Abstract
Objectives. We evaluated a strategy for preventing tuberculosis (TB) in communities most affected by it.
Methods. In 1996, we mapped reported TB cases (1985–1995) and positive tuberculin skin test (TST) reactors (1993–1995) in Smith County, Texas. We delineated the 2 largest, densest clusters, identifying 2 highest-incidence neighborhoods (180 square blocks, 3153 residents). After extensive community preparation, trained health care workers went door-to-door offering TST to all residents unless contraindicated. TST-positive individuals were escorted to a mobile clinic for radiography, clinical evaluation, and isoniazid preventive treatment (IPT) as indicated. To assess long-term impact, we mapped all TB cases in Smith County during the equivalent time period after the project.
Results. Of 2258 eligible individuals, 1291 (57.1%) were tested, 229 (17.7%) were TST positive, and 147 were treated. From 1996 to 2006, there were no TB cases in either project neighborhood, in contrast with the preintervention decade and the continued occurrence of TB in the rest of Smith County.
Conclusions. Targeting high-incidence neighborhoods for active, community-based screening and IPT may hasten TB elimination in the United States.
According to a 1999–2000 tuberculin skin test (TST) survey, an estimated 4.2% of the US population—approximately 11 million people—had latent Mycobacterium tuberculosis infection (LTBI).1 Reactivation of LTBI accounts for an estimated 70% of incident tuberculosis (TB) disease in the United States.2,3 Eliminating TB in the United States will require preventing these cases.
Treating LTBI with 6 to 12 months of isoniazid can substantially reduce TB incidence.2,4–7 But how can 11 million individuals be identified and treated without testing the entire population? Testing for LTBI in the general population is not recommended because the predictive value of a positive TST under conditions of low prevalence is poor, and skin testing should be limited to persons at high risk.2,8,9 Moreover, active screening and preventive treatment programs typically fail because of high rates of nonparticipation and attrition at each step of the process. The keys to active, community-based screening and preventive treatment would be to target high-risk populations with an efficient strategy, maximize participation, and minimize losses to follow-up so that the entire process becomes cost-effective.
Many local health departments map cases of communicable diseases in their communities, displaying wall-mounted maps with color-coded pins indicating each case. Dense clusters of pins identify the hardest-hit neighborhoods. The modern version of this venerable practice involves use of a computerized geographic information system (GIS). We hypothesized that this information could identify neighborhoods at high risk of TB. If TB concentrates in specific neighborhoods, persisting over many years, then cases will likely continue occurring in these same neighborhoods. Targeting these neighborhoods with screening and prevention programs should prevent future TB cases. Using a GIS, we identified 2 high-risk neighborhoods in Smith County, Texas, and conducted a door-to-door screening and preventive treatment project. Ten years later, we assessed the impact of this strategy by comparing TB incidence in the target neighborhoods before and after the project with TB incidence in the rest of the county.
METHODS
The Texas Department of State Health Services provided the home address of record for all reported TB cases in Smith County, Texas from 1985 through 1995 (n = 128) and for all reported positive TST reactors from 1993 through 1995 (n = 311). Reporting of TB cases is required by law, and virtually all cases are reported. Reporting of positive skin test reactions without active disease is not required, so the number of TST reactors underestimates the true prevalence of latent TB infection. Nonetheless, most cases of LTBI are recorded in health department records because it provides testing and treatment at no charge to the individual. We geocoded and displayed addresses using ArcGIS software (ESRI, Redlands, CA). We included TST reactors because they identify transmission of infection and persons at increased risk for developing TB. We delineated the 2 largest, densest clusters of points, identifying the 2 highest incidence neighborhoods in the county. Ten years later, we repeated the process, mapping the home addresses of all reported TB cases in Smith County from 1996 through 2006. We compared the distribution of TB cases before and after the project in the target neighborhoods and the rest of the county. To protect the privacy of individuals, point maps are displayed on plain coordinate axes without landmarks that could identify individuals’ homes.
Community Preparation
We enumerated all housing units in the target neighborhoods and identified all nonresidential establishments. Using a distinctive logo, we prepared bilingual (English and Spanish) posters and leaflets describing the voluntary TST program, displaying posters and distributing leaflets throughout the neighborhoods. Ministers announced the project during worship services and distributed leaflets to their parishioners. Schools sent leaflets home in the report cards of all schoolchildren. Public service announcements conveyed the same information in newspapers and local periodicals and on radio and television stations in English and Spanish, with telephone numbers for those wanting additional information.
Field Work
Field workers wore T-shirts bearing the same logos and conspicuous photo identification badges identifying them as employees of the University of Texas or the Smith County Public Health District. Four to 5 field workers went door-to-door evenings and weekends during 5 summer months of 1996. At each residence, they explained the project, provided information about TB, and invited residents to participate, offering skin tests on the spot at no charge for any part of this project. For residents who declined or were not at home, field workers left printed information and returned at a later date, on different days of the week and at different times of day. To establish a population denominator, we recorded the number, age, gender, and race/ethnicity of each resident in every household.
Residents were eligible for skin testing if they were at least 1 year of age, had not been tested in the past year, and consented in writing to be tested. Residents were not eligible if they had a history of TB, a positive TST, or prior isoniazid preventive treatment (IPT). We administered a standard Mantoux TST, reading the results after 48 to 72 hours. In addition, we recorded country of birth and history of Bacillus Calmette–Guérin (BCG) vaccination, and checked for a BCG scar.
Persons with skin test reactions of 10-mm induration or greater were escorted to our mobile clinic stationed nearby for chest radiography and clinical evaluation. A physician prescribed IPT following Centers for Disease Control and Prevention (CDC) guidelines. After counseling and education, the physician provided the first month’s supply of medication and arranged a 1-month follow-up appointment with the Smith County Health Department to continue treatment and follow-up.
Analysis
Analysis of the results focused on participation, TST reactions, isoniazid treatment, and subsequent TB incidence. We used the Pearson χ2 test and Fisher exact test to compare proportions and cumulative incidence. We used the t test or Wilcoxon rank sum test to compare continuous variables. We used multivariable logistic regression to determine the independent effects of each variable, controlling for potential confounding by the other factors. A P value less than .05 was considered statistically significant.
RESULTS
The successful mapping rate was 88% for TB cases and 92% for the positive reactors in the preintervention period. These were augmented to 91% and 95%, respectively, by field workers who physically located nonmatching addresses and included them on maps.
The maps showed several clusters of points in the city of Tyler, 2 of them larger and denser than the others, corresponding to 2 low- to middle-income neighborhoods (Figures 1 and 2). To account for population density, choropleth maps of US Census Bureau population counts by block are displayed adjacent to the point maps. The maps are displayed on plain coordinate axes, to preserve the spatial pattern and protect individuals’ privacy. The target neighborhoods are outlined in Figures 2 and 3. Neighborhood 1 was 10 × 12 blocks and neighborhood 2 was 6 × 10 blocks. The number of TB cases decreased from 15 of 128 total cases in Smith County in 1985 through 1995 (Figures 2 and 4) to zero of 75 in 1996 through 2006 (Figures 3 and 4; P = .002). One case occurred 1 block outside of neighborhood 2 (Figure 3).
FIGURE 1—

Geographical representation of (a) reported tuberculosis (TB) cases (1985–1995) and positive skin test reactors (1993–1995) and (b) population density by census block according to the 1990 decennial census: Smith County, TX.
FIGURE 2—
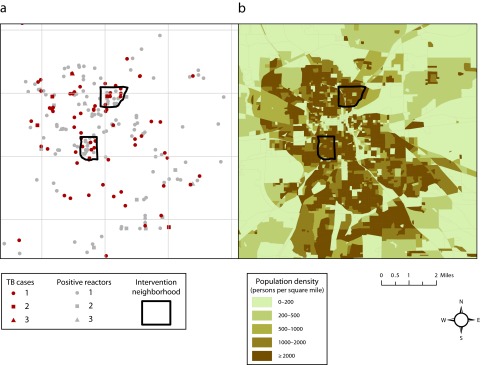
Geographical representation of (a) reported tuberculosis (TB) cases (1985–1995) and positive skin test reactors (1993–1995) and (b) population density by census block according to the 1990 decennial census: Tyler metropolitan area, Smith County, TX.
Note. The map includes the boundaries of 2 neighborhoods targeted for tuberculosis screening and prevention.
FIGURE 3—

Geographical representation of (a) reported tuberculosis (TB) cases (1996–2006) and (b) population density by census block according to the 2000 decennial census: Tyler metropolitan area, Smith County, TX.
Note. The map includes the boundaries of 2 neighborhoods targeted for tuberculosis screening and prevention.
FIGURE 4—
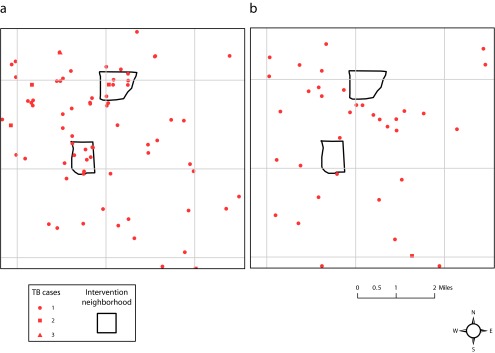
Relative spatial location of reported tuberculosis (TB) cases for (a) 1985–1995 and (b) 1996–2006: Tyler metropolitan area, Smith County, TX.
Note. The map includes the boundaries of 2 neighborhoods targeted for tuberculosis screening and prevention.
Household Characteristics and Relationship to Screening
There were 1013 occupied dwelling units in the 2 neighborhoods (Table 1). Occupants of 512 households (50.5%) opened the door and agreed to be skin tested. There were no significant differences between the neighborhoods in response and participation rates.
TABLE 1—
Household-Level Characteristics in Relation to Tuberculin Skin Testing: Smith County, TX, 1996
| Characteristic | No. (%) or Mean ±SD (Median; Range) |
| Householdsa | 1013 |
| People per household | 3.3 ±2.2 (3; 1–14) |
| Households tested | 512 (50.5) |
| People tested in tested households | 3.8 ±2.3 (3; 1–14) |
| People not tested in tested households | 2.6 ±1.8 (2; 1–11) |
| African American householdsb | |
| Total | 233 (23.0) |
| Tested | 106 (45.5) |
| Hispanic householdsb | |
| Total | 354 (34.9) |
| Tested | 262 (74.1) |
| Non-Hispanic White householdsb | |
| Total | 291 (28.7) |
| Tested | 143 (49.1) |
Households include houses, apartments, mobile homes, and other dwellings in which noninstitutionalized civilians normally eat and sleep.
Mixed households are included in these figures under the race/ethnicity of the head of household. The 14 mixed households included White–Hispanic (n = 5), African American–Hispanic (n = 4), African American–White (n = 4), and White–Asian (n = 1).
Larger households, in terms of the number of residents, were more likely to agree to skin testing. Only 78 of 232 single-occupant households (33.6%) agreed to skin testing, compared with 434 of 714 multioccupant households (60.8%). Households were larger in neighborhood 1 (median = 4; interquartile range [IQR] = 2–5) than in neighborhood 2 (median = 2; IQR = 1–4; P < .001), but the relationships between skin testing and household size held true in both neighborhoods.
The neighborhoods differed in the racial/ethnic composition of households. Neighborhood 1 had a higher proportion of Hispanic households, whereas neighborhood 2 was evenly mixed between Hispanic, African American, and non-Hispanic White households. On average, Hispanic households had more residents and also were more likely to participate: 262 (74.0%) agreed to skin testing, compared with 143 non-Hispanic White households (49.1%) and 106 African American households (45.5%; P < .001), but these proportions were similar for both neighborhoods (P > .5). By multivariable logistic regression, race/ethnicity and household size were each independently associated with the probability of participation. For each additional person in the household (up to 8 or more) the adjusted odds ratio for any testing within the household was 1.26 (95% confidence interval [CI] = 1.15, 1.39).
In terms of personnel time, field work continued for 98 days. Skin tests were placed on 76 of these days, including 65 days of regularly scheduled field work and 11 days with return trips to test a single individual. Field workers read TSTs on 77 days, including 65 regularly scheduled and 12 special trips. Chest radiographs were obtained on 44 days. Field workers completed their visits to the 1013 occupied households at a rate of 10.3 per day of field work (13.3 per day of skin testing). They completed testing of the 512 tested households at a rate of 5.2 per day of field work (6.7 per day of skin testing).
Person-Level Characteristics and Relationship to Screening
We enumerated 3153 residents of these 2 neighborhoods, and complete data were available for 2881 (91.4%; Table 2). Hispanics comprised 1654 (57.4%) of this population, African Americans 651 (22.6%), and non-Hispanic Whites 576 (20.0%). Denominators for each variable and cross-tabulation exclude missing data. Overall, there were 1464 female (50.9%) and 1416 male (49.1%) participants, similar in both neighborhoods. The median age was 23.0 years in neighborhood 1 (IQR = 10.0–38.0) and 27.0 years in neighborhood 2 (IQR = 12.0–40.0; P < .001). Neighborhood 1 included larger families, especially Hispanic families with more children, than neighborhood 2.
TABLE 2—
Person-Level Characteristics in Relation to Participation in Tuberculin Skin Testing: Smith County, TX, 1996
| Characteristic | No (%) or Mean ±SD (Median; Range) | P |
| Total enumerated populationa | 3153 | |
| Complete data availableb | 2881 (91.4) | |
| Total | ||
| Eligible | 2258 (57.1) | |
| Tested | 1291 (57.1) | |
| Refused | 968 (33.6) | |
| Ineligible | 622 (21.6) | |
| Gender | ||
| Tested | < .001 | |
| Male | 585 (20.3) | |
| Female | 706 (24.5) | |
| Refused | < .001 | |
| Male | 537 (18.6) | |
| Female | 430 (14.9) | |
| Ineligible | .3 | |
| Male | 294 (10.2) | |
| Female | 328 (11.4) | |
| Age, y | ||
| Tested | 28.17 ±19.41 (25; 1–92) | .26c |
| Refused testing | 29.73 ±21.47 (27; 0–94) | .001d |
| Ineligible | 24.80 ±19.25 (23; 0–87) | .001e |
| Race/ethnicity | ||
| Tested | < .001 | |
| African American | 202 (7.0) | |
| Hispanic | 859 (29.8) | |
| Non-Hispanic White | 229 (7.9) | |
| Refused | ||
| African American | 275 (9.6) | |
| Hispanic | 445 (15.5) | |
| Non-Hispanic White | 246 (8.6) | |
| Ineligible | ||
| African American | 187 (6.5) | |
| Hispanic | 315 (10.9) | |
| Non-Hispanic White | 119 (4.1) | |
For households refusing to answer any questions, the person answering the door was counted as 1.
Subsequent percentages and statistics are based on a denominator of n = 2881.
For tested vs refused.
For tested vs ineligible.
For refused vs ineligible.
Results of Screening and Isoniazid Preventive Treatment
Of the 2258 (74.3%) eligible for testing, 1291 (57.1%) had skin tests placed, and 1236 of these (95.7%) had their skin test results read (Table 3). We found 229 (18.5%) positive skin test reactions of 10-mm induration or more. The median diameter of positive skin tests was 17 mm (IQR = 13–20). Positive TST reactions were found in 156 of 759 persons (20.6%) in neighborhood 1 and in 73 of 477 persons (15.3%) in neighborhood 2 (P = .025).
TABLE 3—
Results of Descriptive Analysis of Tuberculosis Skin Testing and Initiation of Isoniazid Preventive Treatment: Smith County, TX, 1996
| Category | No. (%) | P |
| People tested | 1291 | |
| People with known results | 1236 (95.7) | |
| People with ≥ 10-mm induration | 229 (18.5) | |
| Positive TST result by gender | .5 | |
| Male | 108 (19.4) | |
| Female | 121 (17.8) | |
| Positive TST results by age group, y | < .001 | |
| 1–14 | 17 (4.6) | |
| 15–24 | 33 (15.6) | |
| 25–44 | 118 (28.2) | |
| 45–64 | 47 (28.7) | |
| ≥ 65 | 14 (20.6) | |
| Positive TST results by race/ethnicity | < .001 | |
| African American | 17 (8.8) | |
| Hispanic | 197 (23.8) | |
| Non-Hispanic White | 15 (6.9) | |
| Positive TST results, by BCG history | < .001 | |
| BCG positive | 138 (35.6) | |
| BCG negative | 77 (9.6) | |
| BCG unknown | 14 (28.0) | |
| Positive TST results, by place of birth | < .001 | |
| Foreign-born | 183 (34.3) | |
| US-born | 44 (6.4) | |
| Isoniazid indicated | ||
| Total tested | 142 (11.0) | |
| TST positive | 141 (64.4) | |
| Isoniazid initiated | 141 (99.3) |
Note. BCG = bacillus Calmette–Guérin vaccination; TST = tuberculin skin test.
Using multivariable logistic regression, we determined that age, African American race or Hispanic ethnicity, foreign birth, and history of BCG vaccination were independent predictors of TST reactivity (Table 3). The strongest risk factors, each relative to its respective reference group, were foreign birth (adjusted odds ratio [AOR] = 3.23; P < .001), Hispanic ethnicity (AOR = 3.16; P = .01), African American race (AOR = 2.26; P = .04), single-occupancy residence (AOR = 2.23; P = .05), and BCG vaccination (AOR = 2.04; P = .001). Gender, neighborhood, and household size other than single occupancy were not independent predictors of tuberculin reactivity.
Of the 229 individuals with positive skin test reactions, 219 (95.6%) had chest radiographs (i.e., only 10 people failed to follow through at this stage). Among these, 184 (84.0%) had normal chest radiographs, 23 (10.5%) showed evidence of old, healed TB (calcified granulomas or fibrosis), and 4 suggested the possibility of an active disease process. These 4 individuals were evaluated at the University of Texas Health Science Center, and active TB disease was ruled out in all 4 cases. The remaining 12 persons had radiographic abnormalities unrelated to TB (e.g., previous surgery or trauma). There were no significant differences between the 2 neighborhoods with respect to the clinical evaluation or radiographic findings.
IPT was indicated for 142 individuals: 62.0% of the 229 with positive tuberculin reactions, or 11.5% of the 1236 with known skin test results. In 1996, the CDC did not recommend IPT for individuals older than 35 years with positive TSTs of indeterminate age (i.e., without evidence of recent skin test conversion). Thus, isoniazid was initiated in 141 of 142 individuals: 99.3% of those in whom it was indicated, 61.1% of those who were TST positive, and 10.9% of those who were tested. There were no significant differences between the 2 neighborhoods in this respect. In addition, 17 further members of the households of these 141 individuals self-referred because they were not available when the field workers visited their homes. They were evaluated and prescribed IPT by the county health department. Of these 158 people, 5 refused treatment and 6 moved away. Of the remaining 147 people, 68 of 147 (46%) completed at least 6 months of isoniazid, 75 (51%) completed at least 5 months, 89 (61%) completed 4 months or more, and 101 (69%) completed at least 3 months of treatment. The remaining 46 individuals received 2 months or less of treatment.
Incidence of Tuberculosis, 1996–2009
TB incidence declined from 15 cases (1985–1995) to zero cases (1996–2006) in the target neighborhoods, compared with 128 cases decreasing to 75 cases in Smith County overall (P = .002). Over this same period, the overall number of cases in Texas decreased from 23 852 to 18 491. Subsequently, 18 cases were reported in Smith County from 2007 through 2009, including one 2007 case within neighborhood 2. None of the people tested and treated in 1996 were among these cases. On the basis of population denominators from the US Census Bureau, TB incidence rates in Smith County averaged 8.1 per 100 000 people per year (95% CI = 5.2, 11.0) from 1985 to 1995 and 3.7 per 100 000 people per year (95% CI = 1.2, 6.1) from 1996 to 2006. Over this same period, the overall rate in Texas decreased from 12.5 per 100 000 people per year (95% CI = 10.2, 14.8) to 8.1 per 100 000 people per year (95% CI = 5.7, 10.4). By contrast, annual TB incidence in the 2 target neighborhoods averaged 39.6 per 100 000 people per year (95% CI = 30.4, 48.8) from 1985 to 1995, zero from 1996 to 2006 (P < .001), and 1.4 per 100 000 people per year (95% CI = 0, 6.0) from 1996 to 2009 (P < .001), which represents a single case in 2007.
DISCUSSION
The Institute of Medicine’s 2000 report Ending Neglect calls for accelerating the decline of TB by increasing targeted tuberculin testing and treatment of latent infection.10 The institute’s recommendation followed a CDC report that 79.7% of potentially preventable TB cases among minorities occurred in only 106 counties with 10 or more such cases, representing only 3.4% of the total 3138 counties in the United States.11 The CDC therefore recommended that “representatives and health care providers from at-risk communities, appropriate government agencies, and interested organizations should work collectively with these counties to intensify TB elimination efforts.”11(p7–8) This application of a GIS to identifying high-risk neighborhoods followed by active, community-based TB screening and preventive treatment fits precisely with this mandate.
In terms of geographic area and population size, counties and zip codes are relatively large, heterogeneous units. TB screening and prevention programs would likely include too many low-risk individuals and would be too large in scope for most local public health project budgets. A better means of targeting high-risk communities was needed. We reasoned that if we mapped TB cases and their infected contacts at the level of their specific home addresses, and aggregated these data over many years, TB would tend to cluster in certain neighborhoods. If the spatial distribution remained relatively stable or increased over many years, it should predict high-risk areas for future TB cases at the neighborhood level. In simple terms, the past location of TB in a community, epidemiologically speaking, may be the best predictor of the location of future TB cases. A similar principle was applied by Moonan et al., who combined GIS analysis with molecular epidemiological surveillance to identify geographic areas of increased same-strain transmission and increased rates of infection.12,13
The rate of tuberculin positivity in the 2 target neighborhoods exceeded the estimated national average by nearly 4.5-fold.1 The CDC has defined a number of high-risk groups that should be targeted for screening and prevention, including foreign-born persons from high-prevalence countries and medically underserved low-income populations, including racial or ethnic minorities.3,9,11 These were precisely the characteristics of the 2 neighborhoods. According to the CDC,
Each health department should assess the prevalence, incidence, and sociodemographic characteristics of cases and infected persons in their community. On the basis of these data, tuberculin screening programs should be targeted to each community’s high-risk groups.14(p1628)
These risk factors could be expanded to included residents of high-incidence communities.
We attribute the success of this project to several factors. First, without address-level mapping and the long time line to accrue baseline data, spatial clustering may not have been apparent. Second, extensive community liaison work and culturally appropriate promotion of this project before starting the actual skin testing gave community residents advance notice and gave the field workers meaningful credibility. Third, from the perspective of the field workers standing at the front door, the statement that there had been many TB cases in that specific neighborhood was the unique “hook” that made the project immediately relevant and clearly affected residents’ decisions to allow themselves to be tested. Fourth, door-to-door outreach by mobile teams of field workers who carried out skin testing on the spot and escorted positive TST reactors to a nearby mobile clinic staffed by a radiology technician and physician maximized participation and minimized attrition since field workers knew where to find each participant. Thus, 57.1% of eligible residents agreed to participate (21.6% of residents were not eligible because of previous skin testing). Of those who had skin tests placed, 95.7% had their skin tests read. Of those with positive TST results, 95.6% had chest radiography. Although IPT was indicated in 142 persons, 147 people actually started IPT because additional household members came forward for testing and treatment.
Demographic changes probably do not account for the drop in TB incidence because the populations increased, including groups considered at high risk of TB. The target neighborhoods fall entirely within 2 census tracts with a 1990 population of 10 475 increasing to 11 473 in 2000. Of these, Hispanics constituted 24% of the population in 1990 and 42% in 2000. Racial categories are not strictly comparable between the 1990 and 2000 census; with that caveat, self-identified race/ethnicity in 1990 and 2000, respectively, was as follows: White, 55% and 50%; African American, 28% and 23%; all other (including Asian/Pacific Islander, Native American/Alaska Native, and people of 2 or more races), 16% and 27%. There were no major shifts in gender or age distribution. In 1990, foreign-born persons accounted for 14% of the population, increasing to 24% in 2000. Of residents aged 5 years or older in 2000, approximately 55% were living in the same house in 1995, 30% came from another house in the same county, and the rest came from outside the county.
The total budget for this project was $65 000, including setting up in-house GIS capabilities, personnel (5 field workers at 30 hours/week for 5 months, overtime pay for a radiology technician, and 15% of a physician), printing and communications costs, skin testing supplies, tuberculin, and isoniazid. The mobile clinic and x-ray unit was owned by the health department, and its use was contributed in kind. On the basis of the number of persons tested and treated and the effectiveness of IPT, we estimated that 7 to 14 TB cases were prevented among participants in this program, consistent with an expected number of 9 to 11 cases in the target neighborhoods on the basis of TB incidence in Smith County over the same time period. These figures do not include secondary cases among contacts of each case. In an era of gradually declining TB incidence, each active case gives rise to fewer than 1 new case. On the basis of a reproductive number of 0.9, assuming 80% effectiveness of IPT, we estimate that 12 to 21 TB cases may have been prevented at a cost of $3096 to $5417 per case prevented. This is substantially lower than the mean national cost per case of $13 500, determined by averaging the estimated $4000 mean cost per case of ambulatory care and the estimated $23 000 mean cost per case of inpatient care, each representing approximately 50% of TB cases in the United States.15–17 In the current era of declining resources for TB control, any cost-saving preventive measures should be seriously considered.
Limitations
This project had important limitations. First, it was a programmatic intervention, not a randomized controlled trial. We targeted neighborhoods with the historically largest, densest aggregations of TB morbidity to maximize the potential public health impact. We did not select the intervention neighborhoods at random, and there were no concurrent control neighborhoods. Instead, we compared our results with the rest of Smith County because the entire county was served by the same TB control program with the same personnel, resources, and procedures. Second, although treatment was turned over to the county health department, the sharp increase in the number of referrals from this project was taxing to the local health department’s capacity in the short term, and completion of treatment rates were suboptimal. This may not be substantially different from the norm; a recent study at public and private clinics in 19 regions of the United States and Canada found that less than half of those who began IPT actually completed therapy.18 In retrospect, we would have supported the health department with 1 half-time additional staff member or retained 1 of the field workers to follow up on IPT. This would affect cost estimates of replicating this project elsewhere.
Conclusions
Screening programs are often carried out in collaboration with community-based organizations, academic centers, and other interested groups outside of the local health department. The type of project described in this report fits well with the CDC’s recommendation that
health departments should work with community-based organizations and health care providers to plan and initiate tuberculin screening and preventive therapy programs specifically adjusted to each community’s at-risk groups.11(p10)
In Smith County, targeting 2 high-risk neighborhoods on the basis of the location of past TB cases and positive skin test reactors followed by active community-based screening and preventive treatment appeared to substantially decrease subsequent TB incidence. Aggressive implementation of screening and chemoprophylaxis in high-risk neighborhoods and communities based on the geographic and historical epidemiology of TB should be further evaluated to determine if the results obtained in this project could be replicated and scaled up.
Acknowledgments
This project was supported by a Tuberculosis Innovative Demonstration Project Grant from the Texas Department of State Health Services, Austin.
We thank Ron Jung and Robert Shepherd, MD, of the Department of Radiology at UTHSC, for their assistance in taking and reading chest radiographs; the computer/GIS contributions of Sara Shepherd, Jack Mills, Leann Giley, and Pat Whitham; field workers Abby Sanchez and Cynthia Ruffin; Texas Department of State Health Services Region 4/5N personnel Teresa Santiago, Brandi Bradford, and Doris Waits; and Smith County Health Department personnel Dominic Sciarrini and Darlene Barnett for their contributions to this project.
Human Participant Protection
This project was approved by the institutional review boards or their equivalent at the University of Texas Health Science Center at Tyler, the Texas Department of State Health Services, and the Centers for Disease Control and Prevention.
References
- 1.Bennett DE, Courval JM, Onorato Iet al. Prevalence of tuberculosis infection in the United States population: The National Health and Nutrition Examination Survey, 1999–2000. Am J Respir Crit Care Med. 2008;177(3):348–355 [DOI] [PubMed] [Google Scholar]
- 2.American Thoracic Society Targeted tuberculin testing and treatment of latent tuberculosis infection. Am J Respir Crit Care Med. 2000;161(4 pt 2):S221–S247 [DOI] [PubMed] [Google Scholar]
- 3.Reported Tuberculosis in the United States, 2009. Atlanta, GA: Centers for Disease Control and Prevention; October 2010 [Google Scholar]
- 4.Ferebee SH. Controlled chemoprophylaxis trials in tuberculosis: a general review. Bibl Tuberc. 1970;26:28–106 [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention The use of preventive therapy for tuberculous infection in the United States: recommendations of the Advisory Committee for Elimination of Tuberculosis. MMWR Recomm Rep. 1990;39(RR–8):6–12 [PubMed] [Google Scholar]
- 6.Comstock GW, Woolpert SF. Preventive therapy. : Kubica GP, Wayne LG, The Mycobacteria: A Sourcebook. New York, NY: Marcel Dekker Inc; 1984:1071–1082 [Google Scholar]
- 7.International Union Against Tuberculosis, Committee on Prophylaxis Efficacy of various durations of isoniazid preventive therapy for tuberculosis: five years of follow-up in the IUAT trial. Bull World Health Organ. 1982;60(4):555–564 [PMC free article] [PubMed] [Google Scholar]
- 8.Horsburgh CR., Jr Priorities for the treatment of latent tuberculosis infection in the United States. N Engl J Med. 2004;350(20):2060–2067 [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention Screening for tuberculosis and tuberculosis infection in high-risk populations: recommendations of the Advisory Council for the Elimination of Tuberculosis. MMWR Recomm Rep. 1995;44(RR–11):19–34 [PubMed] [Google Scholar]
- 10.Geiter L, Ending Neglect: The Elimination of Tuberculosis in the United States. 1st ed Washington, DC: National Academy Press; 2000 [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention Prevention and control of tuberculosis in US communities with at-risk minority populations: recommendations of the Advisory Council for the Elimination of Tuberculosis. MMWR Recomm Rep. 1992;41(RR–5):1–11 [PubMed] [Google Scholar]
- 12.Moonan PK, Bayona M, Quitugua TNet al. Using GIS technology to identify areas of tuberculosis transmission and incidence. Int J Health Geogr. 2004;3(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moonan PK, Oppong J, Sahbazian Bet al. What is the outcome of targeted tuberculosis screening based on universal genotyping and location? Am J Respir Crit Care Med. 2006;174(5):599–604 [DOI] [PubMed] [Google Scholar]
- 14.American Thoracic Society Control of tuberculosis in the United States. Am Rev Respir Dis. 1992;146(6):1623–1633 [DOI] [PubMed] [Google Scholar]
- 15.Brown RE, Miller B, Taylor WRet al. Health-care expenditures for tuberculosis in the United States. Arch Intern Med. 1995;155(15):1595–1600 [PubMed] [Google Scholar]
- 16.Taylor Z, Marks SM, Rios Burrows NM, Weis SE, Stricof RL, Miller B. Causes and costs of hospitalization of tuberculosis patients in the United States. Int J Tuberc Lung Dis. 2000;4(10):931–939 [PMC free article] [PubMed] [Google Scholar]
- 17.Marks SM, Taylor Z, Miller BI. Tuberculosis prevention versus hospitalization: taxpayers save with prevention. J Health Care Poor Underserved. 2002;13(3):392–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Horsburgh CR, Goldberg S, Bethel Jet al. Latent TB infection treatment acceptance and completion in the United States and Canada. Chest. 2010;137(2):401–409 [DOI] [PubMed] [Google Scholar]


