Abstract
Objective
Opioid (including prescription opiate) abuse and overdose rates in the US have surged in the past decade. The dearth and limitations of opioid abuse and overdose surveillance systems impede the development of interventions to address this epidemic. We explored evidence to support the validity of emergency medical services (EMS) data on naloxone administration as a possible proxy for estimating incidence of opioid overdose.
Methods
We reviewed data from Baltimore City Fire Department EMS patient records matched with dispatch records over a thirteen month time period (2008-2009), and census 2008 data. We calculated incidence rates and patient demographic and temporal patterns of naloxone administration, and examined patient evaluation data associated with naloxone administration. Results were compared to the demographic distributions of the EMS patient and city population and to prior study findings.
Results
Of 116,910 EMS incidents during the study period for patients 15 years and older, EMS providers administered naloxone 1,297 times (1.1% of incidents), an average of 100 administrations per month. Overall incidence was 1.87 administrations per 1,000 population per year. Findings indicated naloxone administration peaked in summer months (31% of administrations), weekends (32%), and late afternoon (4-5:00pm [8%]); and there was a trend toward peaking in the first week of the month. The incidence of suspected opioid overdose was highest among males, whites, and those in the 45-54 year age group. Findings on temporal patterns were comparable to findings from prior studies. Demographic patterns of suspected opioid overdose were similar to medical examiner reports of demographic patterns of fatal drug or alcohol related overdoses in Baltimore in 2008-9 (88% of which involved opioids). The findings on patient evaluation data suggest some inconsistencies with previously recommended clinical indications of opioid overdose.
Conclusions
While our findings suggest limitations of EMS naloxone administration data as a proxy indicator of opioid overdose, the results provide partial support of the data for estimating opioid overdose incidence and suggest ways to improve such data. The study findings have implications for an EMS role in conducting real-time surveillance and treatment and prevention of opioid abuse and overdose.
Keywords: emergency medical services, heroin/opiate/opioid abuse, Narcan/naloxone, overdose, epidemiology
INTRODUCTION
The recent surge in opioid abuse and overdose in the US has led to a tripling of unintentional opioid overdose deaths in the past decade.1,2 (We use the term “opioid” to refer to the entire family of opiates, including those naturally derived, synthetic or semi-synthetic.) Prescription drugs are now the second most abused drug in the U.S. after marijuana, with opioids accounting for three-quarters of prescription drugs abused.1,3 Overdose, long the leading cause of death among heroin abusers, is now second only to motor vehicle accidents in leading causes of accidental death in the US, and a major cause of hospitalization.2,4,5
Timely, local surveillance data on population-level opioid overdose, and demographic and temporal patterns of overdose, are needed to inform the development of effective drug abuse treatment and overdose prevention interventions. National drug abuse and overdose surveillance systems have a considerable lag time in availability and have major methodological limitations, rendering them inadequate for keeping up with changing local trends and demographic patterns.6-8 Data from household surveys, such as Substance Abuse and Mental Health Services Administration’s (SAMHSA’s) National Survey on Drug Use and Health, are limited by self-report bias and by under-representation of vulnerable populations, including those homeless or unstably housed.1,3 Data from SAMHSA’s Drug Abuse Warning Network (DAWN), in its reliance on hospital emergency department (ED) records, is subject to misclassification errors and to selection bias in its restriction to EDs in select geographic areas and low response rates of participating hospitals.9 While medical examiner (ME) data is important for understanding local opioid related overdose, it is limited in its utility in informing preventive intervention due to its restriction to cases resulting in death.
EMS data of naloxone administration
Prior research findings suggest that emergency medical services (EMS) data associated with naloxone administration may be an important complement to other opioid abuse and overdose surveillance systems, and may inform targeted preventive intervention.10-17 EMS systems have administered naloxone, a rapid-acting, safe and effective opioid antagonist, for over two decades to patients suspected of experiencing opioid overdose.10-18 EMS records may include objective indicators of opioid involvement; information about circumstances of overdoses, including time; medical care provided; and characteristics of persons who overdose, including those who receive no further medical care.
Researchers have considered naloxone administration by EMS a proxy indicator of suspected opioid overdose, and have noted potential advantages of EMS records for understanding opioid overdose.10-17 The importance of these EMS data is underscored by the observations that many EMS patients who experience opioid overdose, a quarter to a third in recent studies, seek no further care and therefore would otherwise not be included in other health services records;11,12,17 and that persons who experience opioid overdose are at extremely high risk of fatality or of later fatal overdose.4,16,19 In addition, unlike EDs, EMS systems often serve a defined geographic area; and data from such EMS systems may be combined with population census data to provide estimates of population level incidence rates of opioid overdose. Furthermore, by focusing on adverse events associated with opioid use, EMS data potentially avoids complexities of prescription opioid abuse surveillance, such as distinguishing abuse from medically legitimate use.7,8,20
Given the dearth of studies systematically examining opioid overdose on a local population level, it is not clear the extent to which EMS data on naloxone administration may be a reasonable proxy measure of opioid overdose.10 Evidence to date suggests that EMS data on suspected opioid overdose may yield under- or over-estimates of opioid overdose. Some studies suggest a significant proportion of patients experiencing opioid overdose avoid ED transport out of fear of discrimination, harassment or police arrest; to avoid incurring financial costs of medical care; or to avoid opioid withdrawal symptoms, the major side effect of naloxone.21-23 However, overdosing persons may avoid EMS care for some of the same reasons they decline ED transport. In a study on drug overdose among injection drug users in Baltimore, Maryland (the study site), the vast majority of whom had overdosed on opioids, only 46% reported receiving EMS care for their last recent drug overdose, similar to the EMS response level reported by heroin users in another study.16,24 On the other hand, it is also possible that EMS data on naloxone administration may overestimate opioid overdose. Given the high risks of morbidity and mortality consequent to opioid overdose and the safety of naloxone, EMS protocols may indicate naloxone administration for a number of health events.25
The objective of the present study was to explore evidence to support the utility of EMS data on naloxone administration for estimating opioid overdose incidence, and whether it may be a reasonable proxy measure of opioid overdose. Based on the approach of Merchant and colleagues’ prior study of Rhode Island EMS records of naloxone administration, we calculated suspected opioid overdose incidence in the study population, and examined patient demographic and temporal patterns, and patient evaluation data related to naloxone administration to explore evidence of internal consistency of the data.10
METHODS
Data were from the BQUEST (Baltimore Quality Urban Emergency Services and Treatment) study, an examination of Baltimore City EMS service demand and care to substance abusers and other vulnerable populations, conducted by researchers at the Johns Hopkins University Bloomberg School of Public Health in collaboration with the Baltimore City Fire Department and other service agencies. The study was approved by the Johns Hopkins University Bloomberg School of Public Health’s Institutional Review Board (IRB), which authorized a waiver of informed consent.
Study site
Baltimore City has among the county’s highest rates of opioid abuse and overdose. ME data indicates the city has over three times the national rates of drug-, opioid-, or cocaine-related overdose fatalities.26,27 In 2007, Baltimore City had the highest rate of drug-related deaths (49.9 per 100,000 population) among all metropolitan counties, 86% of which were opioid related.27 A prior study found that heroin was the main substance of abuse in Baltimore, reported by 70% of persons in public drug or alcohol abuse treatment.28 Moreover, Baltimore, of all major US metropolitan areas, has the second highest prevalence of injection drug use, the mode of heroin administration most commonly associated with overdose.29
Study design & methods
The BQUEST study used a retrospective epidemiological study design. As part of the study we analyzed Baltimore City Fire Department (BCFD) EMS electronic patient records and Baltimore City computer-assisted emergency (9-1-1 call) dispatch records for medically-related EMS incidents that occurred within the city from October 1, 2008 through October 31, 2009. BCFD EMS is a single tiered, all advanced life response system and the city’s only public EMS system. It serves an 81 square mile area and offers universal access to care.
Baltimore City medical-related 9-1-1 calls were received and processed at a single dispatch center, which used the computer assisted Emergency Medical Dispatch system. We identified probable medical-related incidents from dispatch of an EMS unit or an incident code corresponding to a medical issue, and then matched such dispatch data with EMS patient records by incident number. The observation period coincided with the initiation of electronic EMS patient data collection, which was recorded on mobile devices. Data was collected using the Electronic Maryland Ambulance Information System (EMAIS)30 through a contract with Affiliated Computer Services, Inc., which provided us the patient record data. Patient records included information on the health problem; patient assessment, including vital signs; care and treatments provided; call disposition; and demographics.
Maryland EMS protocols for naloxone use
Naloxone administration is part of the Maryland Institute of Emergency Medical Service System protocols for altered mental state and for suspected overdose by injection, neither of which specifies clinical criteria for naloxone use.25 For altered mental state, patient presentation is broadly defined as “may exhibit confusion, focal motor sensory deficit, unusual behavior, [or] unresponsiveness to verbal or painful stimulus”, and in which the “patient has constricted pupils and respiratory depression or is unresponsive and the provider strongly suspects a narcotic overdose”.25 Treatment protocols for altered mental state list naloxone administration at a 0.4 - 2mg dose as a treatment option after assessing vital signs, administering dextrose, and beginning intravenous fluids.25 Paramedics are directed to administer naloxone gradually until “adequate” respiration is achieved to reverse depressed respiration. Treatment protocols for suspected overdose by injection indicate naloxone administration subsequent to beginning intravenous fluids and improving blood pressure.
Other data sources
As naloxone supplies are highly controlled, we examined purchase records by the Baltimore City Fire Department for calendar year 2008 to 2009, obtained from the SAP Enterprise Resource Planning records of Baltimore City. This data was used to compare with naloxone administration data in EMS patient records. Baltimore city population demographics were from the U.S. Census Bureau for 2008.31
Analysis
We imported dispatch and patient record data into Microsoft Access 2003,32 and used SQL to create flat data files for analysis in SPSS 11.033 and Stata 10.1.34 Cases with missing data were excluded from analysis. Analyses compared incidents with naloxone administration to other EMS incidents using the Wald chi-square statistic. Analyses of incidence rates by time variables were conducted using Poisson regression. We analyzed counts of incidents with naloxone administration within each group with Poisson regression using person-time at risk within each group as the measure of exposure. We evaluated the assumption of Poisson regression of equidispersion (i.e., that the conditional variance is equal to the conditional mean) through negative binomial regression, which allows for overdispersion. We report p-values for statistical tests, and incidence rate ratios with 95% confidence intervals for Poisson regressions.
For time trend analysis we used seasonality tests in the “seast” module of Stata, based on the approaches of Edwards and Walter and Elwood.35 For day of the month, we adjusted the time at risk for the 29th to 31st days due to the fewer number of these days in the data. We used the Edwards test for the day of week and time of day analyses, and the Walter and Elwood test, which allows for variation in person-time at risk, for analysis by day of month.35
RESULTS
EMS runs
In the 13-months period, there were 129,142 medical calls in EMS dispatch data, 117,210 calls in the patient record database, and 116,910 incidents with matching dispatch and patient records. Among incidents in EMS dispatch data, 9% of incidents not involving ED transport was missing patient data, as compared to 3% missing patient data in incidents involving transport.
A total of 1,297 naloxone administration incidents were recorded in the period, averaging 100 per month. Among cases receiving naloxone, age was missing for 11 (0.8%); and for the 37 cases (2.9%) listed as 9 years old or younger, 23 had no recorded estimated weight to enable cross-validation, and several recorded weights appeared implausible for the recorded age. We, therefore, excluded these cases. As there was no record of naloxone administration in patients 10-14 years, the analyses include only patients 15 years or older.
The most common route of administration was intranasal (n=519, 40%), followed by intravenous (n=350, 27%) and intramuscular (n=285, 22%). Route of administration was missing for 17 patients (10%). Mean naloxone dosage was 1.3 mg (range 0.02-2.4 mg). Purchase order records indicate that during the observation period, 226 10-mL vials of naloxone (0.4 mg/mL) were purchased (=904 mg). Assuming no use of reserve naloxone and no remaining supply, the average naloxone dosage in the study period was calculated to be 1.4 mg.
For incidents with naloxone administration, the call summary field most frequently listed “medical illness” (n=389, 30%), followed by “controlled substance overdose” (n=363, 28%), “other/miscellaneous” (n=156, 12%), “prescription drug overdose” (n=130, 10%), and “EtOH (alcohol) overdose” (n=130, 10%). Data on patient respiration was recorded for 96% of naloxone administration incidents (n=1,245), of which 597 patients (46%) had a respiration rate of 12 breaths per minute or lower, including 104 patients (8%) who had a respiratory rate of 0; and 623 patients (48%) had a normal respiratory rate. Glasgow Coma Scale (GCS) scores were recorded for 97% (n=1,258) of patients. The average GCS score was 10; 558 patients (43%) had a GCS score ≤8 (indicative of severe central nervous system depression), and 363 patients (28%) had the maximum 15 score. Among patients with a recorded respiratory rate of zero (n=104), 98% had the minimal GCS score of 3 and 90% had a recorded pulse rate of zero. Eight percent of patients (n=99) who were administered naloxone received cardiopulmonary resuscitation, and 18% of those patients had a return of spontaneous circulation. Patient change in status following naloxone administration was recorded in 85% of incidents (n=1,102): for 62% of total incidents the patient improved (n=804), 23% indicated no change (n=298), 0.2% indicated the patient worsened (n=26), and for 0.4% of incidents, patient change could not be assessed (n=52). Ninety-one percent of incidents in the analysis (n=1,180) involved ED transport for further care.
Patient demographics
Compared to the Baltimore population, EMS patients administered naloxone were more likely to be male (n=829, 64%) than female (n=457, 36%); and compared to other EMS patients, they were more likely to be male, less likely to be African American, and more likely to be white (Table 1). The overall incidence rate (IR) of suspected opioid overdose was 1.87 per 1,000 population per year (Table 2). In Poisson regression, the age-adjusted IR was significantly higher for males than females, and the incidence was highest among patients 45-54 years for both sexes (Table 2). The male to female incidence rate ratios (IRR) were highest for those 60-64 years (IRR=3.28; 95% confidence interval [CI]=1.93-5.59), and lowest for the oldest age (85 years and over; IRR=1.02; 95% CI=0.36-2.87) and youngest age groups (15-19 years; IRR=1.13; 95% CI=0.46-2.77). Including a sex-by-age category interaction term did not significantly improve model fit, indicating IRRs for sex did not significantly vary by age.
Table 1.
Demographic comparisons of Baltimore City Emergency Medical Services patients administered naloxone for suspected opioid overdose (n=1,297), all other EMS patients (n=116,910), and Baltimore City residents (n=636,919) (October 2008-09).a
| Administered naloxone | Other EMS patients | Baltimore residents | |
|---|---|---|---|
| Age | |||
| Median | 46 | 48 | 35.5 |
| Range | 15 - 99 | 0 - 108 | - |
| Sex | |||
| Male | 64.5 | 49.1 | 46.6 |
| Female | 35.5 | 50.9 | 53.4 |
| Race/ethnicity | |||
| Asian/Pacific Islander | 0.2 | 0.5 | 1.9 |
| Black/African American | 64.1 | 70.8 | 63.1 |
| Hispanic/Latino | 0.5 | 1.4 | 2.6 |
| American Indian/Alaska Native | 0.1 | 0.2 | 0.2 |
| White | 34.8 | 26.6 | 30.6 |
| Other | 0.2 | 0.4 | 0.2 |
| More than one | - | - | 1.5 |
Baltimore resident data are from US Census (2008)31.
Table 2.
Incidence rates of EMS naloxone administration by Baltimore City Emergency Medical Services in Baltimore for patients 15 years and over by sex and age (October 2008-09).#
| Baltimore city population estimate | Naloxone administrations | Incidence rate per 1,000 person-years | (95% CI) | |
|---|---|---|---|---|
| Males | ||||
| 15 - 19 | 24,895 | 11 | 0.41 | (0.20, 0.73) |
| 20 - 24 | 23,492 | 38 | 1.49 | (1.06, 2.05) |
| 25 - 34 | 42,370 | 110 | 2.40 | (1.97, 2.89) |
| 35 - 44 | 41,740 | 182 | 4.05 | (3.46, 4.65) |
| 45 - 54 | 42,322 | 290 | 6.37 | (5.62, 7.10) |
| 55 - 59 | 17,307 | 70 | 3.79 | (2.91, 4.72) |
| 60 - 64 | 12,657 | 51 | 3.72 | (2.77, 4.89) |
| 65 - 74 | 15,898 | 33 | 1.92 | (1.32, 2.69) |
| 75 - 84 | 9,811 | 15 | 1.41 | (0.79, 2.33) |
| 85 or older | 2,929 | 5 | 1.58 | (0.51, 3.68) |
| Missing | 24 | |||
| Total | 233,421 | 829 | 2.59 | (2.40, 2.75) |
| Females | ||||
| 15 - 19 | 25,665 | 10 | 0.36 | (0.17, 0.66) |
| 20 - 24 | 25,578 | 19 | 0.72 | (0.41, 1.07) |
| 25 - 34 | 46,996 | 63 | 1.24 | (0.95, 1.58) |
| 35 - 44 | 46,079 | 106 | 2.12 | (1.74, 2.57) |
| 45 - 54 | 50,186 | 136 | 2.50 | (2.10, 2.96) |
| 55 - 59 | 21,063 | 47 | 2.06 | (1.51, 2.74) |
| 60 - 64 | 16,289 | 20 | 1.13 | (0.69, 1.75) |
| 65 - 74 | 22,662 | 20 | 0.81 | (0.50, 1.26) |
| 75 - 84 | 17,626 | 11 | 0.58 | (0.29, 1.03) |
| 85 or older | 7,151 | 12 | 1.55 | (0.80, 2.71) |
| Missing | 13 | |||
| Total | 279,295 | 457 | 1.24 | (1.13, 1.35) |
| City Total | 512,716 | 1,286 | 1.87 | (1.76, 1.96) |
Baltimore resident data are from US Census (2008)31.
The IR of naloxone administration per 1,000 person-years was significantly higher for whites (IR = 2.13, 95% CI = 1.94–2.34) compared to African Americans (IR = 1.93, 95% CI = 1.79 – 2.05) and other race patients (IR= 0.40; CI = 0.22-0.67) (Table 3).
Table 3.
Incidence rates of Baltimore City Emergency Medical Services administration of naloxone for suspected opioid overdose by patient race/ethnicity (October 2008-09).a
| Baltimore city popluation estimate | Naloxone administrations | Incidence rate per 1,000 person-years | (95% CI) | |
|---|---|---|---|---|
| Black/ African American | 398,748 | 828 | 1.93 | (1.79,2.05) |
| White | 195,467 | 452 | 2.13 | (1.94,2.34) |
| Other | 30,070 | 14 | 0.40 | (0.22,0.67) |
Baltimore resident data are from US Census (2008)31.
Temporal patterns
Compared to the monthly mean number of incidents, the number of incidents was significantly lower in the fall and winter (October-February) and higher in summer (June-August) (Figure 1). By day of week, the number of incidents with naloxone administration was lowest on Sunday and increased throughout the week (Table 4). In comparison to the weekly mean, the number of naloxone administrations was significantly higher on Friday and Saturday (Figure 2). By comparison to the pattern of other EMS incidents, naloxone administrations varied by time of day, with a nadir at 6-7:00 am and a peak at 4-5:00 pm (Table 5). The hourly pattern of naloxone administration paralleled the pattern for other EMS incidents (Figure 3).
Figure 1.
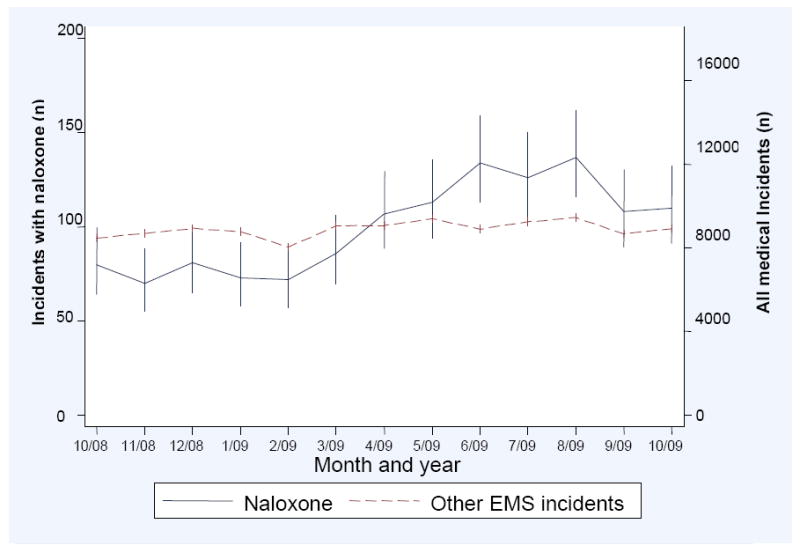
Baltimore City Emergency Medical Services (EMS) naloxone administration incidents and all other EMS incidents by month and year (observed frequency and 95% confidence intervals) (October 2008-09).
Table 4.
Distribution of naloxone administration by Baltimore City Emergency Medical Services by day of week in Baltimore, MD (October 2008-09).
| Total calls | Calls with Naloxone | % of calls on day of week | % of naloxone administrations | |
|---|---|---|---|---|
| Day of week of call | ||||
| Sunday | 16,113 | 156 | 0.97 | 12.03 |
| Monday | 16,607 | 166 | 1.00 | 12.80 |
| Tuesday | 16,315 | 181 | 1.11 | 13.96 |
| Wednesday | 16,591 | 183 | 1.10 | 14.11 |
| Thursday | 16,584 | 192 | 1.16 | 14.80 |
| Friday | 17,310 | 209 | 1.21 | 16.11 |
| Saturday | 17,390 | 210 | 1.21 | 16.19 |
| Total | 116,910 | 1,297 | 1.11 | 100.00 |
Figure 2.
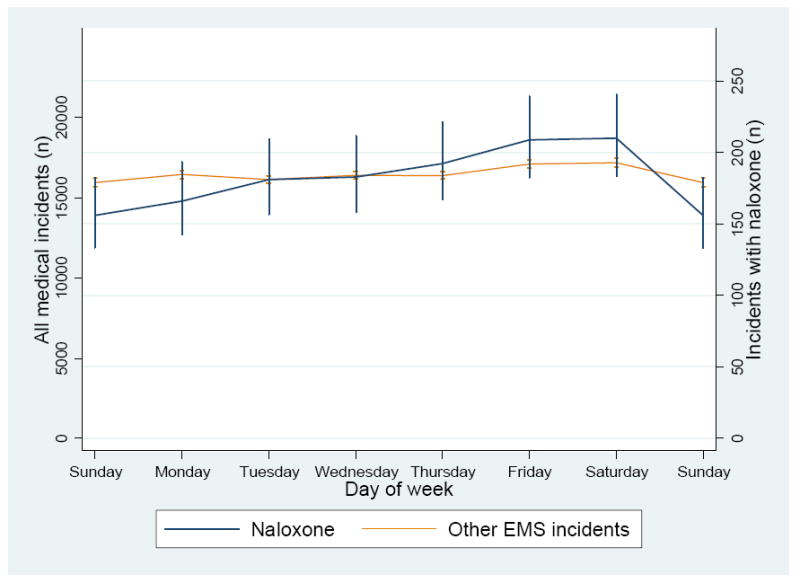
Baltimore City Emergency Medical Services (EMS) incidents of naloxone administration and all other EMS incidents by day of the week (observed frequency and 95% confidence intervals) (October 2008-09).
Table 5.
Distribution of naloxone administration for suspected opioid overdose by Baltimore City Emergency Medical Services (EMS) by hour of day (October 2008-09).
| Total calls | Calls with Narcan | % of calls for hour of day | % of narcan administrations | ||
|---|---|---|---|---|---|
| Hour of day | |||||
| 12:00 AM | 4,005 | 28 | 0.70 | 2.16 | |
| 1:00 AM | 3,683 | 28 | 0.76 | 2.16 | |
| 2:00 AM | 3,455 | 28 | 0.81 | 2.16 | |
| 3:00 AM | 2,805 | 18 | 0.64 | 1.39 | |
| 4:00 AM | 2,392 | 19 | 0.79 | 1.46 | |
| 5:00 AM | 2,364 | 24 | 1.02 | 1.85 | |
| 6:00 AM | 2,894 | 13 | 0.45 | 1.00 | |
| 7:00 AM | 3,761 | 29 | 0.77 | 2.24 | |
| 8:00 AM | 4,826 | 40 | 0.83 | 3.08 | |
| 9:00 AM | 5,477 | 50 | 0.91 | 3.86 | |
| 10:00 AM | 5,964 | 74 | 1.24 | 5.71 | |
| 11:00 AM | 6,048 | 78 | 1.29 | 6.01 | |
| 12:00 PM | 6,061 | 76 | 1.25 | 5.86 | |
| 1:00 PM | 6,101 | 74 | 1.21 | 5.71 | |
| 2:00 PM | 6,021 | 76 | 1.26 | 5.86 | |
| 3:00 PM | 5,928 | 83 | 1.40 | 6.40 | |
| 4:00 PM | 6,089 | 99 | 1.63 | 7.63 | |
| 5:00 PM | 6,001 | 78 | 1.30 | 6.01 | |
| 6:00 PM | 6,023 | 67 | 1.11 | 5.17 | |
| 7:00 PM | 5,924 | 87 | 1.47 | 6.71 | |
| 8:00 PM | 5,788 | 68 | 1.17 | 5.24 | |
| 9:00 PM | 5,528 | 56 | 1.01 | 4.32 | |
| 10:00 PM | 5,250 | 55 | 1.05 | 4.24 | |
| 11:00 PM | 4,522 | 49 | 1.08 | 3.78 | |
| Total | 116,910 | 1,297 | 1.11 | 100.00 | |
Figure 3.
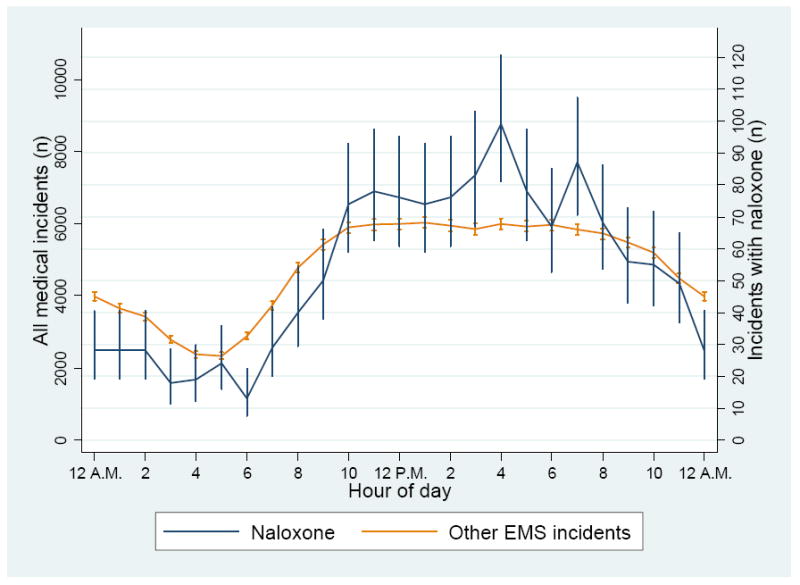
Distribution of Baltimore City Emergency Medical Services (EMS) incidents and 95% confidence intervals of naloxone administration and all other EMS incidents by hour of the day (October 2008-09).
Tests of significance of hourly, day of week, and day of month patterns of naloxone administration all showed significant improvement over the null model of no simple sinusoidal harmonic variation over time (all p < .05) (Figures 4-6). Visual inspection of observed counts and counts predicted by the simple harmonic model suggest that the latter is a reasonable fit for time of day (Figure 4) but not day of the week as there was a discontinuity between weekday and weekend numbers of naloxone administrations (Figure 5). Day of the month analysis revealed a trend, with incidents appearing highest in the first week of the month (Figure 6). However, the restricted time period did not permit conducting a seasonality test of the day of month pattern.
Figure 4.
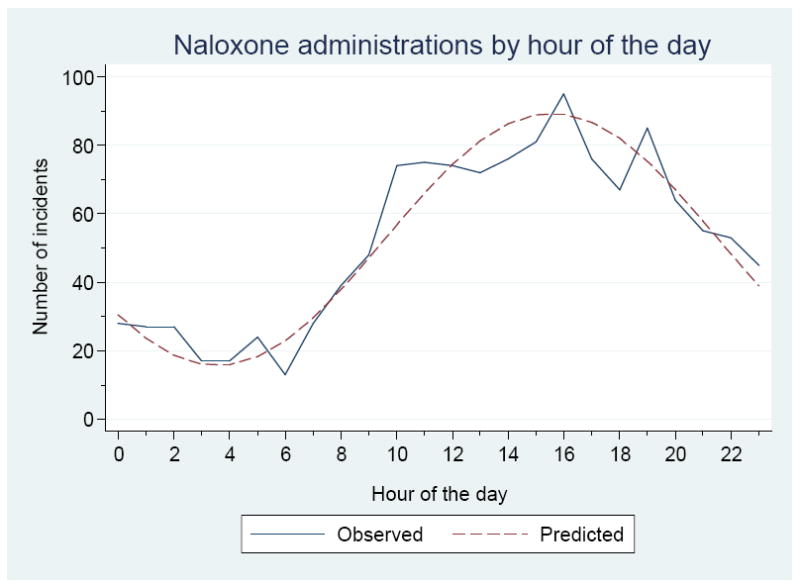
Distribution of naloxone administration by Baltimore City Emergency Medical Services by hour of the day (Walter & Elwood [1975] test of seasonality) (October 2008-09).
Figure 6.
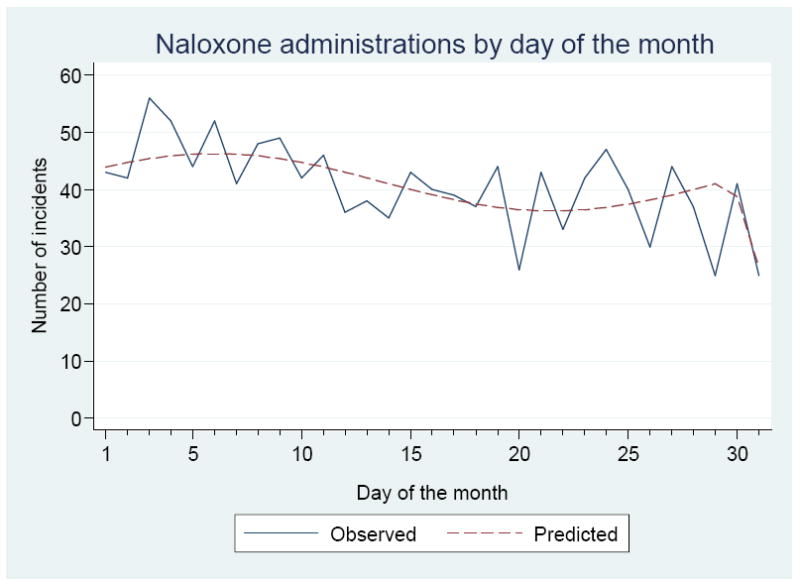
Distribution of naloxone administration by Baltimore City Emergency Medical Services by day of the month (Walter & Elwood [1975] test of seasonality) (October 2008-09).
Note: The predicted number of incidents decreases at the end of the month due to fewer of these days in the data.
Figure 5.
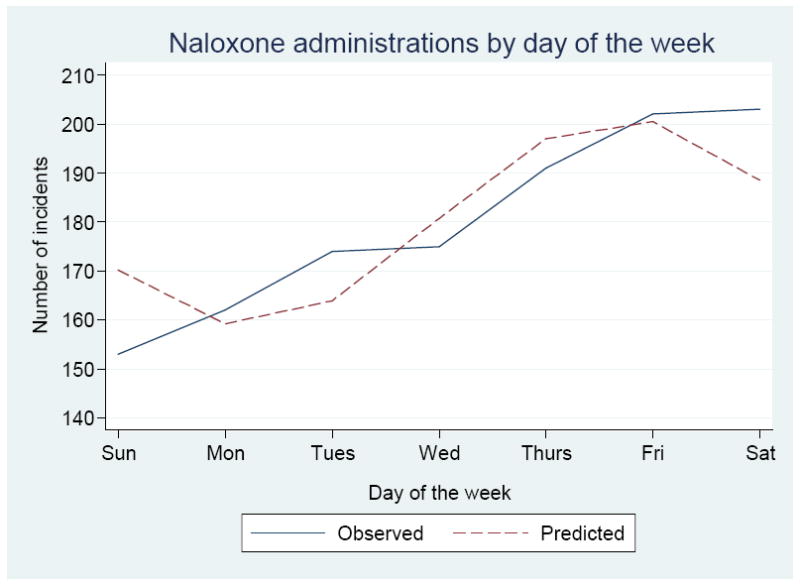
Distribution of naloxone administration by Baltimore City Emergency Medical Services by day of week (Walter & Elwood [1975] test of seasonality) (October 2008-09).
DISCUSSION
Our study findings on EMS administration of naloxone point to limitations of the data as currently collected, but nonetheless provide tentative partial support of the utility of the data as a proxy indicator of opioid overdose. The results indicate that cases of suspected opioid overdose were similar demographically to fatal overdose cases in Baltimore City in a similar time period, and that our findings on temporal patterns of EMS administration of naloxone were similar to results of prior studies. The findings suggest ways to improve the quality of EMS data on suspected opioid overdose, and demonstrate the potential utility of naloxone administration data in real-time population surveillance of opioid overdose and in informing intervention.
Comparison of demographics to the city population and to prior study findings
Our study findings suggested that EMS suspected opioid overdoses were six times higher than ME records of fatal opioid related overdoses but were demographically comparable.26 We found that 65% of suspected opioid overdose cases were male, 64% were African American, and 35% white; the median age was 46 and the mean age 44 years. Compared to the city population, suspected opioid overdose incidents were higher among males and whites, and were older than the population. ME reports on Baltimore’s fatal alcohol or drug related overdose cases in 2008 and 2009 (87%-88% of which were opioid-related) indicated demographic similarities to our findings.26 Indeed, ME reported demographics of Baltimore fatal overdose cases in 2008 were remarkably similar: 67% of fatal overdose cases were male, 64% were African American, and 36% white; the mean age was 44 years.26 The demographics of fatal overdose cases for 2009 were somewhat similar to our results: 72% were male, 61% were African American, and 39% were white, and 46 years was the mean age.26
Some of the first studies using EMS naloxone administration data to examine population demographic and temporal patterns of suspected opioid overdose were conducted by Dietze and colleagues in five states of Australia (1999-2001) and by Merchant and colleagues in Rhode Island (1997-2002).10,11 Comparing our findings on demographic patterns of naloxone administration, we found that cases in Baltimore were older than found in the Rhode Island or Australia studies (median 46, 35, and 28 years, respectively), which is consistent with Baltimore’s aging injection drug user population;and that the proportion male (65%) was within the range of the Australia and Rhode Island study findings (75%, and 53%, respectively).10,11,28
Comparison of incidence rates of suspected opioid overdose
Consistent with the greater estimated opioid abuse rates in Baltimore than Rhode Island,36 results indicated the estimated population incidence rate of suspected opioid overdose in Baltimore in 2008-9 (1.87 per 1,000 person-years) was over seven times higher than the average rate found in Rhode Island a decade prior (0.26 per 1,000 person-years).10 Baltimore, with a population approximately 40% smaller, administered naloxone over three times more often, and naloxone administration constituted 5.5 times the proportion of EMS calls in Baltimore (1.1%) as compared to Rhode Island (0.2%) in the studies’ respective time periods.10
Comparison of temporal patterns of suspected opioid overdose
Comparison of our results on temporal patterns of naloxone administration to findings from the prior Australia and Rhode Island studies indicated that suspected opioid overdoses peaked earlier in the day in Baltimore (4-5:00) and Australia (3-4:00 pm) than in Rhode Island (9:00 pm), though early morning nadir times were similar across studies.10,11 Our monthly data suggested higher levels of suspected overdose in summer months and lower levels in the fall and winter, which is somewhat consistent with the significant annual cycle found in Rhode Island (peak in August-September and trough in December-January).10
Notably, we also found evidence that suspected opioid overdoses peaked early in the month in Baltimore. This finding is consistent with US national data indicating that substance use related deaths peak early in the month; this has been explained in part by early-month federal benefit program disbursements increasing discretionary funds for purchasing substances then.37
EMS provider naloxone administration practices
Results suggest that Baltimore EMS providers most often administer naloxone intranasally or intravenously, and in cases in which overdose was not recorded by providers as the primary reason for the EMS run. In incidents with naloxone administration, less than half of call summaries were listed as overdose related, and over two-fifths were coded as medical illness or other. It is possible that overdose was a secondary condition mentioned in narrative summary records, though we were not able to confirm this. Given naloxone’s safety, it is plausible that in some cases naloxone was used in circumstances in which patients were in an altered mental state in order to facilitate providers’ assessment of patients presenting with other health problems.
Our findings suggest the need for standard EMS provider training on opioid overdose care and data collection, with consideration to safety and feasibility within the EMS care context, in order to ensure data quality and consistency across EMS providers and systems. Our findings indicated comparability between calculations of the average dosage of naloxone administered based on patient treatment records as compared to naloxone purchase order records. However, the findings on patient evaluation data suggest some inconsistencies in clinical indications of naloxone use. For example, while a low respiratory rate has been recommended as an indication for naloxone administration,38 a normal respiratory rate was recorded for almost half of patients. It should be noted, though, that the medical protocol did not specify clinical criteria for naloxone administration, making such findings difficult to interpret.
Study limitations
It is possible that inconsistencies in patient evaluation records related to naloxone use may be due to other substances ingested, or may reflect to some degree patient response to naloxone as patient evaluation data is often recorded subsequent to encounters. The findings may also reflect EMS care practices in the context of the city’s high prevalence of opioid abuse and related somatic conditions and the relative safety of naloxone. For these reasons, the study findings may have limited generalizability to other EMS systems.
Our study may have over-estimated incidence rates of suspected opioid overdose as rates were calculated based on the resident population, though we did not account for patient residence or the weekday commuter population. The number of ME reported fatal opioid related overdoses in Baltimore regardless of residence, as compared to opioid related overdoses among Baltimore residents, was 14% higher in 2008 and 21% higher in 2009.26
Other evidence suggests that our findings may represent under-estimations of opioid overdose incidence. That the ME office recorded fatal opioid related overdoses as young as one year old26 suggests our analysis was an under-count and that efforts should be made to improve EMS recording of child age, and weight for cross-validation, for inclusion of child data in future analysis.
As data were collected at the initiation of a new electronic data collection system, this may increase the likelihood of data recording errors. Errors may have been due in part to limitations in the data collection system itself and to limited provider training prior to implementation. Anecdotal evidence suggests that during the observation period, providers experienced periodic interruptions in data collection hardware and software. However, there was no indication from our analysis that such problems introduced systematic errors in the data.
Our exclusion from analysis cases with incomplete or missing data, which were over-represented by non-transported incidents, may also have affected under-estimation of suspected opioid overdose incidence. We found that 91% of incidents in our analysis were transported, similar to the 99% of ED transports in the Rhode Island study,10 but far higher than levels of ED transport of suspected opioid overdose patients found in other studies.11,13,21 EMS providers may have been unable to collect sufficient information from patients who declined transport. Also, in the Baltimore EMS system, for purposes of cost recovery, transported patients were tracked by a subcontractor, while those not transported were less likely to be included in the tracking system.
Future research needs
Further research is needed to validate EMS data related to naloxone administration as a proxy indicator of opioid overdose and refine a case definition of opioid overdose using EMS data. Linking EMS patient data to ED or ME data on toxicology results and patient outcomes would enable further validation of EMS data. Greater attention to quality control and quality assurance of EMS records would enhance the internal validity of this EMS data.
Enhancing the role of EMS in opioid overdose & public health
Given the role of EMS as a first responder and increasingly a safety net provider, an Institute of Medicine panel has advocated for EMS assuming a greater role in public health.39 Though EMS systems are in a prime position to contribute to public health, their typical lack of coordination with other health services delivery systems restricts their public health impact.39 Results from the present and prior studies suggest the potential of enhancing EMS’ role in public health by improving and utilizing EMS information systems and collaborating with other service delivery systems for local surveillance and targeted intervention on opioid abuse.
Acute care episodes among opioid dependents are a major missed opportunity for intervening on substance abuse.40 In a study of Baltimore injection drug users, talking with caregivers about drug abuse treatment at the time of their recent overdose was associated with a five-fold increase in subsequent treatment seeking.21 Yet of participants who received EMS care for that overdose, only 17% reported talking to an EMS provider then about drug treatment.21 EMS coordination with other services to facilitate opioid abusing patients’ treatment entry may not only improve their health outcomes but also reduce their high healthcare use and costs.40
The Baltimore City Health Department operates the city’s needle exchange program which, like a growing number of countries and US locales, offers take home naloxone and prescriptions to enrolled opioid dependents following naloxone administration training.41-45 This overdose prevention program has been found to improve clients’ response to overdose among themselves and others.41,42 The program, together with expanded availability of addictions treatment, has coincided with the city’s major decline in heroin related fatal overdoses in recent years.26 Yet the city’s rate of fatal overdose related to use of other opioids has increased, and opioids continue to account for the vast majority of the city’s fatal overdoses.26 This underscores the critical importance in Baltimore and other areas affected by epidemic opioid abuse of promoting EMS’ coordination with other services to identify opioid abusers and promote their increased access to opioid overdose treatment and prevention services.
Conclusion
Consistencies between temporal and demographic patterns in this EMS naloxone administration data and prior study and medical examiner findings provide some limited evidence to support the validity of the EMS data. The findings underscore the need for further assessment and enhancement of the validity of EMS records as a proxy indicator of opioid overdose incidence. Such efforts would enable a potential role of EMS in addressing the country’s epidemic opioid abuse and overdose by enhancing real time, local surveillance and informing targeted preventive intervention.
Acknowledgments
The study was supported by National Institute on Drug Abuse grants R01 DA019413 and R34 DA034314 (Amy Knowlton, PI), F31 DA026763 (Brian Weir), and by a grant from the CDC Johns Hopkins Center for Public Health Preparedness (Jonathon Links, PI). We thank the Baltimore City Fire Department Emergency Medical Services providers for data collection.
Footnotes
An earlier version was presented at the Addiction Health Services Research Conference, Lexington, KY, October 26, 2010.
Conflicts of interest: None.
References
- 1.Substance Abuse and Mental Health Services Administration (SAMHSA), Office of Applied Studies. National Survey on Drug Use and Health Report: Trends in Nonmedical Use of Prescription Pain Relievers: 2002 to 2007. 2009 Feb 5; [Google Scholar]
- 2.Kochanek KD, Xu J, Murphy SL, et al. National vital statistics reports. 3. Vol. 60. Hyattsville, MD: National Center for Health Statistics; 2012. Deaths: Final Data for 2009. [PubMed] [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration (SAMHSA), Office of Applied Studies. Results from the 2007 National Survey on Drug Use and Health: National findings. 2008 NSDUH Series H-34, DHHS Publication No. SMA 08-4343. [Google Scholar]
- 4.Smyth B, Hoffman V, Fan J, Hser YI. Years of potential life lost among heroin addicts 33 years after treatment. Prev Med. 2007;44(4):369–374. doi: 10.1016/j.ypmed.2006.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coben JH, Davis SM, Furbee PM, Sikora RD, Tillotson RD, Bossarte RM. Hospitalizations for poisoning by prescription opioids, sedatives, and tranquilizers. Am J Prev Med. 2010;38(5):517–524. doi: 10.1016/j.amepre.2010.01.022. [DOI] [PubMed] [Google Scholar]
- 6.Hall AJ, Logan JE, Toblin RL, Kaplan JA, Kraner JC, Bixler D, Crosby AE, Paulozzi LJ. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300(22):2613–2620. doi: 10.1001/jama.2008.802. [DOI] [PubMed] [Google Scholar]
- 7.Schneider MF, Bailey JE, Cicero TJ, Dart RC, Inciardi JA, Parrino M, Munoz A. Integrating nine prescription opioid analgesics and/or four signal detection systems to summarize statewide prescription drug abuse in the United States in 2007. Pharmacoepidemiol Drug Saf. 2009;18(9):778–790. doi: 10.1002/pds.1780. [DOI] [PubMed] [Google Scholar]
- 8.Cepeda MS, Fife D, Chow W, Mastrogiovanni G, Henderson SC. Assessing opioid shopping behaviour: a large cohort study from a medication dispensing database in the US. Drug Saf. 2012;35(4):325–34. doi: 10.2165/11596600-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 9.Substance Abuse and Mental Health Services Administration (SAMHSA), Office of Applied Studies. Drug Abuse Warning Network 2006: National Estimates of Drug-Related Emergency Department Visits. 2008 DAWN Series D-30, DHHS Publication No. (SMA) 08-4339. [Google Scholar]
- 10.Merchant RC, Schwartzapfel BL, Wolf FA, Li W, Carlson L, Rich JD. Demographic, geographic, and temporal patterns of ambulance runs for suspected opiate overdose in Rhode Island, 1997-2002. Subst Use Misuse. 2006;41(9):1209–1226. doi: 10.1080/10826080600751898. [DOI] [PubMed] [Google Scholar]
- 11.Dietze P, Fry C, Sunjic S, Bammer G, Zador D, Jolley D, Rumbold G. Using ambulance attendances to recruit people who have experienced non-fatal heroin overdose. Drug Alcohol Depend. 2002;67(1):99–103. doi: 10.1016/s0376-8716(02)00009-1. [DOI] [PubMed] [Google Scholar]
- 12.Seidler D, Schmeiser-Rieder A, Schlarp O, Laggner AN. Heroin and opiate emergencies in Vienna: analysis at the municipal ambulance service. J Clin Epidemiol. 2000;53(7):734–741. doi: 10.1016/s0895-4356(99)00216-4. [DOI] [PubMed] [Google Scholar]
- 13.Wampler DA, Molina DK, McManus J, Laws P, Manifold CA. No deaths associated with patient refusal of transport after naloxone-reversed opioid overdose. Prehosp Emerg Care. 2011;15(3):320–324. doi: 10.3109/10903127.2011.569854. [DOI] [PubMed] [Google Scholar]
- 14.Buajordet I, Naess AC, Jacobsen D, Brors O. Adverse events after naloxone treatment of episodes of suspected acute opioid overdose. Eur J Emerg Med. 2004;11(1):19–23. doi: 10.1097/00063110-200402000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Vilke GM, Buchanan J, Dunford JV, Chan TC. Are heroin overdose deaths related to patient release after prehospital treatment with naloxone? Prehosp Emerg Care. 1999;3(3):183–186. doi: 10.1080/10903129908958933. [DOI] [PubMed] [Google Scholar]
- 16.Coffin PO, Tracy M, Bucciarelli A, Ompad D, Vlahov D, Galea S. Identifying injection drug users at risk of nonfatal overdose. Acad Emerg Med. 2007;14(7):616–623. doi: 10.1197/j.aem.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 17.Dietze P, Jolley D, Cvetkovski S, Cantwell K, Jacobs I, Indig D. Characteristics of non-fatal opioid overdoses attended by ambulance services in Australia. Aust N Z J Public Health. 2004;28(6):569–575. doi: 10.1111/j.1467-842x.2004.tb00049.x. [DOI] [PubMed] [Google Scholar]
- 18.Kerr D, Kelly AM, Dietze P, Jolley D, Barger B. Randomized controlled trial comparing the effectiveness and safety of intranasal and intramuscular naloxone for the treatment of suspected heroin overdose. Addiction. 2009;104(12):2067–2074. doi: 10.1111/j.1360-0443.2009.02724.x. [DOI] [PubMed] [Google Scholar]
- 19.Evans JL, Tsui JI, Hahn JA, Davidson PJ, Lum PJ, Page K. Mortality among young injection drug users in San Francisco: a 10-year follow-up of the UFO study. Am J Epidemiol. 2012 Feb 15;175(4):302–8. doi: 10.1093/aje/kwr318. Epub 2012 Jan 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gilson AM. The concept of addiction in law and regulatory policy related to pain management: a critical review. Clin J Pain. 2010 Jan;26(1):70–7. doi: 10.1097/AJP.0b013e3181b12a2d. [DOI] [PubMed] [Google Scholar]
- 21.Pollini RA, McCall L, Mehta SH, Vlahov D, Strathdee SA. Non-fatal overdose and subsequent drug treatment among injection drug users. Drug Alcohol Depend. 2006;83(2):104–110. doi: 10.1016/j.drugalcdep.2005.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Togia A, Sergentanis TN, Sindos M, Ntourakis D, Doumouchtsis E, Sergentanis IN, Bachtis C, Pyrros D, Papaefstathiou N. Drug abuse-related emergency calls: a metropolis-wide study. Prehosp Disaster Med. 2008;23(1):36–40. doi: 10.1017/s1049023x00005537. [DOI] [PubMed] [Google Scholar]
- 23.Tracy M, Piper TM, Ompad D, Bucciarelli A, Coffin PO, Vlahov D, Galea S. Circumstances of witnessed drug overdose in New York City: implications for intervention. Drug Alcohol Depend. 2005;79(2):181–190. doi: 10.1016/j.drugalcdep.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 24.Baca CT, Grant KJ. What heroin users tell us about overdose. J Addict Dis. 2007;26(4):63–68. doi: 10.1300/J069v26n04_08. [DOI] [PubMed] [Google Scholar]
- 25.Maryland Institute for Emergency Medical Services Systems. The Maryland Medical Protocols for Emergency Medical Services Providers. MIEMSS; 2008. p. 348. http://www.miemss.org/home/LinkClick.aspx?fileticket=PcFzAVnOA4M%3d&tabid=106&mid=537. [Google Scholar]
- 26.Office of Epidemiology and Planning. Intoxication Deaths Associated with Drugs of Abuse or Alcohol. 2009 Final Report. Baltimore City, Maryland: Baltimore City Health Department, and Baltimore Substance Abuse Systems; Jul, 2011. http://www.baltimorehealth.org/info/DOA%20Final%20Report%202009--FINAL.pdf. [Google Scholar]
- 27.Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Drug Abuse Warning Network:Area profiles of drug-related mortality. 2008 DHHS Publication No. (SMA). SMA10-4473. [Google Scholar]
- 28.Yacoubian GS, Hsu M, Wish ED. Estimating the Need for Substance Abuse Treatment in Maryland: An Update of Reuter et al (1998) College Park, MD: Center for Substance Abuse Research (CESAR), University of Maryland; 2002. [Google Scholar]
- 29.Friedman SR, Tempalski B, Cooper H, Perlis T, Keem M, Friedman R, Flom PL. Estimating numbers of injecting drug users in metropolitan areas for structural analyses of community vulnerability and for assessing relative degrees of service provision for injecting drug users. J Urban Health. 2004;81(3):377–400. doi: 10.1093/jurban/jth125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maryland Institute for Emergency Medical Services Systems. EMAIS User Manual 3.0. Baltimore, MD: MIEMSS; p. 21. http://www.miemss.org/home/LinkClick.aspx?fileticket=AZFED0if7jQ%3d&tabid=54. [Google Scholar]
- 31.U.S. Census Bureau. Preliminary Annual Estimates of the Resident Population for the United States, Regions, States, and Puerto Rico: April 1, 2000 to July 1, 2010 (NST-PEST2010-01) http://www.census.gov/popest/eval-estimates/eval-est2010.html.
- 32.Microsoft Corporation. Microsoft Office Access 11.5. 2003;11.5 [Google Scholar]
- 33.IBM Corporation. SPSS 11.0. New York: [Google Scholar]
- 34.StataCorp. Stata Statistical Software: Release 10.1. College Station, TX: [Google Scholar]
- 35.Edwards JH. The recognition and estimation of cyclic trends. Ann Hum Genet. 1961;25:83–87. doi: 10.1111/j.1469-1809.1961.tb01501.x. [DOI] [PubMed] [Google Scholar]
- 36.Substance Abuse and Mental Health Services Administration. State Estimates of Substance Use and Mental Disorders from the 2008-2009 National Surveys on Drug Use and Health. 2011 NSDUH Series H-40;DHHS Publication No. (SMA) 11-4641. [PubMed] [Google Scholar]
- 37.Phillips DP, Christenfeld N, Ryan NM. An increase in the number of deaths in the United States in the first week of the month--an association with substance abuse and other causes of death. N Engl J Med. 1999;341(2):93–98. doi: 10.1056/NEJM199907083410206. [DOI] [PubMed] [Google Scholar]
- 38.Hoffman JR, Schriger DL, Luo JS. The empiric use of naloxone in patients with altered mental status: a reappraisal. Ann Emerg Med. 1991;20(3):246–252. doi: 10.1016/s0196-0644(05)80933-3. [DOI] [PubMed] [Google Scholar]
- 39.Institute of Medicine (IOM) Emergency Medical Services: At the Crossroads. Washington, D.C.: The National Academies Press; 2007. [Google Scholar]
- 40.Barnett PG, Masson CL, Sorensen JL, Wong W, Hall S. Linking opioid-dependent hospital patients to drug treatment: Health care use and costs 6 months after randomization. Addiction. 2006;101(12):1797–1804. doi: 10.1111/j.1360-0443.2006.01636.x. [DOI] [PubMed] [Google Scholar]
- 41.Tobin KE, Sherman SG, Beilenson P, Welsh C, Latkin CA. Evaluation of the Staying Alive programme: training injection drug users to properly administer naloxone and save lives. Int J Drug Policy. 2009;20(2):131–136. doi: 10.1016/j.drugpo.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 42.Sherman SG, Gann DS, Tobin KE, Latkin CA, Welsh C, Bielenson P. “The life they save may be mine”: diffusion of overdose prevention information from a city sponsored programme. Int J Drug Policy. 2009;20(2):137–142. doi: 10.1016/j.drugpo.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 43.Baca CT, Grant KJ. Take-home naloxone to reduce heroin death. Addiction. 2005;100(12):1823–31. doi: 10.1111/j.1360-0443.2005.01259.x. [DOI] [PubMed] [Google Scholar]
- 44.Enteen L, Bauer J, McLean R, Wheeler E, Huriaux E, Kral AH, Bamberger JD. Overdose prevention and naloxone prescription for opioid users in San Francisco. J Urban Health. 2010;87(6):931–41. doi: 10.1007/s11524-010-9495-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.George S, Boulay S, Begley D. ‘I saved a life’: a heroin addict’s reflections on managing an overdose using ‘take home naloxone’. BMJ Case Rep. 2010 Sep 7; doi: 10.1136/bcr.05.2010.2986. [DOI] [PMC free article] [PubMed] [Google Scholar]


