Abstract
Introduction:
Few studies have examined the transitions of smokers in the general population through multiple periods of daily, occasional smoking, or abstinence over time. Transitions from daily to occasional smoking are particularly of interest as these may be steps toward cessation.
Methods:
The Ontario Tobacco Survey panel study followed 4,355 baseline smokers, semiannually for up to 3 years. Probabilities of all possible changes in smoking status more than 6 months were estimated using 13,000 repeated measures observations generated from sets of 3 consecutive interviews (n = 9,932 daily smokers, 1,245 occasion smokers, and 1,823 abstinent for at least 30 days, at Time 1).
Results:
For initial daily smokers, an estimated 83% remained daily smokers more than 2 follow-ups. The majority of those who had been abstinent for 30 days at 1 interview, were also former smokers at the following interview. In contrast, occasional smoking status was unstable and future smoking status was dependent upon smoking history and subjective dependence. Among daily smokers who became occasional smokers 6 months later, an estimated 20% became a former smoker, at the next interview, but 50% returned to daily smoking. Daily, turned occasional smokers who rebounded back to daily smoking were more likely to describe themselves as addicted at Time 1. Continuing occasional smokers were somewhat less likely to intend to quit, or have tried, despite considering themselves less addicted.
Conclusions:
Reducing to occasional smoking can be a stepping stone toward cessation but entails a greater risk of return to daily smoking, compared with complete abstinence.
INTRODUCTION
Smoking cessation is a complex process rather than a discrete event (Pierce, Farkas, & Gilpin, 1998; Pierce, Gilpin, et al., 1998) and many smokers move in and out of current smoking status (U.S. Department of Health and Human Services, 2000). While many studies have assessed the predictors of making and succeeding at quit attempts for defined periods of time (Hymowitz et al., 1997; Pierce, Gilpin, et al., 1998; U.S. Department of Health and Human Services, 2000), few have examined the transitions of smokers through multiple stages of daily smoking, occasional smoking, or abstinence (Hyland et al., 2006; Tindle & Shiffman, 2011).
Studying the outcome of movement from daily to occasional smoking is of interest as this may be a step toward future cessation. Hyland et al. (2006) found that nondaily smokers were more likely to quit smoking; while, Tindle and Shiffman (2011), found that occasional smokers, both converted from daily smokers and continuous occasional smokers, were unsuccessful in their quit attempts, despite low scores on measures of dependence. Persistent occasional smoking is also a public health concern. In the United States, up to 33% of smokers now smoke less than daily (Shiffman, 2009; Tindle & Shiffman, 2011). While there is limited evidence that reduction from daily smoking to maintained occasional smoking may decrease mortality risk (Gerber, Myers, & Goldbourt, 2012); the mortality reduction associated with cessation is clearly demonstrated and occasional smokers continue to have excess mortality relative to nonsmokers (Doll, Peto, Boreham, & Sutherland, 2004). Ongoing occasional smoking is, therefore, not seen as a desirable goal for tobacco control (Hughes & Carpenter, 2006).
Most studies of stability and variability in smoking behavior outside clinical settings are limited by the use of cross-sectional data, with few contributions found from follow-ups in panel studies (Herd & Borland, 2009; Hyland et al., 2006). Since most quit attempts end before 30 days, relatively frequent follow-ups are needed to capture the dynamics of the smoking cessation process. The present study examines the dynamics of smoking using a population-based survey with numerous follow-ups (up to seven interviews per person) and relatively short follow-up intervals (6 months).
METHODS
Data were from the Ontario Tobacco Survey (OTS) panel study of smokers (Diemert, Victor, & Bondy, 2010a; Mecredy, Chaiton, & Bondy, 2011). Briefly, the OTS is a representative sample of adults, interviewed by telephone, who had smoked in the past 6 months at recruitment in 2005 through 2008. Participants completed up to six semiannual follow-up interviews. Technical reports presenting the study design, questionnaires, demographic characteristics, and smoking behavior of the overall OTS samples are available in open access (Bondy et al., 2006; Diemert et al., 2010a, 2010b; Mecredy et al., 2011).
Findings presented here are based on 4,352 smokers (18+ years), who had smoked 100+ cigarettes in their lifetime and uses a subset of the OTS observations and a repeated measures design. The present analyses used complete smoking status information over any three consecutive interviews (triads). Complete data were available for 13,000 sets out of a maximum possible 19,582 triads (N of observations of initial daily, occasional, and former smokers were 9,932, 1,245, and 1,823, respectively). Table 1 presents the demographic characteristics, smoking behavior and history, reported quit intentions, and past use of supports to quit for panel study participants, by smoking status at Time 1 defined in the present analysis.
Table 1.
Characteristics of Participantsa in Repeated Measures Analysis of Data From the Ontario Tobacco Study to Examine Probabilities of Changes in Smoking Status Over Three Consecutive Semiannual Interviews
| Smoking statusb reported at Time 1 of three complete interviews (numbers of valid repeated measures observations) | |||
|---|---|---|---|
| Daily | Occasional | Former | |
| N of repeated measures observations (triads)a | 9,932 | 1,245 | 1,823 |
| N cross-sectional observations (individuals)a | 2,802 | 387 | 263 |
| Age | (n = 9,874) | (n = 1,241) | (n = 1,807) |
| Mean | 44.3 | 38.7 | 41.8 |
| Sample SE | 0.38 | 0.86 | 0.76 |
| Sex (%)c | (n = 9,932) | (n = 1,245) | (n = 1,823) |
| Female | 47.8 | 44.0 | 45.2 |
| Male | 52.2 | 56.0 | 54.8 |
| Education (%) | (n = 9,915) | (n = 1,243) | (n = 1,820) |
| High school or less | 47.1 | 30.3 | 31.5 |
| More than high school | 52.9 | 69.7 | 68.5 |
| Marital status (%) | (n = 9,888) | (n = 1,238) | (n = 1,816) |
| Single | 36.9 | 43.1 | 29.7 |
| Married/common law | 63.1 | 56.9 | 70.3 |
| Ever smoked daily (%) | (n = 9,332) | (n = 1,244) | (n = 1,822) |
| No | 0.0 | 17.2 | 8.7 |
| Yes | 100.0 | 82.8 | 91.3 |
| Time since last cigarette (%) | (n = 9,932) | (n = 1,245) | (n = 1,823) |
| Within past week | 100.0 | 64.9 | 0.9 |
| Within past month | 0.0 | 35.1 | 1.0 |
| Within 6 months | 0.0 | 0.0 | 55.3 |
| >since months prior | 0.0 | 0.0 | 42.8 |
| Number of days smoked (prev. 30 days) | (n = 9,932) | (n = 1,245) | N/A |
| Mean | 29.3 | 10.1 | – |
| Sample SE | 0.05 | 0.40 | – |
| Number of cigarettes per day | (n = 9,911) | (n = 1,234) | N/A |
| Mean | 15.6 | 4.8 | – |
| Sample SE | 0.23 | 0.24 | – |
| Heaviness of smoking index | (n = 9,868) | N/A | N/A |
| Mean | 2.6 | – | – |
| Sample SE | 0.04 | – | – |
| Weekly pattern of reported smoking (%)d | (n = 9,930) | (n = 1,245) | N/A |
| Smoked weekends and weekdays | 99.8 | 67.1 | – |
| Weekday or weekend only smokers | 0.2 | 32.9 | – |
| Perceived addiction (%) | (n = 9,915) | (n = 1,230) | (n = 1,791) |
| Less addicted (“somewhat” or “not at all”) | 30.0 | 87.4 | 94.0 |
| Very addicted | 70.0 | 12.6 | 6.0 |
| Prior number of quit attempts (%) | (n = 9,274) | (n = 1,173) | (n = 1,774) |
| None | 6.4 | 9.7 | 1.4 |
| One or more | 93.6 | 90.3 | 98.6 |
| Quit intention (%) | (n = 9,931) | (n = 1,035) | N/A |
| No (incl. don’t know) | 63.1 | 46.0 | – |
| Yes | 36.9 | 54.0 | – |
| Quitting confidence (%) | (n = 9,929) | (n = 1,035) | N/A |
| Less or uncertain confidence (incl. don’t know) | 46.2 | 9.1 | – |
| Fairly or very confident | 53.8 | 90.9 | – |
| Smoking in the home (%) | (n = 9,915) | (n = 1,240) | (n = 1,816) |
| Little or no exposure (less than monthly) | 51.9 | 81.8 | 88.8 |
| Regular exposure (at least monthly) | 48.1 | 18.2 | 11.2 |
| Ever prior use of pharmacotherapy (%) | (n = 9,791) | (n = 1,217) | (n = 1,774) |
| No | 38.9 | 66.8 | 54.5 |
| Yes | 61.1 | 33.2 | 45.5 |
| Ever prior use of behavioral supports (%) | (n = 9,704) | (n = 1,213) | (n = 1,757) |
| No | 71.8 | 77.4 | 76.9 |
| Yes | 28.2 | 22.6 | 23.1 |
Note. SE = standard error of the mean. Demographic characteristics, smoking status, and factors associated with cessation as reported at the first of three interviews (Time 1) by smoking status (at Time 1).
aThis analysis uses a repeated measures approach where one observation is a set of three consecutive complete interviews over the course of the Ontario Tobacco Survey (OTS) panel study (Waves 1–6). The analysis used 13,000 observations reflecting data from 4,352 unique participants in the OTS. All OTS panel study participants had smoked within 6 months at the baseline interview. This analysis was restricted to those who smoked 100+ lifetime cigarettes at baseline. Numbers in parentheses are nonmissing valid responses.
bSmoking status was defined as follows: Daily or occasional smokers had smoked within the past 30 days and described their usual behavior and smoking either daily (daily or almost every day) or occasional. Former smokers were required to have not smoked in the previous 30 days at the time of interview.
cPercentage estimates may not sum to 100% due to rounding.
dSee Edwards et al. (2010) for derivation. Patterned smoking is very rare for daily smokers and reflects very small numbers of daily smokers, reporting smoking on greater than 28 days in the past 30 also reported no smoking on either weekends or weekdays on separate questions within the structured interview.
Source: Ontario Tobacco Survey longitudinal data, baseline to follow-up 6.
At each interview, respondents were asked if they smoked “daily, almost daily, occasionally, or not at all.” Those who had not smoked one cigarette within 30 days of each interview were classified as former smokers (National Advisory Group on Monitoring and Evaluation, 2006). Where smoking status was consistent over consecutive interviews, self-reported changes in smoking status or consumption behavior (periods of cessation, smoking more or less) since the last interview were examined. Participant demographic and smoking-related measures (see Table 1) were obtained from the baseline interview. Measures reflecting cumulative lifetime history (e.g., ever smoked daily or ever use of supports for cessation) were derived from cumulative responses in the OTS baseline up to the Time 1 interview as defined for this analysis. Measures considered in this analysis include self-reported smoking status and history, time to first cigarette and number of cigarettes usually smoked per day (where applicable), time period since last cigarette (as applicable), intention to quit, confidence in one’s ability to quit altogether, and history of use of pharmacological and nonpharmacological supports for cessation (Bondy et al., 2010; Diemert, Bondy, Brown, & Manske, in press; Ip et al., 2012). A derived measure for pattern of smoking primarily on weekends, weekdays, or both was included as previously described (Edwards, Bondy, Kowgier, McDonald, & Cohen, 2010).
The first goal of analysis was to estimate the conditional probabilities of staying in the same smoking status, or moving to another smoking status category, over each of two sequential semiannual follow-up interviews. Specifically, we estimated the percentage of participants in each smoking status at Time 2, conditional on their initial smoking status at Time 1, and then the percentage of participants in each category at Time 3, conditional on their combined status pattern at Time 1 and Time 2. Point estimates for these transition probabilities were population-weighted. Confidence intervals for percentages were obtained using Taylor series methods for survey data, which accounted for the regionally stratified sampling design, weighting, and repeated measures using SAS v. 9.2.
Further analysis focused on comparing and contrasting the demographic and smoking-related characteristics of participants who displayed selected combinations of one-step and two-step changes (or consistency) in smoking status, with a focus on participants who reported being occasional smokers and in whom both recent past smoking status, and smoking status at a following interview were observed.
RESULTS
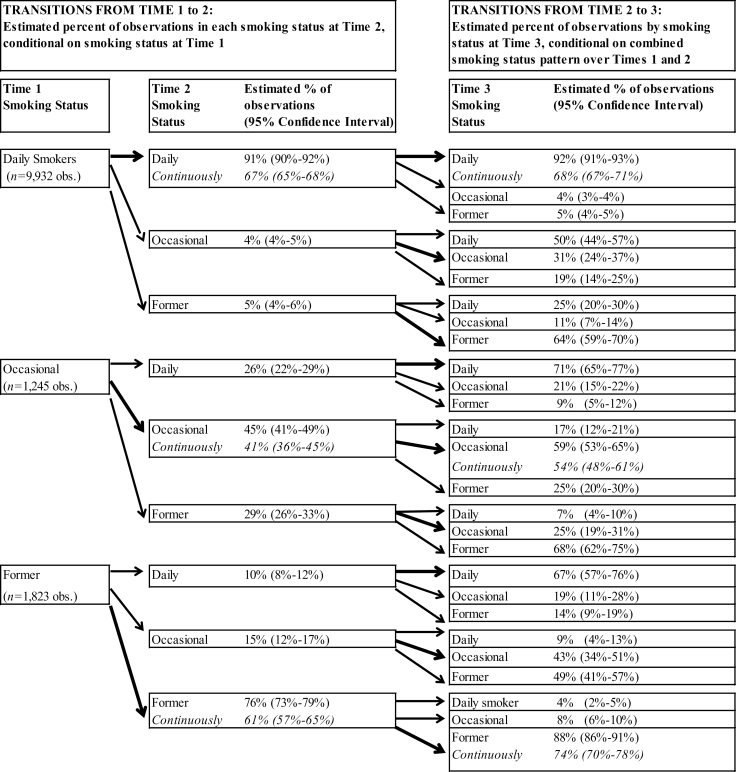
Figure 1 presents a complete set of estimated transition probabilities showing movement between smoking status categories, from one interview to the next, over any 1-year period (three consecutive interviews). Where smoking status remained the same, the second proportion reflects respondents who stayed in the same category and reported no increased or decreased consumption since the last interview. In Figure 1, the probability of being in a specific smoking status at Time 2 is presented, conditional on smoking status at Time 1. Probabilities are expressed as percentages and probabilities of transition from Time 1 to Time 2 sum to 100% within categories of smoking status at Time 1. Estimated probabilities from Time 2 to Time 3 are conditional on prior states and sum to 100% within each unique combination of Time 1 and Time 2 smoking status. The percentage of participants following a specific path from Time 1 to Time 3 may be estimated using the product of conditional probabilities. For example, the percentage of daily smokers, at Time 1, who remain daily smokers over two interviews is 0.91 × 0.92 = 0.837 or approximately 84%.
Figure 1.
Estimated probabilities* of the same (solid arrows) or different (dashed arrows) smoking status over consecutive interviews. Repeated measures analysis of 13,000 triads of consecutive interviews in a population-representative sample of smokers in the Ontario Tobacco Survey smokers cohort.
*Conditional probabilities as percentages. Probabilities of transition from Time 1 to Time 2 sum to 100% by smoking status at Time 1. Values in italics are the percentage of participants who reported unchanged consumption over the entire 6-month period. Estimated probabilities from Time 2 to Time 3 are conditional, and sum to 100% within each unique combination of Time 1 and Time 2 status. The percentage of participants following a specific path from Time 1 to Time 3 may be estimated using the product of conditional probabilities. For example, the percentage of daily smokers, at Time 1, who remain daily smokers over two interviews is 0.91 × 0.92 = 0.837 or approximately 84%. Percentages may not add to 100 due to rounding.
Daily smoking was the most persistent status with 91% of daily smokers at Time 1 being daily smokers at Time 2. When all daily smokers at Time 2 are considered, the probability of remaining a daily smoker from Time 2 to Time 3 varied according to status at Time 1 but was always higher than two thirds. Similarly, all groups of former smokers (i.e., former smokers at either Time 1 or Time 2) had an estimated greater than 60% probability of reporting again, that they had been abstinent for at least 30 days at the respective following interview, regardless of their initial status at Time 1. Newly former smokers at Time 2 (occasional or daily smokers at Time 1, but abstinent for at least 30 days at the Time 2 interview), had roughly the same chance of being a former smoker again at Time 3, regardless of whether they had been a daily or occasional smokers at Time 1 (64% and 68%, respectively), but this rose to an 88% chance of remaining a former smoker at Time 3 for those who had been nonsmokers at both Time 1 and Time 2.
Occasional smokers were the least stable groups with only 45% of those who were occasional smokers at Time 1 reporting the same smoking status at Time 2, and just 27% of initial occasional smokers continuing as such over two consecutive follow-ups. (This can be estimated from the conditional probabilities in Figure 1 as 0.45 × 0.59 = 0.2655 or roughly 27%.) The smoking status into which occasional smokers at Time 2 were most likely to move was conditional on their smoking behavior in the recent past (i.e., status at Time 1). Continuing occasional smokers (those who reported being an occasional smoker over two consecutive interviews) had an estimated conditional probability of 59% of remaining an occasional smoker at Time 3, and otherwise had slightly better chances of becoming a former smoker (25%) than becoming a daily smoker (17%) at the third interview.
Figure 1 also allows one to follow respondents who switched from daily smokers at Time 1 to occasional smokers at Time 2. This group had a 50% chance of returning to daily smoking, at Time 3 versus a 19% probability of being a former smoker at Time 3. Their 19% chance of being abstinent at the subsequent interview was significantly higher than the rate of abstinence at Time 3 (5%) for respondents who were daily smokers at both Time 1 and Time 2. When two groups of daily smokers (Time 1) who changed smoking status at Time 2 are contrasted, namely from daily to occasional smoker versus daily to former smoker, those who quit completely were half as likely to rebound to daily smoking, and 3 times as likely to be abstinent at the following interview.
Table 2 provides a more detailed description of the characteristics of selected subgroups based on the selected combination of smoking status at Time 1 and Time 2. This table allows direct comparison of the characteristics of initially daily smokers who switched to former smokers or to occasional smokers at the middle interview. It also allows a direct comparison of two groups of occasional smokers at Time 2, namely those who were recent switchers from daily to occasional smoker and those who were continuing occasional smokers over Time 1 and Time 2. All three of these groups were similar in terms of demographic characteristics and there were no significant differences in demographic characteristic between occasional smokers who had recently reduced intake or were continuing occasional smokers (all pairwise contrast p values > .10). By definition, these groups differed at Time 1 on consumption-based measures of smoking and dependence. However, smokers who switched from daily to occasional were significantly different, at Time 1, from continuing occasional smokers on subjective measures of dependence and past quitting behaviors. Continuing occasional smokers described themselves as less addicted, and were more confident they could quit completely if they wished, but were also less likely to have expressed an intention to quit altogether, or have tried to quit, or used supports for cessation (p < .001 for each of these contrasts). Overall, daily smokers at Time 1 who either switched to occasional smokers or became former smokers at Time 2 were similar at Time 1 in terms of consumption-based and subjective measures of dependence and past quit attempts, and differed in the same ways when contrasted with continuing occasional smokers.
Table 2.
Demographic Characteristics, Smoking Behavior, and History (at Time 1 Interview) for Selected Groups of Observationsa Defined by Combined Time 1 and Time 2 Smoking Statusb
| Switchers from daily to occasional (from Time 1 to Time 2) | Continuing occasional smokers (Time 1 and Time 2) | Switchers from daily to former (from Time 1 to Time 2) | |
|---|---|---|---|
| N of repeated measures observations (triads)a | 382 | 537 | 512 |
| N cross-sectional observations (individuals)a | 360 | 293 | 491 |
| Age | (n = 381) | (n = 536) | (n = 509) |
| Mean | 40.2 | 38.0 | 43.4 |
| Sample SE | 1.40 | 1.22 | 0.90 |
| Sex (%)c | (n = 382) | (n = 537) | (n = 512) |
| Female | 43.3 | 40.9 | 49.2 |
| Male | 56.7 | 59.1 | 50.8 |
| Education (%) | (n = 381) | (n = 536) | (n = 510) |
| High school or less | 37.7 | 29.0 | 41.4 |
| More than high school | 62.3 | 71.0 | 58.6 |
| Marital status (%) | (n = 380) | (n = 534) | (n = 510) |
| Single | 48.4 | 41.8 | 32.7 |
| Married/common law | 51.6 | 58.2 | 67.3 |
| Ever smoked daily (%) | (n = 382) | (n = 537) | (n = 512) |
| No | 0.0 | 24.9 | 0.0 |
| Yes | 100.0 | 75.1 | 100.0 |
| Time since last cigarette (%) | (n = 382) | (n = 537) | (n = 512) |
| Within past week | 100.0 | 65.7 | 100.0 |
| Within past month | 0.0 | 34.3 | 0.0 |
| Within 6 months | 0.0 | 0.0 | 0.0 |
| >since months prior | 0.0 | 0.0 | 0.0 |
| Number of days smoked (prev. 30 days) | (n = 382) | (n = 537) | (n = 512) |
| Mean | 27.1 | 8.7 | 28.5 |
| Sample SE | 0.53 | 0.54 | 0.25 |
| Number of cigarettes per day | (n = 382) | (n = 531) | (n = 511) |
| Mean | 9.9 | 3.5 | 12.9 |
| Sample SE | 0.06 | 0.24 | 0.55 |
| Heaviness of smoking index | (n = 372) | N/A | (n = 509) |
| Mean | 1.5 | – | 2.0 |
| Sample SE | 0.12 | – | 0.09 |
| Weekly pattern of reported smoking (%) | (n = 382) | (n = 537) | (n = 512) |
| Smoked weekends and weekdays | 99.6 | 64.1 | 98.5 |
| Weekday or weekend smokers | 0.4 | 35.9 | 1.5 |
| Perceived addiction (%) | (n = 379) | (n = 531) | (n = 512) |
| Less addicted (“somewhat” or “not at all”) | 53.2 | 92.1 | 42.0 |
| Very addicted | 46.8 | 7.9 | 58.0 |
| Prior number of quit attempts (%) | (n = 365) | (n = 491) | (n = 491) |
| None | 5.3 | 11.9 | 3.5 |
| One or more | 94.7 | 88.1 | 96.5 |
| Quit intention (%) | (n = 382) | (n = 497) | (n = 512) |
| No (incl. don’t know) | 38.8 | 54.9 | 33.4 |
| Yes | 61.2 | 45.1 | 66.6 |
| Quitting confidence (%) | (n = 382) | (n = 497) | (n = 512) |
| Less or uncertain confidence (incl. don’t know) | 25.0 | 7.6 | 25.1 |
| Fairly or very confident | 75.0 | 92.4 | 74.9 |
| Smoking in the home (%) | (n = 380) | (n = 536) | (n = 511) |
| Little or no exposure (less than monthly) | 71.5 | 83.2 | 63.1 |
| Regular exposure (at least monthly) | 28.5 | 16.8 | 36.9 |
| Ever prior use of pharmacotherapy (%) | (n = 372) | (n = 522) | (n = 505) |
| No | 45.5 | 76.3 | 36.4 |
| Yes | 54.5 | 23.7 | 63.6 |
| Ever prior use of behavioral supports (%) | (n = 370) | (n = 522) | (n = 500) |
| No | 64.9 | 81.8 | 70.7 |
| Yes | 35.1 | 18.2 | 29.3 |
Note. SE = standard error of the mean.
aThis analysis uses a repeated measures approach where one observation is a set of three consecutive complete interviews over the course of the Ontario Tobacco Survey (OTS) panel study (Waves 1–6). The analysis used 13,000 observations reflecting data from 4,352 unique participants in the OTS. All OTS panel study participants had smoked within 6 months at the baseline interview. This analysis was restricted to those who smoked 100+ lifetime cigarettes at baseline. Numbers in parentheses are nonmissing valid responses.
bSmoking status was defined as follows: Daily or occasional smokers had smoked within the past 30 days and described their usual behavior and smoking either daily (daily or almost every day) or occasional. Former smokers were required to have not smoked in the previous 30 days at the time of interview.
cPercentage estimates may not sum to 100% due to rounding.
Table 3 presents the characteristics of smokers who switched from daily to occasional smokers and further divides this group by subsequent smoking status at Time 3. These combinations of smoking status over Time 1 through Time 3 suggest the following behaviors: staged cessation happening more than 1 year (daily smoking, to occasional smoking, to abstinence); reduced smoking (daily to occasional and then remaining an occasional smoker); and rebounding (from daily to occasional, then back to daily smoking). Examination of Time 1 characteristics of these three groups revealed no statistically significant differences in demographic characteristics, prior quit attempts or supports, confidence, or initial intention to quit (all p values on 2df > .10). However, those who followed the pattern of rebounding back to daily smoking were roughly twice as likely as the other groups to have described themselves as very addicted at Time 1 (p value, 2df = .002). The only other statistically significant finding was a slightly lower number of cigarettes smoked at Time 1 by those who reduced to occasional smoking and remained there (p value, 2df = .003).
Table 3.
Characteristics of Selected Participantsa in the Ontario Tobacco Survey Panel Study With a Focus on Longitudinal Transitions Into, and Out of, Self-Reported Occasional Smoking Statusb
| Observed pattern of smoking status: Daily (D), occasional (O), or former (F; abstinence for at least 30 days) over three consecutive interviews | D-O-F (staged cessation) | D-O-O (reduced smoking) | D-O-D (rebound) | p value (2df)d |
|---|---|---|---|---|
| N of repeated measures observations (triads)a | 82 | 90 | 210 | |
| N cross-sectional observations (individuals)a | 76 | 80 | 204 | |
| Age | (n = 82) | (n = 89) | (n = 210) | |
| Mean | 38.0 | 39.4 | 41.5 | .205 |
| Sample SE | 2.19 | 3.05 | 1.49 | |
| Sex (%)c | (n = 82) | (n = 90) | (n = 210) | |
| Female | 54.2 | 34.3 | 44.5 | .117 |
| Male | 45.8 | 65.7 | 55.5 | |
| Education (%) | (n = 82) | (n = 89) | (n = 210) | |
| High school or less | 36.5 | 30.0 | 42.9 | .266 |
| More than high school | 63.5 | 70.0 | 57.1 | |
| Marital status (%) | (n = 81) | (n = 89) | (n = 210) | |
| Single | 52.2 | 54.7 | 43.1 | .301 |
| Married/common law | 47.8 | 45.3 | 56.9 | |
| Time since last cigarette (%) | (n = 82) | (n = 90) | (n = 210) | |
| Within past week | 100.0 | 100.0 | 100.0 | N/A |
| Within past month | 0.0 | 0.0 | 0.0 | |
| Within 6 months | 0.0 | 0.0 | 0.0 | |
| >since months prior | 0.0 | 0.0 | 0.0 | |
| Number of days smoked (prev. 30 days) | (n = 82) | (n = 90) | (n = 210) | |
| Mean | 28.2 | 23.9 | 28.6 | .003 |
| Sample SE | 0.52 | 1.43 | 0.35 | |
| Number of cigarettes per day | (n = 82) | (n = 90) | (n = 210) | |
| Mean | 8.9 | 8.1 | 11.4 | .003 |
| Sample SE | 0.86 | 1.00 | 0.76 | |
| Heaviness of smoking index | (n = 79) | (n = 86) | (n = 207) | |
| Mean | 1.3 | 1.0 | 1.9 | .002 |
| Sample SE | 0.21 | 0.21 | 0.15 | |
| Weekly pattern of reported smoking | (n = 82) | (n = 90) | (n = 210) | |
| Smoked weekends and weekdays | 100.0 | 99.4 | 99.6 | N/A |
| Weekday or weekend smokers | 0.0 | 0.6 | 0.4 | |
| Perceived addiction (%) | (n = 82) | (n = 89) | (n = 208) | |
| Less addicted (“somewhat” or “not at all”) | 64.0 | 66.0 | 41.3 | .002 |
| Very addicted | 36.0 | 34.0 | 58.7 | |
| Prior number of quit attempts (%) | (n = 79) | (n = 86) | (n = 200) | |
| None | 5.5 | 7.1 | 4.1 | .757 |
| One or more | 94.5 | 92.9 | 95.9 | |
| Quit intention (%) | (n = 82) | (n = 90) | (n = 210) | |
| No (incl. don’t know) | 38.3 | 48.0 | 33.4 | .203 |
| Yes | 61.7 | 52.0 | 66.6 | |
| Quitting confidence (%) | (n = 82) | (n = 90) | (n = 210) | |
| Less or uncertain confidence (incl. don’t know) | 26.6 | 18.7 | 28.2 | .354 |
| Fairly or very confident | 73.4 | 81.3 | 71.9 | |
| Smoking in the home (%) | (n = 82) | (n = 90) | (n = 208) | |
| Little or no exposure (less than monthly) | 73.6 | 73.4 | 69.5 | .786 |
| Regular exposure (at least monthly) | 26.4 | 26.6 | 30.5 | |
| Ever prior use of pharmacotherapy (%) | (n = 80) | (n = 85) | (n = 207) | |
| No | 52.8 | 50.4 | 39.8 | .266 |
| Yes | 47.2 | 49.6 | 60.2 | |
| Ever prior use of behavioral supports (%) | (n = 80) | (n = 85) | (n = 205) | |
| No | 76.4 | 67.0 | 59.3 | .104 |
| Yes | 23.6 | 33.0 | 401.7 |
Note. SE = standard error of the mean.
aThis analysis uses a repeated measures approach where one observation is a set of three consecutive complete interviews over the course of the Ontario Tobacco Survey (OTS) panel study (Waves 1–6). The analysis used 13,000 observations reflecting data from 4,352 unique participants in the OTS. All OTS panel study participants had smoked within 6 months at the baseline interview. This analysis was restricted to those who smoked 100+ lifetime cigarettes at baseline. Numbers in parentheses are nonmissing valid responses.
bSmoking status was defined as follows: Daily or occasional smokers had smoked within the past 30 days and described their usual behavior and smoking either daily (daily or almost every day) or occasional. Former smokers were required to have not smoked in the previous 30 days at the time of interview.
cPercentage estimates may not sum to 100% due to rounding.
dFor proportions, p value reflects a chi-square test for nonassociation across all three groups (2df) and for continuous measures, from a one-way analysis of variance for main effect by group (2df). Variance estimates, confidence intervals, and p values account for the nonindependence of observations.
DISCUSSION
Occasional or nondaily smokers make up an important proportion of the smoking population, which may be increasing in prevalence (Schane, Glantz, & Ling, 2009; Shiffman, 2009) or remaining steady despite declines in daily smoking (Shields, 2004). This study adds to growing understanding (Edwards et al., 2010; Shiffman, 2009; Shiffman et al., 2012) of occasional smokers as a mixed population including a small but persistent population of ongoing occasional smokers, as well as individuals who have transitioned from daily smoking to more intermittent smoking and may have difficulty achieving abstinence. This analysis also illustrates that changes in smoking behavior are not just determined by current smoking status and cigarette consumption but also by past changes in smoking status.
Our findings suggest the existence of a subset of occasional smokers who remain occasional smokers for relatively long periods of time with no apparent motivation to quit (here, as evidenced by lower intention to do so and fewer attempts). This group also (often) did not feel they were addicted or unable to quit. This suggests the need to identify public health strategies to motivate occasional smokers to quit altogether.
Our findings also show that occasional smokers who have recently switched from daily smokers include a subgroup of individuals who are motivated to quit, but find this difficult. This group was more likely to relapse back to daily smoking than quit altogether, and rebounders described themselves as more addicted at Time 1. Research is needed to identify the ideal strategies to help these smokers quit completely as most of the available evidence on cessation treatment is based on smokers with relatively high daily consumption, and most cessation trials have not even included nondaily or intermittent smokers (Fiore et al., 2000). The same full mix of treatment models for heavier smokers may be relevant for lower intake and occasional smokers as well. For example, in this same OTS panel study, nearly all smokers with low levels of consumption (fewer than 10 cigarettes/day) but using pharmacological support for cessation self-reported as being addicted to nicotine (Bondy, Diemert, McDonald, Victor, & Cohen, 2012).
It has been suggested that models of dependence requiring frequent nicotine administration are insufficient to explain ongoing occasional smoking (for discussion, see Shiffman et al., 2012). Risk of rebound in occasional smokers who do wish to quit may be associated with individual differences in risk of frequent relapse, despite ability to withdraw from nicotine. Several mechanisms for risk of relapse have been suggested, including cue reactivity (Perkins, 2009), impulsivity (Doran, Spring, McChargue, Pergadia, & Richmond, 2004), and social context including changes in social networks, which may occur when trying to achieve abstinence (Christakis & Fowler, 2008).
Research focused on occasional smokers is a challenge due to their small number within resources such as population surveys. This study had the advantages of deliberate oversampling of smokers within a large representative population sample (Bondy et al., 2006; Diemert et al., 2008), and the ability of the panel study design to capture a large number of episodes of occasional smoking status for analysis. Another challenge, in research on occasional smokers, is with measurement, both in terms of variable definitions for smoking status used in the literature and with the use of self-report measures designed primarily for daily smokers (Edwards et al., 2010). This study considered continuing occasional smokers as those who smoked less than daily over two interviews, which differs slightly from Shiffman et al. (2012) who considered “native” occasional smokers who had never smoked daily. Within our continuing occasional smokers the never daily smokers were similar in age and other characteristics aside from being more likely to be male (data not shown due to very restricted sample size). Future research focusing on occasional smokers should consider deliberate recruitment as done by Shiffman et al. (2012) as well as the formulation of measures specifically for lower consumption or nondaily smokers.
There is considerable interest in evidence regarding the benefits and risks of cutting down to quit as a strategy for cessation (Fagerstrom, 2005; Hughes & Carpenter, 2006). For example, Hyland et al. (2006) found that nondaily smokers were more likely to quit smoking. Falba, Jofre-Bonet, Busch, Duchovny, and Sindelar (2004) and Okuyemi, Thomas, Warren, Guo, and Ahluwalia (2010) found that daily smokers who reduced consumption first were more likely to stay abstinent. We focused on occasional (less than daily) smokers, a group less well understood and often excluded from cessation studies. Our findings resonate with research from Tindle and Shiffman (2011), who reported that occasional smokers, both converted from daily smokers and continuous occasional smokers, were unsuccessful in their quit attempts, despite low levels on common measures of dependence. Similarly, Cheong, Yong, and Borland (2007) reported that those who quit cold turkey were more likely to be smoke free for 1 month or more than those who gradually cut down to quit.
We were able to identify and follow a group of smokers who followed a pattern from daily to occasional smoking to abstinence. Our observations suggest that cutting down to nondaily smoking may increase the future likelihood of cessation in a manner similar to that observed among smokers who deliberately reduce their daily intake before trying to quit (Fagerstrom, 2005). However, the present study included no intervention or advice, so we provide no direct evidence on the effectiveness of guidance to cut down in individualized counseling. We also cannot determine if the shift in pattern from daily to occasional smoking was intended explicitly as staged cessation, nor were we able to obtain detailed information on the content of any advice they had received on strategies to quit. Regardless, it is an important observation that reducing to occasional smoking entailed a greater risk of return to daily smoking and lower chance of abstinence. In contrast, once a smoker reported abstinence at one interview, their chances of remaining a former smoker at the next interview were greater than 60%. Complete abstinence should be the ultimate goal as the longer this is maintained the greater the chances of becoming permanently smoke free.
FUNDING
The Ontario Tobacco Survey is an initiative of the Ontario Tobacco Research Unit, which receives funding from the Ontario Ministry of Health and Long-Term Care.
DECLARATIONS OF INTERESTS
None declared.
ETHICS
The Ontario Tobacco Survey received Research Ethics Board approvals from the University of Toronto and University of Waterloo.
The copyright line was changed from a standard license to an open access license on January 8, 2013, at the request of the author.
REFERENCES
- Bondy S., Brown K. S., Cohen J., Ferrence R., Garcia J., McDonald P. W, … Victor J. C. (2006). Development and design of the Ontario Tobacco Survey. Statistics Canada International Symposium Series - Proceedings. Symposium 2006: Methodological Issues in Measuring Population Health Ottawa, Ontario, Canada: Statistics Canada. [Google Scholar]
- Bondy S., Diemert L., McDonald P., Victor J., Cohen J. (2012). Is NRT being used by those for whom it is indicated? A prospective analysis in a population-based cohort of smokers. Chronic Diseases and Injuries in Canada, 33(1):19–28. [PubMed] [Google Scholar]
- Bondy S. J., Victor J. C., O’Connor S., McDonald P. W., Diemert L. M., Cohen J. E. (2010). Predictive validity and measurement issues in documenting quit intentions in population surveillance studies. Nicotine & Tobacco Research, 12, 43–52. 10.1093/ntr/ntp171 [DOI] [PubMed] [Google Scholar]
- Cheong Y., Yong H.-H., Borland R. (2007). Does how you quit affect success? A comparison between abrupt and gradual methods using data from the International Tobacco Control Policy Evaluation Study. Nicotine & Tobacco Research, 9, 801–810. [DOI] [PubMed] [Google Scholar]
- Christakis N. A., Fowler J. H. (2008). The collective dynamics of smoking in a large social network. The New England Journal of Medicine, 358, 2249–2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diemert L., Victor J. C., Bondy S. J. (2010a). Ontario Tobacco Survey Technical Report 1: Baseline data. Toronto, Ontario, Canada: Ontario Tobacco Research Unit; Retrieved from http://otru.org/research-evaluation/ontario-tobacco-survey/ [Google Scholar]
- Diemert L., Victor J. C., Bondy S. J. (2010b). Ontario Tobacco Survey Technical Report 2: Six month data. Toronto, Ontario, Canada: Ontario Tobacco Research Unit; Retrieved from http://otru.org/research-evaluation/ontario-tobacco-survey/ [Google Scholar]
- Diemert L. M., Bondy S. J., Brown K. S., Manske S. (in press). Young adult smoking cessation: Factors predicting quit attempts and sustained abstinence. American Journal of Public Health. 10.2105/AJPH.2012.300878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diemert L. M., Bondy S. J., Victor J. C., Cohen J. E., Brown K. S., Ferrence R, … Stephens T. (2008). Efficient screening of current smoking status in recruitment of smokers for population-based research. Nicotine & Tobacco Research, 10, 1663–1667. 10.1080/14622200802326152 [DOI] [PubMed] [Google Scholar]
- Doll R., Peto R., Boreham J., Sutherland I. (2004). Mortality in relation to smoking: 50 years’ observations on male British doctors. British Medical Journal, 328, 1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doran N., Spring B., McChargue D., Pergadia M., Richmond M. (2004). Impulsivity and smoking relapse. Nicotine & Tobacco Research, 6, 641–647. [DOI] [PubMed] [Google Scholar]
- Edwards S. A., Bondy S. J., Kowgier M., McDonald P. W., Cohen J. E. (2010). Are occasional smokers a heterogeneous group? An exploratory study. Nicotine & Tobacco Research, 12, 1195–1202. 10.1093/ntr/ntq168 [DOI] [PubMed] [Google Scholar]
- Fagerstrom K. O. (2005). Can reduced smoking be a way for smokers not interested in quitting to actually quit? Respiration, 72, 216–220. 10.1159/000084057 [DOI] [PubMed] [Google Scholar]
- Falba T., Jofre-Bonet M., Busch S., Duchovny N., Sindelar J. (2004). Reduction of quantity smoked predicts future cessation among older smokers. Addiction, 99, 93–102. [DOI] [PubMed] [Google Scholar]
- Fiore M. C., Bailey W. C., Cohen S. J., Dorfman S. F., Goldstein M. G., Gritz E. R, … Wewers M. E. (2000). Treating tobacco use and dependence: Clinical practice guideline (pp. 179). Bethesda, MD: U.S. Department of Health and Human Services. Public Health Service. [Google Scholar]
- Gerber Y., Myers V., Goldbourt U. (2012). Smoking reduction at midlife and lifetime mortality risk in men: A prospective cohort study. American Journal of Epidemiology, 175, 1006–1012. [DOI] [PubMed] [Google Scholar]
- Herd N., Borland R. (2009). The natural history of quitting smoking: Findings from the International Tobacco Control (ITC) Four Country Survey. Addiction, 104, 2075–2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes J. R., Carpenter M. J. (2006). Does smoking reduction increase future cessation and decrease disease risk? A qualitative review. Nicotine & Tobacco Research, 8, 739–749. [DOI] [PubMed] [Google Scholar]
- Hyland A., Borland R., Li Q., Yong H.-H., McNeill A., Fong G, … Cummings K. M. (2006). Individual-level predictors of cessation behaviors among participants in the International Tobacco Control (ITC) Four Country Survey. Tobacco Control, 15(Suppl. III)iii83–iii94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hymowitz N., Cummings K. M., Hyland A., Lynn W. R., Pechacek T. F., Hartwell T. D. (1997). Predictors of smoking cessation in a cohort of adult smokers followed for five years. Tobacco Control, 6(Suppl. 2)S57–S62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ip D. T., Cohen J. E., Bondy S. J., Chaiton M. O., Selby P., Schwartz R, … Ferrence R. (2012). Do components of current ‘hardcore smoker’ definitions predict quitting behaviour? Addiction, 107, 434–440. 10.1111/j.1360-0443.2011.03674.x [DOI] [PubMed] [Google Scholar]
- Mecredy G., Chaiton M. O., Bondy S. (2011). Ontario Tobacco Survey. Follow-up 4 summary report: Twenty-four month data Toronto, Ontario, Canada: Ontario Tobacco Research Unit. [Google Scholar]
- National Advisory Group on Monitoring and Evaluation (2006). Indicators for monitoring tobacco control: A resource for decision-makers, evaluators and researchers Toronto, Ontario, Canada: Canadian Tobacco Control Research Initiative (CTCRI). [Google Scholar]
- Okuyemi K. S., Thomas J. L., Warren J., Guo H., Ahluwalia J. S. (2010). Relationship between smoking reduction and cessation among light smokers. Nicotine & Tobacco Research, 12, 1005–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins K. A. (2009). Does smoking cue-induced craving tell us anything important about nicotine dependence? Addiction, 104, 1610–1616. [DOI] [PubMed] [Google Scholar]
- Pierce J. P., Farkas A. J., Gilpin E. A. (1998). Beyond stages of change: The quitting continuum measures progress towards successful smoking cessation. Addiction, 93, 277–286. 10.1046/j.1360-0443.1998.93227711.x [DOI] [PubMed] [Google Scholar]
- Pierce J. P., Gilpin E. A., Emery S. L., White M. M., Rosbrook B., Berry C. C. (1998). Has the California tobacco control program reduced smoking? [Erratum appears in JAMA 1999 Jan 6;281(1):37]. Journal of the American Medical Association, 280, 893–899. 10.1001/jama.280.10.893 [DOI] [PubMed] [Google Scholar]
- Schane R. E., Glantz S. A., Ling P. M. (2009). Nondaily and social smoking: An increasingly prevalent pattern. Archives of Internal Medicine, 169, 1742–1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shields M. (2004). A step forward, a step back: smoking cessation & relapse. Healthy today, healthy tomorrow? Findings from the National Popuation health Survey. Statistics Canada, Catalogue 82–618 (Vol. 1(1)) Ottawa, Ontario, Canada: Statistics Canada. [Google Scholar]
- Shiffman S. (2009). Light and intermittent smokers: Background and perspective. Nicotine & Tobacco Research, 11, 122–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S., Tindle H., Li X., Scholl S., Dunbar M., Mitchell-Miland C. (2012). Characteristics and smoking patterns of intermittent smokers. Experimental and Clinical Psychopharmacology. 10.1037/a0027546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tindle H. A., Shiffman S. (2011). Smoking cessation behavior among intermittent smokers versus daily smokers. American Journal of Public Health, 101, e1–e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (2000). Reducing tobacco use: A report of the Surgeon General Atlanta, GA: U.S. Centers for Disease Control and Prevention. [Google Scholar]