Abstract
Many believe that the “boarding” of emergency department (ED) patients awaiting inpatient beds compromises quality of care. To better study the quality of care of boarded patients, one should identify and understand the mechanisms accounting for any potential differences in care. This paper present a conceptual boarding “structure-process-outcome” model to help assess quality of care provided to boarded patients, and to aid in recognizing potential solutions to improve that quality, if it is deficient. The goal of the conceptual model is to create a practical framework on which a research and policy agenda can be based to measure and improve quality of care for boarded patients.
INTRODUCTION
Concern about the quality of medical care in the United States has increased over the past 20 years.1,2 Within emergency medicine, many believe that the “boarding” of emergency department (ED) patients awaiting inpatient beds compromises quality of care.3 The Institute of Medicine (IOM) in 2006 reported that “…boarding not only compromises the patient’s hospital experience, but adds to an already stressful work environment, enhancing the potential for errors, delays in treatment, and diminished quality of care.”4 Further, authors recommended hospitals end boarding, except in extreme cases. The American College of Emergency Physicians (ACEP) board of directors emphasizes that the ED should not be used as an extension of inpatient units for admitted patients, contending boarding adversely affects quality and access to care.5 Others consider causes and consequences of ED boarding one of the most important areas for immediate research.6 Literature exists explaining why boarding occurs, and presenting innovations to try to decrease it,3,4,7–14 but to our knowledge, no study has yet examined the general belief that boarded care is likely to be of lower quality than inpatient unit care. Intuitively, while it may be reasonable to believe that boarding leads to lower quality, research should confirm this association and determine its magnitude. While there may be a time when boarding does not exist, there is merit to examining how to deliver quality of care to boarded patients, and to mitigate any negative consequences of boarding until its elimination.
Determining whether boarding, per se, compromises care may be easier through identifying and understanding the mechanisms accounting for any potential differences in care. Such a theoretical approach motivated the development of the “input, throughput, output” model by Asplin and colleagues that has helped researchers and policymakers understand the causes and consequences of ED crowding.6 A similar model is needed to facilitate a more systematicway of assessing quality of care for boarded patients.
The topics of boarding and ED crowding are, of course, inter-related. The Government Accountability Office (GAO) stated that the main contributor to ED crowding is the inability to transfer patients to inpatient units once they are admitted.9 We currently know that ED crowding compromises care, being associated with increased mortality,15 delayed door-to-thrombolysis for myocardial infarction,16 worse pain control,17 and delays in antibiotic administration.18 Thus boarding, as it leads to ED crowding, is likely to compromise care. However, the question of whether and why boarding compromises care for boarded patients independently of crowding has not been adequately addressed.
Research on quality of care for boarded patients is challenging. There is no standard definition of what constitutes high quality of care for these patients. The IOM’s dimensions of quality of care include mortality and morbidity, cost and cost-effectiveness, and patient-centered outcomes such as quality of life and satisfaction.19,20 However, studying outcomes alone would ignore the causal mechanisms, making it difficult for policymakers to design interventions to improve quality. Also, multiple mechanisms may lead to compromised quality of care for boarded patients.
A conceptual model that outlines such potential mechanisms is important for organizing research as well as for designing more specific solutions to complement the current focus on how to reduce boarding itself. Currently, no conceptual model exists, potentially hindering the understanding of boarding and its consequences. This article proposes a conceptual model that breaks down the main question of how quality of care may be compromised into more manageable, discrete components. After a discussion of boarding, we present our model’scomponents and describe how they can be used to frame research.
Definition of Boarding
A lack of consensus exists on the definition of unacceptable boarding times. Boarding has commonly been understood as referring to the time a patient spends in the ED after a bed request has been made.6,9,21 In 2006, participants in the ED Performance Measures and Benchmarking Summit defined “boarding” as the process of holding patients in the ED for extended periods of time. Boarded patients were defined as those for whom the time interval between decision to admit and physical departure of the patient from the ED (decision-to-ED-departure time) exceeds 120 minutes.22 However, these binary cutoffs are not evidence-based.
The Frequency and Determinants of Boarding
Boarding is widespread. In a 2002 GAO survey, 31% of responding hospitals reported that three-fourths of patients spent two hours or more boarding in the ED; nearly 20% reported patients boarding for eight hours or more.9 In an ACEP survey of U.S. ED directors in 2005, 16% reported having more than 10 boarded patients per day.23
Several causes contribute to the high prevalence of boarding: ED visits rose by 10.8% from 2001–2006,24 and ED admissions to hospitals increased by 13% from 1993–2003.4 At the same time, 703 hospitals and 425 hospital EDs closed in response to cost-cutting measures.4 The decision on how to allocate the scant inpatient bed resource between the ED and other sources of inpatient admissions to best enhance revenue generation is also likely to play a role. The literature is mixed on the financial effects of ED admissions.9,25,26 Overall, it is likely that profitability of boarding depends on each hospital’s patient pool and the patients’ insurance status.27 Other contributors to boarding include hospital-wide factors such as inadequate or inflexible nurse-to-patient staffing ratios, delays in patient discharges, or increased need for isolation precautions.6,9,28 If ED visits continue to increase without an expansion of the number of hospital beds, boarding will likely be more prevalent. Hence, there is increasing need to assess the quality of care these patients receive.
CONCEPTUAL MODEL
To assess the quality of care for boarded patients, we used the “structure-process-outcome” framework described by Donabedian.29 His three-part approach makes quality assessment possible assuming structure (e.g. attributes of material or human resources and organizational structure) influences process (what is actually done in giving and receiving care), which influences outcome (e.g. health status).29 We chose Donabedian’s model as it is widely used and allows both researchers and policymakers to conceptualize the underlying mechanisms that may contribute to poor quality of care for boarded patients. We considered focusing only on outcomes, but such focus fails to give insight into the location of the deficiencies or strengths to which the outcome might be attributed.30 If outcome criteria are credible, it should be demonstrated that differences in outcome will result if the processes of care are altered. Similarly, if quality of care criteria based only on structure are to be credible, it should be shown that variations in that structure lead to differences in outcome.31 A measure of quality of care that includes all important meanings of the concept under consideration is more valid than one that only includes one of these dimensions.32 On the other hand, disadvantages of Donabedian’s model include the difficulty in establishing the relationship between structure, process, and outcome.30 Furthermore, there may be difficulty determining whether some factors are strictly part of structure and/or process or outcomes, as overlap between them may exist.
To develop the model, we started with the structure-process-outcome framework; we then incorporated other quality domains such as the IOM quality measures. We added further components that had face validity based on clinical and research experience. All co-authors participated in the development of the model. The model was reviewed by health services researchers not involved in its formulation.
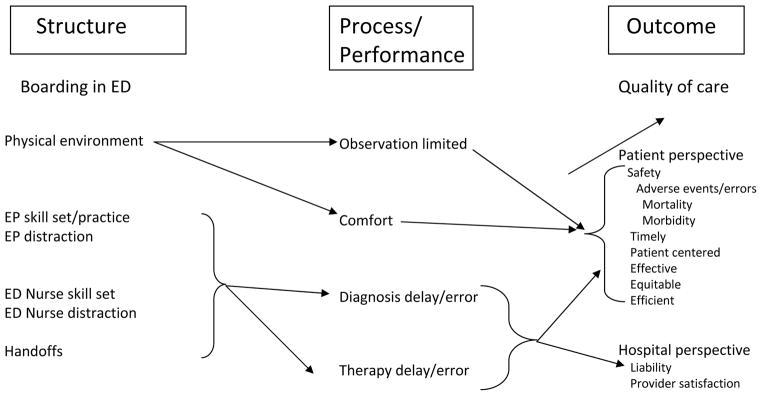
To summarize our boarding model, we propose that impediments posed by structure/organization (i.e. physical environments, provider skill sets/practice, distractions, and handoffs inherent in providing care to boarded patients) may compromise processes (such as patient observation, comfort, diagnosis, and therapy). These structural/organizational and process/performance weaknesses may ultimately lead to poor outcomes (i.e. the IOM six components of quality of care, liability, provider satisfaction, profit/efficiency, and access) from the patient and hospital administrator perspectives (Figure 1).19 The following sections describe our model in detail.
Figure 1.
Structure
Care for boarded patients and that provided on inpatient units involves inherent structural differences. Structure, according to Donabedian, can be thought of not only as the physical setting in which the care takes place, but also the organization of care and the qualifications of the care providers.30 Boarded patients are often placed in hallways to make their ED rooms available for new or more unstable patients, and may be subjected to disruptive and unpredictable fluctuations in environmental noise by the high traffic through the ED. Hallway patients may also be taken off central cardiac monitoring. Furthermore, ED design frequently features high visibility for instant observation of changes in patient stability. This can compromise patient privacy, especially if the patient is in a hallway or separated from other gurneys only by thin curtains.33 Emergency physicians (EPs) and nurses focus more on stabilization, disposition, and preliminary diagnosis than on inpatient management; essentially their skill set does not include the management of boarded patients.34 Boarded patients may hold lower priority for ED staff distracted by new patients. Finally, more handoffs between EPs may occur than on inpatient services as inpatient admitting physicians usually follow patients throughout their admission.35,36 These structural differences may explain why boarded patientscould experience compromised quality of care.
Process
Many potential causal pathways link the above structure with ways that processes can be compromised for boarded patients. Our model highlights potential problems with observation, comfort, diagnosis, and therapy (Figure 1). First, observation of boarded patients in a hallway may be compromised, especially in terms of arrhythmias missed due to the structural lack of central cardiac monitoring. Second, boarded patients may find comfort compromised if they are subjected to a noisy environment, or lacking privacy. Third, handoffs and distracted ED staff working outside their skill sets may lead to delays or errors in diagnosis and/or therapy from a host of issues including delayed or omitted laboratory testing, other diagnostic testing, inpatient consultations not commonly ordered from the ED, medications, or procedures.
Outcome
Examining structure and process measures is important because they ultimately can affect the quality of care outcome from the viewpoint of the patient and hospital administrator (Figure 1). For patients, we chose to define quality according to the IOM six components of quality of care: safety, timeliness, patient-centeredness, effectiveness, equitability, and efficiency.19 Errors or delays in diagnosis and treatment can compromise all six components. Poor monitoring, delays, and errors may compromise patient safety. Decreased comfort and delays in diagnosis/therapy reflect lack of patient-centeredness. Questions of inequity arise if boarded patients wait because inpatient beds are reserved for more profitable patients. Finally, delays in diagnosis and therapy may lead to increased hospital length of stay (LOS), thereby compromising efficiency. Any patient outcomes study should account for individual patient characteristics such as age and comorbidities.
From the point of view of the hospital administrator, minimizing errors and delays in diagnosis and therapy, aside from improving quality of care, can also minimize liability for the department and staff. Additionally, working outside skill sets and continuous distractions from lack of resources can lead to decreased staff satisfaction,37,38 potentially causing burnout and staff attrition.
Model-driven research on quality of care for boarded patients
Our model attempts to illustrate how certain structural problems inherent in providing care to boarded patients can affect processes and lead to poor outcomes. Studies need to demonstrate whether such relationships exist. We searched PubMed using terms (“emergencies” OR “emergency” AND “department” AND “boarding”), which yielded 64 articles. We then searched the references of those articles to identify other literature that may have been relevant. We included articles that examined ED processes or outcomes. We excluded articles that only reviewed ED crowding or flow. We do not review all the literature here, but mention several studies that illustrate the applicability of our model and to identify gaps in the literature
Regarding structure, Guthrie et al. and Garson et al. surveyed a convenience sample of patients and showed that a majority of them would prefer boarding in an inpatient hallway to boarding in the ED.39,40
In terms of process measures, Liu et al. found 28% of patients (42/151) had an undesirable event while boarding, largely due to missed home medications.41 The study was limited by a small sample size and lacked comparison with nonboarded patients. Diercks et al., in a volunteer cohort analysis of 42,780 patients with acute coronary syndrome (ACS), found that patients with longer ED LOS were less likely to receive ACS medications.42 However, they did not examine locations where medical therapies were given and therefore could not attribute medication delays to ED-based health care providers or system failures.
In terms of patient-oriented outcomes, few studies have specifically examined boarding, with most focusing on ED LOS, where most suggest poorer outcomes with increasing ED LOS.42–45 While boarding is a component of ED LOS, we believe that boarding time is sufficiently distinct to warrant separate analysis. One study by Viccellio et al. appears to show that boarding in inpatient hallways (at least for selected patients) is safe, with mortality rates and intensive care unit transfers being higher in standard bed admissions than in patients admitted to hallway beds, although this may have been due to patient complexity and acuity rather than a hallway benefit.46
There may be publication bias in that only studies showing that boarding is associated with negative processes or outcomes are published. Future studies may show that boarding is not associated with poor outcomes.
The literature on boarding is just emerging. We foresee researchers using our conceptual model to design future studies. For example, one could analyze how many handoffs boarded patients undergo (structure) to see if it relates to diagnosis/therapy delays and errors (process), ultimately leading to adverse events (outcomes). We list other potential topics in our Table. While a large multicenter study comparing preventable adverse events among a cohort of ED boarded patients compared to a similar cohort of patients who did not board in the ED might be ideal, there is ample opportunity at this early stage for researchers to conduct smaller qualitative and quantitative studies that can begin to analyze how the components of structure and process relate to outcome. Multiple studies will likely be needed to ultimately determine how to weightstructural and process components in terms of their importance as causal factors.
LIMITATIONS
Our conceptual model has limitations. It was developed by a small group of researchers and doesnot represent a large expert panel consensus; hence, this is not a typical consensus paper. Moreover, the model does not address the causes of boarding or its solutions, as we thought this would detract from our central message. We did not quantify the importance of each component in the model as this would largely rely on value judgments. We did not explicitly include case mix in our model because it does not provide insights into how boarding specifically may compromise outcomes, although there may be differences in outcomes in boarded patients, based on the complexity and severity of their disease. Future outcome studies of boarding should include case mix adjustment, since pre-existing comorbidities and severity of illness are powerful confounders in studying outcomes. We also did not address the potential limitations of inpatient resources in some hospitals. Boarding may be safer for some patients in certain hospitals where EPs are the only physicians present overnight. Likewise, patients may have quicker access to radiology tests while boarding. Furthermore, we focused on the boarded patient herself or himself, to avoid creating an overly complex model, acknowledging that queuing of these patients leads to a cascade of outcomes that affects other ED patients, such as crowding and ambulance diversion. Finally, placement of certain factors in our model is ambiguous. For some, delays in treatment would be considered an outcome, whereas others believe that delays are only process measures that can lead to a poor outcome. While we attempted to place factors according to Donabedian’s definition, we acknowledge there may be overlap in the three areas.
CONCLUSIONS
We believe that the boarding “structure-process-outcome” conceptual model provides a practical framework for a research agenda that can ultimately assess whether boarded patients receive lower quality of care and have worse outcomes. While some may advocate elimination of boarding completely,4 this is not likely to occur in the near future. In the meantime, it is important to understand the mechanisms that link structure and processes to potential poor outcomes for boarded patients so that targeted, evidence-based solutions can be implemented. Testing the relationship between the proposed model components will be vital to assessing whether the quality of care provided to boarded patients is compromised, and to creating effective solutions.
Table.
Potential research topics using boarding “structure-process-outcome model”
| Structure | Process | Outcome |
|---|---|---|
| Boarding in ED | Decreased comfort | Decreased patient satisfaction |
| Patient with rate-controlled atrial fibrillation boarding in ED | Missed or delayed administration of chronic atrial fibrillation medications | Increased frequency of rapid atrial fibrillation |
| Increased number of handoffs for patients boarding in ED | Perception of inaccurate handoff by both ED and receiving inpatient team | Decreased provider satisfaction |
| Elderly patients boarding in ED hallway | Increased noise | Increased frequency of delirium/disorientation, increased hospital length of stay |
| ED staff working outside skill set | Perception of providing care outside their scope of practice | Decreased provider satisfaction |
| Prolonged boarding in ED | No deep vein thrombosis (DVT) prevention | Increased frequency of DVT |
Acknowledgments
The authors would like to thank Alice Storey and Donald Halstead for their assistance in the preparation of the manuscript.
Footnotes
Reprints not available from the authors.
Disclosures: Dr. Sun received support from the UCLA Older Americans Independence Center, NIH/NIA Grant P30-AG028748. The content does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
References
- 1.Chassin MR, Galvin RW and the National Roundtable on Health Care Q. The urgent need to improve health care quality: Institute of Medicine National Roundtable on Health Care Quality. JAMA. 1998;280(11):1000–5. doi: 10.1001/jama.280.11.1000. [DOI] [PubMed] [Google Scholar]
- 2.McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–45. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 3.American College of Emergency Physicians. [Accessed Jan 10, 2011.];Report on Boarding Emergency Department Crowding: High-Impact Solutions. Available at: www.acep.org/WorkArea/DownloadAsset.aspx?id=50026.
- 4.Institute of Medicine. Hospital-based emergency care at the breaking point. Washington DC: National Academies Press; 2006. [Google Scholar]
- 5.American College of Emergency Physicians. [Accessed Jan 10, 2011.];Boarding of Admitted and Intensive Care Patients in the Emergency Department. doi: 10.1016/s0196-0644(01)70038-8. Available at: http://www.acep.org/practres.aspx?id=29132. [DOI] [PubMed]
- 6.Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA., Jr A conceptual model of emergency department crowding. Ann Emerg Med. 2003;42(2):173–80. doi: 10.1067/mem.2003.302. [DOI] [PubMed] [Google Scholar]
- 7.Greene J. Emergency department flow and the boarded patient: how to get admitted patients upstairs. Ann Emerg Med. 2007;49(1):68–70. doi: 10.1016/j.annemergmed.2006.11.020. [DOI] [PubMed] [Google Scholar]
- 8.Asplin BR. Hospital-based emergency care: a future without boarding? Ann Emerg Med. 2006;48(2):121–5. doi: 10.1016/j.annemergmed.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 9.Government Accountability Office. [Accessed Jan 10, 2010.];Hospital emergency departments crowded conditions vary among hospitals and communities. 2003 GAO-03-460. Available at: http://www.gao.gov/new.items/d03460.pdf.
- 10.Moloney ED, Bennett K, O’Riordan D, Silke B. Emergency department census of patients awaiting admission following reorganisation of an admissions process. Emerg Med J. 2006;23(5):363–7. doi: 10.1136/emj.2005.028944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McConnell KJ, Richards CF, Daya M, Bernell SL, Weathers CC, Lowe RA. Effect of increased ICU capacity on emergency department length of stay and ambulance diversion. Ann Emerg Med. 2005;45(5):471–8. doi: 10.1016/j.annemergmed.2004.10.032. [DOI] [PubMed] [Google Scholar]
- 12.Cameron P, Scown P, Campbell D. Managing access block. Aust Health Rev. 2002;25(4):59–68. doi: 10.1071/ah020059. [DOI] [PubMed] [Google Scholar]
- 13.Wiler JL, Gentle C, Halfpenny JM, et al. Optimizing emergency department front-endoperations. Ann Emerg Med. 2009;55(2):142–60. doi: 10.1016/j.annemergmed.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 14.Dickson EW, Anguelov Z, Vetterick D, Eller A, Singh S. Use of lean in the emergency department: a case series of 4 hospitals. Ann Emerg Med. 2009;54(4):504–10. doi: 10.1016/j.annemergmed.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 15.Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 2006;184(5):208–12. doi: 10.5694/j.1326-5377.2006.tb00416.x. [DOI] [PubMed] [Google Scholar]
- 16.Schull MJ, Vermeulen M, Slaughter G, Morrison L, Daly P. Emergency department crowding and thrombolysis delays in acute myocardial infarction. Ann Emerg Med. 2004;44(6):577–85. doi: 10.1016/j.annemergmed.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Pines JM, Hollander JE. Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51(1):1–5. doi: 10.1016/j.annemergmed.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 18.Fee C, Weber EJ, Maak CA, Bacchetti P. Effect of emergency department crowding on time to antibiotics in patients admitted with community-acquired pneumonia. Ann Emerg Med. 2007;50(5):501–9. doi: 10.1016/j.annemergmed.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 19.Institute of Medicine (U.S.). Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academies Press; 2001. [Google Scholar]
- 20.Kohn LT, Corrigan J, Donaldson MS. To err is human: building a safer health system. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 21.Kellermann AL. Crisis in the emergency department. N Engl J Med. 2006;355(13):1300–3. doi: 10.1056/NEJMp068194. [DOI] [PubMed] [Google Scholar]
- 22.Welch SJ, Augustine J, Camargo CA, Jr, Reese C. Emergency department performance measures and benchmarking summit. Acad Emerg Med. 2006;13:1074–80. doi: 10.1197/j.aem.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 23.Benjamin Vanlandingham BM, Tubbs Robert. [Accessed Jan 10, 2011.];On-call specialist coverage in US emergency departments: ACEP survey of emergency department directors. 2006 www.acep.org/workarea/downloadasset.aspx?id=37944.
- 24.Government Accountability Office. [Accessed Jan 10, 2011.];Crowding continues to occur, and some patients wait longer than recommended time frames. 2009 GAO-09–347. Available at: http://www.gao.gov/new.items/d09347.pdf.
- 25.Handel DA, John McConnell K. The financial impact of ambulance diversion on inpatient hospital revenues and profits. Acad Emerg Med. 2009;16:29–33. doi: 10.1111/j.1553-2712.2008.00242.x. [DOI] [PubMed] [Google Scholar]
- 26.Henneman PL, Lemanski M, Smithline HA, Tomaszewski A, Mayforth JA. Emergency department admissions are more profitable than non-emergency department admissions. Ann Emerg Med. 2009;53(2):249–55. doi: 10.1016/j.annemergmed.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 27.Pines JM, Heckman JD. Emergency department boarding and profit maximization for high-capacity hospitals: challenging conventional wisdom. Ann Emerg Med. 2009;53(2):256–8. doi: 10.1016/j.annemergmed.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 28.Asplin BR, Magid DJ. If you want to fix crowding, start by fixing your hospital. Ann Emerg Med. 2007;49(3):273–4. doi: 10.1016/j.annemergmed.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 29.Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260(12):1743–8. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- 30.Donabedian A. Evaluating the quality of medical care (reprint) Milbank Q. 2005;83(4):691–729. doi: 10.1111/j.1468-0009.2005.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brook RH, McGlynn EA, Cleary PD. Quality of health care. Part 2: measuring quality of care. N Engl J Med. 1996;335(13):966–70. doi: 10.1056/NEJM199609263351311. [DOI] [PubMed] [Google Scholar]
- 32.Shi L. Health services research methods. Albany, NY: Delmar Publishers; 1997. [Google Scholar]
- 33.Lin Y-K, Lin C-J. Factors predicting patients’ perception of privacy and satisfaction for emergency care. Emerg Med J. 2010 doi: 10.1136/emj.2010.093807. [DOI] [PubMed] [Google Scholar]
- 34.Hockberger RS, Binder LS, Chisholm CD, et al. The model of the clinical practice of emergency medicine: a 2-year update. Ann Emerg Med. 2005;45(6):659–74. doi: 10.1016/j.annemergmed.2005.01.029. [DOI] [PubMed] [Google Scholar]
- 35.Horwitz LI, Krumholz HM, Green ML, Huot SJ. Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med. 2006;166(11):1173–7. doi: 10.1001/archinte.166.11.1173. [DOI] [PubMed] [Google Scholar]
- 36.Cheung DS, Kelly JJ, Beach C, et al. Improving handoffs in the emergency department. Ann Emerg Med. 2010;55(2):171–80. doi: 10.1016/j.annemergmed.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 37.Rondeau KV, Francescutti LH. Emergency department overcrowding: the impact of resource scarcity on physician job satisfaction. J Healthcare Manag. 2005;50(5):327–40. [PubMed] [Google Scholar]
- 38.Jeanmonod R, Boyd M, Loewenthal M, Triner W. The nature of emergency department interruptions and their impact on patient satisfaction. Emerg Med J. 2010;27:376–9. doi: 10.1136/emj.2008.071134. [DOI] [PubMed] [Google Scholar]
- 39.Guthrie BD, King WD, Monroe KW. Parental preferences for boarding locations when a children’s hospital exceeds capacity. Ann Emerg Med. 2009;53(6):762–6. doi: 10.1016/j.annemergmed.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 40.Garson C, Hollander JE, Rhodes KV, Shofer FS, Baxt WG, Pines JM. Emergency department patient preferences for boarding locations when hospitals are at full capacity. Ann Emerg Med. 2008;51(1):9–12. doi: 10.1016/j.annemergmed.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 41.Liu SW, Thomas SH, Gordon JA, Hamedani AG, Weissman JS. A pilot study examining undesirable events among emergency department-boarded patients awaiting inpatient beds. Ann Emerg Med. 2009;54(3):381–5. doi: 10.1016/j.annemergmed.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 42.Diercks DB, Roe MT, Chen AY, et al. Prolonged emergency department stays of non-ST-segment-elevation myocardial infarction patients are associated with worse adherence to the American College of Cardiology/American Heart Association guidelines for management and increased adverse events. Ann Emerg Med. 2007;50(5):489–96. doi: 10.1016/j.annemergmed.2007.03.033. [DOI] [PubMed] [Google Scholar]
- 43.Richardson DB. The access-block effect: relationship between delay to reaching an inpatient bed and inpatient length of stay. Med J Aust. 2002;177(9):492–5. doi: 10.5694/j.1326-5377.2002.tb04917.x. [DOI] [PubMed] [Google Scholar]
- 44.Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35(6):1477–83. doi: 10.1097/01.CCM.0000266585.74905.5A. [DOI] [PubMed] [Google Scholar]
- 45.Pines JM, Iyer S, Disbot M, Hollander JE, Shofer FS, Datner EM. The effect of emergency department crowding on patient satisfaction for admitted patients. Acad Emerg Med. 2008;15:825–31. doi: 10.1111/j.1553-2712.2008.00200.x. [DOI] [PubMed] [Google Scholar]
- 46.Viccellio A, Santora C, Singer AJ, Thode HC, Jr, Henry MC. The association between transfer of emergency department boarders to inpatient hallways and mortality: a 4-year experience. Ann Emerg Med. 2009;54(4):487–91. doi: 10.1016/j.annemergmed.2009.03.005. [DOI] [PubMed] [Google Scholar]


