIOPSY
Three-dimensional (3-D) transperineal prostate mapping (TPM) biopsy is arguably the most detailed method of pathologically mapping the in vivo prostate to date. 3-D TPM involves sampling the entire prostate using a 5-mm sampling frame guided by a brachytherapy-type template grid placed against the perineum. Initial reports suggest that 3-D TPM has both a sensitivity and a negative predictive value of 95% for clinically significant cancers when assessed against RP specimens [47,48]. 3-D TPM provides several benefits compared with the conventional TRUS-guided biopsy. First, it is able to detect disease with greater accuracy by overcoming random and systematic errors of TRUS-guided biopsy [49]. Second, once cancer is detected, it can characterize and risk stratify the disease accurately in terms of number of tumours present, Gleason score, overall estimate of tumour burden, and the spatial context of each tumour. Third, transperineal biopsies have a considerably lower incidence of sepsis as the rectal wall is not traversed.
Although 3-D TPM biopsy is a reliable and detailed method of mapping individual prostate tumours, it may be a temporary step in our quest for image-guided diagnosis and treatment, as it has several disadvantages that may limit its long-term use. First, it places a heavy burden on resources, commonly requiring general anaesthesia and significant pathologist time. Second, the prostate can change in shape as a result of distortion (from the US probe), rotate, and swell (as a result of the needle, oedema, and haemorrhage), compromising the 3-D spatial information. Third, there is needle deviation, so that when considering focal therapy, for instance, sectors adjacent to the positive biopsy need to be ablated to incorporate an adequate surgical margin. Fourth, morbidity can include temporary erectile dysfunction, perineal ecchymoses, and acute urinary retention.
RECOMMENDATIONS FOR FUTURE DIAGNOSTIC STUDIES
EVALUATING IMAGING IN THE SELECTION OF PATIENTS FOR PROSTATE BIOPSY
Three aspects of any novel imaging approach must be evaluated if we are to integrate it into the diagnostic pathway. First, can imaging confidently exclude clinically significant cancer to negative predictive values approaching 90% to 95%? Second, can imaging reliably detect cancer in the various prostatic zones (posterior, transition, central, and anterior fibromuscular stroma)? Third, can imaging provide detailed characterization of a lesion based on grade, burden and topography? The latter is particularly pertinent, as prostate cancer lesions tend to have a central dense area of malignant cells with associated stems [50].
Previous attempts to study the potential diagnostic utility of imaging in prostate cancer detection and localization have been hampered by methodological limitations. Studies using RP as a reference standard have been limited to men known to have prostate cancer. This causes not only a selection bias in the population, but also an operator bias, as the radiologist who interprets the MRI knows the case is positive for cancer. Many studies have used imaging after, rather than before, biopsy, and have therefore been compromised by biopsy artifact (bleeding, inflammation) which can mimic cancer. Studies have also often segmented the prostate into between 2 and 24 regions of interest, rather than analyze results at the level of the individual patient.
We propose that MRI trials should be performed in men who, on the basis of a prostate cancer risk calculator, are considered at risk of harboring clinically significant cancer, and are therefore due to have a diagnostic prostate biopsy. Subjects should undergo imaging before prostate biopsy. Within this group, the optimal reference standard is 3-D TPM biopsy, as it can be applied to all men [4]. The primary analysis would be at the individual patient level and would examine two equally important issues: (i) the ability of imaging to exclude clinically significant cancer on TPM (specificity and negative predictive value); and (iI) the ability of imaging to identify clinically significant cancer (sensitivity and positive predictive value). Clinical significance would be defined in terms of tumour length and Gleason score [51].
No such study has yet been performed, but the design would also provide considerable added value. First, it would provide further data on the safety and tolerability of TPM. Second, blood and urine samples could be banked before biopsy, so that candidate diagnostic biomarkers could be assessed for the detection of clinically significant cancer. Third, this design would also provide data on the shortcomings of the conventional TRUS-biopsy technique with respect to this reference standard, and would inform the development of image-targeted biopsies.
This type of diagnostic study does raise at least two contentious issues. The first is the accuracy of TPM as a ‘gold standard’ for selection of significant cancers (discussed further below). The second, and more problematic issue, is the choice of tumour volume and grade criteria used to define clinical significance. Without long-term observational studies of the natural history of the untreated disease in men who have had TPM, this issue will remain a matter of speculation rather than evidence. However, it is important to note that data obtained with the proposed study design will allow analysis of the diagnostic utility of imaging for clinically significant cancer, whatever definition of clinical significance one chooses to use.
The economic implications of performing MRI in every man who requires a prostate biopsy will also need to be carefully considered. Pre-biopsy MRI strategies cost, for instance, ≈€300 (in France) and require available MRI time and experienced radiologists. In the USA, costs are considerably higher $2–3000. Ultimately, the cost-utility and cost-effectiveness of incorporating imaging into the diagnostic pathway in this manner will require careful evaluation, as downstream savings that result from not biopsying every man and thus reducing over-diagnosis and over-treatment may be substantial.
EVALUATING 3-D TPM
Despite 3-D TPM biopsy being the most accurate way to pathologically map prostate cancer at present, certain unknowns require research. First, it is not clear how many biopsies are necessary to optimally map the prostate based on prostate volume. Second, defining clinical significance is problematic when the test gives core lengths and not volume of cancer foci. Therefore, it is important that further studies validate TPM against RP whole-mount pathology specimens.
REDUCING OVERTREATMENT
We are currently at a watershed where it is possible to glimpse some of the promise of improved imaging and biopsy techniques for reducing over-treatment of prostate cancer and facilitating novel, minimally-invasive therapies.
POTENTIAL OF IMAGING AND 3-D TPM FOR IMPROVING ACTIVE SURVEILLANCE
For men who are currently managed with active surveillance, the challenge is to identify, at an appropriate time, those who need treatment whilst causing minimum harm to those who will never need treatment. At present, management strategies for surveillance patients are not standardized, although most include regular serum PSA testing, DRE, and repeat prostate biopsy every 1–2 years. Due to the problems outlined in the earlier sections, each of these tests has limited utility in accurately characterizing a man’s burden of disease, the realization of which prompts many physicians to advise patients to seek active treatment, which may be unnecessary [28,52,53]. Indeed, it is likely that the misclassification error of the current diagnostic pathway is predominantly responsible for the observed ‘progression’rate of 30–40% seen in active surveillance series [54,55].
MRI could be added to active surveillance protocols. If the test-retest reliability of imaging is shown to be good, it may even be possible to replace serial biopsy during active surveillance with serial imaging, supplemented by biopsy only as needed. Direct real-time targeted MRI-guided biopsies, either transperineal or transrectal, are becoming increasingly available at USA and European healthcare centers. When combined with multi-parametric MRI, this biopsy approach could potentially play a major role in the screening and monitoring men on active surveillance protocols.
There is growing interest in the use of 3-D TPM biopsy for risk stratification, treatment allocation, and surveillance. However, the substantial burden the procedure places on men and the healthcare system suggests it will probably be of most value as a medium term clinical management and research tool.
RECOMMENDATIONS FOR FUTURE CLINICAL STUDIES IN ACTIVE SURVEILLANCE
One of the significant challenges in trial design in early prostate cancer is the choice of appropriate endpoints for evaluating outcomes. Assessment of the effects of active surveillance on overall survival, disease-specific survival, or even the development of metastases is limited by the prolonged natural history of prostate cancer [56]. An alternative is to use a surrogate marker of clinical outcome. In some active surveillance programmes, a change in a single factor on biopsy, or PSA kinetics, can prompt a recommendation for active treatment, which is in itself an endpoint [55].
When considering the use of imaging as a predictive tool for men considering or undergoing active surveillance, one option is to compare different imaging approaches for their ability to predict pathological outcomes at RP. However, pathological outcomes do not directly reflect long-term clinical outcomes. It would, therefore, be valuable to compare imaging at diagnosis with the longer term outcomes of treated or untreated disease. For example, some early work suggests that ADC values on diffusion-weighted MRI may be a better predictor of clinical outcome than Gleason score [45].
A comparison of MRI and 3-D TPM in men recruited to active surveillance programmes would allow the predictive value of each for the long-term outcome of surveillance to be evaluated. The addition of an imaging method such as multi-parametric MRI to current formal programmes of active surveillance would allow valuable correlation of imaging and clinical parameters, and assessment of the usefulness of repeated imaging studies.
Nomograms have been shown to be useful for the prediction of several outcomes in men with prostate cancer [57], and nomograms that incorporate imaging findings to predict insignificant prostate cancer have been developed [18]. Imaging parameters, TPM findings, and serum biomarkers [17] could potentially be incorporated into nomograms that would aid decision-making processes in active surveillance.
Many studies of active surveillance are currently underway [56], all of which have different entry and exit criteria as well as follow-up schedules. An international registry analysis to pool data from these ongoing studies would allow comparison of the different approaches to active surveillance, and might help to define an optimal approach for future programmes.
POTENTIAL OF IMAGING AND TPM FOR IMPROVING FOCAL THERAPY
The aim of focal therapy is to treat cancer within the prostate, whilst leaving benign prostate and surrounding normal structures intact, in order to offer oncological control with minimum impact on genitourinary and rectal function. Treatment delivery must be guided either by the same imaging method used for initial disease characterization (as in MRI-guided high-intensity focused ultrasound) [58] or registration of pre-therapy images used for disease characterization to live images obtained during treatment (e.g. pre-treatment MRI registered to real-time TRUS images) [59]. 3-D TPM biopsy could play a useful role in assessing the effects of focal ablation as well as validating the accuracy of imaging in evaluating these effects (Fig. 4).
FIG. 4.
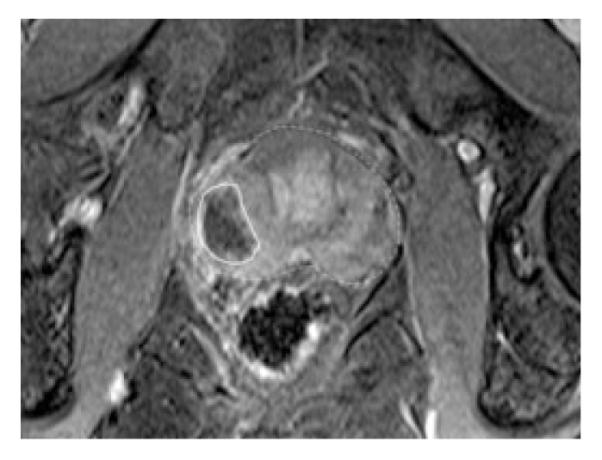
The same man shown in Figs 2 and 3 underwent focal therapy using day-case TRUS-guided high-intensity focused ultrasound. Only the index (measurable) lesion on imaging was ablated. He was fully dry (leak-free, pad-free) after the procedure and had erections sufficient for penetrative sex at 6 weeks.
RECOMMENDATIONS FOR FUTURE CLINICAL STUDIES IN FOCAL THERAPY
The selection of appropriate endpoints is as much of a challenge in studies of focal therapy as it is in studies of active surveillance [60]. Options include absence of disease, or of clinically important disease, in the treated volume or the whole gland and lack of progression to clinically important disease or a drop in the likelihood of curability with radical treatment, as calculated by, for example, a nomogram. The choice of definition will, of course, affect the declared success rates of the methods used, and standardization of these definitions will allow easier comparison of different methods being used for focal treatment.
Several different study designs for evaluating focal therapy are proposed (Table 1). The first question that a new ablative technology must address is whether or not it can reliably ablate cancer in the treated volume. The presence or absence of cancer in the treated volume can be assessed several ways. Although studies in men who have a diagnostic biopsy, an ablation procedure, a post-ablation imaging study, and then a RP would prove of use [61,62], they can be difficult to carry out.
TABLE 1.
Recommended study designs in the assessment of focal therapy for prostate cancer
| Study type | Population | Intervention | Comparator | Outcome |
|---|---|---|---|---|
| Phase I/II | Men due for RP | Focal ablation before RP | None | Whole-mount step-section pathology evaluating absence of disease in treated volume |
| Phase II | Low- and/or intermediate-risk cancer |
Prostate mapping with imaging and 3-D TPM biopsy; focal ablation; repeat TPM biopsy |
None | Absence of (clinically significant) cancer in treated area (derived from either targeted TRUS-guided biopsies [with high density of cores per mL residual tissue] or 3-D TPM biopsy) |
| Phase II | Low- and/or intermediate-risk cancer |
Image-guided biopsy; focal ablation; post-ablation imaging |
None | Lesion ablation as defined by post-treatment imaging |
| Phase III | Low- and/or low- intermediate-risk cancer |
Focal therapy | Active surveillance | Rate of progression to radical treatment |
| Phase III | Low- and/or intermediate to intermediate-high risk cancer |
Focal therapy | Radical whole-gland treatment (surgery or radiotherapy) |
Freedom from metastases |
| Phase III | Low- and/or low- intermediate risk disease |
Prostate mapping with 3-D TPM biopsy + MRI, followed by focal ablation of all known lesions |
Active surveillance | Cancer on 3-D TPM biopsy + MRI at 1 year |
| Phase II/III | Low- and/or intermediate to intermediate-high risk cancer |
Prostate mapping with imaging and 3-D TPM biopsy; focal ablation monotherapy; repeat TPM biopsy |
Prostate mapping with imaging and 3-D TPM biopsy; focal ablation with adjuvant chemoprevention or low-dose radiotherapy; repeat TPM biopsy |
Rate of clinically significant prostate cancer lesion in untreated tissue |
| Phase III (pragmatic design) |
Low- and/or intermediate-risk disease |
Focal therapy (adaptive, i.e. incorporates any new ablative therapy demonstrating phase II efficacy) |
Standard of care (determined by individual equipoise) active surveillance or radical therapy |
Rate of systemic therapy; freedom from progression defined according to each treatment modality |
An alternative design that is likely to provide equally useful data is to use imaging and 3-D TPM to localize and characterize the cancer, ablate focally based on both of these diagnostic methods, and then use imaging and 3-D TPM biopsy again after focal therapy to verify the treatment effect.
It is important that men with significant disease (e.g. disease that is visible on MRI or substantial on biopsy) be included in the evaluation of new ablative therapies; this is necessary to ensure that a negative post-treatment biopsy or image shows treatment effect rather than sampling effect. This is likely to mean that men across the traditional categories of low- and intermediate-risk disease will be included in focal therapy studies, if accurate risk stratification with imaging and/or 3-D TPM supports their eligibility for focal therapy.
Once it has been shown that a method can ablate cancer in a given treatment volume, it must then be determined whether or not focal ablation can result in clinically meaningful results; this should ideally be done in a randomized comparative trial where the choice of comparator will lie between active surveillance and radical treatment. Several different study designs could be used (Table 1). The randomized comparison of focal therapy to either active surveillance or radical therapy is likely to be possible in the UK and Scandinavian countries, where rates of active surveillance are high and clinical equipoise is likely to be maintained. For those countries with a higher radical treatment rate, such as the USA, randomization between focal therapy and radical treatment is likely to lead to higher recruitment, although again there may be little clinical equipoise within a design such as this, as the prevailing view in the USA is that focal therapy is for men who are suitable for active surveillance.
An innovative pragmatic design would be one where the decision to randomize between focal treatment and standard radical treatment, or between focal treatment and active surveillance, is made either on a per-centre or a per-patient basis. Men with high-risk disease would be excluded, due to the known benefits of radical treatment in this population. There would be no set criteria for the randomization group that a man is put into; for example, a man with features of low-risk disease may choose randomization between focal treatment and active surveillance to reduce the toxicity of treatment, whereas a man with similar risk parameters may favour randomization between focal and radical treatment to maximize his chance of oncological benefit. The focal therapy arm would include the most appropriate focal therapy strategy for a particular man’s disease using an ablative technology (e.g. cryosurgery, high-intensity focused ultrasound, photodynamic therapy, radiofrequency ablation, photothermal therapy, or irreversible electroporation) available to the local physician expert in its use, with that ablative technology having already proven ablative efficacy.
An outstanding concern about tissue-preserving focal therapy is development of de novo cancer or true histological progression of untreated malignant lesions. If one were to follow the breast cancer paradigm, then it would be important to evaluate the role of background treatment such as 5α-reductase inhibitors or low-dose external radiation. This would allow concerns about the multi-focality of prostate cancer and the field effect of untreated benign tissue to be addressed. Such a study would also need to determine whether focal therapy with or without background chemoprevention or low-dose radiation can compromise the efficacy of subsequent radical therapies.
Furthermore, exactly what constitutes focal therapy is still open to debate, with ongoing trials investigating the effects of hemiablation, true focal ablation of the cancer areas and focal ablation directed to only the index lesion or areas of presumed clinical significance (based on Gleason grade and size thresholds). Medium- to long-term cancer control data is currently lacking.
CONCLUSION
The changing landscape of prostate cancer epidemiology requires the medical community to re-evaluate the entire prostate cancer diagnostic and treatment pathway in order to minimise harms resulting from over-diagnosis and over-treatment. Precise risk stratification at every point in this pathway is required alongside paradigm shifts in our thinking about what constitutes cancer in the prostate.
What’s known on the subject? and What does the study add?
Active surveillance for prostate cancer is gaining increasing acceptance for low risk prostate cancer. Focal therapy is an emerging tissue preservation strategy that aims for treat only areas of cancer. Early phase trials have shown that side-effects can be significantly reduced using focal therapy.
There is significant uncertainty in both active surveillance and focal therapy. This consensus group paper provides a road-map for clinical practice and research for both tissue-preserving strategies in the areas of patient population, tools for risk stratification and cancer localisation, treatment interventions as well as comparators and outcome measures in future comparative trials.
ACKNOWLEDGEMENTS
The work of the Transatlantic group was fully supported by means of an educational grant from:
The PELICAN CANCER FOUNDATION (http://www.pelicancancer.org)
The Peter Michael Foundation (http://www.petermichaelfoundation.org)
Invivo, N27 W23676 Paul Rd., Pewaukee, WI 53072, USA (http://www.invivocorp.com) Mr Malcolm Isaac
Mark Emberton receives research support from the UK National Institute of Health Research UCLH/UCL Comprehensive Biomedical Research Centre, London UK. Hashim U. Ahmed receives funding from the Medical Research Council, UK.
We thank Ada Muellner and Dagmar Schnau of Memorial Sloan-Kettering Cancer Center for providing substantive editorial assistance.
FUNDING This meeting was sponsored and supported by the Pelican Cancer Foundation, UK, and the Peter Michael Foundation, USA, both of which are charitable organizations committed to improving the diagnosis and treatment of men with localised prostate cancer.
Abbreviations
- RP
radical prostatectomy
- ADC
apparent diffusion coefficient
- 3-D
three-dimensional
- TPM
transperineal prostate mapping
APPENDIX.
All authors are listed in alphabetical order. The full list of names that form the remainder of the Transatlantic Consensus Group are listed here; all are co-authors on this manuscript and have approved the manuscript.
Allen Dr C, Radiologist, Consultant Radiologist University College London Hospitals NHS Foundation Trust, 235 Euston Rd, London NW1, UK
Bangma Professor C, Professor of Urology, Department of Urology, Erasmus MC, Rotterdam, The Netherlands
Barzell Dr W, Urologist, Director of Clinical Applications, Sarasota MC, 1921 Waldemere Street, 310 Sarasota, FL 34239, USA
Beyersdorff Dr med D, Radiologist, Facharzt fur Diagnostiche Radiologie, Institut fur Radiologie, Charite Campus Mitte, Chariteplatz 1, 10117, Berlin, Germany
Crawford Dr D, Urologist, Professor and Head of Urologic Oncology, University of Colorado Cancer Centre, Anschutz Medical Campus, 13001 E. 17th Pl, Aurora, CO 80045, USA
Shukla-Dave Dr A, Assisting Attending Physicist, Memorial Sloan-Kettering Cancer Center, 1275 York Avenue, New York, NY 10065, USA
Eastham Dr J, Urologist, Professor and Head of Urologic Oncology, Memorial Sloan-Kettering Cancer Center, 1275 York Avenue, New York, NY 10065, USA
Ennis Dr R, Radiation Oncologist, Director, Radiation Oncology, St. Luke’s-Roosevelt Hospital Center Associate Director, Continuum Cancer Centres of New York Associate Professor, Radiation Oncology, Albert Einstein College of Medicine
Fowler Dr J, Consultant Physician, Hampshire Clinic, Basing Road, Old Basing, Hampshire, RG24 7AL, UK
Fradet Dr Yves, Urologist, Professor of Surgery and Urology, Quebec City’s Hotel Dieu Hospital, 11 Côte du Palais, Quebec, Canada
Gambhir Dr S, Nuclear Medicine, Director of Molecular Imaging, Stanford Cancer Centre, 318 Campus Drive, East Wing, 1st Floor, Stanford, CA 94305-5427, USA
George Dr D, Oncologist, Associate Professor of Medicine and Surgery, Duke University School of Medicine, Durham, NC 27710, USA
Getzenberg Dr R, Basic Science, Director of Research, John Hopkins University School of Medicine, 733 N. Broadway, Baltimore, MD 21205-2196, USA
Hawkes Professor D, Director, Center for Medical Image Computing, University College London, Gower Street, London WC1E 6BT, UK
Heald Professor R J, Colorectal Surgeon, Surgical Director Pelican Cancer Foundation, The Ark, Dinwoodie Drive, Basingstoke, Hants RG24 9NN, UK
Hindley R Mr, Urologist, Consultant Surgeon, Basingstoke and North Hampshire NHS Foundation Trust, Aldermaston Road, Basingstoke, Hampshire, RG24 9NA, UK
Kirkham Dr A, Radiologist University College London Hospitals NHS Foundation Trust, Gower Street, London WC1E 6BT, UK
Klein Dr E, Urologist, Head of Urologic Oncology, Cleveland Clinic, 9500 Euclid Avenue, Cleveland, OH 44195, USA
Klotz Dr L, Urologist, Chief of Urology, Sunnybrook Health Sciences Centre, 2075 Bayview Avenue, Room MG 204, Toronto, ON, Canada
Menzel Mr W, Executive Director, Peter Michael Foundation, 1 Gate Six Road, Building B, Suite 201, Sausalito, CA 94965, USA
Michael Sir P, Chairman, Peter Michael Foundation, 1 Gate Six Road, Building B, Suite 201, Sausalito, CA 94965, USA Pelican Cancer Foundation, The Ark, Dinwoodie Drive, Basingstoke, Hants RG24 9NN, UK
Padhani Dr A, Radiologist, Department of Radiology, Mount Vernon Cancer Center, Rickmansworth Road, Northwood, Middlesex, HA6 2RN, UK
Rouviere Dr O, Radiologist, Department of Genitourinary Radiology, Hopital E.Herriot, 5, place d’Arsonval 69437 Lyon cedex 03, France
Slawin Dr K, Urologist, Director of Urology, University of Houston, 4800 Calhoun Road, Houston, TX 77004, USA
Tempany-Afdhal Dr C, Ferenc Jolesz Chair of Radiology Research, Brigham Women’s Hospital, Harvard Medical School, 75 Francis Street, Boston, MA 02115 USA
Touijer Dr K, Associated Attending Surgeon, Memorial Sloan-Kettering Cancer Center, 1275 York Avenue, New York, NY 10065, USA
Vickers Dr A, Bio-statistician, Associate Attending Research Methodologist, Memorial Sloan-Kettering Cancer Center, 1275 York Avenue, New York, NY 10065, USA
Vigneron Dr D, Radiologist, Professor of Radiology and Engineering, The University of California, San Francisco, CA 95143, USA
Wheeler Dr T, Pathologist, Professor and Chair of Pathology, Baylor College of Medicine, One Baylor Plaza, Houston, TX 77030, USA
Footnotes
CONFLICT OF INTEREST Hashim U. Ahmed is a Consultant to Steba Biotech and Oncura, and owns shares in Prostate Mapping Ltd. Jonathan A. Coleman is a Study Investigator funded by Sponsors. Mark Emberton is a Consultant to GSK, Sanofi Aventis, and USHIFU, a Director of Mediwatch PLC, holds shares in Prostate Mapping Ltd., and share options in Advanced Medical Diagnostics. Caroline M. Moore is a Paid Consultant to Steba Biotech and receives Research Funding from GSK.
REFERENCES
- 1.Esserman L, Shieh Y, Thompson I. Rethinking screening for breast cancer and prostate cancer. JAMA. 2009;302:1685–92. doi: 10.1001/jama.2009.1498. [DOI] [PubMed] [Google Scholar]
- 2.Schröder FH, Hugosson J, Roobol MJ, et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med. 2009;360:1320–8. doi: 10.1056/NEJMoa0810084. [DOI] [PubMed] [Google Scholar]
- 3.Altekruse SF, Kosary CL, Krapcho M, et al., editors. SEER Cancer Statistics Review, 1975–2007. National Cancer Institute; Bethesda, MD: [Accessed August 2011]. 2010. based on November 2009 SEER data submission, posted to the SEER web site, 2010. Available at: http://seer.cancer.gov/csr/1975_2007/ [Google Scholar]
- 4.Onik G, Miessau M, Bostwick DG. Three-dimensional prostate mapping biopsy has a potentially significant impact on prostate cancer management. J Clin Oncol. 2009;27:4321–6. doi: 10.1200/JCO.2008.20.3497. [DOI] [PubMed] [Google Scholar]
- 5.Ahmed HU, Pendse D, Illing R, Allen C, van der Meulen JH, Emberton M. Will focal therapy become a standard of care for men with localized prostate cancer? Nat Clin Pract Oncol. 2007;4:632–42. doi: 10.1038/ncponc0959. [DOI] [PubMed] [Google Scholar]
- 6.Eggener SE, Scardino PT, Carroll PR, et al. Focal therapy for localized prostate cancer: a critical appraisal of rationale and modalities. J Urol. 2007;178:2260–7. doi: 10.1016/j.juro.2007.08.072. [DOI] [PubMed] [Google Scholar]
- 7.Ahmed HU, Kirkham A, Arya M, et al. Is it time to consider a role for MRI before prostate biopsy? Nat Rev Clin Oncol. 2009;6:197–206. doi: 10.1038/nrclinonc.2009.18. [DOI] [PubMed] [Google Scholar]
- 8.American Urological Association Prostate-specific antigen (PSA) best practice policy. Oncology (Williston Park) 2000;14:267–80. [PubMed] [Google Scholar]
- 9.Vickers A, Cronin A, Roobol M, et al. Reducing unnecessary biopsy during prostate cancer screening using a four-kallikrein panel: an independent replication. J Clin Oncol. 2010;28:2493–8. doi: 10.1200/JCO.2009.24.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Djulbegovic M, Beyth RJ, Neuberger MM, et al. Screening for prostate cancer: systematic review and metaanalysis of randomised controlled trials. BMJ. 2010;341:c4543. doi: 10.1136/bmj.c4543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vickers AJ, Cronin AM, Bjork T, et al. Prostate specific antigen concentration at age 60 and death or metastasis from prostate cancer: case-control study. BMJ. 2010;341:c4521. doi: 10.1136/bmj.c4521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Urological Association [Accessed August 2011];Prostate-Specific Antigen Best Practice Statement. 2009 Update. Available at: http://www.auanet.org/content/guidelines-and-quality-care/clinicalguidelines/main-reports/psa09.pdf.
- 13.Roobol MJ, Steyerberg EW, Kranse R, et al. A risk-based strategy improves prostate-specific antigen-driven detection of prostate cancer. Eur Urol. 2010;57:79–85. doi: 10.1016/j.eururo.2009.08.025. [DOI] [PubMed] [Google Scholar]
- 14.Nam RK, Toi A, Klotz LH, et al. Assessing individual risk for prostate cancer. J Clin Oncol. 2007;25:3582–8. doi: 10.1200/JCO.2007.10.6450. [DOI] [PubMed] [Google Scholar]
- 15.Van den Bergh RC, Roobol MJ, Wolters T, van Leeuwen PJ, Schröder FH. The Prostate Cancer Prevention Trial and European Randomized Study of Screening for Prostate Cancer risk calculators indicating a positive prostate biopsy: a comparison. BJU Int. 2008;102:1068–73. doi: 10.1111/j.1464-410X.2008.07940.x. [DOI] [PubMed] [Google Scholar]
- 16.Vickers AJ, Cronin AM, Aus G, et al. A panel of kallikrein markers can reduce unnecessary biopsy for prostate cancer: data from the European Randomized Study of Prostate Cancer Screening in Göteborg, Sweden. BMC Med. 2008;6:19. doi: 10.1186/1741-7015-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vickers AJ, Cronin AM, Roobol MJ, et al. A four-kallikrein panel predicts prostate cancer in men with recent screening: data from the European Randomized Study of Screening for Prostate Cancer, Rotterdam. Clin Cancer Res. 2010;16:3232–9. doi: 10.1158/1078-0432.CCR-10-0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shukla-Dave A, Hricak H, Kattan MW, et al. The utility of magnetic resonance imaging and spectroscopy for predicting insignificant prostate cancer: an initial analysis. BJU Int. 2007;99:786–93. doi: 10.1111/j.1464-410X.2007.06689.x. [DOI] [PubMed] [Google Scholar]
- 19.Scattoni V, Zlotta A, Montironi R, Schulman C, Rigatti P, Montorsi F. Extended and saturation prostatic biopsy in the diagnosis and characterisation of prostate cancer: a critical analysis of the literature. Eur Urol. 2007;52:1309–22. doi: 10.1016/j.eururo.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 20.Presti JC., Jr Prostate biopsy: how many cores are enough? Urol Oncol. 2003;21:135–40. doi: 10.1016/s1078-1439(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 21.Lawrentschuk N, Haider MA, Daljeet N, et al. Prostatic evasive anterior tumours: the role of magnetic resonance imaging. BJU Int. 2010;105:1231–6. doi: 10.1111/j.1464-410X.2009.08938.x. [DOI] [PubMed] [Google Scholar]
- 22.Ellis WJ, Brawer MK. Repeat prostate needle biopsy: who needs it? J Urol. 1995;153:1496–8. [PubMed] [Google Scholar]
- 23.Franiel T, Stephan C, Erbersdobler A, et al. Areas suspicious for prostate cancer: MR-guided biopsy in patients with at least one transrectal US-guided biopsy with a negative finding–multiparametric MR imaging for detection and biopsy planning. Radiology. 2011;259:162–72. doi: 10.1148/radiol.10101251. [DOI] [PubMed] [Google Scholar]
- 24.Hambrock T, Somford DM, Hoeks C, et al. Magnetic resonance imaging guided prostate biopsy in men with repeat negative biopsies and increased prostate specific antigen. J Urol. 2010;183:520–7. doi: 10.1016/j.juro.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 25.Turkbey B, Shah VP, Pang Y, et al. Is apparent diffusion coefficient associated with clinical risk scores for prostate cancers that are visible on 3-T MR images? Radiology. 2011;258:488–95. doi: 10.1148/radiol.10100667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Villers A, Puech P, Mouton D, Leroy X, Ballereau C, Lemaitre L. Dynamic contrast enhanced, pelvic phased array magnetic resonance imaging of localized prostate cancer for predicting tumor volume: correlation with radical prostatectomy findings. J Urol. 2006;176:2432–7. doi: 10.1016/j.juro.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 27.Puech P, Potiron E, Lemaitre L, et al. Dynamic contrast-enhanced-magnetic resonance imaging evaluation of intraprostatic prostate cancer: correlation with radical prostatectomy specimens. Urology. 2009;74:1094–9. doi: 10.1016/j.urology.2009.04.102. [DOI] [PubMed] [Google Scholar]
- 28.Lemaitre L, Puech P, Poncelet E, et al. Dynamic contrast-enhanced MRI of anterior prostate cancer: morphometric assessment and correlation with radical prostatectomy findings. Eur Radiol. 2009;19:470–80. doi: 10.1007/s00330-008-1153-0. [DOI] [PubMed] [Google Scholar]
- 29.Puech P, Huglo D, Petyt G, Lemaitre L, Villers A. Imaging of organ-confined prostate cancer: functional ultrasound, MRI and PET/computed tomography. Curr Opin Urol. 2009;19:168–76. doi: 10.1097/MOU.0b013e328323f5ed. [DOI] [PubMed] [Google Scholar]
- 30.Berglund RK, Masterson TA, Vora KC, Eggener SE, Eastham JA, Guillonneau BD. Pathological upgrading and up staging with immediate repeat biopsy in patients eligible for active surveillance. J Urol. 2008;180:1964–7. doi: 10.1016/j.juro.2008.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Capitanio U, Karakiewicz PI, Jeldres C, et al. The probability of Gleason score upgrading between biopsy and radical prostatectomy can be accurately predicted. Int J Urol. 2009;16:526–9. doi: 10.1111/j.1442-2042.2009.02270.x. [DOI] [PubMed] [Google Scholar]
- 32.D’Amico AV, Moul J, Carroll PR, Sun L, Lubeck D, Chen MH. Cancer-specific mortality after surgery or radiation for patients with clinically localized prostate cancer managed during the prostatespecific antigen era. J Clin Oncol. 2003;21:2163–72. doi: 10.1200/JCO.2003.01.075. [DOI] [PubMed] [Google Scholar]
- 33.Makarov DV, Trock BJ, Humphreys EB, et al. Updated nomogram to predict pathologic stage of prostate cancer given prostate-specific antigen level, clinical stage, and biopsy Gleason score (Partin tables) based on cases from 2000 to 2005. Urology. 2007;69:1095–101. doi: 10.1016/j.urology.2007.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ahmed H. The index lesion and the origin of prostate cancer. N Engl J Med. 2009;17:1704–6. doi: 10.1056/NEJMcibr0905562. [DOI] [PubMed] [Google Scholar]
- 35.Shukla-Dave A, Hricak H, Ishill NM, et al. Correlation of MR imaging and MR spectroscopic imaging findings with Ki-67, phospho-Akt, and androgen receptor expression in prostate cancer. Radiology. 2009;250:803–12. doi: 10.1148/radiol.2503080473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shukla-Dave A, Hricak H, Ishill N, et al. Prediction of prostate cancer recurrence using magnetic resonance imaging and molecular profiles. Clin Cancer Res. 2009;15:3842–9. doi: 10.1158/1078-0432.CCR-08-2453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gibbs P, Liney GP, Pickles MD, Zelhof B, Rodrigues G, Turnbull LW. Correlation of ADC and T2 measurements with cell density in prostate cancer at 3.0 Tesla. Invest Radiol. 2009;44:572–6. doi: 10.1097/RLI.0b013e3181b4c10e. [DOI] [PubMed] [Google Scholar]
- 38.Itou Y, Nakanishi K, Narumi Y, Nishizawa Y, Tsukuma H. Clinical utility of apparent diffusion coefficient (ADC) values in patients with prostate cancer: Can ADC values contribute to assess theaggressiveness of prostate cancer? J Magn Reson Imaging. 2011;33:167–72. doi: 10.1002/jmri.22317. [DOI] [PubMed] [Google Scholar]
- 39.Woodfield CA, Tung GA, Grand DJ, Pezzullo JA, Machan JT, Renzulli JF., 2nd Diffusion-weighted MRI of peripheral zone prostate cancer: comparison of tumor apparent diffusion coefficient with Gleason score and percentage of tumor on core biopsy. AJR Am J Roentgenol. 2010;194:W316–22. doi: 10.2214/AJR.09.2651. [DOI] [PubMed] [Google Scholar]
- 40.Yoshimitsu K, Kiyoshima K, Irie H, et al. Usefulness of apparent diffusion coefficient map in diagnosing prostate carcinoma: correlation with stepwise histopathology. J Magn Reson Imaging. 2008;27:132–9. doi: 10.1002/jmri.21181. [DOI] [PubMed] [Google Scholar]
- 41.Zelhof B, Pickles M, Liney G, et al. Correlation of diffusion-weighted magnetic resonance data with cellularity in prostate cancer. BJU Int. 2009;103:883–8. doi: 10.1111/j.1464-410X.2008.08130.x. [DOI] [PubMed] [Google Scholar]
- 42.Rastinehad AR, Baccala AA, Jr, Chung PH, et al. D’Amico risk stratification correlates with degree of suspicion of prostate cancer on multiparametric magnetic resonance imaging. J Urol. 2011;185:815–20. doi: 10.1016/j.juro.2010.10.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Verma S, Rajesh A, Morales H, et al. Assessment of aggressiveness of prostate cancer: correlation of apparent diffusion coefficient with histologic grade after radical prostatectomy. AJR Am J Roentgenol. 2011;196:374–81. doi: 10.2214/AJR.10.4441. [DOI] [PubMed] [Google Scholar]
- 44.deSouza NM, Riches SF, Vanas NJ, et al. Diffusion-weighted magnetic resonance imaging: a potential non-invasive marker of tumour aggressiveness in localized prostate cancer. Clin Radiol. 2008;63:774–82. doi: 10.1016/j.crad.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 45.van As NJ, de Souza NM, Riches SF, et al. A study of diffusion-weighted magnetic resonance imaging in men with untreated localised prostate cancer on active surveillance. Eur Urol. 2009;56:981–7. doi: 10.1016/j.eururo.2008.11.051. [DOI] [PubMed] [Google Scholar]
- 46.Zakian KL, Sircar K, Hricak H, et al. Correlation of proton MR spectroscopic imaging with Gleason score based on step-section pathologic analysis after radical prostatectomy. Radiology. 2005;234:804–14. doi: 10.1148/radiol.2343040363. [DOI] [PubMed] [Google Scholar]
- 47.Crawford DE, Wilson SS, Torkko KC, et al. Clinical staging of prostate cancer: a computer-simulated study of transperineal prostate biopsy. BJU Int. 2005;96:999–1004. doi: 10.1111/j.1464-410X.2005.05801.x. [DOI] [PubMed] [Google Scholar]
- 48.Hu Y, Arumainavagam N, Ahmed HU, et al. Comparison between transperineal and transrectal biopsy for the detection of prostate cancer to guide focal therapy. Eur Urol. 2010;9:55. [abstract] [Google Scholar]
- 49.Taira AV, Merrick GS, Galbreath RW, et al. Performance of transperineal template-guided mapping biopsy in detecting prostate cancer in the initial and repeat biopsy setting. Prostate Cancer Prostatic Dis. 2010;13:71–7. doi: 10.1038/pcan.2009.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Langer DL, van der Kwast TH, Evans AJ, et al. Intermixed normal tissue within prostate cancer: effect on MR imaging measurements of apparent diffusion coefficient and T2–sparse versus dense cancers. Radiology. 2008;249:900–8. doi: 10.1148/radiol.2493080236. [DOI] [PubMed] [Google Scholar]
- 51.Ahmed HU, Hu Y, Carter T, et al. Characterising clinically significant prostate cancer using template prostate mapping biopsy. J Urol. 2011;186:458–64. doi: 10.1016/j.juro.2011.03.147. [DOI] [PubMed] [Google Scholar]
- 52.Bouyé S, Potiron E, Puech P, Leroy X, Lemaitre L, Villers A. Transition zone and anterior stromal prostate cancers: zone of origin and intraprostatic patterns of spread at histopathology. Prostate. 2009;69:105–13. doi: 10.1002/pros.20859. [DOI] [PubMed] [Google Scholar]
- 53.Ross AE, Loeb S, Landis P, et al. Prostate-specific antigen kinetics during follow-up are an unreliable trigger for intervention in a prostate cancer surveillance program. J Clin Oncol. 2010;28:2810–6. doi: 10.1200/JCO.2009.25.7311. [DOI] [PubMed] [Google Scholar]
- 54.Klotz L, Zhang L, Lam A, Nam R, Mamedov A, Loblaw A. Clinical results of long-term follow-up of a large, active surveillance cohort with localized prostate cancer. J Clin Oncol. 2010;28:126–31. doi: 10.1200/JCO.2009.24.2180. [DOI] [PubMed] [Google Scholar]
- 55.Carter HB, Kettermann A, Warlick C, et al. Expectant management of prostate cancer with curative intent: an update of the Johns Hopkins experience. J Urol. 2007;178:2364–5. doi: 10.1016/j.juro.2007.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dall’Era MA, Carroll PR. Outcomes and follow-up strategies for patients on active surveillance. Curr Opin Urol. 2009;19:258–62. doi: 10.1097/MOU.0b013e328329eba3. [DOI] [PubMed] [Google Scholar]
- 57.Shariat SF, Kattan MW, Vickers AJ, Karakiewicz PI, Scardino PT. Critical review of prostate cancer predictive tools. Future Oncol. 2009;5:1555–84. doi: 10.2217/fon.09.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pauly KB, Diederich CJ, Rieke V, et al. Magnetic resonance-guided highintensity ultrasound ablation of the prostate. Top Magn Reson Imaging. 2006;17:195–207. doi: 10.1097/RMR.0b013e31803774dd. [DOI] [PubMed] [Google Scholar]
- 59.Hu Y, Ahmed HU, Allen C, et al. MR to ultrasound image registration for guiding prostate biopsy and interventions. Med Image Comput Comput Assist Interv. 2009;12:787–94. doi: 10.1007/978-3-642-04268-3_97. [DOI] [PubMed] [Google Scholar]
- 60.Ahmed HU, Moore C, Lecornet E, Emberton M. Focal therapy in prostate cancer: determinants of success and failure. Focal therapy in prostate cancer: determinants of success and failure. J Endourol. 2010;24:819–25. doi: 10.1089/end.2009.0665. [DOI] [PubMed] [Google Scholar]
- 61.Beerlage HP, van Leenders GJ, Oosterhof GO, et al. High-intensity focused ultrasound (HIFU) followed after one to two weeks by radical retropubic prostatectomy: results of a prospective study. Prostate. 1999;39:41–6. doi: 10.1002/(sici)1097-0045(19990401)39:1<41::aid-pros7>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 62.Lindner U, Lawrentschuk N, Weersink RA, et al. Focal laser ablation for prostate cancer followed by radical prostatectomy: validation of focal therapy and imaging accuracy. Eur Urol. 2010;57:1111–4. doi: 10.1016/j.eururo.2010.03.008. [DOI] [PubMed] [Google Scholar]