Abstract
The decline of coronary heart disease mortality in the United States and Western Europe is one of the great accomplishments of modern public health and medicine. Cardiologists and cardiovascular epidemiologists have devoted significant effort to disease surveillance and epidemiological modeling to understand its causes. One unanticipated outcome of these efforts has been the detection of early warnings that the decline had slowed, plateaued, or even reversed. These subtle signs have been interpreted as evidence of an impending public health catastrophe. This article traces the history of research on coronary heart disease decline and resurgence and situates it in broader narratives of public health catastrophism. Juxtaposing the coronary heart disease literature alongside the narratives of emerging and reemerging infectious disease helps to identify patterns in how public health researchers create data and craft them into powerful narratives of progress or pessimism. These narratives, in turn, shape public health policy.
CORONARY HEART DISEASE (CHD) took a devastating toll on the United States in the 20th century, killing more people than any other disease. It remains the leading cause of death in most countries worldwide. In the United States, the epidemic peaked in the mid-1960s and has now fallen 60% from its zenith. Similar declines have occurred throughout the developed world, from Finland to Australia. When this decline was first recognized in the 1970s, it became a cause of both celebration and inquiry. In the four decades since that time, researchers have sought to determine who or what deserves credit for this decline. They have developed systems of cardiovascular surveillance to collect data from large populations and they have designed sophisticated computer models to enumerate the relative contributions of risk factor reduction and health care in achieving this large-scale public health improvement.1
Efforts to explain the decline in cardiovascular mortality took a surprising twist in the 1980s, when the very mechanisms designed to analyze the decline revealed incredibly subtle signs of resurgence. In certain groups in certain countries the decline of CHD has slowed, plateaued, or even reversed. Some researchers fear that, for the first time, the next generation of Americans might live shorter, less healthy lives than their parents.2 Coupled with the ominous rise of CHD in low- and middle-income countries worldwide, the signs of reversed decline have fostered new narratives of an impending global CHD catastrophe.
Preliminary evidence of reversal, however, does not in itself spell catastrophe. Several years from now we might look back on such reports merely as passing bumps in the road toward continuing global decline in cardiovascular mortality. Or we might look back on these reports as harbingers of far, far worse health outcomes yet to come. Epidemiological observations are rarely read as independent data points. Instead, researchers recruit them into larger narratives of catastrophe or improvement.
In this article, we trace the history of research on CHD decline and reversal and situate it in the context of the broader academic and popular discourses on emerging infectious disease. Late 20th-century public health narratives about communicable and noncommunicable disease have both exhibited oscillations between narratives of progress and doom. Their juxtaposition, read in light of the sociology of expectations, helps to identify patterns in how researchers create and respond to data. Recognizing these patterns is crucial as the international community increasingly acknowledges the need to shift the goals of global health beyond HIV, tuberculosis, and malaria to meet the challenge of cardiovascular disease, cancer, diabetes, and mental illness. The same data can support different public health narratives depending on the author’s vantage, agenda, and audience. Interpretations function as projective tests: the stories that researchers tell give meaning to data such that even small signals, interpreted in the context of growing public health catastrophism, take on great significance. As epidemiological observations become the basis for national and global health policies, it is crucial that these policies not be overly determined by a rhetoric of fear alone.
THE RISE AND DECLINE OF CORONARY HEART DISEASE
The common narrative of CHD in the 20th century is a triumphalist one. Coronary heart disease rose from relative obscurity in the late 19th century to take a devastating toll in the 20th. By 1960 it killed one third of all Americans, striking down men—most visibly—from every rank of society. The first tidings of changing fortune came in 1964 when health officials reported a decline in CHD mortality in California.3 This good news, however, received little attention. Well into the 1970s cardiologists and the national media continued to sound the alarm about the unstoppable rise of heart disease. In March 1974, Los Angeles cardiologist Weldon Walker reported a “sign of spring” in Journal of the American Medical Association (JAMA), pointing out that age-adjusted CHD mortality rates had actually been declining in the United States since 1963.4
Walker’s announcement was met with guarded enthusiasm: not everyone was certain whether the decline was real. Frequent changes in diagnostic taxonomies made it difficult to track mortality trajectories over the 20th century. To make matters worse, the National Center for Health Statistics (NCHS) had fallen several years behind in its work. When it tried to catch up in the early 1970s by releasing a bolus of several years’ data, it was Walker, and not officials at the NCHS or the National Heart Lung Institute, who first recognized the signal.5 By 1975 the biometrics unit at the National Heart Lung Institute had scrutinized its own data and was “prepared to believe that the recent decrease in CHD mortality is probably real.”6 Eager to reach consensus about the reality and causes of decline, the National Heart, Lung, and Blood Institute (NHLBI) called leading researchers to Bethesda, Maryland, in October 1978 for what became known as the “Decline Conference.”7 Participants agreed that the decline—a 20% drop between 1968 and 1978—was indeed “real.” But they were unable to answer the more difficult question: What had changed between 1960 and 1975 that might account for the decline?
Quite simply, the problem was that too many things had changed (Figure 1). The onset of decline in the 1960s had coincided with vigorous efforts to educate Americans about smoking, diet, and other CHD risk factors; with changes in medical care, including aggressive control of hypertension, coronary care units, and bypass surgery, and with the passage of Medicare and Medicaid. Despite a century of debate within infectious disease epidemiology, ambiguity persisted about how to resolve the distinction between correlation and causation. As cardiologist Jeremiah Stamler complained in 1978,
when such multiple socio-medical trends evolve over the years, it is virtually impossible to make a definitive scientific assessment as to the role of each of them singly, and all of them together in causing the decline in mortality rates.8
FIGURE 1—
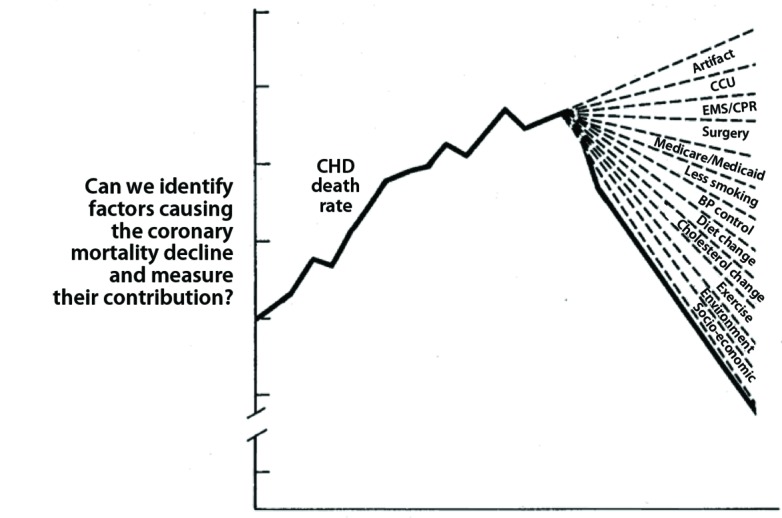
Coronary heart disease decline and the problem of attribution of credit.
Note. BP = blood pressure; CHD = coronary heart disease; CCU = coronary care unit; EMS/CPR = emergency medical service/cardiopulmonary resuscitation.
Source. Reproduced from Havlik and Feinleib.7
Skeptics cautioned that the decline might have been unrelated to any specific interventions. As a Lancet editorial warned about the decline debate,
when John Snow removed the handle from the Broad Street pump the cholera epidemic which he was attempting to abort was already on the wane.9
In the aftermath of the Decline Conference, cardiovascular epidemiologists—an emerging community of researchers with training in medicine, epidemiology, or both, stationed in academic medical centers and various government agencies—saw themselves as part of “a natural experiment of immense importance.”10 They felt an
urgent need for better information about the relative impact of each component if we are to make intelligent decisions about the allocation of scarce resources between competing programs.11
Two distinct programs emerged from this commitment: epidemiological surveillance and epidemiological modeling. Both sought to separate out the contributions of risk factor reduction and health care by determining whether decreased mortality was the result of successful prevention (e.g., reduced incidence) or treatment (e.g., reduced case fatality).
After an initial pilot program that began in 1980, the National Institutes of Health launched Atherosclerosis Research in Communities, a set of 4 cohort studies begun in 1983 that continues today.12 Researchers in North Carolina, Mississippi, Minnesota, and Maryland each enrolled 4000 patients and monitored the occurrence of CHD events (e.g., heart attacks, sudden death), performed routine clinical examinations, collected blood markers of atherosclerosis, and used vascular ultrasound to measure atherosclerosis in the carotid and lower extremity arteries. Similarly motivated by the uncertain outcomes of the Decline Conference, researchers from the World Health Organization began to plan a surveillance program in 1979. Their efforts culminated in Multinational Monitoring of Trends and Determinants in Cardiovascular Disease (MONICA). Researchers at 39 centers in 26 countries collected data from more than 100 000 patients on event rates, case–fatality rates, medical care, risk factors, and so forth.13 By collecting data on the incidence of heart attacks, both fatal and nonfatal, the researchers hoped that they would discern whether prevention had reduced the incidence of heart disease or medical care had improved the survival of patients who developed it.
To generate data with sufficient granularity, these programs needed to focus on discrete, well-circumscribed populations, something that limited the generalizability of the findings.14 They struggled to standardize data collection across their various sites. They had to take cause-of-death data at face value even though they knew that sites varied in their accuracy. And once credible data emerged, researchers often disagreed about its interpretation, especially in light of the ecological fallacy.15 Nonetheless, by the time that NHLBI convened a workshop to follow up on the Decline Conference in 1988, data from Atherosclerosis Research in Communities and MONICA allowed robust comparisons of international trends in CHD mortality. Decline of CHD in the United States had accelerated in the 1980s, falling 4% each year.16 Optimism was tempered by emerging recognition of the growing burden of CHD in developing countries, and by continuing uncertainty about how to assign credit to prevention and medical care.17 Researchers worried that their initial assumptions may have been too simplistic: health care and prevention could each influence both event and case–fatality rates, making it difficult to distinguish their relative impact.18 Decades of surveillance programs did not resolve debates about the causes of the decline. Instead, data supported the original intuition that both prevention and treatment had contributed.
The Decline Conference also motivated a second strand of cardiovascular epidemiology, one that used sophisticated models to discern the causes of CHD decline. These models were made possible not just by the improved data generated by surveillance programs and the ongoing clinical trials of risk factor reduction and medical treatments, but also by rapid improvements in computer technology that made calculation-intensive analyses accessible to clinicians and researchers.
In 1984 Lee Goldman (a cardiologist) and Francis Cook (an epidemiologist) produced an integrated quantitative assessment of preventive and therapeutic interventions. Their model recapitulated the passage of a CHD patient through the health care system, including emergency medical services, coronary care units, and surgical and medical treatment. Each domain was divided into specific interventions that could be quantified with data from observational studies and then reassembled by using simple arithmetic to calculate the number of lives saved. Similar calculations revealed the contributions of lifestyle interventions against dietary fat, cholesterol, smoking, obesity, and exercise. The authors celebrated when the interventions that they modeled—four treatment, four prevention—combined to account for 90% of the decline between 1968 and 1976, a finding they confessed “may be as serendipitous as it is accurate.”19
Simon Capewell, a Scottish cardiologist and epidemiologist, developed an elaborate version of this model in the 1990s. The IMPACT mortality model quantified the utilization and impact of a given intervention, correcting for interactions between interventions, to calculate the total number of deaths prevented by each. Capewell demonstrated his model on Scottish data and found that, of the deaths prevented between 1975 and 1994, 36% could be attributed to decreased smoking, 10% to acute coronary care, 9% to treatment of hypertension, and so forth. Taken together, “risk factor reductions and modern treatments contributed almost equally,” 40% treatment, 51% prevention.20 Collaborating with researchers in many countries, Capewell conducted similar analyses—with similar findings—on countries from Australia to Finland.
Modeling has since become a popular tool in cardiovascular epidemiology, applied both to explain past declines and to predict future possibilities. A 2006 review found 75 articles that used 42 different models to inform CHD policy.21 But models, like surveillance programs, have certain limitations. First, models must make simplifying assumptions to facilitate methodical analysis. Second, the models can be run with different endpoints, and these choices have substantial consequences for how the models allocate credit. Third, because models can only analyze factors that have been quantified and measured, they often exclude relevant variables such as stress or socioeconomic status from their analyses. Finally, because the models have generally shared credit between risk factor reduction and medical care—a finding that might be both accurate and expedient—they have not provided guidance to policymakers facing difficult choices about resource allocation.22 The analyses often end like the Caucus Race in Alice in Wonderland, in which the Dodo Bird, officiating, declared that “everybody has won, and all must have prizes.”23
Despite its overall celebratory tone, the modeling literature, like the surveillance literature, came to include a sense of regret. Even as models accounted for decline, they showed the substantial unrealized potential of both prevention and treatment. A modest increase in the utilization of evidence-based medical interventions could prevent an additional 41 000 deaths annually in Sweden.24 An additional 372 000 deaths could be prevented if Americans achieved “ideal risk-factor levels” not yet attained by 4 decades of public health education.25 Even though researchers presumably knew that such utopian lifestyles would never be achieved, they sought to inspire many readers with statements of hope: if we did more, then even more lives could be saved. But the projections could demoralize readers as evidence of unfulfilled promise: look how much better things could already be. The balance between these narratives began to tilt in the late 1980s as the rate of decline slowed and threatened to reverse.
RECOGNITION OF REVERSAL
Surveillance programs provided the first warnings. When Millicent Higgins and Thomas Thom presented data from the United States at the 1988 NHLBI workshop on international comparisons, they showed that the rate of decline had dropped from 4% in the late 1970s to 3% in the 1980s, a concerning trend accompanied by a rise in obesity.26 The situation was even worse in Finland. Finland had gained notoriety from having the highest rates of CHD mortality in the world. Health officials responded aggressively in the 1970s and implemented regional demonstration projects (e.g., the North Karelia project) and national campaigns to reduce risk factors, especially dairy fat.27 These efforts yielded steep declines in CHD mortality by the late 1970s.
But when Tuomilehto et al. presented Finnish data (national and MONICA) at the 1988 NHLBI workshop, they admitted that “this favourable trend may have levelled off during the 1980s.” Finnish officials blamed a risk factor “relapse”:
After an intensive active period the public may have lost interest. The tobacco and food industries, among others, have taken advantage of this loss of interest. Health professionals and lay people may not fully realize that prevention of mass diseases is an extremely long process. Many people and practitioners may have lost interest in anti-smoking advice, dietary counselling, and other preventive measures, especially as countermessages and competing ideas have arisen.28
Finland provided the first of many narratives about the vulnerability of success. Speaking at the workshop, Geoffrey Rose warned of two things that could go wrong. First, cardiovascular disease–control programs relied on continuing political will, and “a premature end to a preventive effort can sometimes be followed by swift loss of the ground that had been gained.” Second, even when political will remained, populations could tire of the constant exhortation. Rose blamed Finnish backsliding on the “community’s boredom with an oft-repeated message that has lost its novelty.”29 By the turn of the 21st century, ominous signs continued to accumulate. The rate of decline in the United States slowed again, from 3% to 2.7% in the 1990s. Adverse trends in risk factors dimmed prospects for continuing decline. One 2000 review suggested that “a more pessimistic view would predict an actual increase.”30 Surveillance programs in other countries picked up similar signs of the vulnerability of continuing decline. In Australia and New Zealand, for instance, decline had slowed and—possibly—even stopped and begun to reverse.31
No single narrative of risk and reversal received more attention than the alarming increase in childhood obesity. In a 2001 JAMA review, obesity researchers David Ludwig and Cara Ebbeling warned of the linked increase in obesity and type 2 diabetes in American children. This “impending crisis” distorted conventional understandings of the normal and pathological, challenged notions of epidemiological progress, and shook fundamental associations between youth and health on one hand, and aging and chronic disease on the other.32
Four years later, Ludwig teamed up with Chicago sociologist and demographer Jay Olshansky to issue an even more dire warning in the New England Journal of Medicine. Obesity, which increased the risk of death from diabetes, heart disease, and cancer, had increased by 50% since the 1960s. Their models suggested that this had already blunted the century-long rise in life expectancy. If the trend continued, life expectancy might actually start to decrease:
Forecasting life expectancy by extrapolating from the past is like forecasting the weather on the basis of its history. Looking out the window, we see a threatening storm—obesity—that will, if unchecked, have a negative effect on life expectancy.33
The forecasts about future life expectancies remain controversial. Unlike the original decline debate, in which researchers accepted the reality of CHD decline and debated its causes, here the trend itself remains contested. Some prominent demographers continue to predict a future of ever-longer life spans.34 For Olshansky and Ludwig, however, the optimism born of decades of progress against CHD needed to be reassessed: “major threats to the health and longevity of younger generations today are already visible.”35
Meanwhile, the increasing granularity of surveillance programs and the increasing power of computer analyses facilitated detailed subgroup analyses that could detect subtle developments that would otherwise have been hidden within overall trends. Capewell’s team, for instance, began to combine surveillance data and modeling techniques to detect such warning signs. By using a “joinpoint” algorithm they detected shifts in the slope of mortality trajectories in specific population subgroups. Among men aged 35 to 54 years in the United States, the annual rate of decline fell from 6.2% in the 1980s to 0.5% in the 2000s, a disquieting “sentinel event,” a warning that “hard-fought gains in mortality improvements might be arrested or even reversed.”36 The IMPACT modelers found similar warnings wherever they looked: England and Wales, Scotland, the Netherlands, and Australia all showed attenuation of decline, plateauing, and even reversal in some subgroups.37
Having identified concerning trajectories, Capewell used the IMPACT model to explore potential causes. The model showed that the potential benefit from favorable trends in some factors was increasingly offset by adverse trends in others. In the United States, for instance, the contribution to the decline from improvements in cholesterol (24%), blood pressure (20%), and smoking (12%) were attenuated by adverse changes in obesity (8%) and diabetes (10%).38 Why had this happened? Capewell’s analysis echoed that offered by Rose at the 1988 workshop: dissipation of political will and fatigue from prolonged campaigns for risk factor reduction.39 Such complacency threatened to undo decades of progress: “mortality rates among younger adults may represent the leading edge of a brewing storm.”40
Even as projections of future life expectancies remain controversial, reports about slowed and stopped decline continue to accumulate. These are descriptive claims, made visible through precise analyses. Although surveillance data have their limitations, the trajectories and inflections revealed by joinpoint analyses may be more robust than the specific mortality rates. Moreover, the ominous trends have found easy acceptance among researchers and popular media accustomed to reports of a US population increasingly afflicted with chronic disease, backsliding on the prevention and management of cardiovascular risk factors, and likely to live shorter, sicker lives than those of their parents.41
GLOBALIZING THE EPIDEMIC
Pessimistic narratives about the future course of CHD in the United States have likely been amplified by contemporaneous changes in CHD in other countries. Even as monitoring and modeling revealed the vulnerability of CHD in wealthy countries, more concerning developments rose to prominence in Russia, China, and elsewhere. The dynamics of cardiovascular epidemiology vary in these countries, and the resulting stories of resurgence or emergence have different causes and meanings. Nonetheless, each case has contributed to the growing fear of what the future of CHD might be in a world of increasing economic turbulence.
Russia offered a stark example of how quickly decades of health progress could collapse. Postwar improvements in health conditions had brought life expectancy in the Soviet Union to within 2.5 years of the standard set by the United States by the 1960s. Yet by the mid-1980s the failures of the Soviet economy, so successfully hidden from the gaze of Western powers, were evident in Soviet bodies.42 When Soviet researchers presented at the 1988 NHLBI workshop, they noted that age-adjusted mortality had increased in the 1980s, mostly attributable to CHD.43 The collapse of the Soviet Union exacerbated the problem. Between 1990 and 1994 life expectancy in post-Soviet Russia fell by five years; more than one quarter of this was attributed to an increase in mortality from CHD and stroke.44 In a striking echo of earlier explanations of decline, there was no shortage of possible causes for the new increase: social and economic instability, increased alcohol and tobacco use, worsening diet (more fat, fewer fruits and vegetables), stress and depression, and an unraveling health care system. Researchers concluded:
The lesson for the Russian health care system is the same as for the health care system of the United States or other industrialized countries: current levels of life expectancy should not be considered permanent. Life expectancy can decline and under unusual circumstances those declines can be rapid and substantial.45
As economic disruption fueled resurgent CHD in Russia, economic development brought emergent CHD to China. Chinese researchers had described low rates of CHD at the 1988 workshop in spite of high rates of smoking—a finding attributed to the extraordinary qualities of a Chinese diet traditionally low in saturated fat and cholesterol.46 But CHD mortality increased by 50% in Chinese men between 1984 and 1999. IMPACT, with data from MONICA, attributed 77% of the extra deaths to increased cholesterol, the result of “an increasingly ‘Western’ diet.”47 Mortality associated with CHD jumped another 40% by 2010.48
By the turn of the 21st century, overwhelming evidence indicated that the forces of global social change—urbanization, industrialization, migration, and economic instability—were transforming populations worldwide and threatening a dramatic expansion of CHD. As Indian cardiologist Srinath Reddy described, these changes “propelled the developing countries into the vortex of the global CVD epidemic.”49 By the 1990s, CHD had become the leading cause of death in most countries worldwide.50 Between 1980 and 2000 the prevalence of CHD in urban India increased six- to eight-fold.51 Projections of future disease and mortality suggest that the problem of CHD will only get worse.52
In an attempt to draw attention and resources to this problem, the World Heart Federation identified CHD as an “impending global pandemic” in 2000.53 Over the subsequent decade, concern not just with CHD but also with noncommunicable diseases more broadly has developed into a robust movement within global health. Inspired by successes against HIV and tuberculosis (e.g., the President’s Emergency Fund for AIDS Relief, the Global Fund), noncommunicable disease advocates called for similar efforts against heart disease and cancer. Their advocacy led to the September 2011 United Nations General Assembly devoted to the prevention and control of noncommunicable diseases.54 Despite decades of decline in the West, CHD—resurgent in the United States, Australia, or Russia, and emergent in China, India, and elsewhere—now generates rising concern. We call this widespread concern over the retreat of progress public health catastrophism.
INFECTIOUS PRECEDENTS OF PUBLIC HEALTH CATASTROPHISM
The ominous tone in the cardiovascular epidemiology at the turn of the 21st century was not the first time that a literature born of triumphalist celebration transmogrified into one of catastrophism and fear. That story had just played out in the discourse on infectious disease. The parallels between these narratives have many possible causes. They might reflect simple coincidence, they might reflect an underlying malaise, or they might have amplified one another. In at least some cases, however, the concerns about resurgent infectious disease provided a direct precedent for the concerns that soon followed about CHD.
From the heady optimism of the early antibiotic era in the 1950s to the eradication of smallpox in the 1970s, many physicians and researchers celebrated the “conquest” of infectious disease.55 The success fueled the emergence of powerful narratives that linked health conditions to economic development. According to theories of the “epidemiological transition,” societies passed through progressive stages of epidemiological development, from an age of epidemics, to an age of chronic disease, and hopefully toward a future of better health.56 Because progress involved skills (e.g., sanitation, immunization, medical care) that, once learned, would never be forgotten, the transitions should be unidirectional. There should be no turning back the epidemiological clock.
Theories of epidemiological transition immediately raised a crucial question: what determinants truly caused changing demographic patterns of disease, mortality, and fertility? The fiercest debates focused on responsibility for the decline of tuberculosis from Europe and the United States between 1850 and 1950. Many observers assumed that biomedical science had played a decisive role. Physician–demographer Thomas McKeown rejected this consensus and argued that neither medicine nor public health had contributed to the decline of tuberculosis. Instead, he credited nonspecific improvements in economic conditions and the standard of living. His critiques triggered a battle royal in the 1970s about the relative contributions of medicine, public health, and economic growth.57 Ivan Illich took this critique further and argued that medicine was worse than unhelpful: it was a “nemesis” that undermined human freedom.58
It is now clear that there were important problems with the basic assumptions of the models of epidemiological transitions, and with rise-and-fall triumphalist narratives more broadly. First, the narratives necessarily simplified the actual history. In the United States, for instance, the epidemiological transition followed a different time course for different populations (e.g., for men vs women, Blacks vs Whites, urban populations vs rural).59 Second, even though the transition models were explicitly comparative (e.g., juxtaposing the timing of transition in England, Japan, Chile, and Sri Lanka), they remained Eurocentric. They assumed that all other countries would follow the basic path set by England and the United States. Because the populations in low- and middle-income countries were so heterogeneous, the “transition” actually unfolded in complex ways. Writing from the vantage of Mexico in 1989, Julio Frenk characterized this as the problem of a mixed epidemiological transition.60 Partial economic development brought great wealth to some populations in middle-income countries, while leaving others mired in poverty. The result was the emergence of CHD and other “modern diseases” in the wealthy elites even as famine, tuberculosis, and other epidemics continued to assail the poor. Extrapolating from the past to the present and future might prove just as difficult. Changes in medical technology and in risk factor prevalence might have altered disease dynamics, making past precedents less relevant. As MONICA researchers wrote in 2000, “Trends in the prevalence of obesity and the global spread of tobacco use are reasons to expect that the past will not predict the future.”61
Even as critiques from the 1980s into the 2000s challenged the meanings of Eurocentric narratives of progress, the triumphalist assumptions of the narratives themselves began to unravel. Fears of antibiotic resistance appeared in the 1940s and 1950s, within the first decade of antibiotic use.62 They reemerged with the outbreak of multidrug-resistant tuberculosis in prisons and homeless shelters in New York City in the early 1990s.63 Soon anxieties about new “superbugs” from the exotic (e.g., Ebola, Marburg, and “flesh-eating bacteria”) to the mundane (e.g., methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus) eroded the old progressivist histories. The imprint of these fears can be seen in the string of Hollywood hits from Outbreak and 12 Monkeys (both in 1995), to 28 Days Later (2002) and Contagion (2011). These pop narratives had echoes in the scholarly literatures of sociology, anthropology, history, public health, and national security policy.64 Indeed this counterdiscourse about resurgent epidemics is now so common that one hesitates to call it a counterdiscourse at all. As Nicholas King points out, the stock characters in the narratives of emerging infectious disease had, by the closing decades of the 20th century, become part of a commonplace sensibility of fall and rise that characterizes a broad retreat from mid–20th-century modernist narratives of progress.65
The resurgences were all the more disarming because epidemiologists had not foreseen them. Writing on the eve of the millennium, researchers at the Centers for Disease Control and Prevention described their lost confidence:
Until recently, it was assumed that the epidemiologic transition had brought about a permanent reduction in infectious disease mortality in the United States. However, the emergence or reemergence in the 1980s of such diseases as the acquired immunodeficiency syndrome (AIDS) and tuberculosis demonstrated that gains against infectious diseases cannot be taken for granted.66
But once the dynamics of this resurgence had been characterized, researchers had no trouble tweaking their narratives to account for what had happened. Initial success had led to a relaxation of attention and effort that let infectious diseases regain (or secure) their foothold. And once physicians and researchers had recognized the resurgence of infectious disease, they were primed to detect resurgent disease in other domains.
LINKED NARRATIVES OF CATASTROPHISM
The parallels between the literatures on the rise, fall, and rise again of communicable and noncommunicable disease are especially evident in the cross-linked trajectories of tuberculosis and CHD.67 Both were epidemics in slow motion, building not over months but over decades. Tuberculosis rose to prominence in the mid-19th century, peaked around 1900, and then declined substantially by 1950 in Europe and the United States. Coronary heart disease followed a similar trajectory, just shifted 50 years later. Political linkages also exist. When CHD rose to prominence in the early 20th century, advocacy groups looked specifically to tuberculosis as the exemplar for how to draw attention and resources to a health problem. The new American Heart Association studied the experience of the National Tuberculosis Association as it designed its early campaigns against heart disease in the 1930s and 1940s. Similar links exist today. Olshansky and Ludwigs’s 2005 warning about obesity and life expectancy placed CHD into the broader context of the many new threats to public health, including HIV, hospital-acquired infections, and antibiotic resistance.68 Before teaming up with Ludwig, Olshansky himself had written extensively about the threat of new and reemerging infectious diseases.69
Parallels also exist in the debates that emerged about the declines of tuberculosis and CHD. Speakers at the Decline Conference in 1978 worked in the shadow of the McKeown debates. They explicitly invoked Illich as a warning to those who would take the value of medicine for granted. One speaker warned:
Lest the physician become preoccupied with the importance of his or her efforts in altering the course of [CHD], it should be appreciated that there are some who will credit neither surgeons nor cardiologists with changes in the course of the disease.70
While each of the decline debates focused on medicine versus public health, critics worked to broaden the discussion. McKeown focused on socioeconomic conditions in his account of the decline of tuberculosis. Such factors remain on the sidelines of the CHD debates because neither the surveillance programs nor the epidemiological models generated the data that would have been needed for these factors to become serious players in the debates. Lost in each debate was recognition of how much the category of public health has changed. For both tuberculosis and CHD, previous commitments to broad, community-based intervention have increasingly given way to prevention through regimes of medical surveillance and pharmaceutical control.71
MANAGING EXPECTATIONS OF TRIUMPH AND TRAGEDY
The linked debates about the decline of infectious and noninfectious disease and the parallel fears of resurgence demonstrate the importance of setting narratives of expectation for how researchers and societies respond to public health data. Since the 1990s, scholars in science studies have studied the sociology of expectations, showing how scientists’ claims and speculations about the promise of science help them to attract funding and recruit allies and these, in turn, shape future science and policy.72 This is best demonstrated in genetics, the archetypal “promissory science” of the new millennium: promises about how genetics will revolutionize medicine, more than actual contributions of genetics to clinical practice, have motivated the substantial social and scientific commitment to the science.73
It is easy to see how expectations have had a substantial impact on the linked discourses of decline and resurgence. Even though the impacts of AIDS and CHD have been profound, each killing tens of millions of people, many of the hyped threats are startlingly subtle. The much-discussed epidemic of tuberculosis in New York City in the 1990s involved a few thousand cases, some of which were multidrug-resistant. This is a far cry from the millions killed by tuberculosis during its heyday in the United States (or the millions who die each year worldwide). The concern over the slowed or plateaued decline of CHD mortality rates remains a blip in an overall trajectory of dramatic and continuing decline in CHD, whether in Finland or the United States. The subtle signals were only detected because of the substantial efforts in surveillance and modeling that had been created, ironically, to characterize the success story of CHD decline. How is it that subtle signals come to take on such great significance in the public health discourse?
First, the models—whether of epidemiological transitions or CHD trajectories—project trends into the future. This is often a suspect science, in which slight changes in assumptions lead to substantial differences in projected futures. But the models still have great narrative power. A small signal, amplified over time, can become a substantial threat. This poses a real challenge for policymakers. Should they respond to the magnitude of the problem now experienced, or should they trust the models and plan prophylactically to manage a future that might come into being? There are no easy answers.
Second, the resurgence of both infectious and noninfectious disease scored a double-hit against modernist assumptions. By the 1970s the narratives of progressive conquest of disease had saturated commonsense understandings and informed an ontology that linked disease, medicine, public health, and economic and political development. Everyone expected that this conquest would continue. However, by the 1990s, excitement over post–Cold War globalization had given way to new kinds of catastrophism, of economic neocolonialism, of erosion of traditional cultures and values, and of emerging threats to public health. Shattered expectations have had a profound impact. When a population has settled into an expectation of continued, inevitable mortality decline, then even the subtlest deviation from the narrative becomes concerning.
Third, the offended expectations take on broader significance because they become linked to questions of identity and national pride. Health officials in the United States, which rarely leads the world in any health indicator, have long celebrated the status of the United States as the country that has led the decline in CHD. Early signals of reversal threaten this status: the United States might become the poster child not of the conquest of CHD but of its resurgence.
Finally, expectations and their management shape the political imagination of possible responses. Many within the infectious disease community have mobilized the discourse of “emerging infectious diseases” and bioterrorism into an activist response: we had defeated infectious diseases once before, and we can do it again—as long as we provide researchers, physicians, and first responders with suitable resources.74 This move transforms a warning into a call for action, even an opportunity.
Something similar happens with CHD. Researchers invoke catastrophist narratives, issue dire warnings, and demand greater resources for both prevention and treatment. The concern about prevention fatigue demonstrates this as well. Advocates warn that we have the power to control CHD, we just need the individual motivation and the political will to implement the needed reforms. That fact that we had made so much progress in the past affirms what we could do in the future. The recollection of past triumph functions as an inspiration for future action that salves the injury caused by the reversals. The question is whether CHD and other NCDs will motivate the powerful societal responses engendered by smallpox, tuberculosis, and other pathogens. Efforts at risk factor reduction will likely collide with the interests of the multinational corporations that produce and market tobacco and food. If this happens, then differences in the willingness and ability of governments to implement effective public health and medical programs will exacerbate existing health inequalities.75
Public health narratives link data to action because they focus attention on particular problems. What does the future of CHD hold? The answer depends on how the narratives are framed and the extent to which catastrophist visions take root. If scholars focus on the overall experience of populations in developed countries, then the long-term trajectories are still ones of conquest over infections and CHD: mortality from both sets of diseases is dramatically lower now than in the past. If they focus on select populations within those countries, then signs of reversal rise to prominence, foretelling a possible future of increasing mortality rates. If they focus on developing countries, then they find epidemics of infectious diseases and CHD in full swing. All three narratives are relevant for public health policy. It is essential for policymakers to understand the stakes and interests behind them before they formulate their responses. Policymakers must recognize that the public health narratives we produce, whether progressive or catastrophist, are highly dependent upon subject position and envisioned audience. An ongoing and critical task for the social sciences of health will be to attend to which of these narratives wins out in the struggle to set global health priorities in the near future.
Acknowledgments
The authors acknowledge valuable feedback on previous drafts of this work from Henry Blackburn, Simon Capewell, Lee Goldman, Zubair Kabir, Gerry Oppenheimer, Sejal Patel, Sarah Tracy, and three anonymous reviewers.
Endnotes
- 1.D. S. Jones and J. A. Greene, “The Contributions of Prevention and Treatment to the Decline in Cardiovascular Mortality: Lessons From a Forty-Year Debate,” Health Affairs (Millwood) 31, no. 10 (2012): 2250–2258. [DOI] [PubMed] [Google Scholar]
- 2.D. Brown, “Life Expectancy in the US Varies Widely by Region, in Some Places is Decreasing,” Washington Post, June 15, 2011, http://www.washingtonpost.com/national/life-expectancy-in-the-us-va…on-and-in-some-places-is-decreasing/2011/06/13/AGdHuZVH_story.html (accessed June 18, 2012); Sabrina Tavernise, “Life Expectancy Shrinks for Less-Educated Whites in U.S.,” New York Times, September 20, 2012, http://www.nytimes.com/2012/09/21/us/life-expectancy-for-less-educated-whites-in-us-is-shrinking.html?hp&pagewanted=print (accessed September 20, 2012). [Google Scholar]
- 3.N. O. Borhani and H. H. Hechter, “Recent Changes in Cardiovascular Disease Mortality in California,” Public Health Reports 79 (1964): 147–160. [PMC free article] [PubMed] [Google Scholar]
- 4.R. H. Moser, “Signs of Spring?” JAMA 227, no. 9 (1974): 1049; W. J. Walker, “Coronary Mortality: What Is Going On?” JAMA 227, no. 9 (1974): 1045–1046. Walker, a member of JAMA’s editorial board, had published widely in cardiology since the 1950s, but this was his first foray into cardiovascular epidemiology. He followed up with a scathing indictment of Congress. He harangued Congress for subsidizing the tobacco industry even as it spent billions of dollars caring for tobacco’s victims. Even though Congress knew the exact size of the tobacco subsidy, it underfunded the National Center for Health Statistics and had no up-to-date estimates of tobacco-related mortality. See W. J. Walker, “Government Subsidized Death and Disability, Journal of the American Medical Association 230, no. 11 (1974): 1529–1530. [PubMed] [Google Scholar]
- 5.P. Leaverton, “Oral History,” interview by Henry Blackburn, February 21, 2002, http://www.epi.umn.edu/cvdepi/interview.asp?id=43 (accessed November 28, 2011). [Google Scholar]
- 6.Tavia Gordon and Thomas Thom, “The Recent Decrease in CHD Mortality,” Preventive Medicine 4, no. 2 (1975): 115–125, on p. 120. [DOI] [PubMed] [Google Scholar]
- 7.R. J. Havlik and M. Feinleib, eds. Proceedings of the Conference on the Decline in Coronary Heart Disease Mortality (Bethesda, MD: Department of Health, Education, and Welfare, 1979). [Google Scholar]
- 8.Jeremiah Stamler, “Lifestyles, Major Risk Factors, Proof and Public Policy,” Circulation. 58, no. 1 (1978): 3–19, on p. 15. [DOI] [PubMed] [Google Scholar]
- 9.Why the American Decline in Coronary Heart-Disease?” Lancet 315, no. 8161 (1980): 183–184, on p. 183. [DOI] [PubMed] [Google Scholar]
- 10.R. J. Havlik, “Understanding the Decline in Coronary Heart Disease Mortality,” JAMA 247, no. 11 (1982): 1605–1606, on p. 1606. [PubMed] [Google Scholar]
- 11.Michael P. Stern, “The Recent Decline in Ischemic Heart Disease Mortality,” Annals of Internal Medicine 91, no. 4 (1979): 630–640, on p. 639. [DOI] [PubMed] [Google Scholar]
- 12.H. Blackburn, “‘The Decline.’ Surveillance and Trends of Coronary Death,” (unpublished data, 2012); Leaverton, “Oral History”; ARIC Investigators, “The Atherosclerosis Risk in Communities (ARIC) Study: Design and Objectives” American Journal of Epidemiology 129, no. 4 (1989): 687–702. Independent groups undertook similar surveillance programs in Minneapolis and Rochester, MN, and Worcester, MA. [Google Scholar]
- 13.Blackburn, “The Decline”; S. Bothig, “WHO Monica Project: Objectives and Design,” International Journal of Epidemiology 18, suppl 1 (1989): S29–S37; J. Tuomilehto and K. Kuulasmaa, “WHO MONICA Project: Assessing CHD Mortality and Morbidity,” International Journal of Epidemiology 18, suppl 1 (1989): S38–S45. [PubMed] [Google Scholar]
- 14.Blackburn, “The Decline.” [Google Scholar]
- 15.W. Harlan, “CHD Trends in the United States: Overview” International Journal of Epidemiology 18, no. 3, suppl 1 (1989): S56–S57. [PubMed] [Google Scholar]
- 16.Millicent Higgins and Thomas Thom, “Trends in CHD in the United States,” International Journal of Epidemiology 18, suppl 1 (1989): S58–S66. [PubMed] [Google Scholar]
- 17.Millicent W. Higgins and Russel V. Luepker, “Preface,” International Journal of Epidemiology 18, suppl 1 (1989): S1–S2; Wayne D. Rosamond et al. for the ARIC Investigators, “Coronary Heart Disease Trends in Four United States Communities: The Atherosclerosis Risk in Communities (ARIC) Study, 1987–1996,” International Journal of Epidemiology 30 (2001): S17–S22, esp. S21; H. Tunstall-Pedoe et al., “Contribution of Trends in Survival and Coronary-Event Rates to Changes in Coronary Heart Disease Mortality: 10-Year Results from 37 WHO Monica Project Populations: Monitoring Trends and Determinants in Cardiovascular Disease,” Lancet 353, no. 9164 (1999): 1547–1557. [DOI] [PubMed] [Google Scholar]
- 18.Tuomilehto, “WHO MONICA Project”; Tunstall-Pedoe et al., “Contribution of Trends.” [Google Scholar]
- 19.Lee Goldman and E. Francis Cook, “The Decline in Ischemic Heart Disease Mortality Rates: An Analysis of the Comparative Effects of Medical Interventions and Changes in Lifestyle,” Annals of Internal Medicine 101, no. 6 (1984): 825–836, on p. 832. [DOI] [PubMed] [Google Scholar]
- 20.Simon Capewell, C. E. Morrison, and J. J. McMurray, “Contribution of Modern Cardiovascular Treatment and Risk Factor Changes to the Decline in Coronary Heart Disease Mortality in Scotland Between 1975 and 1994,” Heart 81, no. 4 (1999): 380–386, on p. 385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.B. Unal, S. Capewell, and J. A. Critchley, “Coronary Heart Disease Policy Models: A Systematic Review” BioMed Central Public Health. 2006;6:213 [10 pages]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones and Greene, “The Contributions of Prevention and Treatment.” [Google Scholar]
- 23.Lewis Carroll, Alice’s Adventures in Wonderland (1865; reprint, New York, NY: Macmillan, 1920), p. 34. [Google Scholar]
- 24.L. Björck et al., “Increasing Evidence-Based Treatments to Reduce Coronary Heart Disease Mortality in Sweden: Quantifying the Potential Gains,” Journal of Internal Medicine 269, no. 4 (2011): 452–467. [DOI] [PubMed] [Google Scholar]
- 25.E. S. Ford and S. Capewell, “Proportion of the Decline in Cardiovascular Mortality Disease Due to Prevention Versus Treatment: Public Health Versus Clinical Care,” Annual Review of Public Health 32 (2011): 5–22. [DOI] [PubMed] [Google Scholar]
- 26.Higgins and Thom, “Trends”; Blackburn, “The Decline.” [Google Scholar]
- 27.J. T. Salonen, P. Puska, and H. Mustaniemi, “Changes in Morbidity and Mortality During Comprehensive Community Programme to Control Cardiovascular Diseases During 1972–7 in North Karelia,” British Medical Journal 2, no. 6199 (1979): 1178–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.J. Tuomilehto et al., “Trends and Determinants of Ischaemic Heart Disease Mortality in Finland: With Special Reference to a Possible Levelling Off in the Early 1980s,” International Journal of Epidemiology 18, suppl 1 (1989): S109–S117, on pp. 109, 114. [PubMed] [Google Scholar]
- 29.Geoffrey Rose, “Causes of the Trends and Variations in CHD Mortality in Different Countries,” International Journal of Epidemiology 18, suppl 1 (1989): S174–S179, on p. 176. [PubMed] [Google Scholar]
- 30.R. Cooper et al., “Trends and Disparities in Coronary Heart Disease, Stroke, and Other Cardiovascular Diseases in the United States: Findings of the National Conference on Cardiovascular Disease Prevention,” Circulation 102 (2000): 3137–3147, on p. 3145. [DOI] [PubMed] [Google Scholar]
- 31.A. Wilson and V. Siskind, “Coronary Heart Disease Mortality in Australia: Is Mortality Starting to Increase Among Young Men?” International Journal of Epidemiology 24, no. 4 (1995): 678–684; M. Tobias and P. Searle, “Does Geography Explain Ethnic Inequalities in Health in New Zealand? Australia and New Zealand Journal of Public Health 30, no. 5 (2006): 457–460. [Google Scholar]
- 32.David S. Ludwig and Cara B. Ebbeling, “Type 2 Diabetes Mellitus in Children: Primary Care and Public Health Considerations,” JAMA 286, no. 12 (2001): 1427–1430, on p. 1429. [DOI] [PubMed] [Google Scholar]
- 33.S. J. Olshansky et al., “A Potential Decline in Life Expectancy in the United States in the 21st Century,” New England Journal of Medicine 352, no. 11 (2005): 1138–1145, on p. 1139. [DOI] [PubMed] [Google Scholar]
- 34.Karen Wright, “Staying Alive,” Discover, November 6, 2003, http://discovermagazine.com/2003/nov/cover/article_print (accessed May 29, 2012); James W. Vaupel, “Biodemography of Human Ageing,” Nature 464, no. 7288 (2010): 536–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Olshansky et al., “A Potential Decline,” 1143. [Google Scholar]
- 36.E. S. Ford and S. Capewell, “Coronary Heart Disease Mortality Among Young Adults in the US From 1980 Through 2002: Concealed Leveling of Mortality Rates,” Journal of the American College of Cardiology 50, no. 22 (2007): 2128–2132, on pp. 2128, 2131. [DOI] [PubMed] [Google Scholar]
- 37.M. O’Flaherty et al., “Coronary Heart Disease Trends in England and Wales From 1984 to 2004: Concealed Levelling of Mortality Rates Among Young Adults,” Heart 94, no. 2 (2008): 178–181; M. O’Flaherty et al., “Coronary Heart Disease Mortality Among Young Adults in Scotland in Relation to Social Inequalities: Time Trend Study,” British Medical Journal 339 (2009): b2613; I. Vaartjes et al., “Coronary Heart Disease Mortality Trends in the Netherlands 1972–2007,” Heart 97, no. 7 (2011): 569–573; M. O’Flaherty et al., “The Decline in Coronary Heart Disease Mortality Is Slowing in Young Adults (Australia 1976–2006): A Time Trend Analysis, International Journal of Cardiology 158, no. 2 (2012): 193–198. It is possible that subgroup analyses functioned as fishing expeditions: researchers kept looking at subgroups until they found ones with the “right” signal. The fact that different studies generally identified the same concerning signal—worsening trends in the youngest group—suggests that maybe the signal is real, and one that foreshadows what will happen as those subgroups age. However, because the young adult subgroups have so few CHD deaths, they are the ones most susceptible to spurious variations that arise from small sample sizes. Time will tell. [Google Scholar]
- 38.E. S. Ford, et al., “Explaining the Decrease in U.S. Deaths from Coronary Disease, 1980-2000, New England Journal of Medicine 356, no. 23 (2007): 2388–2398. [DOI] [PubMed] [Google Scholar]
- 39.S. Capewell and M. O’Flaherty, “What Explains Declining Coronary Mortality? Lessons and Warnings,” Heart 94, no. 9 (2008): 1105–1108. [DOI] [PubMed] [Google Scholar]
- 40.Ford and Capewell, “Coronary Heart Disease Mortality,” 2131. [Google Scholar]
- 41.“US Adults Are Getting Sicker,” FoxNews.com, July 31, 2012, http://www.foxnews.com/health/2012/07/31/us-adults-are-getting-sicker (accessed October 7, 2012); Tavernise, “Life Spans Shrink.” [Google Scholar]
- 42.V. Shkolnikov, F. Mesle, and J. Vallin, “Health Crisis in Russia. I. Recent Trends in Life Expectancy and Causes of Death from 1970 to 1993,” Population: English Selection 8 (1996): 123–154. See also John Lewis Gaddis, We Now Know: Rethinking Cold War History (Oxford, UK: Oxford University Press, 1997). [PubMed] [Google Scholar]
- 43.A. D. Deev and R. G. Oganov, “Trends and Determinants of Cardiovascular Mortality in the Soviet Union,” International Journal of Epidemiology 18, suppl 1 (1989): S137–S144. [PubMed] [Google Scholar]
- 44.Shkolnikov et al., “Health Crisis in Russia”; V. Shkolnikov, F. Mesle, and J. Vallin, “Health Crisis in Russia. II. Changes in Causes of Death: A Comparison with France and England and Wales (1970 to 1993),” Population: English Selection 8 (1996): 155–189; F. C. Notzon et al., “Causes of Declining Life Expectancy in Russia,” JAMA 279, no. 10 (1998): 793–800; David A. Leon and Vladimir M. Shkolnikov, “Social Stress and the Russian Mortality Crisis,” JAMA 279, no. 10 (1998): 790–791. See also Mark G. Field, David M. Kotz, and Gene Bukhman, “Neoliberal Economic Policy, ‘State Desertion,’ and the Russian Health Crisis” in Dying for Growth: Global Inequality and a the Health of the Poor, ed. Jim Yong Kim et al. (ME Monroe: Common Courage Press, 2000), pp. 155–173. [Google Scholar]
- 45.Notzon et al., “Causes,” 799. [Google Scholar]
- 46.S. C. Tao et al., “CHD and Its Risk Factors in the People’s Republic of China,” International Journal of Epidemiology, 18, suppl 1 (1989): S159–S163. [PubMed] [Google Scholar]
- 47.J. Critchley et al., “Explaining the Increase in Coronary Heart Disease Mortality in Beijing between 1984 and 1999,” Circulation 110, no. 10 (2004): 1236–1244, on p. 1236. [DOI] [PubMed] [Google Scholar]
- 48.J. Cheng et al., “The Impact of Demographic and Risk Factor Changes on Coronary Heart Disease Deaths in Beijing, 1999–2010,” BioMed Central Public Health 9 (2009): 30 [11 pages]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.K. Srinath Reddy, “Foreword,” in Race Against Time: The Challenge of Cardiovascular Disease in Developing Countries, eds. Stephen Leeder, Susan Raymond, and Henry Greenberg (New York, NY: Trustees of Columbia University, 2004), on p. vi. [Google Scholar]
- 50.World Bank. Investing in Health: World Development Report 1993 (New York, NY: Oxford University Press, 1993), on p. 225. [Google Scholar]
- 51.K. Srinath Reddy, “Cardiovascular Disease in Non-Western Countries,” New England Journal of Medicine 350, no. 24 (2004): 2438–2440. [DOI] [PubMed] [Google Scholar]
- 52.Colin D. Mathers and Dejan Loncar, “Projections of Global Mortality and Burden of Disease from 2002 to 2030,” PLoS Medicine 3, no. 11 (2006): 2011–2030, especially table 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.A. Chockalingam et al. “The World Heart Federation’s White Book: Impending Global Pandemic of Cardiovascular Diseases: Challenges and Opportunities for the Prevention and Control of Cardiovascular Diseases in Developing Countries and Economies in Transition,” Canadian Journal of Cardiology 16, no. 2 (2000): 227–229, on p. 227. [PubMed] [Google Scholar]
- 54.R. Beaglehole et al., for The Lancet NCD Action Group and the NCD Alliance, “Priority Actions for the Non-communicable Disease Crisis,” Lancet 377, no. 9775 (2011): 1438–1447; General Assembly of the United Nations, “Political Declaration of the High-Level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases,” Draft Resolution (September 16, 2011), http://www.un.org/en/ga/ncdmeeting2011 (accessed October 30, 2011). The concern about possible futures has been amplified by fear that little will be done. Consider, for instance, the debates and modest proposals that emerged from assembly: Sheri Fink and Rebecca Rabinowitz, “The UN’s Fight Against NCDs: How Politics, Commerce, and Science Complicated the Fight Against an ‘Invisible Epidemic,’” Foreign Affairs (2011), http://www.foreignaffairs.com/articles/68280/sheri-fink-and-rebecca-rabinowitz/the-uns-battle-with-ncds?page=show (accessed November 9, 2011). [DOI] [PubMed] [Google Scholar]
- 55.H. Dowling, Fighting Infection: Conquests of the Twentieth Century (Cambridge, MA: Harvard University Press, 1977). [Google Scholar]
- 56.Abdel R. Omran, “The Epidemiologic Transition: A Theory of the Epidemiology of Population Change,” Milbank Memorial Fund Quarterly 49, no. 4 (1971): 509–538; George Weisz and Jesse Olszynjo-Gryn, “The Theory of Epidemiologic Transition: The Origins of a Citation Classic,” Journal of the History of Medicine and Allied Sciences 65, no. 3 (2010): 287–326. [Google Scholar]
- 57.Thomas McKeown. The Role of Medicine: Dream, Mirage, or Nemesis? (London: Nuffield Provincial Hospitals Trust, 1976); James Colgrove, “The McKeown Thesis: A Historical Controversy and Its Enduring Influence,” American Journal of Public Health 92, no. 5 (2002): 725–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ivan Illich, Medical Nemesis: The Expropriation of Health (New York, NY: Pantheon Books, 1976). [Google Scholar]
- 59.Variations in epidemiological trends within the United States, both overall and specific to cardiovascular disease, have long been recognized. For examples, see: Abdel R. Omran, “Epidemiologic Transition in the United States: The Health Factor in Population Change,” Population Bulletin 32, no. 2 (1977): 1–42; S. Wing et al., “Geographic Variation in the Onset of Decline of Ischemic Heart Disease Mortality in the United States,” American Journal of Public Health 76, no. 12 (1986): 404–408; Cooper et al., “Trends and Disparities,” 3139–3140; S. Jay Olshansky et al., “Differences In Life Expectancy Due to Race And Educational Differences Are Widening, and Many May Not Catch Up,” Health Affairs (Millwood) 31, no. 8 (2012): 1803–1813. [Google Scholar]
- 60.J. Frenk et al., “Health Transition in Middle-Income Countries: New Challenges for Health Care,” Health Policy Plan 4, no. 1 (1989): 29–39. [Google Scholar]
- 61.Kari Kuulasmaa et al., for the WHO MONICA Project, “Estimation of Contribution of Changes in Classic Risk Factors to Trends in Coronary-Event Rates Across the WHO MONICA Project Populations,” Lancet 355, no. 9205 (2000): 675–687, on p. 685. [DOI] [PubMed] [Google Scholar]
- 62.R. Bud, Penicillin: Triumph and Tragedy (Oxford, UK: Oxford University Press, 2007); Scott Podolsky, “Pharmacological Restraint: Antibiotic Prescribing and Physician Autonomy,” in Prescribed: Writing, Filling, Using, and Abusing Prescriptions in Modern America, ed. J. Greene and E. Watkins, (Baltimore, MD: Johns Hopkins University Press, 2012): 46–65. [Google Scholar]
- 63.Thomas R. Frieden et al., “Tuberculosis in New York City—Turning the Tide,” New England Journal of Medicine 333, no. 4 (1995): 229–233. [DOI] [PubMed] [Google Scholar]
- 64.Popular works speculating on imminent infectious dystopias became omnipresent in the 1990s and continue to abound. See Richard Preston, The Hot Zone (New York, NY: Anchor Books, 1994); Laurie Garrett, The Coming Plague: Newly Emerging Diseases in a World Out of Balance (New York, NY: Penguin, 1995). On the historical longevity of infectious anxieties see Allan M. Brandt, No Magic Bullet: A Social History of Venereal Diseases in the United States Since 1980 (Oxford, UK: Oxford University Press, 1985); Howard Markel, When Germs Travel: Six Major Epidemics That Have Invaded America and the Fears They Have Unleashed (New York, NY: Vintage, 2005). For a sociology of biopreparedness narratives, see Andrew Lakoff, “The Generic Biothreat, or, How We Became Unprepared,” Cultural Anthropology 23 (2008): 399–428. [Google Scholar]
- 65.N. B. King “The Scale Politics of Emerging Diseases,” Osiris 19 (2004): 62–76. [DOI] [PubMed] [Google Scholar]
- 66.G. L. Armstrong, L. A. Conn, and R.W. Pinner, “Trends in Infectious Disease Mortality in the United States During the 20th Century,” JAMA 281, no. 1 (1999): 61–66, on p. 61. [DOI] [PubMed] [Google Scholar]
- 67.G. Bukhman and A. Kidder, “Cardiovascular Disease and Global Health Equity: Lessons from Tuberculosis Control Then and Now,” American Journal of Public Health 98, no. 1 (2008): 44–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Olshansky et al., “A Potential Decline.” [Google Scholar]
- 69.S. J. Olshansky et al., “Infectious Diseases—New and Ancient Threats to World Health,” Population Bulletin 52, no. 2 (1997): 1–52. He explained: “As health officials and scientists from various disciplines examined the forces responsible for these unexpected developments, they realized that the hope that IPDs [infectious and parasitic diseases] would soon be conquered was premature” (on p. 3). [PubMed] [Google Scholar]
- 70.Havlik and Feinleib, Proceedings of the Conference, p. 163. [Google Scholar]
- 71.Jones and Greene, “The Contributions of Prevention and Treatment.” [Google Scholar]
- 72.Adam Hedgecoe and Paul Martin, “The Drugs Don’t Work: Expectations and the Shaping of Pharmacogenetics,” Social Studies of Science 33, no. 3 (2003): 327–364; Richard Tutton, “Promising Pessimism: Reading the Futures to Be Avoided in Biotech, Social Studies of Science 41, no. 3 (2011): 411–429. [DOI] [PubMed] [Google Scholar]
- 73.M. Fortun, “Mediated Speculations in the Genomics Futures Markets,” New Genetics and Society 20 (2001): 139–156; Charis Thompson, Making Parents: The Ontological Choreography of Reproductive Technologies (Cambridge, MA: MIT Press, 2005); Kaushik Sunder Rajan, Biocapital: The Constitution of Post-Genomic Life (Durham, NC: Duke University Press, 2006); M. Fortun, Promising Genomics: Iceland and deCODE Genetics in a World of Speculation (Berkeley, CA: University of California Press, 2008); David S. Jones, “The Prospects of Personalized Medicine,” in Genetic Explanation: Sense and Nonsense, ed. Sheldon Krimsky (Cambridge, MA: Harvard University Press, 2013). [Google Scholar]
- 74.King, “Scale Politics”; Lakoff, “The Generic Biothreat.” [Google Scholar]
- 75.For industry as a potential obstacle, see Anna B. Gilmore, Emily Savell, and Jeff Collin, “Public Health, Corporations, and the New Responsibility Deal: Promoting Partnerships with Vectors of Disease,” Journal of Public Health (Oxford) 33, no. 1 (2011): 2–4; Kelly D. Brownell, “Thinking Forward: The Quicksand of Appeasing the Food Industry,” PLoS Medicine 9, no. 7 (2012): e1001254; Simon Capewell, e-mail to authors, October 15, 2012.∣ [DOI] [PubMed] [Google Scholar]


