Abstract
Background
Clinically significant depression is present in 25 % of individuals with type 2 diabetes, its risk being doubled in women.
Purpose
To examine the effectiveness of the Study of Women's Emotions and Evaluation of a Psychoeducational (SWEEP), a group therapy for depression treatment based on cognitive behavioral therapy principles that was developed for women with type 2 diabetes was conducted.
Methods
Women with significantly elevated depression symptoms (Center for Epidemiologic Studies Depression Scale ≥16) were randomized to SWEEP (n=38) or usual care (UC, n=36).
Results
Multilevel modeling indicated that SWEEP was more effective than UC in reducing depression (mean difference of –15 vs. –7, p<.01), decreasing trait anxiety (mean difference of –15 vs. –5, p<.01), and improving anger expression (mean difference of –12 vs. –5, p<.05). Although SWEEP and UC had improvements in fasting glucose (mean difference of –24 vs. –1 mg/dl) and HbA1c (mean difference of –0.4 vs. –0.1 %), there were no statistically significant differences between groups.
Conclusions
SWEEP was more effective than UC for treating depressed women with type 2 diabetes. Addition of group therapy for depression meaningfully expands the armamentarium of evidence-based treatment options for women with diabetes.
Keywords: Diabetes, Depression, Women
Introduction
Depression is present in 25 % of persons with type 2 diabetes and occurs twice as often in women than men with diabetes. Cost for treatment of depressed persons with diabetes is almost four times higher ($247 million) than treatment for nondepressed persons with diabetes ($55 million) [1, 2]. Although treatment of depression in persons with diabetes by antidepressants has been successful [3–5], they may disrupt glycemic control [6, 7]. Problems such as glucose intolerance and diabetes have been reported with some antidepressants [8–10] as well as weight gain [11–13]. Data from the Diabetes Prevention Program demonstrated that continuous antidepressant use was associated with increased diabetes risk in the placebo arm (2.60, CI=1.37–4.94) and in the intensive lifestyle arm (3.39, CI=1.61–7.13) [14]. In mild or moderate depressive symptoms, evidence suggests that the benefit of antidepressant medication may be minimal or nonexistent [15, 16]. Thus, the need for nonpharmocological treatment for depression, such as cognitive behavioral therapy (CBT), becomes increasingly important for persons with diabetes.
CBT is recognized as an effective treatment for depression [17] with lower relapse rates than antidepressant medications [18, 19]. An important study by Lustman and colleagues [20] examined individual CBT (administered by licensed therapists) for treatment of depression in 51 persons with type 2 diabetes. One group (n=25) received CBT for 10 weeks, and the other group received usual care (n=26). Both groups received diabetes education during the treatment phase. Depression remission was 85 % for the CBT group compared to 27.3 % for the controls (p<.0001). In addition, at 6 months follow-up, the CBT group had significantly lower HbA1c compared to the controls (p=.03), indicating a delayed benefit of CBT on glycemic control. These findings are particularly important because depression and depressive symptoms have been found to negatively impact glycemic control and have been attributed to poor self care, particularly for women [21–24].
Following the study of Lustman et al., several other studies have explored whether depression treatment improves metabolic control. However, without the inclusion of diabetes education with depression treatment, one large randomized trial of collaborative care for diabetes and depression (n=329) reported greater improvement in depression outcomes for the treatment group as compared to usual care, but no differences in HbA1c were observed [25]. Recently, Gonzalez et al. [26] reported improvements in depression, HbA1c, and self-care behaviors using a collaborative team approach (psychologist, nurse educator, and dietician). Patients received individual CBT for 10–12 sessions, which focused both on diabetes treatment adherence and depression. A more recent systematic review has suggested that targeted health behaviors combined with depression treatment may be needed to maximize outcomes in persons with diabetes [27].
Anxiety and anger are prevalent in persons with diabetes [28–34]. Women have reported that in addition to depression, anxiety and anger impact their self-care and, more importantly, their relationships with their family members and health-care providers [21, 35]. It has also been reported that women have greater reliance on social support to discuss their anger experiences [36]. Good communication with the health-care provider is critical for persons with diabetes. Swenson et al. [37] reported that patients with diabetes who have depressive symptoms are more likely to have poorer communication with their health-care provider. Patient recognition of depression symptoms is important for better management of their health [38]. Recognition, communication, and treatment of depressive symptoms are particularly important in diabetes care. Gonzalez et al. [39] reported that continuous depressive symptoms, even low levels, are better predictors of nonadherence to diet, exercise, and medications than major depression.
Depression significantly impacts the quality of life of persons with diabetes [40–42]. Negative moods are associated with poorer quality of life in persons who have diabetes [43, 44]. Studies have also reported that health improvements can occur with effective CBT programs for depression and stress in persons with diabetes [20, 45]. In addition, other studies are using a CBT approach to treat mild and major depression in persons with diabetes [46, 47].
Currently, although there are programs targeting depression and depressive symptoms, there are no programs that target recognition and treatment of depression combined with treatment of other moods (anxiety and anger) for persons with diabetes. The Study of Women's Emotions and Evaluation of a Psychoeducational (SWEEP) Program (study intervention) was a group CBT program delivered by a nurse for the recognition and management of depression and other moods (anxiety and anger) in women with type 2 diabetes. The primary aim of the study was to examine the effects of the SWEEP program on depression, anxiety, and anger among women with type 2 diabetes. The secondary aim was to examine the effects of the SWEEP program on glycemic control and health-related quality of life.
Methods
Participant Recruitment
To participate in the study, the inclusion criteria were women: (1) aged 18 and older, (2) having type 2 diabetes >6 months and being medically managed, and 3) having an average score of ≥16 on the Center for Epidemiologic Studies Depression Scale from two screenings (phone and baseline) within 4 weeks of each other. The exclusion criteria were the following: (1) current alcohol or substance abuse disorders, a history of bipolar depression, or any other psychotic disorder; (2) a diabetes knowledge score <70 % on the Brief Diabetes Knowledge Test (since the program emphasis was not diabetes education); and (3) severe complications of diabetes (blindness, renal failure, or amputation). The study took place in a major midwestern medical center in the USA where there are over 800 outpatient visits per month for the treatment of diabetes. The IRB approved study included a recruitment flyer that briefly identified depression symptoms in women with type 2 diabetes and a nurse contact if there was interest regarding the study. The flyers were distributed at the diabetes center and the primary care clinics. In order to increase minority recruitment, a large ministry group within the immediate area was also informed. Potential participants phoned the nurse, the study was described, and then they were screened for inclusion and exclusion criteria. For participants who were depressed and not eligible, a list of counseling centers was provided. If women were not successful on the diabetes knowledge test, they were mailed a basic diabetes information book, called for retesting, and enrolled if they were still eligible.
Design
A randomized, repeated measures, experimental design was used. Women were randomized to either usual care (control group) or the SWEEP program (intervention group). Data were collected on all women at baseline, 12 weeks (i.e., 3 months), and 24 weeks (i.e., 6 months) follow-up. Phone contact was made for all participants at 10 and 22 weeks to schedule follow-up visits. All contact points were used to monitor for potential adverse events. Following randomization, women in the SWEEP program attended eight weekly sessions and two booster sessions (weeks 14 and 22) to reinforce the content learned in class.
Procedures
Enrollment
There was a two step process for enrollment, which included a phone screen and a baseline assessment. Women were phone screened for participation (see recruitment). Once there were 20–24 women (cohort) who met the study criteria, they were invited for a baseline screening. These two screenings occurred within 4 weeks of each other. Subjects came to the School of Nursing Research Laboratory after fasting for 10 h and were told to bring their medications with them. They were informed that the testing would take 1.5–2 h. Upon arrival at the study site, consent was obtained followed by laboratory and physical measures done by a nurse. Subsequently, women were provided breakfast, reminded to take their prescribed medications, and instructed to complete a questionnaire booklet, which included the Center for Epidemiologic Studies Depression Scale. These procedures were followed at the 3- and 6-month follow-up visits. The Diagnostic Interview Schedule based on the Diagnostic and Statistical Manual of Mental Disorders IV was also administered at baseline to verify the mental health exclusion criteria and to prevent women with suicidal ideation who needed immediate treatment from enrolling in the study. For women who reported using psychoactive medications (antidepressants and/or antianxiety) and/or psychotherapy (e.g., psychologist, psychiatrist, social worker) prior to entry into the study, they were allowed to remain on them and participate in the study if they had significant depressive symptoms.
Randomization
Sample size was estimated using data from Lustman's randomized, controlled, CBT trial for persons with type 2 diabetes and depression [20]. Using a Fischer's exact test with an alpha of .05 and power of .80, it was estimated that at least 19 persons per group would be needed to see differences in depression at 3 months and 33 per group at 6 months. To account for possible attrition, it was determined that 80 women (40 per group) would be enrolled with each cohort being 20 (10 treatment and 10 control).
Assignments to the groups were made after the baseline assessment. Because of the small sample size, women were matched on their level of depression (±1.0 standard deviation). It was anticipated that there would be four cohorts of women. Thus, four randomization lists were generated using a random seed number by the statistician. Four cohorts of women were enrolled over the course of the study, which lasted 24 months. Each participant was contacted by phone regarding their assignment, and a follow-up letter was sent with a list of resources for mental health services (this was provided in class to the treatment group). The participants, the data collector, and the intervention staff (nurse and psychologist) were not blinded to the group assignment.
Retention Strategies
Methods for the successful retention of the women in both groups included (1) data collection visits and CBT sessions at convenient times, (2) an honorarium in a stepped compensation manner for data collection visits, (3) paid parking, and (4) reminder phone calls and letters for scheduled visits. SWEEP participants were also provided with a bag that contained a binder for class materials and a compact disc player (valued at $20). In addition, at the end of every weekly SWEEP session, name tags were used for a random drawing of one small gift (e.g., body lotion valued at $10), which facilitated group camaraderie. These retention methods have been previously reported [48].
Interventions
Intervention (Treatment Group)
Women assigned to this group received the SWEEP program, which was a psychoeducational intervention delivered by a trained nurse (who was different than the nurse collecting the participant data) in a group. The program educated women with type 2 diabetes about (1) recognizing the signs and symptoms of depression and other moods (anxiety and anger), (2) the relationship between moods, metabolic control and self-care behaviors, and (3) the management of depression, anxiety, and anger using CBT. The SWEEP program was developed from the experiences of women with type 2 diabetes who participated in focus groups addressing the psychological impact of living with diabetes [21]. The SWEEP Program is synonymous with “cleaning the mind and body of negative thoughts and emotions.” The program was 8 weeks with each session lasting 1 h. Women were invited to arrive 30 min prior to the group session to socialize and refreshments were provided. There has been evidence that booster sessions combined with cognitive therapy is as successful as medication therapy in the treatment of depression [18, 49]. Thus, two booster sessions were also done to review the learned skills, to have group sharing regarding their experiences with the skills, and to assist with retention.
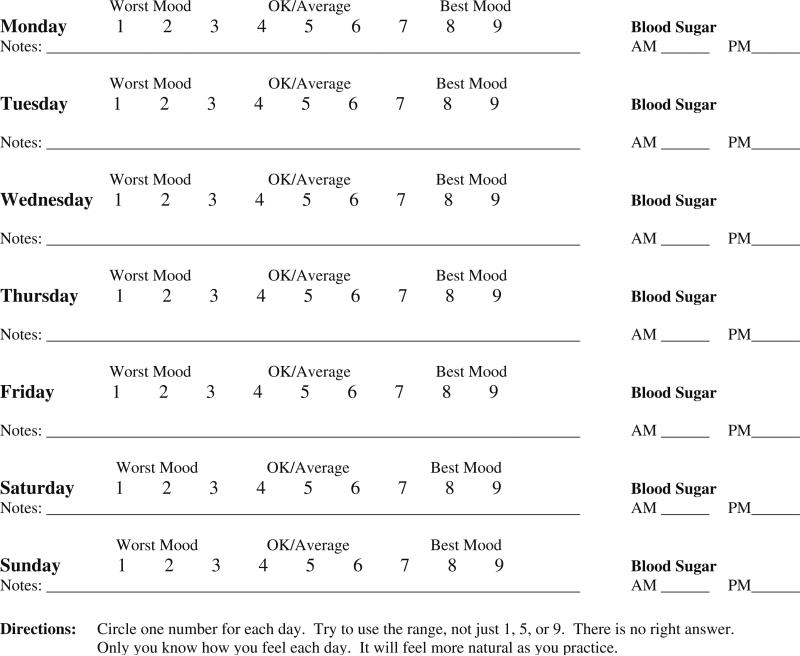
The SWEEP program used elements of pre-existing programs for treating depression, anxiety, and anger. Permission to use elements from each program was obtained. For depression management, the “Reality Management Approach for Persons with Depression” developed by Munoz and colleagues [50, 51] at the University of California San Francisco was used. This group CBT program for depression has practical skills to change mood-related thoughts or behaviors and personal projects to reinforce skill development between group sessions. For anxiety management, a progressive muscle relaxation CD developed by Surwit et al. [45] for persons with diabetes was used. For anger management, The Williams LifeSkills System for Managing Stress and Anger (video and workbook) was utilized [52, 53]. It addresses how to reduce anger, build relationships, manage anxiety, resolve conflict, learn assertive skills, and build positive attitudes. The SWEEP program utilized many of the techniques addressed by Abraham and Michie [54], which include providing information on health behavior, general encouragement, goal setting, self-talk, and stress management. The SWEEP program objectives with established program content for each week are delineated in Table 1. Homework was an essential part of the SWEEP program as previous research has indicated that engagement in the homework component of CBT is important for its success [55]. As recommended by Munoz et al., the term “personal projects” was used as the term “homework” often has a negative connotation. A sample is provided in Fig. 1. One of the key components of SWEEP was mood and glucose monitoring for participants to understand the relationship between their mood, metabolic control, and health behaviors. Another example of a “personal project” has been previously published [48].
Table 1.
Content and personal projects for the SWEEP Program
| Session no. | SWEEP content | Weekly projects in class and at home |
|---|---|---|
| 1 | Welcome to SWEEP; understanding how mood affects blood sugar; learning the symptoms of depression, anxiety, anger | SWEEP Journey-Welcome Rose Ceremony (class) Daily quick mood and blood sugar log (home) |
| 2 | Recognizing signs of stress, understanding how it affects blood sugar & self-care behaviors | Identify personal stressors (class) Practice stress relaxation CD (home) |
| 3 | Learning how depression creates negative thoughts and impacts self-care behaviors, understanding automatic thoughts and using a thought record | Helpful/unhelpful thought assessment (class) Begin thought record: identify the situation, feelings, and thoughts (home) |
| 4 | Celebration of halfway point; learning how to think differently and challenge automatic thoughts | Continue thought record and include evidence to support/not support automatic thoughts (home) |
| 5 | Identifying other methods to decrease negative thoughts and improve self-care behaviors (thought stopping, distraction, physical activity) | Practice thought stopping (class) Identify and schedule activities (e.g., walking) to decrease negative thoughts (home) |
| 6 | Understanding relationships and how they affect mood and self-care behaviors, learning how to communicate effectively | Video clip of poor communication impact on relationships and mood (class) Identify social circle of positive/negative relationships (home) |
| 7 | Learning how to respond differently and asking for what you need | Practice listening skills (class) Using “I” statements (home) |
| 8 | Putting it all together, reviewing skills learned, relapse of mood and behaviors | Identification of most helpful skills (class) Review “Quick mood and blood sugar logs” to assess for improvements (class) |
Participants turn in the “Quick mood and blood sugar log” (Fig. 1) every week
Fig. 1.
SWEEP quick mood log. Note: Adapted with permission from Muñoz et al. [50]
Intervention Fidelity
The SWEEP program was delivered by a nurse who had undergone training for the CBT. There was standardization of the treatment in terms of the content presented (Table 1). A licensed clinical psychologist attended all of the class sessions and evaluated the nurse for fidelity to the sessions and provided feedback.
Usual Care (Control Group)
Women assigned to this group received no study-related intervention but were allowed to receive treatment for diabetes and depression outside of the study as needed. According to Freedland et al. ( [56], p. 330), a “treatment development trial testing whether a novel intervention has any effect at all can use a pure no-treatment control condition if nonstudy care is available.” Patients were offered the SWEEP program after completion of the study if their depression level met the enrollment criteria. All UC participants were given the stress relaxation CD used in the SWEEP program upon completion of the study. Six subjects (17 %) participated in the SWEEP program after first serving as a control.
Patient Safety
For the protection of all the patients, the informed consent document stated that in the event of suicidal ideation upon baseline assessment or during the course of the study, the study psychologist would be contacted, and the primary health-care provider would be informed so that appropriate referral and treatment could be done.
Measurements
Primary Outcome of Moods
Depression
The Center for Epidemiologic Studies Depression Tool is 20 items and measures “depressive symptoms” and their severity. This tool was administered over the telephone for screening and by questionnaire at subsequent time points. Participants were asked to report their symptom severity for the past few weeks with the following choices: (1) rarely or none of the time, (2) some or a little of the time, (3) occasionally or a moderate amount of time, and (4) most or all of the time. It is a well-accepted tool for screening for depressive symptoms in primary care. The tool has excellent internal reliability (Cronbach alpha from .85 to .90) and established validity by correlations with other self-report measures, clinical ratings of depression, and factor analysis [57, 58]. Most recently, it was cited as a tool for effective use in persons with diabetes [59]. For the current study, the Cronbach alpha reliability ranged from .87 to .92 for the three time periods.
Anxiety
The State–Trait Anxiety Inventory is a 40-item scale, which differentiates between the temporary condition of “state anxiety” and the more long-standing quality of “trait anxiety.” There is a four-point Likert scale (1=not at all to 4=very much so) delineating the degree to which an individual experiences the described feeling “at the present time” to measure state anxiety (20 questions). There is another four-point likert scale (1=almost never to 4=almost always) describing the way an individual “generally feels” for trait anxiety (20 questions). The mean score for adults is 35 for each subscale with higher scores reflecting more anxiety. The alpha reliability has been reported, and construct validity has been established [60, 61]. For the current study, the Cronbach alpha ranged from .90 to .95 for both state and trait anxiety.
Anger
The State–Trait Anger Expression Inventory is a 44-item tool that measures the experience of anger as an emotion (State Anger), the predisposition to experience any feelings as a personality trait (Trait Anger), and the manner in which anger is expressed (Anger Expression). For adult females, the mean score for state and trait anger is 18 for each, and for female psychiatric patients, it is 24 and 20, respectively. The mean score for the index of anger expression is 32 for normal female adults and about 37 for female psychiatric patients. Reliability and validity of the tool has been established [62]. The Cronbach alpha reliability ranged from 76 to .95 for the current study at the three time points.
Diagnostic Interview Schedule
This is a structured mental health interview that uses the criteria specified in the Diagnostic and Statistical Manual of Mental Disorders IV to generate diagnoses that can be used for research purposes [63, 64]. It has been reported that results of the Diagnostic Interview Schedule correlate significantly with clinical diagnoses [65–67]. For this study, it was used to obtain a history of depression and to screen for suicidal ideation, which was an exclusionary criterion for participation.
Secondary Outcomes of Glycemic Control and Health-Related Quality of Life
Glycemic Control
For fasting blood glucose, the LDX system, which uses enzymatic methodology and solid-phase technology was used to measure glucose (Cholestech Corporation, Hayward CA). Precision for the LDX ranges between 2 and 6 %, depending on the analyte.
Hemoglobin A1c was measured using the Bayer DCA 2000 (Miles Diagnostic Division). The coefficient of variation for the within-run precision of this measurement is from 2.1 to 4.5 %, and the between-run precision is from 0.8 to 4.4 % [68]. Controls were run on each day to ensure reliable results.
Health-Related Quality of Life
For life satisfaction, the Ferrans and Powers Quality of Life Index—Diabetes III Version was used to assess quality of life. This tool consists of 34 items that measures satisfaction (1=very dissatisfied to 6=very satisfied) and importance (1=very unimportant to 6=very important) in four areas of life (health and functioning, social and economic, psychological/spiritual, and family) that impact quality of life for persons with diabetes. Reliability and validity of the tool is well established [69, 70]. For the current study, the Cronbach alpha ranged from .68 to .93 for the three time points.
For functional status, the SF-12 developed by Ware, Kosninski, and Keller is a well-recognized measurement of perceived health status. It is a shorter version of the Medical Outcomes Study SF-36 and includes the physical component summary and the mental component summary, with Cronbach alpha at .87 and .84. A confirmatory factor analysis also provided evidence of validity [71–73]. For the current study, the Cronbach alpha ranged from .77 to .80 at the various time points.
Other Measures
Other measures include demographics. The Diabetes Care Profile from the Michigan Diabetes Research and Training Center has a section on demographics that was used. Information collected included age, marital status, ethnicity/race, level of education, and employment status. The profile also had a diabetes history, which included current treatment, comorbidities (e.g., complications of diabetes), and medications. Development, validity, and reliability of the Diabetes Care Profile have been reported [74].
Another measure is diabetes knowledge. The Michigan Diabetes Research and Training Center's Brief Diabetes Knowledge Test was used and included 23 questions with a multiple choice response format. For persons not on insulin, only 14 of the 23 items were asked. The test was updated to reflect current diabetes practices. The reliability of the tests has been established [75].
Data Management and Analysis
Data collection forms and a study operations manual were developed before recruitment. All data were recorded by study personnel on protocol specific data forms. An electronic data tracking and management system was developed to assure that forms were completed in a timely fashion and to check for potential data errors. SPSS 17.0, and Hierarchical Linear Models 6.08 were used for data analysis.
Results
Participant Characteristics
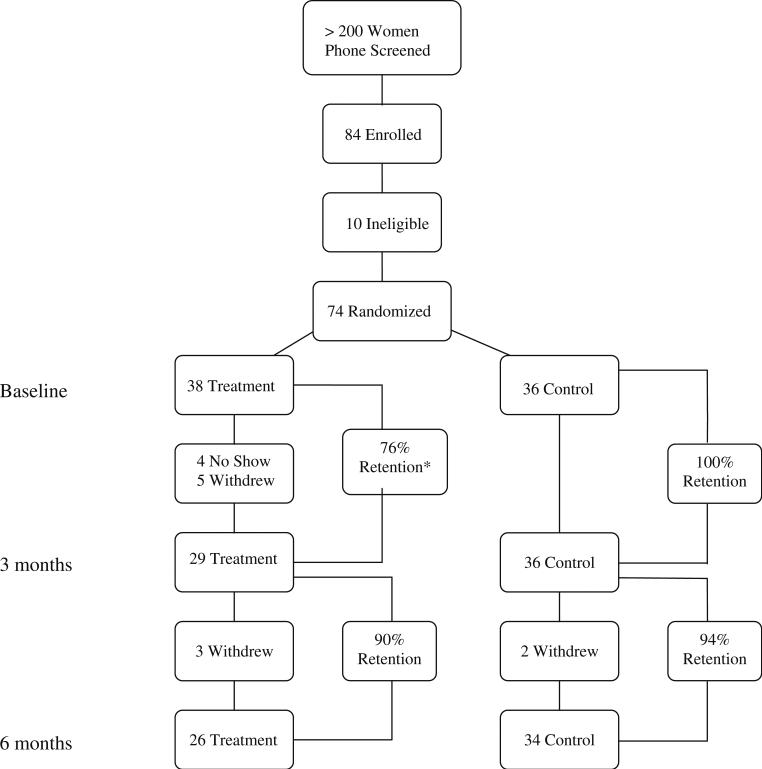
There were 84 women who completed baseline enrollments of whom 10 were not eligible (4 psychiatric reasons as verified by psychologist, 2 not depressed, 1 grief depression, 2 medical conditions, and 1 alcohol abuse) (Fig. 2). Of those who were eligible (n=74), there were no baseline differences between the treatment or control group on key variables (Table 2). There was also no significant difference on self-reported use of psychoactive medications (36 %) or psychotherapy (13 %) between groups. Following randomization, 4 patients never showed up for treatment, leaving 70 persons who actually participated in the trial. At 3 months, 65 remained (92 % retention). Reasons for attrition included one medical problem, one family issue, one no transportation, and two needing psychiatric treatment. At 6 months, 60 remained in the study (85 % retention from baseline), and attrition was due to new medical conditions (1 brain tumor, 2 cardiac, 1 orthopedic surgery, and 1 unknown). Of the women with diabetes and comorbid depression enrolled, 60 (26 treatment and 34 control) completed baseline, 3 and 6 month measures.
Fig. 2.
Recruitment and retention flow diagram. There were four women who never showed up for the first class or thereafter. For those who did show up (n=34), there was an 85 % retention from baseline to 3 months
Table 2.
Baseline characteristics of participants
| Variable | Treatment (N=38) Mean (SD) | Control (N=36) Mean (SD) |
|---|---|---|
| Age (years) | 54.8 (8.8) | 54.0 (8.4) |
| Race (%) | ||
| White | 63 % | 69 % |
| Black | 29 % | 25 % |
| Hispanic | 8% | 6% |
| Weight (lbs) | 229.1 (64.4) | 226.9 (48.7) |
| Diabetes (years) | 10.5 (8.2) | 10.0 (6.5) |
| Mood outcomes | ||
| Depression | 27.7 (9.3) | 28.9 (9.5) |
| Trait anxiety | 51.6 (9.8) | 50.4 (9.2) |
| State anxiety | 45.8 (12.8) | 47.9 (11.9) |
| Anger expression | 40.6 (13.2) | 34.7 (13.9) |
| Trait anger | 19.8 (4.8) | 18.6 (5.7) |
| State anger | 18.7(6.5) | 18.1 (5.2) |
| Glycemic control | ||
| Glucose (mg/dl) | 165.3 (71.1) | 168.8 (74.9) |
| HBA1c (%) | 7.8 (1.8) | 7.9 (2.0) |
| Quality of life outcomes | ||
| Life satisfaction | ||
| Quality of life | 15.0 (5.2) | 15.5 (5.0) |
| Functional status | ||
| Mental health | 36.6 (10.0) | 37.2 (10.9) |
| Physical health | 38.0 (10.5) | 41.4 (9.4) |
There were no statistically significant differences between treatment and control groups for those randomized (38 vs. 36) and those who participated (34 vs. 36).
Treatment Session Participation
There were eight treatment sessions and two booster sessions over the 6-month study period. For those who had missed a group session, materials from that week were provided to the participant, and they were encouraged to review them. For the treatment sessions, 82 % of women completed six or more sessions. For those women who attended less than four sessions, none participated in the follow-up booster sessions. For women who had attended six or more group sessions, the attendance at the two booster sessions was 68 % for both sessions and 21 % for one session, and 11 % of women did not attend any boosters.
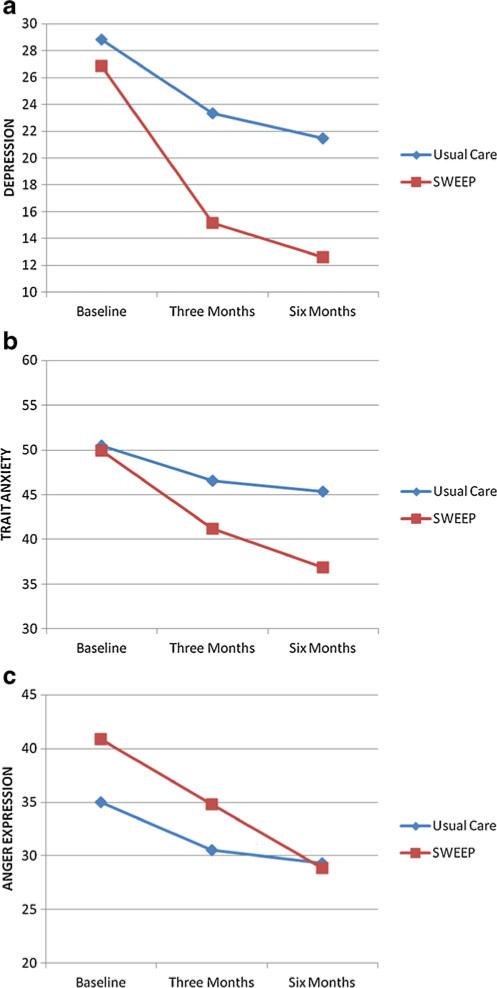
Changes in Primary Outcomes
To examine the effectiveness of SWEEP among those women who completed the study (N=60), a repeated measures analysis of variance (ANOVA) was employed on the primary outcomes and post hoc tests (contrasts) were used to test the hypothesized differences at respective time points if interactions were found to be significant (Table 3 and Fig. 3a–c). The mean raw score for each primary outcome at the respective time points is presented in Table 3 for both the treatment and UC group. Because the intent to treat (ITT) is the more widely accepted method for analysis of controlled, clinical trial, multilevel modeling was employed to examine the primary and secondary outcomes as well. The ITT approach takes into consideration all participants, regardless of whether or not they completed the study (N=74). This analysis examined individual change and variability over time (level 1 model) and treatment effect while controlling for cohort (level 2 model).
Table 3.
Observed means and standard deviations (SD) of outcome measures per time point and group
| Variables | SWEEP |
Usual care |
||||
|---|---|---|---|---|---|---|
| Time | Baseline (n=38) Mean (SD) | 3 months (n=29) Mean (SD) | 6 months (n=26) Mean (SD) | Baseline (n=36) Mean (SD) | 3 months (n=36) Mean (SD) | 6 months (n=34) Mean (SD) |
| Mood outcomes | ||||||
| Depression | 27.7 (9.3) | 15.2 (7.9) | 12.6 (8.0) | 28.9 (9.5) | 23.1 (11.4) | 21.5 (10.2) |
| Trait anxiety | 51.6 (9.8) | 40.9 (10.1) | 36.9 (10.1) | 50.4 (9.2) | 46.1 (12.3) | 45.3 (12.0) |
| State anxiety | 45.8 (12.8) | 38.8 (11.1) | 35.7 (12.4) | 47.9 (11.9) | 43.2 (12.2) | 43.6 (12.6) |
| Anger expression | 40.6 (13.2) | 34.9 (12.2) | 28.9 (13.7) | 34.7 (13.9) | 30.3 (13.9) | 29.6 (14.9) |
| Trait anger | 19.8 (4.8) | 17.1 (3.8) | 16.4 (4.8) | 18.6 (5.7) | 17.5 (6.3) | 16.1 (5.2) |
| State anger | 18.7 (6.5) | 17.8 (4.3) | 16.9 (3.1) | 18.1 (5.2) | 17.9 (5.4) | 18.2 (7.2) |
| Glycemic control | ||||||
| Fasting glucose(mg/dl) | 165.3 (71.1) | 144.6 (44.0) | 141.5 (47.3) | 168.8 (74.9) | 187.0 (78.9) | 167.6 (77.6) |
| HBA1c (%) | 7.8 (1.8) | 7.4 (1.3) | 7.4 (1.3) | 7.9 (2.0) | 7.8 (1.8) | 7.8 (1.6) |
| Quality of life outcomes | ||||||
| Life satisfaction | ||||||
| Overall | 15.0 (5.2) | 18.2 (4.5) | 19.7 (4.3) | 15.5 (5.0) | 17.1 (4.4) | 17.5 (5.5) |
| Health | 13.5 (5.4) | 17.1 (4.6) | 18.5 (5.0) | 14.1 (5.5) | 16.0 (4.7) | 16.5 (5.8) |
| Psychological | 15.2 (6.7) | 19.1 (6.0) | 21.5 (4.9) | 14.6 (6.9) | 16.9 (6.6) | 17.2 (7.7) |
| Family | 18.4 (6.9) | 19.4 (6.4) | 20.1 (6.2) | 18.0 (6.6) | 18.9 (6.1) | 18.5 (6.7) |
| Socioeconomic | 15.7 (6.2) | 18.5 (5.0) | 20.4 (4.8) | 17.6 (5.5) | 18.1 (5.0) | 19.1 (5.7) |
| Functional status | ||||||
| Mental | 36.6 (9.9) | 47.4 (10.8) | 49.4 (8.5) | 37.2 (10.9) | 43.0 (9.8) | 42.8 (12.4) |
| Physical | 38.0 (10.5) | 37.3 (13.6) | 38.1 (12.9) | 41.4 (9.4) | 40.1 (9.7) | 39.8 (9.7) |
Fig. 3.
a Changes in depression as a function of time and treatment. b Changes in trait anxiety as a function of time and treatment. c Changes in anger expression as a function of time and treatment
For those who completed the study, repeated measures ANOVA results yielded a significant main effect of time [F (2, 116)=34.26, p<.001], indicating a decrease in depression over the course of the study on average. More importantly, there was a significant interaction between time and SWEEP [F (2, 116)=3.78, p<.05], and post hoc tests indicated, that at 3 and 6 months, those in SWEEP had significantly lower levels of depression compared to UC (p=.003, p=.001, respectively; Fig. 3a). Using ITT, results demonstrated a significant decrease over time on average (β01=–5.41, SE=0.76, p<.01), and those in SWEEP had a significantly greater rate of decline in depression compared to UC (β11=–3.96, SE=1.43, p<.01). Therefore, results indicate that SWEEP was more effective than UC at reducing depression. Given that 100 % of women were categorized as depressed at baseline, changes in the categories of depressed versus not depressed were examined. At 3 months, 48 % of women in SWEEP and 70 % of women in UC remained depressed (p=.083). During this period of time, two patients were withdrawn from the study, as it was deemed by the psychologist that they needed individualized psychiatric care. By 6 months, only 35 % of those in SWEEP, while 80 % of those in UC remained depressed (p<.001), indicating continued depression improvement for those who had received SWEEP. Over the course of the study, one woman in the treatment group and two in the control group initiated medications to treat their mood, but there was no change in the number of women receiving psychotherapy.
For the outcome of trait anxiety, repeated measures ANOVA results yielded a significant main effect of time [F (2, 116)=27.21, p<.001], indicating a decrease in trait anxiety over the course of the study on average for those who completed the study. More importantly, there was a significant interaction between time and SWEEP [F (2, 116)=4.95, p<.01], and post hoc tests indicated that, at 6 months, those in SWEEP had lower levels of trait anxiety compared with UC (p=.005; Fig. 3b). Using ITT, results demonstrated a significant decrease across time on average (β01=–4.59, SE=0.76, p<.01), and those in SWEEP had a significantly greater rate of decline in trait anxiety compared to UC (β11=–4.28, SE=1.46, p<.01). Results indicate that SWEEP was more effective than UC at decreasing trait anxiety.
For the outcome of state anxiety, repeated measures ANOVA results yielded a significant main effect of time [F (2,116)=7.32, p<.001], indicating a decrease in state anxiety over the course of the study on average. However, there was no significant interaction between time and SWEEP, indicating no differences in the rate of change between SWEEP and UC. Similarly, ITT results indicated a significant decrease in state anxiety over time on average (β01=–3.39, SE=0.97, p<.01), but those in SWEEP did not have a significantly greater rate of decline in state anxiety compared to UC. Findings indicate that SWEEP was not more effective than UC at alleviating state anxiety.
For the outcome of anger expression, repeated measures ANOVA results yielded a significant main effect of time [F (2,114)=21.62, p<.001], indicating a decrease in anger expression over the course of the study on average. The interaction between time and SWEEP indicated a trend towards significance [F (2, 114=3.03, p=.052] (Fig. 3c). ITT results indicated a significant decrease in anger expression over time on average (β01=–1.56, SE=0.27, p<.01), and those in SWEEP had a significantly greater rate of decline in anger expression compared to UC (β11=–1.26, SE=0.22, p<.05). Thus, SWEEP was more effective at reducing anger expression compared to UC using the ITT approach.
For the outcome of trait anger, repeated measures ANOVA results yielded a significant main effect of time [F (2,116)=18.73, p<.001], indicating a decrease in trait anger over the course of the study on average for those who completed the study. However, there was no significant interaction between time and SWEEP. Using ITT, results demonstrated a significant decrease across time on average (β01=–1.59, SE=0.29, p<.001), but those in SWEEP did not have a significantly greater rate of decline in trait anger compared to UC. Results indicate that SWEEP was not more effective than UC at decreasing trait anger.
For the outcome of state anger, repeated measures ANOVA results did not yield a significant main effect of time, and there was no significant interaction between time and SWEEP. Using ITT, there were no significant findings. Results indicate that SWEEP was not more effective than UC at decreasing state anger.
Changes in Secondary Outcomes (Table 3)
For the outcome of fasting glucose and HbA1C, both repeated measures ANOVA, and IIT results indicated there was no significant decrease in fasting glucose or HbA1c over time, and there were no differences in the rate of change on either glycemic outcome between SWEEP and UC, suggesting that SWEEP was not more effective at improving metabolic control relative to UC over the course of the study. Of clinical relevance, however, was the decrease in HbA1c (–0.4 %) and fasting glucose (–22 mg/dl) for those in SWEEP from baseline to 3 months.
For overall quality of life, repeated measures ANOVA results yielded a significant main effect of time [F (2, 116)=22.25, p<.001], indicating an increase in quality of life over the course of the study on average. There was no significant interaction between time and SWEEP, indicating no differences in the rate of change between SWEEP and UC. The ITT results yielded a significant increase over time on average (β01=1.43, SE=0.24, p<.01), and those in SWEEP had a significantly greater rate of increase in overall quality of life compared to UC (β11=1.05, SE=0.47, p<.05). These results suggest that SWEEP was more effective than UC at improving quality of life using an ITT approach.
For the outcome of health and functioning, repeated measures ANOVA results yielded a significant main effect of time [F (2, 116)=22.40, p<.001], indicating an increase in health and functioning over the course of the study on average. In addition, there was no significant interaction between time and SWEEP, indicating no differences in the rate of change between SWEEP and UC. Similarly, the ITT results indicated a significant increase over time on average (β01=1.61, SE=0.29, p<.01), but those in SWEEP did not have a significantly greater rate of increase in health and functioning compared to UC. Overall, these results suggest that SWEEP was not more effective than UC at improving health and functioning.
For the outcome of psychological and spiritual satisfaction, repeated measures ANOVA results yielded a significant main effect of time [F (2, 116)=24.23, p<.001] indicating an increase in psychological and spiritual satisfaction over the course of the study on average. However, there was no significant interaction between time and SWEEP, indicating no differences in the rate of change between SWEEP and UC. The ITT results indicated a significant increase over time on average (β01=1.99, SE=0.33, p<.01), and those in SWEEP had a significantly greater rate of increase in psychological and spiritual satisfaction compared to UC (β11=1.58, SE=0.63, p<.05). Thus, results suggest that SWEEP was more effective than UC at improving psychological and spiritual satisfaction with the ITT approach.
For the outcome functional status (mental health), repeated measures ANOVA results yielded a significant main effect of time [F (2, 116)=16.47, p<.001], indicating an increase in mental functional status over the course of the study on average. However, there was no significant interaction between time and SWEEP, indicating no differences in the rate of change between SWEEP and UC. The ITT results indicated a significant increase over time on average [β01=4.33, SE=0.81, p<.01] and those in SWEEP had a significantly greater rate of increase in mental functional status compared to UC (β11=3.79, SE=1.54, p<.05). Overall, these results suggest that SWEEP was more effective than UC at improving functional status (mental health) with the ITT approach. No effects emerged for functional status (physical health) with either statistical approach.
Intervention Evaluation
The SWEEP program was evaluated by patients with a structured questionnaire (1=not helpful to 4=very helpful). The most helpful content aspects of the program were learning about the signs/symptoms of dysphoric symptoms (M=3.87), learning techniques to stop negative thinking (i.e., thought stopping, thought records, and relaxation) (M03.81), and improving communication (M=3.89). The most helpful skills learned were examining daily blood sugar levels and mood (M=3.71) and sharing experiences with others (M=3.90). In terms of what they would change about SWEEP were that (1) it should have more than two follow-up sessions and (2) it should include diabetes self-management education following SWEEP. Participants indicated that a key benefit of the program was understanding the relationship between their thoughts, emotions, and blood sugar levels.
Discussion
Primary Outcomes
This study demonstrated the effectiveness of a group program delivered by a nurse trained in CBT for depression treatment for women with type 2 diabetes. This has important clinical significance, as women with type 2 diabetes have a disproportionately greater risk for depression and poorer health outcomes than men with type 2 diabetes [22, 76]. For women in SWEEP, there was not only a reduction in depression symptoms over time that was significantly greater than usual care, but also the percent who were depressed by 6 months was substantially less than those who had received usual care (35 vs. 85 %). Women in SWEEP also experienced a greater reduction in trait anxiety. These improvements in mental health are important, given that recent evidence indicates that antidepressant medications may have suboptimal effectiveness and can be associated with side effects, which contribute to negative metabolic outcomes [6–13].
CBT is a well-accepted therapy for persons who have depression [17–19]. In the clinical depression trial by Lustman et al. [20], there was a significant improvement in depression in persons with diabetes who received 10 weeks of individual CBT. The present study also found significant improvement in depression in women with type 2 diabetes who received 8 weeks of group CBT. The 6-month remission rate was also comparable between these two studies (75 vs 65 %, respectively). Most previous depression studies of persons with diabetes have included individual CBT sessions delivered by psychologists [20, 26, 77, 78] rather than group CBT by other health professionals [25, 79, 80]. An important contribution of this study is that a nurse trained in CBT for depression treatment delivered the group program. Nurses are the most frequent contact for the patient with diabetes in the health-care system. Thus, the SWEEP program may be a cost-effective strategy for treating depression and improving health outcomes for persons with diabetes.
SWEEP was developed from the experiences of women with type 2 diabetes who participated in focus groups examining the psychological impact of living with diabetes [21]. In the present study, women reported feeling comfortable in their ability to express their emotions with other women. Recently, a large, randomized trial using a group-based psychosocial intervention to reduce stress for women following a myocardial infarction was published. Women reported feeling more comfortable in discussing sensitive topics like marital and other stressors with other women and received support from each other that was important in their recovery. The gender-specific intervention had a positive effect on reducing mortality (p=.007) [81]. This study was especially important since the Enhancing Recovery in Coronary Heart Disease Patients trial for the treatment of depression following myocardial infarction did not demonstrate a significant benefit for women [82]. Thus, further study of the benefit of group interventions for depression treatment that target specific gender and racial groups is needed.
Because other emotions may be associated with depression, these outcomes were also examined in the present study. Trait anxiety was noted to improve more so with SWEEP. The significance of SWEEP in modifying trait anxiety suggests that the program had an impact on an anxiety that was more durable and perhaps amendable to change. Surwit et al. [45] has demonstrated an improvement in anxiety in persons with type 2 diabetes when using their stress relaxation CD. That CD was used in the present study, and women identified it as their “personal time,” which was very therapeutic. Women in SWEEP also had a greater decline in anger expression. It has been reported that “anger” towards self (e.g., for not taking better care of oneself) and towards others (e.g., constantly on them about what to eat) is a symptom experienced by women with type 2 diabetes, particularly in conjunction with depression and anxiety [21]. Thus, it may be an important emotion that deserves additional study.
Of particular significance is that women in the present study were generally not cognizant of the impact that emotions had on their blood glucose fluctuations, which was learned through the daily use of their mood logs (Fig. 1). There is limited research that addresses the relationship between glucose self-monitoring and its impact on mood [83, 84]. The need to understand this relationship is important since poor self-management decisions may be due to depression or other emotions that make it difficult to adhere to recommended therapies [21].
Secondary Outcomes
In terms of glycemic control, there were no statistically significant differences between groups in fasting glucose and HbA1c over time. However, the study was not powered to detect for changes in glycemic control. For those in SWEEP, clinical improvements in metabolic outcomes were observed at 3 months (Table 3). Whether providing diabetes education after SWEEP could enhance and sustain potential improvements in metabolic control would be worthy of exploration. A large trial of collaborative care for depression in persons with diabetes that did not include diabetes education found a significant improvement in depression, but no improvement in HbA1c [25]. Although Lustman et al. [20] did not find an improvement in glycemic control immediately following individual CBT for depression at 10 weeks, an improvement was noted by 6 months. It was suggested that this delay in benefit may be due to the need to focus on CBT skills vs. diabetes care. It should be noted, however, that all patients received diabetes education in that study. In the present study, although diabetes education was not provided, glucose monitoring and health behaviors (e.g., physical activity as a method to improve mood) (Table 1 and Fig. 1) were emphasized. Thus, it may be very reasonable to provide diabetes self-management training following completion of depression treatment. Once depression improves, it may be an opportunity to “seize the moment” as patients may be more receptive to education and lifestyle changes. This “window of opportunity” may be the optimal time to offer educational support [85].
There is evidence to suggest that negative emotions, such as anxiety, fear, and depression, can affect learning and performance [86, 87] and that depressed persons need more repetitions to reach mastery and have more difficulty with transfer skills [88]. Research has demonstrated that a good mood has a positive effect on one's attention, ability to learn, and ability to engage in self-management behaviors [89–92]. Thus, treating depression and then targeting diabetes self-management may be the most effective approach to improving health outcomes for women with diabetes and would be a logical step for further study.
Improved health-related quality of life was reported by participants, specifically on the mental and psychological components of life. This is not surprising given that the program was targeted at improvements of this aspect of health. Perhaps with education targeted at diet and physical activity following the treatment of depression, improvements in the physical aspects of life may also be possible.
Limitations
Some of the strengths of the study may also be seen as limitations. For this study, the SWEEP program was administered by the same nurse who was trained in group CBT for depression and supervised by a clinical psychologist. Although the materials for the program (e.g., power-point presentations, homework assignments) can be manualized, the need to receive training on the assessment and use of CBT for depression management would be highly recommended. For clinical translation, the testing of the SWEEP program among nurses who receive CBT training and are oriented to the SWEEP program would be the ideal. Given the number of patients with diabetes that experience depression, it may be reasonable to expect that nurses have training in depression assessment to successfully manage their complex care. Secondly, even though the SWEEP program is highly structured and could be readily implemented (Table 1), a number of techniques are used to improve depression and the other moods (e.g., stress relaxation CD, thought stopping). It should also be recognized that the support women received from each other prior to or during the group sessions could have contributed to their improvement in depression. In this study, UC was used as the control condition. Thus, perhaps another study where parallel groups (SWEEP program, diabetes education and support, and usual care) are randomized could tease out the contribution of group support in alleviating depression in women with type 2 diabetes. Several studies like this are currently in progress [46, 93]. Finally, since the study was not powered to test for changes in glycemic control, perhaps a larger study to determine the impact of treating depression and its impact on glycemic control is warranted.
Future Research
The challenges that health-care providers face in addressing the emotional issues for persons with type 2 diabetes has recently been reported [94]. Although medication is often a treatment option prescribed for depression and anxiety, some medications can negatively impact glucose levels and also cause weight gain. There is a need to develop treatment options whereby the emotional needs of persons with type 2 diabetes can be met so that successful diabetes self-management can take place.
Vaccarino [95] reported that gender-specific trials should be conducted as men and women may respond differently to psychosocial interventions. Reports identify that sex-based differences need to be considered in developing health programs [96–99]. One study reported that women with diabetes receive higher levels of social support from their health-care team members than men with diabetes, and thus, their treatment plan needs to be different than their male counterparts [98]. Another study reported that women had a higher prevalence of negative emotions and internal control that prevented them from reaching optimal glycemic control and benefit most from diabetes care offering social support, whereas men benefit by getting information regarding their disease management [99]. Most recently, a successful behavioral intervention targeted at Hispanic women with type 2 diabetes was reported [100]. Differences in approaches to treatment for men and women may be necessary to achieve improved metabolic outcomes, particularly for women.
The SWEEP program was developed specifically for women based on focus group data and is the first CBT program to treat dysphoric symptoms in depressed women in a group setting and to demonstrate an improvement in depression. Given that women had requested diabetes self-management information following the CBT intervention, future research to examine whether persons are more responsive to diabetes education and diabetes self-management training following successful treatment for their mood disorders should be conducted with sample sizes that could detect changes in self-care behaviors and metabolic outcomes.
Acknowledgments
This study was funded by the National Institutes of Health, National Institutes of Health (K-23: NR009420) and Loyola University School of Nursing
Footnotes
Conflict of interest The authors have no conflicts of interest to disclose.
Contributor Information
Sue M. Penckofer, School of Nursing, Loyola University Chicago, Maywood, IL, USA spencko@luc.edu
Carol Ferrans, College of Nursing, University of Illinois, Chicago, IL, USA
Patricia Mumby, School of Medicine, Loyola University Chicago, Maywood, IL, USA
Mary Byrn, Saint Mary's College, Notre Dame, IN, USA
Mary Ann Emanuele, School of Medicine, Loyola University Chicago, Maywood, IL, USA
Patrick R. Harrison, College of Arts and Sciences, Loyola University Chicago, Chicago, IL, USA
Ramon A. Durazo-Arvizu, School of Medicine, Loyola University Chicago, Maywood, IL, USA
Patrick Lustman, School of Medicine, Washington University St. Louis, St. Louis, MO, USA
References
- 1.Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002;25:464–470. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 2.Egede LE. Major depression in individuals with chronic medical disorders: Prevalence, correlates and association with health resource utilization, less productivity, and functional disability. Gen Hosp Psychiatry. 2007;29:409–416. doi: 10.1016/j.genhosppsych.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 3.Lustman PJ, Clouse RE, Nix BD, et al. Sertraline for prevention of depression recurrence in diabetes mellitus. Arch Gen Psychiatry. 2006;63:521–529. doi: 10.1001/archpsyc.63.5.521. [DOI] [PubMed] [Google Scholar]
- 4.Lustman PJ, Williams MM, Sayuk GS, Nix BD, Clouse RE. Factors influencing glycemic control in type 2 diabetes during acute-and maintenance-phase treatment of major depressive disorder with bupropion. Diabetes Care. 2007;30:459–466. doi: 10.2337/dc06-1769. [DOI] [PubMed] [Google Scholar]
- 5.Williams MM, Clouse RE, Nix BD, et al. Efficacy of sertraline in prevention of depression recurrence in older versus younger adults with diabetes. Diabetes Care. 2007;30:801–806. doi: 10.2337/dc06-1825. [DOI] [PubMed] [Google Scholar]
- 6.Lustman PJ, Griffith LS, Clouse RE, et al. Effects of nortripty-line on depression and glycemic control in diabetes: Results of a double-blind, placebo-controlled trial. Psychosom Med. 1997;59:241–250. doi: 10.1097/00006842-199705000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Lisi DM. Diabetes and the psychiatric patient. US Pharmacist. 2010;35:62–79. [Google Scholar]
- 8.Amiel JM, Manguarian CV, Ganguli R, Newcomer JS. Addressing cardiometabolic risk during treatment with anti-psychotic medications. Curr Opin Psychiatry. 2008;21(6):613–618. doi: 10.1097/YCO.0b013e328314b74b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morrato EH, Newcomer JS, Kamat S, Baser O, Harnett J, Cuffel B. Metabolic screening after the American Diabetes Association's consensus statement on antipsychotic drugs and diabetes. Diabetes Care. 2009;32(6):1037–1042. doi: 10.2337/dc08-1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Derijks HJ, Meyboom RH, Heerdink ER, et al. The association between antidepressant use and the disturbance in glucose homeostasis: Evidence from spontaneous reports. Eur J Clin Pharmacol. 2008;64(5):531–538. doi: 10.1007/s00228-007-0441-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bai YM, Lin CC, Chen JY, Chen TT, Su TP, Chou P. Association of weight gain and metabolic syndrome in patients taking cloza-pine: An 8-year cohort. J Clin Psychiatry. 2011;72(6):751–756. doi: 10.4088/JCP.09m05402yel. [DOI] [PubMed] [Google Scholar]
- 12.Torrent C, Amann B, Sanchez-Moreno J, et al. Weight gain in bipolar disorder: Pharmacological treatment as a contributing factor. Acta Psychiatr Scand. 2008;118:4–18. doi: 10.1111/j.1600-0447.2008.01204.x. [DOI] [PubMed] [Google Scholar]
- 13.Schwartz TL, Nihalani N, Virk S, Jindal S, Chilton M. Psychiatric medication-induced obesity: Treatment options. Obes Rev. 2004;5:233–238. doi: 10.1111/j.1467-789X.2004.00149.x. [DOI] [PubMed] [Google Scholar]
- 14.Rubin RR, Ma Y, Marrero DG, et al. Elevated depression symptoms, antidepressant medicine use, and risk of developing diabetes during the diabetes prevention program. Diabetes Care. 2008;31:420–426. doi: 10.2337/dc07-1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fournier JC, DeRubeis RJ, Hollon SD, et al. Antidepressant drug effects and depression severity: A patient-level meta-analysis. JAMA. 2010;303:47–53. doi: 10.1001/jama.2009.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT. Initial severity and antidepressant benefits: A meta-analysis of data submitted to the food and Drug Administration. PLOS Med. 2008;5(2):e045. doi: 10.1371/journal.pmed.0050045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agency for Healthcare Research and Quality . Clinical practice guideline on the management of major depression in adults. National Guideline Clearing House, USDHHS; 2011. [Google Scholar]
- 18.Dozois DJ, Bieling PJ, Patelis-Siotis I, et al. Changes in self-schema structure in cognitive therapy for major depressive disorder: A randomized clinical trial. J Consult Clin Psychol. 2009;77:1078–1088. doi: 10.1037/a0016886. [DOI] [PubMed] [Google Scholar]
- 19.Beck AT, Dozois DJ. Cognitive therapy: Current status and future directions. Annu Rev Med. 2010;62:397–409. doi: 10.1146/annurev-med-052209-100032. [DOI] [PubMed] [Google Scholar]
- 20.Lustman P, Griffith L, Freedand K, Kissel S, Clouse R. Cognitive behavior therapy for depression in type 2 diabetes mellitus: A randomized controlled trial. Ann Intern Med. 1998;129:613–621. doi: 10.7326/0003-4819-129-8-199810150-00005. [DOI] [PubMed] [Google Scholar]
- 21.Penckofer S, Ferrans C, Velsor-Friedrich B, Savoy S. The psychological impact of living with diabetes: Women's day to day experiences. Diabetes Educ. 2007;33:680–690. doi: 10.1177/0145721707304079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Whittemore R, Melkus G, Grey M. Self-report of depressed mood and depression in women with type 2 diabetes. Issues Ment Health Nurs. 2004;25:243–260. doi: 10.1080/01612840490274750. [DOI] [PubMed] [Google Scholar]
- 23.Chiu CJ, Wray LA, Beverly EA, Dominic OG. The role of health behaviors in mediating the relationship between depressive symptoms and glycemic control in type 2 diabetes: A structural equation modeling approach. Soc Psychiatry Psychiatr Epidemiol. 2010;45:67–76. doi: 10.1007/s00127-009-0043-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peyrot M, Rubin R. Persistence of depressive symptoms in diabetic adults. Diabetes Care. 1999;22:448–452. doi: 10.2337/diacare.22.3.448. [DOI] [PubMed] [Google Scholar]
- 25.Katon WJ, Von Korff M, Lin EHB, et al. The Pathways study: A randomized trial of collaborative care in patients with diabetes and depression. Arch Gen Psychiatry. 2004;61:1042–1049. doi: 10.1001/archpsyc.61.10.1042. [DOI] [PubMed] [Google Scholar]
- 26.Gonzalez JS, McCarl LA, Wexler DJ, et al. Cognitive-behavioral therapy for adherence and depression (CBT-AD) in type 2 diabetes. J Cognit Psychother Int Q. 2010;24(4):329–343. doi: 10.1891/0889-8391.24.4.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Markowitz S, Gonzalez, Wilinson JL, Safren SA. Treating depression in diabetes: Emerging findings. Psychosomatics. 2011;52(1):1–18. doi: 10.1016/j.psym.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khuwaja AK, Lalani S, Dhanani R, Azam IS, Rafique G, White F. Anxiety and depression among outpatients with type 2 diabetes: A multi-centre study of prevalence and associated factors. Diabetol Metab Syndr. 2010;2:72. doi: 10.1186/1758-5996-2-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grigsby AB, Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. Prevalence of anxiety in adults with diabetes: A systematic review. J Psychosom Res. 2002;53(6):1053–1060. doi: 10.1016/s0022-3999(02)00417-8. [DOI] [PubMed] [Google Scholar]
- 30.Lloyd CE, Dyer PH, Barnett AH. Prevalence of symptoms of depression and anxiety in a diabetes clinic population. Diabet Med. 2000;17(3):198–202. doi: 10.1046/j.1464-5491.2000.00260.x. [DOI] [PubMed] [Google Scholar]
- 31.Huang CJ, Chiu HC, Lee MH, Wang SY. Prevalence and incidence of anxiety disorders in diabetic patients: A national population-based cohort study. Gen Hosp Psychiatry. 2011;33(1):8–15. doi: 10.1016/j.genhosppsych.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 32.Anderson RJ, Grigsby AB, Freedland KE, et al. Anxiety and poor glycemic control: A meta-analytic review of the literature. Int J Psychiatry Med. 2002;32(3):235–247. doi: 10.2190/KLGD-4H8D-4RYL-TWQ8. [DOI] [PubMed] [Google Scholar]
- 33.Pasquini M, Picardi A, Biondi M, Gaetano P, Morosini P. Relevance of anger and irritability in outpatients with major depressive disorder. Psychopathology. 2004;37(4):155–160. doi: 10.1159/000079418. [DOI] [PubMed] [Google Scholar]
- 34.Yi JP, Yi JC, Vitaliano PP, Weinger K. How does anger coping style affect glycemic control in diabetes patents? Int J Behav Med. 2008;15(3):167–172. doi: 10.1080/10705500802219481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu SF, Huang YC, Liang SY, Wang TJ, Lee MC, Tung HH. Relationships among depression, anxiety, self-care behavior and diabetes education difficulties in patients with type 2 diabetes: A cross-sectional questionnaire survey. Int J Nurs Stud. 2011;48:1376–1383. doi: 10.1016/j.ijnurstu.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 36.Wolfgang L, Hogan B, Rutledge T, Chawla A, Lenz J, Leung D. There is more to anger coping than “in” or “out”. Emotion. 2003;3(1):12–29. doi: 10.1037/1528-3542.3.1.12. [DOI] [PubMed] [Google Scholar]
- 37.Swenson SL, Rose M, Vittinghoff E, Stewart A, Schillinger D. The influence of depressive symptoms on clinician-patient communication among patients with diabetes. Med Care. 2008;46(3):257–265. doi: 10.1097/MLR.0b013e31816080e9. [DOI] [PubMed] [Google Scholar]
- 38.Epstein RM, Duberstein PR, Feldman MD, et al. “I didn't know what was wrong”: How people with undiagnosed depression recognize, name and explain their distress. J Gen Intern Med. 2010;25:954–961. doi: 10.1007/s11606-010-1367-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gonzalez JS, Safren SA, Cagliero E, et al. Depression, self-care, and medication adherence in type 2 diabetes: Relationships across the full range of symptom severity. Diabetes Care. 2007;30(9):2222–2227. doi: 10.2337/dc07-0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Egede LE, Grubaugh AL, Ellis C. The effect of major depression on preventive care and quality of life among adults with diabetes. Gen Hosp Psychiatr. 2010;32(6):563–569. doi: 10.1016/j.genhosppsych.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 41.Uden AL, Elofsson S, Andreasson A, Hillered E, Eriksson I, Brismar K. Gender differences in self-rated health, quality of life, quality of care, and metabolic control in patients with diabetes. Gend Med. 2008;5(2):162–180. doi: 10.1016/j.genm.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 42.Ali S, Stone M, Skinner TC, Robertson N, Davies M, Khunti K. The association between depression and health-related quality of life in people with diabetes: A systematic literature review. Diabetes Metab Res Rev. 2010;26(2):75–89. doi: 10.1002/dmrr.1065. [DOI] [PubMed] [Google Scholar]
- 43.Grandy S, Chapman RH, Fox KM, SHIELD Study Group Quality of life and depression of people living with type 2 diabetes mellitus and those at low and high risk for type 2 diabetes: Findings from the Study to Help Improve Early evaluation and management of risk factors leading to Diabetes. Int J Clin Pract. 2008;62:562–568. doi: 10.1111/j.1742-1241.2008.01703.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kohen D, Burgess AP, Catalan J, Lant A. The role of anxiety and depression in quality of life and symptom reporting in people with diabetes mellitus. Qual Life Res. 1998;7:197–204. doi: 10.1023/a:1024961325084. [DOI] [PubMed] [Google Scholar]
- 45.Surwit RS, van Tilburg MA, Zucker N, et al. Stress management improves long-term glycemic control in type 2 diabetes. Diabetes Care. 2002;25:30–34. doi: 10.2337/diacare.25.1.30. [DOI] [PubMed] [Google Scholar]
- 46.Petrak F, Hautzinger M, Plack K, et al. Cognitive behavioural therapy in elderly type 2 diabetes patients with minor depression or mild major depression: Study protocol of a randomized controlled trial (MIND-DIA). BMC Geriatr. 2010;10:21. doi: 10.1186/1471-2318-10-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schneider KL, Pagoto SL, Handschin B, et al. Design and methods for a pilot randomized clinical trial involving exercise and behavioral activation to treat comorbid type 2 diabetes and major depressive disorder. Mental Health Phys Act. 2011;4(1):13–21. doi: 10.1016/j.mhpa.2011.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Penckofer S, Byrn M, Mumby P, Ferrans C. Improving subject recruitment, retention, and participation in research through Peplau's Theory of Interpersonal Relations. Nurs Sci Q. 2011;24:146–151. doi: 10.1177/0894318411399454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hollon S, DeRubeis RJ, Shelton RC, et al. Prevention of relapse following cognitive therapy vs medications in moderate to severe depression. Arc Gen Psychiatry. 2005;62:417–422. doi: 10.1001/archpsyc.62.4.417. [DOI] [PubMed] [Google Scholar]
- 50.Munoz RF, Ghosh Ippen C, Rao S, Le H-L, Dwyer EV. [March 12, 2012];Manual for group cognitive behavioral therapy of major depression: A reality management approach [participant manual and instructor's manual] http://www.medschool.ucsf.edu/latino/cbtdengl.aspx. from the University of California San Francisco/San Francisco General Hospital Latino Mental Health Research Program Website:
- 51.Muñoz RF, Ying YW, Bernal G, et al. Prevention of depression with primary care patients: A randomized controlled trial. Am J Community Psychol. 1995;23:199–222. doi: 10.1007/BF02506936. [DOI] [PubMed] [Google Scholar]
- 52.Williams VP, Williams RB. Lifeskills: 8 simple ways to build stronger relationships, communicate more clearly, improve your health, and even the health of those around you. Times Books/Random House; New York, NY: 1997. [Google Scholar]
- 53.Kirby ED, Williams VP, Hocking MC, Lane JD, Williams RB. Psychosocial benefits of three formats of a standardized behavioral stress management program. Psychosom Med. 2006;68:816–823. doi: 10.1097/01.psy.0000238452.81926.d3. [DOI] [PubMed] [Google Scholar]
- 54.Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008;27:379–387. doi: 10.1037/0278-6133.27.3.379. [DOI] [PubMed] [Google Scholar]
- 55.Cowan MJ, Freedland KE, Burg MM, et al. Predictors of treatment response for depression and inadequate social support-the ENRICHD randomized clinical trial. Psychother Psychosom. 2008;77(1):27–37. doi: 10.1159/000110057. [DOI] [PubMed] [Google Scholar]
- 56.Freedland KE, Mohr DC, Davidson KW, Schwartz JE. Usual and unusual care: Existing practice control groups in randomized controlled trials of behavioral interventions. Psychosom Med. 2011;73:324–336. doi: 10.1097/PSY.0b013e318218e1fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 58.Zich JM, Attkinsson CC, Greenfield TK. Screening for depression in the primary clinics: The CES-D and the BDI. Int J Psychiatry Med. 1990;20:259–277. doi: 10.2190/LYKR-7VHP-YJEM-MKM2. [DOI] [PubMed] [Google Scholar]
- 59.Roy T, Lloyd CE, Pouwer F, Holt RI, Sartorius N. Screening tools used for measuring depression among people with type 1 and type 2 diabetes: A systematic review. Diabet Med. 2012;29:164–75. doi: 10.1111/j.1464-5491.2011.03401.x. doi 10.1111/j.1464-5491.2011.03401.x. [DOI] [PubMed] [Google Scholar]
- 60.Speilberger C, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. State-trait anxiety inventory for adults. Mind Garden Inc.; Menlo Park, CA: 1977. [Google Scholar]
- 61.Barnes L, Harp D, Jung W. Reliability generalization of scores on the Spieberger state-trait anxiety inventory. Educ Psychol Meas. 2002;62(4):603–618. [Google Scholar]
- 62.Spielberger C. Professional manual. Psychological Assessment Resources; Lutz: 1999. State–trait anger expression inventory—2. [Google Scholar]
- 63.Arean PA, Alvidrez J. The prevalence of psychiatric disorders and subsyndromonal mental illness in low-income, medically ill elderly. Int J Psychiatry Med. 2001;31:9–24. doi: 10.2190/YGL6-N54R-08RW-1BF4. [DOI] [PubMed] [Google Scholar]
- 64.Aaron LA, Bradley LA, Alarcon GS, et al. Psychiatric diagnoses in patients with fibromyalgia are related to health care-seeking behavior rather than to illness. Arthritis Rheum. 1996;39:436–445. doi: 10.1002/art.1780390311. [DOI] [PubMed] [Google Scholar]
- 65.Ross HE, Swinson R, Doumani S, Larkin EJ. Diagnosing comorbidity in substance abusers: A comparison of the test–retest reliability of two interviews. Am J Drug Alcohol Abuse. 1995;21:167–185. doi: 10.3109/00952999509002686. [DOI] [PubMed] [Google Scholar]
- 66.Levitan RD, Blouin AG, Navarro JR, Hill J. Validity of the computerized DIS for diagnosing psychiatric inpatients. Can J Psychiatry. 1991;36:728–731. [PubMed] [Google Scholar]
- 67.Blouin AG, Perez EL, Blouin JH. Computerized administration of the diagnostic interview schedule. Psychiatry Res. 1988;23:335–344. doi: 10.1016/0165-1781(88)90024-8. [DOI] [PubMed] [Google Scholar]
- 68.Cholestech Corporation . Technical brief. Cholestech Corporation; Hayward: 2002. The accuracy and reproducibility of a rapid, fingerstick method for measuring A1c certified by the NGSP. [Google Scholar]
- 69.Ferrans C, Powers M. Quality of Life Index. http://www.uic.edu/orgs/qli/
- 70.Quinn L, Poradzisz M, Ferrans C. Psychometric properties of the Quality of Life Index: Diabetes Version. Diabetes. 1999;48(Supplement 1):A320. [Google Scholar]
- 71.Ware JE, Kosinski M, Keller SD. A 12-item short-from health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 72.Ware JE, Kosinski M, Turner-Bowker DM, Gandek B. How to score version 2 of the SF-12 health survey. Quality Metric Incorporated; Lincoln RI: 2002. [Google Scholar]
- 73.Ware JE, Kosinski M, Kleer SD. SF-12: How to score the SF-12 physical and mental health summary scales. 3rd edn. Lincoln: Quality Metric Incorporated. 1998 [Google Scholar]
- 74.Fitzgerald JT, Davis WK, Connell CM, Hess GE, Funnell MM, Hiss RG. Development and validation of the diabetes care profile. Eval Health Prof. 1996;19:208–230. doi: 10.1177/016327879601900205. [DOI] [PubMed] [Google Scholar]
- 75.Fitzgerald JT, Funnell MM, Hess GE, et al. The reliability and validity of a brief diabetes knowledge test. Diabetes Care. 1998;21:706–710. doi: 10.2337/diacare.21.5.706. [DOI] [PubMed] [Google Scholar]
- 76.Pan A, Lucas M, Sun Q, et al. Increased mortality risk in women with depression and diabetes mellitus. Arch Gen Psychiatr. 2011;68(1):42–50. doi: 10.1001/archgenpsychiatry.2010.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lustman PJ, Freedland KE, Griffith LS, Clouse RE. Predicting response to cognitive behavioral therapy of depression in type 2 diabetes. Gen Hosp Psychiatr. 1998;20:302–306. doi: 10.1016/s0163-8343(98)00039-5. [DOI] [PubMed] [Google Scholar]
- 78.van Bastelaar KM, Pouwer F, Cuijpers P, Twisk JWR, Snoek FJ. Web-based cognitive behavioral therapy (W-CBT) for diabetes patients with co-morbid depression: Design of a randomised controlled trial. BMC Psychiatry. 2008;8:9. doi: 10.1186/1471-244X-8-9. (doi:10.1186/1471-244X/8/9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illness. New Engl J Med. 2010;363(27):2611–2620. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lamers F, Jonkers CCM, Bosma H, Knotternerus JA, van Elijk JThM. Treating depression in diabetes patients: Does a nurse administered minimal psychological intervention affect diabetes-specific quality of life and glycaemic control. A randomized trial. J Adv Nurs. 2011;67(4):788–799. doi: 10.1111/j.1365-2648.2010.05540.x. [DOI] [PubMed] [Google Scholar]
- 81.Orth-Gomer K, Schneiderman N, Wang HX, Walldin C, Blom M, Jernberg T. Stress reduction prolongs life in women with coronary disease: The Stockholm Women's Intervention Trial for Coronary Heart Disease (SWITCHD). Circ Cardiovas Qual Outcomes. 2009;2:25–32. doi: 10.1161/CIRCOUTCOMES.108.812859. [DOI] [PubMed] [Google Scholar]
- 82.Berkman LF, Blumenthal J, Burg M, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: The Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA. 2003;289:3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- 83.Skaff MM, Mullan JT, Hoffman L, et al. Daily negative mood affects fasting glucose in type 2 diabetes. Health Psychol. 2009;28(3):265–272. doi: 10.1037/a0014429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rausch JR. Measures of glycemic variability and links with psychological functioning. Curr Diabetes Rep. 2010;10(6):415–421. doi: 10.1007/s11892-010-0152-0. [DOI] [PubMed] [Google Scholar]
- 85.Schneider KL, Bodenlos JS, Ma Y, et al. Design and methods for a randomized clinical trial treating comorbid obesity and major depressive disorder. BMC Psychiatry. 2008;8:77. doi: 10.1186/1471-244X-8-77. doi:10.1186/1471-244X-8-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Black SJ, Everhart DE, Durham TW, Walker M, Golden J, Demaree HA. The effects of anxiety on affective learning and serial position recall. Int J Neurosci. 2008;118:1269–1285. doi: 10.1080/00207450701242933. [DOI] [PubMed] [Google Scholar]
- 87.Baker JE, Shannon S. The reasoning in depression: Impairment on a concept discrimination learning task. Cognit Emot. 1995;9:579–597. [Google Scholar]
- 88.Brand S, Reimer T, Opwis K. How do we learn in a negative mood? Effects of a negative mood on transfer and learning. Learn Instruct. 2007;17:1–16. [Google Scholar]
- 89.Fredrickson BL, Branigan C. Positive emotions broaden the scope of attention and thought-action repertoires. Cognit Emot. 2005;19:313–332. doi: 10.1080/02699930441000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Huang ES, Brown SE, Ewigman BG, Foley EC, Meltzer DO. Patient perceptions of quality of life with diabetes-related complications and treatments. Diabetes Care. 2007;30:2478–2483. doi: 10.2337/dc07-0499.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Egede LE, Ellis C. The effects of depression on diabetes knowledge, diabetes self-management, and perceived control in indi-gent patients with type 2 diabetes. Diabetes Technol Thera. 2008;10:213–219. doi: 10.1089/dia.2007.0278. [DOI] [PubMed] [Google Scholar]
- 92.Ellis SE, Speroff T, Dittus RS, Brown A, Pichert JW, Elasy TA. Diabetes patient education: A meta-analysis and meta-regression. Patient Educ Couns. 2004;52:97–205. doi: 10.1016/s0738-3991(03)00016-8. [DOI] [PubMed] [Google Scholar]
- 93.Pibernik-Okanovic M, Ajdukovic D, Lovrencic MV, Hermanns N. Does treatment of subsydromal depression improve depression and diabetes related outcomes: Protocol for a randomized controlled comparison of psycho-education, physical exercise and treatment as usual. Trials. 2011;12:17. doi: 10.1186/1745-6215-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Beverly EA, Hultgren BA, Brooks KNM, Ritholz MD, Abrahamson MJ, Weinger KW. Understanding physicians’ challenges when treating type 2 diabetic patients’ social and emotional difficulties. Diabetes Care. 2011;34:1086–1088. doi: 10.2337/dc10-2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Vaccarino V. Depression in the cardiac patient: A call for action. American Heart Association Communities Learning Library. 2008 Sep 29th; http://pt.wkhealth.com/pt/re/aha/addcontent.9467671.htm;jsessionid0MGDbQhGJyW2RbKQkPkRC3QypqyPQR7PX8NTBGFTLzJhZq6RXQvpy!-2027397035!181195628!8091!-1.
- 96.McCollum M, Hansen LB, Lu L, Sullivan PW. Gender differences in diabetes mellitus and effects on self-care activity. Gend Med. 2005;2(4):246–254. doi: 10.1016/s1550-8579(05)80054-3. [DOI] [PubMed] [Google Scholar]
- 97.Long CG, Fulton B, Hollin CR. The development of a ‘best practice’ service for women in medium-secure psychiatric setting: Treatment components and evaluation. Clin Psychol Psychother. 2008;15:304–319. doi: 10.1002/cpp.591. [DOI] [PubMed] [Google Scholar]
- 98.Gucciardi E, Wang SC, DeMelo M, Amaral L, Stewart DE. Characteristics of men and women with diabetes: Observations during patients’ initial visit to a diabetes education centre. Can Fam Physician. 2008;54:219–227. [PMC free article] [PubMed] [Google Scholar]
- 99.Kacerovsky-Bielesz G, Lienhardt S, Hagenhofer M, et al. Sex-related psychological effects on metabolic control in type 2 diabetes. Diabetologia. 2009;52:781–788. doi: 10.1007/s00125-009-1318-7. [DOI] [PubMed] [Google Scholar]
- 100.Barrera M, Toobert DJ, Strycker LA, Osuna D, King D, Glasgow RE. Multiple-behavior-change interventions for women with type 2 diabetes. Diabetes Spectrum. 2011;24:75–80. [Google Scholar]